Abstract
Primary anterior cruciate ligament (ACL) injury prevention training has been shown to reduce the risk of injury. Less is known about the effect of prevention on second injury after ACL reconstruction (ACLR). Given recent findings that second injury rates exceed 20 % in only the first year following the return to sport, it is imperative that rehabilitation after ACLR is scrutinized so that second injury preventative strategies can be optimized. A potential limitation of current rehabilitative processes following ACLR could be a deficiency in the transition from conscious awareness achieved during rehabilitation sessions to unexpected and automatic movements required for athletic activities on the field. Learning strategies with an internally directed focus have traditionally been utilized but may be less suitable for acquisition of control of complex motor skills required for sport reintegration. Conversely, an externally focused rehabilitation strategy may enhance skill acquisition more efficiently and increase the potential to transfer to competitive sport. This article presents new insights gained from the motor learning domain that may improve neuromuscular training programmes via increased retention from improved techniques and may ultimately reduce the incidence of second ACL injuries.
1 Introduction
Athletes who wish to resume high-level activities after an injury to the anterior cruciate ligament (ACL) are advised to undergo surgical reconstruction [1]. Nevertheless, ACL reconstruction (ACLR) does not equate to normal function of the knee or a reduced risk of subsequent injuries. In the general population at 2 years after ACLR, there is a 3 % risk of ipsilateral or contralateral ACL injury [2]. Similarly, at 5 years of follow-up, an 11.8 % incidence of ACL injury in the contralateral knee and a 5.8 % incidence in the ipsilateral knee have been reported [3]. Data from the Swedish National Anterior Cruciate Ligament Register indicate that over a 5-year period after the first ACLR, 5 % of patients have a contralateral ACLR [4]. However, the true incidence of graft failure or contralateral ACL injury is not known, as the register includes only performed reconstructions or revisions. However, these data gathered from a sample most indicative of the general population are reflective of patients who most often choose to eliminate high-risk sports activities from their lifestyle, and may not accurately represent the injury risk in athletic populations.
Injury rates for a second injury exceed 20 % for young highly active athletes returning to sports within the first year after surgery [5]. In Sweden, 22 % of 15- to 18-year-old female soccer players reported a revision or contralateral ACLR during a 5-year period [4]. Recently, it was shown that a return to a high activity level after a unilateral ACLR was the most important risk factor for sustaining a contralateral ACL injury [6].
Risk factors acquired secondary to the ACL injury, such as altered biomechanics and altered neuromuscular function that affect both the injured and the contralateral leg, most likely further increase the risk of a contralateral ACL injury [5, 6].
There is significant literature indicating that altered biomechanics are evident after ACLR during activities of daily living, such as walking and going up and down stairs, but are more pronounced with athletic activities, such as jumping [7–10].
The current evidence indicates that the most common biomechanical factor associated with an increased risk of a second injury is asymmetrical loading during sports-related tasks [5, 11]. Biomechanical and neuromuscular risk factors for injury to the ipsilateral and contralateral knees have recently been established for both male and female patients after ACLR, with high sensitivity and specificity [5]. Regression analyses indicated four predictive factors for secondary injury risk, with excellent specificity (88 %) and sensitivity (92 %): uninvolved hip rotation net moment impulse during landing, frontal-plane knee motion during landing, sagittal plane knee moment asymmetries at initial contact, and deficits in postural stability on the reconstructed leg. The highly predictive model of the second injury risk underscores the importance of targeted return-to-sport rehabilitation, as all predictors are modifiable in nature [12].
Aside from the increased risk of a second injury, patients after ACLR have an increased risk of developing early onset of osteoarthritis (OA) [13]. In the USA, costs associated with OA are estimated to be US$185 billion (in 2007 dollars) on an annual basis [14]. Altered loading of the knee in terms of higher adduction moments during gait has been suggested by some as a causative factor that may lead to early onset of OA [15]. However, no studies thus far have studied this relationship prospectively, so the assumption is still speculative.
Current rehabilitation programmes focus on the range of motion, balance, strengthening and neuromuscular exercises. Criteria to determine an athlete’s readiness to return to sports after ACLR include temporal guidelines as well as balance, strength and hop tests [16]. Unfortunately, current ACLR rehabilitation programmes may not be optimally effective in addressing deficits related to the initial injury and the subsequent surgical intervention [17].
The authors of this article emphasize the need to use objective tools that are sensitive to limb-to-limb deficits and the need to develop rehabilitation protocols that are targeted to eliminate limb asymmetries. The purpose of this article is to present novel training methods that might improve rehabilitation strategies for patients after ACLR returning to pivoting-type sports and that aim to target asymmetrical movement patterns that pose a risk of a second injury. Specifically, we aim to provide a continuum of recently developed prevention programmes using novel training methods for high-risk populations, now tailored to target biomechanical risk factors as identified in patients after ACLR.
2 Motor Learning
Motor learning is defined as the process of an individual’s ability to acquire motor skills with a relatively permanent change as a function of practice or experience [18]. Therefore, researchers use retention or transfer tests (the latter involve a variation on what was practised) that are performed after a certain time interval (i.e. at least 1 day, but sometimes several days or even weeks). The purpose of this interval is to allow dissipation of any temporary performance-enhancing effects (such as effects caused by greater guidance) or performance-degrading effects (such as effects caused by increased fatigue) that certain practice conditions may have created, leaving only the relatively permanent, learning effects. Another important aspect of retention or transfer tests is that all groups perform under the same conditions (e.g. without feedback or demonstrations). Only then can the performance of different groups be compared on a ‘level playing field’, so that conclusions can be drawn about the effectiveness of different practice methods for learning.
