Abstract
Objective Examined the associations between parental and child distress, and moderating effects of child exposure to life events, in families with and without a history of pediatric cancer. Methods Children with cancer and their parents (N = 255) and healthy comparison dyads (N = 142) completed self-report measures of depression, anxiety, and posttraumatic stress symptoms. Children reported on the total number of stressful life events they had experienced. Correlations between parental and child symptoms were examined. Moderating effects of child exposure to life events were tested using multiple regression. Results Parent and child symptoms were significantly related only in the cancer group. Child exposure to life events attenuated this relationship. Moderation effects were significant at or below average levels of life stress. Conclusions The experience of childhood cancer may strengthen the link between parent and child psychological functioning. However, child exposure to other life events may weaken this link.
Keywords: cancer, child, distress, life events, parent
Parental psychological distress, including symptoms of depression, anxiety, and posttraumatic stress, has received much attention in the pediatric psychology literature as a potential risk factor for child distress (e.g., Sawyer, Streiner, Antoniou, Toogood, & Rice, 1998; Trask, Paterson, Trask, Bares, Blirt, & Maan, 2003). Numerous mechanisms are proposed for the link between parental distress and such symptoms in the child. For example, parental distress may be an expression of biological susceptibility to certain disorders that may be passed on to children, including depression (Beardslee, Gladstone, & O'Connor, 2011), anxiety (Hettema, Neale, & Kendler, 2001), and posttraumatic stress (PTS; Cornelis, Nugent, Amstadter, & Koenen, 2010). Alternately, parental distress may interfere with the parent’s provision of emotional support necessary for healthy child adaptation and development. For instance, parental depression may exacerbate child maladjustment (Goodman et al., 2011) and contribute specifically to child depressive symptoms (McLeod, Weisz, & Wood, 2007) via parenting behaviors characterized by lowered sensitivity and consistency (Cummings & Davies, 1994), increased hostility, coerciveness, or withdrawal (Lovejoy, Graczyk, O'Hare, & Neuman, 2000), or decreased scaffolding (Hoffman, Crnic, & Baker, 2006). Prospective links between parental depression and later child anxiety and depression have been found (Halligan, Murray, Martins, & Cooper, 2007), and parental symptoms have been found to predict child symptoms rather than vice versa (Garber & Cole, 2010).
The effects of parental distress on child maladjustment have also been noted for other outcomes such as anxiety and PTS. Elevated parental anxiety may increase the child’s internalizing problems via such processes as providing too much control and granting too little autonomy (McLeod, Wood, & Weisz, 2007), modeling of anxious behaviors (Wood, McLeod, Sigman, Hwang, & Chu, 2003), and reinforcement of anxious or avoidant behaviors (Fisak & Grills-Taquechel, 2007). These parental behaviors also appear to exacerbate PTS in children (Pynoos, Steinberg, & Piacentini, 1999).
Transmission of distress from the parent to the child may occur more readily in families with a serious child illness or injury, given increased levels of distress in these parents compared with parents of healthy children (Cohen, 1999; Landolt, Ystrom, Sennhauser, Gnehm, & Vollrath, 2012). In families coping specifically with pediatric cancer, at least temporary increases in parental distress are reported compared with norms and controls (Dolgin etal., 2007; Pai et al., 2007; Vrijmoet-Wiersma et al., 2008). In turn, increased parental distress has been linked to child distress within some pediatric samples. For example, a meta-analysis found an association between maternal maladjustment and child maladjustment (Lavigne & Faier-Routman, 1993), and increased paternal maladjustment has been linked to child psychopathology 1 year later (Chaney et al., 1997). Higher parental PTS has been associated with smaller decreases in child PTS across 1 year (Landolt et al., 2012) as well. In samples specifically with pediatric cancer, cross-sectional (Trask et al., 2003) and prospective (Sawyer et al., 1998) associations between parental distress and child maladjustment have also been found. However, to ascertain whether these associations between parent and child distress are exacerbated by experiences of child cancer, comparisons with parent–child dyads in demographically matched control or normative samples are needed. The present study sought to fill this gap using a sample of parent–child dyads with pediatric cancer and demographically matched controls.
In addition to examining the association between parental distress and child adjustment, moderators that affect the strength of such association need to be further explored (Drotar, 1997). The present study examined the potential moderating effects of the child's exposure to life events. Life events refer to events in one's life that require significant adaptation, adjustment, or coping, such as moving, loss, or illness of a close family member, exposure to violence, or change in family structure (Coddington, 1972a). Exposure to life events, including illness or death of a family member, parental divorce, and abuse, is linked to increased odds of later psychopathology (Clark, Caldwell, Power, & Stansfeld, 2010; Grant, Compas, Thurm, McMahon, & Gipson, 2004; Harland, Reijneveld, Brugman, Verloove-Vanhorick, & Verhulst, 2002). Exposure to negative life events has been linked to child maladjustment in pediatric samples also (Bruce, 2006; Lavigne & Faier-Routman, 1993).
Because existing research has not yet examined the impact of a child’s exposure to life events on the association between parent and child distress, it is unknown whether such exposure makes the child more or less influenced by parental distress. As existing research suggests that exposure to life events significantly increases child distress even after accounting for family influences, we hypothesized that it would weaken the link between parent and child distress because the child would be distressed at higher levels of life events regardless of parental distress. This view would be consistent with existing models of allostatic load, which suggests that exposure to early stress (e.g., parental conflict or separation, chronic poverty) can alter the child's biological and psychological capacity for adaptation (Juster et al., 2011) in ways that render the child vulnerable to psychopathology even without a precipitating stressor, such as is proposed by diathesis-stress models of psychopathology. For instance, stressful life events, such as illness/death in the family, or parental divorce/separation, have been linked to child maladjustment even after controlling for maternal depression (Fergusson, Horwood, Gretton, & Shannon, 1985) and family characteristics (Harland et al., 2002). Cumulative exposure to life events predicts PTS in children with cancer even after accounting for demographic and medical factors and parental PTS (Currier, Jobe-Shields, & Phipps, 2009). Exposure to potentially traumatic life events (e.g., natural disasters, exposure to violence, sudden loss of a loved one) predicts symptoms of PTS and depression in adolescents admitted for surgery, even after controlling for parental symptoms of PTS and depression (Zatzick et al., 2006). Thus, existing research suggests that exposure to life events is a powerful predictor of child distress, perhaps more so than concurrent parental functioning. Based on existing findings, we hypothesized that parental functioning would influence child distress only at lower levels of child exposure to life events, whereas at higher levels of exposure to life events, the child’s distress would be less contingent on parent distress.
