Abstract
Objective To evaluate feasibility and preliminary efficacy of an intervention directed at parents of childhood cancer survivors (CCSs) with neurobehavioral late effects to improve targeted parenting skills, and thus to indirectly benefit the child’s educational functioning. Methods 44 CCSs and their parents were randomized. Intervention-arm parents participated in eight individual training sessions augmented by a 3-month telephone support period. Pre- and postparent measures and child performance on Wechsler Individual Achievement Test-II and School Motivation and Learning Strategies Inventory assessed intervention effects. Results 90% of intervention parents completed the program with high adherence/perceived benefit. Between-group effect sizes ranged from d = 0.77 to d = 1.45 for parent knowledge, efficacy, frequency of pro-learning behaviors, and d = 0.21 to d = 0.76 for child academic scores. Parental time spent in intervention activities was associated with academic change. Conclusions A parent-directed intervention to indirectly promote academic functioning in CCSs appears feasible and effective in improving targeted parenting outcomes and for selected child academic outcomes.
Keywords: cancer and oncology, intervention outcome, neuropsychology, parenting, randomized controlled trial, rehabilitation
With recent advances in medical treatment, survival rates for childhood cancer have improved substantially, and the numbers of survivors are increasing (American Cancer Society, 2012). As the population of survivors grows, it is increasingly relevant to consider quality of life and long-term functional outcomes, especially because disease- and treatment-related factors place the children at risk for chronic morbidities, such as neurobehavioral impairments (Landier et al., 2004).
Children treated with central nervous system (CNS)-directed therapy (cranial irradiation and intrathecal chemotherapy) for their cancer are at greater risk for adverse neurocognitive and behavioral outcomes. Adverse neurobehavioral outcomes are most frequently observed in children with malignant brain tumor (treated with brain surgery and cranial irradiation) and acute lymphoblastic leukemia (treated with cranial irradiation and/or intrathecal chemotherapy). Additionally, survivors of acute myeloid leukemia and non-Hodgkin’s lymphoma who received intrathecal chemotherapy, as well as children who received hematopoietic stem cell transplant are also at risk for these adverse effects (Landier et al., 2004). Deficits among these survivors in neurocognitive processes that underlie developmentally appropriate learning, such as attention, executive functioning, memory, and processing speed are well documented in the literature. Such deficits in core functions interfere with age-appropriate acquisition of knowledge so that declines may emerge over time in cognitive and academic achievements (Nathan et al., 2007).
Extensive research has identified and quantified cancer-related neurocognitive dysfunction and its impact on educational and adaptive outcomes; however, intervention studies to treat such sequelae are only emerging now. Preliminary data from pharmacotherapy trials suggest that methylphenidate improves attention and behavioral functioning in survivors, and that these effects are sustained over the course of a year but without academic improvement (Conklin et al., 2010). Recent pilot studies using computerized technology to improve specific cognitive functions in long-term survivors are also encouraging (Kesler, Lacayo, & Jo, 2011; Hardy, Willard, Allen, & Bonner, 2013) but have not yet demonstrated transfer of skills or generalization to other tasks, including academic performance.
Butler et al. (2008) conducted the first randomized clinical trial to evaluate a multimodal cognitive remediation intervention for survivors with a documented attention disturbance (Butler et al., 2008). The study targeted basic neurocognitive processes, mainly attention, and showed small to modest improvements in academic achievement and parent-reported behavioral functioning. However, only 60% of the children in the intervention group completed the prescribed treatment, and the beneficial effects were not sustained long term. Clinic-based cognitive remediation efforts directed primarily at the child may be at risk for short-lived effects due to lack of support in maintaining gains without the therapist. In contrast, parents are potentially tremendous agents of ongoing behavioral “remediation” within the cancer survivor’s natural environment and might be an effective indirect route to influence and sustain adaptive gains over the long term. We proposed to teach and/or strengthen a set of parenting skills, such as behavioral modification techniques, cognitive instructional strategies, and compensatory learning techniques, for the primary purpose of positively impacting the child’s educational outcomes.
Support for such an approach is well documented in the learning disability and educational literature, which demonstrates the importance of parent behaviors and involvement in their child’s education for academic achievement across a wide range of populations and ages (Grolnick & Slowiaczek, 1994; Hill & Taylor, 2004; Miedel & Reynolds, 1999). Parents’ helping or specific “pro-learning” behaviors at home often make the difference between children who do poorly in school and those who do well. These include direct monitoring, instruction, and assistance with schoolwork; parent contact with school/teachers; utilization of resources; direct reinforcement of improved academic performance or effort; promoting developmentally and cognitively stimulating activities at home; and parental affirmation of child’s capacity to learn. (Bradley, Caldwell, & Rock, 1988; Hoover-Dempsey et al., 2001; Switzer, 1990; Van Voorhis, 2003). Recent neuropsychological and brain injury literature also support the role of environmental factors, such as family influences, as critical determinants of the child’s cognitive outcomes after acquired brain injury (Taylor, Yeates, Wade, Drotar, Klein, et al., 1999; Taylor, Yeates, Wade, Drotar, Stancin, et al., 2002; Yeates et al., 1997). Although there is not yet research on parents’ pro-learning behaviors in families who have children with cancer, preliminary findings from our own explorations suggested that selected parenting behaviors may be associated with better cognitive functioning in subgroups of survivors (Patel et al., 2014).
In this report, we present results from a pilot behavioral intervention using a randomized control trial design to (1) determine the feasibility of an educational and skills training intervention for parents of a childhood cancer survivor (CCS) with neurocognitive dysfunction using eight parent–therapist sessions; (2) to evaluate the impact on parents’ level of knowledge and self-efficacy in their ability to promote their child’s school success, along with impact on the frequency of their pro-learning parenting behaviors; and (3) to collect preliminary data on the indirect therapeutic impact of the parent intervention on the child’s adaptive functioning. In particular, we selected objectively assessed academic achievement as an ecologically valid measure of the child’s “real world” functioning. Additionally, our exploratory aims were to assess the impact of the intervention on parent stress and to identify factors that might be associated with child behavior change on study outcomes.
Of note, while parental intervention to promote their child’s learning and educational success was viewed as the mechanism of child behavior change, our primary study outcome was child’s academic performance, as measured by the Wechsler Individual Achievement Test-II (WIAT-II, Wechsler, 2001).
Method
Participants
Eligible participants were CCSs aged 6–18 years and their parents, whose treatment included potentially neurotoxic therapies, including CNS-directed therapy and hematopoietic stem cell transplant. Child participants had to be in remission and at least 6 months posttreatment completion, enrolled in school, have adequate English fluency, no premorbid developmental disorder, and exhibit evidence of existing cognitive difficulties on standardized neuropsychological assessment defined as below 16th percentile performance on at least one neurocognitive domain (e.g., Wechsler processing speed index, working memory index; Children’s Memory Scale Immediate and Delayed Memory scores, etc.). Child participants also needed to exhibit below average performance in at least one academic area based on recent school report grades or parent/teacher report. Survivors of a brain tumor were excluded as the intervention was designed for children with mild to moderate dysfunction.
