Abstract
Background
There is a current need to produce a simple, yet effective method for screening and targeting possible deficiencies related to increased anterior cruciate ligament (ACL) injury risk.
Hypothesis
Frontal plane knee angle (FPKA) during a drop vertical jump will decrease upon implementing augmented feedback into a standardized sport training program.
Study Design
Controlled laboratory study.
Methods
Thirty-seven female participants (mean ± SD: age, 14.7 ±1.5 years; height, 160.9 ± 6.8 cm; weight, 54.5 ± 7.2 kg) were trained over 8 weeks. During each session, each participant received standardized training consisting of strength training, plyometrics, and conditioning. They were also videotaped running on a treadmill at a standardized speed and performing a repeated tuck jump for 10 seconds. Study participants were randomized into 2 groups and received augmented feedback on either their jumping (AF) or sprinting (CTRL) form. Average (mean of 3 trials) and most extreme (trial with greatest knee abduction) FPKA were calculated from 2-dimensional video captured during performance of the drop vertical jump.
Results
After testing, a main effect of time was noted, with the AF group reducing their FPKA average by 37.9% over the 3 trials while the CTRL group demonstrated a 26.7% reduction average across the 3 trials (P < .05). Conversely, in the most extreme drop vertical jump trial, a significant time-by-group interaction was noted (P < .05). The AF group reduced their most extreme FPKA by 6.9° (pretest, 18.4° ± 12.3°; posttest, 11.4° ± 10.1°) on their right leg and 6.5° (pretest, 16.3° ± 14.5°; posttest, 9.8° ± 10.7°) on their left leg, which represented a 37.7% and 40.1 % reduction in FPKA, respectively. In the CTRL group, no similar changes were noted in the right (pretest, 16.9° ± 14.3°; posttest, 14.0° ± 12.3°) or left leg (pretest, 9.8° ± 11.1°; posttest, 7.2° ± 9.2°) after training.
Conclusion
Providing athletes with augmented feedback on deficits identified by the tuck jump assessment has a positive effect on their biomechanics during a different drop vertical jump task that is related to increased ACL injury risk. The ability of the augmented feedback to support the transfer of skills and injury risk factor reductions across different tasks provides exciting new evidence related to how neuromuscular training may ultimately cross over into retained biomechanics that reduce ACL injuries during sport.
Clinical Relevance
The tuck jump assessment’s ease of use makes it a timely and economically favorable method to support ACL prevention strategies in young girls.
Keywords: biofeedback, high-risk landing mechanics, knee injury, ACL injury prevention
Altered neuromuscular strategies employed during the execution of sports movements that manifest as altered frontal plane lower limb joint mechanics (increased motions and loads) increase the risk of anterior cruciate ligament (ACL) injury in young female athletes.6,28 Targeting female athletes who demonstrate high-risk lower limb joint mechanics likely improves the efficacy and efficiency of neuromuscular training.1
Three-dimensional (3D) analysis of a drop vertical jump (DVJ) landing has been used to identify predictors for ACL injury and to develop simplified surrogate prediction models.6,16,19,20 In addition, laboratory-based measures can be used to identify high-risk athletes and provide targeted biofeedback modalities, which can be effective in targeting neuromuscular control deficits. However, 3D assessments and innovative biofeedback training require dedicated laboratories that may limit widespread dissemination of those modalities.
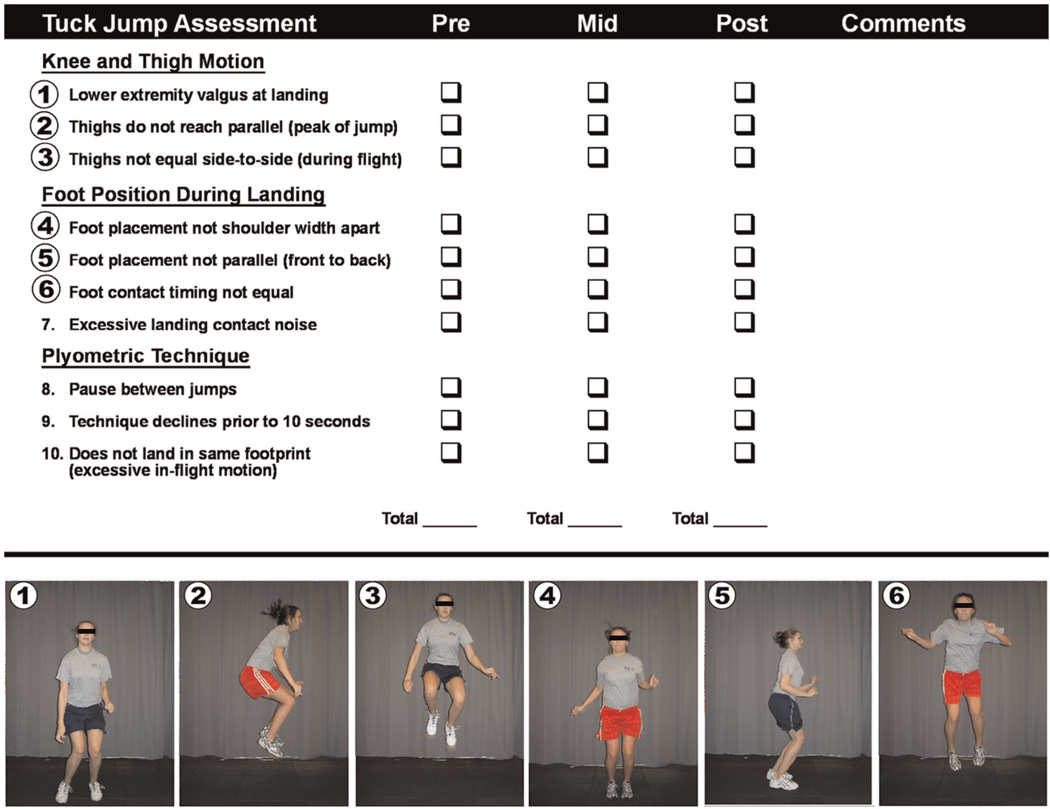
Biomechanical deficiencies can be identified in a simplified screening of a tuck jump maneuver (Figure 1), which can support the assessment of movement deficits that relate to predictors for ACL injuries in young athletes.17 The deficiencies that can be observed include ligament dominance, quadriceps dominance, leg dominance/residual injury deficits, trunk dominance, and technique deficits. Real-time feedback during a tuck jump may prevent knee injury and has implications for the improvement of skill development.14,15,22 Pairing feedback-driven plyometrics with accessory training exercises in a periodized strength and conditioning program can be utilized to develop areas of weakness relative to the previously identified deficits. Specifically, Herman and colleagues4 evaluated the relevant effects of a strength training protocol with feedback on the performance of a horizontal DVJ maneuver. Participants demonstrated decreased peak vertical ground-reaction force, decreased knee valgus moment and hip abduction moment, and increased knee flexion angle, hip flexion angle, and hip abduction angle after the feedback protocol.4
Figure 1.
