Abstract
Background
In the United States, research on health disparities has begun to include people with disabilities as a minority population. However, there is a gap in our knowledge of whether, and to what extent, racial and ethnic disparities may affect the health or healthcare access of people with disabilities.
Objectives
We examined potential disparities in overall health, insurance coverage status and health service use between non-Hispanic whites, non-Hispanic blacks and Hispanics, among a nationally representative U.S. sample of adults with and without disabilities (N=63,257) using both bivariate and multivariate methods. We tested two definitions of disparity.
Results
Under the more conservative definition, we confirmed the presence of both racial and ethnic disparities in overall health, total annual healthcare visits and the percentage reporting no doctor visit during the year among people with less severe disabilities; Hispanics also evidenced a disparity in rates uninsured relative to Non-Hispanic whites in this group. Racial/ethnic disparities were less common among persons with more severe disabilities that affected activities of daily living or instrumental activities.
Conclusions
We conclude that the reduction of disparities between the populations of people with and without disabilities will require specific attention to racial and ethnic disparities in health, insurance coverage and service use.
Keywords: United States, Disabled Persons, Healthcare Disparities, Population Groups, Health Services Accessibility
INTRODUCTION
The scientific understanding of disability has undergone a paradigm shift from a simpler conception of functional limitations as a direct and severe consequence of medical pathology to a much more sophisticated view such as that advanced in the Institute of Medicine conceptual model of disability or the International Classification of Functioning, Disability and Health.1-3 This shift situates the individual, his or her health conditions and possible limitations in functioning, well-being and social participation within the broader environment around the person.4 It allows for a wide continuum of differences in functioning and health between all people and provides a new perspective on how not only the built environment, but social attitudes, professional practices and public policies, co-determine the health and societal participation of people living with many different kinds of health conditions and disabilities.5 From this new vantage point, the health of people with disabilities does not hinge on the biology of their bodies alone, but also on equitable access to healthcare services and supports, societal resources and opportunities to participate.6
Researchers working from this modern disability perspective have documented inequities between people with and without disabilities in overall health, 5,7,8 rates of specific health conditions, 7,9 service access and utilization, 5,10-12 preventive care and screening rates 8,13-15 and doctor-patient communications.16 Of course, people with disabilities can and do experience many of the same access problems as their non-disabled counterparts, including spells without medical insurance17, insufficient cultural (or linguistic) competence among medical providers18, or coordination issues with their health care services.19 However, they may also experience barriers that are specific to having a disability such as physical inaccessibility of facilities or equipment, inadequate provider training or lack of sign language interpreters.20-23
What remains less well documented in this disability literature is the extent to which people with disabilities may also face healthcare barriers specifically related to their race or ethnicity. When race/ethnicity does appear in this research, it is often included as a simple control variable, 7,16 or the focus is more symbolic, as when the disparities recorded between people with and without disabilities are likened to those faced by racial or ethnic minorities.5,24
Key issues in health disparities research
In traditional health disparities research on race or ethnicity, there is considerable debate over how to define the population groups to be compared, when to control potentially confounding variables and whether to label a difference between groups a “disparity”. 25 Two differing theoretical orientations illustrate this debate. In a society where racial and ethnic minority groups face institutionalized disadvantages in social determinants of health, one theory holds that any health or health care difference between the majority and the minority is potentially a disparity. From this standpoint, these determinants sit within a causal chain linking the minority group and the chosen outcome measure.25 As such, they should not be statistically controlled.26 For instance, if African Americans are found to have fewer doctor visits than whites, the results cannot be fairly explained away as a result of wealth differentials if the latter are also the result of racial inequalities; In such an instance, the healthcare system may still have responded inequitably to African Americans through its failure to adequately serve the poor.
A second orientation holds that a minority-majority difference only becomes a disparity after clinical needs and individual preferences for care have been controlled. For example, if African-Americans have higher clinical need for medical services than whites in the first place, from this standpoint it would be a mistake to use the unadjusted findings to determine a disparity; a true disparity in doctor visits could be masked by the elevated health care needs of African Americans unless that difference is first controlled.26-28
Until recently, people with disabilities, whatever their race or ethnicity, have not been considered as a minority group in the traditional field of health disparities. From the work of disability researchers, it is known that people with disabilities are disproportionally high users of care from doctors, hospitals, prescription medications, emergency rooms and home health providers.19,29,30 On average, they must secure treatment for not one, but typically multiple chronic conditions simultaneously, particularly should they need assistance with activities of daily living (ADLs or IADLs).30,31 Medical care is thus a paramount concern for people with disabilities, yet we do not fully know whether, or to what extent, racial or ethnic disparities may be hindering their access.
QUESTIONS FOR RESEARCH
Our primary research question was: Among two separate groups of people with disabilities and a contrast group of people without them, are there racial or ethnic disparities between non-Hispanic whites versus non-Hispanic blacks, or Hispanics, in 1) overall health, 2) insurance coverage status or 3) health service use? Given the well-established disparities in these three areas among blacks and Hispanics in the general adult U.S. population, we sought to determine whether and to what extent these disparities specifically affect people with disabilities. In light of the controversies noted earlier, we assessed the sensitivity of the results to two different definitions of disparity in these analyses, as follows:
Among people with disabilities, racial/ethnic disparities in health or health care are differences not due to age alone that suggest a disadvantage for either non-Hispanic blacks or Hispanics when compared to non-Hispanic whites.
