Abstract
Objectives. We examined the impact of a prenatal exercise intervention on physical activity in 260 women at risk for gestational diabetes mellitus.
Methods. We randomized participants in the Behaviors Affecting Baby and You (BABY) Study, which took place from 2007 to 2012, to either a 12-week individually tailored, motivationally matched exercise intervention (n = 132) or to a comparison health and wellness intervention (n = 128). We assessed physical activity with the Pregnancy Physical Activity Questionnaire. We used linear mixed models to evaluate the impact of the interventions on change in physical activity according to intensity and type, total walking, and sedentary behavior.
Results. Compared with the health and wellness arm, the exercise arm had significantly greater increases in sports or exercise activity (0.3 vs 5.3 metabolic equivalent of task [MET] hours/week; P < .001), and smaller declines in total activity (–42.7 vs –2.1 MET hours/week; P = .02) and activities of moderate to vigorous intensity (–30.6 vs −10.6 MET hours/week; P = .05), and was more likely to achieve recommended guidelines for physical activity (odds ratio = 2.12; 95% confidence interval = 1.45, 3.10).
Conclusions. These findings extend the previous literature by demonstrating the benefits of a clinically feasible exercise intervention in an ethnically and socio-economically diverse population. Given the increased risk of adverse maternal health outcomes in ethnic minority groups, these findings may have important implications for reducing health disparities.
The American College of Obstetricians and Gynecologists (ACOG) recommends that all women who are free from medical or obstetric complications engage in 30 minutes or more of moderate intensity physical activity on most days of the week.1 Physical activity during pregnancy is associated with reduced risk for excess gestational weight gain,2–4 and a reduced risk of gestational diabetes mellitus (GDM)5 and preeclampsia.6 Despite the benefits of physical activity, pregnant women are less likely to meet physical activity recommendations than nonpregnant women of childbearing age.7,8 Furthermore, physical activity levels decline throughout pregnancy, even in women who were active before pregnancy.9,10 Physical activity levels are even lower in Hispanic women; Hispanic women are 40% less likely to meet recommended levels of physical activity than are non-Hispanic White women.11 These numbers are concerning because of the excess risk of adverse maternal outcomes, such as GDM, in Hispanic women.12 Thus, it is important to develop culturally adapted interventions that can engage pregnant women in more active lifestyles.
The impact of exercise interventions during pregnancy has been conflicting. Several interventions have been successful at attenuating the decrease in physical activity levels over the course of pregnancy13–15; however, most studies have observed no impact.16–20 In addition, the majority of the successful interventions to date have been conducted in predominantly White non-Hispanic study populations or have used intensive interventions that may not be feasible in clinical practice.21
Individually tailored, motivationally matched interventions have been shown to be cost-effective approaches to increasing physical activity in nonpregnant women in community settings.22,23 These interventions are also readily translatable to clinical practice. However, whether these programs are effective at increasing physical activity during pregnancy is unknown. Therefore, we assessed the effectiveness of an individually tailored, motivationally matched exercise intervention on physical activity levels in an ethnically diverse sample of pregnant women at high risk for GDM.
METHODS
The Behaviors Affecting Baby and You (BABY) study was a randomized controlled trial of an exercise intervention with the overall goal of preventing the development of GDM in pregnant women at high risk. Our aim was to evaluate 1 of the primary aims of the study: the impact of exercise intervention on change in physical activity. Our study was based in the ambulatory obstetrical practices of Baystate Medical Center, a large tertiary care facility in Western Massachusetts that serves an ethnically and socioeconomically diverse population.
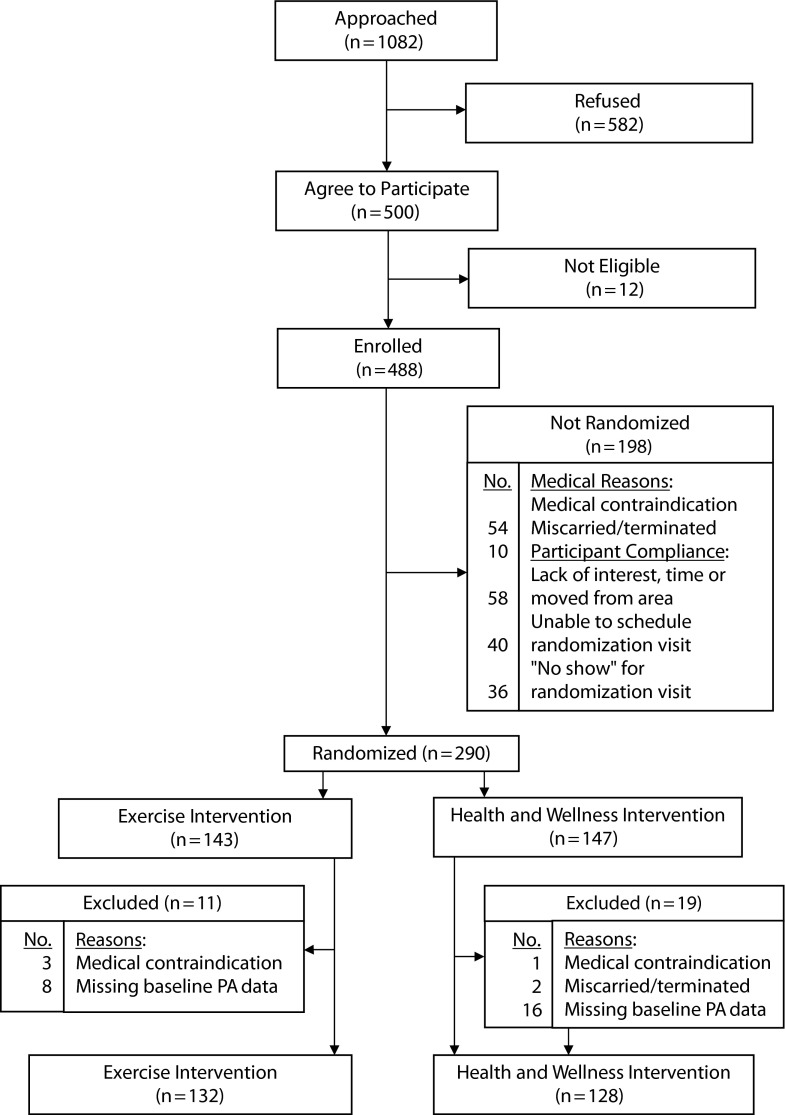
Health educators prescreened eligible patients from 2007 to 2012 using demographic and medical characteristics provided on a daily roster of scheduled patients to generate a list of potential participants. A total of 1082 women were prescreened as potential participants and invited to participate (Figure 1). Those who agreed were further screened for eligibility. Women were considered eligible for the study if they were in their first trimester of pregnancy, were between the ages of 16 and 40 years, and were at high risk for GDM, defined as either (1) overweight or obese with a family history of diabetes, or (2) had a diagnosis of GDM in a previous pregnancy defined according to the American Diabetes Association criteria.24 Exclusion criteria were the following:
