Abstract
Pickardt syndrome (Pickardt-Fahlbusch syndrome) is a rare congenital syndrome characterized by tertiary hypothyroidism caused by the interruption of the portal veins between hypothalamus and adenohypophysis. Typical features of this syndrome are tertiary hypothyroidism with low thyroid stimulating hormone, hyperprolactinemia and other pituitary hormone deficiencies. Pituitary stalk interruption syndrome is characterized by a triad of thin or interrupted pituitary stalk, aplasia or hypoplasia of the anterior pituitary and absent or ectopic posterior pituitary (EPP) seen on magnetic resonance imaging (MRI). It is a congenital anomaly of pituitary whose exact prevalence is unknown. In some cases, it is restricted to EPP or pituitary stalk interruption. We are presenting the case history along with MRI finding of three children's who presented with short stature and delayed puberty.
Keywords: Delayed puberty, ectopic posterior pituitary, multiple pituitary hormones deficiency, pituitary stalk interruption syndrome
Introduction
Pituitary stalk interruption syndrome (PSIS) is a rare entity with an estimated incidence rate of 0.5/1,000,000 births.[1] PSIS are characterized by the presence of a thin or absent pituitary stalk, associated hypoplastic or aplastic anterior pituitary and ectopic posterior pituitary (EPP) on magnetic resonance imaging (MRI).[2] This can be associated with midline defects and various pituitary endocrine deficiencies, ranging from isolated growth hormone deficiency (IGHD) to combined pituitary hormone deficiency (CPHD).[3] The endocrine outcome seems to be a progressive onset of hormone deficiencies leading to panhypopituitarism, but posterior pituitary function is usually maintained, occasionally it may be disturbed depending on the position of the posterior pituitary.[4] PSIS is also associated with higher than normal frequency of breech presentation, difficult delivery, or the consequence of adverse perinatal factors such as birth trauma, prolonged labor, or forceps delivery is unclear.[5] Later in childhood, children may present with short stature, decreased growth rate, seizures, hypotension, intellectual delay and delayed puberty.
Case Reports
Case 1
A 15-year-old boy presented for the evaluation of short stature and delayed puberty in our outpatient department (OPD). Parents noticed that the child is not growing well as compared to his peers, and also noted that the child has not developed any sign of puberty in the form of the moustache, beard growth, pubic hair and scrotal growth. He has been well with no chronic medical problems, no hospitalizations, and no surgeries. The child is a product of nonconsanguineous marriage and uneventful 8 months vaginal delivery in the hospital with breech presentation. The child had a history of birth asphyxia and cried 10 min after birth. There were no history of feeding difficulties, seizures, neonatal jaundice, lactose intolerance; developmental milestones - gross motor, fine motor, social delay. The child is average in studies at school. Social, family and peer interactions are normal and no behavioral problems. The child has two elder siblings with normal growth and development. There is no such history in family members and relatives.
Examination
Height: 126.5 cm (<3rd percentile), standard deviation: 8.0, standard deviation score: 4.75, lower segment (LS): 64 cm, upper segment (US): 64 cm, US/LS: 1.0, arm span (AS): 128 cm, weight: 30.7 kg, miles per hour (MPH): 160.0 cm, corrected MPH: 166.5 cm, Tanner's score: A1P1 TV < 4 ml (bilaterally), stretch penile length (SPL): <4 cm, fundus examination: Within normal limits (WNL).
Investigations
His growth chart showed an average growth velocity of 3 cm/year. Complete blood count (CBC), erythrocyte sedimentation rate (ESR), thyroid function tests (TFT's), urinalysis (UA), and serum electrolytes are normal. Hormonal analysis shows thyroid stimulating hormone (TSH): 3.80 μIU/ml (N = 0.4–5.0 μIU/ml), T4: 2.90 μg/dl (N = 5–12 μg/dl), follicle-stimulating hormone (FSH) (basal): 0.98 mIU/ml (N = 1-10 mIU/ml), luteinizing hormone (LH) (basal): 0.12 mIU/ml (N = 2-8 mIU/ml), prolactin: 50.46 ng/dl (N = 2-15 ng/dl), fasting morning cortisol: 1.5 μg/dl (N = 5-25 μg/dl), testosterone: <0.45 nmol/L (N = 10-35 nmol/L), growth hormone (GH) stimulation test (Insulin): <0.05 ng/ml (normal > 10 ng/ml), X-ray hand (T2-weighted): 7.4 years (bone age). MRI brain: Anterior pituitary hypoplasia, EPP and absent pituitary stalk [Figures 1 and 2].