It is generally assumed that subjects benefit from information about how to best perform a motor skill. After all, subjects must be educated about what constitutes the correct movement. It is commonly believed that direction of the athlete’s attention to step-by-step components of a skill is necessary during the early stages of acquisition [19]. Typically, feedback is given that directs the subject’s attention to various aspects of their movements. The contention is that cognitive control is necessary as a prerequisite before a subject reaches the stage during which movement control occurs more or less automatically. However, this view is not very well supported in the literature [20].
2.1 Attentional Focus
Feedback provided by clinicians during rehabilitation sessions is typically directed towards body movements. The treating clinician may tell a patient who has an altered gait pattern after ACLR to extend the knee more during the stance phase. In the motor learning domain, this type of attentional focus is termed ‘internal focus’ [21]. Conversely, an external focus of attention is induced when a patient’s attention is directed towards the outcome or effects of the movement (e.g. “imagine kicking a ball”, to facilitate extension of the knee). Reports indicate that physical therapists provide feedback that induces an internal focus 95 % of the time [22]. For example, instructions during landing from jumping are directed towards the execution of the movement itself, such as “keep the knees over the toes”, “land with a flexed knee”, “raise the knee to the level of the hip” or “land with your feet shoulder-width apart” [16, 23]. These feedback instructions have been shown to effectively target biomechanical risk factors associated with an increased risk of ACL injury in female athletes [24]. Employing newly developed advanced feedback techniques may help to further improve training adaptations.
Providing feedback that induces an external rather than internal focus may result in greater movement effectiveness (e.g. accuracy, balance) and efficiency (e.g. force production, metabolic costs) [20, 25].
While there may be intuitive reasons that clinicians tend to give internal focus instructions, this approach may not facilitate the full potential in patients after ACLR while they are relearning skills. An internal focus on one’s own movements results in a more conscious type of control that may constrain the automatic control processing of the motor system [26]. An internal focus results in an increase of co-contraction of agonists and antagonists, which in turn may cause ‘freezing’ by limiting the degrees of freedom of movements, and in the recruitment of unnecessary motor units within muscles, which adds ‘noise’ to the motor system [27]. In contrast, an external focus of attention facilitates motor learning more effectively, as a focus on the movement effect promotes utilization of unconscious or automatic processes [26]. A simple change in the wording of instructions or feedback can have dramatic effects on motor performance and learning [20]. For instance, jumping, which is often already present in the repertoire of motor skills in athletes, can be improved by adopting an external focus. In a series of studies, participants performed a jump-and-reach task with the Vertec device (Sports Imports, Hilliard, OH, USA) and were instructed to either focus on the rungs of the Vertec that were to be touched (external focus), or to focus on the finger with which the rungs were to be touched (internal focus), or to focus on jumping as high as possible (control condition) [28]. The participants’ jump-and-reach height was greatest with an external focus, compared with the other two conditions. In addition, the athletes performed the skill with more efficient neuromuscular activity when an external focus was utilized [29–31]. Recently, it was also shown that an external focus increased the accuracy of force production during an isometric plantarflexion task, in contrast to the adoption of an internal focus [27].
The challenge clinicians face is that patients after ACLR often need to reacquire motor skills that constitute good movement form in order to reduce the risk of a second injury. A recent study showed that female ACLR patients demonstrated increased knee and hip flexion during a single-leg hop task after a single day training session including landing instructions and video feedback [32]. On the other hand, studies have demonstrated that learning a movement form can be enhanced even more by wording feedback in a way that induces an external focus [33, 34]. These findings add to the evidence that an external focus could also be effective for reduction of high-risk movement patterns and the associated neuromuscular deficits [31, 35–37].
2.2 Clinical Examples
Clinicians often provide feedback in terms of correction of the patient’s faulty performance of a given task. The results of studies in the motor learning domain highlight the role of motivational influences on acquisition of motor skills [38]. It is worthwhile to give patients positive remarks to enhance learning. In most rehabilitation situations, clinicians determine the details of the training session. For example, they decide in which order tasks are to be practised, the practice duration, and when or if instructions or demonstrations will be given. Thus, while clinicians generally control most aspects of practice, patients assume a relatively passive role. Yet there is converging evidence that the effectiveness of skill learning can be considerably enhanced if the patient is given some control over the practice conditions [39].
In Sects. 2.2.1 and 2.2.2, exercises are presented to illustrate how the scientific background of the various feedback techniques can be implemented for clinical purposes. Feedback with instructions such as “land on your toes”, “straight as an arrow”, “light as a feather”, “shock absorber” and “recoil like a spring” have been shown to improve landing mechanics in a healthy population [40]. These types of neuromuscular training with augmented feedback may also be effective for reduction of observed asymmetries after ACLR [41]. The exercises chosen in Sects. 2.2.1 and 2.2.2 are adopted from earlier work describing a detailed ACLR rehabilitation programme [42]. The protocol is a four-stage, criteria-based programme designed to guide the advanced stages of rehabilitation after ACLR and to facilitate successful and safe progression of the athlete back to sports. The choice of exercises presented in this review is based on a recent study reporting that increased frontal plane knee motion and postural deficits are two specific predictors of a second ACL injury in athletes [5].
2.2.1 Postural Stability
Postural stability deficits were recently shown to be one of the four risk factors for sustaining a second injury after ACLR [5]. A postural deficit of the involved leg after ACLR may limit the ability of the athlete to control the movement of the centre of mass over the base of support during dynamic athletic activities. This underscores the importance of targeted return-to-sport rehabilitation, as postural stability is modifiable in nature. Additionally, it has been established that after a 7-week balance training programme, healthy subjects demonstrate decreased impact force during landing from a single-leg jump [43].
