Abstract
Objective To examine whether individual differences and intraindividual (within-person day-to-day) fluctuations in late adolescents’ self-regulation were associated with daily adherence to the type 1 diabetes regimen. Methods 110 school seniors (M age = 17.78 years) and their mothers assessed adolescents’ skills underlying self-regulation (executive function, attention, self-control, behavioral inhibition and activation, emotion regulation) and adherence, with glycosylated hemoglobin from medical records. Teens completed daily diaries reporting self-regulation failures surrounding monitoring blood glucose, adherence, and number of blood glucose checks each day for 14 days. Results Hierarchical Linear Models indicated that better daily adherence was associated with teen and mother reports of better self-regulation skills and teens’ reports of fewer daily self-regulation failures. Daily adherence was unrelated to temperamental differences in behavioral inhibition and activation. Conclusions Results indicate that both individual and intraindividual differences in self-regulation contribute to daily adherence highlighting the importance of daily self-regulatory challenges to adherence.
Keywords: adherence, adolescents, diabetes, executive function, self-regulation
Adherence to a regimen of type 1 diabetes management involves a complex self-regulation process for adolescents with type 1 diabetes (Hood, Peterson, Rohan, & Drotar, 2009). Youth must coordinate a number of behaviors multiple times each day including testing blood glucose, calculating insulin doses, and administering insulin through injections/bolusing. Successful execution of these daily adherence behaviors relies on self-regulation, defined as the ability to control one’s behaviors, together with emotions and cognitions (Tangney, Baumeister, & Boone, 2004) to accomplish important goals. For example, a behavior such as testing daily blood glucose may be affected by one’s ability to control one’s negative effect (Fortenberry et al., 2009) and cognitions involving planning and remembering supplies needed to test blood glucose.
As self-regulation involves the coordination of behaviors with cognition and emotion, it may draw from teens’ broader cognitive and emotion regulation abilities (Tangney, Baumeister, & Boone, 2004). From a cognitive neuroscience perspective, self-regulation is driven by a set of higher order neurocognitive processes that fall under the umbrella of executive functioning (Blair & Ursache, 2011; Suchy, 2009). Executive functioning allows one to plan, organize, and successfully execute cognitive and behavioral actions, in the face of often competing emotions or drives. From a temperamental perspective, self-regulation is affected by more automatic lower level processes involved in the control of emotion and sensitivity to rewards versus punishments (Rothbart & Bates, 2006). Self-regulation involves both the coordination of this cognitive system together with the temperamental system to produce effective goal-directed action and self-control (Blair & Ursache, 2011; Steinberg, 2010). Teens frequently experience difficulties in self-regulation, as the coordination of emotions, cognitions, and behaviors develops gradually across adolescence and into early adulthood (Blakemore & Choudhury, 2006; Steinberg, 2010).
Recently, research has considered the role of self-regulation in diabetes management, confirming that youth with self-regulation weaknesses exhibit poorer overall adherence to the diabetes regimen (McNally, Rohan, Pendley, Delamater, & Drotar, 2010; Miller et al., 2012). For example, poorer self-control and emotion regulation (awareness of and processing of emotions) are related to poorer adherence, metabolic control, and well-being (Hughes, Berg, & Wiebe, 2012; Housiaux, Luminet, Van Broeck, & Dorchy, 2010; King et al., 2012). Similarly, poorer impulse control (failure to engage in cognitive processing before action) is also related to poorer adherence behaviors (Stupiansky, Hanna, Slaven, Weaver, & Fortenberry, 2013). Such research supports the view that self-regulation skills are related to overall adherence. However, researchers have yet to examine a range of self-regulation skills that tap cognitive and emotion abilities that may underlie better adherence. Additionally, daily adherence has not been examined.
Daily adherence may not only be affected by individual differences in self-regulation but also by intraindividual (i.e., within-person) day-to-day fluctuations in self-regulation. Day-to-day fluctuations in self-regulation refer to how an adolescent may vary each day from his or her own average level of self-regulation. Adolescents’ failures in daily adherence are likely a product of individual differences in teens’ self-regulation skills together with the constraints and opportunities of daily life that create fluctuations in self-regulation from one day to the next. Diabetes management behaviors must be completed multiple times each day, and youth frequently face obstacles that may contribute to self-regulation failures (failures to regulate emotions, behaviors, and cognitions) and subsequently poor adherence (Berg et al., 2013; Mulvaney et al., 2011). For instance, on a daily basis, adolescents are distracted by competing priorities, causing them to put off their blood glucose testing (Mulvaney et al., 2011; Schlundt, Pichert, Rea, & Puryear, 1994). Even individuals with good self-regulation skills may experience self-regulation failures on a daily basis. Thus, understanding teens’ day-to-day fluctuations in their ability to self-regulate may predict day-to-day fluctuations in adherence above and beyond individual differences in self-regulation skills.
The examination of day-to-day fluctuations in self-regulation failures and diabetes adherence was accomplished in the present study via a daily diary approach. In comparison with the traditional approach of measuring adherence through retrospective recall over the preceding week or month, daily assessments reduce recall biases and are linked to the situational contexts that may support or disrupt diabetes management (Mulvaney et al., 2012; Quittner, Espelage, Ievers-Landis, & Drotar, 2000). A daily diary approach is consistent with recent calls to advance our understanding of adherence by examining the rates and patterns of adherence within individuals across time (Modi et al., 2012; Mulvaney et al., 2012). Daily adherence was measured through daily self-report as well as self-reported frequency of daily blood glucose checks. Blood glucose checks are a key feature of adherence (Hood, Peterson, Rohan, & Drotar, 2009) that provide important information for understanding long-term metabolic control as measured by glycosylated hemoglobin (HbA1c) in addition to self-report measures of adherence (Kichler, Kaugars, Maglio, & Alemzadeh, 2012).
