Abstract
Domestic dogs and cats are commonly infected with a variety of protozoan enteric parasites, including Blastocystis spp. In addition, there is growing interest in Blastocystis as a potential enteric pathogen, and the possible role of domestic and in-contact animals as reservoirs for human infection. Domestic animals in shelter environments are commonly recognized to be at higher risk for carriage of enteropathogens. The purpose of this study was to determine the frequency of infection of shelter-resident and client-owned domestic dogs and cats with Blastocystis spp in the Pacific Northwest region of the USA. Fecal samples were collected from 103 shelter-resident dogs, 105 shelter-resident cats, 51 client-owned dogs and 52 client-owned cats. Blastocystis were detected and subtypes assigned using a nested PCR based on small subunit ribosomal DNA sequences. Shelter-resident animals were significantly more likely to test positive for Blastocystis (P<0.05 for dogs, P = 0.009 for cats). Sequence analysis indicated that shelter-resident animals were carrying a variety of Blastocystis subtypes. No relationship was seen between Blastocystis carriage and the presence of gastrointestinal disease signs in either dogs or cats. These data suggest that, as previously reported for other enteric pathogens, shelter-resident companion animals are a higher risk for carriage of Blastocystis spp. The lack of relationship between Blastocystis carriage and intestinal disease in shelter-resident animals suggests that this organism is unlikely to be a major enteric pathogen in these species.
Introduction
Companion animals (specifically, domestic dogs and cats) are prone to several protozoan gastrointestinal infections, with Giardia duodenalis [syn. G. lamblia, G. intestinalis] and Cryptosporidium parvum both being of significant concern in animals with gastrointestinal disease, and as potential zoonotic infections [1], [2]. Recently, increasing interest has been given to the stramenopile organism Blastocystis spp. as a potential cause of gastrointestinal disease in human beings [3], [4]. While the putative link between Blastocystis infection and gastrointestinal disease is not without controversy [5]–[7], a growing body of evidence suggests that Blastocystis is able to produce cysteine proteinases that mediate interleukin-8 release from enterocytes [8], while also potentially evading recognition by Toll-like receptors [9].
The prevalence of both Blastocystis spp. and Giardia spp. show marked variations depending upon geographical location and the host species of interest [10]–[12]. In the domestic dog, carriage rates for Blastocystis spp. as high as 70% were reported from culture-based studies in shelter-resident dogs in a subtropical environment [13], while more recent studies from essentially the same location found markedly lower prevalence using molecular methods [14].
The purpose of the study described here was to estimate the prevalence of Blastocystis spp. in shelter-resident and client-owned companion animals in the US Pacific Northwest region, a geographic region characterized by a moderate, maritime climate. This region has previously been reported to have “hyperendemism” for enteric protozoan infection (specifically, Giardia spp.) in a large scale study of fecal samples from dogs submitted for parasitological examination to a commercial laboratory [15]. We hypothesized that shelter-resident dogs and cats would show higher carriage rates for Blastocystis than client-owned dogs, and that Blastocystis infection would be associated with greater risk of gastrointestinal symptoms in shelter-resident animals.
Materials and Methods
Sample collection
Canine and feline stool samples were collected from the Oregon Humane Society facility in Portland, Oregon, and from the Heartland Humane Society facility in Corvallis, Oregon, throughout the summer months of 2012. A minimum of 50 samples from each species of interest (i.e. 50 dogs, 50 cats) were collected from each site, resulting in a total collection of 103 samples from shelter resident dogs and 105 samples from shelter-resident cats. Historical data regarding the stay duration of each animal, breed and estimated age and the presence of gastrointestinal signs while shelter resident were obtained from the computerized records of each shelter and consolidated.