The tuck jump assessment tool was utilized to score deficits during a jumping and landing movement sequence. To perform the tuck jump exercise, the athlete was instructed to start in an athletic position with her feet shoulder width apart (on lines marked 35 cm apart). To initiate the jump, the athlete was instructed to build momentum by slightly crouching downward and swinging her arms backward into extension. Take off was achieved by throwing her arms forward while simultaneously jumping vertically and pulling her knees upward. The athlete was instructed to pull her thighs parallel to the ground at the peak of the jump. Upon landing, the athlete was encouraged to immediately begin the next tuck jump to decrease downtime between each jump. Additional instruction given to the athlete included directions to land softly, using a toe to midfoot rocker landing, and to land in the same footprint with each jump. The assessment was conducted for 10 sections, however, if the athlete demonstrated a sharp decline in technique during the allotted time frame, she was told to stop the exercise. Figure reproduced from Myer GD, Ford KR, Hewett TE. Tuck jump assessment for reducing anterior cruciate ligament injury risk. Athl Ther Today. 2008;13(5):39–44.
A recent investigation demonstrated that augmented feedback guided by ligament dominance, quadriceps dominance, leg dominance/residual injury, trunk dominance, and technique deficits will directly transfer into task-specific performance of the tuck jump.31 Specifically, deficit-driven feedback guided by the tuck jump assessment reduced criteria-based deficits to a greater extent within the same maneuver compared with participants who only performed the task without guided feedback. In addition, the recent investigation indicated that specific components of the tuck jump assessment appeared to be more modifiable than others. These deficits, including knee valgus at landing, feet shoulder width apart, feet parallel front to back, excessive landing noise, and pause between jumps, appeared to be most amendable for task-specific adaptations after the augmented feedback training program.31 While these prior data indicate that the use of augmented feedback during the tuck jump exercise complements a training protocol to maximize desired training adaptations in a task-specific manner, it was not known if these augmented feedback techniques would transfer to different tasks that may be more directly associated with ACL injury risk.6
Both comprehensive and plyometric-focused training programs that employ feedback and instruction have been moderately effective in the reduction of risk factors associated with ACL injury.13,22 In addition, measurement of these reductions in knee abduction moment and knee abduction angle required the use of 3D motion capture systems.21,22 Therefore, the purpose of this study was to use clinician-friendly screening tools to determine the effects of additive augmented feedback into existing protocols on the relative increase in the effectiveness of injury prevention training protocols. We hypothesized that frontal plane knee angle (FPKA) during a DVJ would decrease upon implementing augmented feedback into a standardized sport training program.
MATERIALS AND METHODS
Participants
On the basis of the randomized controlled trial study design, we planned on continuous response variables from independent control (CTRL) and experimental participants (AF) with 1 control per experimental participant. Frontal plane kinematic data from ACL-injured and ACL-uninjured female athletes were used to determine the clinically significant minimal expected changes for the current study groups.6 Based on these data, a power analysis revealed that to achieve 80% statistical power in the current study, with an exploratory a level of .05, a minimum of 17 participants per group (AF and CTRL) was required. We recruited a high school, with the soccer teams having a minimum of 34 athletes to be randomized into 2 groups.
For randomization, all participants’ identifications (IDs) were entered into a database, and a random number generator was applied that associated a random number to each participant ID. The participant IDs were sorted by their associated random numbers, and ultimately, the 38 recruited female high school soccer players were randomly assigned to 1 of 2 intervention groups based on the type of feedback they would receive (AF vs CTRL). The mean ± standard deviation age of the participants was 14.7 ± 1.7 years for the CTRL group and 14.7 ± 1.4 years for the AF group. Their height and mass were 160.8 ± 5.1 cm and 54.6 ± 7.8 kg for the CTRL group and 160.9 ± 8.1 cm and 54.1 ± 6.8 kg for the AF group. This study was approved by the Cincinnati Children’s Hospital Medical Center review board. Parents or guardians signed informed consent forms before participation in the study. Athletes with a history of ACL injury (n = 1) were allowed to participate with their team in the training program but were excluded from the final data analysis.
Testing
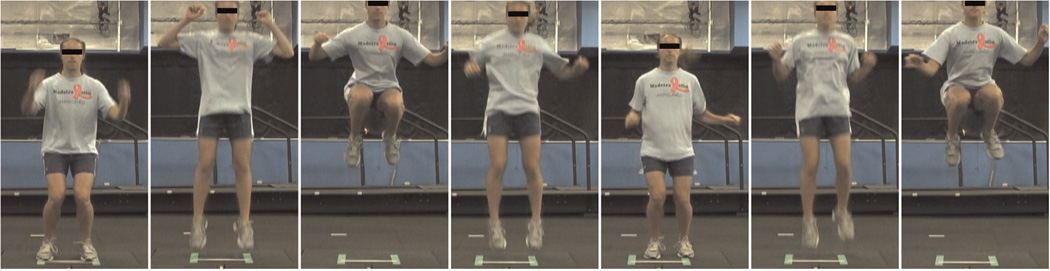
The study design was a double-blind, randomized controlled trial to determine the effects of augmented feedback during tuck jump performance (Figure 2) on measures related to ACL injury risk assessed during the DVJ (Figure 3).6,28 A baseline DVJ was recorded for each participant in both the sagittal and frontal views before the onset of training. Both groups received the same exact standardized off-season training as part of this study and were videotaped for their performance of both the treadmill running and tuck jump to help maintain treatment blinding of the study participants. The 2 groups (AF vs CTRL) were then given augmented feedback according to group affiliation during each training session as the tested intervention. At posttraining testing, the DVJ was again recorded in each view for analysis. All video analyses (digitizing and postprocessing) were performed by a rater blinded to each participant’s training group affiliation (AF vs CTRL) and to training status (pretesting vs posttesting).