Although the literature on the effect of attentional foci in orthopaedic rehabilitation is sparse, more studies have emerged in recent years [44, 45]. Patients who suffered an acute ankle sprain experienced clear benefits from adoption of an external focus, as reported by Laufer et al. [44]. The results of that study indicated that three sessions of balance training with an external focus on a dynamic stabilometer improved the balance capabilities of patients who had sustained an ankle sprain. There was an improvement made immediately following training while retention was maintained. The evidence found in rehabilitation of ankle injury is one of the first demonstrations of the feasibility and relevance of applying specific principles of motor learning to orthopaedic rehabilitation. In addition, it has been shown that adding a suprapostural task may even further enhance balance, as Wulf et al. [46] found that adding a suprapostural task had a positive influence on the learning of a dynamic balance task. For comparison, two examples of instructions for practising a postural task with an internal and external focus, respectively, are presented in Table 1. The instructions should be simple, as high complexity of feedback hampers motor learning [47].
Table 1.
Internal versus external focus instruction to improve postural stability
| Goal: improve postural stability | Internal focus | External focus |
|---|---|---|
| Instructions |
|
|
| Timing of feedback | After the movement | After the movement |
| Frequencya | 33 % | 100 % (one of the instructions) |
Relative feedback, represented by the number of times that feedback is given divided by the number of trials
2.2.2 Jumping
Altered hip and knee dynamics during a dynamic double-legged jump-landing task have been shown to be a risk factor for a second ACL injury [5]. It is therefore important to address these factors before an athlete is discharged for return to pivoting-type sport. Tsai and Powers [32] reported that a combination of internal and external foci of attention resulted in increased hip and knee flexion and a decrease in muscle co-contraction in female ACLR patients. In the following paragraphs, we briefly outline how clinicians can optimally progress patients through the various stages of rehabilitation.
For example, the patient starts off with a jump-to-box to keep eccentric loading relatively low. After demonstrating good proficiency, the patient may progress to plyometric training. A broad jump is a simple, bi-pedal task that provides an appropriate starting point for plyometric activity during the end stages of ACLR rehabilitation. Initially, the patient is instructed to execute a sub-maximal effort broad jump with an extended hold time upon landing. The goal of this initial jump is two-fold. For the patient, it provides an opportunity to attempt a sub-maximal plyometric task to establish confidence in generation and attenuation of force during a plyometric activity. For the clinician, it provides an opportunity to assess proper jumping and landing techniques. Often, limb asymmetries are observed, as the patient typically increases stress on the uninvolved limb in an attempt to unweight the involved limb. Cues such as “light as a feather” and “shock absorber” should be given, since these encourage soft landing, which recruits lower extremity musculature to dampen forces during landing [40].
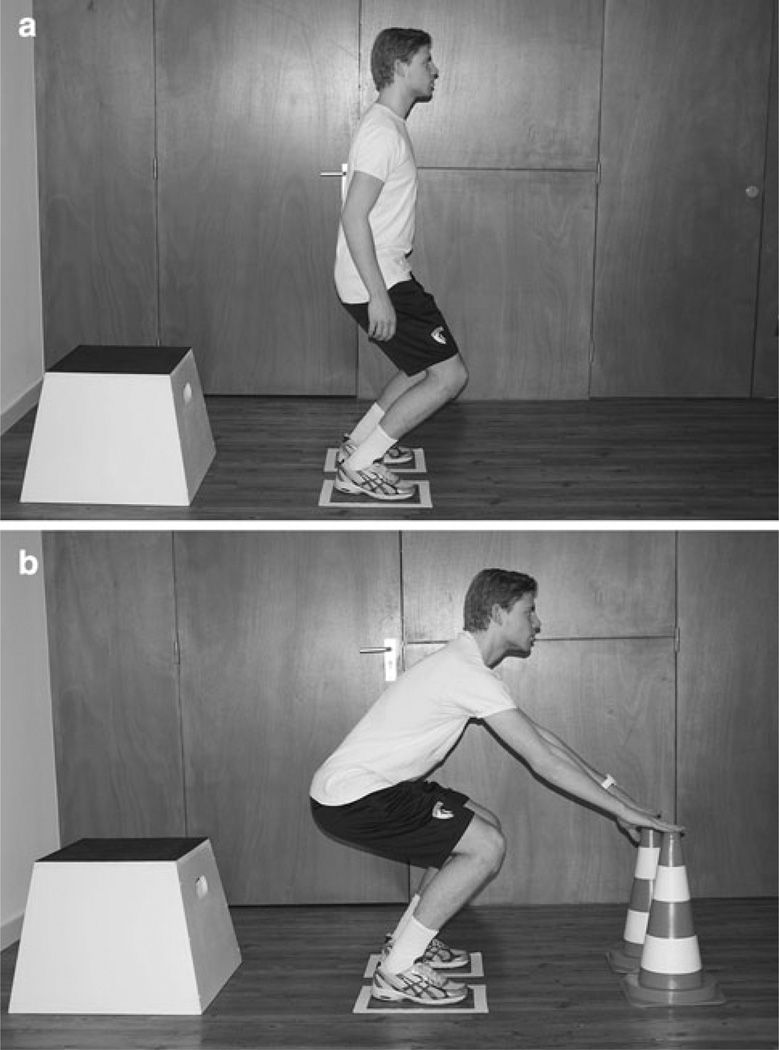
When patients after ACLR demonstrate proficiency with the broad jump task at increased intensities, they may progress to the drop vertical jump. In the internal focus condition (Fig. 1a), the patient might be instructed to land with flexion of the knee. External focus instructions can provide cues such as “land softly” to enhance shock absorption. In addition, targets (cones, foot markers, pieces of tape) can be applied to stimulate proper foot width during landing or to facilitate trunk flexion by touching the cones with the hands (Fig. 1b). More detailed information is provided in Table 2.
Fig. 1.
