Abstract
Context
Trunk control is essential to engage in activities of daily living. Measuring trunk strength and function in persons with spinal cord injury (SCI) is difficult. Trunk function has not been studied in non-traumatic SCI (NTSCI).
Objectives
To characterize changes in trunk strength and seated functional reach in individuals with NTSCI during inpatient rehabilitation. To determine if trunk strength and seated reach differ between walkers and wheelchair users. To explore relationships between trunk and hip strength and seated functional reach.
Design
Observational study.
Setting
Two SCI rehabilitation facilities.
Participants
32 subacute inpatients (mean age 48.0 ± 15.4 years).
Outcome measures
Isometric strength of trunk and hip and function (Multidirectional Reach Test: MDRT) were assessed at admission and within 2 weeks of discharge. Analysis of variance was conducted for admission measures (MDRT, hip and trunk strength) between walkers and wheelchair users. Changes in MDRT, hip and trunk strength were evaluated using parametric and non-parametric statistics. The level of association between changes in values of MRDT and strength was also examined.
Results
Significant differences between walkers and wheelchair users were found for strength measures (P < 0.05) but not for MDRT. Left- and right-sided reaches increased in wheelchair users only (P < 0.05). Associations between changes in hip strength, trunk strength, and reach distance were found (R = 0.67–0.73).
Conclusion
In clinical settings, it is feasible and relevant to assess trunk, hip strength, and MRDT. Future studies require strategies to increase the number of participants assessed, in order to inform clinicians about relevant rehabilitation interventions.
Keywords: Rehabilitation, Trunk control, Function, Muscle strength, Non-traumatic spinal cord injury
Introduction
Individuals with non-traumatic spinal cord injury (NTSCI) present as a unique population among the spinal cord population. NTSCI can result from multiple etiologies including vascular impairment, infection, malignant and benign tumors, spinal stenosis, transverse myelitis, and syringomyelia. Due to the chronicity of the condition, the level of adaptation in response to the sensory and motor decline over time varies considerably among the different etiologies. Surgical intervention in NTSCI is considered when the neuropathology is progressing to life-threatening levels and the decline in sensory and motor function can no longer meet that required for their daily needs. It is well documented that individuals with NTSCI are older, more likely to be female, to suffer from paraplegia, present with less physical disability on admission, require shorter term inpatient rehabilitation,1–3 and present with higher AIS scores than those with traumatic SCI. While individuals with NTSCI have a different etiology of disease, they have been reported to have similar levels of walking function at discharge as measured by functional independence measure (FIM) subscores3 and walking outcomes.4 What is unclear is whether those with different mobility status at discharge have different neurological recovery in trunk function and a differing rehabilitation, i.e. length of stay.
Upright trunk stability is a necessary component in engaging in functional activities including feeding, dressing, and transferring.5,6 Proprioceptive input in addition to adequate synergistic recruitment and force-generating capabilities of the trunk, hip, and lower extremity muscles is necessary to maintain adequate trunk stability.7 Furthermore, prior to the initiation of upper extremity activities in the sitting position, anticipatory activity of the erector spinae and abdominal muscles is required to stabilize the trunk.8
There is increasing literature about trunk stability in SCI. However, most of the studies have focused on the traumatic SCI population and have been tested in the laboratory setting using kinematic or kinetic paradigms. In individuals with traumatic SCI, greater dynamic and static stability has been found in individuals with lower thoracic SCI when compared with those with high thoracic SCI.5,6 Decreased ability to recruit the rectus abdominis, transverse abdominis, external and internal obliques, quadratus lumborum, and erector spinae muscles may lead to compensatory strategies using the non-postural muscles including latissimus dorsi, trapezius, pectoralis major, neck, upper and lower extremity muscles.5,9 It has also been suggested that individuals following SCI develop a new central postural control process in the maintenance of sitting stability.10 With increased trunk instability, the individual with SCI may engage in a posterior pelvic tilt and an increase in thoracolumbar kyphosis. These compensatory strategies increase the base of support thereby improving sitting balance11,12 resulting in increased functional reach.13
Hand-held dynamometry of the upper and lower extremity muscles has been shown to have high inter-class correlation coefficient (ICC = 0.86–0.97) and intra-rater (ICC = 0.89–0.97) reliability in individuals with neuropathic weakness.14 Hand-held dynamometry of the upper extremity has also been evaluated in individuals with paraplegia and tetraplegia during the course of rehabilitation and up to 15 months post-rehabilitation15 and Drolet et al.15 found a high variability in upper extremity recovery, with improving upper extremity strength up to 15 months post-rehabilitation. Not surprisingly, a greater variability in recovery was found for individuals with tetraplegia compared with paraplegia.15. Assessment of trunk muscle strength in SCI has demonstrated high inter- (ICC 0.96–0.99) and high intra-rater (ICC 0.79–0.99) reliability and can be used to evaluate postural muscle strength.16
The seated Multidirectional Reach Test (MDRT) has been used by several researchers as a surrogate measure of postural control in individuals with SCI7,17 and older adults.18 The MDRT distance has been shown to be a reliable and valid indicator of stability limits in healthy community dwelling older adults18 and individuals with SCI.17 Concomitant measures during reach tests include center of pressure (COP), limits of stability,7 time to contact the virtual stability boundary,19 hand/wrist excursion,17,18 and trunk excursion.7 Field-Fote and Ray17 found a significant correlation (r ≥ 0.70) between COP excursion and seated reach distance in the forward, backward, and leftward reaching, using the wrist as the distal marker. Gauthier et al.7 found that the overall stability index in the seated position was best predicted by anterior reaches, left posterior lateral reaches, and right reaches (R2 = 0.98, P < 0.001). However, these measures present some challenges in the clinical setting. Mainly, measuring COP excursion requires specialized laboratory equipment which limits its applicability, and using the wrist/hand as reference marker for reach distance is influenced by the ability to maintain upper extremity position and may overestimate or underestimate the contribution of the trunk.