Figure 2.
Performance of the tuck jump maneuver.
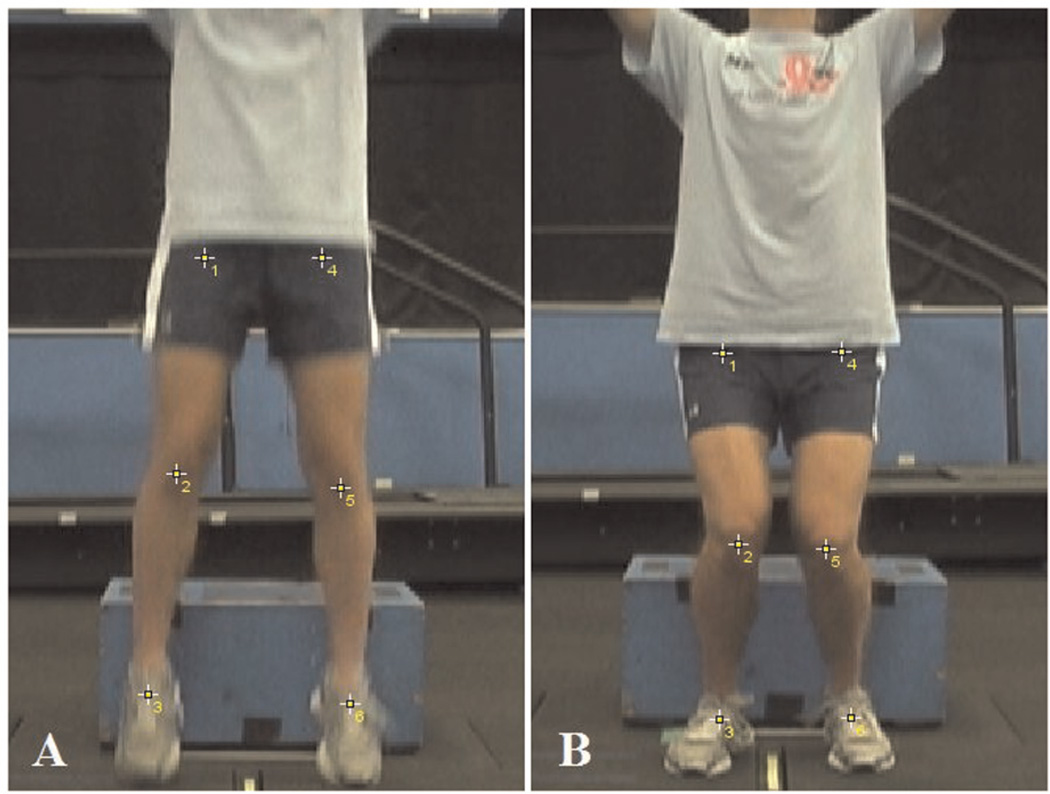
Figure 3.
Digital reconstruction of knee angle at initial contact (A) and maximum medial knee displacement (B) in the frontal plane.
2D Landing Biomechanics
Two-dimensional frontal plane knee kinematic data were collected using standard video cameras during each of the 3 DVJ trials. The cameras were positioned 3 m from the approximated location of landing at a height of 54.6 cm (21.5 inches) to capture lower extremity motion during the DVJ in the frontal view. The frontal plane camera was positioned in alignment with the participant’s midline, as determined by standardized foot position on the box before beginning the task. Landing sequence images were captured using VirtualDub (http://www.virtualdub.org/), and kinematic data were compiled using ImageJ (National Institutes of Health, Bethesda, Maryland). Coordinate data were captured from the video frame just before initial contact and again at maximum medial knee displacement in the frontal view and maximum knee flexion in the sagittal view (Figure 3). Maximum FPKA was calculated from hip, knee, and ankle joint centers at maximum medial knee displacement. In the frontal plane, the hip joint center was estimated relative to a skin-mounted marker placed on the greater trochanter, the knee joint center was estimated as the midpoint between 2 markers placed on the medial and lateral epicondyles, and the ankle joint center was estimated as the midpoint between 2 markers placed on the medial and lateral malleoli. These coordinate data were then exported to MATLAB (MathWorks, Natick, Massachusetts) for processing. The FPKA was reported with positive convention for both right and left limbs, and knee adduction alignment (knee varus) was calculated as 0° of FPKA.
AF Group Training
In each training session, all participants were recorded performing the tuck jump and treadmill running warm-up each for 10 seconds. Participants were selected at random during each training session to receive feedback on their video for the group in which they were assigned (AF group: video of their tuck jump performance; CTRL group: video of their treadmill running performance).
For the AF study group, video feedback was presented at half-speed on a Dell Inspiron 1720 (Round Rock, Texas) using QuickTime (Apple, Cupertino, California). Videos for the tuck jump were analyzed using a 10-point scale for the tuck jump (Figure 1; see the Video Supplement, available in the online version of this article at http://ajs.sagepub.com/supplemental/).9 The participants were observed for individual criteria of the following categories: ligament dominance, quadriceps dominance, leg dominance/residual injury deficits, and trunk dominance. Ligament dominance was deemed evident when the participant was unable to control frontal plane motion during cutting or landing and could be observed in lower extremity valgus at the knee and foot placement not being shoulder width apart upon landing. Quadriceps dominance was operationally defined as an imbalance between knee extensor and flexor strength, recruitment, and coordination17 and may be evidenced by excessive landing noise during the tuck jump. Leg dominance was defined as an asymmetry in strength or coordination between both extremities9 and was most noticeable when the thighs did not move in unison during flight, foot placement was not parallel (front to back) upon landing, and the feet did not land at the same time. Trunk or core dysfunction was observed when there was an imbalance between the force demands of the trunk or core and the coordination needed to resist it.9 Trunk dysfunction was apparent when pauses occurred between jumps, thighs failed to reach a height parallel to the ground, and participants did not land in the same footprint. A trunk dysfunction shows the participant’s inability to control the extremities because of the core’s inadequate capability to overcome the force of the extremities. The participant’s technique was considered a deficit or deficient if it was not properly maintained for 10 seconds. This demonstrates the athlete’s strength and ability to re-create the same pattern multiple times.
