Abstract
With the advent of cardiopulmonary resuscitation techniques, the cardiopulmonary definition of death lost its significance in favor of brain death. Brain death is a permanent cessation of all functions of the brain in which though individual organs may function but lack of integrating function of the brain, lack of respiratory drive, consciousness, and cognition confirms to the definition that death is an irreversible cessation of functioning of the organism as a whole. In spite of medical and legal acceptance globally, the concept of brain death and brain-stem death is still unclear to many. Brain death is not promptly declared due to lack of awareness and doubts about the legal procedure of certification. Many brain dead patients are kept on life supporting systems needlessly. In this comprehensive review, an attempt has been made to highlight the history and concept of brain death and brain-stem death; the anatomical and physiological basis of brain-stem death, and criteria to diagnose brain-stem death in India.
Keywords: Brain death, brain-stem death, coma, consciousness, transplantation of human organs act
Introduction
The concept of Brain death and brain-stem death, its relevance to organ donation and its legal implications are new to most of the general population and are still unclear to many medical students and practitioners.[1,2,3,4] India enacted a law in 1994 to legalize brain-stem death .[5,6] Most of the Indian states have passed this act in their assemblies; however, a few state have yet to accept it. In addition, the state of Maharashtra has recently mandated the notification of brain dead cases.[7] Here, an attempt has been made to elaborate the history and concept of brain death and brain-stem death, the anatomy, physiology and pathophysiology of brain-stem death, and clinical criteria and tests required medically and legally to diagnose brain-stem death.
Historical Glimpse
Despite continuous efforts, our understanding of the concept of death is yet incomplete. Different countries have their own legal definition of death. In India, there is no legal definition of death. Section 46 of Indian Penal Code states, “the word death denotes death of a human being unless the contrary appears from the context.”[8] Question of death is important in resuscitation and organ donation.
Historically before 1960, death was defined as the complete and irreversible cessation of spontaneous cardiac and respiratory functions. Refinement of cardiopulmonary resuscitation techniques and the advent of Intensive Care Units (ICUs) with mechanical ventilators enabled temporary support of cardiopulmonary function in the absence of brain function. Hence, the cardiopulmonary definition of death lost relevance in such cases. Conversely, the functional loss due to damage to the vital centers of the brain is irreversible and hence brain-stem death concept evolved. It is relatively a new concept, and it is hard for relatives to believe that the patient is dead (brain dead) when his/her heart is still beating.
The history of brain death dates back to late 19th century, when many authors reported cessation of respiration but continued heartbeat in patients of cerebral diseases with increased intracranial pressure (ICP).[9,10,11] Hill and Crafoord speculated the cessation of blood flow to the brain as a cause of death.[12,13] In 1959, Wertheimer et al. described the death of the nervous system in comatose patients with respiratory arrest being treated by ventilator.[14] Though these reports were of states similar to brain death, the term was not yet coined. Some months later, in a breakthrough article, Mollaret and Goulon coined the term “coma de' passe'” (a state beyond the coma) for an irreversible state of apneic coma with absent brain-stem reflexes and electroencephalography (EEG) activity, but with preserved cardiac and metabolic activities.[15] It was pointed out that if the ventilation were stopped, the cardiac arrest would follow. In 1963, Guy Alexander used criteria for determination of brain death in a patient from whom a kidney was procured for transplant.[16] Schwab et al., proposed absence of EEG activity as the most important evidence of death of the nervous system.[17]
In 1968, an Ad Hoc Committee of Harvard Medical School on Brain Death published a landmark report, “the definition of irreversible coma.” It defined the criteria for determining brain death as apneic coma and absence of elicitable brain-stem reflexes for a period of 24 h as confirmed by an electroencephalogram.[18] The committee proposed a whole-brain formulation to define death. A major aim of Harvard criteria was claimed to be the avoidance of prolonged futile life-support and promoting death with dignity. After this report, brain death was widely accepted.[19]
In 1971, Mohandas and Chou emphasized the importance of irreversible loss of brain-stem function in brain death (Minnesota criteria).[20] Focusing on the brain-stem function, the Conference of Medical Royal Colleges in the UK published a breakthrough code for the determination of “brain death” (brain-stem death) in 1976.[21] In a subsequent memorandum, it equated brain-stem death with death of the whole person.[22] The code requires confirmation of the “irreversible loss of the capacity for consciousness combined with the irreversible loss of the capacity to breathe.” The brain-stem death concept is based on arguments that asystole inevitably follows the diagnosis and that cognitive processing is incompatible with death of the midbrain. Irreversible loss of brain-stem function is determined clinically in the context of irremediable structural brain damage only if reversible causes of the brain-stem dysfunction are excluded. The code of practice was laid down by Academy of Medical Royal Colleges to provide clear, scientific criteria for diagnosing both brain-stem death and death following cardiac arrest.[23,24]
Many television programs criticized the purely clinical criteria of UK, in contrast to using of confirmatory investigations, like EEG in other places. American neurologists argued that patients have survived in whom the UK. code for brain-stem death had been fully met.[25] Pallis and Harley reject these statements observing that some of these patients did not have irremediable brain damage, and a small number of patients were not timely examined. They presented studies of 1,862 patients who were brain dead by UK. criteria and in whom despite of continued ventilator support asystole invariably occurred.[26]
In 1981, the US President's Commission published a landmark report on the ethical and legal implications of defining death and presented conceptual basis for whole-brain-death.[27] It evaluated nonbrain (circulatory) formulation, whole-brain formulation and higher brain formulation of death and approved the whole-brain formulation. The report defined death as: “The permanent cessation of functioning of the organism as a whole” and the criterion as: “The permanent cessation of functioning of the entire brain.” The commission's concept of brain death rested on the claims that brain is the source of integration for the organism as a whole and brain death is consistent with the traditional cardiopulmonary criterion. Consistency is maintained with supposed fact that after brain-death, cardiopulmonary death quickly follows despite continued intensive care. This is known as the somatic disintegration hypothesis. The commission's report leads to the Uniform Determination of Death Act[28] according to which, “an individual who has sustained either (1) irreversible cessation of circulatory and respiratory functions or (2) irreversible cessation of all functions of the entire brain, including the brain-stem, is dead. A determination of death must be made in accordance with accepted medical standards.” It does not mention what are accepted medical standards. Similar legal developments occurred in Canada in 1981 and 1988.[29,30] Most nations adopted either whole-brain-death or brain-stem death criteria for determination of death.[19] New York and New Jersey in USA have adopted statutes that allow the accommodation of religious, cultural and philosophical differences in respect of death.[19]
In 1995, American Academy of Neurology (AAN) published practice parameters for diagnosis of brain-death.[31] The parameter emphasizes on irreversible coma (with a known cause), absence of brain-stem reflexes and irreversible apnea. The diagnosis of brain-death is clinical in nature and supplementary tests to be used in the presence of confounding factors.