Among people with disabilities, racial/ethnic disparities in health or health care are differences not due to age, clinical needs or preferences for care that suggest a disadvantage for either non-Hispanic blacks or Hispanics when compared to non-Hispanic whites.
As suggested by these definitions, we opted to control for age throughout all analyses because it is highly correlated with disability, because racial/ethnic groups vary by age, and because age is associated with overall health, insurance coverage and service use.
Disability itself can be measured in many different ways depending on the purposes for which a study is conducted in the first place.3,32 We opted for an operational approach that is well-suited to survey-based health services research because it focuses primarily upon phenomena that can be directly reported. These include the presence of functional limitations, activity limitations or limitations in activities of daily living (ADLs). These core domains have been used to capture the disabled population in many previous healthcare related studies.3 We also operationalized the need for supervision or support with ADLs or instrumental ADLs (IADLs) as a means to identify a subgroup of people with disabilities with particularly high needs for medical care and supportive services. In previous studies, ADLs and IADLs have been shown to identify elevated health service needs and utilization across many different kinds of disabilities.17,19,30,31,33
METHODS
Data source
We analyzed the 2006–2008 Medical Expenditure Panel Survey (MEPS).34 After pooling years, we used 63,257 cases to obtain our weighted estimates for approximately 219 million community dwelling civilians aged 18 and up.
Disability measures
Remaining consistent with the MEPS questionnaires35, we measured disability as a self-reported limitation in any combination of the following domains: physical functioning (walking, climbing stairs, grasping objects, reaching overhead, lifting, bending or stooping, or standing for long periods), sensory impairment (moderate, major or total impairment in seeing or hearing after use of glasses or other devices), cognitive difficulties (confusion, memory loss or need for supervision for safety), primary activities (such as work, housework or school), social limitations (such as recreational, family or social events), assistive device use (walkers, grab bars in the bathtub or any other special equipment for personal care or everyday activities) and/or ADLs/IADLs (the need for help or supervision with: bathing, dressing, getting around the house, using the telephone, paying bills, taking medications, preparing light meals, doing laundry or going shopping because of an impairment or a physical or mental health problem during the year). We then divided individuals reporting any of these items into two groups: persons who remained independent with ADLs and IADLs throughout the year, and individuals who instead required help or supervision with ADLs/IADLs at any point during the year.
Race/ethnicity
From the measures available in the MEPS36, we derived the following mutually exclusive categories for our analyses: a) non-Hispanic white - no other races reported; b) non-Hispanic, black - no other races reported; c) non-Hispanic, other race or races; and d) Hispanic of any race or races.
Primary outcome measures
We examined overall health (any report of fair-poor health during the course of the year), insurance coverage status (any month without coverage during the year) and service utilization (including total annual ambulatory health care visits and the percent who reported going without a doctor visit). We limited our insurance analyses to persons age 18-65 since the vast majority of elders are covered by Medicare and/or private insurance.
Additional measures
In order to more fully describe any racial/ethnic disparities in overall health, we also assessed several related variables, including BMI (body mass index >= 30), physical activity (exercise 3 times per week or more) and mental health status (fair or poor at any time during the year). Similarly, to complement the analyses of insurance status, we examined the duration uninsured (part year or full year) and coverage source (public or private). Other measures used include: age (in years), gender, education (< high school diploma or GED), poverty status (<125% of the federal poverty level), census region (Northeast, Midwest, South or West) and MSA status. In a number of the analyses, we controlled for respondent preferences, including endorsements of the beliefs that “I can overcome illness without help from a medically trained person” and “I’m healthy enough that I really don’t need health insurance”.
Statistical methods
To test for racial/ethnic disparities under definition one, we conducted bivariate analyses (chi-square and pairwise T-tests) within three main population groups of adults: people without disabilities, people with non-ADL/IADL disability limitations and people needing help or supervision with ADLs/IADLs. Except where noted, all bivariate analyses were directly age standardized using the weighted analytic sample as the standard population. We controlled the false discovery rate for the primary outcomes.37 The results are weighted to provide nationally representative, average annual estimates for the period of 2006-2008.38
To test for disparities under definition two, we fit separate models for people without disabilities, people with non-ADL/IADL limitations and individuals with ADL/IADL limitations. Age was included as a covariate in all analyses, alongside race/ethnicity, disability status, gender, preferences for care and insurance, and where appropriate, overall health. Logistic regression was used to model dichotomous variables, including fair-poor overall health, any gap in insurance coverage and no doctor visit during the year. Annual ambulatory health visits were modeled with a loglink procedure for count data. The Taylor series linearization was used tp adjust for the complex sampling plan in the MEPS.
RESULTS
We examined three separate U.S. adult population groups: people without disabilities (169.3 million individuals) people with non-ADL/IADL limitations (36.2 million) and people with ADL/IADL limitations (13.3 million). Descriptively, people with ADL/IADL limitations were the smallest population group (6.1% of all adults), the oldest (mean = 62.9 years, before standardization), and potentially the most vulnerable as well (28% had less than a high school level education, 34% reported an income near or below the federal poverty level and 70% reported their health to be fair or poor.) Of the three populations, this group had the highest levels of health service use. Twenty-three percent reported at least one month without insurance coverage during the year.
By contrast, people with non-ADL/IADL limitations were a significantly larger (16.5% of all adults) and younger (mean age=56.9 years) group with greater resources and better health than individuals who were ADL/IADL limited (18% had less than a high-school level education, 24% had an income near or below the federal poverty level, 48% reported their health to be fair or poor and there were lower levels of health service use in this group compared to persons with ADL/IADL limitations.) This group was the most likely to be uninsured of all three populations, with thirty-five percent reporting at least one month without coverage.
