Abstract
Lactobacillus species is a known commensal of the mouth, gastrointestinal, and genitourinary tract. However, its isolation on blood cultures is often overlooked and attributed to bench contamination. We present a case of a 58-year-old immunocompetent male who initially presented with altered mental status, but developed sepsis from Lactobacillus bacteremia during his hospital course, while on mechanical ventilation. He was found to have ischemic colitis on colonoscopy. His condition improved with antibiotics and supportive management. Using this example of ischemic colitis, we stress that in the right clinical setting, Lactobacillus bacteremia is a harbinger for a serious underlying pathology and should not be ignored.
Keywords: Bacteremia, colitis, ischemia, Lactobacillus, sepsis
Introduction
Lactobacillus species is a known commensal colonizer of the mouth, gastrointestinal and occasionally, the female genitourinary tract.[1] However, its significance as a pathogen is overlooked frequently. Moreover, most patients who have Lactobacillus bacteremia are immunosuppressed.[2,3]
Patients with Lactobacillus bacteremia typically present with fever and clinical features localized to the affected tissues, and rarely with sepsis. The diagnosis becomes especially challenging in critically ill patients, who are at an increased risk in the setting of mucosal hypoperfusion and bacterial translocation, but are often diagnosed only after clinically significant hypotension and organ dysfunction occur. We present a case of an immunocompetent patient who was initially hemodynamically stable, while on mechanical ventilation for altered mental status. Subsequently, he was found to have abdominal distension and was in shock. His blood culture yielded Lactobacillus species in multiple bottles. Further evaluation including a colonoscopy identified ischemic colitis as the source of sepsis. To our knowledge, this is the first case of ischemic colitis presenting with confirmed Lactobacillus bacteremia and sepsis.
Case Report
A 58-year-old man with schizophrenia, substance abuse, diabetes mellitus and a history of hypertension presented with headache and chest pain. He was afebrile, hypertensive and tachycardic. The rest of his physical exam was unremarkable. At the emergency department, he became confused and was intubated. Laboratories were unremarkable except for hyperglycemia and acute kidney injury (creatinine 1.6, baseline 1.1). Workup for altered mental status (magnetic resonance imaging of the head with contrast and lumbar puncture) and chest pain (electrocardiogram and computed tomography (CT) chest with contrast) was negative. Blood cultures done on admission showed no growth. The patient was extubated within 24 h of Intensive Care Unit admission. The altered mental status was attributed to synthetic cannabinoid intoxication.
On day 4 of hospital admission, the patient became increasingly agitated, tachycardic and hypertensive. Subsequently, his abdominal distension increased. On day 6, he became progressively hypotensive requiring intravenous fluid resuscitation. On day 8, he became febrile and was re-intubated for respiratory distress. Arterial lactate peaked at 2.1 mmol/L (upper limit of normal: 1.6). He was empirically treated with piperacillin-tazobactam. Blood cultures from both the central line and the periphery grew Lactobacillus species from both aerobic and anaerobic bottles. The rest of his infectious workup was unremarkable. Subsequent blood cultures were negative. However, the patient remained febrile and had persistent bandemia. Because he had progressively worsening diarrhea, metronidazole was added empirically for possible Clostridium difficile-associated diarrhea. A noncontrast CT of his chest, abdomen and pelvis showed wall thickening of the ascending colon with surrounding inflammatory changes, and ileus. Eventually, the C. difficile toxin in his stool was found to be negative. However, a colonoscopy showed diffuse edema from the hepatic flexure to cecum with intermittent areas of sparing. The involved areas had severe ulceration and a necrotic mucosa that did not bleed on biopsy, indicating severe ischemic colitis [Figure 1]. A transesophageal echocardiogram showed no vegetation. He improved clinically during a 14-day course of piperacillin-tazobactam and metronidazole, was extubated and discharged.
Figure 1.