To date, there are limited studies examining trunk function (strength and reach distance) in individuals with SCI.5,7,9,17 Moreover, we were unable to find published studies that have documented changes in trunk function following NTSCI, differences between wheelchair users and walkers, and the relationship between trunk muscle strength and seated postural control. Understanding recovery of the trunk function in individuals with NTSCI during rehabilitation would enable clinicians to determine appropriate rehabilitation potential enabling timely intervention to achieve realistic rehabilitation goals and the duration of rehabilitation required to effect change in this population. The first objective of this observational study was to characterize and follow trunk strength, hip strength, and reach distance in individuals with NTSCI over the course of rehabilitation, and to determine if there were differences between walkers and wheelchair users. The second objective of this study was to determine if a relationship existed between changes in trunk strength, hip strength, and reach distance in individuals with NTSCI. It was hypothesized that individuals with NTSCI would have improved trunk strength, hip strength, and functional reach distance over the course of their rehabilitation program. It was also hypothesized that there would be a positive correlation between changes in trunk strength, hip strength, and functional reach distance.
Materials and methods
The current substudy was part of a larger study (N = 75) investigating trunk recovery post traumatic or non-traumatic SCI. This substudy was designed to determine if individuals with NTSCI who were walkers and wheelchair users presented with different seated trunk function, when admitted to inpatient rehabilitation, and to evaluate changes in trunk function following surgical spinal intervention.
Study population
A sample of 32 patients admitted to inpatient rehabilitation with NTSCI affecting various vertebral levels was recruited from two rehabilitation hospitals. The subsample of the larger study comprised 42% of the population under study. Subjects from the larger study included subacute patients admitted for inpatient rehabilitation, aged 18–75 years with SCI between levels C5 and L1, either of traumatic or non-traumatic etiology and classified as having an AIS score of A or B (able to sit and wheel independently) or AIS score C or D (able to stand, walk). Subjects from the larger study, who were AIS A and B groups, required the capability to maintain an unsupported sitting position for at least 30 seconds, and use a wheelchair as their primary source of mobility for more than 2 hours per day. For the AIS C and D groups, the participants were required to stand without any assistance for at least 30 seconds and to walk 2 minutes with walking aids and no assistants. Participants were required to present with an activity tolerance of at least 45 minutes when multiple rest periods are available. Subjects were excluded from the study if they had pathology to other parts of the nervous system other than the spinal cord (i.e. major head injury), additional musculoskeletal problems such as severe arthritis, history of deep vein thrombosis, cardiovascular, pulmonary, and other comorbidities that would contraindicate the assessment, or could confound the results of the study.
The sample from the larger study represented the most incident demographics for tetraplegia (C5–C8), and paraplegia (T1–L1) for both groups. The subsample used in this analysis from the larger study included individuals with NTSCI only.
Screening for study participants was done by the research coordinator in consultation with the attending participant's physician and a review of medical records by one of the co-investigators. All eligible participants that consented to be in the study were assessed if their data could be captured during the study timeframes for the admission (i.e. within 2 weeks of admission to the rehabilitation unit) and discharge assessments (i.e. within 2 weeks prior to discharge from the rehabilitation unit).
The study was conducted at two rehabilitation hospitals: Institut de Réadaptation Gingras-Lindsay-de-Montréal (IRGLM), Montreal, Quebec, Canada, and at the University Health Network – Toronto Rehabilitation Institute, Toronto, Ontario, Canada. The study was approved by the Research Ethics Boards of both research facilities. All participants reviewed and signed the consent form prior to participating in the study.
Experimental procedure
Subjects were tested over two assessment periods: at admission to the rehabilitation unit (admission assessment), and within 2 weeks prior to discharge (discharge assessment). Clinical measures comprised of maximal static strength of the trunk, upper and lower extremities, range of motion of the trunk, upper and lower extremities, spasticity using the Composite Spasticity Index20 and the MDRT.
While enrolled in the study at both institutions, patients continued to receive the standard of rehabilitative care. Standard of care at the two sties was comprised of interdisciplinary patient customized rehabilitation based on the patient's postural, mobility, and functional status at admission in order to optimize physical and functional outcomes and minimize secondary complications. Customized rehabilitation changed throughout the course of rehabilitation as the patients' needs changed.
Strength measures of the trunk and hip muscles
Maximum static torque generating capabilities were measured during trunk flexion, trunk extension, trunk side flexion, hip extension and flexion using a calibrated hand-held dynamometer (microFET 2, Hoggan Health Industries, West Jordan, UT, USA). For each muscle group tested, subjects performed three trials of 5 seconds, with a 30-second recovery period in between each trial.
Trunk strength measures were performed in the sitting position. At the Montreal site, a rigid frame was used to resist trunk strength assessments. At the Toronto site, resistance during trunk strength was provided manually by the research assistant. For trunk side flexion, the resistance was placed at the acromion. For trunk flexion, the resistance was placed at the upper part of the sternum, and for trunk extension, resistance was placed at the thoracic spine (level of the acromion). Stabilization of the lower limbs was provided with belts at the thighs and we ensured that the subject's feet did not come off the ground. For all muscle groups assessed, the strength was expressed in Nm/kg of body mass and lever arm calculated from the center of the dynamometer and the greater trochanter.