The participants were informed of the 2 most apparent flaws they demonstrated and how to correct the flaws. After receiving feedback, each participant performed a repeated tuck jump exercise for 10 seconds. The tuck jump was recorded from the frontal view using a portable video camera mounted on a tripod. The camera was set to record, and then the participant was instructed to begin. The camera and the stopwatch were controlled by the same person. A previous report indicates that the criteria of the tuck jump assessment are reliable, with average percentage exact agreement (PEA) between testers across all scoring criteria being 93% (range, 80%–100%). In addition, the κ measure of agreement was .88, which is very good/excellent for intertester ratings. The intratester PEA ranged from 87.2% to 100%, with κ = .86 to 1.0 for all criteria of the tuck jump assessment.5
CTRL Group Training
A control treatment (treadmill running feedback) was employed to maintain blinding of the intervention to study participants. Before using the treadmill, all participants (CTRL and AF) were instructed how to properly get on and off the treadmill to avoid possible injury. The instructions were as follows: grasp the bar firmly; then with your left foot, push off several times to get accustomed to the speed of the treadmill; and finally, once comfortable, enter onto the treadmill, and release the bar when ready. Participants were recorded for 10 seconds while running on the treadmill at 8 mph. The stopwatch was controlled by a spotter located on the left side of the treadmill.
During the 1.5-hour training session, the CTRL group participants were randomly chosen from the standardized training to review their video (treadmill running) from their previous session, excluding the first session. Video feedback was presented at half-speed on a Dell Inspiron 1720 using QuickTime. Videos were analyzed using the 8-point scale for treadmill running that has been previously published. The 8 points assessed were maintaining 90° of elbow flexion through the back arm swing, maintaining 90° of elbow flexion through the forward arm swing, wrist swinging past the hip on the back arm swing, wrist not crossing the midline of the torso, maintaining upright position of the torso, shoulders square to the direction of travel, thighs parallel to the ground, and relaxed upper torso. 12The participants were informed of the 2 most apparent flaws they demonstrated and how to correct the flaws.
Standardized Training
The AF and CTRL groups participated in identical standardized training, which was designed to accommodate the off-season needs of a high school soccer player, 3 times per week for 7 weeks. The training sessions lasted 1.5 hours and contained 2 of the following modes of training, which rotated in a cyclical fashion: resistance training, plyometric training, technique training, and metabolic energy systems development. The AF and CTRL groups were recorded by video for both running and tuck jump performance. The only difference between any component of testing or training between the groups was the individualized feedback that was related to tuck jump performance (AF) or running performance (CTRL). All athletes were blinded to the feedback given to their peers in the individual feedback component (AF or CTRL video feedback) and received equivalent feedback and instruction during resistance plyometric and technique-oriented training portions of the team training.
Statistical Analysis
Outcome measurements of FPKA were digitized and analyzed by a rater blinded to both training group (AF vs CTRL) and testing session (pretraining vs posttraining). Statistical analyses were conducted in SPSS Version 17.0 (Chicago, Illinois). A 1-way analysis of variance (ANOVA) was used to evaluate potential group differences in height, mass, and age. A 2 × 2 × 2 repeated-measures ANOVA was used to examine the within-participant effects of time (pretraining vs posttraining) and side (right vs left) and the between-participant factor of condition (AF vs CTRL) on measures of average FPKA and most extreme FPKA, defined as the trial in which the largest valgus motion occurred. Statistical significance was established a priori at P < .05 to test the directional hypothesis that AF would be more effective than CTRL feedback in improving deficits measured during the DVJ.
RESULTS
To test the hypothesis that the augmented feedback would reduce frontal plane measures related to ACL injury, we employed a double-blind randomized trial with a sham feedback control. The current study included 37 female high school soccer players who were randomly assigned to 1 of 2 intervention groups based on the type of feedback they received (AF vs CTRL). The study participants (AF vs CTRL) were not different in age, height, or mass at either pretest or posttest assessment (P > .05).
There was not a significant interaction of time by group for FPKA averaged over 3 DVJ trials (P > .05). However, at posttest follow-up, a main effect of time was noted with the AF group, reducing their FPKA average by 37.9% over the 3 trials, while the CTRL group demonstrated a 26.7% reduction average across the 3 trials (P < .05). Conversely, in the most extreme DVJ trial, a significant time-by-group interaction was noted (P < .05). The AF group reduced their most extreme FPKA by 6.9° (pretest, 18.4° ± 12.3°; posttest, 11.4° ± 10.1°) on their right leg and 6.5° (pretest, 16.3° ± 14.5°; posttest, 9.8° ± 10.7°) on their left leg, representing a 37.7% and 40.1% reduction in FPKA, respectively. In the CTRL group, no similar changes were noted after training in the right (pretest, 16.9° ± 14.3°; posttest, 14.0° ± 12.3°) or left leg (pretest, 9.8° ± 11.1°; posttest, 7.2° ± 9.2°). There were not any interactions or main effect of side identified in the CTRL and AF training groups (P < .05).