These differences between the ADL/IADL and non-ADL/IADL disability populations need to be held in the proper perspective. Though different, both of these groups are significantly older, have substantially fewer resources and report significantly lower overall health than people without disabilities.
Differences in racial/ethnic makeup
Descriptively, we found significant differences in the racial/ethnic make-up of these three population groups. At sixteen percent, NH blacks were over-represented in the ADL/IADL limitation group relative to the no disability group (10.6%, t=5.09, p<.001). With thirteen percent describing themselves as NH Black, the non-ADL/IADL limitation group also differed significantly from the no disability group (t=4.28, p<.001). However, Hispanics were significantly underrepresented in the two disability groups relative to their numbers in the non-disabled group [No disability (13.9% Hispanic), versus non-ADL/IADL limitations (9.9% Hispanic, t=7.07, p<.001) and versus ADL/IADL limitations (10.6% Hispanic, t=4.06, p<.001)].
Disparities on the basis of race/ethnicity among people with disabilities: Two definitions compared
Overall health
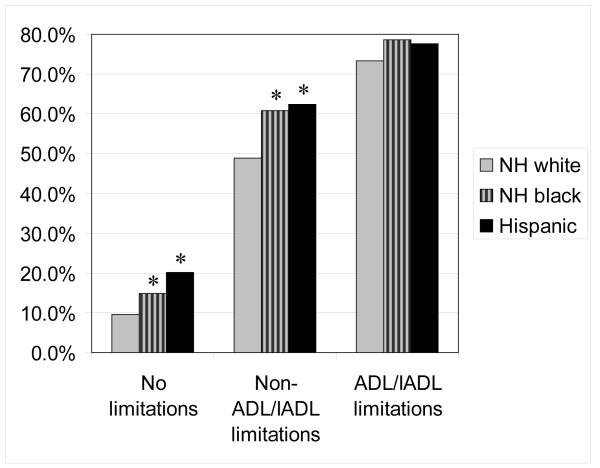
Under our first definition (age standardized, but otherwise uncontrolled), we found evidence of NH white – NH black, and NH white – Hispanic disparities among persons without disabilities; just 10% of NH whites in this group reported fair to poor health during the year, compared to 17% of NH blacks and 25% of Hispanics. We found these same disparities among persons with non-ADL/IADL limitations for whom the percentages were 45%, 57% and 60%, respectively. Among persons with ADL/IADL limitations, we found the greatest absolute rates of fair to poor health, but the racial/ethnic differences were no longer significant at 68%, 73% and 75%, respectively. As shown in figure 1, after modeling overall health on the basis of age, gender, preferences for care and insurance, the findings did not significantly change under our second definition of disparity.
Figure 1. Differences in fair or poor overall health on the basis of race/ethnicity among persons with and without disability limitations: Covariate adjusted, predicted marginal percentages, MEPS 2006-2008 (pooled data).
Estimates based on logistic regression models controlling for age, sex, and beliefs about the importance of medical care and insurance.
* differs significantly (p<.05) from the estimate for non-hispanic whites with the same disability status.
In order to further characterize these results, we also examined simple age-standardized differences in overall mental health, body mass index, and being physically active three times or more per week. In the non-disabled and non-ADL/IADL populations, significant racial/ethnic differences in these measures were detected, generally following the same overall health profiles just described.
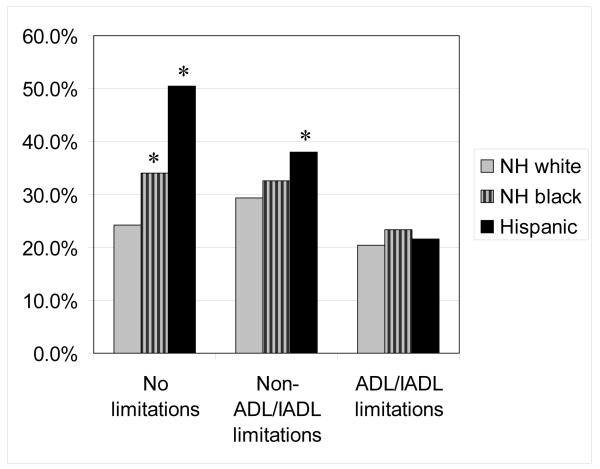
Insurance coverage status
We limited these analyses to the working aged (18-65). For each separate population group, we tested for simple age-standardized disparities in the percentage reporting a full 12 months of coverage (whether public or private) on the basis of race/ethnicity under disparity definition one. Relative to NH whites, we found disparities among NH Blacks and Hispanics among people without disabilities. We also found disparities for Hispanics among people with non-ADL/IADL limitations. We found no evidence of disparities among people with ADL/IADL limitations. As shown in figure two, upon controlling for age, gender, overall health and preferences for care and insurance in the controlled model for definition 2, the findings remained similar.
Figure 2. Any period without insurance coverage during the year on the basis of race/ethnicity among persons with and without disability limitations: Covariate adjusted, predicted marginal percentages, MEPS 2006-2008 (pooled data).
Estimates based on logistic regression models controlling for age, sex, overall health and beliefs about the importance of medical care and insurance.
* differs significantly (p<.05) from the estimate for non-Hispanic whites with the same disability status.