Given the potential contribution of the hip flexors during trunk flexion measures, and hip extensors to trunk extension measures, hip flexion and extension strength were evaluated. Hip flexion and extension measures were performed while the participant was positioned in supine or side lying. During hip flexion, the hips and knees were placed at 90° of flexion with the calves supported on a stool while hip extension was assessed with the hips in neutral position and the knees extended. For hip flexion and extension strength measurements, resistance was placed on the distal thigh.
For each movement, participants were instructed to produce a progressive contraction up to their maximal level of effort without pain. For all muscle groups assessed, the strength was expressed in Nm/kg of body mass with the lever arm calculated from the point of the axis of rotation of the hip joint to the point of resistance. As the difference between sides was not significant (P > 0.05), the mean of three trials for the least affected side was used for analysis.
Seated multidirectional reach distance
Subjects were asked to remain in a seated position on a height adjustable plinth without a backrest, with their hips, knees, and ankles flexed at ∼90° and their feet position planted symmetrically on the floor, with their popliteal fossa ∼5 cm from the edge of the support surface. Using their preferred arm, subjects were asked to reach in one of the six different directions (i.e. forward, back, left, right, forward right, forward left) in random order, towards a target at the level of their acromion, with their opposite hand remaining on their thigh. Subjects were instructed to reach as far towards the target at a self-selected velocity without losing their balance and not to stabilize their trunk with their hand before returning to their initial position. The subjects' legs were not braced; however, testing was stopped if the subjects' feet came off the ground during MDRT to prevent compensatory movements. A passive marker was placed over the first thoracic vertebrae to allow one to measure the vertical and horizontal displacements between the initial and final trunk positions. These distances were recorded using a telemetric laser distance meter (Fluke 411D, Fluke Corporation, Everett, WA, USA) and the resultant displacement was calculated using the Pythagoras theory (Fig. 1). Due to the use of a laser pointer, subjects were provided with protective eyewear to avoid eye damage in the event that the participant looked into the laser. During all reaching tasks, a research associate supervised the participants closely to ensure optimal safety while the other research associate obtained the measurements. Subjects were provided with practice trials to acclimatize them to the testing procedure. In order to account for variations in trunk length, MDRT distance was expressed as a percentage of trunk length. The mean of three trials was used for analyses. The results are interpreted as the longer the displacement, the better seated the reaching ability.
Figure 1 .
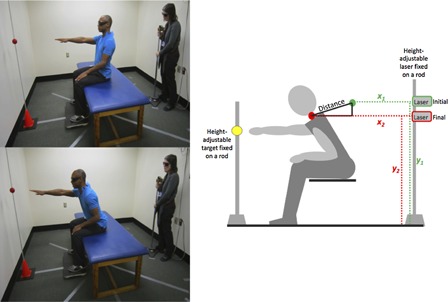
Representation of the MDRT. Using their preferred arm, subjects were asked to reach in one of the six different directions (forward, back, left, right, forward right, forward left) in random order, towards a target at the level of their acromion, with their opposite hand remaining on their thigh.
Statistical analysis
Descriptive statistics (means and standard deviations) were calculated for each of the subject demographics, trunk and hip strength measures, and reach directions, using IBM SPSS Software 22 (IBM Corp., Armonk, NY, USA). A normality test of the data was conducted to determine if the data fit the normal distribution.
Subject demographics of walkers and wheelchair users were analyzed using independent t-tests to determine if walkers and wheelchair users were similar at admission.
Due to the examination of multiple variables, repeated measures analysis of variance (ANOVA) test with a between-group factor was conducted to determine for each outcome (strength and reach tests) whether the data differed between walkers and wheelchair users at admission. Where significance was found, multiple t-tests were conducted to determine if differences between groups were specific for each direction for strength and reach distance. Strength and MDRT data were tested separately to verify group difference at admission.
Repeated measures ANOVA with a between-group factor was conducted to determine if there were significant differences over time between walkers and wheelchair. Where significant interaction effects occurred between the dependent variables of strength and reach distance and group, non-parametric statistics, Wilcoxon tests were used to assess the significant reach directions for each group comparing admission and discharge data.
Pearson product-moment correlation coefficients between trunk strength, hip strength, and MDRT distances were calculated to determine if changes in trunk and hip strength were related to changes in MDRT distance.
Results
Subject demographics and clinical presentation can be found in Table 1. Data were analyzed for 32 individuals with NTSCI who underwent surgical intervention(s) including laminectomy with/without fusion and/or tumor resection. The number of participants in the subgroups of walkers and wheelchairs users was equal. There was no significant difference in demographics between the subgroups of walkers and wheelchair users (P > 0.05). Wheelchair users had longer rehabilitation length of stays; however, the results were not significant. The greatest proportion of participants with NTSCI enrolled in the study had etiologies of tumors (n = 12) and myelopathy (n = 6). The remaining participants presented with abscess (n = 4), transverse myelitis (n = 3), myelopathy and abscess (n = 1), osteomyelitis (n = 1), osteoporosis (n = 1), arteriovenous malformation (n = 1), cord compression (n = 1), cauda equina (n = 1), and spinal stenosis (n = 1).
Table 1 .