Figure 1.
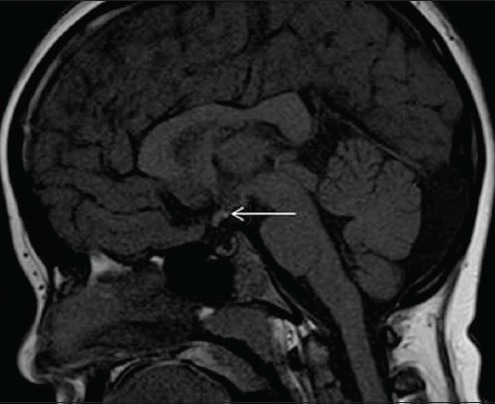
Sagittal T1-weighted image shows ectopic posterior pituitary (white arrow), stalk not visualized
Figure 2.

Postcontrast coronal T1-weighted image – pituitary stalk not visualised (note ectopic posterior pituitary-white arrow)
Case 2
An 11-year-old boy presented in our OPD for the evaluation of short stature, parents reported that he had always been the shortest boy in his class, but they become concerned about his height when they noticed that a neighboring 7-year-old boy was having the same height as their boy. The child has not yet attained any sign of puberty. He has been well with no chronic medical problems, no hospitalizations, and no surgeries. He is currently a student in the seventh grade, and he is shortest in his class. His mother is 173 cm and weighs 68 kg. She attained menarche at age 12. The patient's father is 185 cm and weighs 70 kg. He started shaving at age 15. There is no family history of any medical problems.
Examination
Height: 104 cm (<3rd percentile), AS: 106 cm, LS: 54 cm, US: 52 cm, US/LS: 0.96, weight 17.7 kg (<3rd percentile), MPH: 153.0 cm, corrected MPH: 159.5 cm, Tanner's score: A1P1 TV < 4 ml (bilaterally), SPL: <3 cm, fundus examination: WNL.
Investigations
His growth chart showed an average growth velocity of 3.5 cm/year. CBC, ESR, TFT's, UA, and serum electrolytes are normal. Hormonal analysis shows TSH: 2.48 μIU/ml (N = 0.4-5.0 μIU/ml), T4: 3.48 μg/dl (N = 5-12 μg/dl), FSH (basal): 0.71 mIU/ml (N = 1-10 mIU/ml), LH (basal): 0.08 mIU/ml (N = 2-8 mIU/ml), prolactin: 37.8 ng/dl (N = 2-15 ng/dl), fasting morning cortisol: 2.8 μg/dl (N = 5-25 μg/dl), testosterone: <0.45 nmol/L (N = 10-35 nmol/L), GH stimulation test (insulin): <0.05 ng/ml (normal > 10 ng/ml), X-ray hand (T2-weighted): 6.3 years (bone age). MRI brain: Small adenohypophysis measuring 2.9 mm, [Figure 3] thin and truncated pituitary stalk measuring 1.2 mm with normal neurohypophysis.
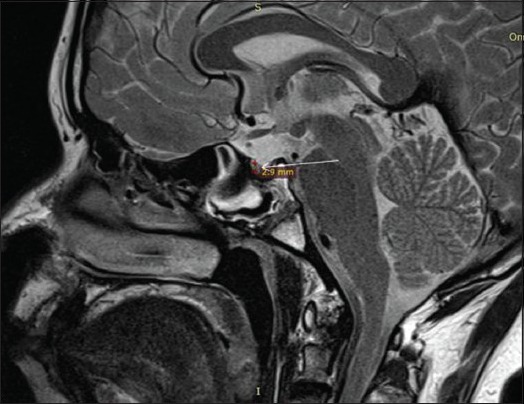
Figure 3.

Sagittal T2-weighted image showing small anterior pituitary measuring 2.9 mm in height (black arrow)
Case 3
An 18-year-old boy presented in our OPD for the evaluation of short stature and delayed puberty. The child has not yet attained any sign of puberty. He has been well with no chronic medical problems, no hospitalizations, and no surgeries. There is no family history of any medical problems.