Samples from client-owned control animals were collected from animals belonging to the faculty, staff and students of the College of Veterinary Medicine at Oregon State University and by collection of left over stool samples provided by clients presenting their animals for wellness/vaccination visits at two local veterinary hospitals, one in the south east of the city of Portland, Oregon (VCA South East Portland), and one in the city of Salem (VCA South Salem). This last practice is geographically located approximately halfway between the Corvallis and Portland sites. A minimum of 50 samples from each species of interest was collected, for a total of 103 samples from client owned animals. Data on breed, age, use of anthelmintic medications and the presence of gastrointestinal disease signs in the last 1 and 4 weeks were collected for each sample.
The Oregon State University Institutional Animal Care and Use Committee (IACUC) oversaw all animal use. As this study used only volunteered fecal samples collected after spontaneous defecation, this study was exempt from full IACUC approval. Owners of client-owned animals provided consent for the use of samples from their animals in this study. Collection of samples from the Oregon Humane Society facility in Portland, Oregon, the VCA hospital in South East Portland, Oregon and the VCA hospital in Salem, Oregon was carried out with the full cooperation and knowledge of the medical directors at the respective sites. No endangered or protected species were studied.
Stool samples were stored frozen (−20°C) until further processing.
Blastocystis control culture
As a source of positive control DNA, Blastocystis hominis (Subtype I; American Type Culture Collection, Manassas, VA) were anaerobically cultured in a biphasic medium of inspissated whole egg slants overlaid with 4.5 ml Stone's modification of Locke's solution and 25% heat-inactivated horse serum (ATCC medium 1671), and incubated at 35°C.
DNA extraction
For positive controls, cultivated Blastocystis hominis organisms were isolated from cultures and washed 2 times in fresh Locke's solution. Harvested organisms were added to 0.2 grams of Blastocystis-negative dog feces to produce a spiked positive control. DNA was extracted using a commercial DNA extraction kit (QIAmp DNA Stool Mini Kit, Qiagen, Valencia, CA) following the manufacturer's protocol, with DNA extracts eluted in 100 µl of AE buffer. Fecal samples previously tested negative for Blastocystis spp were used as negative controls. DNA was stored at −70°C until used. Each DNA extraction batch included a spiked canine fecal sample as a positive control.
For shelter-resident and client-owned canine and feline samples, DNA from 0.20 grams of feces was extracted as described above. The resulting filtrates containing DNA were aliquoted and stored at −70°C until analyzed.
Amplification and sequencing
The SSU rDNA fragment of Blastocystis was amplified using a nested-PCR protocol. Briefly, an approximately 600 base pair fragment of the SSU rDNA was initially amplified using the previously published primers BhRDr and BH1F [1], [16] in a 25 pmol/25 µl reaction using 2 mM MgSO4, 0.2 mM deoxynucleoside triphosphates, 2.5 µg BSA and 1 units of Platinum Taq High-Fidelity DNA polymerase (Invitrogen) with 1 µl of DNA template. Reaction cycles consisted of denaturing step of 94°C for 1 minute, and 30 cycles at 94°C for 1 minute, 55°C for 1 minute and 72°C for 1 minute with a final extension cycle at 72°C for 2 minutes. The second amplification was performed using the sense primer Blasto 2F and the anti-sense primer Blasto 2R using PCR conditions previously described [17].
Amplified products were separated by electrophoresis using 1.5% TBE (89 mM Tris-borate, 2 mM EDTA) agarose gel and fragments visualized under UV light after staining with SYBR Safe DNA gel stain (Life Technologies, Grand Island, NY). The DNA fragment size was confirmed using a 100 base pair ladder, selected bands were excised and purified using a commercial kit (QIAquick Gel Extraction Kit, Qiagen, Valencia, CA) according to manufacturer's instructions, and prepared for sequencing. Purified products were sequenced at the Oregon State University Center for Genome Research and Biocomputing. Dilution studies, using spiked whole control organism in a canine-origin fecal sample previously tested negative, indicate that the PCR assay has a sensitivity of 1 organism/200 mg feces (wet weight).