The Brain-stem death concept is still not accepted by USA, which still believes in whole-brain-death formulation. This fact is again underlined in the recently published White Paper on “Controversies in the Determination of Death” by the President's Council on Bioethics.[32] The Council considered the U.K position a “reduction”, “conceptually suspect” and “clinically dangerous”. The council advocated the term “total brain failure” in place of “whole-brain-death”. Some authors view this new term as philosophically neutral and physiologically clearer, while others find it unhelpful.[33,34] The council rejects 1968 Harvard committee's social construct approach and also the higher brain approach. The council proposed a new-unifying concept of death. Death remains the cessation of the organism as a whole and wholeness depends on the existence of the fundamental vital work of the organism - the work of self-preservation, achieved through the organism's need-driven commerce with the surrounding world. The council emphasizes breathing and consciousness as important forms of the environmental commerce. Thus, on this account, total brain failure can continue to serve as a criterion for declaring death.
Fifteen years after its first report, the AAN issued an evidence-based guideline update in 2010.[35] It concluded that there are no published reports of recovery of neurologic function after a diagnosis of brain-death using the 1995 AAN criteria. There is a paucity of evidence to determine the minimally acceptable observation period and reliability of newer ancillary tests. Apneic oxygenation diffusion to determine apnea is safe. Some reports appeared in 2011 describing the apparent “reversibility” of brain-death and were refuted because of nonadherence to standard guidelines.[36,37,38] In the same year, the Society of Critical Care Medicine of the American Academy of Pediatrics issued an update of the guidelines for the determination of brain-death in infants and children.[39]
Evolution of Concept and Controversies
As aptly said by bioethicists, death remains a subject in health law and bioethics that can be said to be at once well settled and persistently unresolved.[40,41] What is human death? The question is conceptual.[42] Bernat argues that the death is largely a social and moral concept based upon philosophically held tenets and beliefs.[43] According to the definition accepted over centuries, death is the irreversible loss of functioning of the organism as a whole and replaced the concept of death of the whole organism.[44,45] US Presidents commission also defined death as an irreversible loss of integrative unity of the organism.[27]
The whole-brain-death qualifies as death because brain is necessary for the functioning of the organism as a whole as it integrates, interrelates and controls complex bodily activities.[45] Shewmon and other critics point out that certain areas of the brain are intact, and some rudimentary EEG activity is retained in individuals who meet brain-death criteria.[46,47] To this the US President's Commission noted in its report that the guidelines require an irreversible loss of all brain functions, not complete anatomical destruction of the tissue. Isolated metabolic or electrical activity in dispersed cells cannot be a sign that a patient is still alive.[27] However, Shewmon and many authors further reported that pituitary neuroendocrine function like antidiuretic hormone secretion, hypothalamus mediated thermoregulatory control, and other autonomic function may be preserved in patients who fulfill brain-death criteria.[48,49,50,51] In response to this challenge, Bernat, revised both (1) the organismic definition of death to “the permanent cessation of the critical functions of the organism as a whole” and (2) the corresponding standard to permanent cessation of the critical functions of the whole-brain.[52] He also argue that whole-brain criterion does not require the loss of all neuronal activities. Instead, all clinical brain function measurable at bedside must be lost.[53] Wijdicks further illustrates that pituitary blood flow arises from extracranial sources, which is preserved in raised ICP and that preservation of neurohypophyseal functioning is not inconsistent with the whole-brain formulation of brain-death.[54]
Arguing brains role as somatic integrator, Alan Shewmon and others further presented that patients who are diagnosed with “brain-death” continue to exhibit many “somatically integrative” functions like maintenance of hemodynamic stability, body temperature and immune response.[51,55] Integration is an emergent property of the whole organism. Brain's role is modulatory and not integrative. Shewmon also provided documented case studies of brain dead individuals with persistent cardiac activity for significant periods.[56] As both the claims that after brain-death, body is no longer a “somatically integrated whole,” and circulation will cease within a definite span of time were questioned, the US Presidents council proposed a new unifying concept of death that the patient with total brain failure is no longer able to carry out the fundamental work of a living organism, stressing breathing and consciousness as important forms of the environmental commerce.[32] However, this position is also questioned by Shewmon pointing that inner drive to breathe is also absent in conscious patients with lower brain-stem lesions. Therefore, inner drive to breathe is not a necessary feature of organismic wholeness. He also criticized ignorance by the council of other works such as self-development and self-maintenance to be the “fundamental vital work of a living organism.” He provides a counter example that embryo fulfills the council's definition of death, yet it is unquestionably alive.[33]
In a challenge to brain-stem death formulation, Bernat point out the possibility of a “profound locked-in syndrome” in which awareness might be retained in the absence of brain-stem activity.[57] Furthermore, this formulation has not been accepted by followers of whole-brain approach. However, in both whole-brain-death and brain-stem death, the criteria and the tests are similar.[19] Apart from whole-brain and brain-stem formulation of brain-death, a third formulation , “higher brain formulation”, is proposed by Veatch and further refined by others. It is based on another definition of death:" Irreversible loss of personhood." They argue that permanent unconsciousness and loss of cognition negates personhood and that the law should equate death with the loss of higher brain functions.[58,59] Thus, the formulation equates death to destruction of the cerebral cortex. The major problem with this definition is that persistent vegetative state and anencephalic neonates are brain dead by this definition.[57] Higher brain formulation has not been accepted by jurisdictions anywhere.