Examination
Height: 124 cm (<3rd percentile), weight 24.6 kg (<3rd percentile), corrected MPH: 160.5 cm, Tanner's score: A1P1 TV < 4 ml (bilaterally), SPL: <3 cm, fundus examination: WNL.
Investigations
His growth chart showed an average growth velocity of < 3.5 cm/year. CBC, ESR, TFT's, UA, and serum electrolytes are normal. Hormonal analysis shows TSH: 3.48 μIU/ml (N = 0.4-5.0 μIU/ml), T4: 2.18 μg/dl (N = 5-12 μg/dl), FSH (basal): 0.56 mIU/ml (N = 1-10 mIU/ml), LH (basal): 0.12 mIU/ml (N = 2-8 mIU/ml), prolactin: 46.2 ng/dl (N = 2-15 ng/dl), fasting morning cortisol: 2.4 μg/dl (N = 5-25 μg/dl), testosterone: <0.45 nmol/L (N = 10-35 nmol/L), GH stimulation test (Insulin): <0.05 ng/ml (>10 ng/ml), X-ray hand (T2-weighted): 6.3 years (bone age). MRI brain: Small adenohypophysis measuring 2.9 mm, absent pituitary stalk with ectopic neurohypophysis [Figures 4–6].
Figure 4.
Sagittal T2-weighted image showing anterior pituitary measuring 2.9 mm in height (white arrow)
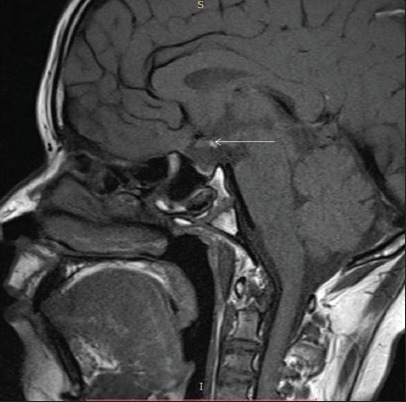
Figure 6.

Midline Sagittal T2-weighted image – pituitary stalk not visualized (white arrow)
Figure 5.
Sagittal T1-weighted image showing ectopic posterior pituitary bright spot (white arrow)
Discussion
Pituitary stalk interruption syndrome was firstly reported by Fujisawa et al. in 1987.[6] PSIS has a male predominance with a male, female sex ratio between 2.3 and 6.9:1,[3,4,7,8,9,10] pointing on X-linked inheritance. Mean age at diagnosis is 9.4 ± 11.6 years with no effect of neonatal distress and breech delivery on the age of presentation.[4]
The cause of PSIS is still unknown and many theories are proposed like perinatal injuries, defective organogenesis due to genetic or environmental factors during pregnancy.[3,11,12] Rare mutations of HESX1, LH4, OTX3 and SOX3 can be the cause of PSIS in familial cases.[4] PSIS are generally of hypothalamic origin having different pathogenesis in IGHD and CPHD.[4] According to current view mode of delivery and/or neonatal hypoxemia are not the cause of PSIS, but are direct or indirect consequence of the hypothalamic-pituitary lesion.[4]
In a large Chinese study of 55 patients, short stature was found in 85.5% patients with bone age delay of 7.26 ± 5.37 years. The prevalence of various hormonal deficiencies was 100% for GH, 95.8% for gonadotropins, 81.8% for corticotrophin and 76.3% for thyrotropin. Hyperprolactinemia was found in 36.4%. More than two anterior pituitary hormone deficiencies were found in 92.7% cases.[10]
Location of EPP has functional prognostic significance with a greater number of anterior pituitary hormone deficiencies when posterior pituitary is present at the median eminence or hypothalamic region.[9] The capacity of the anterior pituitary to respond to stimulation tests using hypothalamic releasing hormones depend on the cause of PSIS, the volume of pituitary and age of presentation.[4]
In our study, three male children present in growth clinic of endocrine OPD with complaints of short stature and inability to attain puberty. There is history of nonintuitional vaginal deliveries at home, with breech presentation and with birth asphyxia. There is no significant past and family history. On examination all the patients have height and weight < 3rd percentile for their age, have no signs of puberty and have micropenis. On investigation, all the patients have CPHD along with delayed bone age. T2-weighted and gadolinium enhanced MRI brain is suggestive of hypoplastic adenohypophysis with EPP and absent stalk. On the basis of these findings, the diagnosis of PSIS was made, and patients were started on hormonal replacement therapy.
