Abstract
Background and Aims:
With the expanding use of diagnostic and therapeutic radiological modalities in critically ill patients, doctors working in Intensive Care Units (ICUs) are increasingly exposed to ionizing radiation. This risk of radiation exposure occurs not only during bedside radiologic procedures, but also when ICU physicians accompany patients to radiology suites. The aim of this study was to quantify levels of radiation exposure among medical professionals working in the ICU.
Materials and Methods:
The study was carried out prospectively over 6 months in the ICU of a tertiary-referral cancer hospital. Two teams consisting of 4 ICU resident doctors each were instructed to wear thermoluminescent dosimeters (TLDs) during their duty shifts. Standard radiation protection precautions were used throughout the study period. TLDs were also placed in selected areas of the ICU to measure the amount of scattered radiation. TLDs were analyzed at the end of every 3 months.
Results:
The readings recorded on TLDs placed in the ICU were almost immeasurable. The mean value of residents' radiation exposure was 0.059 mSv, though the highest individual reading approached 0.1 mSv. The projected maximum yearly radiation exposure was 0.4 mSv.
Conclusions:
If standard radiation safety precautions are followed, the cumulative radiation exposure to ICU resident doctors is well within permissible limits and is not a cause of concern. However, with the increasing use of radiological procedures in the management of critically ill patients, there is a need to repeat such audits periodically to monitor radiation exposure.
Keywords: Dosimetry, Intensive Care Unit, occupational exposure
Introduction
Radiological investigations and therapeutics have become an integral part of the management of critically ill patients in the Intensive Care Unit (ICU). Patients admitted to the ICU routinely undergo bedside imaging procedures such as chest radiographs for diagnosing heart, lung and other pathology, and for confirmation of the position of devices like endotracheal tubes, nasogastric tubes, central venous catheters and intercostal drains. A review article has suggested that among ICU patients, up to 65% of daily chest radiographs and 70-75% of chest computerized tomography (CT) scans reveal significant or unsuspected abnormalities that may lead to a change in the patient's management.[1,2] Further, critically ill patients are frequently transported to the CT scan as well as digital subtraction angiography suites for diagnostic and therapeutic procedures such as angiography, embolization and stenting. In most situations, the ICU team is responsible for the transport and management of the patient in the radiology department for these procedures. This can significantly increase the cumulative radiation exposure to ICU personnel. There is, therefore, potential radiation exposure to healthcare workers, particularly for those working for long periods of time in the ICU. Epidemiological data indicates that the exposure to even low-dose radiation may be a cause for concern because such exposure can result in leukemia, thyroid malignancies and other cancers.[3] Nonneoplastic effects of radiation include genetic mutation and developmental malformation in children whose mothers were exposed to radiation during pregnancy.[3] A number of studies have looked at radiation exposure in critically ill patients undergoing repeated radiological procedures.[4,5] One study has specifically focused on the pediatric age group probably in view of the high ratio of exposure to patient size and the potential for long-term sequelae as the radiation effects have a longer period to become manifest.[6] However, the available literature on the extent of radiation exposure to ICU personnel is scarce and relates mainly to the level of scattered radiation within the ICU.[7,8] The conclusion of these studies is that the level of radiation exposure is extremely low and does not pose a hazard to ICU personnel.[7,8] None of these studies have considered the additional radiation exposure to ICU personnel involved in the management of critically ill patients in the Radiology Department.
In our ICU in a tertiary care cancer referral center, resident doctors working on 12 h shifts in the ICU are also responsible for the transport and management of ICU patients when they undergo diagnostic and therapeutic procedures in the Radiology Department. We, therefore, carried out this study to determine the total radiation exposure to ICU resident doctors involved in the course of their duties.
Materials and Methods
We conducted a prospective, observational study in the ICU and postanesthesia care unit (PACU) of a 500-bedded tertiary care cancer referral center in Mumbai, India from September 2012 to February 2013. The study was approved by the hospital's institutional ethics committee. All resident doctors who gave voluntary written consent to participate in the study were included. Since the study did not involve patient contact, the requirement for obtaining consent from patients was waived by the ethics committee. The study was carried out in accordance with the principles of good clinical research practice.
The resident doctors provide 24 h cover, working in 12 h shifts, with four doctors in each shift. In each shift, these four doctors work in two locations. On one floor, the ICU has a total of 14 beds as shown in Figure 1. On another floor is the PACU with 23 beds, subdivided into 14 postoperative recovery room beds and 9 intensive care beds [Figure 2]. Each resident has 3 days off work in a 2 week period. Residents provide care for patients in the ICU and PACU and also accompany patients from these locations for radiological procedures in the CT scan or interventional radiology suites.
Figure 1.