Characteristics (mean ± SD) for all participants and subgroups
| All participants (n = 32) |
Subgroup walkers (n = 16) |
Subgroup wheelchair users (n = 16) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Range | Mean | SD | Range | Mean | SD | Range | |
| Age (years) | 48.2 | 15.2 | 22.5–75.4 | 46.6 | 13.7 | 26.1–69.2 | 49.8 | 16.8 | 22.5–75.4 |
| Height (m) | 1.73 | 0.15 | 1.22–1.93 | 1.75 | 0.12 | 1.52–1.93 | 1.71 | 0.17 | 1.22–1.88 |
| Mass (kg) | 79.9 | 18.2 | 48.2–120.5 | 79.3 | 18.9 | 58.6–120.5 | 80.4 | 18.1 | 48.2–114.0 |
| BMI (kg/m2) | 26.5 | 4.50 | 18.2–35.1 | 25.7 | 4.70 | 18.7–34.7 | 27.4 | 4.30 | 18.2–35.1 |
| Day post-surgery at assessment 1 | 48.0 | 30.4 | 15.3–130.0 | 47.7 | 29.8 | 15.0–116.0 | 48.3 | 32.0 | 18.0–137.0 |
| Day post-surgery at assessment 2 | 88.6 | 43.7 | 29.0–183.0 | 77.2 | 45.6 | 29.0–170.0 | 98.7 | 42.0 | 54.0–183.0 |
| Rehabilitation length of stay (days) | 61.9 | 21.3 | 28.0–119.0 | 51.4 | 19.2 | 28.0–96.0 | 72.4 | 18.2 | 49.0–119.0 |
| Number | % | Number | % | Number | % | ||||
| Sex (females/males) | 8/24 | 25/75 | 4/12 | 25/75 | 4/12 | 25/75 | |||
| Handedness (R/L/A) | 30/0/2 | 94/0/6 | 16/0/0 | 100/0/0 | 14/0/2 | 88/0/12 | |||
| Level of pathology (C/T/L) | 10/19/3 | 31/59/10 | 7/8/1 | 44/50/6 | 3/11/2 | 19/69/12 | |||
Not all participants enrolled in the study participated in both admission and discharge assessments and not all subjects assessed at admission and discharge were able to participate in the complete trunk strength, hip strength, and or MDRT testing protocol due to scheduling conflicts (n = 6), late recruitment (n = 3), voluntary withdrawal (n = 4), early discharge (n = 5), fatigue (n = 1), infection (n = 1), and decreased tolerance to assessment (n = 2). However, subjects' ability to participate in all components of the testing did not vary based on subject demographics or clinical presentation.
Trunk and hip strength
Mean trunk strengths at admission for the composite group, walkers, and wheelchair users are found in Table 2 and Fig. 2. Mean trunk strength for the composite group at admission was the highest in the extension direction followed by flexion. Walkers had significantly greater trunk and hip strength compared with wheelchair users at admission (P < 0.05). Post hoc analysis using multiple t-tests found significant differences in trunk and hip strength in all directions between walkers and wheelchair users (P < 0.01).
Table 2 .
Means, standard deviations, and range of trunk strength in four directions and hip in flexion and extension at admission and discharge (Nm/kg) for all participants and subgroups
| All participants (n = 32) |
Subgroup walkers (n = 16) |
Subgroup wheelchair users (n = 16) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | Mean | SD | Range | Number | Mean | SD | Range | Number | Mean | SD | Range | |
| Trunk flexion | ||||||||||||
| Admission | 27 | 0.61 | 0.30 | 0.12–1.33 | 14 | 0.77 | 0.28 | 0.35–1.33 | 13 | 0.35 | 0.18 | 0.12–0.79 |
| Discharge | 19 | 0.61 | 0.30 | 0.23–1.34 | 9 | 0.73 | 0.32 | 0.37–1.34 | 10 | 0.43 | 0.22 | 0.23–0.98 |
| Trunk extension | ||||||||||||
| Admission | 27 | 0.80 | 0.63 | 0.08–2.57 | 14 | 1.14 | 0.71 | 0.40–2.57 | 13 | 0.36 | 0.15 | 0.08–0.75 |
| Discharge | 19 | 0.91 | 0.77 | 0.29–2.74 | 9 | 1.25 | 1.00 | 0.31–2.74 | 10 | 0.50 | 0.24 | 0.29–0.93 |
| Trunk right lateral flexion | ||||||||||||
| Admission | 27 | 0.49 | 0.23 | 0.07–0.92 | 14 | 0.63 | 0.18 | 0.25–0.92 | 13 | 0.35 | 0.18 | 0.07–0.62 |
| Discharge | 19 | 0.51 | 0.27 | 0.12–1.23 | 9 | 0.61 | 0.29 | 0.34–1.23 | 10 | 0.43 | 0.22 | 0.12–0.74 |
| Trunk left lateral flexion | ||||||||||||
| Admission | 27 | 0.49 | 0.21 | 0.10–0.91 | 14 | 0.62 | 0.18 | 0.34–0.91 | 13 | 0.36 | 0.15 | 0.10–0.60 |
| Discharge | 19 | 0.51 | 0.26 | 0.23–1.36 | 9 | 0.62 | 0.31 | 0.28–1.36 | 10 | 0.42 | 0.16 | 0.23–0.69 |
| Hip flexion* (less affected) | ||||||||||||
| Admission | 28 | 0.42 | 0.29 | 0–1.20 | 14 | 0.59 | 0.26 | 0.25–1.2 | 14 | 0.25 | 0.22 | 0–0.65 |
| Discharge | 20 | 0.47 | 0.25 | 0–0.96 | 10 | 0.61 | 0.17 | 0.44–0.96 | 10 | 0.32 | 0.23 | 0–0.66 |
| Hip extension* (less affected) | ||||||||||||
| Admission | 27 | 0.54 | 0.33 | 0–1.03 | 14 | 0.73 | 0.24 | 0.17–1.03 | 13 | 0.32 | 0.28 | 0–0.82 |
| Discharge | 18 | 0.50 | 0.31 | 0–1.02 | 9 | 0.63 | 0.23 | 0.25–1.02 | 9 | 0.36 | 0.34 | 0–0.93 |
*Data are for the less affected side demonstrating stronger limb.