In summary, the present study aimed to examine the association between parental and child distress in families with and without a pediatric cancer experience and how such an association is affected by the child's exposure to life events. Based on the literature reviewed above, we hypothesized that (1) Parental distress will be significantly linked to child distress; (2) Parental distress will be more strongly linked to child distress within families with pediatric cancer than in controls; and (3) The total number of stressful life experiences to which the child has been exposed moderates the link between parent and child distress, such that this link is weakened with greater child exposure to stressful life events.
Method
Participants
Patients with a history of cancer were selected at random using a number generator and approached during routine medical appointments by trained research assistants. Of approached dyads, 68% agreed to participate, resulting in a sample of 255 children (51.8% male) and their primary caregiver who was most involved in their medical care (83.1% mothers; 12.2% fathers; 4.7% other adult figures). Eligible participants were between 8 to 17 years of age (mean age = 12.61 years, SD = 2.88), at least 1 month past diagnosis of malignancy, able to speak and read English, and without significant cognitive or sensory deficits. Participants were predominantly White (72.5%) in race/ethnicity (22.7% Black; 4.7% other). Using the Barratt Simplified Measure of Social Status (Barratt, 2006), an updated version of the Hollingshead scale (Hollingshead, 1975) that estimates socioeconomic status (SES) based on parental education and occupation, 27.5% were in SES Levels I and II, 31.9% in Level III, and 40.6% in Levels IV and V. To obtain a broadly heterogeneous and balanced sample in terms of time since diagnosis, children were recruited into one of four strata based on time elapsed since their diagnosis: 1–6 months (n = 64; 25.1%); 6 months–2 years (n = 63; 24.7%); 2–5 years (n = 65; 25.5%); and ≥5 years (n = 63; 24.7%). All cancer diagnoses were included, and a representative sample was obtained in terms of diagnostic categories, including acute lymphoblastic leukemia (23.1%), acute myeloid leukemia (7.3%), lymphoma (13.0%), solid tumors (39.3%), and brain tumors (17.4%). Roughly half of the children (n = 118; 46.3%) were on treatment at the time of study. A small minority (n = 33, 13.4%) of the children had experienced a relapse, but a similar proportion of these children were on treatment as the remainder of the sample.
Participants for the control group were recruited from a pool of children whose parents had responded to cover letters distributed by local participating school districts and provided permission to be contacted for potential enrollment in the study. The eligibility criteria for the control group were the same as those for the cancer group, except the absence of chronic or life-threatening illness. Eligible children who matched the patient sample in demographic characteristics were invited to participate. Participation rate for the control group was 93%. A total of 142 children (52.1% male; mean age = 12.26 years, SD = 2.88) and their guardian (87.3% mothers, 12.7% fathers) were enrolled, using frequency matching on age, sex, and race/ethnicity (76.8% White; 20.4% Black; 2.8% other), and these characteristics did not differ from the cancer group. However, there was a significant group difference in SES, χ2(1, N = 397) = 12.54, p < .01, such that more participants in the control group were in the high SES category and fewer were in the low SES category (40.8% SES Levels I and II; 35.2% Level III; 24.0% Levels IV and V) compared with the participants in the cancer group.
Of the total 397 children enrolled, 8 were excluded from analysis because of concerns about the validity of their responses (e.g., random or uniform responding; concerns raised by research assistants that the child did not seem to understand the measures being administered). These children were all from the cancer group and were significantly younger than the remaining sample of 389 children [mean age = 10.38 years, SD = 2.83; F(1, 395) = 4.41, p = .04].
Procedures
All participants were interviewed and assessed in the outpatient Psychology Clinic of the hospital. After informed consent/assent was obtained, children and their guardians completed survey questionnaires in separate rooms. Trained research assistants were available during data collection to assist and read items aloud if needed. For the assessment of PTS, participants spontaneously identified their most stressful or traumatic event, about which they provided information regarding their posttraumatic symptoms regardless of whether this identified event met the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) A1 criterion. Participants received $25.00 gift cards for their participation as an incentive and to help defray travel costs. Procedures were approved by the institutional review board at the authors’ home institution.
Measures
On self-report measures, parents and children reported on their own symptoms, and children also reported on life events that have occurred in their lives. Reliability and validity information provided below are from the developers of the measure unless indicated otherwise.
Parental Distress
Brief Symptom Inventory (BSI; Derogatis & Melisaratos, 1983) is a 53-item measure based on the Symptom Checklist-90-Revised that was used to assess parental psychological symptoms. Scores were normed by gender, using the adult nonpatient normative sample, to obtain T-scores for the Depression and Anxiety subscales and for the Global Severity Index (GSI). Subscales have good internal consistency (Chronbach’s α = .81 for anxiety; .85 for depression), test-retest reliability (.79 for anxiety, .84 for depression, and .90 for GSI), and convergent and divergent validity (Derogatis & Melisaratos, 1983).
Impact of Events Scale - Revised (IES-R; Weiss, 2004) is a 22-item measure of PTS experienced within the past seven days associated with the event identified as the most traumatic in their lives. It has adequate internal reliability and test-retest reliability (Weiss, 2004). In the present study, sum of all the items (Chronbach’s α = .94) was used as a total indicator of the distress associated with the event identified most traumatic by the parents.
Child Distress
Children’s Depression Inventory (Kovacs, 1992) is a 27-item child-report measure of depressive symptoms. Children chose among three statements that best describe them (e.g., “I am sad once in a while/many times/all the time”) in the past 2 weeks. The measure has adequate internal reliability (Chronbach’s α = .86), and 6-week test-retest reliability ranges from .59 to .67 (Kovacs, 1992).
Screen for Child Anxiety-Related Emotional Disorders (Birmaher et al., 1999) is a 41-item self-report measure of anxiety symptoms. Children rated how much each item (e.g., “I am nervous”) described them over the past 3 months using a 3-point scale (Not/hardly ever true; somewhat/sometimes true; very/often true). The full scale, used to obtain a total score for this study, has adequate internal reliability (Chronbach’s α = .90) and good convergent and divergent validity (Birmaher et al., 1999).