To further characterize these results, we examined simple age standardized comparisons of insurance source (public or private) among those with continuous coverage, and for persons with any gap, whether that gap covered part or all of the year. Among people without disabilities, the racial and ethnic disparities noted above were composed of both part year and yearlong gaps. Among people with non-ADL/IADL limitations (where we found a disparity between NH whites and Hispanics), it appeared that disparity may be more strongly associated with long term uninsurance.
Among the continuously insured, in simple age adjusted analyses, public sources played an increasingly important role in assuring coverage when people with non-ADL/IADL limitations were compared to the non-disabled, and when people with ADL/IADL limitations were compared to individuals with non-ADL/IADL limitations. Further, public sources provided coverage for racial/ethnic minorities at a higher level than they did for NH whites in all three population groups. Accordingly, we found very pronounced rates (and racial/ethnic differences between them) of public coverage among people with ADL/IADL limitations; 51% of NH whites with continuous insurance coverage held it through public sources alone in this group, while for Hispanics this rate climbed to 70% and for NH blacks, to 78%.
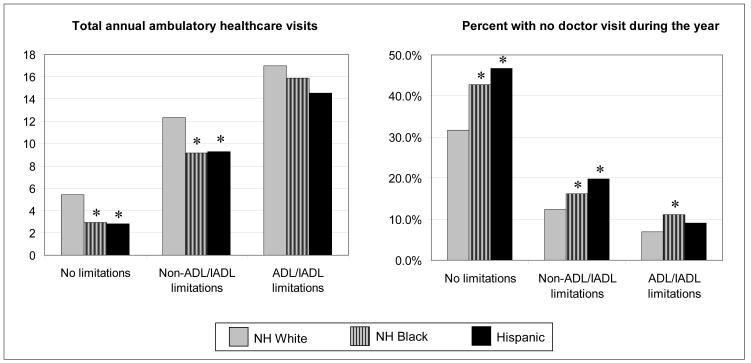
Health service utilization
Regarding total ambulatory visits, we found significant racial/ethnic disparities for NH blacks and for Hispanics when compared to NH whites in all three of the populations examined. In the definition one analyses, among persons with non-ADL/IADL limitations, NH whites averaged 10.6 visits per year, while NH blacks and Hispanics both averaged 8.5. Among persons with ADL/IADL limitations, these averages rose even as the disparities remained (17.6 visits per year among NH whites, 14.0 among NH Blacks, and 13.4 visits among Hispanics). To follow definition two, we fit loglink models of total ambulatory health care visits during the year for each population group on the basis of age, gender, overall health, preferences for care and race/ethnicity. The results included significant racial/ethnic health disparities among people without disabilities and among individuals with non-ADL/IADL limitations (figure 3, first panel). However, we found no disparities among ADL/IADL limited persons on the basis of these models.
Figure 3. Differences in annual healthcare utilization during the year on the basis of race/ethnicity among persons with and without disability limitations: Covariate adjusted, predicted marginal percentages, MEPS 2006-2008 (pooled data).
Estimates of total ambulatory health care visits based on loglink models controlling for age, sex, overall health and beliefs about the importance of medical care and insurance.
* differs significantly (p<.05) from the estimate for non-Hispanic whites with the same disability status.
Turning to the percentage with no doctor visit during the year, among people without disabilities, there were significant disparities between NH whites, NH blacks and Hispanics. In the simple age standardized results, among people with non-ADL/IADL limitations, we found evidence of a disparity between NH whites (17% without a doctor visit) and Hispanics (25%), but not among NH blacks. Among people with ADL/IADL limitations we did not detect any such disparity. However, under definition two, we found further evidence of racial/ethnic disparities among both disability groups (see figure 3, second panel). After controlling for age, sex, overall health and preferences for care and insurance, in the non-ADL/IADL group, both Hispanics and NH blacks were significantly more likely to report going without a doctor visit than were NH whites. Further, under definition two, among ADL/IADL limited individuals we detected a significant disparity between NH blacks and NH whites.
DISCUSSION
The well-known U.S. racial/ethnic disparities in health, insurance coverage and health service utilization reach into the population of adults with disabilities under two different definitions of disparity. Most of the racial/ethnic disparities documented above were detected among individuals with non-ADL/IADL limitations. In at least one sense, this may be welcome news in that people with ADL/IADL limitations are certainly that subgroup with the worst health, the fewest resources and the highest need for health care services. Yet, they are also the numeric minority of people with disabilities. Further, it is critical to recall that individuals with non-ADL/IADL limitations are more likely to be poor, to have less than a high school-level education, to be in fair-poor overall health, to be uninsured and/or to have extensive health care needs when compared to people without disabilities.
It is also striking to consider that under both definitions, among individuals with non-ADL/IADL limitations, racial and ethnic minorities simultaneously reported higher levels of fair-poor health than did whites, yet lower rates of ambulatory health visits than NH whites. In this non-ADL/IADL group, Hispanic individuals fared particularly poorly. Despite the fact that over 60% of such persons reported their health to be fair or poor, over one-third were without insurance coverage at some point during the year and one in five went without any doctor visit.
Overall health
The finding that the overall health of people with disabilities is more likely to be poor than that reported by people without disabilities is not surprising, but do these differences amount to a disparity? One line of argument suggests that since people with disabilities often have pre-existing health problems, differences between people with and without disabilities are inherently differences and not disparities. However, such a strict argument hinges on the assumption that the health of people with disabilities is only biologically determined. A counter-argument suggests that poor or not, the health of people with disabilities still depends on equitable access to health care services – or fair access to other health-related social goods such as education or income. Looking inside the population of people with disabilities, the finding of poorer health among many non-Hispanic blacks and Hispanics than among non-Hispanic whites supports this second argument. It further suggests that at least some portion of the health status of people with disabilities may not be explained by biology alone, but may also stem from a known social inequity based on race/ethnicity.