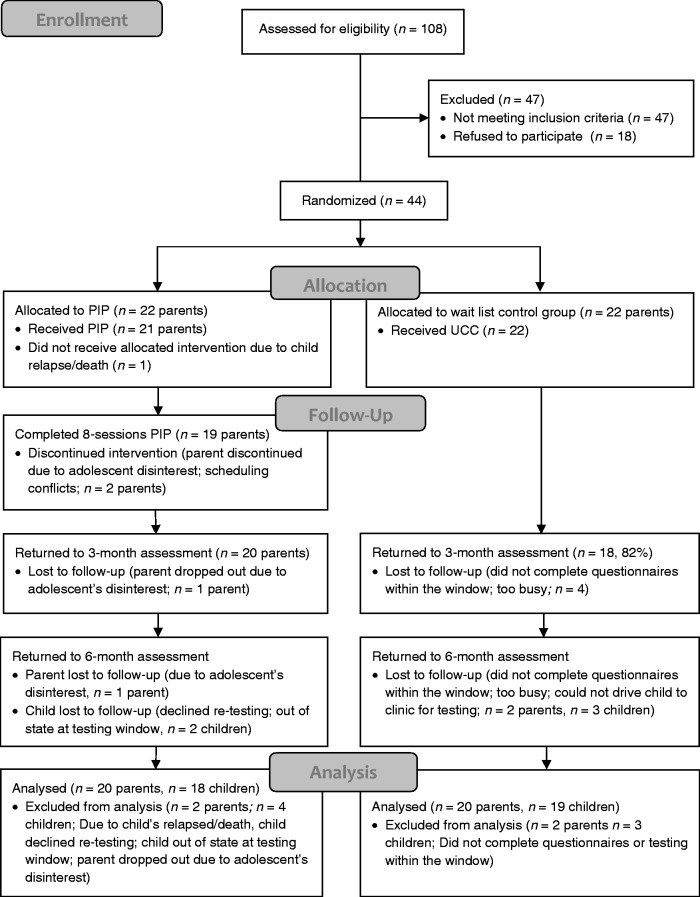
Recruitment consisted of invitation letters mailed to 108 families who were identified from the institutional Childhood Cancer Survivorship and Pediatrics Hematology Oncology programs as meeting initial eligibility criteria. Among the 108 families, the age for 20 children exceeded the eligibility criteria by the time updated contact information was obtained and staff made verbal phone contact. From the remaining 88, 20 (23%) were excluded following phone contact because of parental report of good cognitive and academic functioning in their child; an additional 7 (8%) were excluded because of precancer developmental difficulties. From the remaining 61 eligible families, 43 (71%) consented, the remaining declined because of lack of time and geographic distance. One additional family outside of our institution requested to join the study and was also enrolled (N = 44; Figure 1 illustrates the study flow).
Figure 1.
Parent Intervention Program (PIP) study participant flow.
Procedures
Randomization
Following consent, eligible families were randomized to a study assignment, “Parent Intervention Program” (PIP) or “Wait List Group” (WLG), using a blocked randomization design with block size of four to balance the number of participants in each arm. Twenty-two dyads were allocated to each of the PIP and WLG group.
Design
Parents in the PIP arm underwent a baseline assessment (Time 1), as well as a postintervention assessment after completion of eight training sessions across 3 months (Time 2), and a follow-up assessment, which was an additional 3 months later (Time 3). Essentially, the total duration for study participation was 6 months. Parents in the WLG arm were assessed at matched time intervals but did not receive training sessions until after study completion, although they were encouraged to access standard care services (e.g., school reintegration services). The children themselves underwent brief neuropsychological evaluation at baseline and 6 months later, and they also completed a self-report measure right after the parent intervention (Time 2). All study procedures were approved by the City of Hope institutional review board. Informed consent from the parent(s) and child were obtained in person before baseline measures. A $15 gift card was provided to the participating parent at each assessment point as an appreciation gesture. Pre–post parent and child neuropsychological assessments were conducted by a testing research assistant blinded to study arm, and the intervention therapist was blinded to responses on the study outcome questionnaires.
Intervention Phase 1
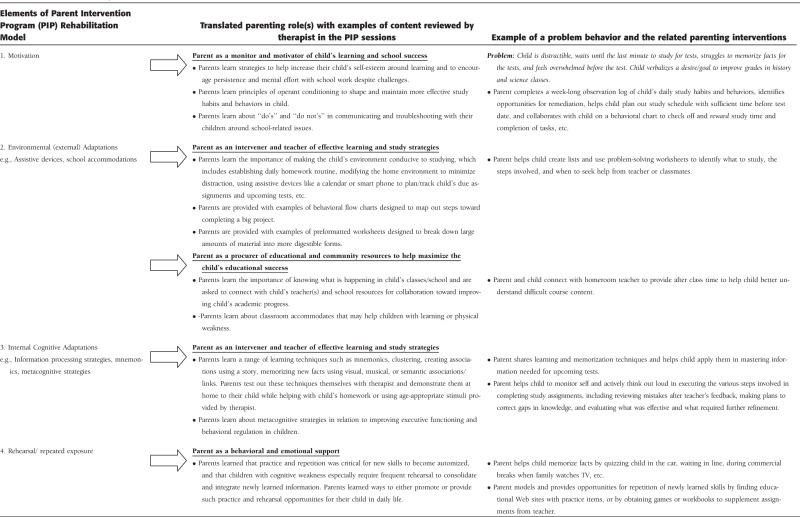
The conceptual model underlying the content and skills taught to parents in our program to apply with their child at home was based on current theoretical approaches in cognitive rehabilitation, where interventions are intended to enhance patterns of effective cognitive activity through (1) external compensatory mechanisms such as environmental structuring and support, (2) the development of internal cognitive compensations for dysfunction, and (3) rehearsal/practice of newly acquired behaviors and strategies (Cicerone et al., 2000; Halligan & Wade, 2005; Solberg and Mateer 2001).
Our intervention model further integrated elements known to promote behavioral change in children. Specifically, children often need help in becoming motivated and mentally engaged toward educational success; require modeling, scaffolding, or coaching toward new behaviors; and may require intermittent monitoring and reinforcement to maintain new habits (Halligan & Wade, 2005; Wilson, Herbet, & Shiel, 2003). To facilitate delivery of the skills by parents in the child’s home environment, we translated these rehabilitative elements into four parenting roles that were targeted in the intervention as follows: (1) parent’s role as a monitor and motivator for school performance; (2) parent’s role as an intervener and “teacher” of effective learning and study strategies, especially when supplementing learning at home is necessary to help the child keep up in class; (3) parent’s role as a procurer of educational and community resources to help maximize the child’s educational success, including services from the school district, the cancer center, community resources, and state/federal parent resources; and (4) parent’s role as a behavioral and emotional support system as the child strives toward learning and educational progress. See Table I for an overview of the intervention components and the associated parenting behaviors within this conceptual model.
Table I.
Overview of Conceptual Model
 |
The intervention consisted of eight parent–therapist training sessions, ∼75–90 min each, using a study manual based on our conceptual model. The same parent was seen for all intervention sessions and assessment points; however, a second parent could join any of the training sessions. Parents themselves tested out many of the learning and memory techniques in clinic with the therapist, such as clustering to memorize a word list and then applied these techniques at home with their child. Using age-appropriate stimuli provided by the therapist for practice, parents also helped the child apply these techniques in daily life (e.g., homework, studying for school tests). See Supplementary Material online for the content of the therapist activities by session. Other than the first and final session, each session was structured to provide information from each of four categories: (1) environmental supports to strengthen child’s study habits and/or strategies to better organize and process academic work, (2) strategies that rely on internal generation of ways to mentally organize information for improved memory, (3) activities and practice drills for child to gain mastery in specific skill, and (4) ways to keep child engaged and motivated for school work.
