Abstract
Purpose
Objective functional outcomes following isolated radial lateral meniscus tears in the athlete between the ages of 14–25 are not clearly defined. The objective of this study was to determine whether patients following lateral meniscectomy demonstrate lower extremity asymmetries relative to control athletes 3 months after surgery. We hypothesized that following lateral meniscectomy, athletes aged 14–25 years old would demonstrate altered landing biomechanics compared to sex, age, height, weight, and sport-matched controls.
Methods
A total of 18 subjects were included in this study. Nine patients (7 men and 2 women, 20.1 ± 2.8 years) who had undergone first-time isolated radial lateral meniscus tears were tested 3 months following partial lateral meniscectomies and compared to nine sex, age, height, weight, and sport-matched controls (7 men and 2 women, 19.7 ± 3.1 years). A ten-camera motion analysis system and two force platforms were used to collect three trials of bilateral drop landings. A 2X2 ANOVA was used to test the interaction between side (involved vs. uninvolved) and group (patient vs. control).
Results
The patient group landed with a decreased internal knee extensor moment compared to the uninvolved side and controls (interaction P < 0.05). The involved limb quadriceps isokinetic torque was not decreased compared to the contralateral or control (n.s.). Decreased knee extensor moments were significantly associated with reduced measures of function (IKDC scores: r = 0.69; P < 0.05).
Conclusions
Athletes who return to sport at approximately 3 months following a partial lateral meniscectomy may employ compensation strategies during landing as evidenced by reduced quadriceps recruitment and functional outcome scores. Clinicians should focus on improving quadriceps function during landing on the involved leg in an attempt to decrease residual limb asymmetries.
Level of evidence
Case–control study, Level III.
Keywords: Landing biomechanics, Knee surgery, Knee function, Case–control study
Introduction
Over the last 30 years, the importance of the menisci for load transmission, shock absorption, improved joint stability, joint nutrition, and proprioception has been reported [2, 7]. With the known importance of the menisci during weight bearing, surgical techniques have evolved to reflect the critical role of the menisci in knee function. In 1962, surgeons began performing arthroscopic partial meniscectomies [27], and more recently, in the 1980s, meniscus repairs were initiated to spare healthy meniscal tissue [27]. While some authors have gone as far as to promote non-surgical treatment for meniscus tears [10], arthroscopic surgery remains the gold standard for the treatment of meniscal injuries. Despite the extensive literature relating to the importance of the meniscus, the literature regarding outcomes following meniscectomy remains limited.
The extent of meniscectomy has been correlated with decreased subjective rating and functional outcome [6]. Rangger et al. found that arthroscopic partial medial and lateral meniscectomy leads to a significant increase in osteoarthritic changes at an average of 4.5 years following surgery [28]. Roos et al. reported a long-term follow-up 19 years following meniscectomy and found an increase in long-term symptoms and functional limitations that were independent of age in the meniscectomized patients compared to controls [29]. Durand et al. looked at gait following partial medial meniscectomy and found that at 8 weeks, the surgical group was performing sub-maximum locomotor activity with reduced range of motion (ROM) and lower levels of muscle contraction compared to healthy controls [9]. However, in all of these studies, the researchers either examined medial meniscus tears alone or grouped both medial and lateral meniscectomies together in their reported outcomes.
There is, to date, very little in vivo research pertaining to the results of isolated partial lateral meniscectomies, though published studies suggest that the outcomes between medial and lateral meniscectomies may be different [25]. There are also no known studies that have evaluated objective functional outcomes following a partial lateral meniscectomy in the athletic population. Therefore, the purpose of this study was to determine whether patients following lateral meniscectomy demonstrate lower extremity asymmetries relative to matched control athletes 3 months after surgery. We hypothesized that following a partial lateral meniscectomy, athletes aged 14–25 years old, would demonstrate altered landing biomechanics during a functional task compared to a sex, age, height, weight, and sport-matched control population.