Insurance coverage status
Uninterrupted health insurance coverage is of vital importance to many people with disabilities for the access it provides to services that are needed on an ongoing basis. It is particularly noteworthy that the group with the largest percentage uninsured was people with non-ADL/IADL disabilities. Another key point is that public sources play a central role in providing coverage to both people with disabilities and racial/ethnic minorities. This can be seen directly in the findings for people with ADL/IADL limitations, where among those with continuous insurance during the year, 51% of NH whites, 78% of NH blacks and 70% of Hispanics received their coverage solely from public sources. Consequently, cutbacks to public insurance programs may not only undercut a vital source of coverage for people with disabilities, they may also disproportionally affect racial and ethnic minorities among them.
Health service use
Among people with disabilities, we found evidence of racial/ethnic disparities in the total volume of health care visits and in the percentage of individuals who reported going without any doctor visit. Of each of the broad areas examined in this study, health service use was the most sensitive to the definition of disparity that we applied. For example, in our analyses of the percentage going without a doctor visit, we found evidence of disparities that would otherwise have gone undetected without the statistical adjustments called for under definition two.
Additional analysis and more detailed measures will be required to map any causal connections between race/ethnicity, disability, health, preferences for care and actual use of health services. However, one point seems clear: with different definitions of disparities, we will surely yield different findings.
Limitations
Though our goal was to define race/ethnicity in a manner that most resembles what can be found in the broader health disparities field, we must acknowledge that the three categories we compared are reductionist. For instance, it is known that healthcare outcomes differ among Mexican, Puerto Rican, Cuban, Central/South American, and other Hispanic/Latino groups.39 Differences between these groups (and other important racial/ethnic groups) were not explored due both to sample size and length constraints.
It should also be noted that there are many ways of measuring disability. With different operationalizations, different findings will result. Much as can be said for race/ethnicity, the underlying issues may be too complicated to allow for one unified definition of disability that suits all purposes.
Conclusion
In this study, we provide an alternative perspective that differs in several important ways from traditional health disparities research. In the mainstream of that work, disability is typically understood as an outcome to be reduced, in much the same way that good health is understood to be a desirable goal. In these analyses, we took a different approach, identifying the primary population groups to be studied directly on the basis of disability and then studying potential racial / ethnic disparities within them.
This conceptual and empirical shift enabled us to analyze a number of possible relationships that, to date, have been too little explored. First, it allowed for the possibility that, while strongly correlated, overall health and disability are distinct concepts. One can have any number of functional or activity limitations and still report good health, and indeed, we found that the health of people with disabilities does vary with their race/ethnicity. Second, by taking this approach, it was possible to demonstrate that access to resources, such as income or education, is constrained on the basis of race/ethnicity even among those individuals most likely to be impoverished in the first place, people with ADL/IADL disabilities. Third, we showed not only that many Hispanics with disabilities are uninsured, but that the protection of public insurance only appears to close the Hispanic, non-Hispanic gap for those with the most severe disabilities. Fourth, we found that despite the fact that overall health service use runs higher among people with disabilities than it does for people without them, there are still many such individuals who go without any annual doctor visit.
The reduction of disparities between the populations of people with and without disabilities will require specific attention to racial and ethnic disparities in health, insurance coverage and service use. Moreover, for researchers, policymakers and providers alike, the reduction of racial/ethnic disparities in health and our healthcare system requires that disability be considered as more than an undesirable health outcome. It is also, and perhaps primarily, a form of human variation around which we can formulate policies and practices that improve health.
Table 1.
Demographics, insurance coverage, health status and service use: Age standardized1 rates on the basis of race/ethnicity among people with and without disabilities, average annual estimates, MEPS 2006-2008.