The primary goal of the study was to examine whether adherence behaviors were associated with individual differences and intraindividual day-to-day fluctuations in self-regulation skills. Teens and mothers completed individual difference measures of self-regulation skills and adherence, and teens completed a 14-day diary reporting daily on failures in self-regulation and adherence. We first examined whether self- and mother-reported individual differences in self-regulation skills were associated with adherence as measured over a week or month, as well as with average daily adherence and daily self-regulation failures. We predicted that both teens’ and mothers’ reports of self-regulation skills would relate to poorer general adherence, as well as lower average levels of daily adherence. Second, we examined how individual differences in self-regulation skills as well as day-to-day fluctuations in self-regulation failures independently predicted daily adherence. Adolescent success or failures in this daily self-regulatory process is likely a product of individual differences in teens’ self-regulation skills together with the constraints and opportunities in their daily setting.
Methods
Participants
Participants included 135 high school seniors (57 male and 78 female, M age = 17.76, SD = 0.38 years), with type 1 diabetes and 127 of their mothers (2 indicating they were too busy to participate, 1 did not speak English or Spanish, 5 did not give a reason for not participating). High school seniors and parents were recruited to participate in a 2-year longitudinal study to examine the transition to emerging adulthood during a routine visit to their outpatient pediatric endocrinology clinic in two southwestern cities. Of the 127 mothers who initially agreed to participate, 119 completed the surveys (2 could not be reached after initially agreeing, 6 never completed the survey). Although fathers were invited to participate, roughly half of fathers participated (N = 64) and thus were not included in the present analyses. Further, four adolescents did not complete the diary, and an additional five adolescents completed <3 days of the diary and were dropped (adolescents completed a mean of 11.08 diary days, SD = 3.3). Thus, all analyses were conducted on 110 adolescent–mother dyads (42 male and 68 females, M age = 17.78, SD = 0.39). The 110 adolescents did not differ from the 25 who were excluded in any study variables, with the exception of one (teens in the 110 sample reported better adherence on the self-care inventory (SCI) than the 25 excluded, with a mean of 3.65 vs. 3.39). Youth were eligible if they had been diagnosed with type 1 diabetes for at least 1 year (M length of diagnosis = 7.51 years, SD = 3.79), had English as their primary language, were in their last year of high school, lived with a parent (84.5% lived at home with both parents, 15.5% with one parent), would be able to have regular contact with parents over the subsequent 2 years, and had no condition that would prohibit study completion (e.g., severe intellectual disability, blindness, etc.). Mothers (N = 110, M age = 45.91 years, SD = 5.24) were recruited regardless of whether they lived with the adolescent. If multiple mothers (biological, step) were eligible, the mother most involved in diabetes management was recruited. Mothers’ participation was not mandatory.
Recruitment was conducted in the respective endocrinology clinics by a research assistant who was present for the patient’s appointment. Of the qualifying individuals approached, 54.95% agreed to participate. Reasons for not participating included lack of interest (42.9%) and being too busy in their senior year to participate (38.8%); 18.4% declined to give a reason. The final sample was 84.2% Caucasian, of which 12.4% self-identified as Latino ethnicity, 7.5% African American, and 8.4% other. 42% of teens used an insulin pump and 26.5% were on continuous glucose monitoring.
Procedure
The study was approved by the appropriate Institutional Review Board, with parents providing informed consent and teens consent or assent. Procedures involved an in-person laboratory session, where individuals were given instructions on how to complete an online survey of self-regulation skills and a 2-week online daily diary. Internet access was not required for participation; a personal electronic device was available to those without access. Participants received an e-mail with a link to their confidential online survey and instructions to complete the survey individually. Following completion of the survey, the 14-day daily diary began, with individuals receiving daily an electronic link and instructions to complete the diary by the end of the day. Teens received phone calls or text messages daily if they had not completed the diary by 9 p.m. to encourage participation and address problems. Teens were paid $50 for laboratory procedures and the online survey, and $5 for each daily diary completed; mothers received $15 for completing their survey.
Measures
Individual Differences in Self-Regulation
Problems With Executive Functions
Teens completed the Behavior Rating Inventory of Executive Function-Self-Report (BRIEF-SR; 80 items), and mothers completed the parent inventory (86 items). These widely used measures are normed for respondents between 5 and 18 years of age (Guy, Isquith, & Gioia, 2004). Participants rated each item (e.g., I don’t plan ahead for future activities) on a 3-point scale (from 0 = never to 2 = often) to indicate how often they (or their adolescent) experienced each problem over the past 6 months. Subscales were combined into a global executive composite score with good reliability (α = .96 and α = .97 for adolescent and mother reports, respectively).
Attentional/Cognitive-Behavioral Control Problems
Teens completed the Conners–Wells’ Adolescent Self-Report Scale-Short (Conners, 2001) and mothers the Parent Rating Scales-Revised (Short Form) to measure inattention and hyperactivity. The scales were normed for ages 12–17 years and have good reliability and validity (Conners, 2001). Participants rated 27 items (e.g., I have trouble organizing my schoolwork) indicating their experience of problems in the past month using a 0 (not true at all) to 3 (very much true) scale. For items that referred to behavioral problems more typical of younger children, parents were instructed to consider how their child was at a younger age. The total score was used. Reliabilities in the present sample for teen and mother report were α = .87 and .92, respectively.
