Abstract
Lymphangioma is a rare, benign mesenchymal neoplasm, which is characterized by numerous intercommunicating cystic spaces containing lymphatic fluid. It is considered a congenital disease resulting from the obstruction of regional lymph drainage during the developmental period. Lymphangioma may be focal/unilateral or diffuse/bilateral, and in the latter case, it is referred to as lymphangiomatosis. Here, we report a case of a 38-year-old man with perirenal lymphangiomatosis. The patient's chief complaint was left flank pain, and left pleural effusion was found on radiological examination. After radical nephrectomy, the pathological examinations revealed that the kidney was enclosed by a multicystic mass with intrarenal cystic dilatations. We report the case and discuss the management of perirenal lymphangiomatosis with a literature review.
Keywords: Kidney, Lymphangioma, Lymphatic diseases, Neoplasms
Lymphangioma is a rare mesenchymal disorder, which is characterized by the developmental malformation of lymphatic channels [1]. Renal lymphangioma, or peripyelic-pericalyceal lymphangiectasis, is an even rarer multiple cystic disorder of the kidneys resulting from abnormal lymphatic tissues [2]. This disease entity usually presents in children, but infrequently, it also presents in adults. The cervical neck and axilla are the most common locations for lymphangioma, but it can also occur in the retroperitoneum, mediastinum, mesentery, omentum, colon, and pelvis [3,4]. Therefore, lymphangioma may arise in any organs where congenital obstruction of regional lymph drainage can occur during the developmental period. If lymphangiomas occur diffusely, the condition is referred to lymphangiomatosis. Here, we report a case of perirenal lymphangiomatosis and discuss its diagnosis and management with a literature review.
CASE REPORT
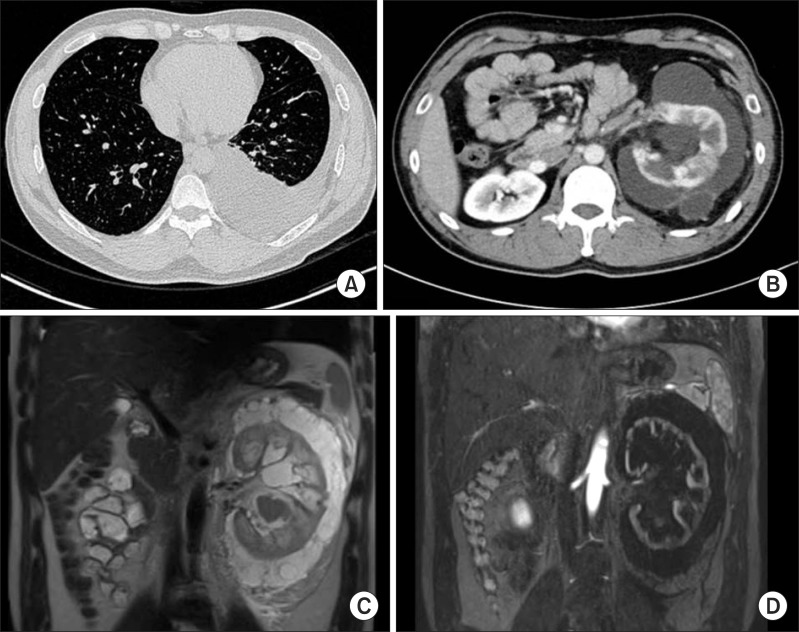
A 38-year-old man visited Pusan National University Hospital due to severe left flank pain for 2 months. The patient had a medical history significant for cerebrovascular accident 2 years prior to presentation. The laboratory results, including complete blood counts, serum electrolytes, liver and renal function parameters, and urinalysis, were within the normal range. During the evaluation for this left flank pain, left-sided pleural effusion was found on the chest X-ray and the computed tomography (CT) scan (Fig. 1A). The lesion was suspicious for tuberculosis pleural effusion, and thoracentesis was performed; 280 mL of the effusion was drained. However, laboratory studies of the pleural fluid did not reveal any evidence of malignancy or tuberculosis. Upon further evaluation, an abdominal CT revealed an enlarged left kidney surrounded by multilocular cystic lesions in the perinephric space. The CT study also showed mild pelvicalyceal dilatation, decreased contrast enhancement, and irregular contour of the left kidney, which implied decreased kidney function (Fig. 1B). Upon magnetic resonance imaging, the cystic lesions exhibited high signal intensity on T1-weighted images and low signal intensity on T2-weighted images (Fig. 1C, 1D). A majority of the cystic lesions were located in the perirenal space, with focal cystic dilations in the renal parenchyma.
Fig. 1.
