Abstract
We used a structured approach to assess whether active smokers presented with pictorial warnings on cigarette packages (PWCP) had a higher probability of quitting, reducing, and attempting to quit smoking than did unexposed smokers.
We identified 21 articles from among nearly 2500 published between 1993 and 2013, prioritizing coverage over relevance or quality because we expected to find only a few studies with behavioral outcomes. We found very large heterogeneity across studies, poor or very poor methodological quality, and generally null or conflicting findings for any explored outcome.
The evidence for or against the use of PWCP is insufficient, suggesting that any effect of PWCP on behavior would be modest. Determining the single impact of PWCP on behavior requires studies with strong methodological designs and longer follow-up periods.
Smoking and its associated health and mortality risks have been well established. Nearly one fifth of the world’s population smoke, and close to 6 million die each year from tobacco use,1 a figure estimated to reach 10 million by 2020.2 In an attempt to curb this trajectory, governments have and continue to implement various tobacco control policies aimed at reducing smoking.
Common tobacco control policies include increased taxes, bans or restrictions on advertising, sponsorships, point-of-sale displays, smoking in public places,3 and, pertaining to this article, health warning labels on cigarette packages. Currently, most countries require warnings to be printed on cigarette packs, though format varies in terms of size, number, and how information is presented, ranging from vague text statements to graphic images alongside the text.4
Pictorial warnings on cigarette packages (PWCP) were first implemented in 2001.5 Since then, studies have assessed the perceptions and reactions elicited among smokers and nonsmokers and also the motivation or intention to quit or reduce smoking.6,7 However, research investigating whether PWCP bring about a change in smoking behavior has been limited.
HISTORICAL CONTEXT
Health warning labels on cigarette packages have evolved through 3 phases. The first began in 1965 when the United States first implemented a law requiring tobacco companies to print a small text warning on 1 side of the pack.5,8 Throughout the following 2 decades, this phase saw several other countries, such as the United Kingdom, Canada, and Australia, follow suit with similar warning-label arrangements.3,9 In the second phase, new legislative measures or modifications to existing laws were introduced in the 1980s–1990s; the small bland text messages were updated to appear with larger font on the front or back of the package and with greater variation in the types of warning messages.10,11 The third phase began in 2001 when Canada started using PWCP.5 By February 2012, more than 45 countries had implemented legislation that required the addition of a pictorial health warning alongside the text warning on cigarette packages.12
Globalization provided an avenue for widespread international cooperation to fight against the tobacco epidemic. The World Health Organization Framework Convention on Tobacco Control entered into force via the United Nations in 2005.13 With 168 signatory states, the treaty covered a wide array of tobacco control policies, including price and tax measures, exposure, education, advertising, and packaging and labeling of tobacco products.14
An important element in this global collaboration is the International Tobacco Control Policy Evaluation Project, a research program whose aim is to evaluate Framework Convention on Tobacco Control policies by conducting homogeneous, population-level surveys to determine effective tobacco control policies.15 The Framework Convention on Tobacco Control treaty covers the recommendations for packaging and labeling of tobacco products.14 The fact that the inclusion of pictures is optional for participating states means that it is crucial for the research community to guide countries with appropriate recommendations and justifications for incorporating PWCP into their legislative tobacco control policies.
THE CIGARETTE PACKAGE AS A TOOL FOR COMMUNICATION
Both the tobacco industry and tobacco control advocates have agreed that the cigarette package serves as a crucial marketing tool and a means of communicating with the population.5,16,17 As a consequence of the increasing number of countries implementing marketing restrictions, the tobacco industry has reacted by improving their advertisement strategy,17 including the use of new cigarette pack designs that involve innovations in shape, color, size, and plastic wrapping.5
Besides providing a direct link to the consumer, the pack also becomes a portable advertisement device for the tobacco brand because the smoker puts it on display every time a cigarette is used.5 From the tobacco control perspective, the cigarette package can be an equally effective tool for communicating the dangers of tobacco consumption to the public, especially among low-literacy smokers and children because the warnings will be put on display as often as the cigarette pack itself.5
EFFECTS OF PWCP ON BEHAVIOR
Although most smokers are aware of the harmful effects of tobacco, lack of knowledge and underestimation of the specific health risks associated with smoking constitute relevant factors that affect people’s decision to quit or reduce smoking.9,18 It is therefore important to instigate tactics and policy enhancements that drive individuals toward more probable behavior change.