| Measures | All2 | Without disability | With disability (not affecting ADLs or IADLs) |
With disability (affecting ADLs or IADLs) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Non-Hispanic White |
Non-Hispanic Black |
Hispanic (any race) |
Non-Hispanic White |
Non-Hispanic Black |
Hispanic (any race) |
Non-Hispanic White |
Non-Hispanic Black |
Hispanic (any race) |
||
|
| ||||||||||
| Sample and group sizes | ||||||||||
| N | 63,257 | 24,223 | 7,671 | 12,711 | 6,437 | 1,947 | 1,493 | 2374 | 955 | 703 |
| Population size in millions | 218.84 | 113.90 | 18.65 | 25.07 | 27.27 | 4.14 | 2.92 | 9.40 | 1.87 | 1.26 |
| Percent of analytic group (SE) | n/a | 68.76 (.70) | 10.57 (.44) | 13.91 (.53) | 71.42 (.93) | 12.76 (.64) | 9.87 (.63) | 66.50 (1.59) | 15.97 (1.18) | 10.63 (.88) |
|
| ||||||||||
| Demographics, % (SE): | ||||||||||
| Female | 51.79 (.21) | 49.75 (.31)b | 53.19 (.82)wh | 48.24 (.75)b | 53.92 (1.02)b | 60.60 (1.60)wh | 52.64 (2.04)b | 59.54 (1.96) | 60.03 (3.05) | 54.70 (3.46) |
| < high school ed | 14.99 (.30) | 7.47 (.27) bh | 16.94 (.84)wh | 42.60 (1.08)wb | 13.58 (.68)bh | 25.26 (1.72)wh | 42.69 (1.91)wb | 22.31 (1.66)bh | 40.12 (3.09)wh | 50.13 (3.29)wb |
| <= 125% FPL | 14.75 (.28) | 8.33 (.29) bh | 20.17 (.77)wh | 22.66 (.86)wb | 21.30 (.87)bh | 38.59 (1.80)wh | 31.41 (1.91)wb | 29.09 (1.79)bh | 49.98 (3.03)w | 43.00 (3.31)w |
| Census region: | ||||||||||
| Northeast | 18.59 (.58) | 20.14 (.88)bh | 16.60 (1.19)w | 13.83 (1.10)w | 17.45 (1.05) | 15.94 (1.57) | 16.11 (1.84) | 17.63 (1.68) | 16.89 (3.20) | 15.70 (2.47) |
| Midwest | 21.99 (.65) | 26.30 (.89)bh | 17.06 (1.57)wh | 8.03 (.87)wb | 27.07 (1.26)hb | 20.57 (1.96)wh | 7.25 (1.24)wb | 23.23 (1.92)h | 25.79 (3.31)h | 5.83 (1.69)wb |
| South | 36.41 (.75) | 33.73 (.96)b | 57.59 (2.11)wh | 37.50 (2.35)b | 35.72 (1.56)b | 52.82 (2.60)wh | 38.35 (3.10)b | 36.70 (2.07)b | 47.92 (3.83)wh | 34.64 (3.94)b |
| West | 23.01 (.65) | 19.83 (.80)bh | 8.75 (.99)wh | 40.64 (1.94)wb | 19.75 (1.32)bh | 10.67 (1.49)wh | 38.30 (2.75)wb | 22.43 (1.99)bh | 9.40 (2.31)wh | 43.83 (3.81)wb |
| Resides in MSA | 83.75 (.89) | 81.10 (1.11)bh | 89.51 (1.37)w | 92.82 (1.40)w | 77.90 (1.71)bh | 88.41 (1.61)wh | 93.53 (1.38)wb | 76.01 (2.33)bh | 89.75 (1.79)w | 93.82 (1.68)w |
|
| ||||||||||
|
Beliefs about health care and
insurance, % (se) |
||||||||||
| I can overcome illness without medical help |
22.88 (.27) | 26.18 (.41)bh | 20.49 (.69)w | 19.66 (.72)w | 20.41 (.82)b | 15.90 (1.22)w | 17.16 (1.98) | 10.84 (1.31) | 8.45 (1.57) | 9.93 (1.99) |
| I don’t need health insurance | 11.05 (.23) | 11.30 (.35)h | 11.52 (.56)h | 16.61 (.61)wb | 5.64 (.47)h | 6.31 (.84) | 9.15 (1.33)w | 4.14 (1.02) | 3.61 (.93) | 5.90 (1.57) |
|
| ||||||||||
| Health status, % (se): | ||||||||||
| Overall health fair/poor | 22.12 (.30) | 10.25 (.28)bh | 16.97 (.70)wh | 24.59 (.76)wb | 45.34 (1.11)bh | 56.99 (1.80)w | 60.18 (1.91)w | 68.53 (1.91) | 73.48 (2.72) | 75.12 (2.65) |
| Mental health fair/poor | 12.98 (.23) | 6.48 (.23)h | 7.23 (.45)h | 8.64 (.47)wb | 29.33 (.99)bh | 34.74 (1.65)w | 34.20 (1.75)w | 53.28 (1.93) | 54.71 (3.15) | 60.33 (3.13) |
| BMI >= 30 | 28.14 (.31) | 23.24 (.38)bh | 35.08 (.91)wh | 29.10 (.90)wb | 37.88 (1.02)b | 45.98 (1.63)w | 42.33 (2.31) | 39.23 (1.83) | 43.32 (2.53) | 44.91 (3.32) |
| Physically active >= 3X per wk | 57.50 (.40) | 65.50 (.54)bh | 56.56 (.91)wh | 51.60 (1.07) | 51.43 (1.01)bh | 43.70 (1.70)w | 47.12 (1.93)w | 33.38 (1.62)h | 35.67 (2.97)h | 27.04 (2.75)wb |
|
| ||||||||||
| Insurance coverage, % (se) 3 : | ||||||||||
| Insured all year | 70.35 (.41) | 76.71 (.47)bh | 66.19 (.94)wh | 48.42 (1.05)wb | 66.03 (1.13)h | 64.80 (1.97)h | 57.30 (2.25)wb | 78.81 (1.79) | 72.37 (3.00) | 74.36 (3.07) |
| Any private | 89.69 (.32) | 96.38 (.26)bh | 87.36 (83)w | 87.03 (.88)w | 79.21 (1.25)bh | 55.03 (2.65)wh | 64.70 (2.85)wb | 48.63 (2.66)bh | 22.18 (3.00)w | 29.13 (4.00)w |
| Public only | 10.31 (.32) | 3.62 (.26)bh | 12.64 (.83)w | 12.97 (.76)w | 20.79 (1.25)bh | 44.97 (2.65)wh | 35.30 (2.85)wb | 51.37 (2.66)bh | 77.82 (3.00)w | 70.87 (4.00)w |
| Uninsured part year | 12.06 (.20) | 10.78 (.31)bh | 13.97 (.52)w | 13.82 (.46)w | 14.86 (.85) | 14.04 (1.36) | 16.24 (1.44) | 10.23 (1.14) | 14.19 (2.05) | 11.19 (1.82) |
| Uninsured all year | 17.59 (.34) | 12.51 (.39)bh | 19.83 (.75)wh | 37.77 (1.08)wb | 19.11 (1.05)h | 21.16 (1.72) | 26.47 (2.02)w | 10.96 (1.35) | 13.44 (2.40) | 14.44 (2.45) |
|
| ||||||||||
| Health care service use: | ||||||||||
| Total annual ambulatory visits mean (se) |
6.35 (.07) | 5.57 (.09)bh | 3.22 (.13)w | 3.17 (.11)w | 10.64 (.29)bh | 8.52 (.65)w | 8.50 (.55)w | 17.61 (1.12)bh | 14.00 (.98)w | 13.43 (.95)w |
| No doctor visit during year % (se) |
31.29 (.27) | 30.51 (.36)bh | 40.33 (.78)wh | 44.57 (.82)wb | 17.39 (.79)h | 19.69 (1.53) | 24.63 (1.87)w | 10.60 (1.36) | 13.88 (1.91) | 14.13 (2.05) |
Notes:
With the exception of the findings on health insurance status (see note 3), all results are weighted to represent the U.S., community-dwelling population age 18 and over and are directly standardized by age in approximately ten-year increments.