Implementation
Individualized Goals
In the intervention arm, parents and their child at home collaboratively established goals for program participation (e.g., complete homework assignments on time, obtain better test scores, reduce anxiety-related school absences, etc.) and signed a parent–child agreement before the second session. Parents also kept an observational diary of their child’s study habits and brought this to the therapist for review at the second session. The therapist helped the parent formulate homework goals at each session that the parents were to execute before the next visit. Assignments/parenting goals typically focused on using what was learned in session by applying them at home with their child.
Time Requirement
Parents were required to spend a minimum of 30 min at home with their child using what was learned in training sessions for 4 of the 7-week days. For most families, this was integrated into the daily homework routine, and exercises were mostly applied within the context of schoolwork. For example, planning and organizational strategies might use preparation for an upcoming school test as the stimuli for application of newly learned techniques. Adherence and completion of homework assignments, with problem-solving of any obstacles, were tracked by the therapist at the next session.
Parent–Child Observation
An audio, video, or in-person observation of the parent implementing newly learned tools with their child was conducted after the fourth parent–therapist training session to provide additional feedback to the parent. The majority of parents opted to bring in videos and audiotapes rather than bring the child to clinic for direct observation.
Intervention Phase 2
After the eight sessions and the Time 2 assessment, parents entered Phase 2, where they were to sustain the parent–child goals more independently and continue to help their child generalize the learning techniques. Bi-weekly check-in phone contact was initiated by the therapist to provide support as needed. All parents were given an option for a “booster” PIP session with the therapist if they wished.
Feasibility Measures
Completion. The primary criterion to evaluate feasibility was a 70% completion rate set a priori. In other words, to view the PIP intervention as feasible, 70% of the parents randomized to the intervention arm would need to complete all of the prescribed sessions. This was measured by tracking number of sessions the primary parent completed with the therapist. We also collected adherence and perceived benefit/satisfaction data to examine feasibility.
Adherence: Therapist’s Log and Rating of Parent Adherence. Parents’ report of the amount and frequency of time (minutes and days) spent with their child on PIP-related activities was recorded at each session (post Session 1). Compliance with the specific homework goals established in the previous session was recorded and rated by the PIP therapist at each session (post Session 1) on a 10-point Likert scale. The rating incorporated therapist’s perception of parent’s effort and compliance based on review of homework documents and/or discussion of parent’s behaviors and experiences in applying PIP activities with their child (i.e., “Therapist rating” variable in Table III).
Table III.
Adherence and Perceived Benefit
| Item/scale | M | SD | Response format |
|---|---|---|---|
| Adherence to parent-child Parent Intervention Program (PIP) homework activities across training sessions | |||
| Average daily time spent in PIP activities with child | 30.39 | (8.11) | Minutes |
| Average number of days spent in PIP activities with child | 3.5 | (1.11) | Days |
| Average weekly parent–child effectiveness | 7.00 | (2.00) | 1–10 |
| Therapist rating of parent adherence | 7.42 | (2.81) | 1–10 |
| Parent ratings of program benefit: | |||
| Parents’ weekly rating for perceived child benefit | 7.82 | 1.67 | 1–10 |
| Time 2 (post Phase 1) | |||
| Parent benefit | 4.26a | 0.59 | 1–5 |
| Perceived child benefit | 3.64b | 0.68 | 1–5 |
| Time 3 (post Phase 2) | |||
| Parent benefit | 4.39a | 0.54 | 1–5 |
| Perceived child benefit | 4.00b | 0.73 | 1–5 |
Note. aParent benefit from Time 2 to Time 3 remained stable over time.
bPerceived child benefit increased from Time 2 to Time 3 (p < .01).
Response format: larger values reflect higher adherence or higher perceived benefit.
Parents Self-Report of Adherence. Parents self-reported their adherence with the homework assignments (amount of time spent with child applying PIP activities) and also responded to the following three items at each session (post Session 1): “How much effort do you think you have spent engaging your child in PIP activities since the last session,” “How effective do you think you were,” and “How cooperative/responsive was your child during your PIP activities,” rated on a scale ranging from 1 (A Little) to 10 (A Lot). Cronbach’s alpha for these three items was .67 (i.e., average weekly “Parent–child effectiveness” variable in Table III). Responses to these survey items were used to facilitate discussion and problem-solving of obstacles at each session, such as managing time with other children in the home and how to keep the child motivated for the program activities.
Perceived Benefit/Satisfaction. Parents rated their experience and perception of the program at Time 2 and Time 3 on a 5-point scale. The items included: “My ability to work on learning and academics with my child has improved,” “I feel better prepared to help my child more because of my participation in this program,” and “I feel that my time spent in this program is worthwhile.” Cronbach’s alpha for these items at Time 2 and Time 3 were α = .90 and α = .85, respectively (i.e., “Parent benefit” variable in Table III).
Perceived Child Benefit. Additionally, parents were asked to rate at each session (post Session 1) how helpful they thought the parent–child homework activities were to the child (i.e., a single item assessing weekly perceived child benefit), and they also rated overall perceived child benefit at Time 2 and Time 3 using the following two items: “My child has improved because of our participation in this program” (e.g., doing better on math, spelling, or reading tests, understanding/completing homework assignments) and “My child’s behavior and motivation toward learning and schoolwork has improved because of our participation in the program.” Cronbach’s alpha for these two items at Time 2 and Time 3 were α = .73 and α = .70, respectively (i.e., “Perceived child benefit” variable in Table III).
Parent Outcome Measures
The Parent Beliefs and Behaviors Questionnaire-second revision is an adapted version of a parent-report measure developed by our group specifically to assess parental beliefs and knowledge about cancer-related cognitive late effects and to measure parents’ participation in pro-learning behaviors that are conceptually and empirically associated with cognitive and academic promotion for children. Items for the original questionnaire were derived from existing frameworks of parent involvement, and basic psychometrics were first obtained using a community sample of 121 parents with healthy children (Verner, 2005). A revised version with additional subscales, including parent efficacy, was then piloted with 56 parents of CCSs at risk for cognitive dysfunction due to CNS-directed therapies (Patel et al, 2014). The questionnaire items were modified for the present study to measure the impact on three factors: knowledge, efficacy, and behaviors. The Knowledge scale consists of 19 items (Cronbach’s α = .94), which evaluate the caregiver’s knowledge of specific learning techniques and strategies, behavioral modification principals, and general factors that help with positive school achievement, for example, “how much do you know about study strategies that may help your child with academic skills?” The Efficacy scale consists of nine items (Cronbach’s α = .91), which evaluate the caregiver’s belief in their personal ability to help their child with learning and school, for example, “I am able to help my child learn,” “I feel successful in my efforts to help my child learn,” and “I have enough time and energy to supervise my child’s homework.” Items are rated on a 5-point Likert scale ranging from 1 (A Little) to 5 (A Lot). The Pro-learning Behaviors scale consists of 40 items (Cronbach’s α = .86), which assess the frequency of parental participation in specific pro-learning behaviors, such as monitoring and helping with homework, building their child’s cognitive skills, and having contact with their child’s teachers. Parents were asked to rate how often they participated in a list of behaviors and activities on a 5-point scale ranging from 1 (Never) to 5 (Daily) or from 1 (Never) to 5 (7 or more times a year). Sample items include the following: “ask your child about his/her homework,” “reward your child for improved or good school grades,” “ask school personnel about ways to supplement what is learned at school in the home,” “encourage your child to play with computer programs or games to help with academic and cognitive skills,” “check to make sure your child’s homework is completed,” and “discuss with your child his or her academic progress.”