University of California at Los Angeles (UCLA) Posttraumatic Stress Disorder (PTSD) Reaction Index for DSM-IV (Pynoos, Rodriguez, Steinberg, Stuber, & Frederick, 1998) is a 22-item self-report measure assessing DSM-IV PTSD criteria based on the most traumatic stressful event identified by the respondent, regardless of whether it met the A1 criterion. Children rated the frequency of each item (e.g., “I watch out for danger or things that I am afraid of”) occurring within the past month on a 5-point Likert scale ranging from 0 = none to 4 = most. Excellent internal reliability and test-retest reliability have been reported (Steinberg, Brymer, Decker, & Pynoos, 2004), and in prior studies conducted in our laboratory, the full-scale α ranged from .88 to .90.
Child Life Events
Life Events Scale (Johnston, Steele, Herrera, & Phipps, 2003) is a modified version of the Coddington Life Events Questionnaire (Coddington, 1972b). It lists 30 life events that are assumed to be stressful (e.g., death of close others; exposure to violence; birth of a sibling; relocation). Children indicated whether each event has ever occurred to them, and the number of endorsed events was summed. Overall agreement between parents and children is .93 (Johnston et al., 2003).
Analytic Plan
Descriptive analyses were first conducted. To identify covariates, effects of demographic and medical factors on child symptoms were examined using one-way analysis of variance (for categorical factors) and correlations (for continuous factors). To test the first hypothesis that parental distress is associated with child distress, partial bivariate correlations were run, controlling for the covariates that were identified. To test the second hypothesis that associations between parent and child symptoms are stronger within the cancer group than the control group, the same partial correlations were estimated for each group, and coefficients were compared using Fisher's r-to-z transformation. Finally, to test the third hypothesis that child exposure to life events negatively moderates the association between parent and child distress, tests of moderation were conducted using hierarchical multiple regression. Covariates were entered into the first block, followed by the predictor (parental distress), the moderator (life events), and the interaction term between the predictor and the moderator, each entered in separate blocks. To reduce multicollinearity, both the predictor and the moderator variables were centered before analysis. Post hoc probes of significant moderation effects (Holmbeck, 2002) were then conducted to identify the levels of life events at which the moderation effect was significant. Sufficient power was available to detect small to medium moderation effects. All analyses were run using PASW Statistics 18.
Results
Descriptive analyses were run on the study variables (Table I). Effects of demographic and medical factors on child distress were then examined to identify potential covariates. With regard to demographic characteristics of the sample, child age, child gender, family SES, and parental gender had significant associations with child symptoms. Girls reported significantly higher levels of anxiety (M = 21.62, SD = 10.85) than boys (M = 17.44, SD = 12.53), F(1, 385) = 12.21, p = .001. Child age was associated with lower anxiety [r(387) = −.14, p = .01]. SES was associated with lower child depression [r(389) = −.11, p = .03], anxiety [r(387) = −.12, p = .02], and PTS [r(389) = −.17, p = .001]. Surprisingly, gender of the parent (86.4% female; 13.6% male) did not influence parental symptoms but influenced child symptoms. Children whose mother was the participating parent scored higher in depressive symptoms (M = 6.66, SD = 5.45) and anxiety symptoms (M = 20.10, SD = 12.00) than children whose father was the participant (M = 5.11, SD = 4.18), F(1, 387) = 3.91, p = .05, and (M = 15.31, SD = 10.56), F(1, 385) = 7.40, p = .007, respectively. These differences were not accounted for by the gender of the child. With regards to medical factors, children in the cancer group reported approximately one more stressful life event than those in the control group [F(1, 387) = 6.09, p = .01]. This difference is likely largely attributable to the experience of cancer, as children in the cancer group endorsed experiencing a serious illness in their lifetime at a significantly higher rate (80.9%) than controls (10.0%), χ2(1, N = 386) = 181.32, p < .001. Within the cancer group, medical factors such as diagnosis type, whether the child was currently in treatment, the intensity of treatment, or strata representing time since diagnosis were not significantly associated with child distress. However, surprisingly, children with a relapse history (n = 33) reported significantly lower levels of anxiety (M = 14.51, SD = 7.56) than those without a relapse (M = 19.18, SD = 12.18), Welch's F(1, 58.60) = 8.80, p = .004. Overall, child age, child gender, parent gender, family SES, and relapse history influenced child distress and were treated as covariates in subsequent analyses.
Table I.
Means and Standard Deviations for the Study Variables
| Full sample | Group |
F | p | η2 | ||
|---|---|---|---|---|---|---|
| Cancer | Control | |||||
| Parent distress | ||||||
| BSI depression T-score | 51.16 (9.18) | 51.77 (9.41) | 50.08 (8.70) | 3.03 | .08 | .008 |
| BSI anxiety T-score | 50.56 (9.77) | 51.66 (10.00) | 48.65 (9.08) | 8.68 | .003 | .02 |
| BSI global severity index T-score | 52.46 (10.33) | 52.88 (10.78) | 51.73 (9.50) | 1.10 | .30 | .003 |
| Impact of events scale - revised IES-R (PTS) total score | 22.90 (17.30) | 24.06 (17.45) | 20.90 (16.92) | 3.02 | .08 | .008 |
| Child distress | ||||||
| CDI (Depression) total score | 6.45 (5.32) | 6.29 (5.22) | 6.73 (5.48) | .62 | .43 | .002 |
| SCARED (Anxiety) total score | 19.46 (11.91) | 18.57 (11.77) | 20.99 (12.04) | 3.74 | .05 | .01 |
| UCLA (PTS) total score | 18.17 (13.88) | 17.84 (13.42) | 18.73 (14.67) | .36 | .55 | .001 |
| Life events | ||||||
| Child: total number experienced | 7.33 (3.37) | 7.64 (3.46) | 6.77 (3.13) | 6.09 | .01 | .02 |
Note. Standard deviations are reported in parentheses. The final three columns display statistics associated with one-way analyses of variance comparing cancer and control groups. Degrees of freedom for the F statistic were (1, 387) except for IES-R (1, 386), SCARED (1, 385), and UCLA (1, 384).
BSI = Brief Symptom Inventory; CDI = Children's Depression Inventory; PTS = Posttraumatic stress; SCARED = Screen for Child Anxiety-Related Emotional Disorders; University of California at Los Angeles Posttraumatic Stress Disorder Reaction Index.
