Abstract
Background
Recent trends indicate research targeting outcomes of importance to people with disabilities, such as spinal cord injury (SCI), may be best informed by those individuals; however, there are very few published rehabilitation intervention studies that include people with disabilities in the research process in a role beyond study participant.
Objective
To describe a community-based participatory research (CBPR) approach to the development and pilot testing of an intervention using community-based Peer Navigators with SCI to provide health education to individuals with SCI, with the goal of reducing preventable secondary conditions and rehospitalizations, and improving community participation.
Methods
A CBPR framework guides the research partnership between academic researchers and a community-based team of individuals who either have SCI or provide SCI-related services. Using this framework, the processes of our research partnership supporting the current study are described including: partnership formation, problem identification, intervention development, and pilot testing of the intervention. Challenges associated with CBPR are identified.
Results
Using CBPR, the SCI Peer Navigator intervention addresses the partnership’s priority issues identified in the formative studies. Utilization of the framework and integration of CBPR principles into all phases of research have promoted sustainability of the partnership. Recognition of and proactive planning for challenges that are commonly encountered in CBPR, such as sharing power and limited resources, has helped sustain our partnership.
Conclusions
The CBPR framework provides a guide for inclusion of individuals with SCI as research partners in the development, implementation, and evaluation of interventions intended to improve outcomes after SCI.
Keywords: spinal cord injury, community-based participatory research, intervention, navigation, secondary conditions
Introduction
CBPR in Disability and Rehabilitation Research
A recent review of the rehabilitation literature revealed there are very few published rehabilitation intervention studies that include people with disabilities in research in a role beyond study participant.1 Research implemented with the goal of improving the lives of persons with disabilities, such as spinal cord injury (SCI), must reflect the demands of living in their environment of choice and engaging in activities that are of importance to them.2 The disability community has expressed a need for inclusive, action-based research methodologies in which people with disabilities function as partners and consultants, not as research subjects.3 Disability scholars emphasize that research involving people with disabilities should embrace respect for human rights, and work towards the advancement of social justice for people with disabilities.4
Developing a program of disability research that does not marginalize people with disabilities but promotes empowerment and autonomy can be challenging, especially for the able-bodied researcher. A community-based participatory research (CBPR) approach engages community members as decision-making partners in the research process and provides a means to elicit community concerns and priorities that otherwise might not enter into the researchers’ agenda.5,6 Additionally, community members can advise about suitable research processes that are respectful of and acceptable to the community. Ideally, CBPR processes promote shared ownership of research projects between academic investigators and participants, provide for community-based analysis of social problems, and support interventions that involve community action.7 The fundamental principles of CBPR position the community as an equal partner in all phases of research, from defining the research question to knowledge dissemination.8 The processes of CBPR build upon the community’s strengths, ensure local relevance, and promote capacity building and, more specifically, engage people with disabilities, such as SCI, as partners in research.8, 9 Additionally, participatory approaches to disability and rehabilitation research hold the potential to temper threats to the social validity of research, defined as the “extent to which potential adopters of research products judge them as useful and actually use them”(p. S20).10
