Abstract
Background
The use of tacrolimus (TAC) in patients after heart transplantation (HTX) has increased over the last few years.
Aim
In this retrospective study, we evaluated the effects of a TAC (conventional and extended-release TAC)-based immunosuppressive therapy regarding rejection profile in comparison to a cyclosporine A (CSA)-based regimen in patients after HTX.
Methods
The data of 233 patients who underwent HTX at the Heidelberg Heart Transplantation Center from May 1998 until November 2010 were retrospectively analyzed. Primary immunosuppressive therapy was changed from a CSA (n=114) to a TAC (n=119)-based regimen in February 2006 according to center routine. Follow-up period was 2 years post-HTX. Primary endpoint was time to first biopsy-proven rejection requiring therapy. In all patients, routine follow-up at the Heidelberg Heart Transplantation Center was mandatory.
Results
Multivariate risk factor analysis regarding time to first rejection episode showed no statistically significant differences regarding recipient age, donor age, recipient sex, donor sex, sex mismatch, ischemic time, and diagnosis leading to HTX between the two groups (all P= not statistically significant). Time to first biopsy-proven rejection was significantly longer in the TAC group (intention-to-treat analysis, n=233, log-rank test P<0.0001; per-protocol analysis, n=150, log-rank test P=0.0003). In patients who underwent a change of primary immunosuppression (n=49), a significantly longer time to first biopsy-proven rejection was also found in the primary TAC subgroup (log-rank test P=0.0297). Further subgroup analysis in the TAC subgroups showed no statistically significant differences in time to biopsy-proven rejection under extended-release TAC compared to conventional TAC (intention-to-treat analysis, log-rank test P=0.1736).
Conclusion
Our study demonstrated that a TAC-based primary immunosuppressive therapy is superior to a CSA-based immunosuppressive regimen in patients after HTX regarding time to first biopsy-proven rejection.
Keywords: extended-release tacrolimus, cyclosporine A, renal function
Introduction
After clinical introduction at the end of the 1980s, tacrolimus (TAC) is now used as a primary calcineurin inhibitor (CNI) in most patients after heart transplantation (HTX).1–6 TAC and cyclosporine A (CSA) have different chemical structures, but the main mechanism of action is similar.7 As TAC needs a 100-times lower concentration, possible favorable effects regarding prevention of allograft rejection might be explained.8 In addition to conventional TAC, extended-release TAC is also available.9
Recently, published data comparing CNI immunosuppressive treatment in patients after HTX showed a superior rejection profile in patients with a TAC-based immunosuppressive regimen.2,10–12 In particular, analysis of a European cohort, published by Grimm et al detected advantageous effects of a TAC-based immunosuppressive regimen compared to a CSA-based immunosuppression regimen within the first year after HTX.13
However, data comparing both CNI regimes, in patients after HTX, remain limited. Current International Society for Heart and Lung Transplantation (ISHLT) registry data show that TAC is applied more often in patients after HTX, but there is still no general recommendation regarding specific CNI treatment after HTX.14 For this reason, the present study focused on the rejection profile in patients after HTX regarding time to first biopsy-proven rejection, depending on the primarily applied CNI. Furthermore, renal function 2 years after HTX was analyzed.
Patients and methods
Patients
In total, we retrospectively analyzed data of 233 patients who underwent HTX at the Heidelberg Heart Transplantation Center (Heidelberg, Germany) between May 1998 and November 2010. One hundred and fourteen patients received a CSA-based and 119 a TAC-based primary immunosuppressive drug regimen. Primary immunosuppressive therapy was changed from a CSA- to a TAC-based regimen in February 2006 according to center routine.
Exclusion criteria were a primarily non-CNI-based immunosuppressive regimen, external follow-up, and primary graft failure.
All patients received standardized routine follow-up examinations according to center practice, including physical examination, routine laboratory testing including drug level monitoring, endomyocardial biopsies, and echocardiography. Baseline data were collected immediately after HTX. In patients who changed transplantation center during the observation period, only baseline demographic data were analyzed.
Immunosuppressive regimen and drug monitoring
Immunosuppressive therapy was given according to the center’s routine protocol. Immunosuppression was monitored by in-house laboratory-measured trough levels. All patients received a dual immunosuppression. Azathioprine was replaced by mycophenolate mofetil (MMF) in 2001 according to the center’s practice. Additionally, steroids were routinely given for 6 months after HTX and weaned off these according to the investigator’s discretion whenever possible.