Self-Control
Teens and mothers completed the 13-item Brief Self-Control Scale (BSC; Tangney, Baumeister, & Boone, 2004) to index self-control in the face of competing emotions or contexts in general with no time period specified (higher scores reflect better self-control). The scale has excellent validity, with higher scores related to higher levels of achievement, psychological adjustment (Tangney, Baumeister, & Boone, 2004), and better metabolic control (Hughes, Berg, & Wiebe, 2012). Items (e.g., I am able to work effectively towards long-term goals) were rated on a 1 (not at all like me/my child) to 5 (very much like me/my child) scale and averaged. Reliability in the present study was α = .83 and α = .88 for teen and mother reports, respectively.
Behavioral Inhibition and Activation
Teens and mothers completed the Behavioral Inhibition (BIS; 7 items) and Activation Scales (BAS; 13 items) that tap into motivational and temperamental systems underlying behavior and affect with no time frame specified (Carver & White, 1994; Gray, Gale, & Edwards, 1986). The BAS captures whether people are motivated toward rewards (e.g., “When I’m doing well at something, I love to keep at it,” reverse scored), whereas the BIS captures whether people are motivated to avoid punishment (e.g., I worry about making mistakes, reverse scored). Items were rated on a scale from 1 (very true for me/my teen) to 4 (very false for me/my teen), with summed scores analyzed. These scales have adequate validity and reliability (Carver & White, 1994; Smits & Boeck, 2006); in the present study, α = .79 and .82 for teen and mother reports of BIS, and α = .65 and .70 for teen and mother reports of BAS, respectively.
Emotion Regulation Problems
Teens and mothers completed the Difficulties in Emotion Regulation Scale (DERS) to assess difficulties with emotional awareness, acceptance, and regulation (Gratz & Roemer, 2004) in general, with no time period specified. Participants rated 37 items (e.g., “I experience my emotions as overwhelming and out of control”) using a 1 = almost never to 5 = almost always scale. This scale has excellent construct validity in adolescent (Weinberg & Klonsky, 2009) and adult samples (Gratz & Roemer, 2004). Reliabilities in the present sample were excellent α = .94 for both teen and mother reports. A summed score was used.
Individual Differences in Adherence
Teens and mothers completed two self-report measures of adherence. First, the revised Diabetes Behavior Rating Scale (DBRS) assessed adherence behaviors in the past 7 days (Iannotti et al., 2006). This 37-item scale taps current practice recommendations and problem solving relevant to daily diabetes management (e.g., “Were blood sugar levels tested as often as recommended by the doctor”). Scores were calculated as the proportion of the maximum possible score, ranging from 0 to 1, with higher scores indicating better adherence (Iannotti et al., 2006). The DBRS was used, as it correlates highly with more time-intensive interview measures of adherence and with HbA1c and has good internal consistency (α = .86) (Iannotti et al., 2006). Reliabilities were α = .85 and .82 for teens on a pump, α = .87 and .79 for teens not on pump (teens and mothers, respectively, in present study). Second, a brief index of adherence assessed seven diabetes management tasks, from which our measure of daily adherence was modeled. Items from the Self Care Inventory (La Greca, Follansbee, & Skyler, 1990; Lewin et al., 2009) were reviewed by a diabetes educator and a pediatric endocrinologist to identify management behaviors that should occur daily; items were then revised to capture currently recommended daily diabetes behaviors. Teens and mothers rated how often the behavior was completed as recommended in the past month (1 = did not do to 5 = always did without fail): Checking blood glucose with meter, administering the correct insulin dose, administering insulin at the right time, adjusting insulin based on blood glucose values, having quick-acting sugar available, eating the proper foods or counting all carbohydrates, and using a pump (e.g., programming the pump, making sure there is enough insulin) or continuous monitor (e.g., wearing the sensor) correctly. In the present study, the scale had good reliability (α = .85 and .89 for teen and mother, respectively), with an average score used.
Metabolic Control
Metabolic control was indexed using HbA1c obtained from medical records. HbA1c represents the average blood glucose over the prior 2 or 3 months, with higher levels indicating poorer metabolic control. HbA1c is the current standard for whether diabetes treatment goals are being achieved. At one site, HbA1c was measured by clinic staff using the Bayer DCA 2000; at the other site, HbA1c was measured using Bayer DCA Vantage.
Day-to-Day Fluctuations in Self-Regulation and Adherence: Daily Diary Measures
Daily Self-Regulation Failures
At the end of each day, teens reported on their experience of eight failures in self-regulation involving cognitive, behavioral, and emotional control using a 1 (strongly disagree) to 5 (strongly agree) scale. These failures were assessed in the context of monitoring blood glucose, a crucial and difficult daily behavior (Berg et al., 2013; Hood, Peterson, Rohan, & Drotar, 2009), and were designed by the authors to tap key components of regulation involving planning, initiation, memory, and emotional control: (a) I kept putting off my blood glucose testing, (b) I had a lot going on and had a hard time figuring out the best time or place to do my blood glucose tests, (c) I kept meaning to test my blood glucose, but in the end it didn’t quite happen the way it was supposed to, (d) Each time I was about to test my blood glucose, I got distracted by something else, (e) Testing my blood glucose kept slipping my mind, (f) I figured that if I skipped some of my blood glucose testing, it wouldn’t be a big deal, (g) I was so involved in doing something else I was enjoying that I didn’t stop to test my blood glucose when I was supposed to, and (h) I was in a bad mood today and didn’t really care about testing my blood glucose. An average score was used. Interitem consistency reliability of the eight items was calculated via Hierarchical Linear Modeling (HLM) random intercept models, with both time and item treated as nested levels, and was excellent (reliability = .98).