Although CBPR has many advantages, there are also associated challenges. Barriers created by academic institutional practices, such as research ethics boards and university reimbursement processes are commonly cited.11,12 CBPR requires increased time and resources to facilitate partnerships, including establishing a trusting relationship and providing training.13,14 Building and maintaining the equitable partnerships required for CBPR is a complex process that requires consistent attention to power, accountability, and ownership of the products of research within the partnership.11-14
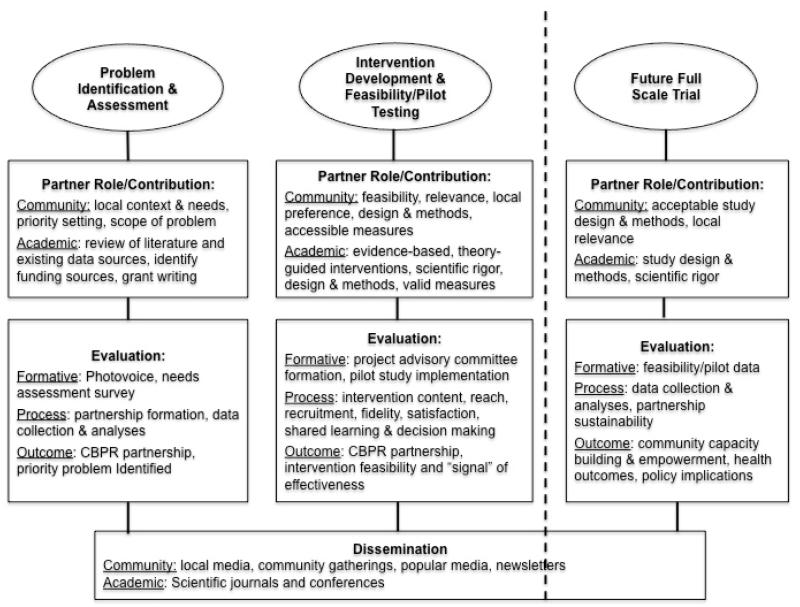
In this paper we describe a CBPR framework (Figure 1) to inform intervention research.15 Our current study investigates using community-based Peer Navigators with SCI to provide health education and support to individuals with SCI, with the goal of reducing preventable secondary conditions and rehospitalizations, and improving community participation. Guided by this framework, we describe the processes and related activities and outcomes of our seven-year research partnership supporting the current SCI Peer Navigator study including: partnership, problem identification, intervention development, and pilot testing of the intervention (Table 1). Additionally, we describe challenges we encountered and addressed.
Figure 1.
CBPR framework to guide intervention research
Table 1. Timeline, processes, and activities of CBPR collaboration for intervention development.
| Time | Process | Activities |
|---|---|---|
| 2006 - 2007 |
Partnership Development |
|
| 2008 - 2010 |
Problem Identification |
|
| 2011 - 2012 |
InterventionDevelopment |
|
| 2012- Present |
Proof of Concept & Pilot testing |
|
CBPR = Community-based Participatory Research, dRC = disAbility Resource Center, CTSA = Clinical & Translational Science Award, AP = Academic partner, CP = Community Partner, SCI = Spinal Cord Injury, PN = Peer Navigator, CITI = Collaborative Institutional Training Initiative
Methods
CBPR Processes & Outcomes
Partnership
New partnerships are often encouraged to start small and involve a few community-based organizations that are highly regarded by community members.16,17 With this in mind in 2006, the academic researcher (SN) sought to establish a relationship with the disAbility Resource Center (dRC), a Center for Independent Living (CIL) in North Charleston, SC. Since this was a first attempt by an academic researcher to engage individuals with SCI in a CBPR study in our community, the researcher volunteered with the dRC for several months to develop a relationship with the organization prior to initiating development of a research partnership. The leadership and staff of the dRC appreciated the value of research to support advocacy efforts i.e., “evidence-based advocacy,” thus were ready to engage a research partnership. The dRC executive director and peer counselor became the primary representatives of the agency who helped guide the development and implementation of our initial study together. As participants enrolled in the study, they also provided input into the proceeding of study implementation and dissemination, becoming an informal advisory board for the partnership.
Over time, as we narrowed our focus on the needs of people with SCI, and simultaneously sought to expand the reach of our research, we began to identify and engage other potential research partners.17 In, 2010, our research team sought collaboration with the South Carolina Spinal Cord Injury Association (SCSCIA). The SCSCIA, based in Columbia, SC, provides a statewide resource for SCI-related information, education, and support. Our initial relationship with the SCSCIA was facilitated by two of our team members who served on the board of directors, as well as the SCSCIA’s interest in growing collaborations supporting the agency’s mission. The SCSCIA initially provided support to the partnership by facilitating distribution of a needs assessment survey, however their involvement has grown into a more significant role by contributing to intervention development and pilot testing, and serving as a study site.