Acute rejection (AR)
Endomyocardial biopsies were performed according to the center’s routine protocol. Biopsies were performed weekly during the first month after HTX, monthly during months 2 to 6, yearly from month 12, and when clinically indicated. Rejection episodes were graded according to the revised ISHLT classification (ISHLT R).15
Statistical analysis
Statistical analysis was performed using SAS software (v 9.3; SAS Institute Inc., Cary, NC, USA). Freedom from AR was evaluated using Kaplan–Meier analysis and log-rank test. Numerical data were expressed as mean value ± standard deviation or were listed as absolute numbers (n) or percentage (%). To determine differences in groups and subgroups, Student’s t-tests for continuous data and chi-square tests for categorical data were used. To determine possible risk factors, a multivariable Cox proportional-hazards model was used, if necessary.
A P-value of <0.05 was considered to be statistically significant. Whenever appropriate, statistical graphics were used to illustrate findings.
Results
Patient baseline characteristics
Two hundred and thirty-three patients were included in the present study, of whom 114 received CSA and 119 TAC as initial immunosuppressive therapy. Included in the TAC group were 64 patients on extended-release TAC. In the CSA group, 55 patients received azathioprine as initial concomitant immunosuppression. In the TAC group, no patient received azathioprine as initial concomitant immunosuppression.
Baseline characteristics are described in Table 1. No differences between groups were found regarding mean recipient age, recipient sex, and sex mismatch (all P= not statistically significant [ns]). Donors for patients primarily on CSA were significantly younger (P<0.0001) and had a significantly shorter ischemic time (P<0.0001) and significantly higher percentage of male donors (P=0.016). Considering reasons for HTX, more patients underwent transplantation due to cardiac amyloidosis in the TAC group (P=0.0110). In the CSA group, three patients changed HTX center during the study period (P= ns).
Table 1.
Baseline clinical and demographic data
| Characteristics | CSA group | TAC group | P-value |
|---|---|---|---|
| Number of patients | 114 | 119 | |
| Mean recipient age (years) ± SD | 51.7±10.9 | 52.15±9.58 | ns |
| Mean donor age (years) ± SD | 37.6±13.2 | 45.3±12.2 | <0.0001 |
| Recipient sex (m/f) | 88/26 | 88/31 | ns |
| Donor sex (m/f) | 52/62 | 36/83 | 0.016 |
| Sex mismatch (n/%) | 43/37.7 | 58/48.7 | ns |
| Diagnosis leading to HTX (patients) | |||
| DCM | 62 | 64 | ns |
| CAD | 40 | 29 | ns |
| Organic heart defect | 1 | 2 | ns |
| Lung | 1 | 0 | ns |
| Other | 3 | 4 | ns |
| Cardiac amyloidosis | 7 | 20 | 0.0110 |
| Ischemic time (min) ± SD | 203.2±55.2 | 247.0±52.2 | <0.0001 |
| Change of HTX center (n) | 3 | 0 | ns |
Abbreviations: CAD, coronary artery disease; CSA, cyclosporine A; DCM, dilated cardiomyopathy; HTX, heart transplantation; m/f, male/female; ns, not statistically significant; SD, standard deviation; TAC, tacrolimus.
Survival
In total, 13.3% (31/233) of all included patients died within 2 years after HTX: 9.6% (11/114) in the CSA group and 16.8% (20/119) of TAC patients (P= ns). As shown in Table 2, more patients died due to infections in the TAC group (P=0.0123); regarding all other causes of death, statistical significance was not reached (all P= ns).
Table 2.
Causes of death
| Cause of death | CSA group | TAC group | P-value |
|---|---|---|---|
| Transplant failure | 0 | 0 | na |
| Infection | 3 | 13 | 0.0123 |
| Acute rejection | 1 | 1 | ns |
| CAD | 0 | 0 | na |
| Lymphoma | 1 | 0 | ns |
| Carcinoma | 0 | 0 | na |
| Other | 6 | 4 | ns |
| Unknown | 0 | 2 | ns |
| Total (n/% of group) | 11/9.6 | 20/16.8 | ns |
Abbreviations: CAD, coronary artery disease; CSA, cyclosporine A; na, not applicable; ns, not statistically significant; TAC, tacrolimus.