contraindications to participating in moderate physical activity;
inability to read English at a sixth grade level;
self-reported current participation in more than 30 minutes of moderate or vigorous intensity exercise more than 3 days per week;
a diagnosis of diabetes outside of pregnancy, or diagnosis of hypertension, heart disease, or chronic renal disease;
use of current medications that adversely influence glucose tolerance; or
nonsingleton pregnancy.
FIGURE 1—
Flow diagram: Behaviors Affecting Baby and You (BABY) Study, Massachusetts, 2007–2012.
Note. PA = physical activity.
All women were required to sign a written informed consent as approved by the Institution Review Board of the University of Massachusetts-Amherst and Baystate Medical Center. The final sample included 260 participants: 132 in the exercise arm and 128 in the health and wellness arm (Figure 1).
A detailed description of the study design has been presented elsewhere.25 Briefly, eligible women were recruited at a prenatal visit in early pregnancy (mean = 11 weeks’ gestation) and randomized to either a 12-week individually tailored exercise intervention or a comparison health and wellness intervention. Women were not blinded to their assigned intervention group. The intervention began with 1 in-person session with a health educator who administered a tailoring questionnaire and set behavioral goals. Over the course of the study, both intervention arms received monthly booster telephone calls at 2, 6, and 10 weeks from health educators who provided individualized feedback and reviewed participants’ progress toward their behavioral goals. In addition, tip sheets were mailed weekly for the first 4 weeks of the intervention and then every other week thereafter. All intervention materials were written at a sixth grade reading level.
The intervention drew from the trans-theoretical model26 and social cognitive theory27 constructs for physical activity, which accounted for the individual’s stage of motivational readiness for change and the processes that help facilitate that change. The intervention took into account findings by our research group on the specific social, cultural, economic, and environmental resources and challenges faced by women of diverse backgrounds.28
Exercise Intervention
The overall goal of the exercise intervention was to encourage pregnant women to achieve ACOG guidelines for physical activity during pregnancy.29 The specific activities women engaged in were self-selected and included activities such as dancing, walking, and yard work. The weekly goals were to increase time spent in moderate intensity physical activity by 10% each week to safely progress toward the overall activity goals. The participants were provided a digital pedometer and an activity diary to encourage self-monitoring.
The 65-item tailoring questionnaire assessed the participants’ current stage of motivational readiness for physical activity adoption, self-efficacy, decisional balance, use of cognitive and behavioral processes of change, and time spent in physical activity. In light of responses to this questionnaire, health educators discussed barriers and facilitators to adopting physical activity. A stage-matched manual targeting the specific stage of motivational readiness to adopt physical activity was then given to the participants. These manuals included the benefits of physical activity, tips for stretching, building social support, goal setting, and strategies for overcoming barriers to physical activity.
Participants’ progress toward their behavioral goals was assessed via follow-up tailoring questionnaires that were mailed monthly with a postage paid return envelope. Based on the responses to these questionnaires, individually tailored reports were generated and mailed monthly to the participant, along with the corresponding stage-matched manual. Each tailored report described the individual’s current stage of motivational readiness for becoming active, mediators for physical activity (i.e., self-efficacy, benefits, and barriers for physical activity, and cognitive and behavioral processes), normative feedback, and feedback regarding progress toward physical activity goals since the previous assessment. If a tailoring questionnaire was not returned, the subsequent stage-matched manual was based on responses to the previous returned questionnaire. Monthly booster telephone calls provided individualized feedback based on their motivational readiness for physical activity adoption.