Figure 2 .
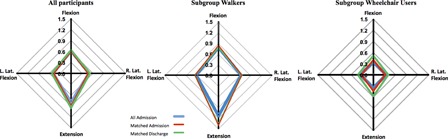
Mean trunk strength (Nm/kg) for all participants (n = 27) at admission and for matched pairs of walkers (n = 8) and wheelchair users (n = 9) at admission and discharge. Wheelchair users have lower trunk strength, particularly for extensors at both admission and discharge.
Repeated measures ANOVA demonstrated non-significant differences between walkers and wheelchair users with respect to absolute change over time in trunk and hip strength.
Multidirectional reach distance
Mean reaches expressed in percentage of trunk length at admission for the composite group, walkers, and wheelchair users are found in Table 3 and Fig. 3. Mean reaches for the composite group at admission and discharge were highest in the forward reach direction. Significant differences in reaches at admission were found between walkers and wheelchair users (P < 0.05). Post hoc t-test analyses revealed that left and right reaches were significantly greater in the walkers vs. wheelchair users (P < 0.02).
Table 3 .
Means, standard deviations, and range of MDRT in six directions at admission and discharge (% of trunk length) for all participants and subgroups
| All participants (n = 32) |
Subgroup walkers (n = 16) |
Subgroup wheelchair users (n = 16) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | Mean | SD | Range | Number | Mean | SD | Range | Number | Mean | SD | Range | |
| Front | ||||||||||||
| Admission | 25 | 0.54 | 0.17 | 0.37–0.90 | 13 | 0.52 | 0.15 | 0.33–0.75 | 12 | 0.56 | 0.19 | 0.27–0.90 |
| Discharge | 19 | 0.68 | 0.18 | 0.40–1.02 | 9 | 0.62 | 0.14 | 0.41–0.77 | 10 | 0.73 | 0.21 | 0.42–1.02 |
| Back | ||||||||||||
| Admission | 22 | 0.34 | 0.10 | 0.19–0.56 | 11 | 0.30 | 0.08 | 0.22–0.46 | 11 | 0.38 | 0.10 | 0.19–0.56 |
| Discharge | 17 | 0.37 | 0.16 | 0.19–0.68 | 8 | 0.34 | 0.15 | 0.25–0.68 | 9 | 0.39 | 0.17 | 0.19–0.65 |
| Left | ||||||||||||
| Admission | 24 | 0.34 | 0.17 | 0.07–0.67 | 12 | 0.45 | 0.15 | 0.23–0.67 | 12 | 0.23 | 0.10 | 0.07–0.47 |
| Discharge | 19 | 0.40 | 0.23 | 0.03–1.1 | 9 | 0.39 | 0.16 | 0.19–0.69 | 10 | 0.40 | 0.29 | 0.03–1.1 |
| Right | ||||||||||||
| Admission | 25 | 0.32 | 0.14 | 0.1–0.63 | 13 | 0.38 | 0.15 | 0.10–0.63 | 12 | 0.25 | 0.10 | 0.12–0.43 |
| Discharge | 19 | 0.40 | 0.15 | 0.20–0.9 | 9 | 0.39 | 0.07 | 0.28–0.5 | 10 | 0.42 | 0.20 | 0.20–0.9 |
| 45° left | ||||||||||||
| Admission | 24 | 0.40 | 0.17 | 0.15–0.78 | 12 | 0.43 | 0.14 | 0.26–0.66 | 12 | 0.38 | 0.20 | 0.15–0.78 |
| Discharge | 18 | 0.46 | 0.19 | 0.08–0.94 | 9 | 0.51 | 0.19 | 0.28–0.94 | 9 | 0.41 | 0.19 | 0.08–0.71 |
| 45° right | ||||||||||||
| Admission | 24 | 0.46 | 0.26 | 0.09–1.12 | 12 | 0.55 | 0.26 | 0.26–1.12 | 12 | 0.38 | 0.23 | 0.09–0.76 |
| Discharge | 18 | 0.56 | 0.23 | 0.20–1.13 | 9 | 0.51 | 0.11 | 0.40–0.71 | 9 | 0.60 | 0.31 | 0.20–1.13 |
Figure 3 .
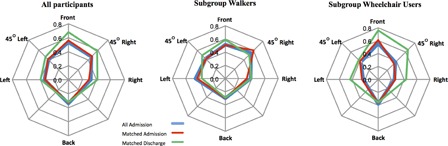
Mean sitting MDRT (% trunk length) for all participants (n = 22–25) at admission and for matched pairs of walkers (n = 7) and wheelchair users (n = 7–8) at admission and discharge. Wheelchair users gain further reach distances to the left and right than walkers.