AR
Freedom from AR in CSA and TAC patients is shown in Figure 1. Kaplan–Meier analysis demonstrated a superior rejection profile in the TAC group (intention-to-treat analysis [ITT], log-rank test P<0.0001). Analysis of patients without changes of their CNI-based immunosuppressive regimen showed similar results (per-protocol analysis, log-rank test P=0.0003).
Figure 1.
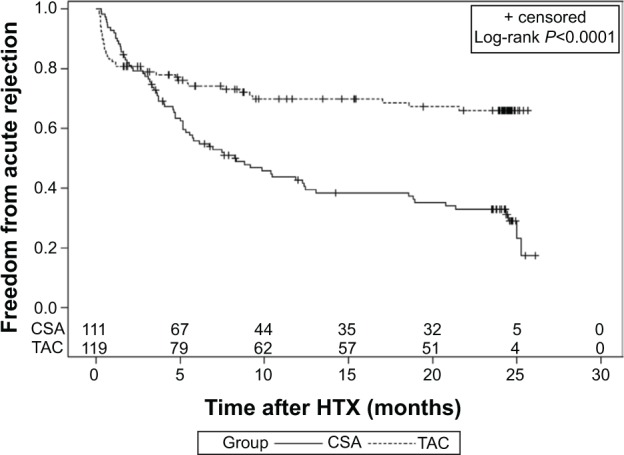
Freedom from acute rejection (intention-to-treat analysis): rejection profile of CSA- and TAC-based immunosuppressive therapy during the first 2 years after HTX.
Abbreviations: CSA, cyclosporine A; HTX, heart transplantation; TAC, tacrolimus.
Subgroup analysis of conventional TAC and extended-release TAC showed no statistically significant differences regarding rejection-free time (ITT, P=0.1736).
In order to analyze significant differences or characteristics concerning many patients at baseline, multivariate risk analysis with regard to time to first rejection episode was used. As demonstrated by risk analysis for occurrence of AR, the only independent risk factor for development of an AR episode was a CSA-based immunosuppressive regimen (Table 3). All other considered risk factors did not reach statistical significance (all P= ns).
Table 3.
Risk factor analysis regarding time to first rejection
| Factor | Hazard ratio | 95% CI | P-value |
|---|---|---|---|
| CSA-based immunosuppressive therapy | 2.261 | 1.415–3.612 | 0.006 |
| Recipient age | 0.986 | 0.965–1.008 | ns |
| Donor age | 1.000 | 0.985–1.014 | ns |
| Male recipient | 0.729 | 0.390–1.362 | ns |
| Male donor | 0.810 | 0.429–1.527 | ns |
| Mismatch | 1.041 | 0.556–1.948 | ns |
| Reason for HTX | |||
| DCM | 0.542 | 0.236–1.245 | ns |
| CAD | 0.754 | 0.302–1.881 | ns |
| Cardiac amyloidosis | 0.905 | 0.335–2.446 | ns |
Abbreviations: CAD, coronary artery disease; CI, confidence interval; CSA, cyclosporine A; DCM, dilated cardiomyopathy; HTX, heart transplantation; ns, not statistically significant.
Renal function, laboratory and physical data
Renal function was evaluated by serum creatinine and the Modification of Diet in Renal Disease (MDRD) equation (Figures 2 and 3).16 At baseline, serum creatinine was 1.1±0.5 mg/dL versus 1.5±0.8 mg/dL in the TAC group (P<0.0001). Three months after transplantation, serum creatinine was 1.2±0.4 mg/dL in the CSA group versus 1.6±0.8 mg/dL in the TAC group (P<0.0001). Six months after HTX, serum creatinine increased to 1.4±0.6 mg/dL in the CSA group versus 1.7±1.0 mg/dL in the TAC group (P=0.0206). Starting 1 year after HTX, no significant differences regarding serum creatinine between both groups were found. Analysis of renal function by using the MDRD equation showed similar results. In the CSA group, serum creatinine increased significantly and MDRD decreased significantly during follow-up (2-year values versus baseline: both P<0.0001), whereas, in TAC patients, only MDRD values were significantly different 2 years after HTX (2-year values versus baseline: creatinine P=0.2239, MDRD P=0.0094). Evaluation of blood chemistry results showed a significantly higher serum sodium level at baseline in TAC patients compared to CSA patients (P=0.0428). Regarding serum potassium levels, no significant differences between groups were observed at baseline.
Figure 2.