Health and Wellness Intervention
The health and wellness intervention received tips sheets and telephone booster calls on the same contact schedule as the exercise arm; this controlled for contact time, while keeping the content of the 2 interventions distinct. Specifically, after completion of the initial tailoring questionnaire, the health educator focused on general issues related to health and wellness during pregnancy instead of issues related to physical activity.
A series of ACOG informational booklets on general issues related to health and wellness during pregnancy were mailed to the participants weekly during the first 4 weeks of the intervention and then biweekly thereafter. These booklets were selected to represent high-quality standard, low-cost, self-help material currently available to the public. A follow-up tailoring questionnaire was mailed at week 12. Monthly booster telephone calls provided individualized feedback on progress toward health and wellness behavioral goals.
Physical Activity Assessment
The Pregnancy Physical Activity Questionnaire (PPAQ) was used to measure physical activity before randomization (baseline) and at the end of the 12-week intervention period by interviewers blinded to the study arm. The PPAQ is a semiquantitative instrument that has been previously validated in this study population.30 The PPAQ queries the usual time spent participating in 32 activities of either light, moderate, or vigorous intensity during the past month according to 4 activity types: household or caregiving, occupational, sports or exercise, and transportation. The number of minutes spent in each reported activity was multiplied by its metabolic equivalent of task (MET) level and summed to arrive at an estimate of average weekly MET hours per week. MET intensity scores were based on the Compendium of Physical Activities,31 with the exception of walking and light housework activities, for which field-based measures among pregnant women were used.30 In addition to total MET hours per week, physical activity was classified by intensity, type, and total walking. We combined moderate and vigorous intensity physical activity into a category of moderate-vigorous activity (MVPA) because few women reported spending time in vigorous activity. To estimate hours per week of sedentary behavior, participants were asked to report the amount of time spent watching TV or videos, or sitting or standing at home, work, or during transportation. Women with more than 7.5 MET hours per week of moderate-vigorous intensity activity in sports or exercise activities (i.e., 30 minutes/day of activity at ≥ 3 METs multiplied by 5 days/week) were considered to have met the ACOG physical activity guidelines.1
Demographic characteristics including age, ethnicity, education, annual household income, marital status, living situation (e.g., with a spouse or partner), smoking status (before pregnancy and during pregnancy), and the number of adults and children in the household were collected at the time of enrollment via standardized questionnaires. Weight and height before pregnancy were abstracted from the medical record. If weight before pregnancy was missing from the medical record (n = 3; 1%), it was based upon self-reported weight collected at the time of enrollment. Gestational age was abstracted from the medical records.
Statistical Analysis
We assessed all analyses using an intent-to-treat approach. We used the χ2 test or the Fisher exact test to compare the distribution of sociodemographic, medical history, and behavioral characteristics between the intervention arms at baseline. We used a Wilcoxon rank sum test to compare baseline physical activity between the study arms.
We used mixed model analyses, using PROC mixed in SAS version 9.3 (SAS Institute, Cary, NC), to evaluate the outcome of change in physical activity and sedentary behavior in the exercise intervention arm relative to the health and wellness intervention arm. The mixed model used fixed treatment and assessment period effects. We modeled the expected response at baseline as common for both arms because the participants were randomly assigned to treatment arms, and the assessment shortly preceded the randomization. The random effects in the model corresponded to participants and days (nested in participants). An advantage of this approach was that data could be included for women with only baseline measures. For such women, the missing data were assumed to be missing at random. We used logistic regression to compare the odds of achieving ACOG physical activity guidelines between intervention arms after the intervention. Because there were no statistically significant differences in baseline sociodemographic or medical history characteristics, we did not assess multivariable models.
RESULTS
Overall, the majority of the participants were young (mean age = 26.5 years), Hispanic (55%), and obese (61.9%; Table 1). There were no statistically significant differences between the intervention arms in any sociodemographic, medical history, or behavioral characteristic, such as cigarette smoking, at baseline, indicating that the randomization was successful (Table 1). There were no adverse effects of the intervention reported in either arm. Retention to delivery was slightly higher in the exercise arm (92%) compared with the health and wellness arm (87%; P = .19). Follow-up data on physical activity were similar in both arms, with approximately 66% and 67% of women in the exercise and health and wellness arms, respectively, completing the PPAQ after the intervention (P = .58). There were no statistically significant differences between those with and without PPAQ data after the intervention with respect to baseline sociodemographic, medical history, or physical activity characteristics, with the exception of small differences in activities of light intensity (125.2 vs 127.1 MET hours/week; P = .03) and walking METs (37.7 vs 33.9 MET hours/week; P = .045).