Repeated measures ANOVA demonstrated a significant interaction effect of group (walkers vs. wheelchair users) and multidirectional reaches between admission and discharge. The ANOVA revealed non-significant differences for changes in reach distance between admission and discharge in walkers while it was significant for wheelchair users. Thus, we pursued with non-parametric statistics to determine the reaching directions that differed from admission to discharge with Wilcoxon tests in the wheelchair users. Differences between admission and discharge reach data in the wheelchair users (P < 0.05) were significant for right and left reach direction in the wheelchair users (P ≤ 0.05).
Relationship between MDRT and muscle strength
Fig. 4 shows significant associations between the less affected hip flexion strength and right reach (R = 0.731), left lateral trunk flexion and right reach (R = 0.700), trunk extension strength and left reach (R = 0.735), and trunk flexion strength and left reach (R = 0.669). Walkers presented with a greater effect on the association when compared with wheelchair users.
Figure 4 .
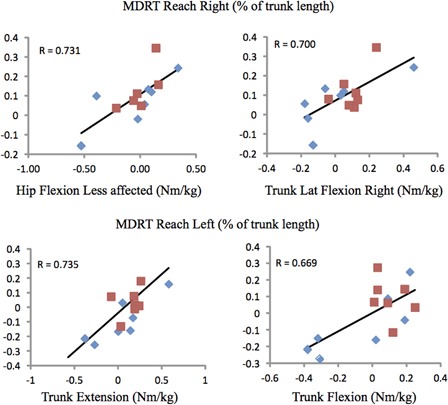
Scatterplots showing significant (P = 0.01) association between changes in sitting MDRT (% trunk length) for matched pairs of walkers (blue diamonds) (n = 7) and wheelers (red squares) (n = 7) and hip or trunk strength changes.
Discussion
The purpose of this study was to characterize and follow trunk strength, hip strength, and reach distance in individuals with NTSCI over the course of rehabilitation, to determine if there were differences between walkers and wheelchair users with respect to trunk and hip strength and reach distance, and to determine if a relationship existed between the changes in trunk strength, hip strength, and reach distance in individuals with NTSCI. This observational study is the first of its kind to document the changes in trunk function following surgical intervention for NTSCI during rehabilitation.
We analyzed the NTSCI subjects separately, as the NTSCI population presented with various etiologies of non-incident SCI (i.e. oncology, cervical myelopathy, etc.). Participants presented with multiple levels of spinal pathology (C2–L4), different surgical intervention(s). Given that their history and course of their disease processes and health status prior to surgery was variable, they were considered to be a distinct SCI population.
We were not able to characterize these patients using the International Standards for Neurological Classification of Spinal Cord Injury with any degree of sensitivity based on the types of pathology of our participants. An alternative classification system for NTSCI has been suggested,21 which considers the history of etiology and International Classification of Diseases coding. However, this is not the current practice in Canada and therefore such data are not available in the health record coding. Therefore, we elected to separate the participants into two mobility subpopulations (walkers and wheelchair users) for our analysis to address our question as we anticipated that they would show differences in trunk neuromotor capacity at admission to rehabilitation.
Assessment measures were scheduled around admission and discharge times to and from rehabilitation presenting challenges in the evaluation of both the impairments and functional limitations. Despite challenges in the evaluation of trunk function in individuals with NTSCI, we were able to demonstrate that walkers, not surprisingly had significantly greater trunk and hip strength than wheelchair users at admission for all directions measured.
Trunk strength has been evaluated minimally in individuals with SCI20,22 and there is a paucity of research on specific rehabilitation strategies for improving trunk control in these individuals. One study has demonstrated that with a 10-week kayak training protocol, trunk stability improved in individuals with chronic paraplegia.16 However, this was not with subacute post-operative study participants. Not surprisingly, our findings showed significant increase in trunk strength measures over the course of rehabilitation in patients with NTSCI in both walkers and wheelchair users.
Our study found significant differences in hip strength between walkers and wheelchair users at admission; however, no significant differences for the magnitude of strength change between walkers and wheelchair users over the course of rehabilitation. Static strength of the ankle plantar flexors and dorsiflexor muscles has been related to ambulatory capacity in individuals with incomplete traumatic SCI.23 Reduction in knee extensor and ankle plantar flexion torque and reduced ability to generate instantaneous muscle strength has been found in individuals with chronic incomplete SCI when compared with healthy matched controls.24 However, there have not been previous studies measuring trunk and proximal lower limb musculature in NTSCI in the subacute phase, so further studies with larger sample sizes are required to determine if proximal lower extremity strength changes in walkers and wheelchair users over the course of rehabilitation influences their mobility status and walking capacity.
We were able to demonstrate significant increases in sitting MDRT distance in the left and right directions between rehabilitation admission and discharge assessments for wheelchair users but not for walkers. We interpret that this increased difference may be related to having to reach in their extra-corporeal environment for all activities of daily living and that this group has optimized their performance through necessity/practice. Interestingly, the most dramatic increases in MDRT distance were found in the right direction. Fourteen of our 16 wheelchair users were right handed suggesting that, it may be possible to explore the interaction of trunk postural control, limb dominance, intensity of use, and reach distance during recovery and rehabilitation, particularly for those who will be required to reach from the sitting position for future activities if they do not recover the ability to walk. Grangeon et al.25 suggest that individuals with SCI may use their dominant upper extremity for reaching more frequently while providing support through their non-dominant limb, thereby developing superior seated stability with their dominant limb elevated.