Parent Stress Index-Short Form (Abidin, 1995), a standardized self-report questionnaire was used to evaluate the impact on parent stress. Parents respond to statements on a 5-point Likert scale ranging from 1 (Strongly Agree) to 5 (Strongly Disagree), to generate a total parent stress score.
Child Outcomes Measures
Wechsler Individual Achievement Test-II (WIAT-II; Wechsler, 2001), a nationally standardized objective measure was used to assess impact on the child’s academic functioning. The a priori primary measures for child outcomes were the WIAT math and reading composite scores. Math subtests assessed include the following: The Numerical Operations subtest measures the ability to solve written calculation problems and simple equations involving all basic operations (addition, subtraction, multiplication, and division). The Math Reasoning subtest assesses the ability to reason mathematically, for example, word problems, interpret graphs, identify mathematical patterns, and solve problems related to statistics and probability. The Reading subtests include the Word Reading subtest, which assesses phonological awareness and decoding skills (e.g., reading letters to complex words); the Reading Comprehension subtest involves reading sentences or paragraphs and then responding to questions; and the Pseudoword Decoding subtest assesses the ability to apply phonetic decoding skills, for example, reading aloud a list of nonsense words. The WIAT was administered to the child in the clinic at baseline and again 6 months later.
School Motivation and Learning Strategies Inventory (Stroud & Reynolds, 2006). The School Motivation and Learning Strategies Inventory (SMALSI) is a self-report inventory for ages 8–18 years, which assesses constructs related to learning strategies, academic motivation, test-taking strategies, and test anxiety. Items are rated on a 4-point Likert scale with Cronbach’s α > .75. The SMALSI subtests of Low Academic Motivation, Study Strategies, and Test Anxiety cross the different age versions of this survey and were used to evaluate child impact. Children completed this questionnaire at three time points: At baseline and Time 3, this questionnaire was completed when the child came to clinic for the performance testing, while for Time 2, it was mailed to the child to complete and return in a sealed envelope.
The Behavior Rating Inventory of Executive Function (BRIEF). Parent and Teacher report questionnaire (Gioia, Isquith, Guy, & Kenworthy, 2000) assesses the child’s executive functioning in daily life on a 3-point Likert scale. Cronbach’s α ranged from .80 to .98.
Medical and Clinical Information. Medical records were reviewed, and cancer treatment for each child was assigned to one of four operationally defined categories of treatment intensity using the Intensity of Treatment Rating scale-second edition (ITR-2) (Werba et al., 2007). The ITR-2 has significant agreement between criterion ratings (r = .95) and has high interrater reliability (r = .87).
Statistical Analysis
Descriptive statistics and repeated measure analysis of variance (ANOVA) were used to examine sample characteristics at baseline and feasibility indicators across time (completion, adherence, perceived benefit, etc.). Generalized estimating equation (GEE) was used to examine longitudinal change on outcomes with three assessment points, with the primary focus on differences in the slope of change between the PIP and WLG arms from Time 1 (baseline) to Time 2 and from Time 1 to Time 3. Distribution of responses on the parent knowledge, efficacy, and pro-learning behaviors was skewed and was normalized with log transformation before GEE analyses. Compound symmetry was assumed for the covariance matrix. Analysis of covariance (ANCOVA) was used to examine longitudinal change for outcomes with two assessment points using pre–post difference scores, controlling for any statistically significant differences between groups on outcomes that existed at baseline. Key conceptual covariates such as child gender, child age, time since diagnosis, age at diagnosis, cancer diagnosis/treatment, primary parent’s education, marital status, and household size were assessed for significant effects between groups and/or on outcomes before constructing analytical models. Any such significant variables were controlled as covariates in the models that examined change between study arms as relevant. Alpha was set at p < .05 for statistical significance. Given the small sample size with limited power to detect statistical significance, the potential impact of the intervention on the primary study outcomes was also assessed using effect sizes of differences in change between the study arms. Exploratory analyses examined correlates of child change on academic performance in the intervention group, and also explored correlates of parent change. Analyses were done using SPSS 21 and SAS 9.3.
Results
Sample Characteristics
Mothers made up the majority of participating parents (86.36%; n = 38). A large proportion of the sample was White, including Hispanic Americans (57%) and Anglo Americans (23%), and was married (70%). Some parents worked full time (42%), while the remaining worked part time (27%), attended school (12%), and were homemakers (18%). Of the 44 children, 21 (48%) were male. The average age at diagnosis was 4.91 years (SD = 3.64, range = 0.08–14.83), and age at study participation was 11.92 (SD = 3.28, range = 6–17 years).
The two arms were not significantly different with respect to age at study, age at diagnosis, time since diagnosis, parent education, or cancer diagnosis (ALL vs. non-ALL) and treatment intensity (based on ITR2 ratings). See Table II.
Table II.
Demographic and Clinical Characteristics
| Wait list group (WLG) (N = 22) |
Parent Intervention Program (PIP) (N = 22) |
|||
|---|---|---|---|---|
| Variable | n | % | n | % |
| Child’s age (months)a,b | 144.18 (38.85) | 141.95 (40.71) | ||
| Child’s age at diagnosis (months)a,c | 61.45 (46.44) | 56.41 (41.61) | ||
| Genderd | ||||
| Male | 10 | 45.45 | 11 | 50.00 |
| Female | 12 | 54.55 | 11 | 50.00 |
| Ethnicitye | ||||
| Latina/Hispanic | 16 | 72.73 | 14 | 63.64 |
| Not Latina/Hispanic | 6 | 27.27 | 8 | 36.36 |
| Type of diagnosisf | ||||
| Acute lymphoblastic leukemia | 17 | 77.27 | 14 | 63.64 |
| Non-Acute lymphoblastic leukemia | 5 | 22.73 | 8 | 36.36 |
| Acute myeloid leukemia | 2 | 9.09 | 4 | 18.18 |
| Non-Hodgkin’s lymphoma/lymphoblastic lymphoma | 2 | 9.09 | 2 | 9.09 |
| Other | 1 | 4.55 | 2 | 9.09 |
| Time since diagnosis (months)a,g | 82.73 (41.15) | 85.55 (40.37) | ||
| Treatment | ||||
| Surgery | 1 | 4.55 | 2 | 9.09 |
| Chemotherapy | 22 | 100.00 | 21 | 95.45 |
| Radiation | 9 | 40.91 | 10 | 45.45 |
| Hematopoietic stem cell transplant | 8 | 36.36 | 9 | 40.91 |
| Intensity of Treatment Rating scale 2.0 | ||||
| Moderately intensive | 8 | 36.36 | 8 | 36.36 |
| Very intensive | 5 | 22.73 | 4 | 18.18 |
| Most intensive | 9 | 40.91 | 10 | 45.45 |
| Primary parent participanth | ||||
| Mother | 20 | 90.91 | 20 | 90.91 |
| Father | 2 | 9.09 | 2 | 9.09 |
| Primary parent age (years)a,i | 40.82 (11.05) | 42.09 (8.26) | ||
| Primary parent participant’s educationj | ||||
| Less than or high school graduate | 7 | 31.82 | 7 | 31.82 |
| Some college | 8 | 36.36 | 8 | 36.36 |
| College graduate or postgraduate | 7 | 31.82 | 7 | 31.82 |
Note. aMean (SD).