TABLE 1—
Baseline Characteristics of Participants (n = 260): Behaviors Affecting Baby and You (BABY) Study, Massachusetts, 2007–2012
| Variables | Total Population (n = 260), No. (%) | Exercise (n = 132), No. (%) | Health and Wellness (n = 128), No. (%) | P |
| Prepregnancy BMI, k/m2 | .18 | |||
| < 30 | 99 (38) | 45 (34) | 54 (42) | |
| ≥ 30 | 161 (62) | 87 (66) | 74 (58) | |
| Previous GDM | .21 | |||
| Yes | 26 (10) | 9 (7) | 17 (13) | |
| No | 211 (81) | 111 (84) | 100 (78) | |
| Missing | 23 (9) | 12 (9) | 11 (9) | |
| Family history of diabetes | .68 | |||
| Yes | 241 (93) | 124 (94) | 117 (91) | |
| No | 5 (2) | 2 (2) | 3 (2) | |
| Missing | 14 (5) | 6 (5) | 8 (6) | |
| Age, y | .69 | |||
| 16–19 | 28 (11) | 17 (13) | 11 (9) | |
| 20–24 | 101 (39) | 54 (41) | 47 (37) | |
| 25–29 | 60 (23) | 27 (20) | 33 (26) | |
| ≥ 30 | 71 (27) | 34 (26) | 37 (29) | |
| Ethnicity | .27 | |||
| Hispanic | 143 (55) | 67 (51) | 76 (59) | |
| Non-Hispanic | 117 (45) | 65 (49) | 52 (41) | |
| Education | .08 | |||
| < high school | 63 (24) | 29 (22) | 34 (27) | |
| High school graduate | 82 (32) | 36 (27) | 46 (36) | |
| > high school | 111 (43) | 66 (50) | 45 (35) | |
| Missing | 4 (2) | 1 (1) | 3 (2) | |
| Income, $ | .5 | |||
| < 15 000 | 108 (42) | 52 (39) | 56 (44) | |
| > 15 000–30 000 | 39 (15) | 24 (18) | 15 (12) | |
| > 30 000 | 59 (23) | 27 (20) | 32 (25) | |
| Don’t know/missing | 54 (21) | 29 (22) | 25 (20) | |
| Marital status | .73 | |||
| Single | 189 (73) | 95 (72) | 94 (73) | |
| Married | 70 (27) | 37 (28) | 33 (26) | |
| Missing | 1 (0) | 0 (0) | 1 (1) | |
| Living with spouse/partner | .92 | |||
| Yes | 170 (65) | 44 (33) | 43 (34) | |
| No | 87 (33) | 87 (66) | 83 (65) | |
| Missing | 3 (1) | 1 (1) | 2 (2) | |
| Adults in household (≥ 18 y)a | .57 | |||
| 1 | 52 (15) | 22 (17) | 30 (23) | |
| 2 | 142 (42) | 74 (56) | 68 (53) | |
| ≥ 3 | 142 (42) | 35 (27) | 29 (23) | |
| Missing | 2 (1) | 1 (1) | 1 (1) | |
| Children in household (< 18 y)a | .36 | |||
| 0 | 60 (23) | 35 (27) | 25 (20) | |
| 1 | 99 (38) | 53 (40) | 46 (36) | |
| 2 | 65 (25) | 27 (20) | 38 (30) | |
| ≥ 3 | 33 (13) | 16 (12) | 17 (13) | |
| Missing | 3 (1) | 1 (1) | 2 (2) | |
| Prepregnancy smoking status | .97 | |||
| None | 167 (64) | 85 (64) | 82 (64) | |
| < 10 cigarettes/d | 69 (27) | 34 (26) | 35 (27) | |
| > 10 cigarettes/d | 20 (8) | 11 (8) | 9 (7) | |
| Missing | 4 (2) | 2 (2) | 2 (2) | |
| Pregnancy smoking status | .56 | |||
| None | 211 (81) | 104 (79) | 107 (84) | |
| < 10 cigarettes/d | 34 (13) | 19 (14) | 15 (12) | |
| > 10 cigarettes/d | 3 (1) | 1 (1) | 2 (2) | |
| Missing | 12 (5) | 8 (6) | 4 (3) |
Note. BMI = body mass index; GDM = gestational diabetes mellitus.
Including the participant as appropriate: if < 18 years, included as a child; if ≥ 18 years, included as an adult.
At baseline, there were no differences in physical activity or sedentary behavior between intervention arms. After the 12-week intervention, there was a significant difference in change in total physical activity between the 2 arms. Specifically, the health and wellness arm reported a mean (SD) of 42.7 (105.9) MET hours per week decrease in total activity, whereas the exercise arm reported a smaller decrease in total activity of 2.1 (104.1) MET hours per week (P = .03; Table 2). In addition, approximately 55.2% (n = 48) of the women in the exercise arm reported meeting ACOG recommendations for physical activity after the intervention, compared with 35.3% (n = 30) of women in the health and wellness arm (P = .01). In other words, women in the exercise arm had an odds ratio of 2.12 (95% confidence interval = 1.45, 3.10) of achieving ACOG physical activity recommendations after the intervention compared with the health and wellness arm. Change in reported sedentary behavior was small and not statistically different between the intervention arms (Table 2).