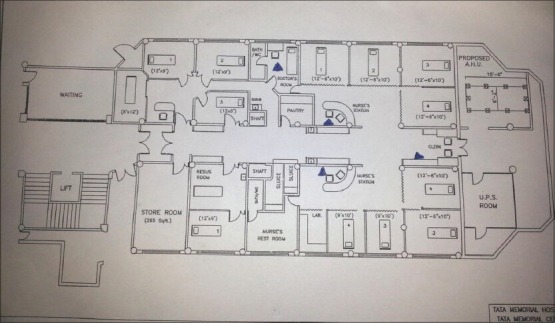
Layout of 14 bedded Intensive Care Unit. Location of thermoluminescent dosimeters are shown with filled triangles
Figure 2.
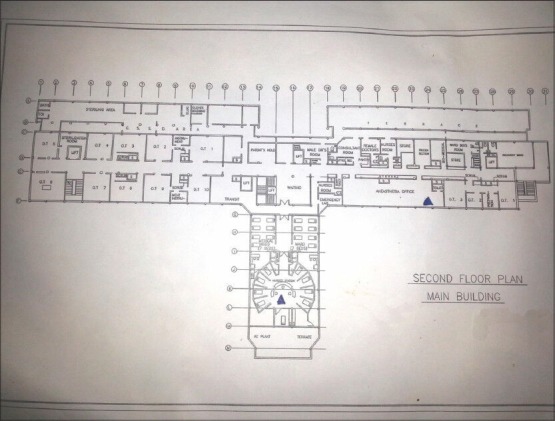
Layout of postanesthesia care unit showing location of thermoluminescent dosimeter in PACU (TLD surrounded by beds) and other in long lobby as control TLD
To detect levels of radiation, we used thermoluminescent dosimeters (TLDs) which are a type of radiation detector. The TLD measures cumulative dose of ionizing radiation exposure by measuring the amount of visible light emitted from a crystal in the detector when the crystal is heated. The amount of light emitted is dependent upon the amount of radiation exposure. TLDs can measure a wide dosimetric range (from 10 μGray to 10 Grays) of radiation exposure[9] and are routinely used as personal dosimeters because they are small in size, convenient to use and not expensive.[10] A TLD was given to each of the four resident doctors; they were handed over to the next team during shift changeover. In addition, three TLDs were kept in nursing stations in ICU, and one TLD was placed in the PACU. One TLD was kept in the doctors' duty room which was within the premises of the ICU, and the last was kept as a control in the office of the department of anesthesia, critical care and pain, remote from ICU and PACU, and where no radiological procedures were performed. Thus, a total of ten TLDs were used in the study. Each of the TLDs was numbered for easy identification and for analysis. The layout of ICU and PACU is represented by Figures 1 and 2 respectively and locations of TLDs are marked with filled triangles.
The participating resident doctors were instructed to wear the TLDs at all times during their duty hours. Standard radiation protection precautions were practiced throughout the study period. Staff not required to be present during radiographic procedures were kept at least 3 m away from the patient (a distance at which exposure from scattered radiation is considered negligible).[7] It was ensured that patients who were shifted from ICU to the radiology suite were accompanied by one ICU resident and that the resident was wearing his TLD throughout. Residents, if required to be directly involved in the radiologic procedure in suites, wore lead aprons, and the TLD was underneath the lead apron.
Bedside chest X-rays in the ICU were done by Siemens Multimobil 2.5 (Manufactured by Siemens Ltd, Goa, India), CT and CT guided biopsies were performed on Siemens Somatom Emotion 16 (manufactured by Siemens Shanghai medical equipments Ltd, Shanghai China) and GE light speed 16 (Manufactured by General Electric Co., Milwaukee, USA) respectively. Interventional radiology procedures were carried out using GE Innova 4100 IQ (Manufactured by GE Medical Systems, France).
The study was carried out in two phases of 3 months each. At the end of the first phase, the TLDs were handed over to Department of Nuclear Medicine for analysis and another set of TLDs was issued at the same time. During the period of the study, we maintained a database of procedures performed both in the ICU and in the radiological suites along with the bed number and the patient's hospital registration number.
The primary outcome of this study was to quantify the cumulative radiation exposure to the resident doctors working in the ICU over a period of 6 months in the course of their duties. The secondary outcomes were to measure the cumulative scattered radiation exposure in various areas of the ICU calculated as the average of readings of ICU TLD badges over 6 months and the estimated cumulative radiation exposure to the resident doctors per year.