To test the first hypothesis that parental distress would be linked to child distress, bivariate partial correlations were run, controlling for identified covariates (Table II). For the full sample, weak and significant correlations were found for parental depression and child depression, anxiety, and PTS (rs = .10–.13), and between parental GSI and child PTS (r = .10). Surprisingly, parental anxiety and PTS were not correlated with child distress. Thus, there was only limited support for the first hypothesis.
Table II.
Bivariate Correlations Between Parent and Child Variables
| Predictors | Full sample |
Group |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Cancer |
Control |
||||||||
| CDI | SCARED | UCLA | CDI | SCARED | UCLA | CDI | SCARED | UCLA | |
| Parent distress | |||||||||
| BSI depression | .10* | .10* | .13* | .18** | .22*** | .27*** | −.03 | −.08 | −.10 |
| BSI anxiety | .07 | .07 | .04 | .09 | .13*a | .09 | .04 | .004a | −.04 |
| BSI global severity index | .08 | .08 | .10* | .11 | .16* | .19** | .02 | −.05 | −.06 |
| IES-R post-traumatic stress | .04 | −.03 | .04 | .08 | .09 | .16** | −.04 | −.19* | −.16 |
| Child life events, lifetime | .30*** | .34*** | .34*** | .33*** | .39*** | .33*** | .27** | .31*** | .38*** |
Note. Partial correlation coefficients, controlling for child age, child gender, parent gender, and family socioeconomic status, are reported. For the cancer group only, relapse status was also controlled.
BSI = Brief Symptom Inventory, CDI = Children's Depression Inventory; IES-R = Impact of Events Scale - Revised; SCARED = Screen for Child Anxiety-Related Emotional Disorders; UCLA = University of California at Los Angeles Posttraumatic Stress Disorder Reaction Index.
aDid not significantly differ between cancer and control groups, based on Fisher's r-to-z transformation.
*p < .05. **p < .01. ***p < .001.
To test the second hypothesis that parental distress and child distress would be more strongly linked in the cancer group compared with the control group, the same partial correlations were examined by group (Table II). Parent and child symptoms were positively correlated within the cancer group. Specifically, parental depression was linked to all three types of child symptoms (depression, anxiety, and PTS; rs = .17–.26), and parental GSI was linked to child anxiety and PTS (r = .15 and .19, respectively). Links were also found in anxiety (r = .13) and PTS (r = .17). In contrast, parent and child symptoms were not linked within the control group, except for a negative correlation between parental PTS and child anxiety (r = −.19). Comparison of the correlation coefficients using Fisher's r-to-z transformation revealed that all but one (i.e., the correlation between parental and child anxiety) were significantly stronger in the cancer group than the control group. Thus, there was support for the second hypothesis.
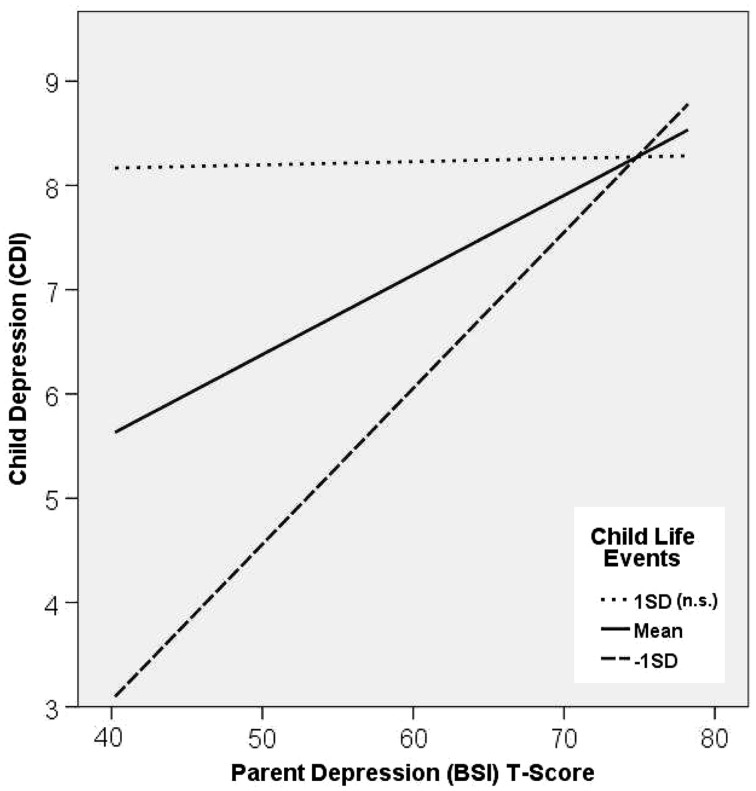
Finally, to test the third hypothesis that the total number of stressful life events reported by the child would moderate the associations found between parent and child symptoms, hierarchical multiple regression was run. Because there were significant differences in the associations between parent and child symptoms between the cancer and control groups, analyses were run separately within each group to obtain clearer results. In the control group, no significant moderation effect was found. In the cancer group, child life events significantly moderated four of the seven associations found between parental and child symptoms (Table III). Figure 1 depicts the moderating effect of child life events. Post hoc probes indicated that moderation was significant when child-reported life events were at or below the mean. Post hoc probes using the Johnson–Neyman technique (Hayes & Matthes, 2009), which indicate the number of life events at or below which moderation was significant, are reported in Table III. For all models, the association (positive slope) between parental and child distress was stronger at lower levels of child life events and weaker at higher levels of child life events. Thus, there was partial support for the third hypothesis.
Table III.
Hierarchical Multiple Regressions Within the Cancer Group, With Moderating Effects of Child Life Events
| Parental predictor/Child outcome |
||||||||
|---|---|---|---|---|---|---|---|---|
| BSI depression |
BSI GSI |
|||||||
| CDI |
SCARED |
UCLA |
SCARED |
|||||
| ΔR2 | β | ΔR2 | β | ΔR2 | Β | ΔR2 | β | |
| Step 1: demographic covariates | .06* | .18*** | .08*** | .18*** | ||||
| Step 2: parental distress | .03** | .04*** | .07*** | .02* | ||||
| BSI depression | .14* | .16** | .22*** | |||||
| BSI GSI | .11* | |||||||
| Step 3: life events | .09*** | .10*** | .08*** | .11*** | ||||
| Child life events | .35*** | .37*** | .33*** | .37*** | ||||
| Step 4: interaction | .02* | .02** | .02** | .01* | ||||
| Parental distress × Child life events | −.15* | −.14** | −.15** | −.12* | ||||
| Total R2 | .19 | .34 | .24 | .32 | ||||
| N | 247 | 245 | 244 | 245 | ||||
| Cohen's ƒ2 for moderation | .03 | .03 | .03 | .02 | ||||
| Johnson–Neyman significance value | 8.17 | 9.07 | 10.07 | 7.70 | ||||
Note. Standardized regression coefficients from the final model are reported. Demographic covariates included child age and gender, parent gender, family socioeconomic status, and presence/absence of relapse. Johnson–Neyman significance value indicates the value of child life events at or below which the moderation effect is significant.