TABLE 2—
Change in Physical Activity and Sedentary Behavior From Before to After Intervention by Intervention Arm: Behaviors Affecting Baby and You (BABY) Study, Massachusetts, 2007–2012
| Exercise |
Health and Wellness |
||||||
| Variable | Before Intervention, Mean (SD) | After Intervention, Mean (SD) | Change,a Mean (SD) | Before Intervention, Mean (SD) | After Intervention, Mean (SD) | Change,a Mean (SD) | Pb |
| Total physical activity,c MET hrs/wk | 212.8 (106.4) | 205.5 (104.1) | −2.1 (109.7) | 215.2 (124.2) | 177.4 (89.1) | −42.7 (105.9) | .03 |
| Physical activity by intensity, MET hrs/wk | |||||||
| Light intensity | 124.5 (55.8) | 129.2 (59.7) | 8.5 (63.6) | 127.2 (63.3) | 118.6 (57.0) | −11.0 (64.0) | .08 |
| Moderate-vigorous intensity | 87.1 (73.9) | 76.2 (61.0) | −10.6 (73.0) | 87.9 (85.2) | 58.7 (50.7) | −30.6 (74.7) | .09 |
| Physical activity by type, MET hrs/wk | |||||||
| Household | 112.9 (77.6) | 106.0 (62.0) | −1.4 (67.3) | 122.5 (77.9) | 104.1 (62.6) | −19.9 (76.5) | .16 |
| Occupational | 55.0 (59.6) | 48.5 (55.8) | −9.9 (70.8) | 55.6 (67.4) | 36.2 (44.1) | −18.9 (56.1) | .22 |
| Sports/exercise | 7.9 (11.2) | 13.1 (11.4) | 5.3 (11.4) | 6.7 (7.8) | 7.0 (9.1) | 0.3 (9.8) | .002 |
| Transportation | 25.7 (21.9) | 28.8 (30.5) | 3.6 (33.1) | 23.4 (25.5) | 23.3 (24.2) | −3.3 (31.2) | .35 |
| Total walking | 37.1 (42.1) | 38.9 (41.9) | 1.6 (51.7) | 35.8 (49.8) | 28.4 (36.7) | −9.4 (49.0) | .18 |
| Total sedentary behavior (hrs/wk) | 2.6 (2.7) | 2.5 (2.2) | 0.03 (2.6) | 2.4 (2.1) | 2.1 (1.6) | −0.3 (2.2) | .45 |
Note. MET = metabolic equivalent of task.
Change from before to after intervention.
P value for difference in change between the exercise and health and wellness intervention arms.
Time spent in each type of activity may not equal total physical activity because of missing data for individual types and intensities of activity.
Next, we examined the impact of the 2 interventions on change in physical activity according to activity intensity. Both the health and wellness arm and exercise arm experienced decreases in MVPA from before to after the intervention; however, there was a suggestion of a smaller decrease in MVPA in the exercise arm (Table 2). Specifically, from before to after the intervention, the mean (SD) MVPA decreased by 30.6 (74.7) MET hours per week in the health and wellness arm, whereas in the exercise arm, the MVPA decreased 10.6 (73.0) MET hours per week (P = .09). There was also the suggestion of a difference between the arms in change in light intensity physical activity from before to after the intervention. In the exercise arm, light intensity physical activity increased by 8.5 (63.6) MET hours per week, whereas in the health and wellness arm, light intensity activity decreased by 11.0 (64.0) MET hours per week (P = .08).
Finally, we examined the impact of the intervention on physical activity by activity type. Although participants in the health and wellness arm did not report a change in sports or exercise from before to after the intervention, women in the exercise arm reported a significant increase of 5.3 (11.4) MET hours per week in sports or exercise (P = .002; Table 2). In all other types, changes in physical activity were not statistically different between the intervention arms. Finally, there was a no difference in change in total walking between intervention arms (P = .18; Table 2).
As a measure of compliance with the study protocol, we assessed the number of returned completed tailoring questionnaires in each intervention arm. After completion of the baseline questionnaire with the health educator, the exercise arm was sent 3 additional tailoring questionnaires over the course of follow-up at 4, 8, and 12 weeks, whereas the comparison health and wellness arm was sent 1 additional tailoring questionnaire at 12 weeks. Compliance with the intervention was similar in both groups (P = .21). In the exercise arm, 41% (n = 54) of the women complied with this protocol, returning at least 3 of the 4 tailoring questionnaires sent. In the health and wellness arm, 49% (n = 63) of the women returned the 2 tailoring questionnaires sent. There were no differences in physical activity, sedentary behavior, or any sociodemographic or medical characteristic at baseline between women who were compliant with this protocol (≥ 3 returned tailoring questionnaires) and women who were noncompliant (< 3 returned tailoring questionnaires).