Internal focus a versus external focus b instructions during a drop vertical jump. In a, the patient was instructed to land while bending the hips and knees; in b, the patient was instructed to touch the cones when landing. Note the increased hip and knee flexion with the external focus instructions compared with the internal focus instructions
Table 2.
Use of internal versus external focus instructions while learning a drop vertical jump task
| Goal: improve symmetrical landing mechanics |
Internal focus | External focus |
|---|---|---|
| Instructions |
|
|
| Timing of feedback | After the movement | After the movement |
| Frequencya | 33 % | 100 % (one of the three instructions after the movement) |
Relative feedback, represented by the number of times that feedback is given divided by the number of trials
In regard to performance, increasing the distance of attention, relative to the body, immediately improves standing long jump performance compared with focus near the body [36]. These results indicate that focusing on more distant effects results in enhanced learning by promotion of utilization of more natural control mechanisms. The findings are in line with the ‘constrained action’ hypothesis, which accounts for the relatively poorer learning associated with an attentional focus directed towards effects in close proximity to the body, or towards the body itself [48]. As mentioned before, in addition to jump distance, jump height and movement efficacy can be enhanced when an external focus is used while practising the skill. These two examples illustrate that optimizing jumping technique benefits from adopting an external focus.
3 Practicing in Dyads
Providing the athlete with a visual model (dyad), like a peer athlete, can also be an effective training method. In particular, observation and practice appear to provide unique contributions to learning, such that the combination of the two can result in more effective and cumulative learning than either type of practice alone [49]. Practice in dyads can have additional learning advantages due to factors such as social interaction, competition or increased motivation. The learning advantages of dyad practice are primarily found in the opportunity to observe another learner in addition to practising without observing [50]. An effective way to practice dyad training with peers would be to alternate roles from each exercise repetition rather than one partner performing all repetitions within a set while the other partner observed, before switching roles (Table 3).
Table 3.
Practising in dyads
| Type of exercise | Instruction | Timing | Frequency |
|---|---|---|---|
| Single-leg hops with two-feet landings | In this pair-exercise, one player performs single-leg hopping forwards and from side to side, and ends by landing on two feet. The other player observes the performance of the teammate. This is followed by the players changing roles | Real time (observing) with pauses to change | After ever trial |
4 Real-Time Feedback
The use of motion analysis to display real-time biomechanics has been used in gait retraining [51, 52]. Real-time biomechanical feedback during relatively slow exercises may be a beneficial method to target persistent side-to-side asymmetries and specific movement abnormalities found in patients rehabilitating after ACLR surgery. In a recent study, subjects performed drop vertical jump trials and received immediate feedback on their knee flexion angle, trunk lean and frontal plane thigh angular velocity [53]. The subjects were able to quickly and effectively improve these variables in a single training session.
4.1 Clinical Examples of Real-Time Feedback
A slow deep bilateral squat is an exercise that is often used for real-time feedback in patients with side-to-side asymmetries. Feedback focused on external ground reaction force (GRF) is collected on force platforms and delivered either visually or audibly. An audible alert is activated if a side-to-side difference in GRF exceeds 15 % during both the descent and ascent of a squat. The benefit of this form of feedback is that the patient can perform the task and is only alerted when an error of an adjustable magnitude is exceeded. Conversely, audible cues can also be provided to reward correct performance in the form of scoring a certain number of points.
Feedback can also be displayed visually with a horizontal bar chart that represents the real-time side-to-side balance of the external force during the movement (Table 4). Incorporation of relatively inexpensive balance boards has also been utilized to provide side-to-side balanced feedback and is potentially useful in a clinical setting [54]. In a recent pilot study, a bilateral squat task was performed with real-time kinetic or kinematic data displayed [55]. This type of feedback may be utilized in athletes attempting to return to sport following an ACL injury to reduce any residual imbalances or asymmetries and specifically can be implemented in patients who are not responding well to verbal or simpler forms of instruction.
Table 4.
Examples of instructions for real-time feedback with an internal and external focus
| Goal: improve symmetrical landing mechanics |