BSI = Brief Symptom Inventory; GSI = Global Severity Index; CDI = Children's Depression Inventory; SCARED = Screen for Child Anxiety-Related Emotional Disorders; UCLA = University of California at Los Angeles Posttraumatic Stress Disorder Reaction Index.
*p < .05. **p < .01. ***p < .001.
Figure 1.
Moderating effect of child life events within the cancer group. A graphic representation of the moderating effect of child life events on the association between parental depression as measured by the Brief Symptom Inventory and child depression as measured by the Children's Depression Inventory. All of the moderating effects found in the present study revealed a similar effect.
Discussion
The present study examined the link between parental and child distress in families with and without pediatric cancer and tested the impact of child exposure to life events on those links. Surprisingly, there was only partial support for the hypothesis that parent and child distress would be linked, as this relationship was found only in families of children with cancer. Within the cancer group, parental depression and global distress severity were associated with multiple types of child distress (depression, anxiety, and/or PTS), whereas parental anxiety and PTS were related only to the same type of symptoms in the child. The findings are consistent with existing research suggesting that parental depression may be a risk factor for multiple types of child psychopathology (Lieb, Isensee, Höfler, Pfister, & Wittchen, 2002). It is unclear why parental anxiety and PTS predict only the same type of child symptoms. The stress of child diagnosis and treatment may increase parental overcontrol or modeling of anxious behaviors that specifically increase child anxiety (Murray, Creswell, & Cooper, 2009). Although transmission of PTS is not as well understood (Yehuda & Bierer, 2007), similar parenting behaviors may also contribute to the transmission of PTS (Pynoos et al., 1999).
In contrast, within a control sample of healthy children and their parents, parental distress was not linked to child distress. This finding was unexpected, as the developmental psychopathology literature suggests that parental distress would negatively impact child adjustment via parenting problems (Berg-Nielsen, Vikan, & Dahl, 2002) or a complex interaction among personal and environmental characteristics (Beardslee et al., 2011). If these processes are exacerbated in the presence of significant environmental stress, the control group may not have been experiencing sufficient stress to make such disturbances detectable. Additionally, the control group had higher SES than the cancer group, which may have been protective. As developmental psychopathology research is often based on at-risk samples, and pediatric psychology research focuses on families undergoing significant illness or medically related stress, the control group, by comparison, may not have had as much risk. At minimum, lower variability in parental distress was observed within the control group.
There are several potential explanations for the associations found between parental and child distress in the cancer group. The experience of a life-threatening pediatric illness, such as cancer, may strengthen the link between parent and child functioning due to increased contact. Cancer-related illness and treatment typically require parents and their children to spend more time together than they might otherwise, for instance, if the children were in school and participating in normative activities instead. Moreover, they might share experiences (e.g., frequent medical visits and procedures) that elicit intense emotional reactions or sense of solidarity that could increase co-occurring distress within the dyad. This view is consistent with prior work hypothesizing that PTS may be transmitted within families with pediatric cancer (Bruce, 2006) and findings by Clawson, Jurbergs, Lindwall, & Phipps (2013) that parent and child reports of child PTS become concordant when they are based on the same event, such as the child’s cancer diagnosis. Also, children with cancer frequently view their parents as key sources of social support (Trask et al., 2003), which may increase the child's susceptibility to parental distress.
The experience of cancer may also strengthen the link between parental and child distress by creating disturbances within the parent–child relationship. Some parents of children diagnosed with cancer report increased family conflict (Pai et al., 2007), difficulty in managing the parenting role (Stewart & Mishel, 2000), and increased overprotection and indulgence of the child (Long & Marsland, 2011), and these changes can increase child maladjustment (McLeod, Wood et al., 2007; Pynoos et al., 1999). Additionally, transmission of distress may be affected by parental coping behaviors (Suzuki & Kato, 2003), such that distressed parents may have difficulties demonstrating and teaching effective coping behaviors to their children and inadvertently reinforce or fail to reduce child distress. This is not to say that families will necessarily be distressed, as many if not most families successfully adapt to changes brought about by a child's cancer diagnosis (McCubbin, Balling, Possin, Frierdich, & Bryne, 2002).
Although parents in the cancer group reported mildly increased distress relative to controls in the present study, children in the cancer group reported comparable levels of adjustment to the control group, and their mean symptom scores were comparable with or lower than those of normative validation samples. Thus, on average, children in the cancer group were not distressed, possibly because of an adaptive style of coping (Phipps, 2007; Phipps, Jurbergs, & Long, 2009) or a minimal impact of and successful adjustment to cancer diagnosis and treatment (Bonanno & Diminich, 2013). The low level of child distress may also have attenuated our findings. It should be noted, however, that children with cancer comprise a heterogeneous group, with different severity of illness and intensity of treatment, and small subsets of children in the cancer group may be experiencing clinically significant levels of distress.
Finally, the child's lifetime exposure to stressful life events was associated with child symptoms of depression, anxiety, and PTS, with medium effect sizes (rs = .30), for children with and without a history of cancer. Total exposure to life events was the only factor that had medium rather than small effect size in this study, thus it had a stronger influence on child adjustment than demographic or medical factors or parental distress. This finding is consistent with cumulative stress (e.g., Appleyard, Egeland, Dulmen, & Sroufe, 2005) and allostatic load (Juster etal., 2011) models of child maladjustment, which suggests that chronic and/or frequent exposure to significant environmental stress strongly influences child distress and that its effects may surpass the impact of any one type of stressor. Future studies may explore mechanisms by which life events influence child adjustment, possibly through studies of perceived impact or severity of these events or through prospective studies that assess for changes in child functioning after the occurrence of a life event. Of note, children in the cancer group reported approximately one more life event than those in the control group, which likely reflects the cancer experience, but the presence of this extra life event did not appear to increase the average level of distress found in the cancer group.