Our study demonstrated that the changes in strength of the less affected hip and left trunk flexion strength were related to changes in right MDRT distance while the corresponding value of trunk extension strength was related to left MDRT distance. These findings are in contradiction with previous studies of Chen et al.5 that examined trunk flexion and extension strength as a predictor of dynamic sitting stability and found no relationship between strength and reach distance in individuals with paraplegia;5 however, they did not measure hip muscle strength. They did find that the injury level and trunk length were better predictors of functional reach explaining 43.5% of the variance,5 hence we elected to normalize reach distance by trunk length. One would expect that the requirement to generate the forces to both stabilize the lower extremities and control trunk movement, is necessary to maintain seated stability. A larger sample size with precise characterization of the site of pathology and neurological status would be important to explore these relationships and the changes post-surgery between the level of pathology, injury, and surgical intervention, lower limb motor scores, trunk strength, and MDRT.
Study limitations
We did not document or evaluate the specific rehabilitation interventions that would challenge trunk control sitting balance in our participants; therefore, we were unable to identify if any of our participants underwent specific trunk strengthening exercises. However, given our preliminary findings, the importance of understanding the relationships between trunk strength and rehabilitation interventions to facilitate the development of customized therapies for individual patients to improve sitting balance during functional activities becomes more paramount.
Our study measured MDRT distances in six directions and trunk strength in only four directions as our protocol did not evaluate the strength of the oblique muscles through assessment of resisted trunk flexion in cross flexion or rotation as some patients had post-operative restrictions for resisted testing in an oblique or rotational direction. As such, we were unable to assess correlations between MDRT distances in the 45° to the left and 45° to the right directions with strength of the key rotator muscle group, including the oblique muscles.
In addition, we did not conduct kinematic assessment of the trunk and lower extremity movement during the MDRT, and are therefore unable to comment on compensatory strategies of the pelvis used during the reaching task, nor establish if the trunk moved out of the primarily plane during testing. It has been established previously that individuals with poor trunk control engage in a posterior pelvic tilt and show an increased thoracic kyphosis in sitting to increase their base of support.11,12 Sprigle et al.13 demonstrated that with posterior pelvic tilt functional reach distance increased. This compensatory strategy may increase reach ability, due to increased base of support through contact of the sacrum to the supporting surface and posterior displacement of the center of mass over the base of support, offsetting the anterior displacement of the center of mass during forward reaching. Using three-dimensional motion analysis in addition to electromyography of the trunk muscles (i.e. quadratus lumborum, external obliques, rectus abdominis) and lower extremity muscles (i.e. gluteus maximus) would help elucidate trunk posture during the reach task and determine if postural movement strategies or compensations change over the course of rehabilitation.
Our study was conducted using 32 individuals with NTSCI. Given the small n-values for the matched pairs of walkers and wheelchair users, we are unable to generalize our findings to the total sample of all individuals with NTSCI. Larger scale multisite studies are recommended with implementation of strategies to reduce attrition of study participants and incorporate broader inclusion criteria.
Conclusion
This study demonstrated that monitoring changes in trunk and hip strength and reach distance is complex in individuals with NTSCI, particularly when multiple measures are being assessed and individuals are assessed at varying timepoints during their recovery post-surgery. Trunk and hip strength did not improve over the course of rehabilitation in both walkers and wheelchair users. MDRT distance in the right and left lateral directions improved over the course of inpatient rehabilitation for wheelchair users only. Measuring trunk control using static trunk strength and the MDRT in the right and left directions which were sensitive to changes over the course of 61 days of inpatient rehabilitation, appears to show promise as a clinical assessment approach to track changes and to demonstrate outcome.
Disclaimer statements
Contributors SG has made a substantial contribution to the acquisition of data, data analysis and interpretation of data, drafted the article, and approved the version to be published. MCV has made a substantial contribution to the concept and design, acquisition of data and analysis and interpretation of data, revised the draft critically for important intellectual content, approved the version to be published. SN has made a substantial contribution to the concept and design, acquisition of data and analysis and interpretation of data, revised the draft critically for important intellectual content, approved the version to be published. DN has made a substantial contribution to the concept and design, acquisition of data and analysis and interpretation of data, revised the draft critically for important intellectual content, approved the version to be published. AR has made a substantial contribution to the acquisition of data. HF has made a substantial contribution to the acquisition of data.
Funding The study was funded by a grant from the Craig H. Neilsen Foundation #164422.
Conflicts of interest None.
Ethics approval The study was conducted at two rehabilitation hospitals: Insitut de Réadaptation Gingras-Lindsay-de-Montréal (IRGLM) in Montreal, and University Health Network-Toronto Rehabilitation Institute (UHN-TRI). The study was approved by the Research Ethics Boards of both research facilities.
Acknowledgments
We acknowledge clinicians of the SCI units at IRGLM and the UHN-TRI and Cyril Duclos for their collaboration.
