Sir,
Since Aflibercept became commercially available, there have been several publications describing favourable early experience, particularly in cases previously refractory to other anti-vascular endothelial growth factor (anti-VEGF) and cases with persistent pigment epithelial detachment (PED).1, 2, 3, 4, 5 However, there is very little clinical experience of Aflibercept in polypoidal choroidal vasculopathy. We present our favourable experience with Aflibercept in the treatment of persistent PED after photodynamic therapy (PDT) combined with Ranibizumab.
Case report
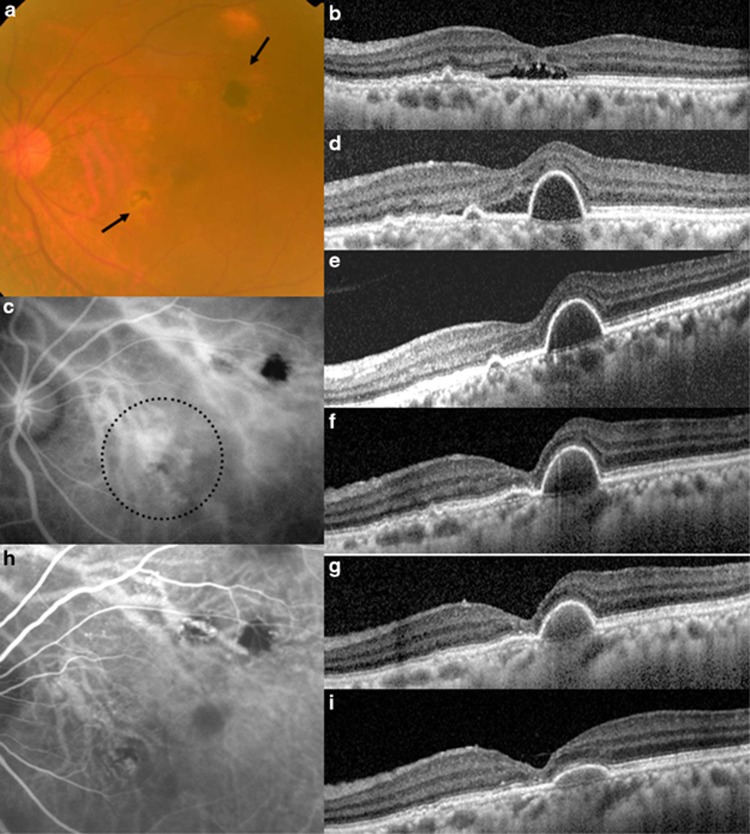
A 64-year-old Chinese lady who first presented with submacular haemorrhage from an extrafoveal PCV in 2010. The lesion was successfully lasered with resolution of blood and vision returned to 6/6. A recurrent episode of subretinal haemorrhage occurred 2 years later, which resolved with focal laser and three intravitreal Ranibizumab injections. Vision recovered from 6/18 to 6/9. In March 2013, recurrent fluid developed, which coincided with vision dropping to 6/15 (Figures 1a and b). A cluster of polyps was seen eminating from the laser scar (Figure 1c). Combination therapy with full fluence PDT, (spot size 3800 μm) and Ranibizumab (0.5 mg) was performed. However, at 1 month review, vision did not improve and a new PED had developed (Figure 1d). A further Ranibizumab injection was given, which resolved the subretinal fluid 1 month later, but the PED persisted (Figure 1e). The patient was acutely aware of distortion, with a visual acuity of 6/12. Aflibercept became available at this time. After the first Aflibercept injection (2 mg), vision remained at 6/12 although patient reported subjective improvement (Figure 1f). Noticeable flattening of the PED was noted after further Aflibercept monthly injections (Figures 1g and i). Repeat angiogram showed significant regression of polyps (Figure 1h). Vision was 6/7.5 at last follow-up.
Figure 1.
(a) The colour fundus photograph shows two areas of previous laser to extrafoveal polyps (arrows). (b) Optical coherence tomography scan through the fovea showed the presence of subretinal fluid. (c) Indocyanine green angiography (ICGA) performed showed a cluster of polyps eminating from the area lasered previously. Intravitreal ranibizumab with Photodynamic therapy was performed using a spot size of 3800 μm (dotted circle). (d) At 1 month review, a new pigment epithelial detachment (PED) had developed, and persistent subretinal fluid was apparent. (e) One month after a further intravitreal ranibizumab injection was given, there was reduction in subretinal fluid, but the PED persisted. (f) One month after first aflibercept injection, foveal contour improved, but PED persisted. (g, i) Progressive flattening of PED was observed after the second and third monthly dosing of aflibercept. (h) Repeat ICGA showed significant regression of the cluster of polyps.
Comment
This case shows promising results of intravitreal Aflibercept in the treatment of PCV refractory to the combination PDT and Ranibizumab. The benefit of initial three monthly loading was clearly demonstrated as significant flattening of the PED only occurred after the second and third injections. The resolution of polyps on ICGA was likely to be due to the combined effect of PDT and anti-VEGF therapy.
The authors declare no conflict of interest.
References
- Yannuzzi LA, Wong DW, Sforzolini BS, Goldbaum M, Tang KC, Spaide RF, et al. Polypoidal choroidal vasculopathy and neovascularized age related macular degeneration. Arch Ophthalmol. 1999;117:1503–1510. doi: 10.1001/archopht.117.11.1503. [DOI] [PubMed] [Google Scholar]
- Chaikitmongkol V, Bressler NM. Dramatic resolution of choroidal neovascular abnormalities after single aflibercept injection following years of ranibizumab use. JAMA Ophthalmol. 2013;131:260–262. doi: 10.1001/jamaophthalmol.2013.1733. [DOI] [PubMed] [Google Scholar]
- Kumar N, Marsiglia M, Mrejen S, Fung AT, Slakter J, Sorenson J, et al. Visual and anatomical outcomes of intravitreal aflibercept in eyes with persistent subfoveal fluid despite previous treatments with ranibizumab in patients with neovascular age-related macular degeneration. Retina. 2013;33:1605–1612. doi: 10.1097/IAE.0b013e31828e8551. [DOI] [PubMed] [Google Scholar]
- Patel KH, Chow CC, Rathod R, Mieler WF, Lim JI, Ulanski LJ, 2nd, et al. Rapid response of retinal pigment epithelial detachments to intravitreal aflibercept in neovascular age-related macular degeneration refractory to bevacizumab and ranibizumab. Eye (Lond) 2013;27:663–667. doi: 10.1038/eye.2013.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonekawa Y, Andreoli C, Miller JB, Loewenstein JI, Sobrin L, Eliott D, et al. Conversion to aflibercept for chronic refractory or recurrent neovascular age-related macular degeneration. Am J Ophthalmol. 2013;156:29–35. doi: 10.1016/j.ajo.2013.03.030. [DOI] [PubMed] [Google Scholar]