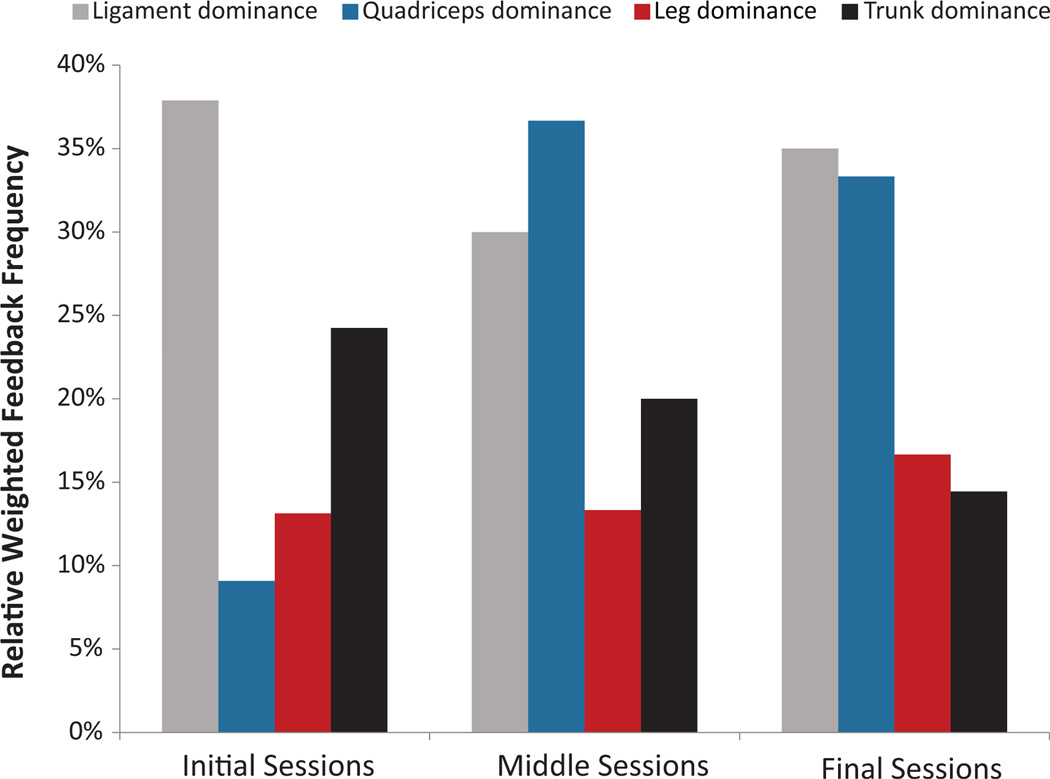
The most common deficit that was deemed the most flagrant error and that subsequently provided the primary feedback at the initial training session was the measure of ligament dominance and included feedback in valgus knee positioning and keeping the feet shoulder width apart at landing (Figure 4). As the training progressed and consequently the skill in performing the tuck jumps improved, athletes were more commonly given feedback on the training deficits related to the sagittal plane (eg, reducing landing contact noise). In the final training session, deficits deemed most flagrant were more evenly distributed among the group categorizations of ligament, quadriceps, leg, and trunk dominance. While the relative overall focus on ligament dominance feedback was reduced, the ligament dominance measures of valgus knee positioning and keeping the feet shoulder width apart at landing were the most common primary feedback provided at end-stage training sessions (Figure 4).
Figure 4.
Relative weighted feedback frequency (primary and secondary) given to the jumping (AF) group relative to their prior session performance of the tuck jump. Feedback data were averaged from the first 2, middle 2, and final 2 training sessions and weighted to the number of deficits included in each of the dominance categorizations.
DISCUSSION
Previous reports indicate that the use of augmented feedback during tuck jump performance influences training adaptations in a task-specific manner31; however, it was not known if these augmented feedback techniques would transfer to the DVJ task, which has been directly associated with ACL injury risk.6 The purpose of this study was to determine if visual and verbal feedback would improve neuromuscular control during the DVJ and potentially reduce associated ACL injury factors in young girls. The tested hypothesis was supported by the findings of significantly greater improvements during the DVJ in the AF group compared with the CTRL group. Proper techniques for basic movements such as jumping are frequently absent from many training protocols. Both groups received identical training, with the exception of the type of augmented feedback (tuck jump or running). Our findings highlight the importance of the implementation of feedback within a standardized training protocol.
It has been established that 3D assessments can improve risk factors associated with ACL injury risk; however, the costly resource- and time-intensive natures of these assessments limit their widespread implementation.14 The importance of being able to quickly and accurately identify athletes at risk for ACL injury indicates that the implementation of innovative feedback modalities can benefit clinicians, coaches, and other practitioners. Previous studies support the use of augmented feedback as a component of a training program.26,27 Athletes who received augmented video feedback of a DVJ significantly reduced their vertical ground-reaction force compared with controls.30 The use of the 2D landing biomechanics screening tool is a clinically applicable means by which assessments of frontal plane kinematic factors associated with ACL injury risk, including knee valgus excursion and FPKA, can be made effectively and efficiently. Responsiveness to the augmented feedback generated from the tuck jump assessment indicates that this type of feedback can be an effective complement to a traditional strength and conditioning protocol.
Knee valgus motion has often been regarded as an important contributing factor to ACL injury, as it has been shown to contribute to a high knee abduction moment.23 Modification of the landing technique through augmented feedback can reduce this risk factor, decreasing an athlete’s risk for this type of injury. Enhancements in neuromuscular control may be responsible for this improvement. For example, neuromuscular training that included tuck jump training significantly reduced knee abduction moments and angles during landing in female athletes.7,13,21,22 A benefit of using the tuck jump assessment to provide feedback may be the mechanism that drove the greater improvement in FPKA reported in the current study and that has also been previously achieved without AF techniques. In addition, because the tuck jump is an advanced plyometric exercise, feedback must be delivered in an efficient and understandable manner to maximize neuromuscular control. Prior studies have provided the feedback in a real-time fashion, whereas the current investigation employed AF techniques assisted with video.7–9,14,15,22 The benefits of providing feedback with video before training with an exercise may have also contributed to the increased improvements in FPKA compared with those previously reported.