Radiologic images of perirenal lymphangiomatosis. (A) Chest computed tomography (CT) reveals pleural effusion of the left pleural cavity. (B) An enlarged left kidney has decreased radio-contrast enhancement with septated perirenal cystic fluid collections on abdominal CT. (C) High signal intensity is found around the left kidney with enlarged pelvo-calyceal system on T1-weighted magnetic resonance (MR). (D) Cortical thinning and irregularity of the left kidney is demonstrated in contrast enhanced T2-weighted MR.
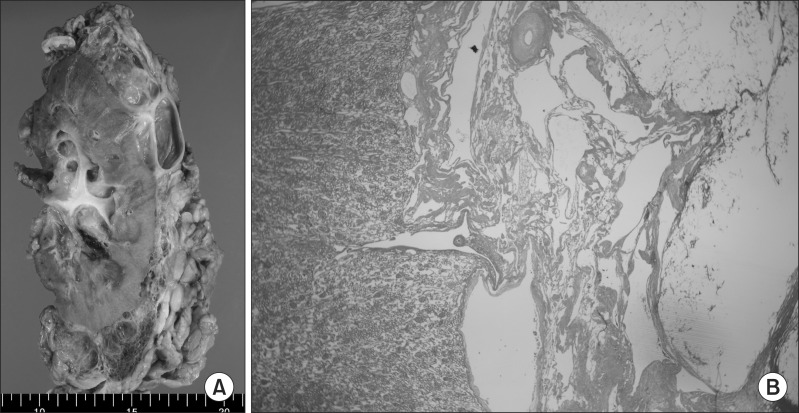
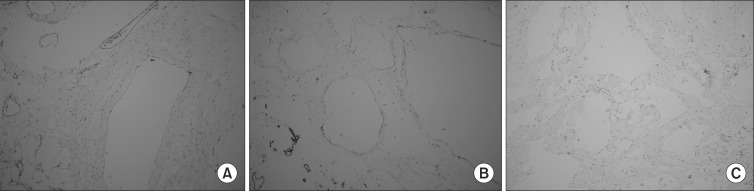
A left radical nephrectomy was indicated because of the flank pain and pleural effusion with a left kidney, which appeared to have decreased renal function on radiologic studies. Intraoperative findings revealed the left kidney to be encircled by multiple thin-walled cystic lesions with severe inflammation, which caused the rupture of some cystic lesions (Fig. 2). The renal parenchyma was grossly unremarkable except for hydronephrosis with a focal thrombus. The renal capsule and the renal parenchyma were involved by the foci of dilated cystic lesions. Histopathologically, these lesions were composed of multilocular cysts that encircled the entire renal capsule. Microscopic examination revealed dilated lymphovascular channels in the perirenal fat and renal sinus fat. Some cysts contained a thrombus. Upon immunohistochemical straining, the cystic walls were weakly positive for CD34, but not for D2-40/CD31 or EMA/HMB-45/WT-1. These results were suggestive of lymphangioma (Fig. 3).
Fig. 2.
Gross and microscopic findings. (A) Multilocular cystic mass is enclosing the kidney. The mass consists of multiple cysts having thin fibrous walls and contains clear serous fluid. (B) Low power (×40) microscopic view shows multiloculated cystic spaces with various caliber of muscular and fibrous walls and without definite epithelial lining on H&E staining.
Fig. 3.
Flattened endothelial lining is visualized by immunohistochemical staining for CD31 (A), CD34 (B), and HMB-45 (C) (A~C: ×100).
The patient was discharged at seven days after the operation without any complications. When the patient visited the outpatient clinic, he reported resolution of the flank pain, and no recurrence of cystic lesions or pleural effusion was evident on the follow-up thoracoabdominal CT study. He has been monitored for 12 months and remains well, without any evidence of recurrence.
DISCUSSION
Lymphangioma is a rare malformation of the lymphatic system. A majority of lymphangiomas occur in the cervical (75%) and axillary regions (20%) with the remaining occurring in the retroperitoneum, mediastinum, mesentery, omentum, colon, and pelvis [3,4]. Renal lymphangioma is a very rare disease entity that is caused by obstructions of the lymphatic system around the kidney during the developmental period. Approximately 50 cases of renal lymphangioma have been reported, and little is known about its prevalence, pathogenesis, and natural history.
In the literature review, some patients had presented with intrarenal dilatation of lymphatic channels, and perirenal abnormality in others. In this current case, these abnormalities were observed in the perirenal space along with diffuse multifocal lesions. Therefore, the patient was diagnosed with perirenal lymphangiomatosis.