Subtyping and phylogenetic analysis of blastocystis isolates
Where available, robust and complete sequences from the detected Blastocystis organisms were assigned to subtypes using the Blastocystis Sequence Typing website (http://www.publmst.org/blastocystis) [18], [19].
Phylogenetic analyses were conducted using MEGA 5.2.2. Sequences from the Blastocystis organisms detected in canine and feline samples were aligned with a collection of sequences for the “barcoding region” [18] of SSU rRNA retrieved from GenBank, with retrieved sequences selected from prior publications[20], [21] to provide representatives of most known subtypes of Blastocystis using the subtyping terminology originally proposed by Stensvold and colleagues [22]. Retrieved sequences were aligned using the MUSCLE algorithm [23] as implemented by MEGA 5.2.2, using default parameters. The nucleotide substitution model with the lowest Bayesian information criterion score (Tamura 3-parameter model + discrete Gamma distribution) was selected, and a Maximum-Likelihood phylogenetic tree was calculated using 1500 bootstrap replicates. Proteromonas lactertae (AY224080) was used for an out-group.
Statistical analyses
Data were analyzed using a commercial biological statistics program (GraphPad Prism 5.0 for Macintosh, GraphPad Software, La Jolla, CA). Contingency table analysis (Fischer's Exact Test) was used to assess the frequency of carriage of Blastocystis between shelter-resident and client-owned animals, and the frequency of carriage of each parasite between canine and felines. For each host species, additional contingency table analyses were carried out to assess the relative risk of showing signs of gastrointestinal disease during their shelter-resident period (in the case of shelter-resident animals) or during the preceding 1- and 4-week periods in the case of client-owned animals. For all statistical analyses, a calculated value of P<0.05 was assigned for statistical significance.
Sequence data repositories
Robust sequence data from Blastocystis spp. organisms identified in this study were deposited to GenBank.
Results and Discussion
Prevalence of Blastocystis spp. infection is higher in shelter-resident than client-owned animals
No Blastocystis spp. were detected in any fecal samples from any client-owned animals in this study, with only two very faint bands observed from two separate samples from client-owned animals. These results could not be replicated, and thus these samples were considered either negative or indicative of a very low parasite burden. (The PCR assay has a sensitivity of 1 organism/200 mg feces, see Materials). By comparison, Blastocystis organisms were readily detected in 10/103 (9.7%) shelter-resident canines, and 12/103 (11.65%) shelter-resident felines (Table 1). There was no significant difference in Blastocystis spp. carriage rates between the shelter-resident dogs and cats (P = 0.686, Fisher's Exact Test). It is interesting to compare the results of this study to previous reports of Blastocystis carriage in dogs and cats, and particularly shelter-resident animals. Duda et al [13] reported the prevalence of Blastocystis in both dogs and cats (70.8% and 67.3%, respectively) from a shelter in southeast Queensland, Australia, a semi-tropical environment, using enrichment culture and light microscopy techniques. In contrast to this, a recent publication using a PCR methodology found only two positive samples from 45 shelter-resident dogs from the same semi-tropical environment [24], and no positive samples from client-owned dogs. Wang et al [24] suggest that both methodological differences (light microscopy may be prone to false positive identifications) and differences in hygiene and management of shelter-resident dogs in the intervening years may account for the different prevalence detected. The data reported here indicate a higher prevalence of Blastocystis in shelter-resident dogs in the Pacific Northwest of the USA than in the shelter-resident dogs in southeast Queensland, this may be due to differences in management of shelter-resident dogs in the cooler, maritime environment of the Pacific Northwest, or a higher environmental risk of contracting the organism.