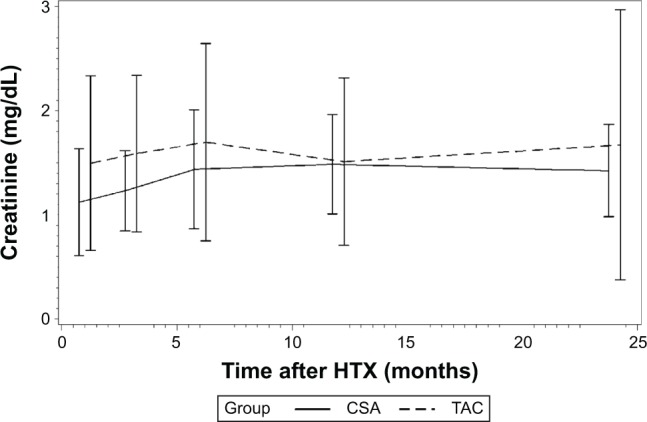
Renal function (serum creatinine) during the first 2 years after HTX in CSA and TAC patients.
Abbreviations: CSA, cyclosporine A; HTX, heart transplantation; TAC, tacrolimus.
Figure 3.
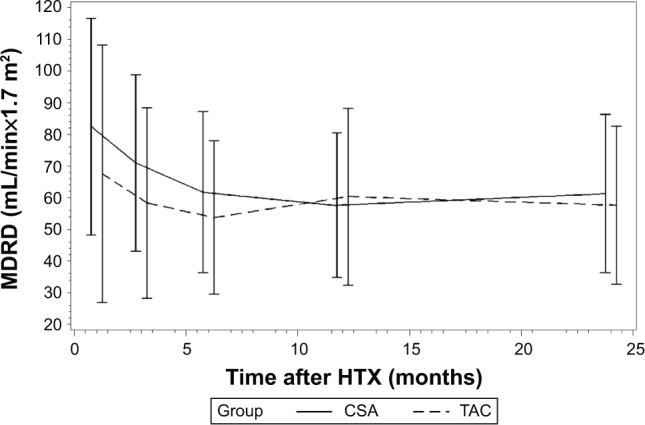
Renal function (MDRD) during the first 2 years after HTX in CSA and TAC patients.
Abbreviations: CSA, cyclosporine A; HTX, heart transplantation; MDRD, Modification of Diet in Renal Disease; TAC, tacrolimus.
No statistically significant differences between both groups were detected at baseline and 2 years after HTX concerning blood glucose levels (baseline P= ns, 2 years after HTX P= ns); accordingly, no significant decrease of blood glucose trough levels within either group was detectable. Total blood cholesterol levels (baseline P=0.0021, 2 years after HTX P=0.0252) and low-density lipoprotein levels were higher in CSA patients (baseline P=0.0002, 2 years after HTX P=0.0006). During the study period, in both groups, a statistically significant reduction of total blood cholesterol levels was seen (CSA group P=0.0010, TAC group P=0.0003). Regarding serum triglycerides, a significant decrease was detected in TAC patients during the study period (P=0.0031).
Regarding liver function tests, significantly lower aspartate aminotransferase could be observed in CSA patients at baseline and 2 years after HTX (baseline P=0.0007, 2 years after HTX P=0.0014); alanine aminotransferase was significantly higher at baseline in the TAC group (P=0.0048), and decreased significantly during the study period in both groups. Significantly higher gamma-glutamyl transferase was observed in the TAC group, both at baseline and 2 years after HTX. Again, GGT decreased significantly during the study period in both groups.
Systolic blood pressure was significantly higher in CSA patients at baseline and 2 years after HTX (baseline P=0.0317, 2 years after HTX P=0.0405). No significant change of blood pressure was observed within either group during the study period. All laboratory and clinical parameters are described in Table 4.
Table 4.