In spite of so much grappling and laid down standards, the equivalence of brain and brain-stem death with death, though welcomed largely, is not universally accepted.[19,60]
Indian Context
Awareness about brain-death is extremely low in India.[2,3,4] Various aspects of brain-death, its importance for organ donation and its legality needs to be elaborated. India follows the UK concept of brain-stem death and the Transplantation of Human Organs (THO) Act was passed by Indian parliament in 1994 which legalized the Brain-stem death.[5,6] In 1995, THO rules were laid down which describe brain-death certification procedure.[61,62] Despite this, the brain-death is not promptly declared in India due to lack of awareness and doubts about the legal procedure of certifying brain-death.
In view of this, the state of Maharashtra has recently passed a resolution making it mandatory to declare and certify “brain-death”.[7] The Government Resolution underlines the responsibilities of hospitals registered under THO Act 1994 that is, authorized transplant centers. As the large number of brain-death occurs in nontransplant hospitals, it makes for the appropriate authority (Director of Health Services) to register all hospitals in the state that have an operation theatre and ICU as NonTransplant Organ Retrieval Centers (NTORCs). These hospitals are permitted to certify brain-death as per procedure and then conduct organ retrieval for therapeutic purposes but not permitted to perform actual transplantation. Thus, it is mandatory now for all NTORCs and authorized transplant centers in the State to certify and notify the brain-death cases to Zonal Transplantation Co-ordination committee. This is a strong step to streamline the procedure for cadaveric organ retrieval and transplantation.
Anatomical and Physiological Basis of Brain-stem Death
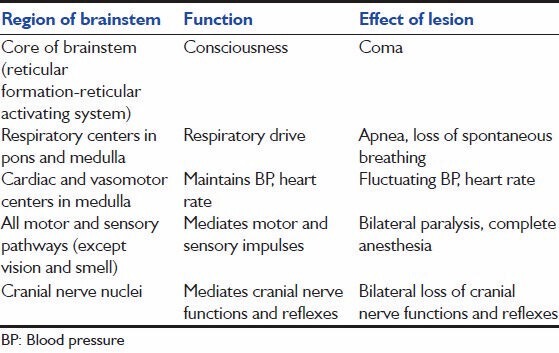
The brain-stem consists of the midbrain, pons and medulla. It contains the nuclei of last ten cranial nerves and ascending and descending tracts. The reticular formation (RF) is a complex network of nuclei and interconnecting fibers. The reticular activating system (RAS), which occupies the core of the brain-stem, provides the anatomical and physiological basis for wakeful consciousness. The medullary RF contains the vital centers controlling the heartbeat, breathing and circulation. The pontine RF contains centers for coordination of acoustic, vestibular, respiratory and cardiovascular processes. The midbrain RF contains centers for visuospatial orientation and eating behavior. As brain-stem is structurally and functionally very compact, even small lesions can destroy vital cardiac and respiratory centers; disconnect cerebral cortex from brain-stem; damage sensory fibers from higher centers of consciousness, perception and cognition. Damage to RF may lead to loss of cognition, persistent unconsciousness and coma.[63,64] The parts of brain-stem with associated functions and effects of their lesion are depicted in Table 1.
Table 1.
Tests of Brain-stem Function
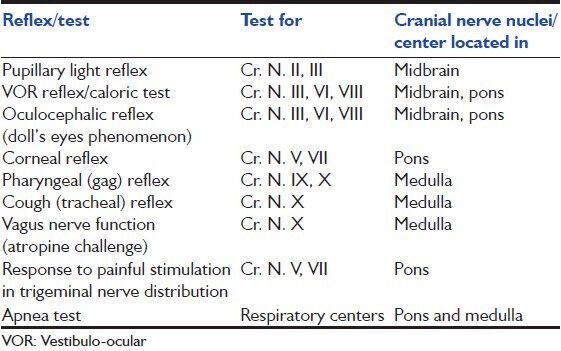
Function of the brain-stem is determined by the presence or absence of spontaneous respiration and by testing the cranial nerves whose nuclei are within the brain-stem. The tests commonly used to determine brain-stem function are depicted in Table 2.
Table 2.
Role of Cerebral Cortex in Consciousness-
Consciousness is wakefulness and awareness of oneself and surroundings for which normal functioning of RF and cerebral cortex is necessary respectively. Hence, consciousness is altered in the lesions of cortex and RF.
To assess the function of the entire brain diagnostic tests of cerebral cortex function and of brain-stem function are done. Cerebral cortical function can be assessed by testing for electrical activity with an electroencephalogram. Absence of cerebral cortical function can also be determined by a lack of verbal response and lack of spontaneous or coordinated eye movements. Absence of cerebral circulation is also indicative of cortical death.
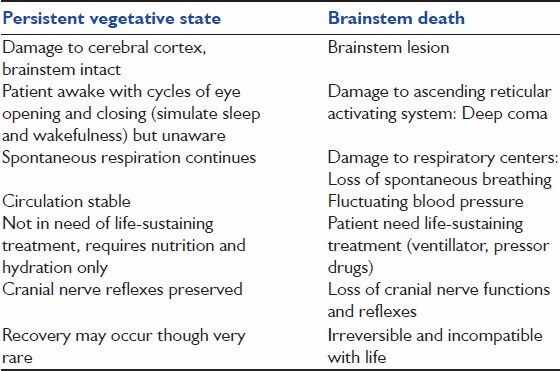
Brain-death and brain-stem death has to be differentiated from vegetative state [Table 3].
Table 3.
Causes and pathophysiology of brain-(stem) death
Direct traumatic injury to the head (e.g. road accident), subarachnoid hemorrhage and ischemic stroke are the most common causes of brain-death.[65,66] Others include intracerebral hemorrhage, hypoxic-ischemic encephalopathy etc., These cause severe damage of neuronal tissue leading to edema and increase in ICP. Elevated ICP in turn reduces cerebral perfusion pressure and cerebral blood flow. A vicious cycle is established in which decreasing cerebral perfusion and increasing ICP reinforce one another until blood no longer enters the cranial cavity and transtentorial herniation and coning at foramen magnum occurs.[46,67] This herniation crush the brain-stem. At this point, the brain including brain-stem is rendered permanently dysfunctional. Late neuronal injury can be explained by reperfusion mechanism associated with hypoxic-ischemic brain injury.