Daily Adherence and Blood Glucose Checks
At the end of each day, teens rated their adherence using six items from the modified SCI described above (the two items about dose and time of insulin were combined into a single item to minimize the number of items). Teens rated how well they followed recommendations in the past 24 h on a 1 (did not do it) to 5 (did it exactly as recommended) scale with reliability being high (.97). Teens also recorded each blood glucose reading taken off their glucometer at the end of each day and total number of blood glucose checks reported each day was analyzed.
Data Analysis
First, to examine the links between self-regulation skills and adherence, associations among individual differences in self-regulation skills, global adherence, and daily adherence and self-regulation failures averaged across the 14 days were examined via correlations. Second, to examine how both individual differences in self-regulation and day-to-day fluctuations in self-regulation failures related to daily adherence, daily diary data were analyzed with HLM6 (Raudenbush, Bryk, & Condon, 2004) as days were nested within participant. At Level 1, we examined the daily associations between teens’ reports of self-regulation failures and adherence, and at Level 2, we added global indicators of self-regulation skills (on the intercept), allowing us to consider both individual differences in self-regulation skills and within-person day-to-day fluctuations in self-regulation failures as predictors of daily adherence. Separate models were conducted for teen versus mother reports of individual difference measures of self-regulation. The following model illustrates the analysis of the BRIEF (additional models included other self-regulation skills).
Level 1:
- Level 2:
Daily predictor variables were person-mean centered and thus reflect deviations from an individual’s mean, and Level 2 variables were grand centered. At the daily level (Level 1) for each person, daily adherence (Adherenceti) was predicted from day as well as the individual’s self-regulation failures on a given day. β1i is the within-person effect of day on adherence and represents whether adherence varied by the day in which the diary was completed (centered at day 7.5), with γ10 representing the sample average within-person day effect. β2i reflects the within-person effect of self-regulation failures on adherence and represents whether day-to-day fluctuations in self-regulation (around an individual’s mean) were associated with day-to-day fluctuations in adherence, with γ20 representing the sample average within-person effect of self-regulation failures. At Level 2, individual differences in self-regulation (such as the BRIEF) predicted average adherence (when all Level 1 variables are 0, as these are group centered that reflects day 7.5 and average self-regulation failures), with the coefficient γ01 indicating the effect of individual differences in self-regulation on daily adherence after controlling for daily self-regulation failures and day. u0i, u1i, and u2i are random effects allowing for individual differences in the average level of adherence and within-person day and self-regulation effect, respectively. eti is the Level 1, or residual variance. Each facet of self-regulation was examined in a separate analysis, as the utility of these measures for assessment of self-regulation had not been previously examined.
In all analyses, we analyzed 10 multiply imputed data files using Norm (Schafer, 1999) to account for missing data. Missing items on surveys were imputed as a function of the other scale items, and missing daily diary values were imputed as a function of the other set of diary values. Our procedure imputed data for items or days, rather than entire scale values. This resulted in a recovery of 39 cases in comparison with using a listwise procedure. The amount of missingness by item ranged from 1.2% as a lower bound to 28.9% as an upper bound. Data were examined for skew with several variables having positive skew (HbA1c, BRIEF, Conners-Wells' Adolescent Self-Report Scale-Short, and DERS) and others negative skew (teens’ and mothers’ BAS reward responsiveness and adherence); however, analyses conducted on appropriate transformations yielded no changes in results, so data were kept in their original scales for ease of interpretation. Data were examined for differences across sites, with site differences existing for mothers’ reports of adherence, average self-regulation failures in the diary, teen reports of difficulties in emotion regulation, and the proportion of those on a pump. Analyses were conducted both with site as a control versus not, and the results were the same, thus the results are reported without site controlled.
Results
Individual Differences in Adherence and Self-Regulation
Correlations were examined among teens’ and mothers’ reports of the primary study variables (see Table I). Adherence as measured globally and across days was correlated. Greater adherence (from both teen and mother reports and measured both globally and across days) as well as better metabolic control (lower HbA1c) were associated with fewer problems in executive function, fewer attention problems, fewer difficulties in emotion regulation, and better self-control. Teen reports of more daily self-regulation failures were associated with teens’ reports of more problems in executive function, more attention problems, more difficulties in emotion regulation, and poorer self-control. Teens’ and mothers’ reports of problems in executive function, attention, emotion regulation, and self-control were related. Teens’ and mothers’ reports of adherence were neither associated with behavioral inhibition nor with behavioral activation.
Table I.
Means and Correlations of Study Variables
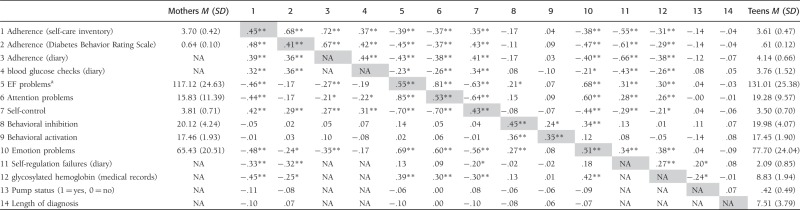 |
Note. Means and correlations above the diagonal are for teen reports, below the diagonal are for mother reports. The diagonal presents correlations between teen and mother reports, when available. NA = not available because mothers did not complete daily diary measures.
aEF, executive function.