Table 1. Prevalence of Blastocystis spp. infection in shelter-resident dogs and cats in the US Pacific Northwest.
| Species | Blastocystis Positive | Blastocystis Negative |
| Canine | 10 | 93 |
| Feline | 12 | 93 |
Carriage of Blastocystis was not associated with increased risk of gastrointestinal signs in shelter-resident or client-owned dogs and cats
While records of gastrointestinal disease signs, typically diarrhea, were relatively frequent in the medical records of the shelter-resident cats (26/105, 24.7%) and less so in dogs (9/103, 8.7%), there was no significant relationship seen between carriage of Blastocystis and the presence of gastrointestinal signs in the shelter-resident animals. Four of 52 (7.7%) client owned cats showed owner-reported gastrointestinal signs in the week prior to collection, while 2/51 (3.9%) of client-owned dogs showed gastrointestinal signs in the week prior to collection. None of the client-owned animals showing gastrointestinal signs tested positive for Blastocystis. Shelter-resident cats were significantly more likely to have gastrointestinal disease signs overall than client-owned cats (P = 0.0099, Relative Risk 3.21, Fischer's Exact Test), while there was no significant relationship between shelter-residence and presence of gastrointestinal signs in dogs (P = 0.339, Fischer's Exact Test). Similar data regarding the frequency of diarrhea in shelter-resident dogs and cats have been reported previously [25]. From the data reported in this study, it appears unlikely that the presence of Blastocystis infection is a significant contributor to diarrhea in shelter-resident cats in the Pacific Northwest of the USA.
Shelter-resident dogs and cats carried several different Blastocystis spp. subtypes
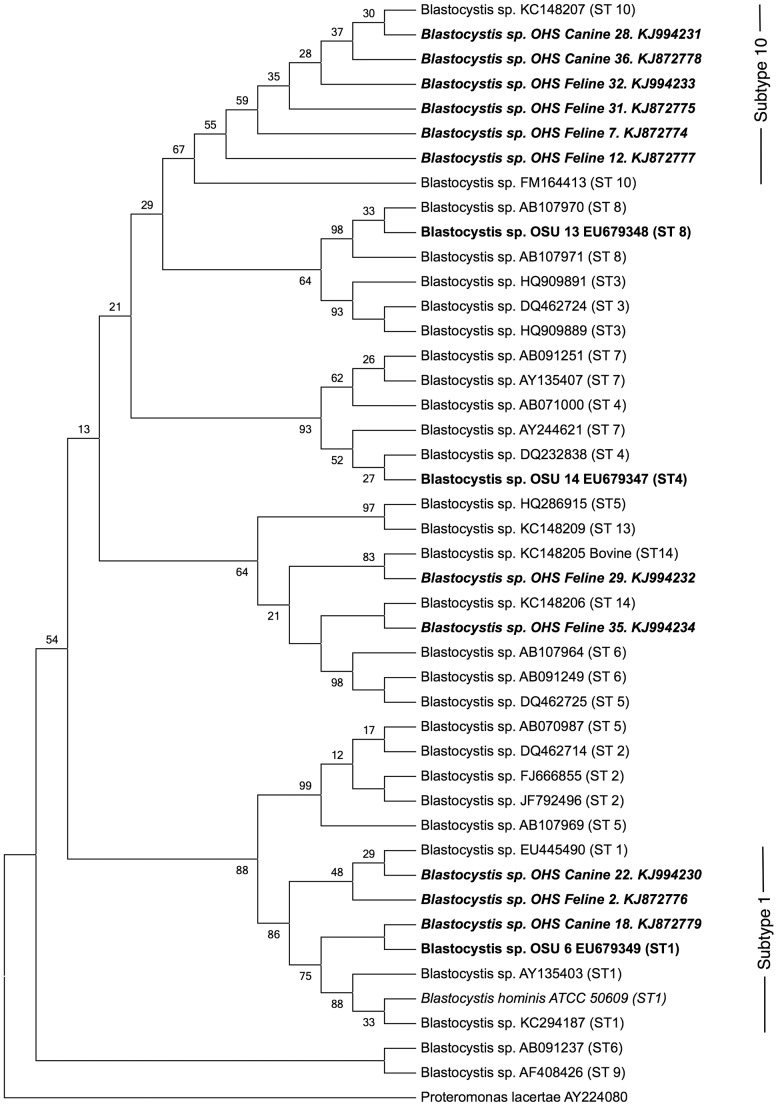
Phylogenetic analysis of sequences for SSU rDNA recovered from shelter-resident dogs and cats revealed the presence of several different Blastocystis spp. Subtypes (Figure 1, Table 2). Three of the recovered organisms grouped with representative organisms for Subtype 1, using subtype designations previously defined by Stensvold et al. [22] The majority of the remaining sequences were identified as subtype 10, a subtype that has previously been identified with highest frequency in artiodactyls, and was not identified in human beings in the same study [26]. One sequence from a shelter-resident feline (KJ994232) was not assigned a type by the sequence-typing database, while the phylogenetic analysis grouped this organism with a subtype 14 strain. A second feline-origin sequence (KJ994234) was assigned to subtype 3 by the sequence-typing database, and again phylogenetic analysis grouped this organism with subtype 14.