Internal focus | External focus (real-time) |
|---|---|---|
| Instructions |
|
|
| Timing of feedback | After the movement | During the movement |
| Frequencya | 33 % | Real-time feedback during each trial, progressively decreased throughout training |
Relative feedback, represented by the number of times that feedback is given divided by the number of trials
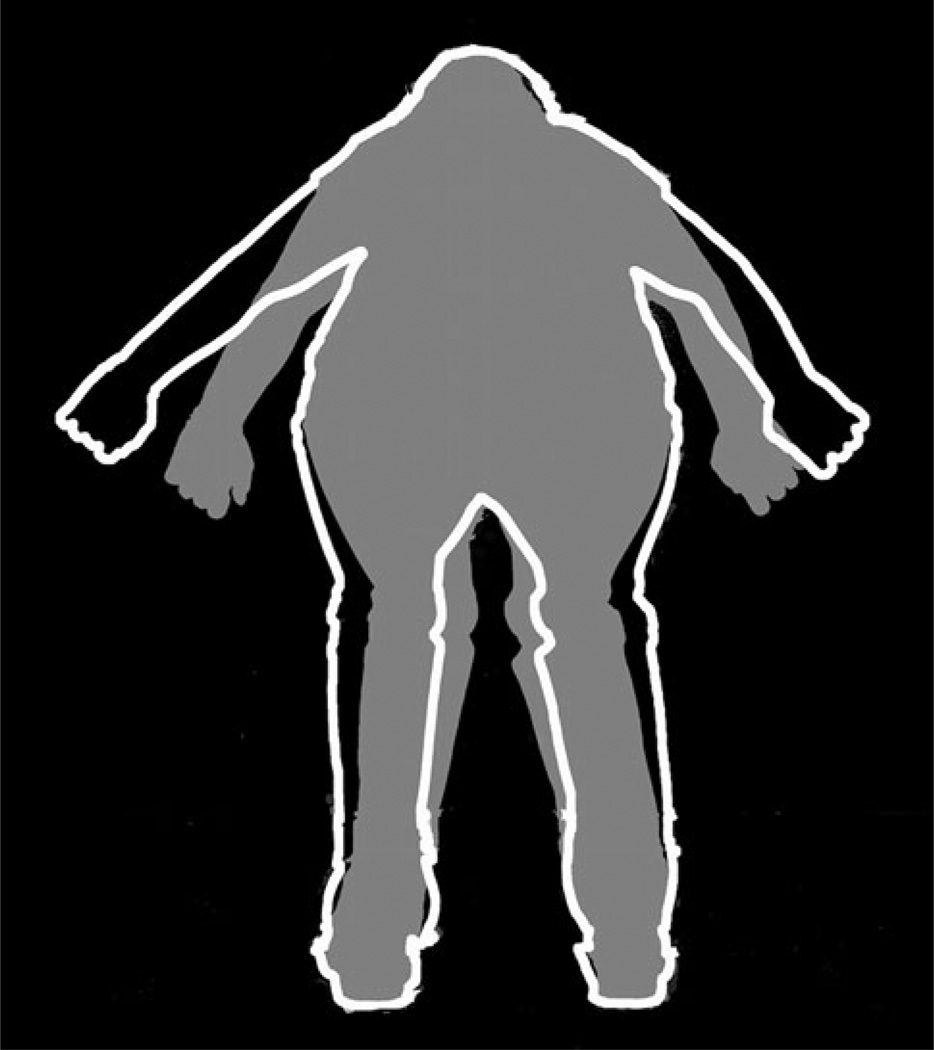
Additionally, response to feedback likely relates to certain learning styles that may differ amongst a diverse patient population. For instance, it is common to encounter a patient who does not realize that they exhibit force asymmetries during squatting (Fig. 2). Visualization of the GRF magnitudes, from each side separately, anecdotally improves the progression of their rehabilitation. We expect novel application of feedback-enhanced motor skill learning to increase with the development of wireless sensors and portable methodology. Future work to determine the potential effects of the proposed real-time feedback techniques is warranted to determine the effects on successful rehabilitation.
Fig. 2.
Real-time feedback during a squat. The patient receives information on the magnitude and direction of ground reaction forces. Visual and auditory cues are provided to correct imbalances
5 Video Overlay of Ideal Movement Pattern
In this section, we present a novel technique based on a video overlay in providing ACLR patients with feedback on their movement patterns. Over the last two decades, promising strategies in neurorehabilitation have been introduced, which are based on the so-called simulation hypothesis [56]. The hypothesis suggests that the neural networks of an action-observation system are activated not only during motor execution but also during observation or imagery of the same motor action [57]. Activation of these brain areas following observation or motor imagery may thereby facilitate subsequent movement execution by directly matching the observed or imagined action with the internal simulation of that action [58]. It is therefore possible that this multi-sensory action-observation system enables patients to (re)learn impaired motor functions through activation of these internal action-related representations [59].
5.1 Clinical Examples of Video Overlay
During the application of video overlay, the patient sees their whole body and that of a model. While looking at the screen, they ‘step into’ the template of a gender- and size-matched model on the screen. The contour of the model (‘goal pattern’), as well as the contour of the patient, is shown in an overlay. The contour of the model works like a target for the patient by instructing them to replicate the model’s movement as closely as possible. A ‘realistic’ feeling is created, and whole-body awareness is stimulated (embodied cognition). The software calculates the overlapping surface of the bodies from the patient and the model, which allows the patient to compare their performance with the performance of the model. The results are presented for 5 s by superimposing the goal movement pattern over the actual pattern from the model (video overlay) (Fig. 3). In addition, the percentage overlap is displayed on the screen in the form of a visual bar. An example of traditional instructions versus video feedback using a model overlay is presented in Table 5. Recently, readily available and affordable technology has been introduced for ACLR rehabilitation. In a randomized controlled trial that compared a Nintendo Wii Fit (Nintendo, Kyoto, Japan) balance board programme with conventional rehabilitation after ACLR, similar results were obtained in improving muscle strength, balance, coordination and response time tasks [60].
Fig. 3.
Video overlay of the model performing a drop vertical jump. Immediate after the drop vertical jump, the patient can view the overlap and try to increase their overlap with the model in the subsequent trial
Table 5.
Drop vertical jump with internal focussed instructions and video feedback with overlay
| Goal: improve bilateral symmetry |
Internal focus | Video feedback with overlay |
|---|---|---|
| Instructions |
|
|
| Timing of feedback | After the movement | During the movement After the movement when requested |
| Frequencya | <50 % | 100 % (one of the instructions after the movement) |
Relative feedback, represented by the number of times feedback is given divided by the number of trials
6 Conclusion
Motor learning with an externally directed focus, dyad training and self-controlled learning appear to be potentially beneficial for ACLR rehabilitation. As we have demonstrated, external attentional focus may enhance automatic movement control, as well as performance improvements. Ideally, properly learned motor skills will become permanent and, therefore, coaches and athletes will require less time to review and reinforce desired actions, as the newly learned skills need only periodic maintenance.
Several novel feedback techniques have been presented in this article. Future research should determine which of these techniques or whether particular combinations of these techniques work optimally, create the least dependency on feedback and yield a good transfer for ACLR patients returning to sports.
