Abstract
Objective
To evaluate the clinical effectiveness and patients’ acceptance of soft tissue diode laser, for the elimination of hyper pigmented areas of the gingivae and buccal mucosa.
Subjects and methods
Twenty patients complaining of dark localized areas in their gingivae of upper and lower jaws, or in cheek mucosa were included in this study. All are females ages ranged from 18–37 with average of 27.5 years. The patients were all not pregnant, and free from any systemic diseases, and had no other areas of hyperpigmentation.
Results
Most of the patients (18 Pts.) required two treatment sessions to remove the melanotic lesions satisfactorily. The patients were seen after one, two, and three weeks respectively. Eight patients (40%) had a good response after one week, Ten patients (50%) had a very good response after two weeks, while only two patients (10%) had a bad result and required a third treatment session after two weeks. At the third week postoperatively in the successful cases, restoration of the normal gingival and mucosal texture and color was achieved with optimal esthetic results. Most of the patients had no postoperative discomfort including: pain, edema and disfigurement.
Conclusion
The soft tissue diode laser can be considered as a reliable mean for elimination of melanotic lesions of the gingivae or buccal mucosa, and is well tolerated by the patients.
Keywords: hyperpigmentation, soft tissue diode laser, patient response
Introduction
Oral pigmentation can appear at any age in the gingivae, mucosa, hard palate and tongue. These can be of genetic origin as racial or physiological pigmentation, Pigmented nevi, and Albright syndrome. Acquired oral pigmentation can occur as a result of endogenous or exogenous factors. The endogenous pigmentation often occurs during the course of certain diseases like Addison’s disease, Acanthosis Nigricans, and Cooley’s anemia, while exogenous pigmentation may be due to amalgam tattoo, lead poisoning, Argyria, antimalarial drugs or smoker’s melanosis. (1) Hyper pigmentation of gingiva often occurs in the gingiva due to abnormal deposition of melanin in the basal and supra basal layer of the epithelium, creating a unaesthetic appearance. The effective elimination of such melanotic areas was attempted by variable means such as ; scalpel surgery; gingivectomy with free-gingival autografting or allografting, (2,3) electrosurgery, cryosurgical depigmentation through the use of gas expansion system, (4) chemical agents such as phenol 90% and alcohol 95%, (5) abrasion with diamond burs (3) as well as laser surgery such as; Neodymuim–Yttrium garnet (ND:YAG) Laser, Co2 Laser and semiconductor diode Laser. (6) Researchers in selective photothermolysis and treatment of cutaneous pigmented lesions have been performed with various lasers. (7,8) Selective photothermolysis to treat melanotic lesions was first proposed by Anderson and Parrish in 1983. (9) This phenomenon is based on the fact that some structures absorb light of certain wavelength better than others. The absorption of light leads to heat production and consequently to damage of structures when a high enough temperature is reached. As absorption by each structure is wavelength dependent, it is possible to selectively damage certain regions in a tissue by choosing a wavelength with high absorption by the target and low absorption by others. (2,9) Although the literature reports great variability in the values, (3,10) the absorption coefficient of melanosomes for red light may be estimated to be several hundreds of reciprocals centimeters. In addition to the wavelength the proper pulse length is another parameter that is essential for the achievement of selective photocoagulation decreases the selectivity of tissues to photothermolysis. Research in selective photothermolysis and treatment of pigmented lesions has been accomplished with various lasers, including 10.600 nm Co2, (2) 1060nm, 532 nm and 355 nm Neodymuim–Yttruim garnet 351 nm excimer, (8) 694 nm Quartz-switched ruby (7) and 488/514 nm argon laser. (7,9,10) Most of these are pulsed lasers that are able to produce pulses smaller than, or in the order of magnitude of, the thermal relaxation time of a melanosome which is around 1 microsecond. The soft tissue Diode laser SoftLase Pro is a compact and reliable surgical instrument for use in dental applications. Flexible fiber optic cables are the most widely accepted delivery system for diode laser power; the 400μm diameter single-core quartz fiber is mounted into standard connectors. It produces an invisible infra-red and a visible aiming beam. The wavelength is 808±5nm, such wavelength characteristics specially target the soft tissues. It has an affinity for hemoglobin and melanin; therefore it is more efficient and better equipped to address deeper soft tissue problems. (5, 11)
Aim of the work
The purpose of this study was to assess the clinical effectiveness and patients’ responsiveness for the Soft Tissue Diode Laser in the elimination of gingival and mucosal hyperpigmentation.