This column (“All”) represents all adults aged 18 and over regardless of race, ethnicity or disability status.
The findings that regard health insurance status and source are limited to working-age (18-64) individuals. These results are weighted to represent the U.S., community-dwelling population age 18-64 and are directly standardized by age in approximately ten-year increments.
Significance (p<.05) is flagged as follows:
= Differs significantly from the finding for non-Hispanic white persons in the same analytic group
= Differs significantly from the finding for non-Hispanic black persons in the same analytic group
= Differs significantly from the finding for persons of Hispanic ethnicity in the same analytic group
Significance is flagged after adjusting the false discovery rate for the tests of overall health, insurance coverage status, total ambulatory visits, and no doctor visit during the year.
Acknowledgments
Support: NIH Intramural Research Program
REFERENCES
- 1.Pope AM, Tarlov A. Disability in America: Toward a national agenda for prevention. National Academy Press; Washington, DC: 1991. [Google Scholar]
- 2.World Health Organization [Accessed July 1, 2012];The International Classification of Functioning, Disability and Health. 2001 2012, at http://www.who.int/classifications/icf/en/
- 3.Altman BM. Population Survey Measures of Functioning: Strengths and Weaknesses. In: Wunderlich GS, editor. Improving the Measurement of Late-Life Disability in Population Surveys: Beyond ADLs and IADLs. The National Academies Press; Washington, DC: 2009. [PubMed] [Google Scholar]
- 4.Agency for Healthcare Research and Quality . Developing Quality of Care Measures for People with Disabilities: Summary of Expert Meeting. Agency for Healthcare Research and Quality; Rockville, MD: 2010. [Google Scholar]
- 5.Iezzoni LI. Eliminating health and health care disparities among the growing population of people with disabilities. Health affairs. 2011;30:1947–54. doi: 10.1377/hlthaff.2011.0613. [DOI] [PubMed] [Google Scholar]
- 6.Becker H. Measuring health among people with disabilities. Family & community health. 2006;29:70S–7S. doi: 10.1097/00003727-200601001-00011. [DOI] [PubMed] [Google Scholar]
- 7.Reichard A, Stolzle H, Fox MH. Health disparities among adults with physical disabilities or cognitive limitations compared to individuals with no disabilities in the United States. Disability and Health Journal. 2011;4:59–67. doi: 10.1016/j.dhjo.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 8.Chevarley FM, Thierry JM, Gill CJ, Ryerson AB, Nosek MA. Health, preventive health care, and health care access among women with disabilities in the 1994-1995 National Health Interview Survey, Supplement on Disability. Womens Health Issues. 2006;16:297–312. doi: 10.1016/j.whi.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 9.Kinne S, Patrick DL, Doyle DL. Prevalence of secondary conditions among people with disabilities. Am J Public Health. 2004;94:443–5. doi: 10.2105/ajph.94.3.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chirikos TN, Roetzheim RG, McCarthy EP, Iezzoni LI. Cost disparities in lung cancer treatment by disability status, sex, and race. Disability and Health Journal. 2008;1:108–15. doi: 10.1016/j.dhjo.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harrington C, Kang T. Disparities in service utilization and expenditures for individuals with developmental disabilities. Disability and Health Journal. 2008;1:184–95. doi: 10.1016/j.dhjo.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 12.Smith DL. Disparities in health care access for women with disabilities in the United States from the 2006 National Health Interview Survey. Disability and Health Journal. 2008;1:79–88. doi: 10.1016/j.dhjo.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Nosek MA, Howland CA. Breast and cervical cancer screening among women with physical disabilities. Arch Phys Med Rehabil. 1997;78:S39–44. doi: 10.1016/s0003-9993(97)90220-3. [DOI] [PubMed] [Google Scholar]
- 14.Wei W, Findley PA, Sambamoorthi U. Disability and receipt of clinical preventive services among women. Womens Health Issues. 2006;16:286–96. doi: 10.1016/j.whi.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Altman BM. Does Access to Acute Medical Care Imply Access to Preventive Care? Journal of Disability Policy Studies. 1997;8:99–125. [Google Scholar]
- 16.Smith DL. Disparities in patient-physician communication for persons with a disability from the 2006 Medical Expenditure Panel Survey (MEPS) Disability and Health Journal. 2009;2:206–15. doi: 10.1016/j.dhjo.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Gulley SP, Rasch EK, Chan L. Ongoing coverage for ongoing care: access, utilization, and out-of-pocket spending among uninsured working-aged adults with chronic health care needs. American journal of public health. 2011;101:368–75. doi: 10.2105/AJPH.2010.191569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaw SJ, Huebner C, Armin J, Orzech K, Vivian J. The role of culture in health literacy and chronic disease screening and management. Journal of immigrant and minority health / Center for Minority Public Health. 2009;11:460–7. doi: 10.1007/s10903-008-9135-5. [DOI] [PubMed] [Google Scholar]