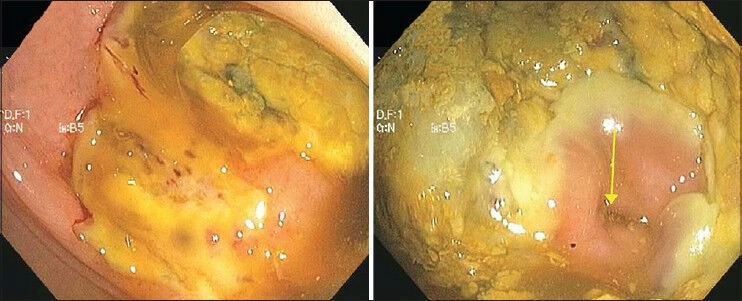
Colonoscopy images showing diffuse edema, severe ulceration and mucosal necrosis in the large intestine consistent with ischemic colitis. The region of the ileocecal valve is spared (arrow)
Discussion
True Lactobacillus bacteremia accounts for only 0.1% of all positive blood cultures.[4] Hence, it is not surprising that its presence in blood cultures is often ascribed to bench contamination. However, the attributable mortality rate in its presence can approach 30%.[5] To differentiate true Lactobacillus bacteremia from contamination, the bacteria need to be isolated either in two sets of blood cultures, or in blood and another sterile site of clinical infection.[1] Patients recently treated with immunosuppressive therapy or broad-spectrum antibiotics and those with diabetes, malignancy, organ transplants, or indwelling venous catheters are at increased risk for symptomatic bacteremia.[1,4,5]
Lactobacillus bacteremia in the setting of colitis has been well-described in immunocompromised patients, but this association is extremely rare in immunocompetent patients.[4,5] In addition, Lactobacillus sepsis has been described with probiotic use, especially in the setting of inflammatory bowel disease and critical illness.[4,6,7] Our patient did not receive probiotics either prior to or during his admission. To the best of our knowledge, this is the first case of ischemic colitis associated with Lactobacillus bacteremia. However, more important than the association itself is the recognition that Lactobacillus enters the bloodstream through the mucosal translocation. Thus, our case emphasizes that the presence of true Lactobacillus bacteremia in a clinically deteriorating patient should prompt urgent evaluation of a pathology that facilitates this translocation such as colitis, pyelonephritis, endometritis, and their underlying etiologies.[4,5,8] Such patients should be treated empirically with broad-spectrum antibiotics, which can be subsequently narrowed down based on susceptibility testing. Patients should receive antibiotics for at least 7-10 days from the date the first negative blood culture was drawn.[8,9] Most isolates are susceptible to ampicillin, piperacillin-tazobactam, carbapenems, and clindamycin.[9] However, vancomycin, cephalosporins and metronidazole should not be the first choice without susceptibility results.[9] Hospital laboratories often do not routinely check drug susceptibility for anaerobes. This was one of the limitations in our diagnostic workup. Sensitivities should be specifically requested, especially if the patient's condition is not improving. Moreover, endocarditis must be ruled out because it is the most common clinically reported infection in these patients.[4] These conditions are potentially treatable and if detected early; the underlying organ can be salvaged.
Acknowledgements
The authors would like to thank Michael Risbano, MD, FCCP for his advisory role in the management of the patient and editing the original and revised versions of the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Antony SJ, Stratton CW, Dummer JS. Lactobacillus bacteremia: Description of the clinical course in adult patients without endocarditis. Clin Infect Dis. 1996;23:773–8. doi: 10.1093/clinids/23.4.773. [DOI] [PubMed] [Google Scholar]
- 2.Bourne KA, Beebe JL, Lue YA, Ellner PD. Bacteremia due to Bifidobacterium, Eubacterium or Lactobacillus; twenty-one cases and review of the literature. Yale J Biol Med. 1978;51:505–12. [PMC free article] [PubMed] [Google Scholar]
- 3.Farina C, Arosio M, Mangia M, Moioli F. Lactobacillus casei subsp. rhamnosus sepsis in a patient with ulcerative colitis. J Clin Gastroenterol. 2001;33:251–2. doi: 10.1097/00004836-200109000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Gouriet F, Million M, Henri M, Fournier PE, Raoult D. Lactobacillus rhamnosus bacteremia: An emerging clinical entity. Eur J Clin Microbiol Infect Dis. 2012;31:2469–80. doi: 10.1007/s10096-012-1599-5. [DOI] [PubMed] [Google Scholar]
- 5.Cannon JP, Lee TA, Bolanos JT, Danziger LH. Pathogenic relevance of Lactobacillus: A retrospective review of over 200 cases. Eur J Clin Microbiol Infect Dis. 2005;24:31–40. doi: 10.1007/s10096-004-1253-y. [DOI] [PubMed] [Google Scholar]
- 6.Sanders ME, Akkermans LM, Haller D, Hammerman C, Heimbach J, Hörmannsperger G, et al. Safety assessment of probiotics for human use. Gut Microbes. 2010;1:164–85. doi: 10.4161/gmic.1.3.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crooks NH, Snaith C, Webster D, Gao F, Hawkey P. Clinical review: Probiotics in critical care. Crit Care. 2012;16:237. [Google Scholar]
- 8.Salminen MK, Rautelin H, Tynkkynen S, Poussa T, Saxelin M, Valtonen V, et al. Lactobacillus bacteremia, species identification, and antimicrobial susceptibility of 85 blood isolates. Clin Infect Dis. 2006;42:e35–44. doi: 10.1086/500214. [DOI] [PubMed] [Google Scholar]
- 9.Könönen E. Anaerobic gram-positive nonsporulating bacilli. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas and Bennett's Principles and Practice of Infectious Diseases. 7th ed. New York: Churchill Livingstone; 2009. pp. 3125–8. [Google Scholar]