Subjects and Methods
Twenty patients complaining of unsightly hyper pigmented areas in their gingivae, labial and cheek mucosa were included in this study, especially those patients with gummy smile (very high gum line). The patients were all females, their ages ranged from 18–37 with average of 27.5 years, from those attending the Outpatient Dental Clinic of Taif University Girl’s branch. Clinical assessment was made prior to treatment at the first visit. All patients were non pregnant, they were apparently healthy without any systemic diseases, or manifestations of other areas of hyper pigmentations, as nail pigmentation–etc. All patients were non-smokers and were not exposed to metal vapors as occupational hazards i.e. the melanotic spots were of physiological or racial nature. The procedure was explained verbally and animatedly to the patients and informed signed consents were obtained according to the World Declaration Statement of Helsinki. (12)
Methods (Treatment technique)
Patient and operating staff wore special diode-laser protective eye glasses. Highly reflective instruments or instruments with mirrored surfaces were avoided as there could be reflection of the laser beam. A soft tissue diode surgical laser unit (Discuss SoftLase Pro, LLC of ZAP Lasers, Culver City, CA90232 USA), delivered by a 400-μm diameter fiber wavelength 808nm ± 5, power 1–2 W was used for depigmentation of the maxillary and mandibular anterior gingiva and buccal mucosa. The diode laser was emitted in continuous mode, and was operated in a contact method using a flexible fiber optic hand piece with initiated tip. The Laser settings used were: fluent between 5 and 15J/cm2, pulse length between 20 and 50 ms, spot diameter of 2 mm and thermal relaxation times of 0.15 to 0.20 milliseconds. No topical or local anesthesia was given to patients. Laser ablation started from the mucogingival junction toward the free gingival margin, including papillae. Regarding the labial or cheek mucosa the motion of ablation was circular with overlapping circles. During the procedure, laser ablated the gingival and or mucosal epithelial surfaces little by little to reach the pigments without causing any bleeding which was beneficial for clear visualization. To enhance visualization, normal saline-soaked cotton or gauze was used to remove epithelial remnant. The power output at the end of the fiber was adjusted with power increase or power decrease touch pad until it measured from 1.2W up till 2W. The used treatment was aiming beams to irradiate the pigmented lesions at 1.5 W. Pulse rate selected was with contact fiber mode (initiated tip). Anesthesia was not used in all cases, but if needed according to patient’s desire; local anesthesia was achieved using 1.8ml mepivacaine 2% without vasoconstrictor, although more than one carpule was used when large areas were treated. After about 3–5 minutes, the treatment began. Irradiation was done by a contact mode for the fiber; a slight degree of carbonization at the gingival or mucosal surface was seen. During treatment the temperature of the tissue often quickly reaches high values. It was not necessary to treat the entire surface of the lesion. In spite of the beam being focused to a spot size of only 2mm in diameter, the heat effect exceeded this diameter as a result of conduction. Irradiation of spots approximately 1mm apart appeared to sufficiently affect the area in-between. A thin layer of carbonized material appeared at the irradiated spot. After having irradiated the pigmented lesions, the wounds appeared fresh with no bleeding and there were no need to apply periodontal dressing or pack. The patients were instructed to avoid eating hot or spicy food for the first 24 hours and to gargle with Aloe Dent mouth wash 3 times/a day preferably after meals for one week. No pain medications were generally prescribed, but if needed a mild analgesic anti-inflammatory (sodium diclofenac 50mg =Rofenac) twice a day was given.
Post-operative assessment
The patients were seen after one, two, and three weeks post-operatively, and were examined for post-operative discomfort; including pain, edema, and disfigurement in the form of hypopigmentation (i.e. treatment response). Clinical parameters were measured using Visual Analogue Scale (VAS), through answering a questionnaire specifically designed for this research. (13)
Results
No patients had marked complications, and infection did not occur during the healing of the gingivae. In two patients (10%), some areas of pigmentation remained and required a third session after two weeks. Regarding pain: it was assessed using Visual Analogue Scale. (13,14) Operationally a VAS is usually a horizontal line, 100 mm in length, anchored by word descriptors at each end (no pain at one end till very severe pain on the other end). Patients were asked to mark on the line the point that they feel represents their perception of their current state. The VAS score is determined by measuring in millimeters from the left hand end of the line to the point that the patient marks.