Figure 1. Bootstrap consensus phylogenetic tree for aligned small subunit rDNA sequences from Blastocystis spp. isolated from shelter-resident canines and felines, and previously published representative sequences, using Proteromonas lacerate as an outgroup.
The tree was derived using the Maximum Likelihood method based on a Tamura 3-parameter model, with 1500 bootstrap replicates. Numbers at branch bases indicate the percentage of bootstrap replicates in which the taxa clustered together. Taxa isolated from canine and feline samples are shown in bold, italic typeface, while organisms isolated from human patients in the same geographical region are shown in bold typeface. The positive control organism for the PCR method is shown in italic.
Table 2. Blastocystis spp. subtypes detected in shelter-resident dogs and cats in the US Pacific Northwest.
| Genbank ID | Host Species | Subtype |
| KJ872774 | Feline | 10 |
| KJ872775 | Feline | 10 |
| KJ872776 | Feline | 1 |
| KJ872777 | Feline | 10 |
| KJ872778 | Canine | 10 |
| KJ872779 | Canine | 1 |
| KJ994230 | Canine | 1 |
| KJ994231 | Canine | 10 |
| KJ994232 | Feline | Unclear, most related to 14 |
| KJ994233 | Feline | 10 |
| KJ994234 | Feline | 3 |
Subtype designations assigned using the Blastocystis Sequence Typing website (http://www.publmst.org/blastocystis) [18], [19].
Interestingly, one strain identified in this study, OHS Canine 18 (Subtype 1), segregated with an organism previously identified in a human being within the Willamette valley (OSU 6 EU679349), the location of the study reported here [16]. The human patient from whom this strain was isolated was reportedly demonstrating signs of gastrointestinal disease, while no gastrointestinal signs were noted in the dog from which this strain was isolated. Other workers have reported high rates of Blastocystis carriage in domestic animals associated with human beings symptomatic for Blastocystosis [27], however later evidence regarding Blastocystis diversity in varying geographic settings suggests that dogs are transient hosts of subtypes with potential for human pathogenicity [24], and thus that dogs do not represent a significant reservoir species for infection of humans. Given that the majority of identifiable subtypes in the study reported here were subtype 10, a subtype with little evidence of carriage in human beings, we feel that it is unlikely that shelter resident animals in the Pacific Northwest of the USA represent a potential source of zoonotic infection of animal handlers or owners.
Acknowledgments
We with to thank the staff of the Oregon Humane Society, VCA hospitals in both southeast Portland and Salem, OR, and the staff and students of the Oregon State University College of Veterinary Medicine for their assistance in obtaining samples and historical data for this study.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant epidemiological data are within the paper. Small subunit ribosomal DNA sequences are available from the GenBank database (Accession numbers KJ872774–KJ872779 and KJ994230–KJ994234).