Wijdicks and Pfeifer studied neuropathology in 41 brain dead patients. Although neuronal ischemic changes were frequently profound, respirator brain with extensive ischemic neuronal loss and tissue fragmentation was not observed. They concluded that the neuropathologic examination is not diagnostic of brain-death.[68]
Diagnosis of Brain-Stem Death In India
Brain-stem death is medically and legally defined as the total and irreversible cessation of all brain-stem functions. Diagnosis of brain-stem death is required to discontinue artificial ventilation and to ask legal consent for organ donation from relatives.
In India the THO Act 1994 and the THO Rules, 1995 are the only laws wherein brain-death certification procedures have been laid down.[5,6,61,62] Form 8 of THO Act and Rules prescribed as Brain-Death Certification format is to be utilized to certify brain-stem death.[62] It states:
-
Who should diagnose: Team of four medical experts including
- Medical Administrator In charge of the hospital.
- Authorized Specialist
- Authorized Neurologist/Neuro-Surgeon
- Medical Officer treating the patient.
Amendments in the THO Act (2011) have allowed selection of a surgeon/physician and an anesthetist/intensivist, in the event of the nonavailability of approved neurosurgeon/ neurologist.[6]
Criteria for Diagnosis of Brain-stem Death in India
Patient should be deeply comatose (due to irreversible brain damage of known etiology); exclude reversible causes of coma
Patient should be on a ventilator because of the cessation of spontaneous respiration. Exclude neuromuscular blocking agents as a cause of respiratory failure
-
All brain-stem reflexes should be absent:
- Pupillary light reflex - Pupils are dilated, fixed and do not react to light
- Doll's head eye movements (oculocephalic reflex) (absence of conjugate deviation of eyes when head is fully rotated to one side. Performed only when there is no fracture or instability of the cervical spine
- Corneal reflex is absent
- No motor response to stimulation within any cranial nerve distribution (e.g. no response to the supraorbital pressure)
- No Gag (Pharyngeal) reflex (to stimulation of pharynx)
- No Cough reflex (to suction catheter in the trachea)
- Vestibulo-occular reflex (oculovestibular reflex/caloric testing) is absent (No eye movements after installation of 50 ml of ice cold water into each external acoustic meatus for 1 min)
- Apnea test (absence of respiratory movements after disconnection from the ventilator for sufficient duration to have pCO2 rise above threshold (>50-60 mmHg) for stimulating respiration)
All the prescribed tests are required to be repeated, after minimum interval of 6 h, “to ensure that there has been no observer error” and persistence of the clinical state can be documented.[5,6,61,62]
Role of investigations
The diagnosis is based only on the clinical examination. A neurophysiological or imaging study neither form part of the diagnostic requirements nor are legally required. Confirmatory tests may however be carried out if the panel of doctors is in doubt or disagreement of the diagnosis.
Diagnosis of Brain-(Stem) Death Worldwide-Consensus and Controversies
Despite global acceptance of Brain-death, differences in concept, clinical criteria and ancillary tests persist.[19,69,70] The conceptual differences of brain-death have been discussed earlier in this review. Variations in clinical criteria, assessment and ancillary tests are discussed below.
Differences in Clinical Criteria
A major article on international brain-death criteria by Wijdicks reveals that the majority of nations have guidelines for determination of brain-death.[19] There are differences in assessment of pupillary response to light and degree of dilatation without any scientific basis.[71] Most guidelines do not mention oculocephalic reflex. Pallis and Harley recommend it though not required by the UK code.[26] Wijdicks does not include this reflex, arguing that it lacks sensitivity in the adult brain injured patients.[54] Though the second clinical examination is required in many countries, there is no evidence for its necessity and time interval between the two examinations.[19] The qualification, experience and number of doctors required to determine brain-death also varies widely.[19] Age-specific pediatric criteria are also variable in different guidelines.[72]
The specified core temperature thresholds range from 32.2°C to 36.0°C without clear evidence base for any of these limits.[73] While Canadian guidelines permit a core temperature as low as 32.2°C during the apnea test,[74] the American require a core temperature of more than 36°C.[35]
Apnea Test
Apnea must be demonstrated as part of any brain-death declaration.[19] The test has several techniques and may lead to complications; hence needs elaboration. Apneic diffusion oxygenation is the procedure most commonly utilized.[54]
Prerequisites for the apnea test
Ensure that certain prerequisites are satisfied before the apnea test. Core body temperature of minimum 36°C, blood pH normal to low basic, systolic blood pressure (SBP) of at least 100 mmHg, euvolemia and eucapnia (PaCO2 35-45 mmHg) are recommended. There should be absence of hypoxia and prior CO2 retention. Apnea test should not be performed when the subject is under the influence of paralyzing drugs e.g. pancuronium.[35]
Apnea test procedure
Preoxygenate with 100% oxygen for 10 min to a PaO2 more than 200 mm Hg. Disconnect the patient from the ventilator. Place a catheter through the endotracheal tube close to the level of the carina and deliver 100% O2 at 6 L/min. Look closely for respiratory movements for 8-10 min. Respiration is defined as abdominal or chest excursions. Patients with an intact brain-stem can be expected to breathe within the first few minutes as hypercarbia develops at a rate of 3 mmHg/min.[75,76] Abort if SBP falls to <90 mmHg or if oxygen saturation measured by pulse oximetry is <85% for more than 30 s. If no respiratory drive is observed, repeat blood gas (PaO2, PaCO2, pH, bicarbonate, base excess) analysis after approximately 8 min. If respiratory movements are absent and arterial PCO2 is 60 mmHg or more (or 20 mmHg above baseline), the apnea test result is positive (i.e. supports the clinical diagnosis of brain-death). If the test is inconclusive but the patient is hemodynamically stable during the procedure, it may be repeated for a longer period (10-15 min).[35]
There are wide variations in the conduct of the apnea test. Less than 60% of jurisdictions include induced hypercarbia to a specified PaCO2 target (and confirmation with arterial blood gas analysis) in their guidance. Others only stipulate disconnection from the ventilator for a defined period.[19]
Contraindications to apnea testing include arterial hypotension (SBP <90 mmHg), hypoxemia (pO2 <90 mmHg) and severe acidosis (pH < 7.20).[77] If present, these abnormalities should be corrected before the test.