Previous reports have described non-specific symptoms including hematuria, flank pain, and abdominal pain in patients with lymphangiomatosis [5,6]. In the case presented, the flank pain appeared to be caused by reactive plural effusion. Lymphangioma may be unilocular or multilocular and may contain serous or chylous fluid. In this case, the cysts contained serous fluid, which was observed with the rupture of cysts during the operation. The cysts were separated by multiple fibrous septa and might communicate with each other or with the lymphatic system [7]. Complications of lymphangioma have been reported to include infection, rupture, or hemorrhage [8]. Other studies have also reported the deterioration of renal function, which progressed over a follow-up period of 6 years [7]. In the case presented, CT imaging revealed intrarenal lymphangioma and decreased cortical thickening, which implied a progressive decease in renal function in the long term.
Renal lymphangiomatosis can be diagnosed with needle aspiration of the chylous fluid from perinephric fluid collections [6]. Fine needle aspiration (FNA) and cytological examination of the fluid may help to confirm the malignant nature of the lesion, although the sensitivity of FNA cytology is low [3]. The cystic patterns on CT and ultrasonography are characteristic of this disease and allow the diagnosis to be made with confidence [9].
Treatment is not required for a majority of asymptomatic patients. Less invasive treatment modalities such as percutaneous or laparoscopic aspiration and cyst marsupialization should be considered in the case of focal or regional lymphangioma. However, patients with 'decompensated lymphangioma' with increasing perirenal fluid collection, flank pain, ascites, or hypertension should be considered for nephrectomy [3]. A recent review reported 29 (83%) cases of lymphangioma, which were treated with radical or partial nephrectomy [3]. Some authors recommend nephrectomy in patients with lymphangiomas, to differentiate the kidney lesions from renal or perirenal malignancies such as renal cell carcinoma, multilocular cystic nephroma, Wilms' tumor, mesoblastic nephroma, and clear cell sarcoma [8]. In our patient, nephrectomy was indicated for flank pain and a significant extent of pleural effusion. No case of recurrent perirenal lymphangioma was reported after the nephrectomy.
ACKNOWLEDGEMENTS
This work was supported by a 2013 clinical research grant from Pusan National University Hospital.
References
- 1.Westphalen A, Yeh B, Qayyum A, Hari A, Coakley FV. Differential diagnosis of perinephric masses on CT and MRI. AJR Am J Roentgenol. 2004;183:1697–1702. doi: 10.2214/ajr.183.6.01831697. [DOI] [PubMed] [Google Scholar]
- 2.Lindsey JR. Lymphangiectasia simulating polycystic disease. J Urol. 1970;104:658–662. doi: 10.1016/s0022-5347(17)61804-4. [DOI] [PubMed] [Google Scholar]
- 3.Honma I, Takagi Y, Shigyo M, Sunaoshi K, Wakabayashi J, Harada O, et al. Lymphangioma of the kidney. Int J Urol. 2002;9:178–182. doi: 10.1046/j.1442-2042.2002.00437.x. [DOI] [PubMed] [Google Scholar]
- 4.Leder RA. Genitourinary case of the day. Renal lymphangiomatosis. AJR Am J Roentgenol. 1995;165:197–198. doi: 10.2214/ajr.165.1.7785592. [DOI] [PubMed] [Google Scholar]
- 5.Murray KK, McLellan GL. Renal peripelvic lymphangiectasia: appearance at CT. Radiology. 1991;180:455–456. doi: 10.1148/radiology.180.2.2068311. [DOI] [PubMed] [Google Scholar]
- 6.Varela JR, Bargiela A, Requejo I, Fernandez R, Darriba M, Pombo F. Bilateral renal lymphangiomatosis: US and CT findings. Eur Radiol. 1998;8:230–231. doi: 10.1007/s003300050368. [DOI] [PubMed] [Google Scholar]
- 7.Laurent F, Joullie M, Biset JM, Simon JM, Drouillard J. Cystic lymphangioma of the kidney: a rare cause of multiloculated renal masses. Eur J Radiol. 1991;12:67–68. doi: 10.1016/0720-048x(91)90137-k. [DOI] [PubMed] [Google Scholar]
- 8.Kutcher R, Mahadevia P, Nussbaum MK, Rosenblatt R, Freed S. Renal peripelvic multicystic lymphangiectasia. Urology. 1987;30:177–179. doi: 10.1016/0090-4295(87)90191-9. [DOI] [PubMed] [Google Scholar]
- 9.Cutillo DP, Swayne LC, Cucco J, Dougan H. CT and MR imaging in cystic abdominal lymphangiomatosis. J Comput Assist Tomogr. 1989;13:534–536. doi: 10.1097/00004728-198905000-00038. [DOI] [PubMed] [Google Scholar]