*p < .05, **p < .01.
Daily Adherence Predicted From Daily Regulation Failures and Individual Differences in Self-Regulation
HLM analyses were conducted predicting teens’ reports of daily adherence from teens’ reports of self-regulation failures at the daily level (Level 1) and individual differences in self-regulation (Level 2) on the intercept. As can be seen in Table II, teens’ reports of daily adherence were predicted from teens’ reports of daily self-regulation failures. That is, on days in which teens reported fewer self-regulation failures relative to their average number of failures, they also reported better adherence. In addition, when controlling for daily self-regulation failures, individual differences in self-regulation also predicted average adherence across the 14-day period. As was found in the correlations, daily adherence was better when teens perceived fewer long-standing problems in executive function, attention, and difficulties in emotion regulation, and better self-control. Separate analyses on mothers’ perceptions of her teen’s self-regulation skills revealed that teen’s reports of better daily adherence were associated with mothers’ perceptions of fewer problems in executive function, fewer attention difficulties, greater self-control, and fewer difficulties in emotion regulation over and above the day-to-day fluctuations in teen-reported self-regulation failures. Behavioral inhibition and activation were not associated with daily adherence.
Table II.
HLM Analyses of Teen Reports of Daily Adherence and Number of Blood Glucose Checks (Dependent Variables [DVs]) From Teen Self-Regulation Failures and Teen and Mother Reports of Self-Regulation Skills (Independent Variables [IVs])
| DV teen report | Teena |
Motherb |
||
|---|---|---|---|---|
| Adherence b (SE) | Blood glucose checks b (SE) | Adherence b (SE) | Blood glucose checks b (SE) | |
| Base model | ||||
| Intercept | 4.15 (.06)** | 3.77 (.14)** | 4.15 (.06)** | 3.77 (.14)** |
| Day | −.01 (.004) | −.04 (.01)** | −.006 (.004) | −.04 (.01)** |
| Self-regulation failures | −.17 (.03)** | −.36 (.08)** | −.17 (.03)** | −.36 (.08)* |
| Individual difference measures tested in separate models together with base model | ||||
| Executive function problems | −.01 (.002)** | −.01 (.005)* | −.007 (.002)** | −.01 (.006) |
| Attention problems | −.02 (.006)** | −.03(.01)* | −.01 (.006) | −.025 (.01) |
| Self-control | .33 (.09)*** | .59 (.21)** | .24 (.09)** | .61 (.22)** |
| Behavioral inhibition | −.02 (.01) | .03 (.03) | .008 (.02) | .02 (.04) |
| Behavioral activation | .01 (.03) | −.06 (.08) | .04 (.04) | −.08 (.09) |
| Difficulties in emotion regulation | −.01 (.002)*** | −.01 (.006) | −.01 (.003)** | −.01 (.007) |
aIVs in these model include teen report of individual differences in self-regulation.
bIVs in these models include mother report of individual differences in self-regulation.
All models included an intercept, day, and daily self-regulation failure (teen report) effects, but are only reported for the first model, as they were consistent across models, *p < .05, **p < .01, ***p < .001.
Similar analyses were performed predicting teens’ reports of the number of daily blood glucose checks from their reports of daily self-regulation failures and teens’ and mothers’ reports of self-regulation skills. The results were similar to those reported above for adolescents’ reports of adherence (see Table II). Teens reported more blood glucose checks on days they reported fewer self-regulation failures, and teens’ perceptions of fewer problems in executive function and attention, and teens’ and mothers’ perceptions of greater self-control predicted higher levels of daily blood glucose checks. Behavioral inhibition and activation were not associated with daily blood glucose checks.
Discussion
Consistently across reporter, teens’ global adherence to their diabetes regimen was associated with numerous facets of self-regulation that tap cognitive and emotional control. These facets of regulation were also involved in teens’ daily adherence behaviors and self-regulation failures, suggesting that these self-regulation abilities are important resources that teens draw on to reduce failures that limit their daily adherence. Finally, in addition to individual differences in self-regulation, day-to-day fluctuations in self-regulation failures (i.e., increases or decreases across days from an individual’s average level of self-regulation failure) independently predicted daily adherence. Thus, even those with good self-regulation abilities may experience fluctuations in their ability to regulate blood glucose on a daily basis.
Adherence was related to numerous facets of self-regulation skills as reported by both teens and mothers. Teens’ global adherence behaviors (as reported by both teens and mothers) and daily adherence (as assessed by teens’ reports of adherence behaviors) were associated with both teens’ and mothers’ reports of general executive functioning, attention, self-control, and emotion regulation. The consistency of these results across multiple metrics adds to the current literature (which has typically focused on only one facet of self-regulation) and is suggestive that a broader cognitive construct such as executive functioning or attentional control may be the key for successful completion of any goal-directed behavior, especially successful diabetes management. Self-regulation, as assessed by teens’ and mothers’ reports on the BSC, was also consistently related to teens’ reports of the number of blood glucose checks per day, whereas other measures of self-regulation skills were less consistently related to blood glucose checks across reporters. The more consistent relations for teens’ reports of blood glucose checks with their own reports of self-regulation than with mothers’ could be due to common method variance or because mothers may be less aware of teens’ blood glucose testing.