Laboratory and clinical characteristics
| Characteristics (all parameters), mean ± SD | CSA group | TAC group | P-value |
|---|---|---|---|
| Creatinine (mg/dL) | |||
| Baseline | 1.1±0.5 | 1.5±0.8 | <0.0001 |
| 2 years after HTX | 1.4±0.4a | 1.7±1.3b | ns |
| MDRD (mL/min*1.73 m2) | |||
| Baseline | 82.4±34.2 | 67.6±40.7 | 0.0030 |
| 2 years after HTX | 61.3±25.0a | 57.6±24.9a | ns |
| Sodium (mmol/L) | |||
| Baseline | 136.5±3.8 | 137.5±3.4 | 0.0428 |
| 2 years after HTX | 138.6±3.5a | 139.2±2.8a | ns |
| Potassium (mmol/L) | |||
| Baseline | 4.2±0.5 | 4.3±0.6 | ns |
| 2 years after HTX | 4.3±0.4b | 4.4±0.5b | ns |
| Serum urea (mg/dL) | |||
| Baseline | 69.7±45.3 | 78.6±41.4 | ns |
| 2 years after HTX | 56.8±20.1a | 57.3±25.8b | ns |
| Uric acid (mg/dL) | |||
| Baseline | 5.9±2.3 | 6.8±2.6 | 0.0075 |
| 2 years after HTX | 6.6±1.9a | 6.8±2.2b | ns |
| Blood glucose trough level (mg/dL) | |||
| Baseline | 117.2±49.7 | 127.0±56.4 | ns |
| 2 years after HTX | 109.2±30.2b | 114.0±37.0b | ns |
| Creatine phosphokinase (U/L) | |||
| Baseline | 23.3±23.3 | 35.9±21.8 | <0.0001 |
| 2 years after HTX | 141.0±157.3a | 150.8±142.9a | ns |
| ASAT (U/L) | |||
| Baseline | 17.3±10.7 | 24.2±16.7 | 0.0007 |
| 2 years after HTX | 16.4±8.3b | 29.8±32.8b | 0.0014 |
| ALAT (U/L) | |||
| Baseline | 35.7±31.3 | 49.0±36.7 | 0.0048 |
| 2 years after HTX | 17.6±13.6a | 24.3±15.2a | 0.0061 |
| GGT (U/L) | |||
| Baseline | 111.7±112.0 | 306.4±271.1 | <0.0001 |
| 2 years after HTX | 30.6±29.7a | 83.3±99.4a | <0.0001 |
| Total blood cholesterol level (mg/dL) | |||
| Baseline | 220.5±56.6 | 198.0±50.1 | 0.0021 |
| 2 years after HTX | 193.7±46.6a | 178.1±35.5a | 0.0252 |
| HDL (mg/dL) | |||
| Baseline | 60.3±22.5 | 61.4±20.6 | ns |
| 2 years after HTX | 48.7±15.6a | 50.1±16.3a | ns |
| LDL (mg/dL) | |||
| Baseline | 128.9±48.1 | 104.2±32.4 | 0.0002 |
| 2 years after HTX | 114.0±30.5a | 95.8±31.4b | 0.0006 |
| Triglycerides (mg/dL) | |||
| Baseline | 184.5±95.5 | 183.1±78.2 | ns |
| 2 years after HTX | 163.2±135.5b | 158.8±84.2a | ns |
| Lactate dehydrogenase (U/L) | |||
| Baseline | 282.9±109.3 | 297.0±104.9 | ns |
| 2 years after HTX | 196.9±86.8a | 252.3±76.1a | 0.0002 |
| Alkaline phosphatase (U/L) | |||
| Baseline | 149.3±96.9 | 145.1±114.4 | ns |
| 2 years after HTX | 106.6±58.9b | 95.9±54.8a | ns |
| Hemoglobin (g/dL) | |||
| Baseline | 11.4±1.3 | 11.0±1.2 | 0.0080 |
| 2 years after HTX | 12.7±1.6a | 12.8±1.8a | ns |
| Thrombocytes (/nL) | |||
| Baseline | 273.3±129.0 | 314.7±136.1 | 0.0189 |
| 2 years after HTX | 244.3±66.5b | 215.8±67.3a | 0.0109 |
| Leukocytes (/nL) | |||
| Baseline | 10.0±5.2 | 10.1±4.5 | ns |
| 2 years after HTX | 6.7±2.0a | 6.3±2.0a | ns |
| Systolic blood pressure (mmHg) | |||
| Baseline | 125.5±14.3 | 120.8±17.5 | 0.0317 |
| 2 years after HTX | 126.2±15.8b | 121.1±14.4b | 0.0405 |
| Diastolic blood pressure (mmHg) | |||
| Baseline | 77.0±9.6 | 73.1±11.20 | 0.0060 |
| 2 years after HTX | 77.2±9.6b | 75.4±10.6b | ns |
Notes:
P<0.05 vs baseline, statistically significant
P<0.05 vs baseline, ns.