Acknowledgments
We owe thanks to the patient and their relatives for having patience and their contribution to this undertaking.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.El Chehadeh-Djebbar S, Callier P, Masurel-Paulet A, Bensignor C, Méjean N, Payet M, et al. 17q21.31 microdeletion in a patient with pituitary stalk interruption syndrome. Eur J Med Genet. 2011;54:369–73. doi: 10.1016/j.ejmg.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Simmons GE, Suchnicki JE, Rak KM, Damiano TR. MR imaging of the pituitary stalk: Size, shape, and enhancement pattern. AJR Am J Roentgenol. 1992;159:375–7. doi: 10.2214/ajr.159.2.1632360. [DOI] [PubMed] [Google Scholar]
- 3.Tauber M, Chevrel J, Diene G, Moulin P, Jouret B, Oliver I, et al. Long-term evolution of endocrine disorders and effect of GH therapy in 35 patients with pituitary stalk interruption syndrome. Horm Res. 2005;64:266–73. doi: 10.1159/000089425. [DOI] [PubMed] [Google Scholar]
- 4.Pinto G, Netchine I, Sobrier ML, Brunelle F, Souberbielle JC, Brauner R. Pituitary stalk interruption syndrome: A clinical-biological-genetic assessment of its pathogenesis. J Clin Endocrinol Metab. 1997;82:3450–4. doi: 10.1210/jcem.82.10.4295. [DOI] [PubMed] [Google Scholar]
- 5.Rona RJ, Tanner JM. Aetiology of idiopathic growth hormone deficiency in England and Wales. Arch Dis Child. 1977;52:197–208. doi: 10.1136/adc.52.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fujisawa I, Kikuchi K, Nishimura K, Togashi K, Itoh K, Noma S, et al. Transection of the pituitary stalk: Development of an ectopic posterior lobe assessed with MR imaging. Radiology. 1987;165:487–9. doi: 10.1148/radiology.165.2.3659371. [DOI] [PubMed] [Google Scholar]
- 7.Maghnie M, Larizza D, Triulzi F, Sampaolo P, Scotti G, Severi F. Hypopituitarism and stalk agenesis: A congenital syndrome worsened by breech delivery? Horm Res. 1991;35:104–8. doi: 10.1159/000181883. [DOI] [PubMed] [Google Scholar]
- 8.Arrigo T, Wasniewska M, De Luca F, Valenzise M, Lombardo F, Vivenza D, et al. Congenital adenohypophysis aplasia: Clinical features and analysis of the transcriptional factors for embryonic pituitary development. J Endocrinol Invest. 2006;29:208–13. doi: 10.1007/BF03345541. [DOI] [PubMed] [Google Scholar]
- 9.Chen S, Léger J, Garel C, Hassan M, Czernichow P. Growth hormone deficiency with ectopic neurohypophysis: Anatomical variations and relationship between the visibility of the pituitary stalk asserted by magnetic resonance imaging and anterior pituitary function. J Clin Endocrinol Metab. 1999;84:2408–13. doi: 10.1210/jcem.84.7.5849. [DOI] [PubMed] [Google Scholar]
- 10.Guo Q, Yang Y, Mu Y, Lu J, Pan C, Dou J, et al. Pituitary stalk interruption syndrome in Chinese people: Clinical characteristic analysis of 55 cases. PLoS One. 2013;8:e53579. doi: 10.1371/journal.pone.0053579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melo ME, Marui S, Carvalho LR, Arnhold IJ, Leite CC, Mendonça BB, et al. Hormonal, pituitary magnetic resonance, LHX4 and HESX1 evaluation in patients with hypopituitarism and ectopic posterior pituitary lobe. Clin Endocrinol (Oxf) 2007;66:95–102. doi: 10.1111/j.1365-2265.2006.02692.x. [DOI] [PubMed] [Google Scholar]
- 12.Simon D, Hadjiathanasiou C, Garel C, Czernichow P, Léger J. Phenotypic variability in children with growth hormone deficiency associated with posterior pituitary ectopia. Clin Endocrinol (Oxf) 2006;64:416–22. doi: 10.1111/j.1365-2265.2006.02484.x. [DOI] [PubMed] [Google Scholar]