Augmented Feedback Techniques Used to Reduce Injury Risk Biomechanics
Identification of global deficits during performance of the tuck jump maneuver is most easily accomplished via focus on specific faults throughout the movement. However, when classifying a specific deficit as most flagrant for the current study, the movement must present throughout a significant portion of the 10-second trial or must have significantly altered the surrounding kinematics of another assessment point. After the identification of the major concerns, feedback and subsequent manipulation were possible. The study of modifiable risk factors has focused on the working hypothesis that ACL injury risks are related to measurable deficits in neuromuscular control in female athletes.2,3,6 Neuromuscular control deficits are defined as muscle strength, power, or activation patterns that lead to increased knee joint and ACL loads.17 Female athletes demonstrate neuromuscular control deficits that increase lower extremity joint loads during sports activities.7 During landing, pivoting, or deceleration, the motion of the female athlete’s trunk is often excessive and directed, to a greater extent, by that body segment’s inertia rather than by the athlete’s core muscle function.8 This decrease in core control and the inability to dissipate force result in excessive trunk motion, especially in the frontal plane, as well as high ground-reaction forces and knee joint abduction torques (knee load). The 4 potential neuromuscular control deficits (ligament dominance, quadriceps dominance, leg dominance, and trunk dominance) are postulated to be important contributors to knee and ACL injury incidence in female athletes.6,11,29,32
Ligament Dominance
One neuromuscular deficit, which is operationally termed “ligament dominance,” can be defined as an imbalance between the neuromuscular and ligamentous control of dynamic knee joint stability.17 This control imbalance is demonstrated by an inability to control lower extremity frontal plane motion during landing and cutting. In the current study, the most common deficit that was deemed the flagrant error and on which the primary feedback was subsequently provided at the initial training sessions was the construct of ligament dominance. This included feedback in valgus knee positioning and keeping the feet shoulder width apart at landing (Figure 4). The first step to address ligament dominance was to make the athlete aware of the proper form and technique as well as undesirable and potentially dangerous positions.17 A valgus collapse was recognized by one or both knees deviating toward the participant’s midline. The overall reduction of ligament dominance measures was likely related to the changed outcomes of reduced FPKA in the AF training group. However, the continued prevalence of this deficit as a common error may indicate that continued feedback-driven training beyond the 7 weeks employed in the current investigation may be needed to alleviate ligament dominance measures in female athletes.
Quadriceps Dominance
A second modifiable neuromuscular control deficit often observed in female athletes, which is termed “quadriceps dominance,” can be defined as an imbalance between knee extensor and flexor strength, recruitment, and coordination.17 As the training progressed in the current study, the focus of the feedback during training shifted from deficits in the frontal plane to deficits that were related to the sagittal plane, and thus, feedback was given with the intent of reducing landing contact noise (Figure 4). To decrease the tendency toward quadriceps dominance, exercises that emphasize co-contraction of the knee flexor/extensor muscles were employed.1 We hypothesize that the repetitive achievement of proper positioning facilitated increased muscle co-activation and possibly led to reduced ACL loads.17 Excessive landing noise was evident by the contact of the entire foot and heel on the ground between jumps. Landing with decreased hip and knee flexion exacerbated this deficit. To decrease landing noise, athletes in the current investigation were given feedback to land on the balls of their feet and make the least amount of noise possible.
Leg Dominance
A third neuromuscular control deficit often observed in female athletes was “leg dominance,” which can be defined as an imbalance between the 2 lower extremities in strength, coordination, and control.17 Thighs not equal side to side was corrected by either informing the participants to drive their knees straight to their shoulders, or they were told to touch their palms (with elbows flexed to 90° and held straight ahead) to their knees at the peak of flight. Feet not being parallel was identified as deficient when a participant’s foot contact position was not aligned evenly with each other. Often, athletes will attempt to shift their forces to one leg or the other based on leg dominance or as a residual movement flaw from a previous injury. Foot contact timing was considered deficient in the current investigation when the participant’s initial ground contact did not occur simultaneously. Equal leg-to-leg strength, balance, and foot placement were stressed throughout training. For example, to perform tuck jumps (Figure 4), the leg-dominant athletes may have repeatedly placed their weaker limb under greater stress to maintain symmetry throughout the performance of a double-legged jump. As the current study population was free from prior lower extremity injury, leg dominance measures were the least common deficit on which feedback was given. It is more common to find this deficit in athletes who have sustained a lower extremity injury, especially ACL injury and reconstruction.18,23,24 During the tuck jump, athletes having undergone ACL reconstruction often unload their involved side, as is visually evidenced by uneven foot placement and asymmetrical limb alignment during the flight of jumping (Figure 5).23 Training the athlete to employ safe cutting and landing techniques in sports-related situations may help instill technique adaptations that more readily transfer onto the field of play. The “ligament-dominant” and “leg-dominant” athlete may become muscle dominant and symmetrical if the desired training adaptations are achieved, thus ultimately reducing their risk factors of future primary or secondary ACL injury.6,17,22,29
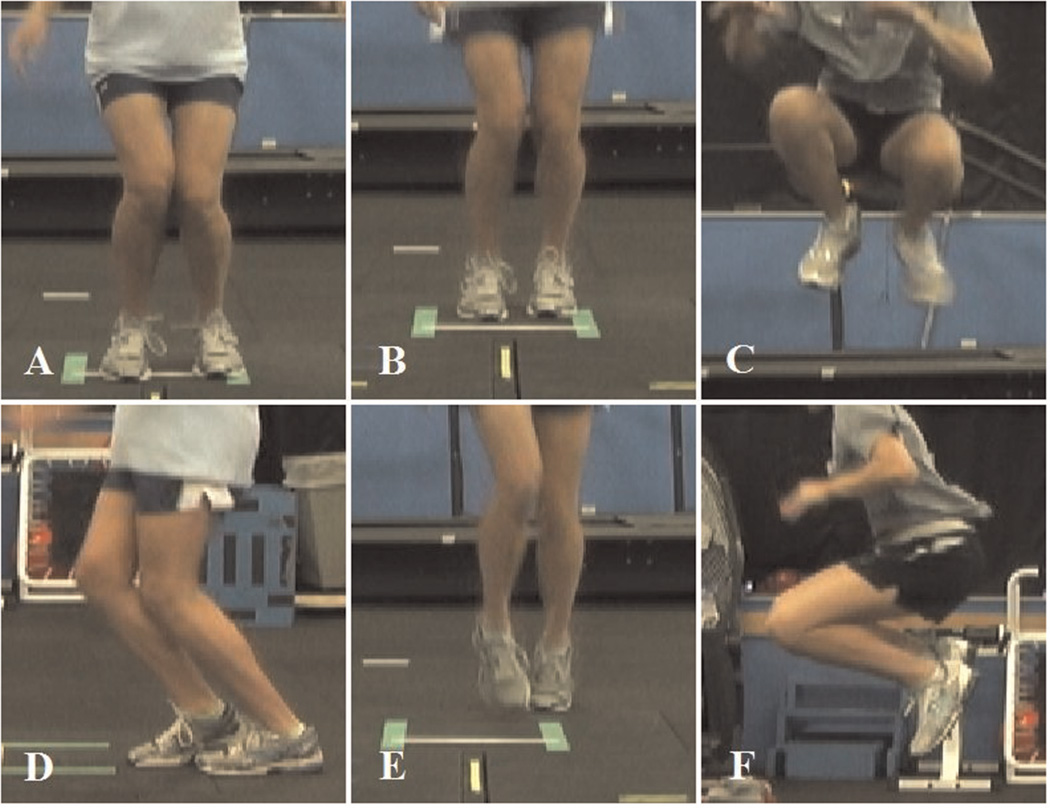
Figure 5.