Abbreviations: ALAT, alanine aminotransferase; ASAT, aspartate aminotransferase; CSA, cyclosporine A; GGT, gamma-glutamyl transferase; HDL, high-density lipoprotein; HTX, heart transplantation; LDL, low-density lipoprotein; MDRD, Modification of Diet in Renal Disease; ns, not statistically significant; SD, standard deviation; TAC, tacrolimus.
Immunosuppressive therapy
The immunosuppressive regimen was monitored by measuring drug trough levels. In both groups, drug trough levels were significantly reduced during the study period. In patients continuously on CSA, trough levels were 266.1±102.0 μg/L at baseline, 174.5±83.7 μg/L 1 year after HTX (P-value versus baseline <0.0001), and 130.8±56.7 μg/L 2 years after HTX (P-value versus baseline <0.0001). In patients continuously on TAC, trough levels were 12.6±4.4 μg/L at baseline, 8.89±4.23 μg/L 1 year after HTX (P-value versus baseline <0.0001), and 7.22±2.2 μg/L 2 years after HTX (P-value versus baseline <0.0001). Mycophenolic acid (MPA) trough levels did not differ significantly in patients continuously on CSA or TAC. Baseline MPA trough level was 2.09±1.09 mg/L in the CSA group versus 2.43±1.52 mg/L in the TAC group (P= ns). One year after HTX, MPA trough levels were 2.51±1.71 mg/L in the CSA group versus 2.29±1.24 mg/L in the TAC group (P= ns). Two years after HTX, MPA levels were 2.50±1.53 mg/L (CSA) versus 2.15±1.22 mg/L (TAC) (P= ns). Further analysis of given MMF doses showed statistically significantly lower MMF doses in TAC patients. MMF doses in TAC patients were 2,300.7±902.0 mg at baseline (P-value versus CSA group =0.0116), 1,804.4±739.6 mg 1 year after HTX (P-value versus CSA group <0.0001), and 1,625.0±670.4 mg 2 years after HTX (P-value versus CSA group <0.0001).
Concomitant medication
Analysis of concomitant medication at end of study period showed significantly more patients on beta-blocker therapy in the TAC group (P<0.0001). Considering concomitant medication with ACE inhibitors, statins, or AT1 inhibitors, no statistically significant differences between groups were detected 2 years after HTX (all P= ns).
Discussion
The primary endpoint of this retrospective study in patients after HTX was to evaluate the rejection profile on CSA-and TAC-based immunosuppressive therapies. In line with previously published data, our study confirmed a superior rejection profile, ie, a longer time to first biopsy-proven rejection, in patients on a TAC-based primary immunosuppressive regimen in comparison to those on a CSA-based regimen.10,12,13,17 This might be partially explained by better patient adherence under extended-release TAC. However, we want to point out that the number of included patients in previously published studies in patients after HTX was comparatively low or time of observation was shorter.2,10,13 A significantly longer rejection-free interval under TAC was demonstrated in per-protocol and ITT analysis. Additionally, our study showed no statistically significant differences regarding time to first biopsy-proven rejection in patients on extended-release TAC; the statistically insignificant benefit of extended-release TAC might possibly be explained by advantageous patient adherence on extended-release TAC, which has been demonstrated previously.18 This has also recently been seen in patients after renal transplantation.9 In contrast to Meiser et al we continually found no differences in measured MPA levels in our study cohort, and a significantly lower MMF dose in TAC patients was observed as well.19 The different MPA level at month 3 between CSA and TAC patients in the study by Meiser et al might be explained by the lower patient number.
Additional emphasis was put on development of renal function after HTX. Despite statistically significantly better renal function tests in TAC patients at baseline compared to the CSA group, renal function tests 2 years after HTX no longer showed a statistically significant difference. As analysis of concomitant medication showed no significant differences between both groups, except for beta-blocker therapy, the main reason for deterioration of renal function might be immunosuppressive therapy. Regarding the development of chronic rejection, a published study in renal transplant patients showed no effects regarding development of chronic rejection depending on beta-blocker usage.20 The lower percentage of patients on beta-blocker therapy might be attributed to an era effect. Moreover, this indicates advantageous effects of TAC therapy on renal function in line with previously published data.2,21 Higher levels of total blood cholesterol in CSA patients and a better blood lipid profile under TAC therapy were also observed in patients after renal transplantation.17 In contrast to a meta-analysis performed by Penninga et al a higher number of infection-related deaths were observed in TAC patients in our study cohort.22 Regarding total mortality, however, no statistically significant differences were observed. It has to be admitted that, regarding mortality, mean donor age and ischemic time were higher in TAC patients, reflecting the shortage of donor organs. A reported higher blood pressure in patients with CSA as primary immunosuppression was seen in our study cohort as well as in other published studies.22,23
Limitations
This study was performed as a single-center study. As all patients were followed-up according to center’s specific protocol, results cannot be completely compared with other HTX centers. Therefore, further randomized multicenter studies must be performed. However, possible confounding factors, eg, effects of different induction therapies, were minimized by this study approach. To exclude possible confounders, multivariate risk analysis regarding development of AR was applied. Given the long inclusion period, an era effect cannot be completely excluded.