Moreover, in the cancer group, child exposure to life events moderated the effects of parental depression and distress severity on child distress. Exploration of this effect suggested that, the child's distress is more closely aligned with parental distress at lower levels of life events. At higher-than-mean levels of life events, the child was more distressed regardless of parental functioning. However, the interaction between parental distress and child exposure to life events explained only a small amount of variance (1–2%) out of the total variance in child distress that was accounted for by our models (17–32%). On the whole, direct effects of life events and demographic factors explained more variance, with parental distress accounting for ∼2–7% of the variance in child distress.
The present study has several limitations. The findings need to be replicated using samples from other pediatric treatment sites and regions, as the sample in this study was recruited from a single site and its surrounding community. Moreover, because the study used cross-sectional data, the direction of the influence between parental distress and child functioning could not be elucidated. Additionally, it is possible that the moderation effects explored in this study operate in the opposite direction, such that parental distress moderates the link between life events and child distress, but this could not be tested because of the cross-sectional nature of the data. Future research may use a longitudinal design to test a transactional model and to clarify the direction of the moderation effect.
More research examining specific processes and mechanisms that explain the effects found in this study are also needed (Drotar, 1997). For example, deterioration in parenting as evidenced by decreased consistency in discipline, overprotection, or withdrawal has been hypothesized as a potential mechanism by which increased parental distress contributes to child distress, but this need to be empirically tested. It is also possible that a deterioration in the family environment that could facilitate child adjustment to cancer diagnosis and treatment, such as family cohesion and expressiveness (Wallander & Varni, 1998), may be part of the mechanism that would link parent and child distress. Reporter effects also need to be taken into consideration, as life events were child reported. The associations found between child life events and child outcomes were likely strengthened by shared method variance. However, parent distress and child distress were captured using separate reporters, which represents a strength of this study. We were able to avoid inflating the findings based on shared method variance associated with the measurement of predictors and outcomes using the same reporter.
Conclusion
Parent distress, particularly in the form of depression, and severity of distress across a number of symptoms, appears to be linked to child distress in families of children with cancer. The child's cumulative exposure to stressful life events moderates this link, such that a significant relationship between parent and child distress is seen only with average or lower-than-average exposure to life events. An assessment of the child’s exposure to stressful life events may be a useful screen for identifying different approaches to the prevention of child maladjustment to cancer. For children who have faced numerous life stressors, direct intervention with the child may be indicated. In contrast, children with relatively low exposure to life events may be more sensitive to parental distress and thus benefit more from interventions targeting parental distress and parenting difficulties. To facilitate child adaptation following a cancer diagnosis, continued research on the influence of parental distress and prior adversities experienced by the child is warranted.
Funding
This research was supported in part by grants from the National Institutes of Health, R01 CA136782, and by the American Lebanese-Syrian Associated Charities (ALSAC).
Conflicts of interest: None declared.
References
- Appleyard K, Egeland B, Dulmen M, Sroufe L. When more is not better: The role of cumulative risk in child behavior outcomes. Journal of Child Psychology and Psychiatry. 2005;46:235–245. doi: 10.1111/j.1469-7610.2004.00351.x. doi:10.1111/j.1469-7610.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- Barratt W. The Barratt simplified measure of social status. 2006. Retrieved from http://socialclass-bpd.wikispaces.com/file/view/Barratt_Simplifed_Measure_of_Social_Status.pdf. [Google Scholar]
- Beardslee W R, Gladstone T R, O'Connor E E. Transmission and prevention of mood disorders among children of affectively ill parents: A review. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:1098–1109. doi: 10.1016/j.jaac.2011.07.020. doi:10.1016/j.jaac.2011.07.020. [DOI] [PubMed] [Google Scholar]
- Berg-Nielsen T S, Vikan A, Dahl A A. Parenting related to child and parental psychopathology: A descriptive review of the literature. Clinical Child Psychology and Psychiatry. 2002;7:529–552. doi:10.1177/1359104502007004006. [Google Scholar]
- Birmaher B, Brent D A, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. doi:10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Bonanno G A, Diminich E D. Annual Research Review: Positive adjustment to adversity – trajectories of minimal–impact resilience and emergent resilience. Journal of Child Psychology and Psychiatry. 2013;54:378–401. doi: 10.1111/jcpp.12021. doi:10.1111/jcpp.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce M. A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clinical Psychology Review. 2006;26:233–256. doi: 10.1016/j.cpr.2005.10.002. doi:10.1016/j.cpr.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Chaney J M, Mullins L L, Frank R G, Peterson L, Mace L D, Kashani J H. Transactional patterns of child, mother, and father adjustment in insulin-dependent diabetes mellitus: A prospective study. Journal of Pediatric Psychology. 1997;22:229–244. doi: 10.1093/jpepsy/22.2.229. [DOI] [PubMed] [Google Scholar]
- Clark C, Caldwell T, Power C, Stansfeld S A. Does the influence of childhood adversity on psychopathology persist across the lifecourse? A 45-year prospective epidemiologic study. Annals of Epidemiology. 2010;20:385–394. doi: 10.1016/j.annepidem.2010.02.008. doi:10.1016/j.annepidem.2010.02.008. [DOI] [PubMed] [Google Scholar]