Complications
Hypotension, acidosis and hypoxemia were reported during apnea test in more than two thirds of patients (n = 129) in a study. Major complications like pneumothorax, cardiac arrhythmia, myocardial infarction and barotrauma have also been reported during the test.[78,79,80]
Wijdicks et al. reported higher completion rate and no major complication during apnea test in a large study.[66] They concluded that if preconditions are met, apnea testing using an oxygen-diffusion technique is safe. In a recent study by Yingying et al., more than 50% of patients who satisfied clinical brain-death criteria did not meet the prerequisites for the apnea test.[81] The test was interrupted in about one-third of the patients because of decreasing blood pressure and heart rates, unstable oxygen saturations and inadequate loading of PCO2. Some studies report another reason for failure of the test as noncompliance with the guidelines, reason being the doctors not formally trained or lack the skill.[82]
Ancillary Testing
Confirmatory tests are optional in most guidelines and are reserved where clinical diagnosis of brain-death including apnea test cannot be completed or is doubtful.[83,84] Cerebral angiography particularly a four-vessel angiogram demonstrating absent cerebral circulation remains the gold-standard supplementary test for brain-death. Computed tomographic (CT) angiography, CT perfusion and magnetic resonance angiography though mentioned in some of the guidelines, have not been validated or recommended.[70] EEG continues to be the most commonly applied supplementary test for brain-death worldwide and was mandatory in a number of European countries in the mid -1990s.[26] The EEG is significantly affected by hypothermia, drug administration and metabolic disturbances, diminishing its clinical utility. Transcranial Doppler (TCD) is a noninvasive technique and was found to be highly sensitive in determining absent cerebral perfusion as reported by Ducrocq.[85] Radionuclide imaging techniques like Technetium-99 m scan has been widely performed. There is no uptake of isotope in brain parenchyma ("hollow the skull phenomenon") in brain-death. The use of multimodal evoked potentials in the diagnosis of brain-death was described by de Tourtchaninoff et al.[86] A combination of median nerve somatosensory, brain-stem auditory and visual evoked potentials was used in the evaluation of brain-death. Although of questionable reliability, they remain an acceptable technique in many guidelines. In a recent study by Yingying et al., EEG had the highest completion rate, sensitivity and specificity; TCD followed completion rate but poor sensitivity and specificity; SEP had the lowest completion rate, good sensitivity and poor specificity. After the combination of SEP or TCD with EEG, the specificity can increase to 100%.[81]
Confirmatory laboratory testing was mandatory in 28 of 70 practice guidelines in earlier years.[19] AAN recommended use of ancillary testing (only one of the cerebral angiogram, hexa-methyl-propylene-amine-oxime, single-photon emission computed tomography, EEG or TCD) only if clinical examination cannot be fully performed due to patient factors, or if apnea testing is inconclusive or aborted.[35]
Conclusion
Despite the fact that the concept of brain-death was introduced more than 40 years ago and has been widely accepted, differences continue with its concept and justification. There is a scarcity of evidence-based literature on practices of brain-death determination. There is no sufficient evidence to determine the minimally acceptable observation period between clinical exams; role of newer ancillary tests and safety of apnea test techniques.[34,39] Future research should be directed towards these issues. Although guidelines are available in many countries for the diagnosis of brain-death, the variations and inconsistencies necessitate an international consensus and uniform guidelines.[35,34]
Considering the success of organ transplants and the organ transplant being the only hope for end stage organ failures; in view of acute shortage of organs and availability of a large number of brain dead patients as potential organ donors; we must promote the timely diagnosis and declaration of brain dead patients. It will allow the organ transplantation to gift the life and will relieve the relatives of brain dead individual from undue anxiety and fruitless hope.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Wijdicks EF. Brain Death. Philadelphia: Lippincott Williams and Wilkins; 2001. p. 175. [Google Scholar]
- 2.Wig N, Gupta P, Kailash S. Awareness of brain death and organ transplantation among select Indian population. J Assoc Physicians India. 2003;51:455–8. [PubMed] [Google Scholar]
- 3.Bapat U, Kedlaya PG, Gokulnath Organ donation, awareness, attitudes and beliefs among post graduate medical students. Saudi J Kidney Dis Transpl. 2010;21:174–80. [PubMed] [Google Scholar]
- 4.Shroff S, Navin S, Abraham G, Rajan PS, Suresh S, Rao S, et al. ‘Ramachandra protocol’ for organ donation. Antiseptic. 1997;94:73–4. [Google Scholar]
- 5.Government of India. Ministry of Law, Justice and Company Affairs (Legislative Department) New Delhi. The Transplantation of Human Organs Act, 1994. Central Act 42 of 1994. [Last accessed on 2014 Jul 11]. Available from: http://www.health.bih.nic.in/Rules/THOA-1994.pdf .
- 6.Government of India. Ministry of Law, Justice and Company Affairs (Legislative Department) New Delhi. The Transplantation of Human Organs (Amendment) Act, 2011. (No. 16 of 2011) [Last accessed on 2014 Jul 11]. Available from: http://www.mohanfoundation.org/THO-amendment-act-2011.pdf .