The most recent expansion of the partnership includes the Center for Spinal Cord Injury (CSCI), in Charleston, SC, which provides SCI-specialized medical and rehabilitation services. An existing relationship with the academic researcher, who had previously worked as a nurse at the rehabilitation facility, enabled collaboration with the CSCI. The rehabilitation hospital initially engaged the academic researcher for assistance in developing an inpatient SCI Peer Mentoring program, and this created a natural progression to the CSCI’s support of our community-based Peer Navigator study. Currently, the CSCI serves as a primary recruitment site, but also provides ongoing support as a healthcare resource for our current study.
Problem Identification
Photovoice
The initial research partnership between the academic researcher and the dRC supported a study using Photovoice as a needs assessment and issue selection tool. Photovoice is a qualitative participatory research method that capitalizes on the power of photography.18 The 3 goals of Photovoice are to enable people to document the community’s strengths and concerns from their perspective through photography, promote knowledge through discussion of photographs, and reach “policy makers” and others who can be mobilized for change.18 Our partnership’s first study implemented the Photovoice method with a group of 10 people with SCI to gather evidence of the environmental factors affecting their participation in the community.19,20
One of the most striking findings from this research was the repeated theme of difficulty in identifying and accessing essential resources, such as durable medical equipment, health care, vocational rehabilitation, and adapted driving training. Participants often related stories of their frustrations in dealing with lack of responsiveness and understanding of SCI by many service providers in our community. Many participants expressed a desire to assist others with SCI in the hopes that they could share knowledge gained through their experiences in navigating “the system.” Data from this study informed the initial idea of the SCI Peer Navigator intervention. Additionally, this study supported the establishment of a strong and ongoing partnership with a community-based cohort of people with SCI, as well as a community agency that supports independent living of individuals with disabilities.
Needs Assessment Survey
Our partnership developed and implemented a local SCI consumer needs assessment survey to supplement data generated by the Photovoice study. Although a small pilot study, the survey allowed our partnership to begin to quantify, and thus prioritize and address the service needs of individuals with SCI and associated barriers encountered in our community. Consistent with CBPR best processes,21 we formed a Survey Steering Committee, composed of community members with SCI, dRC staff, and the researcher. The Steering Committee facilitated a process of shared decision-making among the partners to assure that diverse needs were identified and addressed. Activities of the Steering Committee are described in Table 1.
The survey was distributed to individuals with SCI, for whom the SCSCIA had contact information and lived within the 5 county service area of the dRC, via the Internet, mail, and telephone, with the majority of respondents returning completed surveys by mail (78%). Demographic and injury characteristics of the respondents (n=73, 56% response rate) are provided in Table 2. Education level was high, with 88% reporting high school or college as the highest level of education completed. The majority of respondents lived in areas classified as urban (75%).22
Table 2.
Demographic and injury characteristics of survey respondents
| n(%) | |
|---|---|
| Gender | |
| Male | 52(71.2) |
| Female | 21(29.8) |
| Race | |
| White | 41(56.2) |
| Black | 30(41) |
| Native American/Alaska Native | 1(1.4) |
| Other | 1(1.4) |
| Ethnicity | |
| Hispanic | 2(3) |
| Non-Hispanic | 71(97) |
| Level of Injury | |
| Cervical | 37(50.7) |
| Non-cervical | 32(43.8) |
| I don’t know | 4(5.5) |
| Severity of Injury | |
| Complete | 20(27.4) |
| Incomplete | 52(71.2) |
| I don’t know | 2(1.4) |
Key findings of the survey included: 60% of participants reported urinary tract infections (UTI) requiring medical attention and 42% reported experiencing pressure ulcers (PU) within the past year; 68% reported needing help getting or managing services after SCI; and “I didn’t know where to get help” was the most commonly reported barrier (35.3%). Cost was the most frequently reported barrier for those who reported an unmet personal assistance (38.7%), medical (25%) or assistive technology (41.9%) need. 73% of respondents indicated that they would benefit from working with someone who also had an SCI and had received additional training on accessing SCI information and resources.