Materials and methods
Nine patients (7 men and 2 women, 20.1 ± 2.8 years) who had undergone first-time isolated radial lateral meniscus tears were tested 3 months following partial lateral meniscectomies and compared to nine sex, age, height, weight, and sport-matched control subjects (Table 1). Based on the group differences in knee range of motion (mean and standard deviation) from a previous case–control study with similar analyses, we determined that a minimum of 8 subjects were required [13]. At the time of testing, all subjects had undergone a supervised physical therapy program and were discharged to full return to sports activities by an MD. In addition, all subjects completed an informed consent prior to inclusion in this study, and the research was approved by the Cincinnati Children’s Hospital and University of Cincinnati Institutional Review Boards.
Table 1.
Subject demographics
| Patients (n = 9) | Controls (n = 9) | |
|---|---|---|
| Age (years) | 19.7 ± 3.1 | 20.4 ± 2.6 |
| Height (cm) | 181.9 ± 6.6 | 182.5 ± 10.7 |
| Mass (kg) | 88.9 ± 16.7 | 82.9 ± 14.6 |
Inclusion criteria for this study were arthroscopically confirmed isolated radial lateral meniscus tear. For the purpose of this study, an athlete was defined as an individual who participates in athletic activity at least 2 h a session at least three times per week. Subjects were excluded if they had a history of major ligament injury or prior meniscal or ligamentous surgery. In addition, subjects were excluded if they had prior lower extremity injuries where symptoms had not subsided greater than 1 year ago or had a discoid meniscus.
A motion analysis system with ten digital cameras (Eagle Digital, Motion Analysis Corporation) was used in conjunction with two force platforms (Model OR6, AMTI) embedded in the floor. Test–retest reliability comparing the waveform data with coefficients of multiple correlations (CMC) has been previously reported as high for knee flexion angle (r = 0.98) and moment (r = 0.96) during landing [12]. The video was sampled at 240 Hz and time synchronized with the analog force data sampled at 1,200 Hz. Each day prior to data collection, the motion analysis system was calibrated to manufacturer recommendations. An isokinetic dynamometer (System 2, Biodex Medical Systems) was used to test knee extension torque.
Isokinetic testing utilized a counterbalance randomization technique to determine limb order for testing. Isokinetic knee extension (concentric/concentric muscle action) torque was collected with each subject seated on the dynamometer and the trunk perpendicular to the floor, the hip flexed to 90°, and the knee flexed to 90°. Prior to each data collection set, a warm-up set, which consisted of 5 sub-maximal knee flexion/extensions for each leg at 60°/sec and then 300°/s, was performed. The test session consisted of five knee isokinetic extension/flexion (100° to 0° range of motion) repetitions for each leg at 60°/s (Fig. 1) and 10 repetitions at 300°/s. Peak extension torques were recorded (Nm/kg). The isokinetic concentric torque measures of the hamstrings and quadriceps muscles utilized in the current study demonstrate excellent reliability [1].
Fig. 1.
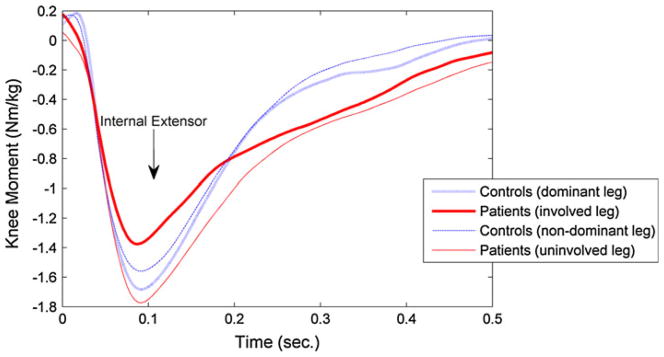
Patients following lateral meniscus surgery exhibited decreased internal knee extensor moment during landing on the involved leg compared to their uninvolved leg and both dominant and non-dominant legs of Controls. Decreasing values represent internal knee extensor moment from the first 0.5 s of a bilateral drop landing
Carefully documented and validated subjective assessment of the patient’s ability to progress in rehabilitation may be a key factor for the determination of an athlete’s readiness to enter a return to sport program. The International Knee Documentation Committee (IKDC) Subjective Knee Form is a reliable and valid tool for the determination of a patient’s rating of their knee symptoms, function, and ability to participate in sport following knee injury, specifically ACL injury [16]. The constructs validated for the IKDC were swelling, pain level, and functional ability [16].