Examples of tuck jump deficits: knee valgus (A), feet not shoulder width apart (B), thighs not in unison (C), feet not parallel (D), feet timing not equal (E), and thighs not reaching parallel (F).
Trunk Dominance
The fourth and final neuromuscular control deficit often observed in female athletes, trunk dominance or “core” dysfunction, can be defined as an imbalance between the inertial demands of the trunk and control and coordination to resist it. If a pause between jumps, caused by weakness or fatigue, was recognized during the 10 seconds, it was considered as warranting a deficiency. This measure was not considered an issue if the athletes became off-balance and realigned themselves quickly to complete the tuck jump. Instead, it was only considered a deficit when no other glaring deficits were present to correct. If pausing between jumps was observed, it was corrected by informing the athletes to continually drive their knees to their chest during the entire 10 seconds. When looking at “thighs reaching parallel,” participants were classified as deficient if they presented with short quick jumps where, at no point during the 10 seconds, their thighs reached parallel. If a participant was characterized with the specific deficit for “thighs not being equal side to side,” the participant did not maintain symmetrical positioning of the thighs during flight. If the knees reaching parallel were an issue, the participants were informed to drive their knees to their chest as high as they could throughout the entire 10 seconds. If the participant showed small form breakdowns only within the last 3 to 4 jumps, then this was addressed.
The current study also showed a relatively consistent focus on trunk dominance measures as the most flagrant deficits throughout the training. The continued feedback to improve trunk and hip control likely supported the adaptations of improved lower extremity biomechanics after training in the AF group.8,10
Optimization of Technique
If the uncontrolled movements or other primary assessed deficits enhanced any other deficiency, then this flaw was provided as the primary feedback. If participants had multiple glaring weaknesses, the deficiency that was most modifiable, or the one that could have the potential to alter other weaknesses when corrected, was selected for the primary feedback. Technique decline was addressed by informing the participants to stay focused and continue pushing hard through the entire 10 seconds. Upon initiation of training, feedback should be aimed at correcting the most flagrant or impactful errors. Valgus knee motion during the tuck jump maneuver was selected most frequently during the initial sessions to eliminate the athletes from replication of the position most commonly correlated with the ACL injury mechanism. As the training progressed, athletes were given feedback on areas that are more difficult to fix, which became evident in the most common feedback cues that were given, including “keep the feet shoulder width apart” and “land in the same footprint.” While these deficits may not be a visually evident component of the injury mechanism, they are indicative of reduced motor control mastery. Finally, as the athletes began to exhibit improved scoring through decreased errors, the trainer gave cues on a continuum. While the athletes may not demonstrate “excess contact noise,” the cue of landing quieter and softer can be given to any athlete to reduce their landing forces regardless of proximity to perfection on the test overall.
When training to prevent injury, it is imperative for the clinician and athlete to interact. This interactive form of movement training requires intense instructor-to-athlete technique analysis with immediate and consistent feedback. The goal is to program the neuromuscular system to perform athletic maneuvers in a powerful, efficient, and safe manner. The training focus should be on perfection of the technique of each training exercise, especially early in the training program implementation. If the athlete is allowed to perform the exercise maneuvers improperly, then the training will reinforce improper techniques. The clinician should give continuous and immediate feedback both during and after each exercise bout to make the athlete aware of the proper form and technique as well as undesirable and potentially dangerous positions.30 Ultimately, as the current study results indicate, there is a strong benefit of instructor-driven feedback, which can be provided during the tuck jump exercise and can cross over to other tasks. The measureable benefits of improved frontal plane knee control during the DVJ that are associated with increased ACL injury risk6 may ultimately cross over into reductions in ACL injury during sport. Future work is warranted to determine this mechanistic link between reduced biomechanical deficits from targeted feedback training and ACL injury reduction in younger athletes.25
CONCLUSION
Female athletes may demonstrate one or more deficits that can be identified using simple video camera techniques and the provided tuck jump assessment tool. Correction of neuromuscular deficits is important for optimal biomechanics of athletic movements and may be beneficial for the reduction of knee injury incidence. Objective standardized jump-landing risk assessments, such as the tuck jump assessment, that can be quickly and easily administered by clinicians may aid in the feedback provided in injury prevention training for potentially at-risk female athletes. The results of this study indicate that providing athletes with augmented feedback has a positive effect on their biomechanics related to ACL injury measured in a different task such as the DVJ. Inclusion of a feedback-intensive plyometric program is warranted in populations that are at an increased risk of ACL injury. While the role of feedback in injury prevention training requires further investigation, this study provides additional evidence that well-planned and directed training can positively influence risk factors associated with injury. The ability of augmented feedback to support the transfer of skills and injury risk factor reductions across different tasks is novel, exciting evidence that demonstrates how neuromuscular training may ultimately cross over into retained biomechanics that reduce ACL injury during sport.
Supplementary Material
ACKNOWLEDGMENT
The authors thank Dan Brady and the Madeira High School girls’ soccer team for their participation as well as Wellington Orthopaedics, including Richelle Gwin for her invaluable support to complete this project. This project could not have been completed without the valuable help of our testing and training staff members: Kendall Christerson, Brian Richards, and Brianna Ulanowski, and the Robert S. Heidt, Sr.–Wellington Foundation.
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding was received from the National Institutes of Health (grants R01-AR049735, R01-AR055563, and R01-AR056259). Funding was also received from the National Football League Charities.