Funding Statement
This study was supported by a grant from The Maddie's Fund (http://www.maddiesfund.org/Grant_Giving/Colleges_of_Veterinary_Medicine.html). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Esch KJ, Petersen CA (2013) Transmission and epidemiology of zoonotic protozoal diseases of companion animals. Clinical Microbiology Reviews 26: 58–85 10.1128/CMR.00067-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Traub RJ, Monis PT, Robertson ID, Irwin P, Mencke N, et al. (2004) Epidemiological and molecular evidence supports the zoonotic transmission of Giardia among humans and dogs living in the same community. Parasitology 128: 253–262 10.1017/S0031182003004505 [DOI] [PubMed] [Google Scholar]
- 3. Boorom K, Smith H, Nimri L, Viscogliosi E, Spanakos G, et al. (2008) Oh my aching gut: irritable bowel syndrome, Blastocystis, and asymptomatic infection. Parasites & Vectors 1: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stensvold CR, Arendrup MC, Nielsen HV, Bada A, Thorsen S (2008) Symptomatic infection with Blastocystis sp. subtype 8 successfully treated with trimethoprim–sulfamethoxazole. Ann Trop Med Parasitol 102: 271–274 10.1179/136485908X278847 [DOI] [PubMed] [Google Scholar]
- 5. Markell EK (1995) Is there any reason to continue treating Blastocystis infections? Clin Infect Dis 21: 104–105. [DOI] [PubMed] [Google Scholar]
- 6. Stenzel DJ, Boreham PF (1996) Blastocystis hominis revisited. Clinical Microbiology Reviews 9: 563–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Boreham RE, Benson S, Stenzel DJ, Boreham PF (1996) Blastocystis hominis infection. The Lancet 348: 272–273. [DOI] [PubMed] [Google Scholar]
- 8. Puthia MK, Lu J, Tan KSW (2008) Blastocystis ratti contains cysteine proteases that mediate interleukin-8 response from human intestinal epithelial cells in an NF-kappaB-dependent manner. Eukaryotic Cell 7: 435–443 10.1128/EC.00371-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Teo JD, MacAry PA, Tan KSW (2014) Pleiotropic effects of Blastocystis spp. Subtypes 4 and 7 on ligand-specific toll-like receptor signaling and NF-κB activation in a human monocyte cell line. PLoS ONE 9: e89036 10.1371/journal.pone.0089036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Scaramozzino P, Di Cave D, Berrilli F, D′Orazi C, Spaziani A, et al. (2009) A study of the prevalence and genotypes of Giardia duodenalis infecting kennelled dogs. Vet J 182: 231–234 10.1016/j.tvjl.2008.07.003 [DOI] [PubMed] [Google Scholar]
- 11. Bissett SA, Stone ML, Malik R, Norris JM, O′Brien C, et al. (2009) Observed occurrence of Tritrichomonas foetus and other enteric parasites in Australian cattery and shelter cats. J Feline Med Surg 11: 803–807 10.1016/j.jfms.2009.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Robben SR, le Nobel WE, Döpfer D, Hendrikx WM, Boersema JH, et al. (2004) [Infections with helminths and/or protozoa in cats in animal shelters in the Netherlands]. Tijdschrift voor diergeneeskunde 129: 2–6. [PubMed] [Google Scholar]
- 13. Duda A, Stenzel DJ, Boreham PF (1998) Detection of Blastocystis sp. in domestic dogs and cats. Vet Parasitol 76: 9–17. [DOI] [PubMed] [Google Scholar]
- 14. Parkar U, Traub RJ, Kumar S, Mungthin M, Vitali S, et al. (2007) Direct characterization of Blastocystis from faeces by PCR and evidence of zoonotic potential. Parasitology 134: 359 10.1017/S0031182006001582 [DOI] [PubMed] [Google Scholar]