- Clawson A H, Jurbergs N, Lindwall J, Phipps S. Concordance of parent proxy report and child self-report of posttraumatic stress in children with cancer and healthy children: Influence of parental posttraumatic stress. Psycho-Oncology. 2013;22:2593–2600. doi: 10.1002/pon.3321. doi:10.1002/pon.3321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coddington R D. The significance of life events as etiologic factors in the diseases of children: I. A survey of professional workers. Journal of Psychosomatic Research. 1972a;16:7–18. doi: 10.1016/0022-3999(72)90018-9. doi:10.1016/0022-3999(72)90018-9. [DOI] [PubMed] [Google Scholar]
- Coddington R D. The significance of life events as etiologic factors in the diseases of children-II: A study of a normal population. Journal of Psychosomatic Research. 1972b;16:205–213. doi: 10.1016/0022-3999(72)90045-1. doi:10.1016/0022-3999(72)90045-1. [DOI] [PubMed] [Google Scholar]
- Cohen M S. Families coping with childhood chronic illness: A research review. Families, Systems, and Health. 1999;17:149–164. doi:10.1037/h0089879. [Google Scholar]
- Cornelis M C, Nugent N R, Amstadter A B, Koenen K C. Genetics of post-traumatic stress disorder: Review and recommendations for genome-wide association studies. Current Psychiatry Reports. 2010;12:313–326. doi: 10.1007/s11920-010-0126-6. doi:10.1007/s11920-010-0126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings E, Davies P. Maternal depression and child development. Journal of Child Psychology and Psychiatry. 1994;35:73–122. doi: 10.1111/j.1469-7610.1994.tb01133.x. doi:10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- Currier J M, Jobe-Shields L E, Phipps S. Stressful life events and posttraumatic stress symptoms in children with cancer. Journal of Traumatic Stress. 2009;22:28–35. doi: 10.1002/jts.20382. doi:10.1002/jts.20382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis L, Melisaratos N. The brief symptom inventory: An introductory report. Psychological Medicine. 1983;13:595–605. doi:10.1017/S0033291700048017. [PubMed] [Google Scholar]
- Dolgin M J, Phipps S, Fairclough D L, Sahler O J Z, Askins M, Noll R B. Trajectories of adjustment in mothers of children with newly diagnosed cancer: A natural history investigation. Journal of Pediatric Psychology. 2007;32:771–782. doi: 10.1093/jpepsy/jsm013. [DOI] [PubMed] [Google Scholar]
- Drotar D. Relating parent and family functioning to the psychological adjustment of children with chronic health conditions: What have we learned? What do we need to know? Journal of Pediatric Psychology. 1997;22:149–165. doi: 10.1093/jpepsy/22.2.149. [DOI] [PubMed] [Google Scholar]
- Fergusson D M, Horwood L, Gretton M, Shannon F. Family life events, maternal depression, and maternal and teacher descriptions of child behavior. Pediatrics. 1985;75:30–35. [PubMed] [Google Scholar]
- Fisak B, Jr, Grills-Taquechel A E. Parental modeling, reinforcement, and information transfer: Risk factors in the development of child anxiety? Clinical Child and Family Psychology Review. 2007;10:213–231. doi: 10.1007/s10567-007-0020-x. doi:10.1007/s10567-007-0020-x. [DOI] [PubMed] [Google Scholar]
- Garber J, Cole DA. Intergenerational transmission of depression: A launch and grow model of change across adolescence. Development and Psychopathology. 2010;22:819–830. doi: 10.1017/S0954579410000489. doi:10.1017/S0954579410000489. [DOI] [PubMed] [Google Scholar]
- Goodman S H, Rouse M H, Connell A M, Broth M R, Hall C M, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. doi:10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Grant K E, Compas B E, Thurm A E, McMahon S D, Gipson P Y. Stressors and child and adolescent psychopathology: Measurement issues and prospective effects. Journal of Clinical Child and Adolescent Psychology. 2004;33:412–425. doi: 10.1207/s15374424jccp3302_23. doi:10.1207/s15374424jccp3302_23. [DOI] [PubMed] [Google Scholar]
- Halligan S, Murray L, Martins C, Cooper P. Maternal depression and psychiatric outcomes in adolescent offspring: A 13-year longitudinal study. Journal of Affective Disorders. 2007;97:145–154. doi: 10.1016/j.jad.2006.06.010. doi:10.1016/j.jad.2006.06.010. [DOI] [PubMed] [Google Scholar]
- Harland P, Reijneveld S, Brugman E, Verloove-Vanhorick S, Verhulst F. Family factors and life events as risk factors for behavioural and emotional problems in children. European Child and Adolescent Psychiatry. 2002;11:176–184. doi: 10.1007/s00787-002-0277-z. [DOI] [PubMed] [Google Scholar]
- Hayes A F, Matthes J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behavior Research Methods. 2009;41:924–936. doi: 10.3758/BRM.41.3.924. doi:10.3758/BRM.41.3.924. [DOI] [PubMed] [Google Scholar]
- Hettema J M, Neale M C, Kendler K S. A review and meta-analysis of the genetic epidemiology of anxiety disorders. American Journal of Psychiatry. 2001;158:1568–1578. doi: 10.1176/appi.ajp.158.10.1568. doi:10.1176/appi.ajp.158.10.1568. [DOI] [PubMed] [Google Scholar]
- Hoffman C, Crnic K, Baker J. Maternal depression and parenting: Implications for children's emergent emotion regulation and behavioral functioning. Parenting. 2006;6:271–295. doi:10.1207/s15327922par0604_1. [Google Scholar]
- Hollingshead A B. Four factor index of social status. New Haven, CT: Yale University Press; 1975. [Google Scholar]
- Holmbeck G N. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. doi:10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Johnston C A, Steele R G, Herrera E A, Phipps S. Parent and child reporting of negative life events: Discrepancy and agreement across pediatric samples. Journal of Pediatric Psychology. 2003;28:579–588. doi: 10.1093/jpepsy/jsg048. doi:10.1093/jpepsy/jsg048. [DOI] [PubMed] [Google Scholar]
- Juster R P, Bizik G, Picard M, Arsenault-Lapierre G, Sindi S, Trepanier L, Marin M, Wan N, Sekerovic Z, Lord C, Fiocco A J, Plusquellec P, McEwen B S, Lupien S J. A transdisciplinary perspective of chronic stress in relation to psychopathology throughout life span development. Development and Psychopathology. 2011;23:725–776. doi: 10.1017/S0954579411000289. doi:10.1017/S0954579411000289. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children's Depression Inventory (CDI) manual. North Tonawanda, NY: Multi-Health Systems, Inc; 1992. [Google Scholar]