Our Steering Committee noted the majority of our survey respondents were well educated and lived in urban areas, and recognized the limitation of our results in reflecting the broader population with SCI in SC, which is largely a rural state. We surmised that by using the SCSCIA membership roster to recruit, we were sampling individuals who had the means to engage a community resource. This observation lead to discussions on how our team could connect with individuals with SCI, who were potentially more isolated in rural areas with less access to resources. The committee recognized, even with our limited sample, our survey results indicated that people with SCI in our community are experiencing potentially preventable secondary conditions and report challenges in knowing where to turn for help. The committee acknowledged, while we would not be able to directly address the financial barriers reported by many of our respondents, we had the resources to develop an intervention to support accessing SCI-related information and services in our community.
Results
Intervention Development
Building on evidence from our formative work and other fields, such as cancer care,23,24 we proposed an intervention using community-based “peer navigators” with SCI to provide tailored health education, proactively mitigate barriers, and facilitate access to community-based services by people with SCI. “Peer Navigators” in the context of SCI are people with SCI who have a wealth of knowledge from their personal experiences and are ready to share what they have learned with others with SCI. The primary goals of our intervention are to reduce preventable secondary conditions (UTI and PU) and rehospitalizations, and improve the community participation of individuals with SCI. Moving into the intervention development phase, our Survey Steering Committee expanded into a 12-member, self-named “SCI Peer Navigator Task Force.” During this formative phase, the value of the shared contributions of all partners to intervention development was evident. We identified one existing SCI Navigator program at the National Rehabilitation Hospital (NRH) in Washington, DC.25 The NRH SCI Navigator program was hospital-based, and located in an urban, inner city environment served by a large rehabilitation facility with nationally recognized SCI expertise. Our community team members identified the need to make modifications to the NRH program to meet the goals of our community-based program and address the specific context of our community in South Carolina, which is less urban with fewer SCI specialized services and resources. Key components of our SCI Peer Navigator intervention include 4 weekly in-person sessions in participants’ homes for health education, goal setting, and barrier identification, with scheduled follow-up contacts of decreasing frequency over the remainder of the intervention to address progress to goals, barriers encountered, skin or bladder issues, or hospitalization since last contact.
Pilot Testing
Pilot testing provides data to evaluate multiple aspects of intervention feasibility including participant recruitment, randomization, and retention, methods and measures, and intervention implementation.26 Currently we are conducting an exploratory trial of the SCI Peer Navigator intervention at two sites in South Carolina. We initially conducted a small 6-month “proof of concept” trial (n=4). The proof of concept trial allowed us to assess the logistics of the Peer Navigators conducting the intervention in study participants’ homes. During intervention development, the Task Force recognized the potential of limited transportation for some study participants, thus we decided to test administering the intervention in participants’ homes. Accordingly, study inclusion criteria require living in a wheelchair accessible home, however we set up a process for assistance referral for anyone identified as living in an inaccessible home during screening. The brief proof of concept trial is followed by a 9-month pilot randomized trial (n=20), adding a non-navigated control group that receives bi-monthly mailed educational materials with follow-up phone calls.
Preliminary evaluations indicate a positive effect in improvement of pressure ulcers present on enrollment, and increased participation in productive and preferred community activities. As the study progresses, the Task Force is involved in ongoing process evaluation, provides guidance and feedback to the Navigators, assists with recruitment, makes recommendations to refine and improve the intervention, and will ultimately assist with data interpretation and dissemination (Table 1).
Discussion
In this paper, we described a CBPR approach to intervention research. While CBPR clearly supports the development of scientifically valid interventions and the translation of research results into sustainable community change, the principles that guide CBPR are recognized as exemplars that partnerships are constantly challenged to achieve.21,27-30 An essential element of our sustained partnership is participation by the academic and community partners, together, in formal training on the principles and processes of CBPR. This training facilitated our recognition of, and proactive planning for, challenges that are commonly encountered in CBPR, such as sharing power and maximizing limited time and resources. This insight has helped our partnership avoid many of the pitfalls that often lead to dissolution of partnerships.