DISCUSSION
In this randomized trial of an individually tailored, motivationally matched exercise intervention in an ethnically and socioeconomically diverse population of pregnant women at high risk for GDM, we found that the exercise arm had significantly greater increases in sports or exercise activity (equivalent to 1.33 hours/week of sports exercise) compared with the health and wellness arm. Similarly, a greater percentage of women in the exercise arm met recommended guidelines for physical activity during pregnancy compared with the health and wellness arm (55.2% vs 35.3%, respectively). Although both arms experienced a decline in total physical activity, this decline was smaller among women in the exercise arm compared with the health and wellness arm. There was a similar trend of a positive impact of the intervention in activities of moderate to vigorous intensity, light intensity, total walking, and transportation; however, these findings were not statistically significant.
Our findings are consistent with a feasibility study conducted in the first 110 participants in the BABY study (58 in exercise, 52 in health and wellness).32 In that study, Chasan-Taber et al. found that women in the exercise intervention had lower declines in total physical activity compared with the health and wellness arm from before to after the intervention (−1.0 MET hours/day vs −10.0 MET hours/day, respectively; P = .03). The exercise arm also reported increases in physical activity during sports or exercise compared with a slight decrease in the health and wellness arm (0.09 MET hours/day vs −0.01 MET hours/day, respectively; P = .02). After converting our present findings to hours per day for comparison purposes, we found a −0.3 MET hours per day versus −6.1 MET hours per day decrease for total activity and 0.76 MET hours per day versus 0.04 MET hours per day increase for sports or exercise in the exercise arm compared with the health and wellness arm. However, unlike our present study, the analysis did not use an intent-to-treat approach, which could have produced a biased estimate of the intervention effect.33
Other studies that examined the impact of prenatal exercise interventions on physical activity levels during pregnancy have been conflicting. A review of 9 interventions by Pearce et al. indicated that only 3 found a statistically significant impact.34 However, the authors found no unique strategies or techniques consistently associated with positive outcomes. The study limitations of these 9 trials included lack of statistical power, failure to test for baseline differences between the intervention and control groups, lack of a theoretical model, and use of a physical activity questionnaire not validated for pregnant women. Finally, the majority of these studies, with the exception of 1,35 were conducted predominantly in non-Hispanic White populations.34
Study Limitations
The strengths of our study included grounding in a theoretical model of behavioral change,36 the diverse study population, and use of an activity questionnaire validated for pregnancy. However, several study limitations must be noted. We lacked postintervention physical activity data on approximately 33% (n = 86) of the population. Although the protocol was designed to coordinate assessments with routine prenatal care visits, women could not always be located at the time of their visit or had inadequate time. However, there were no statistically significant differences between those with and without physical activity data with respect to baseline sociodemographic or medical history characteristics, with the exception of small differences in light intensity activity that were likely not clinically meaningful. In addition, we further addressed the concern of missing data by using mixed models to determine change in physical activity.
Only 41% of the women in the exercise arm completed 3 or more tailoring questionnaires. Women who failed to return a tailoring questionnaire received booklets based on their previous tailoring questionnaire. To the extent that this did not reflect their current stage of change, the intervention effect might have been attenuated. By contrast, the design of the intervention, which relied on a combination of in-person and telephone sessions, as opposed to requiring attendance at group sessions, might have improved participation and compliance rates.
For a small percentage of women, we relied upon self-reported weight before pregnancy at the time of the first prenatal care visit. However, based on data from Phelan et al., self-reported weight before pregnancy has a high correlation with measured weight (r = 0.95).37
Women who agreed to participate might have been healthier in some overall way than women who did not agree to participate. However, the study population excluded women with comorbidities and contraindications to exercise in pregnancy. In addition, although healthier women might have been more likely to engage in sports and exercise, they might have had little choice whether to undertake occupational or household activity. Finally, caution had to be taken in generalizing findings to different ethnicities and cultures because the broader social and ecological factors that affect physical activity might have varied considerably. However, our observed rates of behaviors during pregnancy, such as smoking (14%), were comparable to pregnancy smoking rates in Springfield, Massachusetts, where the study population was based (12.8%).38 By contrast, our ethnic distribution (55% Hispanic) was higher than the general population in Springfield (39.5% Hispanic).39 Such differences were likely the result of the requirement that the study population be pregnant and at high risk for GDM.
Conclusions
We extended the previous literature by demonstrating the benefits of an exercise intervention in an ethnically and socioeconomically diverse population. Specifically, this individually tailored, motivationally matched exercise intervention led to increases in activity during sports or exercise in pregnant women at high risk for GDM. The intervention is readily translatable to clinical practice. Because of the increased risk of adverse maternal health outcomes in ethnic minority groups, identifying strategies to increase physical activity in these groups might have important implications for reducing health disparities. Future studies should consider partnerships with local communities to increase support and incentives, as well as expand intervention participation to include the pregnant woman’s family members and social network.34
Acknowledgments
The BABY study was supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (grant 1R01DK074876).
Human Participant Protection
This study was approved by the institution review board of the University of Massachusetts-Amherst and Baystate Medical Center.