- 19.Gulley SP, Rasch EK, Chan L. If we build it, who will come? Working-age adults with chronic health care needs and the medical home. Medical care. 2011;49:149–55. doi: 10.1097/MLR.0b013e3182028380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Story MF, Schwier E, Kailes JI. Perspectives of patients with disabilities on the accessibility of medical equipment: Examination tables, imaging equipment, medical chairs, and weight scales. Disability and Health Journal. 2009;2:169–79. doi: 10.1016/j.dhjo.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 21.Morrison EH, George V, Mosqueda L. Primary care for adults with physical disabilities: perceptions from consumer and provider focus groups. Fam Med. 2008;40:645–51. [PubMed] [Google Scholar]
- 22.Grabois EW, Nosek MA, Rossi CD. Accessibility of primary care physicians’ offices for people with disabilities. An analysis of compliance with the Americans With Disabilities Act. Arch Fam Med. 1999;8:44–51. doi: 10.1001/archfami.8.1.44. [DOI] [PubMed] [Google Scholar]
- 23.Drainoni M-L, Lee-Hood E, Tobias C, Bachman SS, Andrew J, Maisels L. Cross-Disability Experiences of Barriers to Health-Care Access. Journal of Disability Policy Studies. 2006;17:101–15. [Google Scholar]
- 24.Krahn GL, Hammond L, Turner A. A cascade of disparities: health and health care access for people with intellectual disabilities. Ment Retard Dev Disabil Res Rev. 2006;12:70–82. doi: 10.1002/mrdd.20098. [DOI] [PubMed] [Google Scholar]
- 25.Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–94. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- 26.Hebert PL, Sisk JE, Howell EA. When does a difference become a disparity? Conceptualizing racial and ethnic disparities in health. Health Aff (Millwood) 2008;27:374–82. doi: 10.1377/hlthaff.27.2.374. [DOI] [PubMed] [Google Scholar]
- 27.Institute of Medicine . Unequal treatment: Confronting racial and ethnic disparities in health care. National Academies Press; Washington, DC: 2002. [PubMed] [Google Scholar]
- 28.Le Cook B, McGuire TG, Zuvekas SH. Measuring trends in racial/ ethnic health care disparities. Med Care Res Rev. 2009;66:23–48. doi: 10.1177/1077558708323607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rasch EK, Gulley SP, Chan L. Use of emergency departments among working age adults with disabilities: a problem of access and service needs. Health services research. 2013;48:1334–58. doi: 10.1111/1475-6773.12025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alecxih L, Shen S, Chan I, Taylor D, Drabek J. Individuals Living in the Community with Chronic Conditions and Functional Limitations: A Closer Look. U.S. Department of Health and Human Services; Washington, DC: 2010. [Google Scholar]
- 31.Gulley SP, Rasch EK, Chan L. The complex web of health: relationships among chronic conditions, disability, and health services. Public health reports. 2011;126:495–507. doi: 10.1177/003335491112600406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Altman BM, Gulley SP. Convergence and divergence: differences in disability prevalence estimates in the United States and Canada based on four health survey instruments. Social science & medicine. 2009;69:543–52. doi: 10.1016/j.socscimed.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 33.Chan L, Ciol MA, Shumway-Cook A, et al. A longitudinal evaluation of persons with disabilities: does a longitudinal definition help define who receives necessary care? Archives of physical medicine and rehabilitation. 2008;89:1023–30. doi: 10.1016/j.apmr.2007.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.The Medical Expenditure Panel Survey [Accessed July 1, 2013];Agency for Healthcare Research and Quality. at http://www.meps.ahrq.gov/mepsweb/
- 35.The Medical Expenditure Panel Survey [Accessed July 1, 2013];Health Status Questionnaire. 2006 2013, at http://meps.ahrq.gov/survey_comp/hc_survey/2006/HE105.pdf.
- 36.The Medical Expenditure Panel Survey [Accessed July 1, 2013];Reeunumeration Questionnaire. 2006 2013, at http://meps.ahrq.gov/survey_comp/hc_survey/2006/REB105.pdf.
- 37.Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the royal statistical society. 1995;57:289–300. [Google Scholar]
- 38. [Accessed July 1, 2013];Household component statistical estimation issues. 2013, at https://apha.confex.com/apha/135am/recordingredirect.cgi/id/18758.
- 39.Weinick RM, Jacobs EA, Stone LC, Ortega AN, Burstin H. Hispanic healthcare disparities: challenging the myth of a monolithic Hispanic population. Med Care. 2004;42:313–20. doi: 10.1097/01.mlr.0000118705.27241.7c. [DOI] [PubMed] [Google Scholar]