Historically, the distribution of power and control of resources has overwhelmingly favored the academic partner. In our partnership, balancing power among partners who represent diverse abilities, socioeconomic status, and education level is challenging. One of the ways we strive to maintain sharing of power is through recognition and mutual respect of the expertise that each partner brings to the team. The academic brings knowledge of the science of intervention research (planning, implementation, and evaluation) to the partnership’s initiatives, while the community partners establish the context (i.e. the how, when, and where) to apply the science within the community. The development of mutual respect was not a single occurrence, but a process that occurred over time. Actions, such as following through with delegated responsibilities or engaging in respectful debate, often tempered with humor, during meetings, demonstrated accountability and respect to the team and subsequently supported the development of trust and respect among the partners.
We attempt to maintain an equal sharing of resources and responsibilities between the academic and community partners within our funders’ guidelines. To date, all of our funding opportunities have disallowed subcontracts that would provide funds directly to the community partners. Although we were precluded from directly paying our task force members, we discussed options for providing recognition and compensation for participation in meetings. While many members stated they did not want to be paid, the group decided that having a meal at each meeting would be acceptable compensation. Our partnership openly discussed the financial aspects of working together and developed a mutual understanding that the initial, low budget pilot projects would support the development of applications for larger grant awards with the opportunity to share financial resources, including payment to task force members. Recent initiatives by funding agencies, such as the Patient Centered Outcomes Research Institute (PCORI) now require genuine community and stakeholder engagement in research and have facilitated processes that allow distribution of funding to non-academic partners.
Many practitioners of CBPR have noted the additional time requirement, and our partnership has not escaped this challenge.13,14 Our 7-year history presents a different timeline of processes than a “traditional” research approach in which the academic PI controls problem identification, selection and implementation of interventions, and progression of the project. The development of our Peer Navigator training manual took several months as various members of the Task Force took primary responsibility, based on their expertise, for writing sections of the manual. We held bi-weekly meetings during this phase of the project, and occasionally not all members had completed their “homework” by the next meeting and required additional time. However, because we had established agreement to value everyone’s expertise and input, we were willing to be flexible to accommodate others’ work style or provide assistance as needed. Additionally, significant time was spent addressing Human Subjects Protections requirements, which included obtaining certificates of Federalwide Assurance for the Protection of Human Subjects (FWA) for the community agencies, and completion of the Collaborative Institutional Training Initiative (CITI) training of the Peer Navigators and the community site coordinators. The academic researcher collaborated with the IRB and received permission to provide a facilitated CITI training.
An additional challenge that we face, for which we have not yet identified a clear solution, is assuring appropriate representation of the broader SCI community in South Carolina on our Task Force. Similar to the limitations we encountered with our needs assessment survey, the members of our Task Force have access to resources, such as transportation, and had an existing relationship with one of our partnering community organizations. Our concern is we potentially lack clear insight into the priorities of more marginalized individuals, thus we are currently seeking to engage the collaboration of a state agency that provides services to this population.
Even in the presence of the challenges we have faced, a CBPR approach has provided the framework to allow our partnership to include people with disabilities in meaningful roles throughout the research process. The nature of CBPR supports the identification of factors affecting health after SCI from the perspective of those experiencing them, and in turn, guides the development of SCI health promotion interventions addressing the unique community-based needs of people with SCI.
Conclusion
Our research partnership’s approach to improve health and community participation in people with SCI complements the philosophy of independent living that seeks to empower people with disabilities to exert control in their lives. The CBPR framework provides a guide for inclusion of individuals with SCI as research partners in the development, implementation, and evaluation of interventions intended to improve outcomes after SCI.
Acknowledgements
The authors wish to acknowledge and thank all those who have supported and contributed to this work, including the staff of the disAbility Resource Center and the Center for Spinal Cord Injury, the staff and board of directors the South Carolina Spinal Cord Injury Association, and members of our Steering Committee and Task Force, past and present, who graciously shared their expertise and time.
Funding: Research reported in this paper was supported by the Agency for Healthcare Research and Quality under award number R36HS016941, the Rehabilitation Nursing Foundation, the South Carolina Clinical & Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina, through NIH Grant Number UL1 TR000062, and the National Institute of Child Health and Human Development of the NIH under award number K23HD062637. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality, the Rehabilitation Nursing Foundation, or the National Institutes of Health.