Only three patients (15%) marked on a point equivalent to mild pain and thus they required mild analgesic. Regarding edema: It was measured by a graduated tape (14) although it was not seen in most of the patients at the first week, only two patients(10%) presented with slight edema in the attached gingiva at the mucogingival junction, which disappeared completely at the 2ndweek. While in patients with cheek mucosal depigmentation no post ablation edema was seen.
Regarding the post-operative appearance and the patient acceptance for the treatment (treatment response): It was registered on a scale measuring patients’ satisfaction with the present situation and the psychologic impact of their oral health status with their responses marked on a Visual Analog Scale (VAS) with four values subjectively (very good, good, fair, and bad). A very good score was registered when both the dentist and the patient were satisfied with the final result. A good response was considered to be achieved when the doctor was satisfied by the result, but the patient considered that it would have been better. A fair result was scored when both the doctor and the patient estimated that the treatment could have given a better result. A bad result (no response) was registered when the treatment did not produce noticeable positive changes from the initial status.
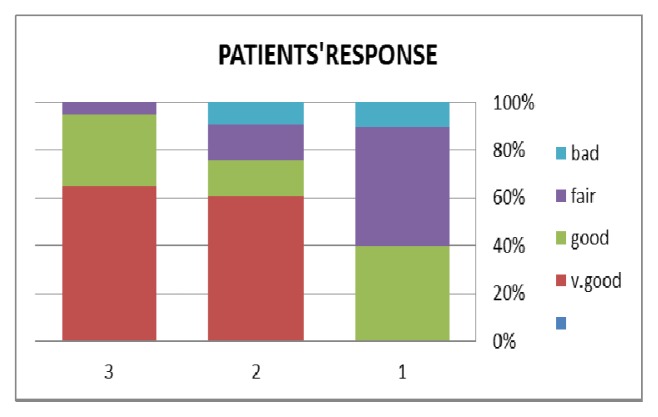
Results were graphed as seen in Figure (1).
Fig (1).
Patients’ responsiveness for the esthetic outcome of laser treatment of their gingival and cheek mucosa.
At the First post-operative week
Eight patients (40%) were classified as having a good result. Ten (50%) as having a fair result, while only two patients (10%) as having a bad result i.e. no response.
At the Second week post-operatively: twelve patients representing (60%) were seen with a very good result, three patients (15%) with good result and another three patients (15%) had fair result, and two patients (10%) came with a bad result.
At the third post-operative week: thirteen patients representing (65%) were seen with a very good results, while six patients (30%) came with good results, and only one patient (5%) presented with a fair result. More than half of the patients(12pts.) included in the study were available within nine months follow-up, during this period no recurrence of the pigmentation appeared, while the remaining patients did not show up.
Discussion
Although the melanin pigmentation of the gingiva is a completely benign condition and does not present a medical problem, yet complaints of black gums are common. Demand for treatment is usually made for esthetic reasons however; there is not much information in the literature about the depigmentation of the gingiva. (7)
Several treatment modalities were applied for the treatment of such melanotic spots Perlmutter et al, (7, 15) and Dummett and Bolder (16) have reported surgical removal of portions of pigmented gingiva. After surgery, it was necessary to cover the exposed lamina propria with periodontal packs for 7to 10 days; the wound took 6 weeks to heal and left a delicate scar.