After consent to participate was obtained, the subject completed the IKDC short-form survey [17] and height and weight were recorded. Thirty-seven retroreflective markers were placed on the subject as previously described [11]. A bilateral drop landing was performed from a 31 cm box. We instructed the subjects to “drop down off the box with both feet leaving at the same time.” The task was repeated three times. Motion and force data were imported into Visual3D (Version 3, C-Motion, Inc.) for data reduction and analysis. The three-dimensional Cartesian marker trajectories from each trial were estimated using the direct linear transformation method. The video and force data were filtered at the same cut-off frequency (12 Hz) using a low-pass Butter-worth filter. Peak knee flexion angle and internal extensor moment were calculated from each trial [12].
Statistical analysis
A 2X2 ANOVA was used to test the interaction between side (involved vs. uninvolved) and group (patient vs. control) for the isokinetic torque and biomechanical data. A spearman rank correlation was also performed to correlate knee joint torques (extensor moment during landing) with subjective measures of function (IKDC survey). A P value of less than 0.05 was used to determine statistical significance.
Results
Differences in landing kinetics were observed in patient versus controls. There was a side-by-group interaction for the knee external extensor moment (P = 0.025). Figure 1 shows the kinetic landing results in the patient and control subject cohorts. The patient group landed with a decreased internal knee extensor moment during the drop landing task compared to the uninvolved side and controls (interaction P < 0.05). The mean peak knee extensor moment was −1.5 ± 0.4 Nm/kg for the involved leg and −1.8 ± 0.2 Nm/kg for the non-involved leg of patients (post hoc analysis: P < 0.05 between legs). The mean peak knee extensor moment was −1.7 ± 0.3 Nm/kg on the dominant leg and −1.7 ± 0.3 Nm/kg on the non-dominant leg of control subjects.
Differences in kinematics were observed in patients versus controls. There was a side-by-group interaction for knee flexion angle (P = 0.028). Knee flexion angle was observed to be different between the involved limb and uninvolved limb of patients and control limbs. Figure 2 shows the kinematic landing results in the patient and control subject cohorts. The patient group landed with greater knee flexion angle during the drop landing task compared to controls (interaction P < 0.05). Mean peak knee flexion angle was −70.2 ± 17.4 for the involved leg and −67.5 ± 15.7 for the non-involved leg of patients. Mean peak knee flexion was −58.4 ± 14.3 on the dominant leg and −59.0 ± 13.1 on the non-dominant leg of control subjects.
Fig. 2.
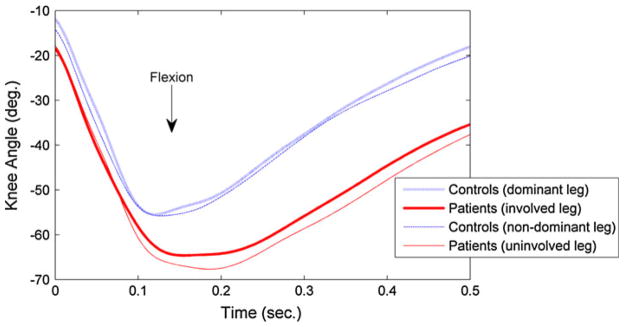
Patients following lateral meniscus surgery exhibited increased knee flexion during landing on their involved and uninvolved legs compared to the dominant and non-dominant legs of Control subjects. Decreasing values represent increased knee flexion from the first 0.5 s of a bilateral drop landing
IKDC scores were significantly related (r = 0.69; P < 0.05) to internal knee extensor moment of the involved limb for the investigational subjects. The average IKDC score was 99.4% for the control subjects and 86.7% for the surgical subjects. Table 2 shows the results of dynamometer testing in the test and control subject cohorts. No differences in isokinetic torque were observed between the involved limb and either the uninvolved side or control limbs at either 60°/s (n.s.) or 300°/s (n.s.)
Table 2.