Conclusion
Our study analyzed the rejection profile of patients on CSA-based therapy and patients on TAC-based therapy after HTX. We detected a superior rejection profile in patients with a primary TAC-based immunosuppressive regimen. Moreover, subgroup analysis showed a trend toward superiority of prolonged-release TAC. Analysis of renal parameters showed a favorable effect on renal function under TAC therapy. We conclude that a TAC-based immunosuppressive regimen is superior in avoidance of ARs after HTX. In conclusion, we suggest that both extended-release TAC and conventional TAC are effective in protecting from AR.
Footnotes
Disclosure
Andreas O Doesch received a research grant from Astellas Pharma GmbH, Munich, Germany. All human studies have been reviewed by the ethics committee of the University of Heidelberg and have therefore been performed in accordance with the ethical standards laid down in the 2008 Declaration of Helsinki. The authors report no other conflicts of interest in this work.
References
- 1.Stehlik J, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: Twenty-eighth Adult Heart Transplant Report – 2011. J Heart Lung Transplant. 2011;30(10):1078–1094. doi: 10.1016/j.healun.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 2.Guethoff S, Meiser BM, Groetzner J, et al. Ten-year results of a randomized trial comparing tacrolimus versus cyclosporine a in combination with mycophenolate mofetil after heart transplantation. Transplantation. 2013;95(4):629–634. doi: 10.1097/TP.0b013e318277e378. [DOI] [PubMed] [Google Scholar]
- 3.Todo S, Fung JJ, Demetris AJ, Jain A, Venkataramanan R, Starzl TE. Early trials with FK 506 as primary treatment in liver transplantation. Transplant Proc. 1990;22(1):13–16. [PMC free article] [PubMed] [Google Scholar]
- 4.Starzl TE, Fung J, Jordan M, et al. Kidney transplantation under FK 506. JAMA. 1990;264(1):63–67. [PMC free article] [PubMed] [Google Scholar]
- 5.Armitage JM, Kormos RL, Fung J, et al. Preliminary experience with FK 506 in thoracic transplantation. Transplantation. 1991;52(1):164–167. doi: 10.1097/00007890-199107000-00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Armitage JM, Kormos RL, Griffith BP, et al. A clinical trial of FK 506 as primary and rescue immunosuppression in cardiac transplantation. Transplant Proc. 1991;23(1 Pt 2):1149–1152. [PMC free article] [PubMed] [Google Scholar]
- 7.Azzi JR, Sayegh MH, Mallat SG. Calcineurin inhibitors: 40 years later, can’t live without …. J Immunol. 2013;191(12):5785–5791. doi: 10.4049/jimmunol.1390055. [DOI] [PubMed] [Google Scholar]
- 8.Kino T, Hatanaka H, Miyata S, et al. FK-506, a novel immunosuppressant isolated from a Streptomyces. II. Immunosuppressive effect of FK-506 in vitro. J Antibiot (Tokyo) 1987;40(9):1256–1265. doi: 10.7164/antibiotics.40.1256. [DOI] [PubMed] [Google Scholar]
- 9.Ho ET, Wong G, Craig JC, Chapman JR. Once-daily extended-release versus twice-daily standard-release tacrolimus in kidney transplant recipients: a systematic review. Transplantation. 2013;95(9):1120–1128. doi: 10.1097/TP.0b013e318284c15b. [DOI] [PubMed] [Google Scholar]
- 10.Kobashigawa JA, Miller LW, Russell SD, et al. Study Investigators Tacrolimus with mycophenolate mofetil (MMF) or sirolimus vs cyclosporine with MMF in cardiac transplant patients: 1-year report. Am J Transplant. 2006;6(6):1377–1386. doi: 10.1111/j.1600-6143.2006.01290.x. [DOI] [PubMed] [Google Scholar]