Cryosurgery is a method of tissue destruction by rapid freezing. There have been several reports on the cryosurgical treatment of a variety of oral lesions (15, 16) but only Tal et al, (10) described the depigmentation of gingival by cryosurgery. Others reported the successful use of liquid nitrogen and cotton swabs to eliminate the pigmented areas. (3)
Various lasers have been utilized for the treatment of cutaneous pigmented lesions. (17, 18, 19) Trelles et al, (19, 20) were the first to treat patients with pigmented gingiva by Argon laser. The Ruby laser has been successfully used in Q- switched mode to treat a variety of pigmented lesions. (3, 6, 11) The short pulses of the light emitted in the nanosecond domain by the Q-switched Ruby laser produce thermal and or mechanical damage to melanosomes, which results in cellular destruction confirmed to the targeted melanocyte, a process, which has been termed selective photothermolysis. Regarding the post-operative clinical assessment of pain and edema, diode laser was well tolerated by the patients where analgesics were not prescribed only if necessary, in accordance with other investigations, (21,22) as well as edema was minimally found and in limited cases. (23, 24)
In agreement with this study, several studies have shown melanosomes to be suitable targets for selective photothermolysis at various laser wavelengths when irradiated in sub microsecond pulses with energy densities around1J/cm2. (9, 25, 26) The pulse length is the important difference between the parameters as used in this clinical study for elimination of melanotic lesions, and those described in most of the literature of the pigmented lesions of the skin. (6,9,11) Excellent results were achieved with pulse lengths of 300ms being much longer than the estimated relaxation time for the melanosomes. It is obvious that a mechanism different from ordinary photothermolysis plays a role in the elimination of the pigmented oral lesions using the described parameters. During the relatively long pulses, a considerable part of heat is conducted away from the targets to surrounding structures and general heating is the result. (9,10) Although a relatively low power is used (1.4W) in the present study, this in combination with a spot size of 0.5mm and a pulse length 300ms leads to a very high energy densities. As a result of both the heat diffusion and the light diffusion through scattering, two main effects appear from irradiation with the previously mentioned parameters; a coagulated and necrotized layer, together with an underlying area that is only partially coagulated, the extent of irreversibly damaged melanocytes gradually decreases with depth in this underlying area. This may be a crucial point in the mechanism of action, (24,25) although the remaining melanocytes may be fewer than normal, yet they may produce enough melanin to re-pigment the newly formed mucosa during and after the healing period, thus equalizing the pigmentation with the surrounding tissue. (16) In the present study, it appeared that the melanocytes where not sufficiently destructed in all cases, so that repeated laser applications were necessary especially in the patients with fair and bad results. It was reported that, enough melanocytes are destroyed to remove the over pigmentation but, at the same time, some underlying melanocytes are not sufficiently affected by the heat to be destroyed. (26, 27) Some other mechanisms of re-pigmentation might be found in those areas in which melanocytes have been removed or destroyed. As for example migration of melanocytes several weeks after treatment. Although the 300ms pulses allowed the heat produced to partially damage the non melanin containing structures, the wounds healed with a good cosmetic appearance, this finding was previously supported in the literature. (19, 20) Treatment with short pulsed Lasers may be theoretically safe but those lasers are not commonly available in hospitals or clinics. In contrast, the soft tissue diode laser is a common instrument, available in most clinics and hospitals due to its cheapness and lightness so it is easily transported from place to place. although the Co2 laser is preferred over the Argon laser and the Nd: YAG lasers, because it is most selectively absorbed, the Co2 laser totally evaporates the tissue layer by layer, as its light is very well absorbed by any tissue containing water, (1,5,28) while the Argon and Diode Lasers light share the same mechanism of action of the ND:YAG laser which penetrates into the gingival tissue and is only absorbed by the melanin, resulting in much more selective destruction and far less damage to normal gingival tissue than does the Co2 laser. (29,30,31) In accordance to what previously mentioned in this present study, Bradley (17) in a review for the use of the Nd: YAG Laser in oral and maxillofacial surgery, reported that Nd: YAG Laser wavelength exhibits minimal tissue absorption and maximal penetration by comparison with the Co2 laser’s maximal temporo-mandibular joint. Promising developments include Co2; Nd: YAG lasers combination and the introduction of diode technology. (18)
We conclude that in comparison with the treatment modalities discussed previously to treat the pigmented areas of the gums, the diode laser is a useful and a safe mean and is the preferred laser when no other short pulse lasers are available.
Conclusion
In conclusion, it is reported that the soft tissue diode laser wavelength exhibits maximal tissue absorption and minimal penetration by comparison with the Nd: YAG Laser’s minimal tissue absorption and maximal penetration. (1) These properties allow a variety of uses in maxillofacial surgery particularly coagulation of angiomatous lesions, hemostasis in bleeding diatheses, arthroscopic surgery of temporo-mandibular joint. Promising developments include Co2, ND: YAG combination Lasers, Potassium titanyl-phosphate (KTP): ND: YAG apparatus and the introduction of Diode technology. (9) Therefore, in comparison with the treatment modalities mentioned previously to treat the pigmented areas of the gums, the Diode Laser is a useful and a safe mean, and is the preferred laser when no other short pulse Lasers are available.
Fig (2).

Preoperative photo showing hyperpigmentation in the upper attached gingival
Fig (3).

Immediate operative view after Laser application
Fig (4).

two weeks postoperatively showing the disappearance of the pigmentation
Fig (5).
showing the application of soft tissue diode Laser beam.