After an ACL injury, many actions have to be performed with limited amplitude and limited loading of the injured knee joint. Examples are numerous in the literature, in that loading on the ACLR knee is avoided and shifted to the uninjured side [7, 9, 12]. The current evidence indicates that an increased risk of a second injury is highly related to asymmetrical loading [5]. Biomechanical and neuromuscular risk factors include altered hip rotation in the uninvolved leg, frontal plane knee motion during landing, sagittal plane knee moment asymmetries at initial contact, and deficits in postural stability on the reconstructed leg. The highly predictive model of the second injury risk underscores the importance of targeted return-to-sport rehabilitation, as all predictors are modifiable in nature.
Although there are good intuitive reasons to suggest a more novice-like mode of motor learning by induction of an internal focus in an attempt to target these asymmetries, this strategy may not be sufficient [27].
Primary ACL injury prevention programmes are successful; however, a high number needed to treat (NNT) of 120 athletes to prevent one ACL injury may cause difficulty in gaining support from the coaching staff to implement and maintain injury prevention programmes [61]. This has likely influenced compliance, which has historically been relatively low, with reported compliance rates as low as 10.7 % when the training intervention is focused only on injury prevention [61]. As we have outlined in this article, rehabilitation employing instructions with a combination of internal and external attentional focus may enhance automatic movement control, as well as performance improvements. Ideally, properly learned motor skills will become permanent, and the newly learned skills will need only periodic monitoring.
Acknowledgments
The authors would like to acknowledge funding support from National Football League Charities and from National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases grant numbers R01-AR049735, R01-AR05563 and R01-AR056259. The authors have no conflicts of interest that are directly relevant to the content of this article.
Contributor Information
Alli Gokeler, Email: a.gokeler@umcg.nl, University of Groningen, University Medical Center Groningen, Center for Rehabilitation, P.O. Box 30.001, 9700 RB Groningen, The Netherlands.
Anne Benjaminse, University of Groningen, University Medical Center Groningen, Center for Human Movement Sciences, Groningen, The Netherlands; School of Sport Studies, Hanze University Groningen, Groningen, The Netherlands.
Timothy E. Hewett, OSU Sports Medicine, The Sports Health & Performance Institute, Departments of Physiology & Cell Biology, Orthopaedic Surgery, Family Medicine and Biomedical Engineering, The Ohio State University, Columbus, OH, USA Sports Medicine, Cincinnati Children’s Hospital Medical Center, Department of Pediatrics, College of Medicine, University of Cincinnati, Cincinnati, OH, USA.
Mark V. Paterno, Division of Occupational Therapy and Physical Therapy, Division of Sports Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA Department of Pediatrics, University of Cincinnati, College of Medicine, Cincinnati, OH, USA.
Kevin R. Ford, Department of Physical Therapy, School of Health Sciences, High Point University, High Point, NC, USA Department of Pediatrics, College of Medicine, University of Cincinnati, Cincinnati, OH, USA; Sports Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA.
Egbert Otten, Center for Rehabilitation, University of Groningen, University Medical Center Groningen, Center for Human Movement Sciences, Groningen, The Netherlands.
Gregory D. Myer, Division of Sports Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA Departments of Pediatrics and Orthopaedic Surgery, University of Cincinnati, Cincinnati, OH, USA.
References
- 1.Marx RG, Jones EC, Angel M, et al. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19(7):762–770. doi: 10.1016/s0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- 2.Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35(7):1131–1134. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]
- 3.Wright RW, Magnussen RA, Dunn WR, et al. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93(12):1159–1165. doi: 10.2106/JBJS.J.00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahlden M, Samuelsson K, Sernert N, et al. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40(10):2230–2235. doi: 10.1177/0363546512457348. [DOI] [PubMed] [Google Scholar]
- 5.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sward P, Kostogiannis I, Roos H. Risk factors for a contralateral anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):277–291. doi: 10.1007/s00167-009-1026-3. [DOI] [PubMed] [Google Scholar]
- 7.Gokeler A, Hof AL, Arnold MP, et al. Abnormal landing strategies after ACL reconstruction. Scand J Med Sci Sports. 2010;20(1):e12–e19. doi: 10.1111/j.1600-0838.2008.00873.x. [DOI] [PubMed] [Google Scholar]
- 8.Ortiz A, Olson S, Libby CL, et al. Landing mechanics between noninjured women and women with anterior cruciate ligament reconstruction during 2 jump tasks. Am J Sports Med. 2008;36(1):149–157. doi: 10.1177/0363546507307758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paterno MV, Ford KR, Myer GD, et al. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17(4):258–262. doi: 10.1097/JSM.0b013e31804c77ea. [DOI] [PubMed] [Google Scholar]