As the BSC was designed to measure the coordination of cognitive, behavioral, and emotional components of self-regulation, such coordination may be especially predictive of daily adherence behaviors. For example, for successful adherence to occur, one needs to generate a plan for when and how blood glucose testing will occur and problem solve alternative solutions when an original plan is thwarted. Completing the cognitive tasks of planning, organization, and problem solving, however, is not sufficient. Behavioral control processes are required to initiate and complete the blood glucose testing and insulin adjustments, not once but repeatedly during the day. Finally, emotion regulation processes are crucial as one experiences negative emotions that may prevent one from engaging in adherence behaviors.
Although our results are consistent with a view that a broad array of self-regulation skills underlie teens’ adherence behaviors, an important caveat must be noted. Behavioral activation (sensitivity to rewards) and behavioral inhibition (sensitivity to punishment) were not associated with adherence either as measured over the past month or daily. We had anticipated that higher behavioral activation especially would be associated with poorer adherence, as adolescents display more reward sensitivity (Cauffmann etal., 2010) than young adults, and adherence competes with other potentially more immediately rewarding activities (e.g., eating high carbohydrate foods without checking blood glucose in the presence of friends). The lack of significant results could be due to the specific self-report measures we used; additional research with other temperamental questionnaires (Rothbart & Bates, 2006) and behavioral measures is needed. However, Hofmann, Baumeister, Forster, and Vohs (2012) found that self-reported sensitivity to rewards was involved only in the strength of one’s daily desires, but not in how well one enlists self-control to resist desires. Thus, the lack of significant effects for the BIS/BAS may indicate that adherence is not associated with trait-level activation of motivation in response to rewards and punishment.
In addition to individual differences in self-regulation skills, teens varied across days in self-regulation failures and adherence. Higher levels of most facets of self-regulation were associated with fewer average daily regulation failures and better average daily adherence across the 14 days. Beyond these average effects, however, there remained day-to-day fluctuations in the experience of self-regulation failures related to monitoring blood glucose, and these fluctuations in failures were associated with fluctuations in self-reported adherence and blood glucose checks. Thus, even when controlling for individual differences in self-regulation skills, variation across days in self-regulation failures, presumably reflecting barriers or situational demands, predicted adherence. Although daily self-regulation failures were related to adherence, these constructs are clearly not interchangeable. Self-regulation failures are potentially problematic for teens managing type 1 diabetes. Hoffman and colleagues (2012) demonstrated that healthy adults face self-regulatory challenges (e.g., resisting temptation) during about half of their waking hours, and such challenges may be even more common or problematic for teens with type 1 diabetes (eating without testing, not wanting to test when out with friends). Although it is widely recognized that type 1 diabetes requires ongoing daily management, we know little about the daily challenges that teens face or about how these challenges are associated with adherence (see Mulvaney et al., 2011 for exception). Future research involving experience-sampling techniques where adolescents are queried multiple times per day regarding their self-regulation failures, adherence, and daily diabetes stressors will help address the daily barriers to diabetes management.
Our results need to be interpreted in light of some limitations of the study. Our findings suggesting the importance of broad self-regulation ability for adherence may be due to the inability of self-report measures to distinguish different components of self-regulation. Future research using performance-based measures of self-regulation may reveal greater discrimination in terms of components of executive function (e.g., attention, executive control, speed of processing, general intelligence) that may be especially sensitive to facets of daily adherence. Second, our participation rate was somewhat lower than researchers’ experience in younger adolescent samples (Berg et al., 2013; Miller et al., 2012). Emerging adults are a difficult sample to recruit, as individuals report being “too busy” in their senior year of high school to participate. The sample recruited may be biased in some important ways (e.g., may have better self-regulation skills than those who did not participate). However, such bias makes our results a conservative test of the association between self-regulation and adherence, with the strong results reported especially notable. The sample was primarily Caucasian, which is consistent with the incidence rates of type 1 diabetes (Pettitt et al., 2014). Although the sample was limited to seniors in high school to better understand diabetes management during emerging adulthood, a time when neurocognitive developments affect self-regulation (Steinberg, 2010), our results might not generalize to other age ranges (e.g., Miller et al., 2012). The online survey and diary method is limited in that we were unable to verify who was completing the measure (although we regularly reminded adolescents to complete the diary on their own). Adolescents also may have multiple glucometers (one at home and at school) and may have been only reporting the number of blood glucose checks for 1 meter. Further, blood glucose checks were recorded by adolescents rather than downloaded directly from their glucometers and as such should be interpreted with caution. This method was used because glucometers are not routinely downloaded in the clinics that participated and because it was not feasible to access glucometers in subsequent years of the longitudinal study.
These findings have numerous clinical implications for addressing adherence and self-regulation in teens with type 1 diabetes. Interventions that support the development of self-regulation skills, including executive functions, attention, and emotion regulation, will be helpful for improving adherence in late adolescence. Additionally, interventions aimed at limiting the effect of attention deficit/hyperactivity disorder on disease management may also be beneficial for adolescents with attention problems (Sanchez, Chronis, & Hunter, 2006). Our results also hold promise for measures that can identify teens at risk for poor self-regulation skills within clinic settings. For instance, the BSC is a short, easy to administer measure that can be used in clinical settings for identifying adolescents at risk for problems with self-regulation that may require further assessment and appropriate cognitive and medical interventions. Our findings that day-to-day fluctuations in self-regulation failures were associated with adherence independently of individual differences in self-regulation, suggests that even those with good self-regulation may face challenges regulating their day-to-day management. Tailored problem-solving interventions identifying the contexts in which self-regulation failures occur and identifying the motivational and behavioral skills that may underlie failures regarding self-monitoring of blood glucose (Fisher, Kohut, Schachner, & Stenger, 2011) would be beneficial. Established interventions for problem solving and proactive coping (e.g., Grey, Boland, Davidson, Li, & Tamborlane, 2000) may be useful, with tailoring that addresses daily regulation failures specific to teens’ experience.