Isokinetic torque parameters
| Patients (n = 9)
|
Controls (n = 9)
|
|||
|---|---|---|---|---|
| Dominant | Non-dominant | Involved | Uninvolved | |
| Quadriceps torque | ||||
| 60°/s (Nm/kg) | 2.5 ± 0.7 | 2.7 ± 0.7 | 2.7 ± 0.5 | 2.6 ± 0.6 |
| 300°/s (Nm/kg) | 1.6 ± 0.3 | 1.6 ± 0.3 | 1.4 ± 0.2 | 1.4 ± 0.3 |
Discussion
The most salient finding of the present study was that patients following lateral meniscus surgery land with asymmetries which are likely influenced from transference of the knee joint moments to the contralateral lower extremity when compared to controls. It is possible that the decreased knee extensor moment may be indicative of quadriceps weakness. However, the involved limb quadriceps isokinetic torque was not decreased compared to the contralateral or control limbs in unloaded open chain testing (n.s.). The patients appeared to have adopted an increased sagittal plane motion strategy during landing. Similar strategies have been identified and termed either a soft, flexion style landing or a stiff, bounce landing [5, 8]. The “softer” type of landing appeared to be adopted by the patients following lateral meniscus surgery. While this landing strategy does not necessarily indicate a “safer” or less injurious style of landing, it may be a neuromuscular adaptation to compensate for the injured and rehabilitated knee. During gait, a similar pattern of decreased knee extensor moment has been reported with patients following partial meniscectomy [33]. However, the meniscectomy group displayed decreased knee flexion range of motion during gait. This is in contrast to our results during a drop landing with increased knee flexion angle. Our younger population and the relatively more challenging maneuver of a landing compared to gait may explain these differences. Similar results to the current study are evident in young patients with juvenile idiopathic arthritis with increased knee flexion angle and decreased knee extensor moment during bilateral landing compared to controls [13]. Patients after anterior cruciate ligament reconstruction land from a single leg hop with decreased knee flexion range of motion and decreased power absorption on the involved [24]. Landing adaptations likely indicate that normal joint mechanics may not be restored following reconstruction and rehabilitation [24].
Previous authors have suggested that the outcomes following a lateral meniscectomy are worse than those following a medial meniscectomy [7]. For example, Chatain et al. showed that while subjective and clinical results were similar between the two groups, radiographic outcomes following lateral meniscectomy were much worse in comparison with medial meniscectomy [7]. In addition, Pena et al. showed that peak contact stresses are 200% more in the articular cartilage following a lateral meniscectomy compared to a medial meniscectomy [26]. In support of these differences, Levy et al. showed that, contrary to a medial meniscus, the lateral meniscus had insufficient affixations to stabilize the tibia from anterior translation, affecting knee stability [18]. Subtotal medial meniscectomy in ACL deficient knees results in greater tibial lateral shift and anterior translation [30]. The lateral meniscus is a critical secondary knee stabilizer during axial loads [20]. This important functional role may help explain the poor clinical outcomes in patients following lateral meniscectomy, especially concomitant with ACL deficiency or reconstruction [20]. In the most extensive study to compare medial versus lateral arthroscopic partial meniscectomies, in a 10-year follow-up, radiographic results were much worse for the lateral partial meniscectomy as compared to the medial, while subjective and clinical results were similar [7]. Additionally, a recent systematic review related to the risk of knee osteoarthritis indicated that patients following arthroscopic partial lateral meniscectomy had higher incidence of osteoarthritis compared to patients following arthroscopic partial medial meniscectomy [25]. Future studies investigating the biomechanical and neuromuscular adaptations between patients with a partial lateral meniscectomy and partial medial meniscectomy may be warranted.
The findings of this study demonstrate that at 3 months following surgery and supervised rehabilitation, these athletes demonstrate compensatory landing patterns, which do not appear to be related to quadriceps isokinetic measured torque deficits. While all subjects had returned to sports at the testing session, biomechanical deviations compared to the uninjured leg and to controls were observed. Also of note from these findings is that decreased internal knee extensor moments of the involved limb for investigational subjects was related to decreased subjective function. These results agree with previous research that has shown subjective knee surveys to correlate with task performance following knee surgery [19]. Therefore, perceived perception of knee function had a significant carryover into a functional task, as determined by objective measures. However, it should be noted that at 3 months postoperative, the IKDC scores in our current study were higher (87) than previously reported (78) in 104 prospective patients following lateral meniscus lesion [31]. The differences in subjective function likely relate to our younger and more active population. Seventy-one percent of the patients [31] reported sport participation compared to all of the subjects in our current study.