Footnotes
Disclosure of financial interests and potential conflicts of interest: None of the authors have any financial interests or potential conflicts of interest relating to this manuscript to disclose.
The information in this paper was previously presented in poster format at the Science of Community Engaged Research: Future Directions Conference, August 2013, Bethesda, MD.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Susan D. Newman, Medical University of South Carolina (MUSC), College of Nursing, 99 Jonathan Lucas St, MSC 160, Charleston, SC 29425.
Gwen Gillenwater, disAbility Resource Center (former Executive Director).
Sherwood Toatley, South Carolina Spinal Cord Injury Association, MUSC College of Nursing.
Marka D. Rodgers, Center for Spinal Cord Injury, MUSC College of Nursing
Nathan Todd, disAbility Resource Center.
Diane Epperly, South Carolina Spinal Cord Injury Association.
Jeannette O. Andrews, University of South Carolina College of Nursing.
References
- 1.Ehde DM, Wegener ST, Williams RM, et al. Developing, testing and sustaining rehabilitation interventions via participatory action research. Arch Phys Med Rehabil. 2013;94(1 Suppl 1):S30–42. doi: 10.1016/j.apmr.2012.10.025. [DOI] [PubMed] [Google Scholar]
- 2.Kitzman PH, Hunter EG. Developing a community based rehabilitation network for people with spinal cord injury: a case study in Appalachian Kentucky. J Rural Comm Develop. 2011;6(1):95–104. [Google Scholar]
- 3.Oliver M. Emancipatory research: Realistic goal or impossible dream? In: Barnes C, Mercer G, editors. Doing disability research. The Disability Press; Leeds: 1997. pp. 15–31. [Google Scholar]
- 4.Kitchin R. The researched opinions on research: Disabled people and disability research. Disabil and Society. 2000;15(1):25–47. [Google Scholar]
- 5.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu. Rev. Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 6.Wallerstein N, Duran B. The conceptual, historical, and practice roots of community based participatory research and related participatory traditions. In: Minkler M, Wallerstein N, editors. Community based participatory research for health: From process to outcomes. 2nd ed. Jossey-Bass; San Francisco: 2008. pp. 27–52. [Google Scholar]
- 7.Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7:312–323. doi: 10.1177/1524839906289376. [DOI] [PubMed] [Google Scholar]
- 8.Israel BR, Eng E, Schulz AJ, Parker EA, editors. ed. Jossey-Bass; San Francisco, CA: 2005. Methods in Community-Based Participatory Research for Health. [Google Scholar]
- 9.Hassouneh D, Alcala-moss A, McNeff E. Practical strategies for promoting full inclusion of individuals with disabilities in community-based participatory intervention research. Res Nurs and Health. 2011;34:253–265. doi: 10.1002/nur.20434. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seekins T, White GW. Participatory action research designs in applied disability and rehabilitation science: protecting against threats to social validity. Arch Phys Med Rehabil. 2013;94(1Suppl 1):S20–29. doi: 10.1016/j.apmr.2012.07.033. [DOI] [PubMed] [Google Scholar]
- 11.Durham Community Research Team . Community-based participatory research: ethical challenges. Centre for Social Justice and Community Action, Durham University; Durham, UK: c2011. [cited 2014 Mar 10] Available from: https://www.dur.ac.uk/resources/beacon/CCDiscussionPapertemplateCBPRBanksetal7Nov2011.pdf. [Google Scholar]
- 12.Freeman E, Brugge D, Bennett-Bradley WM, Levy JI, Carrasco ER. Challenges of conducting community based participatory research in Boston’s neighborhoods to reduce disparities in asthma. Journal of Urban Health. 2006;83(6):1013–1021. doi: 10.1007/s11524-006-9111-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Strickland J. Challenges in community-based participatory research implementation: experiences in cancer prevention with Pacific Northwest American Indian tribes. Cancer Control. 2006;13(3):230–236. doi: 10.1177/107327480601300312. [DOI] [PubMed] [Google Scholar]