Fig (6).

Immediate post-operative photo showing slight reduction in gingival hyperpigmentation in upper rather than the lower gingiva.
Fig (7).

Post-operative photo after application of Laser for upper gingiva only. Notice the difference between upper and lower untreated (one week postoperatively).
Fig (8).
Preoperative photo showing hyperpigmentation in the cheek mucosa.
Fig (9).

Immediate postoperative photo showing the effect of laser beams on the cheek mucosa.
Fig (10).

Two weeks postoperatively showing the improvement of the dark appearance of the cheek mucosa
References
- 1.Esen E, Haytac MC, Oz IA, Erdoğan O, Karsli ED. Gingival melanin pigmentation and its treatment with CO2 laser. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:522–7. doi: 10.1016/j.tripleo.2004.02.059. [DOI] [PubMed] [Google Scholar]
- 2.Lagdive S, Doshi Y, Marawar PP. Management of gingival hyperpigmentation using surgical blade and diode laser therapy: A comparative study. J Oral Laser Appl. 2009;9:41–7. PubMed. [Google Scholar]
- 3.Humagain M, Nayak DG, Uppoor AS. Gingival depigmentation: A case report with review of Literature. J Nepal Dent Assoc. 2009;10:53. [Google Scholar]
- 4.Suthprasertporn S. Treatment of gingival melanin hyperpigmentation by Er, Cr:YSGG laser: Report of 2 cases. Thai J Periodontol. 2007;1:46–55. PubMed. [Google Scholar]
- 5.Ozbayrak S, Dumlu A, Ercalik-Yalcinkaya S. Treatment of melanin pigmented gingiva and oral mucosa with CO 2 laser. Oral Surg. Oral Med Oral Pathol. Oral Radiol. Endod. 2000;90:14–5. doi: 10.1067/moe.2000.106396. [DOI] [PubMed] [Google Scholar]
- 6.Miyasaki MA. Shedding light on the soft tissue laser. Signature. 2004;11:11–3. [Google Scholar]
- 7.Perlmutter S, Tal H. Re-pigmentation of the gingiva following surgical injury. J Periodontol. 1986;57:48–50. doi: 10.1902/jop.1986.57.1.48. [DOI] [PubMed] [Google Scholar]
- 8.Atsawasuwan P, Greethong K, Nimmanon V. Treatment of gingival hyperpigmentation for esthetic purposes by Nd: YAG laser: Report of 4 cases. J Periodontol. 2000;71:315–21. doi: 10.1902/jop.2000.71.2.315. [DOI] [PubMed] [Google Scholar]
- 9.Anderson RR, Parrish JA. Selective photothermolysis. Precise Microsurgery by Selective Absorption of Pulsed Radiation. Science. 1983;220:524–526. doi: 10.1126/science.6836297. [DOI] [PubMed] [Google Scholar]
- 10.Tal H, Oeglesser D, Tal M. Gingival depigmentation by Erbium: YAG laser: Clinical observation and patient responses. J Periodontol. 2003;74:1660–7. doi: 10.1902/jop.2003.74.11.1660. PubMed. [DOI] [PubMed] [Google Scholar]
- 11.Sommer S, Render C, Burd R, Sheehan-Dare R.Ruby Laser Treatment for hirutism, Clinical response and patient toleranceBr Journal of Dermatol 19981009–1014. 138 [DOI] [PubMed] [Google Scholar]
- 12.World Medical Association Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects. Adopted by the 18th WMA General Assembly; Helsinki, Finland. June 1964. [Google Scholar]; and amended by the 59th WMA General Assembly; Seoul. October 2008. [Google Scholar]
- 13.Gould D, et al. Visual Analogue Scale (VAS) Point of Information., Blackwell Science Ltd. Journal of Clinical Nursing. 2001;10:697–706. doi: 10.1046/j.1365-2702.2001.00525.x. [DOI] [PubMed] [Google Scholar]
- 14.Wewers ME, Lowe NK. A critical review of visual analogue scales in measurement of clinical phenomena. Research in Nursing and Health. 1990;(13):227–236. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 15.Yeh Chin-Jyh. Cryosurgical treatment of melanin pigmented gingival. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:660–3. doi: 10.1016/s1079-2104(98)90199-8. [DOI] [PubMed] [Google Scholar]