Acknowledgments
The authors thank the physicians and staff at the Utah Diabetes Center, Mountain Vista Medicine, Children’s Medical Center Dallas, and the teens and parents who participated in this study.
Funding
This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health (grant number R01 DK092939, co-PIs Berg and Wiebe).
Conflicts of interest: None declared.
References
- Berg C A, Butner J, Butler J M, King P S, Hughes A E, Wiebe D J. Parental persuasive strategies in the face of daily problems in adolescent type 1 diabetes management. Health Psychology. 2013;32:719–728. doi: 10.1037/a0029427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair C, Ursache A. A bidirectional model of executive functions and self-regulation. In: Vohs K, Baumeister R, editors. Handbook of self-regulation, Second Edition. New York, NY: Guildford Press; 2011. pp. 300–320. [Google Scholar]
- Blakemore S J, Choudhury S. Development of the adolescent brain: Implications for executive function and social cognition. Journal of Child Psychology and Psychiatry. 2006;47:296–312. doi: 10.1111/j.1469-7610.2006.01611.x. [DOI] [PubMed] [Google Scholar]
- Carver C S, White T L. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. Journal of Personality and Social Psychology. 1994;67:319–333. [Google Scholar]
- Cauffman E, Shulman E P, Steinberg L, Claus E, Banich M T, Graham S, Woolard J. Age differences in affective decision making as indexed by performance on the Iowa Gambling Task. Developmental Psychology. 2010;46:193–207. doi: 10.1037/a0016128. [DOI] [PubMed] [Google Scholar]
- Conners C K. Conners' rating scales–revised: Technical manual. North Tonawanda, NY: Multi-Health Systems Inc; 2001. [Google Scholar]
- Fisher W A, Kohut T, Schachner H, Stenger P. Understanding self-monitoring of blood glucose among individuals with type 1 and type 2 diabetes: An information-motivation-behavioral skills analysis. The Diabetes Educator. 2011;37:85–94. doi: 10.1177/0145721710391479. [DOI] [PubMed] [Google Scholar]
- Fortenberry K T, Butler J M, Butner J, Berg C A, Upchurch R, Wiebe D J. Perceived diabetes task competence mediates the relationship of both negative and positive affect with blood glucose in adolescents with type 1 diabetes. Annals of Behavioral Medicine. 2009;37:1–9. doi: 10.1007/s12160-009-9086-7. [DOI] [PubMed] [Google Scholar]
- Gratz K L, Roemer L. Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessessment. 2004;26:41–54. [Google Scholar]
- Gray J A, Gale A, Edwards J A. Physiological correlates of human behaviour, Vol. 3: Individual differences and psychopathology. San Diego, CA: Academic Press; 1986. Anxiety, personality and the brain; pp. 31–43. [Google Scholar]
- Grey M, Boland E A, Davidson M, Li J, Tamborlane W V. Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. The Journal of Pediatrics. 2000;137:107–113. doi: 10.1067/mpd.2000.106568. [DOI] [PubMed] [Google Scholar]
- Guy S C, Isquith P K, Gioia G A. Behavior rating inventory of executive function–self-report version: Professional manual. Lutz, FL: PAR; 2004. [Google Scholar]
- Hofmann W, Baumesiter R F, Forster G, Vohs K D. Everyday temptations: An experience sampling study of desire, conflict, and self-control. Journal of Personality and Social Psychology. 2012;102:1318–1335. doi: 10.1037/a0026545. [DOI] [PubMed] [Google Scholar]
- Hood K K, Peterson C M, Rohan J M, Drotar D. Association between adherence and glycemic control in pediatric type 1 diabetes: A meta-analysis. Pediatrics. 2009;124:e1171–e1179. doi: 10.1542/peds.2009-0207. [DOI] [PubMed] [Google Scholar]
- Housiaux M, Luminet O, Van Broeck N, Dorchy H. Alexithymia is associated with glycaemic control of children with type 1 diabetes. Diabetes and Metabolism. 2010;36:455–462. doi: 10.1016/j.diabet.2010.06.004. [DOI] [PubMed] [Google Scholar]
- Hughes A E, Berg C A, Wiebe D J. Emotional processing and self-control in adolescents with type 1 diabetes. Journal of Pediatric Psychology. 2012;37:925–934. doi: 10.1093/jpepsy/jss062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iannotti R J, Nansel T R, Schneider S, Haynie D L, Simons-Morton B, Sobel D O, Zietzoff L, Plotnick L P, Clark L. Assessing regimen adherence of adolescents with type 1 diabetes. Diabetes Care. 2006;29:2263–2267. doi: 10.2337/dc06-0685. [DOI] [PubMed] [Google Scholar]
- Kichler J C, Kaugars A S, Maglio K, Alemzadeh R. Exploratory analysis of the relationships among different methods of assessing adherence and glycemic control in youth with type 1 diabetes mellitus. Health Psychology. 2012;31:35–42. doi: 10.1037/a0024704. [DOI] [PubMed] [Google Scholar]