Clinically, isokinetic torque measurements are typically used as an evaluation tool for return to sports capability. However, the results of this study indicate that following lateral meniscectomy, athletes show biomechanical compensation during landing that appears to be independent of their thigh isokinetic torque capacities and these compensation patterns may persist for an undetermined amount of time following surgery. Similarly, concentric quadriceps torque differences in a large cohort of patients 11 weeks following arthroscopic partial meniscectomy showed no related differences in knee extensor moment during gait [32]. Interestingly, Sturnieks and colleagues [32] reported higher knee frontal plane load in the weak quadriceps group compared to subjects who presented with normal quadriceps strength. Additional investigation of the relationship among frontal plane loading, motion, and strength appears to be warranted in patients following meniscus surgery and rehabilitation.
There were limitations to the present study that may decrease the ability to generalize the current results. First, there were a small number of subjects with solely a lateral meniscus injury. Also, this study specifically looked at athletes and not a general population. In addition, the follow-up time was relatively small, at 3 months following surgery. Future studies should include different types of meniscal tears, a larger population of subjects, and later more comprehensive studies would be needed to compare these results to those of medial meniscus tears or false-positive subjects who had arthroscopy but no tear.
The clinical relevance of this work is clearly linked to the identification of limb asymmetries in athletes following isolated meniscectomies after they have been returned to full sport participation. Clinicians should focus on improving quadriceps function during landing on the involved leg in an attempt to decrease residual limb asymmetries and potentially decrease the rate of future injury or decreased function. Innovative motor learning techniques that include feedback may be useful for clinicians to incorporate during late stages of rehabilitation [4, 22, 23]. Furthermore, neuromuscular training programs may be an important component for initially improving and maintaining proper lower extremity biomechanics during landing maneuvers [3, 14, 15, 21].
Conclusions
At approximately 3 months following lateral meniscus surgery and return to sports, athletes continue to demonstrate compensation with landing compared to the uninjured extremity and control subjects, and this compensation may not be solely attributed to isokinetic torque deficits. Biomechanical differences were observed by both a decreased internal knee extension moment and increase in peak knee flexion angle. Further attention may be warranted in returning an athlete to competition following this type of surgery, as the long-term consequences suggest poor long-term outcomes.
Acknowledgments
The authors would like to acknowledge funding support from The University Orthopaedic Research and Education Foundation, University of Cincinnati department of Orthopaedic Surgery and National Institutes of Health/NIAMS Grants R01-AR049735, R01-AR05563 and R01-AR056259.
Contributor Information
Kevin R. Ford, Email: kevin.ford@cchmc.org, Cincinnati Children’s Hospital Medical Center Sports Medicine, Biodynamics Center and Human Performance Laboratory, 3333 Burnet Avenue, MLC 10001, Cincinnati, OH 45229, USA. Department of Pediatrics, College of Medicine, University of Cincinnati, Cincinnati, OH, USA
Stephen J. Minning, Cincinnati Children’s Hospital Medical Center Sports Medicine, Biodynamics Center and Human Performance Laboratory, 3333 Burnet Avenue, MLC 10001, Cincinnati, OH 45229, USA. A Division of Select Medical Corporation, NovaCare Rehabilitation/University of Cincinnati Sports Medicine, Cincinnati, OH, USA