- 11.Mehra MR, Uber PA, Scott RL, Park MH. Ethnic disparity in clinical outcome after heart transplantation is abrogated using tacrolimus and mycophenolate mofetil-based immunosuppression. Transplantation. 2002;74(11):1568–1573. doi: 10.1097/00007890-200212150-00014. [DOI] [PubMed] [Google Scholar]
- 12.Sánchez-Lázaro IJ, Almenar L, Martínez-Dolz L, et al. A prospective randomized study comparing cyclosporine versus tacrolimus combined with daclizumab, mycophenolate mofetil, and steroids in heart transplantation. Clin Transplant. 2011;25(4):606–613. doi: 10.1111/j.1399-0012.2010.01309.x. [DOI] [PubMed] [Google Scholar]
- 13.Grimm M, Rinaldi M, Yonan NA, et al. Superior prevention of acute rejection by tacrolimus vs cyclosporine in heart transplant recipients – a large European trial. Am J Transplant. 2006;6(6):1387–1397. doi: 10.1111/j.1600-6143.2006.01300.x. [DOI] [PubMed] [Google Scholar]
- 14.Lund LH, Edwards LB, Kucheryavaya AY, et al. International Society for Heart and Lung Transplantation The Registry of the International Society for Heart and Lung Transplantation: Thirtieth Official Adult Heart Transplant Report – 2013; focus theme: age. J Heart Lung Transplant. 2013;32(10):951–964. doi: 10.1016/j.healun.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 15.Stewart S, Winters GL, Fishbein MC, et al. Revision of the 1990 working formulation for the standardization of nomenclature in the diagnosis of heart rejection. J Heart Lung Transplant. 2005;24(11):1710–1720. doi: 10.1016/j.healun.2005.03.019. [DOI] [PubMed] [Google Scholar]
- 16.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 17.Wang CH, Ko WJ, Chou NK, Wang SS. Efficacy and safety of tacrolimus versus cyclosporine microemulsion in primary cardiac transplant recipients: 6-month results in Taiwan. Transplant Proc. 2004;36(8):2384–2385. doi: 10.1016/j.transproceed.2004.08.059. [DOI] [PubMed] [Google Scholar]
- 18.Doesch AO, Mueller S, Akyol C, et al. Increased adherence eight months after switch from twice daily calcineurin inhibitor based treatment to once daily modified released tacrolimus in heart transplantation. Drug Des Devel Ther. 2013;7:1253–1258. doi: 10.2147/DDDT.S52820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meiser BM, Groetzner J, Kaczmarek I, et al. Tacrolimus or cyclosporine: which is the better partner for mycophenolate mofetil in heart transplant recipients? Transplantation. 2004;78(4):591–598. doi: 10.1097/01.tp.0000129814.52456.25. [DOI] [PubMed] [Google Scholar]
- 20.Zezina L, Vessby B, Larsson E, Backman U, Fellström B. Carvedilol treatment of kidney graft recipients with chronic rejection. Clin Transplant. 1999;13(6):484–490. doi: 10.1034/j.1399-0012.1999.130608.x. [DOI] [PubMed] [Google Scholar]
- 21.Ekberg H, Tedesco-Silva H, Demirbas A, et al. ELITE-Symphony Study Reduced exposure to calcineurin inhibitors in renal transplantation. N Engl J Med. 2007;357(25):2562–2575. doi: 10.1056/NEJMoa067411. [DOI] [PubMed] [Google Scholar]
- 22.Penninga L, Møller CH, Gustafsson F, Steinbrüchel DA, Gluud C. Tacrolimus versus cyclosporine as primary immunosuppression after heart transplantation: systematic review with meta-analyses and trial sequential analyses of randomised trials. Eur J Clin Pharmacol. 2010;66(12):1177–1187. doi: 10.1007/s00228-010-0902-6. [DOI] [PubMed] [Google Scholar]
- 23.Ye F, Ying-Bin X, Yu-Guo W, Hetzer R. Tacrolimus versus cyclosporine microemulsion for heart transplant recipients: a meta-analysis. J Heart Lung Transplant. 2009;28(1):58–66. doi: 10.1016/j.healun.2008.10.004. [DOI] [PubMed] [Google Scholar]