References
- 1.ACOG Committee on Obstetric Practice. ACOG Committee opinion, number 267, January 2002: exercise during pregnancy and the postpartum period. Obstet Gynecol. 2002;99(1):171–173. doi: 10.1016/s0029-7844(01)01749-5. [DOI] [PubMed] [Google Scholar]
- 2.Claesson IM, Sydsjo G, Brynhildsen J et al. Weight gain restriction for obese pregnant women: a case-control intervention study. BJOG. 2008;115(1):44–50. doi: 10.1111/j.1471-0528.2007.01531.x. [DOI] [PubMed] [Google Scholar]
- 3.Shirazian T, Monteith S, Friedman F, Rebarber A. Lifestyle modification program decreases pregnancy weight gain in obese women. Am J Perinatol. 2010;27(5):411–414. doi: 10.1055/s-0029-1243368. [DOI] [PubMed] [Google Scholar]
- 4.Choi J, Fukuoka Y, Lee JH. The effects of physical activity and physical activity plus diet interventions on body weight in overweight or obese women who are pregnant or in postpartum: a systematic review and meta-analysis of randomized controlled trials. Prev Med. 2013;56(6):351–364. doi: 10.1016/j.ypmed.2013.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tobias DK, Zhang C, van Dam R, Bowers K, Hu F. Physical activity before and during pregnancy and risk of gestational diabetes mellitus: a meta-analysis. Diabetes Care. 2011;34(1):223–229. doi: 10.2337/dc10-1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weissgerber TL, Wolfe LA, Davies GA, Mottola MF. Exercise in the prevention and treatment of maternal-fetal disease: a review of the literature. Appl Physiol Nutr Metab. 2006;31(6):661–674. doi: 10.1139/h06-060. [DOI] [PubMed] [Google Scholar]
- 7.Evenson KR, Wen F. National trends in self-reported physical activity and sedentary behaviors among pregnant women: NHANES 1999–2006. Prev Med. 2010;50(3):123–128. doi: 10.1016/j.ypmed.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 8.Evenson KR, Savitz DA, Huston SL. Leisure-time physical activity among pregnant women in the US. Paediatr Perinat Epidemiol. 2004;18(6):400–407. doi: 10.1111/j.1365-3016.2004.00595.x. [DOI] [PubMed] [Google Scholar]
- 9.Poudevigne MS, O’Connor PJ. A review of physical activity patterns in pregnant women and their relationship to psychological health. Sports Med. 2006;36(1):19–38. doi: 10.2165/00007256-200636010-00003. [DOI] [PubMed] [Google Scholar]
- 10.Zhang J, Savitz DA. Exercise during pregnancy among US women. Ann Epidemiol. 1996;6(1):53–59. doi: 10.1016/1047-2797(95)00093-3. [DOI] [PubMed] [Google Scholar]
- 11.Petersen AM, Leet TL, Brownson RC. Correlates of physical activity among pregnant women in the United States. Med Sci Sports Exerc. 2005;37(10):1748–1753. doi: 10.1249/01.mss.0000181302.97948.90. [DOI] [PubMed] [Google Scholar]
- 12.Yun S, Kabeer NH, Zhu BP, Brownson RC. Modifiable risk factors for developing diabetes among women with previous gestational diabetes. Prev Chronic Dis. 2007;4(1):A07. [PMC free article] [PubMed] [Google Scholar]
- 13.Hui A, Back L, Ludwig S et al. Lifestyle intervention on diet and exercise reduced excessive gestational weight gain in pregnant women under a randomised controlled trial. BJOG. 2012;119(1):70–77. doi: 10.1111/j.1471-0528.2011.03184.x. [DOI] [PubMed] [Google Scholar]
- 14.Aittasalo M, Raitanen J, Kinnunen TI, Ojala K, Kolu P, Luoto R. Is intensive counseling in maternity care feasible and effective in promoting physical activity among women at risk for gestational diabetes? Secondary analysis of a cluster randomized NELLI study in Finland. Int J Behav Nutr Phys Act. 2012;9(1):104. doi: 10.1186/1479-5868-9-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Callaway LK, Colditz PB, Byrne NM et al. Prevention of gestational diabetes: feasibility issues for an exercise intervention in obese pregnant women. Diabetes Care. 2010;33(7):1457–1459. doi: 10.2337/dc09-2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luoto R, Kinnunen TI, Aittasalo M et al. Primary prevention of gestational diabetes mellitus and large-for-gestational-age newborns by lifestyle counseling: a cluster-randomized controlled trial. PLoS Med. 2011;8(5):e1001036. doi: 10.1371/journal.pmed.1001036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guelinckx I, Devlieger R, Mullie P, Vansant G. Effect of lifestyle intervention on dietary habits, physical activity, and gestational weight gain in obese pregnant women: a randomized controlled trial. Am J Clin Nutr. 2010;91(2):373–380. doi: 10.3945/ajcn.2009.28166. [DOI] [PubMed] [Google Scholar]
- 18.Polley BA, Wing RR, Sims CJ. Randomized controlled trial to prevent excessive weight gain in pregnant women. Int J Obes Relat Metab Disord. 2002;26(11):1494–1502. doi: 10.1038/sj.ijo.0802130. [DOI] [PubMed] [Google Scholar]