Gregory D. Myer, Cincinnati Children’s Hospital Medical Center Sports Medicine, Biodynamics Center and Human Performance Laboratory, 3333 Burnet Avenue, MLC 10001, Cincinnati, OH 45229, USA. Department of Pediatrics, College of Medicine, University of Cincinnati, Cincinnati, OH, USA. Departments of Physiology and Cell Biology, Orthopaedic Surgery, Family Medicine and Biomedical Engineering, Ohio State University Sports Medicine, Columbus, OH, USA
Robert E. Mangine, A Division of Select Medical Corporation, NovaCare Rehabilitation/University of Cincinnati Sports Medicine, Cincinnati, OH, USA
Angelo J. Colosimo, Department of Orthopaedic Surgery, University of Cincinnati, Cincinnati, OH, USA
Timothy E. Hewett, Cincinnati Children’s Hospital Medical Center Sports Medicine, Biodynamics Center and Human Performance Laboratory, 3333 Burnet Avenue, MLC 10001, Cincinnati, OH 45229, USA. Department of Pediatrics, College of Medicine, University of Cincinnati, Cincinnati, OH, USA. Department of Orthopaedic Surgery, University of Cincinnati, Cincinnati, OH, USA. Departments of Biomedical Engineering and Rehabilitation Sciences, University of Cincinnati, Cincinnati, OH, USA. Departments of Physiology and Cell Biology, Orthopaedic Surgery, Family Medicine and Biomedical Engineering, Ohio State University Sports Medicine, Columbus, OH, USA
References
- 1.Bandy WD, McLaughlin S. Intramachine and intermachine reliability for selected dynamic muscle performance tests. J Orthop Sports Phys Ther. 1993;18:609–613. doi: 10.2519/jospt.1993.18.5.609. [DOI] [PubMed] [Google Scholar]
- 2.Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14:270–275. doi: 10.1177/036354658601400405. [DOI] [PubMed] [Google Scholar]
- 3.Barber-Westin SD, Smith ST, Campbell T, Noyes FR. The drop-jump video screening test: retention of improvement in neuromuscular control in female volleyball players. J Strength Cond Res. 2010;24:3055–3062. doi: 10.1519/JSC.0b013e3181d83516. [DOI] [PubMed] [Google Scholar]
- 4.Benjaminse A, Otten E. Acl injury prevention, more effective with a different way of motor learning? Knee Surg Sports Traumatol Arthrosc. 2010 doi: 10.1007/s00167-010-1313-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bobbert MF, Huijing PA, van Ingen Schenau GJ. Drop jumping. I. The influence of jumping technique on the biomechanics of jumping. Med Sci Sports Exerc. 1987;19:332–338. [PubMed] [Google Scholar]
- 6.Bonneux I, Vandekerckhove B. Arthroscopic partial lateral meniscectomy long-term results in athletes. Acta Orthop Belg. 2002;68:356–361. [PubMed] [Google Scholar]
- 7.Chatain F, Adeleine P, Chambat P, Neyret P. A comparative study of medial versus lateral arthroscopic partial meniscectomy on stable knees: 10-year minimum follow-up. Arthroscopy. 2003;19:842–849. doi: 10.1016/s0749-8063(03)00735-7. [DOI] [PubMed] [Google Scholar]
- 8.DeVita P, Skelly WA. Effect of landing stiffness on joint kinetics and energetics in the lower extremity. Med Sci Sports Exerc. 1992;24:108–115. [PubMed] [Google Scholar]
- 9.Durand A, Richards CL, Malouin F, Bravo G. Motor recovery after arthroscopic partial meniscectomy. Analyses of gait and the ascent and descent of stairs. J Bone Joint Surg Am. 1993;75:202–214. doi: 10.2106/00004623-199302000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Fitzgibbons RE, Shelbourne KD. “Aggressive” nontreatment of lateral meniscal tears seen during anterior cruciate ligament reconstruction. Am J Sports Med. 1995;23:156–159. doi: 10.1177/036354659502300205. [DOI] [PubMed] [Google Scholar]
- 11.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35:1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 12.Ford KR, Myer GD, Hewett TE. Reliability of landing 3d motion analysis: implications for longitudinal analyses. Med Sci Sports Exerc. 2007;39:2021–2028. doi: 10.1249/mss.0b013e318149332d. [DOI] [PubMed] [Google Scholar]