Even though many countries have incorporated PWCP into their legislation,12 some are still hesitant or restrained because of insufficient evidence that PWCP can actually reduce smoking rates. In the United States, for example, the Food and Drug Administration was given the authority to regulate tobacco products in 2009 via the Family Smoking Prevention and Tobacco Control Act,16 which opened up the path to initiate the implementation of PWCP. However, the United States has not yet introduced PWCP because the overarching theme is still set in legal contentions.19 Thus, in countries with complex legal systems, substantial evidence to support PWCP is clearly needed.
So far, evidence has shown that PWCP are a cost-effective health communication, have high awareness and visibility among nonsmokers and youths, and are significantly more effective than text-only messages because they depict health risks vividly.5,6 Research has also shown that regularly updated, large, and prominent PWCP located on the top of packages are credible, have public support, and can increase health knowledge and motivation to quit.5,6 Frequent reminders about behavior change have generally been shown to be effective.20 PWCP might have this effect.
However, evidence in terms of behavior change has not been systematically reviewed. Therefore, we conducted this review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendations to assess the evidence pertaining to the effect of PWCP on smoking behavior.21 We used a structured approach consisting of 5 criteria (type of population, intervention, comparator group, outcome, and study design) to frame our research question, namely, whether active smokers presented with PWCP had a higher probability of quitting, reducing, and attempting to quit smoking than smokers not presented with the PWCP.21 We purposely excluded outcomes not related to behavior change, such as those looking at perceptions, attitudes, reactions, knowledge, or even motivation and intention to quit.
METHODS
Because we expected the number of articles with original data investigating the effect of PWCP on behavior change to be small, we opted to ease the criteria for selecting studies to include all available evidence on the topic rather than identifying only methodologically rigorous studies.
Variables Examined
Participants had to be current, active smokers of manufactured or hand-rolled cigarettes and aged 10 years or older. Although the most common definition of “current smoker” refers to individuals who have smoked at least 100 cigarettes in their lifetime and who are currently smoking every day or some days,22 for the purpose of this review we used a much broader definition of any smoking at the time of the assessment. We examined the effect of any graphic, pictorial, photographic, or symbolic warning image of any size, color, content, and position, with or without text, printed or intended for printing on cigarette or hand-rolling tobacco packages.
Inclusion of a comparison group was a requisite and could have consisted of any of the following: smokers not exposed to PWCP or exposed to a variant of the PWCP intervention that could serve as comparison group, such as when pictorial warnings were used in combination with another exposure (e.g., plain packaging, media campaign, or self-affirmation); smokers exposed to text-only warnings such as in time periods or study settings in which PWCP had not yet been implemented; smokers with lower cognitive responses to PWCP (i.e., level of understanding) or who were unaware of the warnings.
The primary outcome was smoking cessation, following the definition of “not having smoked, not even a puff, in the 7 days before the follow-up measure.”23 The secondary outcomes included reduction, defined as “any self-reported as absolute or percentage decrease of the quantity of cigarettes smoked per day, with or without biochemical confirmation,”24 and attempt to quit, based on an affirmative response to questions about a “serious attempt to stop smoking for good that lasted for at least 24 hours” in the recent past.22 However, to preserve a largely inclusive approach, we mostly used these definitions as a reference standard rather than as strict selection criteria.
We considered experimental (e.g., randomized controlled trials [RCTs]) and quasi-experimental (e.g., time-series or pre–post design) studies and relevant observational studies with any type of follow-up period (e.g., prospective or retrospective cohorts), including repeated surveys in different time periods with different samples.