- 7.Government of Maharashtra, Public Health Department, Government Resolution No. MAP2012/C.R.289/AROGYA-6. Mumbai: Mantralaya; 2012. Sep 13, [Last accessed on 2014 Jul 11]. Available from: https://www.maharashtra.gov.in/Site/Upload/Government%20Resolutions/English/201209141533080800.pdf;/201209141531450800.pdf;/201209141533590800.pdf . [Google Scholar]
- 8.Reddy KS. Ch. 6. 27th ed. 2008. The Essentials of Forensic Medicine and Toxicology; p. 119. [Google Scholar]
- 9.Horsley V. On the mode of death in cerebral compression and its prevention. Q Med J. 1894;2:306–9. [Google Scholar]
- 10.Duckworth D. Some cases of cerebral disease in which the function of respiration entirely ceases for some hours before that of the circulation. Edinb Med J. 1898;3:145–52. [Google Scholar]
- 11.Cushing H. Some experimental and clinical observations concerning states of increased intracranial tension. Am J Med Sci. 1902;124:375–400. [Google Scholar]
- 12.Crafoord C. Do¨dsorsaken vid obturerande lungemboli [The cause of death by obstructing pulmonary embolism] Nord Med. 1939;2:1043–4. [Google Scholar]
- 13.Hill L. On cerebral anaemia and the effects which follow ligation of the cerebral arteries. Philos Trans. 1900;39:69–122. [Google Scholar]
- 14.Wertheimer P, Jouvet M, Descotes J. Diagnosis of death of the nervous system in comas with respiratory arrest treated by artificial respiration. Presse Med. 1959;67:87–8. [PubMed] [Google Scholar]
- 15.mollaret P, Goulon M. The depassed coma (preliminary memoir) Rev Neurol (Paris) 1959;101:3–15. [PubMed] [Google Scholar]
- 16.Powner DJ, Ackerman BM, Grenvik A. Medical diagnosis of death in adults: Historical contributions to current controversies. Lancet. 1996;348:1219–23. doi: 10.1016/S0140-6736(96)04015-9. [DOI] [PubMed] [Google Scholar]
- 17.Schwab RS, Potts F, Bonazzi A. EEG as an aid in determining death in the presence of cardiac activity ethical, legal, and medical aspects. Electroencephalogr Clin Neurophysiol. 1963;15:147–8. [Google Scholar]
- 18.A definition of irreversible coma. Report of the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death. JAMA. 1968;205:337–40. [PubMed] [Google Scholar]
- 19.Wijdicks EF. Brain death worldwide: Accepted fact but no global consensus in diagnostic criteria. Neurology. 2002;58:20–5. doi: 10.1212/wnl.58.1.20. [DOI] [PubMed] [Google Scholar]
- 20.Mohandas A, Chou SN. Brain death. A clinical and pathological study. J Neurosurg. 1971;35:211–8. doi: 10.3171/jns.1971.35.2.0211. [DOI] [PubMed] [Google Scholar]
- 21.Diagnosis of brain death. Statement issued by the honorary secretary of the conference of medical royal colleges and their Faculties in the united Kingdom on 11 October 1976. Br Med J. 1976;2:1187–8. doi: 10.1136/bmj.2.6045.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diagnosis of death. Memorandum issued by the honorary secretary of the conference of medical royal colleges and their faculties in the UK. Lancet. 1979;313:261–2. doi: 10.1136/bmj.1.6159.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.A code of practice for the diagnosis of brain stem death. Working Party Established through the Royal College of Physicians on Behalf of the Academy of Medical Royal Colleges at the Request of the Health Departments. 1998. Mar, [Last accessed on 2014 Jul 11]. Available from: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4035462.pdf .
- 24.A Code of Practice for the Diagnosis and Confirmation of Death. London: Academy of Medical Royal Colleges; 2008. [Last accessed on 2014 Jul 11]. Available from: http://www.aomrc.org.uk/doc_view/42-a-code-of-practice-for-the-diagnosisand-confirmation-of-death . [Google Scholar]
- 25.Youngner SJ, Arnold RM, Schapiro R. The Definition of Death: Contemporary Controversies. Baltimore: Johns Hopkins University Press; 1999. pp. 1–348. [Google Scholar]
- 26.Pallis C, Harley DH. ABC of Brainstem Death. 2nd ed. London: BMJ Publishing Group; 1996. pp. 8–12. [Google Scholar]
- 27.President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research, Defining Death: Medical, Legal and Ethical Issues in the Determination of Death. Washington, D.C: Government Printing Office; 1981. [Last accessed on 2014 Jul 11]. Available from: http://www.euthanasia.procon.org/sourcefiles/PresCommDefiningDeath.pdf . [Google Scholar]
- 28.Uniform Determination of Death Act. [Last accessed on 2014 Jul 11]. Available from: http://www.lchc.ucsd.edu/cogn_150/Readings/death_act.pdf .
- 29.Law Reform Commission of Canada, Criteria for the Determination of Death. Ottawa: Law Reform Commission of Canada; 1981. [Last accessed on 2014 Jul 11]. Available from: http://www.lareau-law.ca/LRCReport15.pdf . [Google Scholar]
- 30.Death and brain death: A new formulation for Canadian medicine. Canadian Congress Committee on Brain Death. CMAJ. 1988;138:405–6. [PMC free article] [PubMed] [Google Scholar]
- 31.Practice parameters for determining brain death in adults (summary statement). The Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 1995;45:1012–4. doi: 10.1212/wnl.45.5.1012. [DOI] [PubMed] [Google Scholar]
- 32.Controversies in the determination of death: A white paper of the President's Council on Bioethics 2008. Washington, DC: 2008. [Last accessed on 2014 July 11]. The President's Council on Bioethics. Available from: http://www.bioethics.georgetown.edu/pcbe/reports/death/Controversies% 20in%20the%20Determination%20of%20Death%20for%20the%20Web%20%282%29.pdf . [Google Scholar]
- 33.Shewmon DA. Brain death: Can it be resuscitated. Hastings Center Report. 2009 Mar-Apr;:18–24. doi: 10.1353/hcr.0.0122. [DOI] [PubMed] [Google Scholar]