- King P S, Berg C A, Butner J, Drew L M, Foster C, Donaldson D, Murray M, Swinyard M, Wiebe D J. Longitudinal trajectories of metabolic control across adolescence: Associations with parental involvement, adolescents' psychosocial maturity, and health care utilization. Journal of Adolescent Health. 2012;50:491–496. doi: 10.1016/j.jadohealth.2011.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca A M, Follansbee D, Skyler J S. Developmental and behavioral aspects of diabetes management in youngsters. Children's Health Care. 1990;19:132–139. [Google Scholar]
- Lewin A B, La Greca A M, Geffken G R, Williams L B, Duke D C, Storch E A, Silverstein J H. Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: The self-care inventory (SCI) Journal of Pediatric Psychology. 2009;34:999–1007. doi: 10.1093/jpepsy/jsp032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally K, Rohan J, Pendley J S, Delamater A, Drotar D. Executive functioning, treatment adherence, and glycemic control in children with type 1 diabetes. Diabetes Care. 2010;33:1159–1162. doi: 10.2337/dc09-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modi A C, Pai A L, Hommel K A, Hood K K, Cortina S, Hilliard M E, Guilfoyle S M, Gray W N, Drotar D. Pediatric self-management: A framework for research, practice, and policy. Pediatrics. 2012;129:e473–e485. doi: 10.1542/peds.2011-1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M M, Rohan J M, Delamater A, Shroff-Pendley J, Dolan L M, Reeves G, Drotar D. Changes in executive functioning and self-management in adolescents with type 1 diabetes: A growth curve analysis. Journal of Pediatric Psychology. 2012;38:18–29. doi: 10.1093/jpepsy/jss100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulvaney S, Rothman R L, Dietrich M S, Wallson K A, Grove E, Elasy T A, Johnson K B. Using mobile phones to measure adolescent diabetes adherence. Health Psychology. 2012;31:43–50. doi: 10.1037/a0025543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulvaney SA, Hood KK, Schlundt DG, Osborn CY, Johnson KB, Rothman RL, Wallston KA. Development and initial validation of the barriers to diabetes adherence measure for adolescents. Diabetes Research Clinical Practice. 2011;94:77–83. doi: 10.1016/j.diabres.2011.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettitt D J, Talton J, Dabelea D, Divers J, Imperatore G, Lawrence J M, Liese A D, Linder B, Mayer-Davis E J, Pihoker C, Saydah S H, Standiford D A, Hamman R F. doi: 10.2337/dc13-1838. SEARCH for Diabetes in Youth Study Group. (2014). Prevalence of diabetes mellitus in US youth in 2009: The SEARCH for diabetes in youth study. Diabetes Care, 37, 402–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quittner A L, Espelage D L, Ievers-Landis C E, Drotar D. Measuring adherence to medical treatments in childhood chronic illness: Considering multiple methods and sources of information. Journal of Clinical Psychology in Medical Settings. 2000;7:41–54. [Google Scholar]
- Raudenbush S, Bryk A, Congdon R. HLM 6: Hierarchical linear and nonlinear modeling. Chicago, IL: Scientific Software International; 2004. [Google Scholar]
- Rothbart M K, Bates J E. Temperament. In: Eisenberg N, Damon W, editors. Handbook of child psychology, Vol. 3. Hoboken, NJ: Wiley; 2006. pp. 99–166. [Google Scholar]
- Sanchez L M, Chronis A M, Hunter S J. Improving compliance with diabetes management in young adolescents with attention-deficit/hyperactivity disorder using behavior therapy. Cognitive and Behavioral Practice. 2006;13:134–145. [Google Scholar]
- Schafer J L. NORM users’ guide (Version 2) University Park: The Methodology Center, Penn State; 1999. Retrieved from http://methodology.psu.edu. [Google Scholar]
- Schlundt D G, Pichert J W, Rea M R, Puryear W. Situational obstacles to adherence for adolescents with diabetes. The Diabetes Educator. 1994;20:207–211. doi: 10.1177/014572179402000305. [DOI] [PubMed] [Google Scholar]
- Smits D J M, Boeck P D. From BIS/BAS to the big five. European Journal of Personality. 2006;20:255–270. [Google Scholar]
- Steinberg L. A dual systems model of adolescent risk-taking. Developmental Psychobiology. 2010;52:216–224. doi: 10.1002/dev.20445. [DOI] [PubMed] [Google Scholar]
- Stupiansky N W, Hanna K M, Slaven J E, Weaver M T, Fortenberry J D. Impulse control, diabetes-specific self-efficacy, and diabetes management among emerging adults with type 1 diabetes. Journal of Pediatric Psychology. 2013;38:247–254. doi: 10.1093/jpepsy/jss110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchy Y. Executive functioning: Overview, assessment, and research issues for non-neuropsychologists. Annals of Behavioral Medicine. 2009;37:106–116. doi: 10.1007/s12160-009-9097-4. [DOI] [PubMed] [Google Scholar]
- Tangney J P, Baumeister R F, Boone A L. High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. Journal of Personality. 2004;72:271–322. doi: 10.1111/j.0022-3506.2004.00263.x. [DOI] [PubMed] [Google Scholar]
- Weinberg A, Klonsky E D. Measurement of emotion dysregulation in adolescents. Psychological Assessment. 2009;21:616–621. doi: 10.1037/a0016669. [DOI] [PubMed] [Google Scholar]