The two arms were not significantly different with respect to: bChild’s age, t(42) = −0.19, p = .854, cage of diagnosis, t(42) = −0.38, p = .706, dgender, χ2 = 0.09, p = .763, eethnicity, χ2 = 0.42, p = .517, ftype of diagnosis, χ2 = 0.98, p = .322, gtime since diagnosis, t(42) = 0.23, p = .820, hprimary parent participant, χ2 < .001, p = 1.00, iprimary parent participant’s age, t(42) = 0.433, p = .667, and jparent education, χ2 < .001, p = 1.00.
Intervention Feasibility
Retention and Completion. Of the 22 families randomized to the intervention arm, one child was withdrawn due to cancer relapse, leaving 21 families. Of the 21 intervention families, 19 (90%) completed the intervention, which exceeded the a priori 70% criterion set for feasibility.
Parent Adherence and Perceived Benefit. Based on data collected at each session, parents were able to adhere to PIP homework requirement of 30 min a day (M = 30.39, SD = 1.67) for 4 days a week (M = 3.50, SD = 1.11). See Table III for data on parent adherence and perceived benefit of the program to themselves and for their child. Repeated measure ANOVA results indicated that perceived parent benefit remained stable over time, F(1,19) = 3.67, p = .07, whereas perceived child benefit increased from Time 2 to Time 3, F(1, 19) = 12.25, p < .01). Of note, during Phase 2, 13 parents (62%) requested a “booster” session with the therapist.
Impact on Parent Outcomes
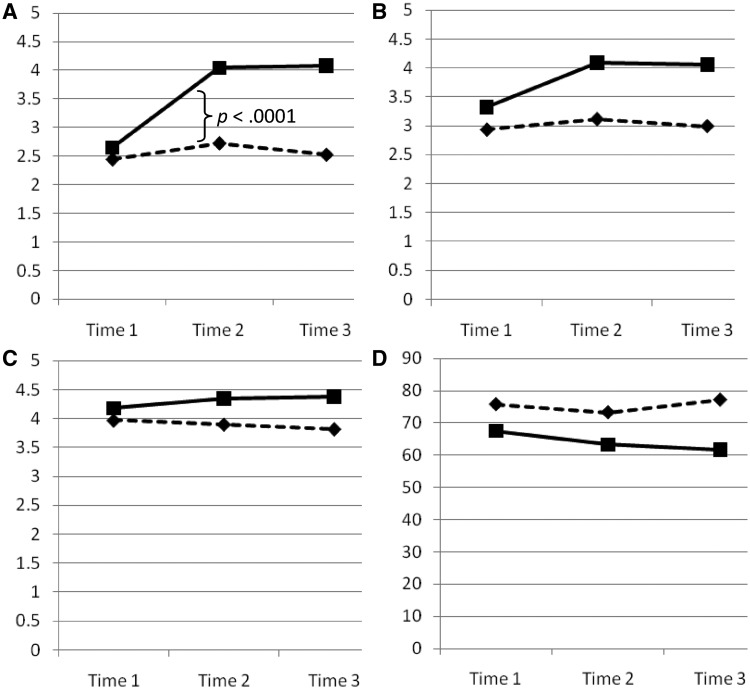
Parent Knowledge. There was a large effect size (d = 1.45) (Cohen, 1988) for group differences in the slope of longitudinal change in parent knowledge from baseline to Time 2, with greater increase in the intervention group (p < .0001). See Table IV and Figure 2. This increase was sustained 3 months later, as the slope of change from baseline to Time 3 between groups remained different (p < .0001).
Table IV.
Comparison of Group Differences, Effect Sizes, and Generalized Estimating Equation Results for Parent-Reported Outcomes
| Wait list group (WLG) |
Parent Intervention Program (PIP) |
WLG vs. PIP slope differences |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictors | n | M | SD | Change in M | n | M | SD | Change in M | Effect size | z | p |
| Parent knowledge | |||||||||||
| T1 | 22 | 2.44 | 0.83 | 22 | 2.65 | 0.74 | |||||
| T2 | 22 | 2.74 | 0.84 | T2 − T1 = +0.30 | 20 | 4.04 | 0.74 | T2 − T1 = +1.39 | T2 − T1 = 1.45 | 4.81 | <.0001*** |
| T3 | 20 | 2.52 | 0.77 | T3 − T1 = +0.08 | 20 | 4.08 | 0.72 | T3 − T1 = +1.43 | T3 − T1 = 1.49 | 4.94 | <.0001*** |
| Parent efficacy | |||||||||||
| T1 | 22 | 2.93 | 1.06 | 22 | 3.32 | 0.75 | |||||
| T2 | 22 | 3.11 | 1.09 | T2 − T1 = +0.18 | 20 | 4.09 | 0.85 | T2 − T1 = +0.77 | T2 − T1 = 0.71 | 2.33 | .020* |
| T3 | 20 | 2.99 | 1.05 | T3 − T1 = +0.06 | 20 | 4.06 | 0.64 | T3 − T1 = +0.74 | T3 − T1 = 0.70 | 2.33 | .020* |
| Pro-learning parenting behaviors | |||||||||||
| T1 | 22 | 3.97 | 0.62 | 22 | 4.18 | 0.53 | |||||
| T2 | 20 | 3.90 | 0.74 | T2 − T1 = −0.07 | 20 | 4.35 | 0.48 | T2 − T1 = +0.17 | T2 − T1 = 0.79 | 2.60 | .0094** |
| T3 | 20 | 3.82 | 0.82 | T3 − T1 = −0.15 | 20 | 4.06 | 0.64 | T3 − T1 = −0.12 | T3 − T1 = 0.71 | 2.33 | .020* |
| Parent stress | |||||||||||
| T1 | 21 | 75.76 | 16.04 | 22 | 67.50 | 26.22 | |||||
| T2 | 16 | 73.25 | 18.68 | T2 − T1 = −2.51 | 18 | 63.28 | 20.66 | T2 − T1 = −4.22 | T2 − T1 = −0.10 | −0.31 | .76 |
| T3 | 19 | 77.16 | 24.97 | T3 − T1 = +1.40 | 19 | 61.58 | 21.96 | T3 − T1 = −5.92 | T3 − T1 = −0.47 | −1.53 | .13 |
Note. T1 = baseline; T2 = postintervention (3 months postbaseline); T3 = 3 months postintervention (6 months postbaseline). M = mean. SD = standard deviation. Change in M = change in unadjusted mean between Time 1 to Time 2 (or Time 1 to Time 3). Higher scores indicate better outcomes for parent knowledge, parent efficacy, and pro-learning parenting behaviors. Lower parent stress scores indicate less stress. *p < .05. **p < .01. ***p < .001.