- 34.Smith M. Brain death: Time for an international consensus. Br J Anaesth. 2012;108(Suppl 1):i6–9. doi: 10.1093/bja/aer355. [DOI] [PubMed] [Google Scholar]
- 35.Wijdicks EF, Varelas PN, Gronseth GS, Greer DM. American Academy of Neurology. Evidence-based guideline update: Determining brain death in adults: Report of the quality standards subcommittee of the American academy of neurology. Neurology. 2010;74:1911–8. doi: 10.1212/WNL.0b013e3181e242a8. [DOI] [PubMed] [Google Scholar]
- 36.Webb AC, Samuels OB. Reversible brain death after cardiopulmonary arrest and induced hypothermia. Crit Care Med. 2011;39:1538–42. doi: 10.1097/CCM.0b013e3182186687. [DOI] [PubMed] [Google Scholar]
- 37.Wijdicks EF, Varelas PN, Gronseth GS, Greer DM. There is no reversible brain death. Crit Care Med. 2011;39:2204–5. doi: 10.1097/CCM.0b013e318222724e. [DOI] [PubMed] [Google Scholar]
- 38.Webb A, Samuels OB. There is no reversible brain death. Crit Care Med. 2011;39:2206. doi: 10.1097/CCM.0b013e3182186687. [DOI] [PubMed] [Google Scholar]
- 39.Nakagawa TA, Ashwal S, Mathur M, Mysore M. Society of Critical Care Medicine, Section on Critical Care and Section on Neurology of American Academy of Pediatrics, Child Neurology Society. Clinical report—Guidelines for the determination of brain death in infants and children: An update of the 1987 task force recommendations. Pediatrics. 2011;128:e720–40. doi: 10.1542/peds.2011-1511. [DOI] [PubMed] [Google Scholar]
- 40.Rosenbaum SH. Ethical conflicts. Anesthesiology. 1999;91:3–4. doi: 10.1097/00000542-199907000-00003. [DOI] [PubMed] [Google Scholar]
- 41.Capron AM. Brain death: Well settled yet still unresolved. N Engl J Med. 2001;344:1244–6. doi: 10.1056/NEJM200104193441611. [DOI] [PubMed] [Google Scholar]
- 42.The Definition of Death. Stanford Encyclopedia of Philosophy. [Last accessed on 2014 Jul 11]. Available from: http://www.plato.stanford.edu/entries/death-definition/ First Published [2007 Oct 26, Fri]; Substantive Revision, [2011 Aug 25, Thu]
- 43.Bernat JL. Ethical Issues in Neurology. 2nd ed. Boston: Butterworth Heinemann; 2002. pp. 243–81. [Google Scholar]
- 44.Becker LC. Human being: The boundaries of the concept. Philos Public Aff. 1975;4:334–59. [PubMed] [Google Scholar]
- 45.Bernat JL, Culver CM, Gert B. On the definition and criterion of death. Ann Intern Med. 1981;94:389–94. doi: 10.7326/0003-4819-94-3-389. [DOI] [PubMed] [Google Scholar]
- 46.Shewmon DA. Recovery from “brain death”: A neurologist's apologia. Linacre Q. 1997;64:30–96. doi: 10.1080/20508549.1999.11878373. [DOI] [PubMed] [Google Scholar]
- 47.Grigg MM, Kelly MA, Celesia GG, Ghobrial MW, Ross ER. Electroencephalographic activity after brain death. Arch Neurol. 1987;44:948–54. doi: 10.1001/archneur.1987.00520210048018. [DOI] [PubMed] [Google Scholar]
- 48.Powner DJ, Hendrich A, Lagler RG, Ng RH, Madden RL. Hormonal changes in brain dead patients. Crit Care Med. 1990;18:702–8. doi: 10.1097/00003246-199007000-00004. [DOI] [PubMed] [Google Scholar]
- 49.Veatch RM. The impending collapse of the whole-brain definition of death. Hastings Cent Rep. 1993;23:18–24. [PubMed] [Google Scholar]
- 50.Potts M. A requiem for whole brain death: A response to D. Alan Shewmon's ‘the brain and somatic integration’. J Med Philos. 2001;26:479–91. doi: 10.1076/jmep.26.5.479.3005. [DOI] [PubMed] [Google Scholar]
- 51.Shewmon AD. The brain and somatic integration: Insights into the standard biological rationale for equating “brain death” with death. J Med Philos. 2001;26:457–78. doi: 10.1076/jmep.26.5.457.3000. [DOI] [PubMed] [Google Scholar]
- 52.Bernat JL. A defense of the whole-brain concept of death. Hastings Cent Rep. 1998;28:14–23. [PubMed] [Google Scholar]
- 53.Bernat JL. The whole-brain concept of death remains optimum public policy. J Law Med Ethics. 2006;34:35–43, 3. doi: 10.1111/j.1748-720X.2006.00006.x. [DOI] [PubMed] [Google Scholar]
- 54.Wijdicks EF. Brain Death. Philadelphia: Lippincott Williams and Wilkins; 2000. pp. 29–43. [Google Scholar]
- 55.Brody BA. How much of the brain must be dead? In: Youngner SJ, Arnold RM, Schapiro R, editors. The Definition of Death: Contemporary Controversies? Baltimore: The Johns Hopkins University Press; 1999. p. 73. [Google Scholar]
- 56.Shewmon DA. “Brainstem death,” “brain death” and death: A critical re-evaluation of the purported equivalence. Issues Law Med. 1998;14:125–45. [PubMed] [Google Scholar]
- 57.Bernat JL. Philosophical and ethical aspects of brain death. In: Wijdicks EF, editor. Brain Death. Philadelphia: Lippincott Williams and Wilkins; 2001. pp. 171–87. [Google Scholar]
- 58.Veatch RM. Death, Dying, and the Biological Revolution: Our Last Quest for Responsibility. New Haven, Conn: Yale University Press; 1976. [Google Scholar]
- 59.Zaner RM, editor. Death: Beyond Whole-Brain Criteria. Dordrecht, The Netherlands: Kluwer Academic; 1988. [Google Scholar]
- 60.Bernat JL. Ethical issues in the perioperative management of neurologic patients. Neurol Clin. 2004;22:viii–ix, 457. doi: 10.1016/j.ncl.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 61.Government of India. Ministry of Law, Justice and Company Affairs (Legislative Department) New Delhi. The Transplantation of Human Organs Rules, 1995 (GSR NO. 51(E), dr. [1995 Feb 04]) [As amended vide GSR 571(E) 2008 Jul 31; [Google Scholar]
- 62.Government of India. Ministry of Law, Justice and Company Affairs (Legislative Department) New Delhi. Transplantation of Human Organs (Amendment) Rules. 2008. [Last accessed on 2014 July 11]. Available from: http://www.health.bih.nic.in/Rules/THO-A-Rules-2008.pdf .