References
- 1.Simmons RK, van Sluijs EM, Hardeman W, Sutton S, Griffin SJ; ProActive Project Team. Who will increase their physical activity? Predictors of change in objectively measured physical activity over 12 months in the ProActive cohort. BMC Public Health 2010;10:226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cosar SNS, Yemisci OU, Oztop P, Cetin N, Sarifakioglu B, Yalbuzdag SA, et al. Demographic characteristics after traumatic and non-traumatic spinal cord injury: a retrospective comparison study. Spinal Cord 2010;48(12):862–6 [DOI] [PubMed] [Google Scholar]
- 3.New PW, Simmonds F, Stevermuer T. A population-based study comparing traumatic spinal cord injury and non-traumatic spinal cord injury using a national rehabilitation database. Spinal Cord 2010;49(3):397–403 [DOI] [PubMed] [Google Scholar]
- 4.Marinho AR, Flett HM, Craven C, Andrea Ottensmeyer C, Parsons D, Verrier MC. Walking-related outcomes for individuals with traumatic and non-traumatic spinal cord injury inform physical therapy practice. J Spinal Cord Med 2012;35(5):371–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen C-L, Yeung K-T, Bih L-I, Wang C-H, Chen M-I, Chien J-C. The relationship between sitting stability and functional performance in patients with paraplegia. Arch Phys Med Rehabil 2003;84(9):1276–81 [DOI] [PubMed] [Google Scholar]
- 6.Sprigle S, Maurer C, Holowka M. Development of valid and reliable measures of postural stability. J Spinal Cord Med 2007;30(1):40–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gauthier C, Gagnon D, Jacquemin G, Duclos C, Masani K, Popovic M. Which trunk inclination directions best predict multidirectional-seated limits of stability among individuals with spinal cord injury? J Spinal Cord Medicine 2012;35(5):343–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tyler AE, Hasan Z. Qualitative discrepancies between trunk muscle activity and dynamic postural requirements at the initiation of reaching movements performed while sitting. Exp Brain Res 1995;107:87–95 [DOI] [PubMed] [Google Scholar]
- 9.Larson C, Tezak W, Malley M, Thornton W. Assessment of postural muscle strength in sitting: reliability of measures obtained with hand-held dynamometry in individuals with spinal cord injury. J Neurol Phys Ther 2010;34(1):24. [DOI] [PubMed] [Google Scholar]
- 10.Seelen H, Potten Y, Adam JJ, Drukker J, Spaans F, Huson A. Postural motor programming in paraplegic patients during rehabilitation. Ergonomics 1998;41(3):302–16 [DOI] [PubMed] [Google Scholar]
- 11.Triolo RJ, Nogan Bailey S, Miller ME, Lomardo LM, Audu ML. Effects of stimulating hip and trunk muscles on seated stability, posture, and reach after spinal cord injury. Arch Phys Med Rehabil 2013;94(9):1766–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hobson DA, Tooms RE. Seated lumbar/pelvic alignment: a comparison between spinal cord-injured and noninjured groups. Spine 1992;17(3):293–8 [PubMed] [Google Scholar]
- 13.Sprigle S, Wooten M, Sawacha Z, Theilman G. Relationships among cushion type, backrest height, seated posture and reach of wheelchair users with spinal cord injury. J. Spinal Cord Med 2003;26(3):236–43 [DOI] [PubMed] [Google Scholar]
- 14.Kilmer DD, McCrory MA, Wright NC, Rosko RA, Kim HR, Aitkens SG. Hand-held dynamometry reliability in persons with neuropathic weakness. Arch Phys Med Rehabil 1997;78(12):1364–8 [DOI] [PubMed] [Google Scholar]
- 15.Drolet M, Noreau L, Vachon J, Moffet H. Muscle strength changes as measured by dynamometry following functional rehabilitation in individuals with spinal cord injury. Arch Phys Med Rehabil 1999;80(7):791–800 [DOI] [PubMed] [Google Scholar]
- 16.Bjerkefors A, Carpenter MG, Thorstensson A. Dynamic trunk stability is improved in paraplegics following kayak ergometer training. Scand J Med Sci Sports 2007;17(6):672–9 [DOI] [PubMed] [Google Scholar]
- 17.Field-Fote EC, Ray SS. Seated reach distance and trunk excursion accurately reflect dynamic postural control in individuals with motor-incomplete spinal cord injury. Spinal Cord 2010;48(10):745–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newton RA Validity of the multi-directional reach test: a practical measure for limits of stability in older adults. J Gerontol A Biol Sci Med Sci 2001;56(4):M248–52 [DOI] [PubMed] [Google Scholar]
- 19.Shin S, Sosnoff J. Spinal cord injury and time to instability in seated posture. Arch Phys Med Rehabil 2013;94(8):1615–20 [DOI] [PubMed] [Google Scholar]
- 20.Levin MF, Hui-Chan CW. Are H and stretch reflexes in hemiparesis reproducible and correlated with spasticity? J Neurol 1993;240(2):63–71 [DOI] [PubMed] [Google Scholar]
- 21.New PW, Marshall R. International Spinal Cord Injury Data Sets for non-traumatic spinal cord injury. Nature Publishing Group 2013;52(2):123–32 [DOI] [PubMed] [Google Scholar]
- 22.Vanlandewijck YC, Verellen J, Tweedy SM. Towards evidence-based classification – the impact of impaired trunk strength on wheelchair propulsion. Adv Rehabil 2010;3(1):1–5 [Google Scholar]
- 23.Ellaway PH, Kuppuswamy A, Balasubramaniam AV, Maksimovic R, Gall A, Craggs MD, et al. Development of quantitative and sensitive assessments of physiological and functional outcome during recovery from spinal cord injury: a clinical initiative. Brain Res Bull 2011;84(4–5):343–57 [DOI] [PubMed] [Google Scholar]
- 24.Jayaraman A, Gregory CM, Bowden M, Stevens JE, Shah P, Behrman AL, et al. Lower extremity skeletal muscle function in persons with incomplete spinal cord injury. Spinal Cord 2005;44(11):680–7 [DOI] [PubMed] [Google Scholar]
- 25.Grangeon M, Gagnon D, Gauthier C, Jacquemin G, Masani K, Popovic MR. Effects of upper limb positions and weight support roles on quasi-static seated postural stability in individuals with spinal cord injury. Gait Posture 2012;36(3):572–9 [DOI] [PubMed] [Google Scholar]