- 10.Webster KE, Feller JA, Wittwer JE. Longitudinal changes in knee joint biomechanics during level walking following anterior cruciate ligament reconstruction surgery. Gait Posture. 2012;36(2):167–171. doi: 10.1016/j.gaitpost.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(1):216–224. doi: 10.1177/0363546512459638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Myer GD, Martin L, Jr, Ford KR, et al. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: evidence for objective return-to-sport criteria. Am J Sports Med. 2012;40(10):2256–2263. doi: 10.1177/0363546512454656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oiestad BE, Holm I, Aune AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38(11):2201–2210. doi: 10.1177/0363546510373876. [DOI] [PubMed] [Google Scholar]
- 14.Kotlarz H, Gunnarsson CL, Fang H, et al. Insurer and out-of-pocket costs of osteoarthritis in the US: evidence from national survey data. Arthritis Rheum. 2009;60(12):3546–3553. doi: 10.1002/art.24984. [DOI] [PubMed] [Google Scholar]
- 15.Butler RJ, Minick KI, Ferber R, et al. Gait mechanics after ACL reconstruction: implications for the early onset of knee osteoarthritis. Br J Sports Med. 2009;43(5):366–370. doi: 10.1136/bjsm.2008.052522. [DOI] [PubMed] [Google Scholar]
- 16.Wilk KE, Macrina LC, Cain EL, et al. Recent advances in the rehabilitation of anterior cruciate ligament injuries. J Orthop Sports Phys Ther. 2012;42(3):153–171. doi: 10.2519/jospt.2012.3741. [DOI] [PubMed] [Google Scholar]
- 17.Simoneau GG, Wilk KE. The challenge of return to sports for patients post-ACL reconstruction. J Orthop Sports Phys Ther. 2012;42(4):300–301. doi: 10.2519/jospt.2012.0106. [DOI] [PubMed] [Google Scholar]
- 18.Schmidt RA, Wrisberg C. Motor learning and performance. Champaign: Human Kinetics; 2005. [Google Scholar]
- 19.Beilock SL, Carr TH, MacMahon C, et al. When paying attention becomes counterproductive: impact of divided versus skillfocused attention on novice and experienced performance of sensorimotor skills. J Exp Psychol Appl. 2002;8(1):6–16. doi: 10.1037//1076-898x.8.1.6. [DOI] [PubMed] [Google Scholar]
- 20.Wulf G. Attentional focus and motor learning: a review of 15 years. Int Rev Sport Exerc Psychol. 2013;6(1):77–104. [Google Scholar]
- 21.Wulf G, Hoss M, Prinz W. Instructions for motor learning: differential effects of internal versus external focus of attention. J Mot Behav. 1998;30(2):169–179. doi: 10.1080/00222899809601334. [DOI] [PubMed] [Google Scholar]
- 22.Durham K, Van Vliet PM, Badger F, et al. Use of information feedback and attentional focus of feedback in treating the person with a hemiplegic arm. Physiother Res Int. 2009;14(2):77–90. doi: 10.1002/pri.431. [DOI] [PubMed] [Google Scholar]
- 23.Risberg MA, Holm I. The long-term effect of 2 postoperative rehabilitation programs after anterior cruciate ligament reconstruction: a randomized controlled clinical trial with 2 years of follow-up. Am J Sports Med. 2009;37(10):1958–1966. doi: 10.1177/0363546509335196. [DOI] [PubMed] [Google Scholar]
- 24.Myer GD, Ford KR, Brent JL, et al. An integrated approach to change the outcome part II: targeted neuromuscular training techniques to reduce identified ACL injury risk factors. J Strength Cond Res. 2012;26(8):2272–2292. doi: 10.1519/JSC.0b013e31825c2c7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lohse KR, Wulf G, Lewthwaite R. Attentional focus affects movement efficiency. London: Routledge; 2012. [Google Scholar]
- 26.Wulf G, McNevin N, Shea CH. The automaticity of complex motor skill learning as a function of attentional focus. Q J Exp Psychol A. 2001;54(4):1143–1154. doi: 10.1080/713756012. [DOI] [PubMed] [Google Scholar]
- 27.Lohse KR, Sherwood DE. Thinking about muscles: the neuromuscular effects of attentional focus on accuracy and fatigue. Acta Psychol (Amst) 2012;140(3):236–245. doi: 10.1016/j.actpsy.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 28.Zachry TL, Wulf G, Mercer JA. Effects of focus of attention on reach height. J Sport Exerc Psychol. 2005;27:S162–S163. [Google Scholar]
- 29.Makaruk H, Porter JM, Czaplicki A, et al. The role of attentional focus in plyometric training. J Sports Med Phys Fitness. 2012;52(3):319–327. [PubMed] [Google Scholar]
- 30.Wulf G, Dufek JS. Increased jump height with an external focus due to enhanced lower extremity joint kinetics. J Mot Behav. 2009;41(5):401–409. doi: 10.1080/00222890903228421. [DOI] [PubMed] [Google Scholar]
- 31.Wulf G, Dufek JS, Lozano L, et al. Increased jump height and reduced EMG activity with an external focus. Hum Mov Sci. 2010;29(3):440–448. doi: 10.1016/j.humov.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 32.Tsai LC, Powers CM. Increased hip and knee flexion during landing decreases tibiofemoral compressive forces in women who have undergone anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(2):423–429. doi: 10.1177/0363546512471184. [DOI] [PubMed] [Google Scholar]
- 33.Wulf G, Shea C, Lewthwaite R. Motor skill learning and performance: a review of influential factors. Med Educ. 2010;44(1):75–84. doi: 10.1111/j.1365-2923.2009.03421.x. [DOI] [PubMed] [Google Scholar]
- 34.An J, Wulf G, Kim S. Increased carry distance and X-factor stretch in golf through an external focus of attention. J Motor Learn Dev. 2013;1:2–11. [Google Scholar]
- 35.Zachry T, Wulf G, Mercer J, et al. Increased movement accuracy and reduced EMG activity as the result of adopting an external focus of attention. Brain Res Bull. 2005;67(4):304–309. doi: 10.1016/j.brainresbull.2005.06.035. [DOI] [PubMed] [Google Scholar]
- 36.Porter JM, Anton PM, Wu WF. Increasing the distance of an external focus of attention enhances standing long jump performance. J Strength Cond Res. 2012;26(9):2389–2393. doi: 10.1519/JSC.0b013e31823f275c. [DOI] [PubMed] [Google Scholar]