- 14.Turnbull AP, Friesen BJ, Ramierez C. Participatory action research as a model for conducting family research. Research and Practice for Persons with Disabilities. 1998;23(3):178–188. [Google Scholar]
- 15.Andrews JO, Tingen MS, Crawford Jarriel S, et al. Application of a CBPR framework to inform a multi-level tobacco cessation intervention in public housing neighborhoods. Am J Community Psychol. 2012;50(1-2):129–40. doi: 10.1007/s10464-011-9482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Israel BA, Lichtenstein R, Lantz P, et al. The Detroit Community-Academic Urban Research Center: lessons learned in the development, implementation, evaluation of a community-based participatory research partnership. J. Public Health Manag. Pract. 2001;7(5):1–19. doi: 10.1097/00124784-200107050-00003. [DOI] [PubMed] [Google Scholar]
- 17.Beach Center on Disability . Tips for researchers using PAR for the first time. University of Kansas; Lawrence, KS: c2014. [cited 2014 Mar 10]. Available from: http://www.beachcenter.org/resource_library/beach_resource_detail_page.aspx?intResourceID=79&Type=tip. [Google Scholar]
- 18.Wang C, Burris MA. Photovoice: concept, methodology, and use for participatory needs assessment. Health Educ Behav. 1997;24(3):369–387. doi: 10.1177/109019819702400309. [DOI] [PubMed] [Google Scholar]
- 19.Newman SD, SCI Photovoice Participants Evidence-based advocacy: using photovoice to identify barriers and facilitators to community participation after spinal cord injury. Rehabil Nurs. 2010;35(2):47–59. doi: 10.1002/j.2048-7940.2010.tb00031.x. [DOI] [PubMed] [Google Scholar]
- 20.Newman SD, Maurer D, Jackson A, et al. Gathering the evidence: photovoice as a tool for disability advocacy. Prog Comm Health Partnership. 2008;3(2):139–144. doi: 10.1353/cpr.0.0074. [DOI] [PubMed] [Google Scholar]
- 21.Newman SD, Andrews JO, Magwood GS, et al. Community advisory boards in community-based participatory research: a synthesis of best processes. Prev Chronic Dis. 2011;8(3):A70. [cited November 25, 2013] Available from: http://www.cdc.gov/pcd/issues/2011/may/10_0045.htm. [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Medicare and Medicaid National Breakout of geographic area definitions by zip code. c2014 [updated 2014 Feb 10; cited 2014 Mar 10]. Available from: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AmbulanceFeeSchedule/
- 23.Calhoun EA, Whitley EM, Esparza A, et al. A National Patient Navigator Training Program. Health Promot Pract. 2010;11(2):205–215. doi: 10.1177/1524839908323521. [DOI] [PubMed] [Google Scholar]
- 24.Freeman HP. Patient Navigation: A Community Based Strategy to Reduce Cancer Disparities. J Urban Health. 2006;83:139–141. doi: 10.1007/s11524-006-9030-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Capital Spinal Cord Injury Model System: 2006-2011 SCI Navigator Program. c2013 [cited November 26, 2013]. Available from: http://dcscims.org/research/sci-navigator-program.
- 26.Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011 May;45(5):626–9. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Institutes of Health Community Participation in Research (R01) PAR-07-283. 2008 http://grants.nih.gov/grants/guide/pa-files/PAR-07-283.html. Accessed [March 10, 2014]
- 28.National Institutes of Health Community participation research targeting the medically underserved (R01) 2009 http://grants.nih.gov/grants/guide/pa-files/PAR-08-075.html. Accessed [March 10, 2014]
- 29.Israel BA, Schulz A, Parker EA, Becker AB, Allen AJ, Guzman JR. Critical issues in developing and following CBPR principles. In: Minkler M, Wallerstein N, editors. Community-based participatory research for health: From process to outcomes. 2 nd ed. Jossey-Bass; San Francisco: 2008. pp. 47–66. [Google Scholar]
- 30.Mercer SL, Green LW, Cargo M, et al. Reliability-tested guidelines for assessing participatory research projects. In: Minkler M, Wallerstein N, editors. Community-based participatory research for health: From process to outcomes. 2 nd ed. Jossey-Bass; San Francisco: 2008. pp. 407–418. [Google Scholar]