Results
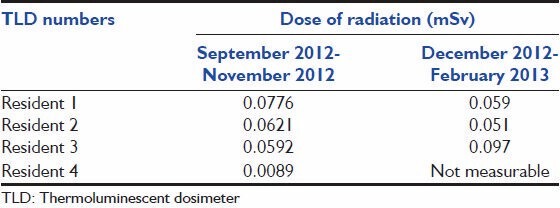
Table 1 summarizes the procedures performed during the study period. The control TLD placed in the Department of Anesthesia served as a measure of baseline atmospheric ionizing radiation, and all other values are reported above this baseline. The results of dosimetric analysis of residents TLDs during the two phases are shown in Table 2. Readings from TLDs placed in the nursing station and doctors' duty room during both phases were immeasurable. The mean value of residents' radiation exposure was 0.059 mSv. The mean values in the first and last 3 months were 0.052 and 0.069 mSv respectively, though the highest individual value approached 0.1 mSv. Since this was recorded in a 3 month period, the projected reading for similar exposure throughout the year, even assuming a 24 h duty period, would be 0.4 mSv, which is well below the safety limit of 20 mSv/year.[11]
Table 1.
Radiodiagnostic and therapeutic procedures during the study
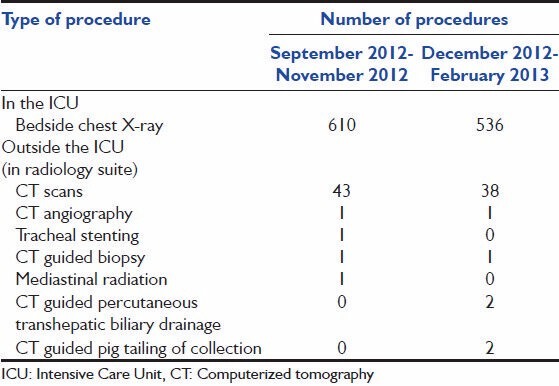
Table 2.
Dose of radiation received by residents
Discussion
Revolutionary progress in the field of medical imaging has given a big leap to advances in medical diagnostics and therapeutics. This development has also infiltrated the field of critical care medicine, and radio-diagnosis and interventional radiological procedures now play a key role in the management of critically ill patients. While this advancement offers the advantages of rapid bedside diagnosis, and cost-effective and minimally invasive treatment options to critically ill patients, it carries the danger of exposure of patient and physician to radiation. The detrimental effects of exposure to even low-level ionizing radiation have always been known; however, there is renewed concern because of its wide-spread use in medical radio-diagnosis and therapeutics in critically ill patients. It is, therefore, natural that there may be concerns about the long-term effects of radiation exposure to doctors working for long periods of time in the ICU. In addition, where ICU doctors are responsible for transport of patients to the radiology suite, the extent of radiation exposure is increased. It is reassuring that the results of our study confirm that the extent of radiation exposure to critical care physician during the course of his duty is well within acceptable limits.
There is considerable literature on occupational hazards of radiation exposure among radiologists; however, it is difficult to directly extrapolate the conclusions of these studies to the ICU.[12,13,14] Working conditions in the ICU do not mimic those in radiology suites-working hours tend to be long, there is a need to accompany mechanically ventilated and hemodynamically unstable patients inside the radiology suite for procedures, and ICU doctors may sometimes take radiation safety norms lightly. Few previous studies have looked at radiation exposure among ICU personnel. A study performed in a trauma ICU (TICU) has concluded that radiation exposure is not a significant occupational hazard for the TICU personnel.[7] Similarly, another study looked into the radiation exposure to ICU nurses and found that the exposure was well below the permissible level.[8] The findings of our study have reiterated the results of these previous studies.
The strength of our study is that it was planned in a more pragmatic way - apart from bedside radiological procedures, we also took into account the radiation exposure to ICU residents accompanying the patient to radiological suites for diagnostic and therapeutic procedures. Ionizing radiation from fluoroscopy in the CT scan or interventional radiology suites may be significant and were not considered in the previous studies. We also tried to measure the amount of scattered radiation within the ICU and the PACU, which contributes to overall radiation exposure. Even after taking these additional sources of radiation exposure into account, we found that the cumulative radiation exposure was negligible.
Our study has some limitations. The number and types of bedside and out-of-ICU radiological procedures can vary on a day-to-day basis according to the case-mix of the ICU population, and this may affect the overall radiation exposure; however, this study was carried out over a period of 6 months, and the data obtained would have been adequately representative. The other limitation relates to the generalizability of the study; differences in the types of cases, working pattern of resident doctors, quality and maintenance of radiological equipment between hospitals may restrict the applicability of these results to other hospitals. However, given the large margin of safety that our study has shown, it is unlikely that exposure levels would be dangerously high in any other setting. Though, with advances in technology, the number and types of radiological procedures performed on patients are likely to increase. Furthermore, there is a growing trend toward using radionuclide-based positron emission tomography scans for diagnostic procedures in critically ill patients especially when they are admitted to ICU during their diagnostic work-up. Some of these patients may continue to emit radiation long after their procedures are completed. Though none of these patients featured in our study, it will add to the radiation exposure to doctors.