- 16.Dummet CO, Bolden TE. Post-surgical clinical re-pigmentation of the gingiva. Oral Surg Oral Med Oral Pathol. 1963;16:353–65. [Google Scholar]
- 17.Bradely PF. A review for the use of Neodymuim YAG laser in Oral and maxillofacial Surgery. Br Journal of Oral and Maxillofac Surg. 1997;35:26–35. doi: 10.1016/s0266-4356(97)90005-x. [DOI] [PubMed] [Google Scholar]
- 18.Gupta G. Management of gingival hyperpigmentation by semiconductor diode laser. J Cutan Aesthet Surg. 2012;4(25):208–10. doi: 10.4103/0974-2077.91256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trelles MA, Verkrysse W, Segui JM, Udaeta A. Treatment of melanotic spots in the gingiva by Argon Laser. J. Oral & Maxillofac Surg. 1993;51:759–761. doi: 10.1016/s0278-2391(10)80416-1. [DOI] [PubMed] [Google Scholar]
- 20.Trelles MA, Verkrysse W, Pickering JW. Monoline argon laser (514nm) treatment of melanin pigmented lesions with long pulse lengths. Photo Chem. Photobiol. 1992;16:357. doi: 10.1016/1011-1344(92)80023-o. [DOI] [PubMed] [Google Scholar]
- 21.Dalia AR, Nermeen HM, Ahmed AZ. Effectiveness of Low Power Laser Therapy and Betamethasone in Minimizing Postoperative Edema and Trismus after Third Molar Surgery: a Clinical Trial. Journal of American Science. 2010;6(12):986–989. [Google Scholar]
- 22.Carrillo SJ, Calatayud J, Manso JF, Barberia E, Martinez MJ, Donado M. Randomized double-blind clinical trial on effectiveness of helium-neon laser in the prevention of pain swelling and trismus after removal of impacted third molars. Int Dent J. 1990;40:31–36. [PubMed] [Google Scholar]
- 23.Shahzad AS, Irfanullah K, Humer K. Effectiveness of Sub mucosal Dexamethasone to Control Postoperative Pain & Swelling in Apicectomy of Maxillary Anterior Teeth. Int. J Health Sci. Qassim Univ. 2011;5(2):156–165. [PMC free article] [PubMed] [Google Scholar]
- 24.Fontana, Kurachi, Mendonca, et al. Temperature variation at soft periodontal and rat bone tissues during a medium-power diode laser exposure. Photo med. Laser Surg. 2004 Dec;22(6):519–522. doi: 10.1089/pho.2004.22.519. [DOI] [PubMed] [Google Scholar]
- 25.Jacques SL, Mc Auliffe DJ. The melanosome threshold temperature for explosive vaporization and internal absorption coefficient during pulsed laser irradiation. Photochem Photobiol. 1991;6:79. doi: 10.1111/j.1751-1097.1991.tb09891.x. [DOI] [PubMed] [Google Scholar]
- 26.Ara G, Anderson RR, Mandel KJI. Irradiation of pigmented melanosomes cells with high intensity pulse radiation generates acoustic waves and kills cells. Lasers Surg Med. 1990;10:52–54. doi: 10.1002/lsm.1900100112. [DOI] [PubMed] [Google Scholar]
- 27.Borrajo, Varela, Castro, et al. Diode laser (980 nm) as adjunct to scaling and root planning. Photomed Laser Surg. 2004;22:509–512. doi: 10.1089/pho.2004.22.509. [DOI] [PubMed] [Google Scholar]
- 28.Ciancio, Kazmierczak, Zambon, et al. Clinical effects of diode laser treatment on wound healing. AADR. 2006 abs 2183. [Google Scholar]
- 29.Castro, Gallas, Nunez, et al. Histological evaluation of the use of diode laser as an adjunct to traditional periodontal treatment. Photo medicine and Laser Surgery. 2006;24(1):64–68. doi: 10.1089/pho.2006.24.64. [DOI] [PubMed] [Google Scholar]
- 30.Bach, Neckel, Mall, et al. Conventional versus laser assisted therapy of peri-implantitis: a five-year comparative study. Implant Dent. 2003;9:247–251. doi: 10.1097/00008505-200009030-00010. [DOI] [PubMed] [Google Scholar]
- 31.Beeher ME, Houston GD, Young JD. Oral pigmentation secondary to minocycline therapy. J Oral Maxillofac Surg. 1986;44:582–584. doi: 10.1016/s0278-2391(86)80104-5. [DOI] [PubMed] [Google Scholar]