WLG vs. PIP slope differences = the rate of change in outcome between Time 1 to Time 2 (or from Time 1 to Time 3) between groups. Effect size = Cohen’s d. Difference between the change in Time 1 to Time 2 (or Time 1 to Time 3) between WLG and PIP, divided by the pooled standard deviation (value of 0.2 = small, 0.5 = medium, and 0.8 = large effect size).
Figure 2.
Graphs with plotted means representing longitudinal trajectories for (A) parent’s knowledge, (B) parent’s efficacy, (C) pro-learning parenting behaviors, and (D) parent stress for the PIP (solid squares) and wait list groups (dashed diamonds). See Table IV for p-values and data. Note: Time 1 = baseline, Time 2 = posttreatment, and Time 3 = 3 months after intervention. Lower scores represent better functioning for parent stress measure only.
Parent Efficacy. There was a medium to large effect size (d = .77) for group differences in the slope of longitudinal change in parent efficacy from baseline to Time 2, with higher increase in the intervention group. This increase was sustained 3 months later, as the slope of change from baseline to Time 3 between the two groups remained different (p < .0001). Given its significant association with parent efficacy where parents of younger children reported higher self-efficacy, child age was accounted for as a covariate in the aforementioned between-group analyses.
Pro-Learning Parenting Behaviors. There was a medium to large effect size (d = .79) for group differences in the slope of longitudinal change from baseline to Time 2 in frequency of pro-learning parenting behaviors, with greater increase in the intervention group. This increase was sustained 3 months later, as the slope of change from baseline to Time 3 remained different (p < .001). Child age was accounted for as a covariate in the between-group analyses, as it was associated with parent behaviors in the entire sample, such that parents of younger children tended to have greater change (increase) in frequency of pro-learning behaviors.
Parent Stress. There was negligible effect of the intervention in slope of change between groups in parent stress from baseline to Time 2. However, there was a small to medium effect (d = −.47) in change from baseline to Time 3, such that parents in the intervention group reported lowered stress relative to the control group 3 months after training sessions.
Impact on Child Outcomes
The means and standard deviations of child scores on academic achievement are presented in Table V across the two time points assessed, along with a column for unadjusted pre–post change in standardized scores. Because scores on two WIAT-II subtests (Numerical Operations and Reading Comprehension) were significantly different at baseline between arms, the analyses examining pre–post change between arms adjusted for baseline values of these outcomes. Male child gender, higher parent education, married status for parent, and larger household size were associated with more positive change on child’s academic scores for the entire sample for at least one WIAT-II score and so were included as covariates in examining differences in change between the two arms.
Table V.
Comparison of Group Differences, Effect Sizes, and Results of Analysis of Covariance (ANCOVA) Examining Change Scores for Child Academic Achievement
| Wait list group (WLG) |
Parent Intervention Program (PIP) |
T1 to T3 change (WLG vs. PIP) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| WIAT-II | n | M | SD | Change in M | n | M | SD | Change in M | Effect size | F | p |
| Mathematic composite | |||||||||||
| T1 | 22 | 91.32 | 18.64 | 21 | 84.14 | 15.36 | |||||
| T3 | 19 | 93.26 | 22.99 | T3 − T1 = +1.94 | 18 | 92.28 | 20.36 | T3 − T1 = +8.13 | 0.70 | 3.55 | 0.070† |
| Numerical operations | |||||||||||
| T1 | 22 | 101.05 | 18.12 | 22 | 86.73 | 14.05 | |||||
| T3 | 19 | 99.37 | 18.78 | T3 − T1 = −1.68 | 18 | 97.56 | 18.24 | T3 − T1 = +10.83 | 0.76 | 4.45 | 0.043* |
| Math reasoning | |||||||||||
| T1 | 22 | 84.18 | 16.99 | 21 | 85.33 | 15.37 | |||||
| T3 | 19 | 87.32 | 20.06 | T3 − T1 = +3.13 | 18 | 89.00 | 19.24 | T3 − T1 = +3.67 | 0.09 | 0.07 | 0.790 |
| Reading composite | |||||||||||
| T1 | 22 | 91.36 | 15.32 | 21 | 96.10 | 10.05 | |||||
| T3 | 19 | 92.89 | 14.06 | T3 − T1 = +1.53 | 17 | 100.35 | 14.86 | T3 − T1 = +4.26 | 0.31 | 0.72 | 0.404 |
| Word reading | |||||||||||
| T1 | 22 | 93.27 | 15.40 | 22 | 96.82 | 10.02 | |||||
| T3 | 19 | 96.11 | 16.71 | T3 − T1 = +2.83 | 18 | 98.94 | 13.93 | T3 − T1 = +2.13 | 0.23 | 0.42 | 0.520 |
| Reading comprehension | |||||||||||
| T1 | 22 | 90.55 | 18.12 | 21 | 100.52 | 11.57 | |||||
| T3 | 19 | 91.95 | 13.87 | T3 − T1 = +1.40 | 17 | 104.59 | 14.71 | T3 − T1 = +4.06 | 0.72 | 3.87 | 0.059† |
| Pseudoword decoding | |||||||||||
| T1 | 22 | 96.91 | 12.89 | 22 | 95.32 | 10.51 | |||||
| T3 | 19 | 97.11 | 12.61 | T3 − T1 = +0.20 | 18 | 98.06 | 12.85 | T3 − T1 = +2.74 | 0.21 | 0.37 | 0.548 |
Note. WIAT-II = Wechsler Individual Achievement Test-II. T1 = baseline; T3 = 3 months postintervention (6 months postbaseline). M = mean scores presented as standardized scores where M = 100, and SD = 15. Higher scores indicate better performance. Change in M = change in unadjusted mean scores between Time 1 to Time 3.
Effect size = Cohen’s d calculated based on partial-eta squared, comparing the change in performance from Time 1 to Time 3 between groups (effect size value of 0.2 = small, 0.5 = medium, 0.8 = large; Cohen, 1988). The p-value indicates the level of significance in change scores between groups after controlling for covariates. †p < .10. *p < .05.
Tests of Academic Achievement. Adjusted for the aforementioned covariates, there was a medium to large effect size (d = .70) for group differences in the degree of change from baseline to 6 months on the WIAT-II Math Composite score, with higher gains among children in the intervention arm. Group differences controlling for covariates approached statistical significance (p = .070). No significant between-group difference was observed for WIAT-II Reading Composite score, although the estimated effect size (d = .31) was in the small to medium range. With respect to individual subtests, both Numerical Operations and Reading Comprehension showed medium to large effect sizes with higher gains in the intervention arm (d = .76 and d = .72, respectively); group differences after controlling for covariates were significant for numerical operations (p = .043) and approached statistical significance for the reading comprehension subtest (p = .059). Effect sizes for the remaining subtests were small and less than small (d = .09) for the Math Reasoning subtest. See Table V.
School Motivation and Learning Strategy. There was a medium to large effect size (d = .77) for group differences in the slope of longitudinal change in use of study strategies from baseline to Time 2, with greater increase in the intervention group (p = .03). This was not evident 3 months later, and the effect size was very small (d = −.07) in change from baseline to Time 3. There were no significant differences and/or very small effect sizes (d = <.20) on the other SMALI subscales.
Parent and Teacher Report of Child Executive Functioning. There were no statistically significant changes on the parent report BRIEF scores from baseline to repeated assessments in either arm. For the Teacher BRIEF, only six teachers mailed back completed questionnaires at postintervention and so was excluded from analyses.