- 37.Porter JM, Ostrowski EJ, Nolan RP, et al. Standing long-jump performance is enhanced when using an external focus of attention. J Strength Cond Res. 2010;24(7):1746–1750. doi: 10.1519/JSC.0b013e3181df7fbf. [DOI] [PubMed] [Google Scholar]
- 38.Chiviacowsky S, Wulf G. Feedback after good trials enhances learning. Res Q Exerc Sport. 2007;78(2):40–47. doi: 10.1080/02701367.2007.10599402. [DOI] [PubMed] [Google Scholar]
- 39.Lewthwaite R, Wulf G. Motor learning through a motivational lens. London: Routledge; 2012. [Google Scholar]
- 40.Hewett TE, Stroupe AL, Nance TA, et al. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24(6):765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 41.Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(1):216–224. doi: 10.1177/0363546512459638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Myer GD, Paterno MV, Ford KR, et al. Neuromuscular training techniques to target deficits before return to sport after anterior cruciate ligament reconstruction. J Strength Cond Res. 2008;22(3):987–1014. doi: 10.1519/JSC.0b013e31816a86cd. [DOI] [PubMed] [Google Scholar]
- 43.Myer GD, Ford KR, Brent JL, et al. The effects of plyometric vs. dynamic stabilization and balance training on power, balance, and landing force in female athletes. J Strength Cond Res. 2006;20(2):345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 44.Laufer Y, Rotem-Lehrer N, Ronen Z, et al. Effect of attention focus on acquisition and retention of postural control following ankle sprain. Arch Phys Med Rehabil. 2007;88(1):105–108. doi: 10.1016/j.apmr.2006.10.028. [DOI] [PubMed] [Google Scholar]
- 45.Rotem-Lehrer N, Laufer Y. Effect of focus of attention on transfer of a postural control task following an ankle sprain. J Orthop Sports Phys Ther. 2007;37(9):564–569. doi: 10.2519/jospt.2007.2519. [DOI] [PubMed] [Google Scholar]
- 46.Wulf G, Weigelt M, Poulter D, et al. Attentional focus on suprapostural tasks affects balance learning. Q J Exp Psychol A. 2003;56(7):1191–1211. doi: 10.1080/02724980343000062. [DOI] [PubMed] [Google Scholar]
- 47.Marchant DC, Clough PJ, Crawshaw M. The effects of attentional focusing strategies on novice dart throwing performance and their task experiences. Int J Sport Exerc Psychol. 2007;5(3):291–303. [Google Scholar]
- 48.McNevin NH, Shea CH, Wulf G. Increasing the distance of an external focus of attention enhances learning. Psychol Res. 2003;67(1):22–29. doi: 10.1007/s00426-002-0093-6. [DOI] [PubMed] [Google Scholar]
- 49.Shea CH, Wulf G, Whitacre C. Enhancing training efficiency and effectiveness through the use of dyad training. J Mot Behav. 1999;31(2):119–125. doi: 10.1080/00222899909600983. [DOI] [PubMed] [Google Scholar]
- 50.Granados C, Wulf G. Enhancing motor learning through dyad practice: contributions of observation and dialogue. Res Q Exerc Sport. 2007;78(3):197–203. doi: 10.1080/02701367.2007.10599417. [DOI] [PubMed] [Google Scholar]
- 51.Barrios JA, Crossley KM, Davis IS. Gait retraining to reduce the knee adduction moment through real-time visual feedback of dynamic knee alignment. J Biomech. 2010;43(11):2208–2213. doi: 10.1016/j.jbiomech.2010.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2011;45(9):691–696. doi: 10.1136/bjsm.2009.069112. [DOI] [PubMed] [Google Scholar]
- 53.Dowling AV, Favre J, Andriacchi TP. Inertial sensor-based feedback can reduce key risk metrics for anterior cruciate ligament injury during jump landings. Am J Sports Med. 2012;40(5):1075–1083. doi: 10.1177/0363546512437529. [DOI] [PubMed] [Google Scholar]
- 54.McGough R, Paterson K, Bradshaw EJ, et al. Improving lower limb weight distribution asymmetry during the squat using Nintendo Wii Balance Boards and real-time feedback. J Strength Cond Res. 2012;26(1):47–52. doi: 10.1519/JSC.0b013e318220b515. [DOI] [PubMed] [Google Scholar]
- 55.Ford KR, DiCesare C, Myer GD, et al. Real-time biofeedback for ACL injury prevention. Gainesville: American Society of Biomechanics Annual Meeting; 2012. [Google Scholar]
- 56.Holper L, Muehlemann T, Scholkmann F, et al. Testing the potential of a virtual reality neurorehabilitation system during performance of observation, imagery and imitation of motor actions recorded by wireless functional near-infrared spectroscopy (fNIRS) J Neuroeng Rehabil. 2010;7:57. doi: 10.1186/1743-0003-7-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lotze M, Montoya P, Erb M, et al. Activation of cortical and cerebellar motor areas during executed and imagined hand movements: an fMRI study. J Cogn Neurosci. 1999;11(5):491–501. doi: 10.1162/089892999563553. [DOI] [PubMed] [Google Scholar]
- 58.Rizzolatti G. The mirror neuron system and its function in humans. Anat Embryol. 2005;210(5–6):419–421. doi: 10.1007/s00429-005-0039-z. [DOI] [PubMed] [Google Scholar]
- 59.Fadiga L, Fogassi L, Pavesi G, et al. Motor facilitation during action observation: a magnetic stimulation study. J Neurophysiol. 1995;73(6):2608–2611. doi: 10.1152/jn.1995.73.6.2608. [DOI] [PubMed] [Google Scholar]
- 60.Baltaci G, Harput G, Haksever B, et al. Comparison between Nintendo Wii Fit and conventional rehabilitation on functional performance outcomes after hamstring anterior cruciate ligament reconstruction: prospective, randomized, controlled, double-blind clinical trial. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):880–887. doi: 10.1007/s00167-012-2034-2. [DOI] [PubMed] [Google Scholar]
- 61.Sugimoto D, Myer GD, McKeon JM, et al. Evaluation of the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a critical review of relative risk reduction and numbers-needed-to-treat analyses. Br J Sports Med. 2012;46(14):979–988. doi: 10.1136/bjsports-2011-090895. [DOI] [PMC free article] [PubMed] [Google Scholar]