REFERENCES
- 1.Fitzgerald G, Axe M, Snyder-Mackler L. Proposed practice guidelines for nonoperative anterior cruciate ligament rehabilitation of physically active individuals. J Orthop Sports Phys Ther. 2000;30(4):194–203. doi: 10.2519/jospt.2000.30.4.194. [DOI] [PubMed] [Google Scholar]
- 2.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35(10):1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 3.Ford KR, Myer GD, Smith RL, Byrnes RN, Dopirak SE, Hewett TE. Use of an overhead goal alters vertical jump performance and biomechanics. J Strength Cond Res. 2005;19(2):394–399. doi: 10.1519/15834.1. [DOI] [PubMed] [Google Scholar]
- 4.Herman DC, Onate JA, Weinhold PS, et al. The effects of feedback with and without strength training on lower extremity biomechanics. Am J Sports Med. 2009;37(7):1301–1308. doi: 10.1177/0363546509332253. [DOI] [PubMed] [Google Scholar]
- 5.Herrington L, Myer GD, Munro A. Intra- and inter-tester reliability of the tuck jump assessment [published online October 16, 2012] Phys Ther Sport. doi: 10.1016/j.ptsp.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 7.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24(6):765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 8.Myer GD, Brent JL, Ford KR, Hewett TE. A pilot study to determine the effect of trunk and hip focused neuromuscular training on hip and knee isokinetic strength. Br J Sports Med. 2008;42(7):614–619. doi: 10.1136/bjsm.2007.046086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Myer GD, Brent JL, Ford KR, Hewett TE. Real-time assessment and neuromuscular training feedback techniques to prevent ACL injury in female athletes. Strength Cond J. 2011;33(3):21–35. doi: 10.1519/SSC.0b013e318213afa8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Myer GD, Chu DA, Brent JL, Hewett TE. Trunk and hip control neuromuscular training for the prevention of knee joint injury. Clin Sports Med. 2008;27(3):425–448. doi: 10.1016/j.csm.2008.02.006. ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Myer GD, Ford KR, Barber Foss KD, Liu C, Nick TG, Hewett TE. The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med. 2009;19(1):3–8. doi: 10.1097/JSM.0b013e318190bddb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Myer GD, Ford KR, Brent JL, Divine JG, Hewett TE. Predictors of sprint start speed: the effects of resistive ground-based vs. inclined treadmill training. J Strength Cond Res. 2007;21(3):831–836. doi: 10.1519/R-20886.1. [DOI] [PubMed] [Google Scholar]
- 13.Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:39. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric versus dynamic balance training on landing force and center of pressure stabilization in female athletes. Br J Sports Med. 2005;39(6):397. [Google Scholar]
- 15.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric versus dynamic balance training on power, balance and landing force in female athletes. J Strength Cond Res. 2006;20(2):345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 16.Myer GD, Ford KR, Hewett TE. New method to identify athletes at high risk of ACL injury using clinic-based measurements and freeware computer analysis. Br J Sports Med. 2011;45(4):238–244. doi: 10.1136/bjsm.2010.072843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Myer GD, Ford KR, Hewett TE. Rationale and clinical techniques for anterior cruciate ligament injury prevention among female athletes. J Athl Train. 2004;39(4):352–364. [PMC free article] [PubMed] [Google Scholar]
- 18.Myer GD, Ford KR, Hewett TE. Tuck jump assessment for reducing anterior cruciate ligament injury risk. Athl Ther Today. 2008;13(5):39–44. doi: 10.1123/att.13.5.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Myer GD, Ford KR, Khoury J, Hewett TE. Three-dimensional motion analysis validation of a clinic-based nomogram designed to identify high ACL injury risk in female athletes. Phys Sportsmed. 2011;39(1):19–28. doi: 10.3810/psm.2011.02.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Development and validation of a clinic-based prediction tool to identify female athletes at high risk for anterior cruciate ligament injury. Am J Sports Med. 2010;38(10):2025–2033. doi: 10.1177/0363546510370933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34(3):445–455. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 22.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19(1):51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 23.Myer GD, Paterno MV, Ford KR, Hewett TE. Neuromuscular training techniques to target deficits before return to sport after anterior cruciate ligament reconstruction. J Strength Cond Res. 2008;22(3):987–1014. doi: 10.1519/JSC.0b013e31816a86cd. [DOI] [PubMed] [Google Scholar]
- 24.Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36(6):385–402. doi: 10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
- 25.Myer GD, Sugimoto D, Thomas S, Hewett TE. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a meta-analysis [published online October 9, 2012] Am J Sports Med. doi: 10.1177/0363546512460637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Onate JA, Guskiewicz KM, Marshall SW, Giuliani C, Yu B, Garrett WE. Instruction of jump-landing technique using videotape feedback. Am J Sports Med. 2005;33(6):831–842. doi: 10.1177/0363546504271499. [DOI] [PubMed] [Google Scholar]
- 27.Onate JA, Guskiewicz KM, Sullivan RJ. Augmented feedback reduces jump landing forces. J Orthop Sports Phys Ther. 2001;31(9):511–517. doi: 10.2519/jospt.2001.31.9.511. [DOI] [PubMed] [Google Scholar]
- 28.Padua DA. Prospective cohort study of biomechanical risk factors of ACL injury: the JUMP-ACL Study. Paper presented at: American Orthopaedic Society of Sports Medicine Annual Meeting; Keystone, Colorado. 2009. [Accessed July 12, 2009]. Available at: http://www.sportsmed.org/uploadedFiles/Content/Medical_Professionals/Events/Meetings/Annual_Meeting/AM_2009/AOSSM%202009%20Final%20Program%20COMPLETE%20_lores.pdf. [Google Scholar]
- 29.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prapavessis H, McNair PJ. Effects of instruction in jumping technique and experience jumping on ground reaction forces. J Orthop Sports Phys Ther. 1999;29(6):352–356. doi: 10.2519/jospt.1999.29.6.352. [DOI] [PubMed] [Google Scholar]
- 31.Stroube B, Myer GD, Brent JL, Ford KR, Heidt RS, Jr., Hewett TE. Effects of task-specific augmented feedback on deficit modification during performance of the tuck jump assessment [published online December 11, 2012] J Sport Rehabil. doi: 10.1123/jsr.22.1.7. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. The effects of core proprioception on knee injury: a prospective bio-mechanical-epidemiological study. Am J Sports Med. 2007;35(3):368–373. doi: 10.1177/0363546506297909. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.