Exploratory Analyses: Correlates of Child’s Academic Change in Intervention Group. There were a significant correlation between quantity of time the intervention-group parents spent with their child in PIP activities at home and pre–post change in child’s academic performance, such that more time spent was associated with greater change on the WIAT-II Reading Comprehension score (r = .75; p = .001). Having more people in the home was associated with higher change in the Math Composite score (r = .65; p = .005). Gender showed trends or had significant associations such that male children tended to have higher pre–post intervention change on both the WIAT-II Math and Reading Composite scores(r = −.39; p = .02; r = −.27; p = .10, respectively).
Child Correlates of Parenting Change in Intervention Group. Child gender, child’s age, and time since diagnosis were not significantly associated with the amount of time parents spent with their child in PIP activities. Although child’s age was significantly associated with change in parents’ pro-learning behaviors in the entire sample (r = −.30; p = .05) with parents of younger children having greater change, the association was not significant when examined within the intervention arm sample alone.
Discussion
The purpose of this randomized pilot study was to evaluate feasibility and preliminary efficacy of a behavioral intervention directed at parents of CCSs with neurobehavioral late effects for the purpose of improving parent knowledge, efficacy, and frequency of pro-learning parenting behaviors on behalf of their child, and thus to indirectly improve the child’s educational functioning. As 90% of the parents in the intervention arm completed the prescribed program with good adherence and high perceived benefit ratings, the parent-directed intervention was deemed feasible. Our aim to increase parents’ level of knowledge and self-efficacy in their ability to promote their child’s school success, along with impact on the frequency of their pro-learning parenting behaviors, was met as parents in the intervention significantly changed on these outcomes, whereas those in the control arm did not.
Study results partially supported the exploratory aim to positively impact parent stress as intervention-arm parents had reduced stress at the final assessment relative to those in the control arm. The intervention was not designed to directly address parenting stress; however, we speculated that parents would experience reduced stress if they were given skills to help their child manage learning struggles. Of note, parents’ ratings in perceived benefit of the intervention program for their child’s functioning increased even more at the follow-up period and may have contributed toward the finding of lowered parenting stress at Time 3 but not at Time 2.
With respect to our aim to collect preliminary data on the indirect therapeutic impact of the parent intervention on the child’s adaptive functioning, we found modest support in the form of medium effect sizes for group differences in pre–post change on the WIAT composite scores, mostly driven by change on the Reading Comprehension and Numerical Operations subtests, with higher gains in the intervention arm.
Other data to support beneficial impact on child outcomes were observed in child-reported use of study strategies. Specifically, children in the intervention significantly increased in their use of study strategies (“I use a plan to remember things for tests,” “When I study, I make a study sheet with important things to remember,” etc.) at Time 2. However, this effect was not sustained at Time 3. It is possible that the children used newly learned strategies only for the short term and did not integrate them well enough to become “habits” that could be maintained over time. We further speculate that although parents were effective in introducing their children to the study strategies, they may not have sufficiently monitored ongoing use of these strategies during Phase 2.
With respect to parent report of behavioral functioning in daily life, we did not observe notable gains on the BRIEF. This was surprising, given the consistently positive qualitative feedback from the parents in the intervention arm of improved child scores on tests, quizzes, and homework assignments. The intervention might have positively impacted performance on very specific daily tasks, such as those in academic setting, rather than the general executive functioning skills measured by the BRIEF. We hoped to also evaluate pre–post teacher ratings; however, it was logistically difficult to obtain both baseline and follow-up measures from the same set of teachers. We were successful in obtaining official school grades at baseline because the parents brought in report cards, but we did not request postintervention report cards, although this might be a good ecologically valid measure of child outcome for future studies.
Findings from our exploratory analyses to examine correlates of child change on academic tests in the intervention group showed a significant association between the quantity of time parents spent with their child in PIP activities at home and pre–post change in child’s academic performance, such that more time spent was associated with greater change on WIAT-II Reading Comprehension score. Male gender and having more people in the home was associated with higher change in the Math Composite score within the intervention group.
While these associations should be viewed with caution given the small sample size, multiple tests of significance, and increased probability of type-one error, they serve as hypothesis generating for future research, as do other results from this pilot study. On the whole, these associations suggest that intervention-related impact may vary based on family and child characteristics. We observed that higher parent education, married parent, and larger household size were associated with more positive change in child academic scores in general for the overall sample, suggesting that children from families with fewer resources particularly should be targeted for future intervention research. The feasibility and utility of a parent-directed intervention for children from lower socioeconomic backgrounds should be considered for future research.
Overall, we view the modest effects in child outcomes observed in this study by targeting the parenting skills and behaviors as promising but in need of further development. Over 50% of the intervention parents accepted the option for an additional “booster” session during Phase 2, suggesting they wanted additional support after the core intervention was over. Although eight training sessions were sufficient to modestly impact some of our study outcomes, we suspect many parents would require ongoing support for a longer time to sustain their efforts and impact on the child’s progress in educational activities. Parents of younger children across the sample tended to have higher change in pro-learning behaviors, and it is likely that parents would require more assistance as children advance into higher grade levels. There is the possibility of parent–child conflict among some adolescents if parents are perceived as excessively directive and overly involved in the child’s school work. In our sample, we had one parent who dropped out of the intervention at his adolescent son’s request who reportedly did not want his father engaged in school-related issues with him. Future research will need to track parent and child adherence over the long term to assess our rationale that parents can function as interventionists, or at the least “educational coaches” to positively impact educational success over the long term.
Future research directions might also include a design with intervention directed at the parents but also incorporate more direct involvement with the child, as this may yield increased and/or sustained positive impact on child’s outcomes. We also recommend more extended support to parents in helping to maintain adequate adherence to intervention-related activities over the long term. We strongly recommend inclusion of measures that better capture the small successes parents described in Phase1, such as improved performances on weekly quizzes and completed assignments. These types of experiences may not translate into noticeable gains on measures such as the WIAT-II academic tests but are still meaningful and perhaps reflect the “seeds” for gains over the long term. Our intervention was designed for children with small to moderate deficits, yet even within this restricted range, it will be important to identify the characteristics of the subgroups for which this type of family-based intervention approach is helpful versus those for whom there is no benefit. Additionally, for future directions, we recommend developing interactive Web-based versions of similar intervention programs so that families who reside in remote geographical locations or those who are too busy to travel to the clinic can also access services.
Supplementary Data
Supplementary data can be found at: http://www.jpepsy.oxfordjournals.org/.
Funding
This project was supported by the National Cancer Institute at the National Institutes of Health (Grant number: R03 CA130731 to S.P.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Conflicts of interest: None declared.