The results of this study do not in any way underrate the need to follow safety precautions, while carrying out radiological procedures in critically ill patients. The levels of exposure found in this study should be interpreted bearing in mind that standard protection norms were used by all personnel involved in the study. With these precautions in place, radiation exposure to doctors managing critically ill patients in the ICU is minimal and acceptable.
Conclusions
Literature on radiation exposure among ICU doctors is scarce. In addition to bedside radiological procedures, the risk of exposure may be increased if the same doctors accompany ICU patients for out-of - ICU radiological investigations. However, we found that if standard safety precautions were followed, cumulative radiation exposure to ICU resident doctor was well within permissible limits and was not the cause of concern and hence routine personal dosimetric monitoring is not needed for residents in ICU. However, in view of changing practice, there is a need to repeat such audits periodically to monitor radiation exposure.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Trotman-Dickenson B. Radiology in the intensive care unit (Part I) J Intensive Care Med. 2003;18:198–210. doi: 10.1177/0885066603251897. [DOI] [PubMed] [Google Scholar]
- 2.Trotman-Dickenson B. Radiology in the intensive care unit (part 2) J Intensive Care Med. 2003;18:239–52. doi: 10.1177/0885066603254087. [DOI] [PubMed] [Google Scholar]
- 3.Al-Lamki L. Radiation Exposure from Medical Imaging: A Wake-up Call for Oman! Sultan Qaboos. Univ Med J. 2011;11:1–4. [PMC free article] [PubMed] [Google Scholar]
- 4.Kim PK, Gracias VH, Maidment AD, O'Shea M, Reilly PM, Schwab CW. Cumulative radiation dose caused by radiologic studies in critically ill trauma patients. J Trauma. 2004;57:510–4. doi: 10.1097/01.ta.0000141028.97753.67. [DOI] [PubMed] [Google Scholar]
- 5.Rohner DJ, Bennett S, Samaratunga C, Jewell ES, Smith JP, Gaskill-Shipley M, et al. Cumulative total effective whole-body radiation dose in critically ill patients. Chest. 2013;144:1481–6. doi: 10.1378/chest.12-2222. [DOI] [PubMed] [Google Scholar]
- 6.Kim PK, Zhu X, Houseknecht E, Nickolaus D, Mahboubi S, Nance ML. Effective radiation dose from radiologic studies in pediatric trauma patients. World J Surg. 2005;29:1557–62. doi: 10.1007/s00268-005-0106-x. [DOI] [PubMed] [Google Scholar]
- 7.Mostafa G, Sing RF, McKeown R, Huynh TT, Heniford BT. The hazard of scattered radiation in a trauma intensive care unit. Crit Care Med. 2002;30:574–6. doi: 10.1097/00003246-200203000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Cupitt JM, Vinayagam S, McConachie I. Radiation exposure of nurses on an intensive care unit. Anaesthesia. 2001;56:183. doi: 10.1046/j.1365-2044.2001.01870.x. [DOI] [PubMed] [Google Scholar]
- 9.Khan FM, Doppke KP, Hogstrom KR, Kutcher GJ, Nath R, Prasad SC, et al. Clinical electron-beam dosimetry: Report of AAPM Radiation Therapy Committee Task Group No 25. Med Phys. 1991;18:73–109. doi: 10.1118/1.596695. [DOI] [PubMed] [Google Scholar]
- 10.Izewska J, Rajan G. Radiation dosimeters. In: Podgorsak EB, editor. Radiation Oncology Physics: A Handbook for Teachers and Students. Vienna: IAEA; 2005. pp. 71–99. [Google Scholar]
- 11.Bajaj SS. Atomic Energy Regulatory Board, Government of India. AERB Directive No. 01/2011 [Under Rule 15 of the Atomic Energy (Radiation Protection) Rules 2004] 2011. Apr 27, [Last accessed on 2013 Dec 09]. http://www.aerb.gov.in/AERBPortal/pages/English/Constitution/directives_jsp.action .
- 12.Sánchez RM, Vano E, Fernández JM, Rosales F, Sotil J, Carrera F, et al. Staff doses in interventional radiology: A national survey. J Vasc Interv Radiol. 2012;23:1496–501. doi: 10.1016/j.jvir.2012.05.056. [DOI] [PubMed] [Google Scholar]
- 13.Niklason LT, Marx MV, Chan HP. Interventional radiologists: Occupational radiation doses and risks. Radiology. 1993;187:729–33. doi: 10.1148/radiology.187.3.8497622. [DOI] [PubMed] [Google Scholar]
- 14.Al-Abdulsalam A, Brindhaban A. Occupational radiation exposure among the staff of departments of nuclear medicine and diagnostic radiology in Kuwait. Med Princ Pract. 2014;23:129–33. doi: 10.1159/000357123. [DOI] [PMC free article] [PubMed] [Google Scholar]