- 13.Ford KR, Myer GD, Melson PG, Darnell SC, Brunner HI, Hewett TE. Land-jump performance in patients with juvenile idiopathic arthritis (jia): a comparison to matched controls. Int J Rheumatol. 2009 doi: 10.1155/2009/478526:478526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34:490–498. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- 15.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes. Decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24:765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 16.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 17.Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80:1132–1145. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Levy IM, Torzilli PA, Gould JD, Warren RF. The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg Am. 1989;71:401–406. [PubMed] [Google Scholar]
- 19.Minning SJ, Myer GD, Mangine RE, Eifert-Mangine M, Colosimo AJ. Serial assessments to determine normalization of gait following anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 2008;19:569–575. doi: 10.1111/j.1600-0838.2008.00818.x. [DOI] [PubMed] [Google Scholar]
- 20.Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38:1591–1597. doi: 10.1177/0363546510364402. [DOI] [PubMed] [Google Scholar]
- 21.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuro-muscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19:51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 22.Myer GD, Paterno MV, Ford KR, Hewett TE. Neuro-muscular training techniques to target deficits before return to sport after anterior cruciate ligament reconstruction. J Strength Cond Res. 2008;22:987–1014. doi: 10.1519/JSC.0b013e31816a86cd. [DOI] [PubMed] [Google Scholar]
- 23.Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2010 doi: 10.1136/bjsm.2009.069112. [DOI] [PubMed] [Google Scholar]
- 24.Orishimo KF, Kremenic IJ, Mullaney MJ, McHugh MP, Nicholas SJ. Adaptations in single-leg hop biomechanics following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1587–1593. doi: 10.1007/s00167-010-1185-2. [DOI] [PubMed] [Google Scholar]
- 25.Papalia R, Del Buono A, Osti L, Denaro V, Maffulli N. Meniscectomy as a risk factor for knee osteoarthritis: a systematic review. Br Med Bull. 2011 doi: 10.1093/bmb/ldq043. [DOI] [PubMed] [Google Scholar]
- 26.Pena E, Calvo B, Martinez MA, Palanca D, Doblare M. Why lateral meniscectomy is more dangerous than medial meniscectomy. A finite element study. J Orthop Res. 2006;24:1001–1010. doi: 10.1002/jor.20037. [DOI] [PubMed] [Google Scholar]
- 27.Petrosini AV, Sherman OH. A historical perspective on meniscal repair. Clin Sports Med. 1996;15:445–453. [PubMed] [Google Scholar]
- 28.Rangger C, Klestil T, Gloetzer W, Kemmler G, Benedetto KP. Osteoarthritis after arthroscopic partial meniscectomy. Am J Sports Med. 1995;23:240–244. doi: 10.1177/036354659502300219. [DOI] [PubMed] [Google Scholar]
- 29.Roos EM, Ostenberg A, Roos H, Ekdahl C, Lohmander LS. Long-term outcome of meniscectomy: symptoms, function, and performance tests in patients with or without radiographic osteoarthritis compared to matched controls. Osteoarthr Cartil. 2001;9:316–324. doi: 10.1053/joca.2000.0391. [DOI] [PubMed] [Google Scholar]
- 30.Seon JK, Gadikota HR, Kozanek M, Oh LS, Gill TJ, Li G. The effect of anterior cruciate ligament reconstruction on kinematics of the knee with combined anterior cruciate ligament injury and subtotal medial meniscectomy: an in vitro robotic investigation. Arthroscopy. 2009;25:123–130. doi: 10.1016/j.arthro.2008.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Servien E, Acquitter Y, Hulet C, Seil R. Lateral meniscus lesions on stable knee: a prospective multicenter study. Orthop Traumatol Surg Res. 2009;95:S60–S64. doi: 10.1016/j.otsr.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 32.Sturnieks DL, Besier TF, Hamer PW, Ackland TR, Mills PM, Stachowiak GW, Podsiadlo P, Lloyd DG. Knee strength and knee adduction moments following arthroscopic partial meniscectomy. Med Sci Sports Exerc. 2008;40:991–997. doi: 10.1249/MSS.0b013e318167812a. [DOI] [PubMed] [Google Scholar]
- 33.Sturnieks DL, Besier TF, Mills PM, Ackland TR, Maguire KF, Stachowiak GW, Podsiadlo P, Lloyd DG. Knee joint biomechanics following arthroscopic partial meniscectomy. J Orthop Res. 2008;26:1075–1080. doi: 10.1002/jor.20610. [DOI] [PubMed] [Google Scholar]