Supplementary Material
References
- Abidin R R. Manual for the parenting stress index: Short form. 3rd ed. Odessa, FL: Psychological Assessment Resources, Inc; 1995. [Google Scholar]
- American Cancer Society. Cancer facts and figures. 2012. American Cancer Society. Retrieved from http://www.cancer.org/research/cancerfactsfigures/cancerfactsfigures/cancer-facts-figures-2012. [Google Scholar]
- Bradley R H, Caldwell B M, Rock S L. Home environmental and school performance: A ten-year follow-up and examination of three models of environmental action. Child Development. 1988;59:852–867. doi: 10.1111/j.1467-8624.1988.tb03239.x. doi:10.2307/1130253. [DOI] [PubMed] [Google Scholar]
- Butler R W, Copeland D R, Fairclough D L, Mulhern R K, Katz E R, Kazak A E, Noll R B, Patel S K, Olle J Z. A multicenter, randomized clinical trial of a cognitive remediation program for childhood survivors of a pediatric malignancy. Journal of Consulting and Clinical Psychology. 2008;76:367–378. doi: 10.1037/0022-006X.76.3.367. doi:10.1037/0022-006X.76.3.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicerone K D, Dahlberg C, Kalmar K, Langenbahn D M, Malec J F, Bergquist T F, Felicetti T, Giacino J T, Harley J P, Harrington D E, Herzog J, Kneipp S, Laatsch L, Morse PA. Evidence-based cognitive rehabilitation: Recommendations for clinical practice. Archives of Physical Medicine and Rehabilitation. 2000;81:1596–1615. doi: 10.1053/apmr.2000.19240. doi:10.1053/apmr.2000.19240. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Conklin H M, Reddick W E, Ashford J, Ogg S, Howard S C, Morris E B, Brown R, Bonner M, Christensen R, Wu S, Xiong X, Khan R B. Long-term efficacy of methylphenidate in enhancing attention regulation, social skills, and academic abilities of childhood cancer survivors. Journal of Clinical Oncology. 2010;28:4465–4472. doi: 10.1200/JCO.2010.28.4026. doi:10.1200/JCO.2010.28.4026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gioia G, Isquith P, Guy S, Kenworthy L. The behavior rating inventory of executive function (BRIEF): A professional manual. Odessa, FL: Psychological Assessment Resources; 2000. [Google Scholar]
- Grolnick W S, Slowiaczek M L. Parents’ involvement in children’s schooling: A multidimensional conceptualization and motivational model. Child Development. 1994;65:237–252. doi: 10.1111/j.1467-8624.1994.tb00747.x. doi:10.1111/j.1467.8624.1994.tb00747.x. [DOI] [PubMed] [Google Scholar]
- Halligan P W, Wade D T, editors. Effectiveness of rehabilitation for cognitive deficits. New York: Oxford University Press Inc; 2005. [Google Scholar]
- Hardy K K, Willard V W, Allen T M, Bonner M J. Working memory training in survivors of pediatric cancer: A randomized pilot study. Psycho-Oncology. 2013;22:1856–1865. doi: 10.1002/pon.3222. doi:10.1002/pon.3222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill N E, Taylor L C. Parental school involvement and children’s academic achievement: Pragmatics and issues. Current Directions in Psychological Science. 2004;13:161–164. Doi: 10.1111/j.0963-7214.2004.00298.x. [Google Scholar]
- Hoover-Dempsey K V, Battiato A C, Walker J M, Reed R P, DeJong J M, Jones K P. Parental Involvement in homework. Educational Psychologist. 2001;36:195–209. doi:10.1207/S15326985EP3603_5. [Google Scholar]
- Kesler S R, Lacayo N J, Jo B. A pilot study of an online cognitive rehabilitation program for executive function skills in children with cancer-related brain injury. Brain Injury. 2011;25:101–112. doi: 10.3109/02699052.2010.536194. doi:10.3109/02699052.2010.536194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landier W, Bhatia S, Eshelman D A, Forte K J, Sweeney T, Hester A L, Darling J, Armstrong F D, Blatt J, Constine L S, Freeman C R, Friedman D L, Green D M, Marina N, Meadows A T, Neglia J P, Oeffinger K C, Robison L L, Ruccione K S, Sklar C A, Hudson MM. Development of risk-based guidelines for pediatric cancer survivors: The Children's Oncology Group Long-Term Follow-Up Guidelines from the Children's Oncology Group Late Effects Committee and Nursing Discipline. Journal of Clinical Oncology. 2004;22:4979–4990. doi: 10.1200/JCO.2004.11.032. doi:10.1200/JCO.2004.11.032. [DOI] [PubMed] [Google Scholar]
- Miedel W T, Reynolds A J. Parent involvement in early intervention for disadvantaged children: Does it matter? Journal of School Psychology. 1999;37:379–402. doi:10.1016/S0022-4405(99)00023-0. [Google Scholar]
- Nathan P C, Patel S K, Dilley K, Goldsby R, Harvey J, Jacobsen C, Kadan-Lottick N, McKinley K, Millham A K, Moore I, Okcu M F, Woodman C L, Brouwers P, Armstrong FD. Guidelines for identification of, advocacy for, and intervention in neurocognitive problems in survivors of childhood cancer: A report from the Children's Oncology Group. Archives of Pediatrics and Adolescent Medicine. 2007;161:798–806. doi: 10.1001/archpedi.161.8.798. doi:10.1001/archpedi.1618.8.798. [DOI] [PubMed] [Google Scholar]
- Patel S K, Peters B B, Bell T, Verner J, Katz E R, Baron M N, Buckwalter J G. Parent involvement and neurocognitive functioning in childhood cancer survivors. Journal of Behavioral Health. 2014;3:43–52. [Google Scholar]
- Solberg M M, Mateer C A. Cognitive rehabilitation: An integrative neuropsychological approach. New York: The Guilford Press; 2001. [Google Scholar]
- Stroud K C, Reynolds C R. School motivation and learning strategies inventory (SMALSI) Torrance, CA: Western Psychological Services; 2006. [Google Scholar]
- Switzer L S. Family factors associated with academic progress for children with learning disabilities. Elementary School Guidance and Counseling. 1990;24:200–206. [Google Scholar]
- Taylor H G, Yeates K O, Wade S L, Drotar D, Klein S K, Stancin T. Influences on first-year recovery from traumatic brain injury in children. Neuropsychology. 1999;13:76–89. doi: 10.1037//0894-4105.13.1.76. doi:10.1037/0894-4105.13.1.76. [DOI] [PubMed] [Google Scholar]
- Taylor H G, Yeates K O, Wade S L, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. doi:10.1037/0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- Van Voorhis F. Interactive homework in middle school: Effects on family involvement and science achievement. Journal of Educational Research. 2003;96:323–338. doi:10.1080/00220670309596616. [Google Scholar]
- Verner J A. 2005. Measures of parent involvement behaviors at home and in school (Unpublished master’s thesis). School of Psychology at Fuller Theological Seminary, Pasadena, CA. [Google Scholar]
- Wechsler D. Wechsler individual achievement test-II. San Antonio, TX: The Psychological Corporation; 2001. A brand of Harcourt Assessment. [Google Scholar]
- Werba B E, Hobbie W, Kazak A E, Ittenbach R F, Reilly A F, Meadows A T. Classifying the intensity of pediatric cancer treatment protocols: The intensity of treatment rating scale 2.0 (ITR-2) Pediatric Blood and Cancer. 2007;48:673–677. doi: 10.1002/pbc.21184. doi:10.1002/pbc.21184. [DOI] [PubMed] [Google Scholar]
- Wilson B A, Herbert C M, Shiel A. Behavioural approaches in neuropsychological rehabilitation: Optimising rehabilitation procedures. New York: Psychology Press; 2003. [Google Scholar]
- Yeates KO, Taylor HG, Drotar D, Wade SL, Klein S, Stancin T, Schatschneider C. Preinjury family environment as a determinant of recovery from traumatic brain injuries in school-age children. Journal of the International Neuropsychological Society. 1997;3:617–630. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.