- 63.Snell RS. Clinical Neuroanatomy. 7th ed. New Delhi Philadelphia: Wolters Kluwer/Lippincott Williams and Wilkins; 2010. pp. 196–297-8.pp. 305–12. [Google Scholar]
- 64.Posner JB, Saper CB, Schiff ND, Plum F. Plum and Posner's Diagnosis of Stupor and Coma. 4th ed. New York: Oxford University press; 2007. [Google Scholar]
- 65.Saposnik G, Bueri JA, Mauriño J, Saizar R, Garretto NS. Spontaneous and reflex movements in brain death. Neurology. 2000;54:221–3. doi: 10.1212/wnl.54.1.221. [DOI] [PubMed] [Google Scholar]
- 66.Wijdicks EF, Rabinstein AA, Manno EM, Atkinson JD. Pronouncing brain death: Contemporary practice and safety of the apnea test. Neurology. 2008;71:1240–4. doi: 10.1212/01.wnl.0000327612.69106.4c. [DOI] [PubMed] [Google Scholar]
- 67.Sutcliffe AJ. Current issues in the diagnosis of brain stem death. Indian J Crit Care Med. 2004;8:185–9. [Google Scholar]
- 68.Wijdicks EF, Pfeifer EA. Neuropathology of brain death in the modern transplant era. Neurology. 2008;70:1234–7. doi: 10.1212/01.wnl.0000289762.50376.b6. [DOI] [PubMed] [Google Scholar]
- 69.Powner DJ, Hernandez M, Rives TE. Variability among hospital policies for determining brain death in adults. Crit Care Med. 2004;32:1284–8. doi: 10.1097/01.ccm.0000127265.62431.0d. [DOI] [PubMed] [Google Scholar]
- 70.Greer DM, Varelas PN, Haque S, Wijdicks EF. Variability of brain death determination guidelines in leading US neurologic institutions. Neurology. 2008;70:284–9. doi: 10.1212/01.wnl.0000296278.59487.c2. [DOI] [PubMed] [Google Scholar]
- 71.Baron L, Shemie SD, Teitelbaum J, Doig CJ. Brief review: History, concept and controversies in the neurological determination of death. Can J Anaesth. 2006;53:602–8. doi: 10.1007/BF03021852. [DOI] [PubMed] [Google Scholar]
- 72.Report of special Task Force. Guidelines for the determination of brain death in children. American Academy of Pediatrics Task Force on Brain Death in Children. Pediatrics. 1987;80:298–300. [PubMed] [Google Scholar]
- 73.Danzl DF, Pozos RS. Accidental hypothermia. N Engl J Med. 1994;331:1756–60. doi: 10.1056/NEJM199412293312607. [DOI] [PubMed] [Google Scholar]
- 74.Guidelines for the diagnosis of brain death. Canadian Neurocritical Care Group. Can J Neurol Sci. 1999;26:64–6. [PubMed] [Google Scholar]
- 75.Wijdicks EF. In search of a safe apnea test in brain death: Is the procedure really more dangerous than we think? Arch Neurol. 1995;52:338–9. doi: 10.1001/archneur.1995.00540280018005. [DOI] [PubMed] [Google Scholar]
- 76.Wijdicks EF. The diagnosis of brain death. N Engl J Med. 2001;344:1215–21. doi: 10.1056/NEJM200104193441606. [DOI] [PubMed] [Google Scholar]
- 77.Wijdicks EF. 10 questions about the clinical determination of brain death. Neurologist. 2007;13:380–1. doi: 10.1097/NRL.0b013e3181343cca. [DOI] [PubMed] [Google Scholar]
- 78.Goudreau JL, Wijdicks EF, Emery SF. Complications during apnea testing in the determination of brain death: Predisposing factors. Neurology. 2000;55:1045–8. doi: 10.1212/wnl.55.7.1045. [DOI] [PubMed] [Google Scholar]
- 79.Saposnik G, Rizzo G, Vega A, Sabbatiello R, Deluca JL. Problems associated with the apnea test in the diagnosis of brain death. Neurol India. 2004;52:342–5. [PubMed] [Google Scholar]
- 80.Brandstetter RD, Choi MY, Mallepalli VN, Klass S. An unusual cause of pulmonary barotrauma during apneic oxygenation testing. Heart Lung. 1994;23:88–9. [PubMed] [Google Scholar]
- 81.Su Y, Yang Q, Liu G, Zhang Y, Ye H, Gao D, et al. Diagnosis of brain death: Confirmatory tests after clinical test. Chin Med J (Engl) 2014;127:1272–7. [PubMed] [Google Scholar]
- 82.Earnest MP, Beresford HR, McIntyre HB. Testing for apnea in suspected brain death: Methods used by 129 clinicians. Neurology. 1986;36:542–4. doi: 10.1212/wnl.36.4.542. [DOI] [PubMed] [Google Scholar]
- 83.Young GB, Shemie SD, Doig CJ, Teitelbaum J. Brief review: The role of ancillary tests in the neurological determination of death. Can J Anaesth. 2006;53:620–7. doi: 10.1007/BF03021855. [DOI] [PubMed] [Google Scholar]
- 84.Molina DK, McCutcheon JR, Rulon JJ. Head injuries, pentobarbital, and the determination of death. Am J Forensic Med Pathol. 2009;30:75–7. doi: 10.1097/PAF.0b013e31818738dd. [DOI] [PubMed] [Google Scholar]
- 85.Ducrocq X, Braun M, Debouverie M, Junges C, Hummer M, Vespignani H. Brain death and transcranial Doppler: Experience in 130 cases of brain dead patients. J Neurol Sci. 1998;160:41–6. doi: 10.1016/s0022-510x(98)00188-9. [DOI] [PubMed] [Google Scholar]
- 86.de Tourtchaninoff M, Hantson P, Mahieu P, Guérit JM. Brain death diagnosis in misleading conditions. QJM. 1999;92:407–14. doi: 10.1093/qjmed/92.7.407. [DOI] [PubMed] [Google Scholar]