- 19.Aittasalo M, Pasanen M, Fogelholm M, Kinnunen TI, Ojala K, Luoto R. Physical activity counseling in maternity and child health care – a controlled trial. BMC Womens Health. 2008;8:14. doi: 10.1186/1472-6874-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ong MJ, Guelfi KJ, Hunter T, Wallman KE, Fournier PA, Newnham JP. Supervised home-based exercise may attenuate the decline of glucose tolerance in obese pregnant women. Diabetes Metab. 2009;35(5):418–421. doi: 10.1016/j.diabet.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 21.Downs DS, Chasan-Taber L, Evenson KR, Leiferman J, Yeo S. Physical activity and pregnancy: past and present evidence and future recommendations. Res Q Exerc Sport. 2012;83(4):485–502. doi: 10.1080/02701367.2012.10599138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marcus BH, Napolitano MA, King AC et al. Examination of print and telephone channels for physical activity promotion: rationale, design, and baseline data from Project STRIDE. Contemp Clin Trials. 2007;28(1):90–104. doi: 10.1016/j.cct.2006.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marcus BH, Napolitano MA, King AC et al. Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project STRIDE. Health Psychol. 2007;26(4):401–409. doi: 10.1037/0278-6133.26.4.401. [DOI] [PubMed] [Google Scholar]
- 24.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2004;27(suppl 1):S5–S10. doi: 10.2337/diacare.27.2007.s5. [DOI] [PubMed] [Google Scholar]
- 25.Chasan-Taber L, Marcus BH, Stanek E, 3rd et al. A randomized controlled trial of prenatal physical activity to prevent gestational diabetes: design and methods. J Womens Health (Larchmt) 2009;18(6):851–859. doi: 10.1089/jwh.2008.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prochaska JO, DiClemente CC, Velicer WF, Rossi JS. Standardized, individualized, interactive, and personalized self-help programs for smoking cessation. Health Psychol. 1993;12(5):399–405. doi: 10.1037//0278-6133.12.5.399. [DOI] [PubMed] [Google Scholar]
- 27.Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: Freeman; 1997. [Google Scholar]
- 28.Marquez DX, Bustamante EE, Bock BC, Markenson G, Tovar A, Chasan-Taber L. Perspectives of Latina and non-Latina white women on barriers and facilitators to exercise in pregnancy. Women Health. 2009;49(6–7):505–521. doi: 10.1080/03630240903427114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American College of Obstetricians and Gynecologists. Exercise during pregnancy and the postpartum period. Clin Obstet Gynecol. 2003;46(2):496–499. doi: 10.1097/00003081-200306000-00028. [DOI] [PubMed] [Google Scholar]
- 30.Chasan-Taber L, Schmidt MD, Roberts DE, Hosmer D, Markenson G, Freedson PS. Development and validation of a Pregnancy Physical Activity Questionnaire. Med Sci Sports Exerc. 2004;36(10):1750–1760. doi: 10.1249/01.mss.0000142303.49306.0d. [DOI] [PubMed] [Google Scholar]
- 31.Ainsworth BE, Haskell WL, Whitt MC et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 suppl):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 32.Chasan-Taber L, Silveira M, Marcus BH, Braun B, Stanek E, Markenson G. Feasibility and efficacy of a physical activity intervention among pregnant women: the behaviors affecting baby and you (B.A.B.Y.) study. J Phys Act Health. 2011;8(suppl 2):S228–S238. doi: 10.1123/jpah.8.s2.s228. [DOI] [PubMed] [Google Scholar]
- 33.Gupta SK. Intention-to-treat concept: a review. Perspect Clin Res. 2011;2(3):109–112. doi: 10.4103/2229-3485.83221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pearce EE, Evenson KR, Downs DS, Steckler A. Strategies to promote physical activity during pregnancy: a systematic review of intervention evidence. Am J Lifestyle Med. 2013;7(1) doi: 10.1177/1559827612446416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ferrara A, Hedderson MM, Albright CL et al. A pregnancy and postpartum lifestyle intervention in women with gestational diabetes mellitus reduces diabetes risk factors: a feasibility randomized control trial. Diabetes Care. 2011;34(7):1519–1525. doi: 10.2337/dc10-2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marcus BH, Bock BC, Pinto BM, Forsyth LH, Roberts MB, Traficante RM. Efficacy of an individualized, motivationally-tailored physical activity intervention. Ann Behav Med. 1998;20(3):174–180. doi: 10.1007/BF02884958. [DOI] [PubMed] [Google Scholar]
- 37.Phelan S, Phipps MG, Abrams B, Darroch F, Schaffner A, Wing RR. Randomized trial of a behavioral intervention to prevent excessive gestational weight gain: the Fit for Delivery Study. Am J Clin Nutr. 2011;93(4):772–779. doi: 10.3945/ajcn.110.005306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. MassCHIP Perinatal Report: Smoking: Hampden County. Available at: http://www.mass.gov/eohhs/researcher/community-health/masschip/smoking.html#counties. Accessed January 1, 2014.
- 39. U.S. Census Bureau. Census Summary; Table DP-1 Profile of General Population and Housing Characteristics: Springfield, Massachusetts 2010 Demographic Profile Data; American FactFinder. Available at: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_12_5YR_DP05&prodType=table. Accessed April 9, 2014.