- 15. Little SE, Johnson EM, Lewis D, Jaklitsch RP, Payton ME, et al. (2009) Prevalence of intestinal parasites in pet dogs in the United States. Vet Parasitol 166: 144–152 Available: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=19716659. [DOI] [PubMed] [Google Scholar]
- 16. Whipps CM, Boorom K, Bermudez LE, Kent ML (2010) Molecular characterization of Blastocystis species in Oregon identifies multiple subtypes. Parasitol Res 106: 827–832 10.1007/s00436-010-1739-8 [DOI] [PubMed] [Google Scholar]
- 17. Souppart L, Sanciu G, Cian A, Wawrzyniak I, Delbac F, et al. (2009) Molecular epidemiology of human Blastocystis isolates in France. Parasitol Res 105: 413–421 10.1007/s00436-009-1398-9 [DOI] [PubMed] [Google Scholar]
- 18. Scicluna SM, Tawari B, Clark CG (2006) DNA barcoding of blastocystis. Protist 157: 77–85 10.1016/j.protis.2005.12.001 [DOI] [PubMed] [Google Scholar]
- 19. Jolley KA, Maiden MC (2010) BIGSdb: Scalable analysis of bacterial genome variation at the population level. BMC Bioinformatics 11: 595 10.1186/1471-2105-11-595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stensvold CR, Alfellani MA, Taner-Mulla D, Jacob AS, Imeede CA, et al. (2013) Genetic diversity of blastocystis in livestock and zoo animals. Protist 164: 497–509 10.1016/j.protis.2013.05.003 [DOI] [PubMed] [Google Scholar]
- 21. Noel C, Dufernez F, Gerbod D, Edgcomb VP, Delgado-Viscogliosi P, et al. (2005) Molecular Phylogenies of Blastocystis Isolates from Different Hosts: Implications for Genetic Diversity, Identification of Species, and Zoonosis. J Clin Microbiol 43: 348–355 10.1128/JCM.43.1.348-355.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Stensvold CR, Traub RJ, Suresh GK, Tan KSW, Thompson RCA, et al. (2007) Terminology for Blastocystis subtypes – a consensus. Trends Parasitol 23: 93–96 10.1016/j.pt.2007.01.004 [DOI] [PubMed] [Google Scholar]
- 23. Edgar RC (2004) MUSCLE: multiple sequence alignment with high accuracy and high throughput. Nucleic Acids Res 32: 1792–1797 10.1093/nar/gkh340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wang W, Traub RJ, Cuttell L, Bielefeldt-Ohmann H, Inpankaew T, et al. (2013) Diversity of Blastocystis subtypes in dogs in different geographical settings. Parasites & Vectors 6: 1–1 10.1186/1756-3305-6-215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bybee SN, Scorza AV, Lappin MR (2011) Effect of the Probiotic Enterococcus faecium SF68 on Presence of Diarrhea in Cats and Dogs Housed in an Animal Shelter. J Vet Intern Med 25: 856–860 10.1111/j.1939-1676.2011.0738.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stensvold CR, Alfellani MA, Nørskov-Lauritsen S, Prip K, Victory EL, et al. (2009) Subtype distribution of Blastocystis isolates from synanthropic and zoo animals and identification of a new subtype. Int J Parasitol 39: 473–479 10.1016/j.ijpara.2008.07.006 [DOI] [PubMed] [Google Scholar]
- 27. Nagel R, Cuttell L, Stensvold CR, Mills PC, Bielefeldt-Ohmann H, et al. (2012) Blastocystis subtypes in symptomatic and asymptomatic family members and pets and response to therapy. Intern Med J 42: 1187–1195 Available: http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=22032439&retmode=ref&cmd=prlinks. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant epidemiological data are within the paper. Small subunit ribosomal DNA sequences are available from the GenBank database (Accession numbers KJ872774–KJ872779 and KJ994230–KJ994234).