Information Sources and Search Strategy
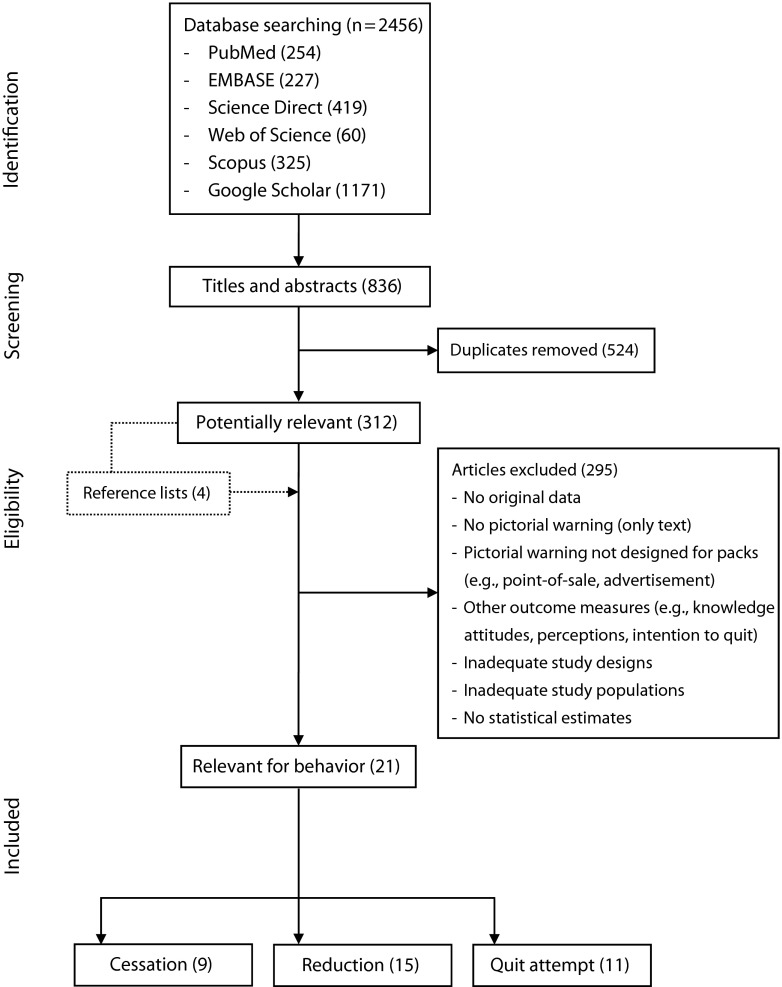
We identified articles published between 1993 and 2013 in PubMed, EMBASE, ScienceDirect, Web of Science, and Scopus using combinations of the keywords and MeSH terms (including plural forms): warning + (at least 1 of) graphic, image, visual, photo, picture, pictorial, design, label, pack + (at least 1 of) smoke, smoking, cigarette, tobacco (Figure 1).
FIGURE 1—
Search strategy to identify articles for the systematic review assessing the effect of PWCP on smoking behavior: 1993–2013.
Note. PWCP = pictorial warnings on cigarette packages.
We completed identification of relevant material using Google Scholar. Because of the limitations of this search engine, we had to screen document titles only. We used the following descriptors (including plural forms): warning + (at least 1 of) smoke, smoker, smoking, tobacco, cigarette, pack, package, graphic, image, visual, photo, picture, pictorial, and design.
We finalized the search by screening the reference lists of all relevant articles selected from the previous searches, including reviews related to the topic, to identify other potential documents. We limited the review to documents written in Chinese, Korean, Danish, Dutch, English, French, German, Italian, Norwegian, Portuguese, Spanish, and Swedish because someone on the team or a close colleague was able to read these languages.
Study Selection and Data Extraction
First, we conducted a screening of titles and abstracts of all the hits obtained through the 7 search engines. Then, we excluded duplicate documents and expanded the list of those that were potentially relevant with articles recovered from reference lists. Finally, we performed a careful reading of hard copies to assess eligibility. Excluded documents were those containing no original data, looking at text warnings only or pictorial warnings not aimed for use on cigarette packs (e.g., point of sale and advertisements), or studying only cognitive effects of PWCP, such as people’s knowledge, perceptions, reactions, attitudes, or intentions. We also excluded studies because of inadequate methodological designs (e.g., cross-sectional studies, no comparison group) and study populations not fulfilling the inclusion criteria (e.g., nonsmokers) or because no statistical estimates were reported. The screening and assessment process was performed independently by 3 of us (B. L., F. G., and J. M.-E.), and disagreements were resolved by discussion.
We retrieved the following data from the selected articles: first author’s last name, country and year of publication, journal of publication, study period, data source, relevant outcomes, study population, study design, sample size, outcome definition, exposure assessment, measurement instruments, statistical analyses and measures, control for potential confounders, and main results of interest. When the analyses were adjusted by confounding factors, we used the adjusted measures instead of the crude results. Two of us (B. L. and F. G.) extracted information separately for each of the outcomes, and differences were resolved after discussion with the first author (J. M.-E.).
Study Quality and Data Synthesis
Most of the selected studies did not primarily aim to assess the impact of PWCP on smoking behavior. In most cases, the results associated with the outcomes were secondary, and in few studies we had to specifically search for those potentially relevant to this review.
Articles were published in various types of journals, including the fields of psychology and marketing, which have a different approach than that of biomedical journals. This resulted in an extreme heterogeneity of designs, samples, definitions, exposure methods, study periods, and statistical analyses, precluding not only the possibility of meta-analyses, but even the use of a standard assessment with homogeneous criteria to determine the quality of the studies.