- Landolt M A, Ystrom E, Sennhauser F H, Gnehm H E, Vollrath M E. The mutual prospective influence of child and parental post-traumatic stress symptoms in pediatric patients. Journal of Child Psychology and Psychiatry. 2012;53:767–774. doi: 10.1111/j.1469-7610.2011.02520.x. doi:10.1111/j.1469-7610.2011.02520.x. [DOI] [PubMed] [Google Scholar]
- Lavigne J V, Faier-Routman J. Correlates of psychological adjustment to pediatric physical disorders: A meta-analytic review and comparison with existing models. Journal of Developmental and Behavioral Pediatrics. 1993;14:117–123. doi:10.1097/00004703-199304000-00007. [PubMed] [Google Scholar]
- Lieb R, Isensee B, Höfler M, Pfister H, Wittchen H U. Parental major depression and the risk of depression and other mental disorders in offspring: A prospective-longitudinal community study. Archives of General Psychiatry. 2002;59:365–374. doi: 10.1001/archpsyc.59.4.365. doi:10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- Long K A, Marsland A L. Family adjustment to childhood cancer: A systematic review. Clinical Child and Family Psychology Review. 2011;14:57–88. doi: 10.1007/s10567-010-0082-z. doi:10.1007/s10567-010-0082-z. [DOI] [PubMed] [Google Scholar]
- Lovejoy M, Graczyk P, O'Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- McCubbin M, Balling K, Possin P, Frierdich S, Bryne B. Family resiliency in childhood cancer. Family Relations. 2002;51:103–111. doi:10.1111/j.1741-3729.2002.00103.x. [Google Scholar]
- McLeod B D, Weisz J, Wood J. Examining the association between parenting and childhood depression: A meta-analysis. Clinical Psychology Review. 2007;27:986–1003. doi: 10.1016/j.cpr.2007.03.001. doi:10.1016/j.cpr.2007.03.001. [DOI] [PubMed] [Google Scholar]
- McLeod B D, Wood J, Weisz J. Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review. 2007;27:155–172. doi: 10.1016/j.cpr.2006.09.002. doi:10.1016/j.cpr.2006.09.002. [DOI] [PubMed] [Google Scholar]
- Murray L, Creswell C, Cooper P. The development of anxiety disorders in childhood: An integrative review. Psychological Medicine. 2009;39:1413–1423. doi: 10.1017/S0033291709005157. doi:10.1017/S0033291709005157. [DOI] [PubMed] [Google Scholar]
- Pai A L, Greenley R N, Lewandowski A, Drotar D, Youngstrom E, Peterson C C. A meta-analytic review of the influence of pediatric cancer on parent and family functioning. Journal of Family Psychology. 2007;21:407–415. doi: 10.1037/0893-3200.21.3.407. doi:10.1037/0893-3200.21.3.407. [DOI] [PubMed] [Google Scholar]
- Phipps S. Adaptive style in children with cancer: Implications for a positive psychology approach. Journal of Pediatric Psychology. 2007;32:1055–1066. doi: 10.1093/jpepsy/jsm060. doi:10.1093/jpepsy/jsm060. [DOI] [PubMed] [Google Scholar]
- Phipps S, Jurbergs N, Long A. Symptoms of post-traumatic stress in children with cancer: Does personality trump health status? Psycho-Oncology. 2009;18:992–1002. doi: 10.1002/pon.1496. doi:10.1002/pon.1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pynoos R S, Rodriguez N, Steinberg A, Stuber M, Frederick C. The UCLA PTSD reaction index for DSM IV. Los Angeles, CA: Unpublished manual. UCLA Trauma Psychiatry Service; 1998. [Google Scholar]
- Pynoos R S, Steinberg A M, Piacentini J C. A developmental psychopathology model of childhood traumatic stress and intersection with anxiety disorders. Biological Psychiatry. 1999;46:1542–1554. doi: 10.1016/s0006-3223(99)00262-0. doi:10.1016/S0006-3223(99)00262-0. [DOI] [PubMed] [Google Scholar]
- Sawyer M G, Streiner D L, Antoniou G, Toogood I, Rice M. Influence of parental and family adjustment on the later psychological adjustment of children treated for cancer. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:815–822. doi: 10.1097/00004583-199808000-00011. doi:10.1097/00004583-199808000-00011. [DOI] [PubMed] [Google Scholar]
- Steinberg A, Brymer M, Decker K, Pynoos R S. The University of California at Los Angeles post-traumatic stress disorder reaction index. Current Psychiatry Reports. 2004;6:96–100. doi: 10.1007/s11920-004-0048-2. doi:10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Stewart J L, Mishel M H. Uncertainty in childhood illness: A synthesis of the parent and child literature. Research and Theory for Nursing Practice. 2000;14:299–319. [PubMed] [Google Scholar]
- Suzuki L K, Kato P M. Psychosocial support for patients in pediatric oncology: The influences of parents, schools, peers, and technology. Journal of Pediatric Oncology Nursing. 2003;20:159–174. doi: 10.1177/1043454203254039. doi:10.1177/1043454203254039. [DOI] [PubMed] [Google Scholar]
- Trask P C, Paterson A G, Trask C L, Bares C B, Birt J, Maan C. Parent and adolescent adjustment to pediatric cancer: Associations with coping, social support, and family function. Journal of Pediatric Oncology Nursing. 2003;20:36–47. doi: 10.1053/jpon.2003.5. doi:10.1053/jpon.2003.5. [DOI] [PubMed] [Google Scholar]
- Vrijmoet-Wiersma C J, van Klink J M, Kolk A M, Koopman H M, Ball L M, Egeler R M. Assessment of parental psychological stress in pediatric cancer: A review. Journal of Pediatric Psychology. 2008;33:694–706. doi: 10.1093/jpepsy/jsn007. [DOI] [PubMed] [Google Scholar]
- Wallander J L, Varni J W. Effects of pediatric chronic physical disorders on child and family adjustment. Journal of Child Psychology and Psychiatry. 1998;39:29–46. doi:10.1111/1469-7610.00302. [PubMed] [Google Scholar]
- Weiss D. The impact of event scale-revised. In: Wilson J, Keane T, editors. Assessing psychological trauma and PTSD. 2004. (2nd ed., pp. 168-189). New York: Guilford. [Google Scholar]
- Wood J, McLeod B D, Sigman M, Hwang W, Chu B. Parenting and childhood anxiety: Theory, empirical findings, and future directions. Journal of Child Psychology and Psychiatry. 2003;44:134–151. doi: 10.1111/1469-7610.00106. doi:10.1111/1469-7610.00106. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Bierer L M. Transgenerational transmission of cortisol and PTSD risk. Progress in Brain Research. 2007;167:121–135. doi: 10.1016/S0079-6123(07)67009-5. doi:10.1016/S0079-6123(07)67009-5. [DOI] [PubMed] [Google Scholar]
- Zatzick D, Russo J, Grossman D C, Jurkovich G, Sabin J, Berliner L. Posttraumatic stress and depressive symptoms, alcohol use, and recurrent traumatic life events in a representative sample of hospitalized injured adolescents and their parents. Journal of Pediatric Psychology. 2006;31:377–387. doi: 10.1093/jpepsy/jsj056. doi:10.1093/jpepsy/jsj056. [DOI] [PubMed] [Google Scholar]