We therefore decided to use a simplified arbitrary quality assessment based on 4 basic criteria as judged independently by the 2 reviewers (J. M.-E. and B. J.): study design, outcome definition, exposure definition, and statistical analyses. Agreement between raters was very high because the assessment instrument used was straightforward with clear definitions. There were minor disagreements in just a few studies or criteria, which were resolved by consensus between reviewers. Full details about the assessment can be found in Table 1.
TABLE 1—
Quality Assessment of the Studies Included in the Systematic Review of the Effect of Pictorial Warnings on Cigarette Packages on Smoking Behavior for the 3 Outcomes Measured: 1993–2013
| Author, Study Area, and Study Period | Outcome Assessed | Study Designa | Outcome Definitionb | Exposure Definitionc | Statistical Analysesd | Total Score | Overall Qualitye |
| Hammond et al.,25 southwest Ontario, CAN, 2001–2002f | C + R + A | 1 | 2 | 1 | 1 | 5 | Fair |
| Christie and Etter,26 Switzerland, France, Belgium, 2001 | C | 0 | 0 | 1 | 1 | 2 | Very poor |
| R + A | 0 | 2 | 1 | 1 | 4 | Poor | |
| Hammond et al.,27 southwest Ontario, CAN, 2001–2002f | C + R + A | 1 | 1 | 1 | 1 | 4 | Poor |
| Environics Research Group Ltd.,28 CAN, 2000–2004 | A | 0 | 2 | 2 | 1 | 5 | Fair |
| Hammond et al.,29 AUS, UK, CAN, US, 2002–2005g | R | 1 | 1 | 2 | 2 | 6 | Fair |
| Harris et al.,30 University of Sheffield, UK, no period reported | R | 2 | 2 | 0 | 1 | 5 | Fair |
| Silpasuwan et al.,31 5 regions, Thailand, 2005–2006 | C | 0 | 1 | 1 | 1 | 3 | Poor |
| Borland et al.,32 AUS, UK, CAN, US, 2002–2006g | C | 1 | 2 | 1 | 1 | 5 | Fair |
| A | 1 | 2 | 1 | 2 | 6 | Fair | |
| Borland et al.,33 AUS, UK, CAN, US, 2002–2006f | R | 1 | 1 | 2 | 2 | 6 | Fair |
| Shanahan and Elliott,34 AUS, 2000 and 2008 | R | 0 | 1 | 1 | 1 | 3 | Poor |
| A | 0 | 2 | 1 | 1 | 4 | Poor | |
| Fathelrahman et al.,35 Penang State, Malaysia, 2008 | R | 2 | 1 | 0 | 1 | 4 | Poor |
| Heydari et al.,36 Tehran, Iran, 2008–2009 | R | 0 | 1 | 1 | 1 | 3 | Poor |
| Miller et al.,37 South AUS, 2005–2006 | C | 0 | 0 | 0 | 1 | 1 | Very poor |
| Moodie et al.,38 Glasgow, Scotland, UK, 2010 | R | 1 | 1 | 1 | 1 | 4 | Poor |
| Malouff et al.,39 AUS, no period reported | C + A | 2 | 0 | 1 | 1 | 4 | Poor |
| R | 2 | 2 | 1 | 1 | 6 | Fair | |
| Thrasher et al.,40 2012, 7 cities, Mexico, 2010 and 2011h | C | 0 | 0 | 1 | 1 | 2 | Very poor |
| A | 0 | 1 | 1 | 2 | 4 | Poor | |
| Zhao et al.,41 mid-Atlantic university, US, no period reported | R | 2 | 2 | 2 | 1 | 7 | Good |
| Azagba and Sharaf,42 CAN, 1998–2008 | A | 1 | 1 | 2 | 2 | 6 | Fair |
| Malouff et al.,43 cities in the United States, no period reported | C | 0 | 0 | 1 | 1 | 2 | Very poor |
| R | 0 | 2 | 1 | 1 | 4 | Poor | |
| A | 0 | 1 | 1 | 1 | 3 | Poor | |
| Thrasher et al.,44 Mexico, 2010–2012h | R + A | 0 | 1 | 1 | 1 | 3 | Poor |
| Yong et al.,45 Thailand and Malaysia, 2005–2008 | R | 1 | 1 | 2 | 1 | 5 | Fair |
Note. A = attempt; AUS = Australia; C = cessation; CAN = Canada; PWCP = pictorial warnings on cigarette packages; R = reduction.
2 = randomized controlled trial; 1 = cohort study; 0 = other study designs.
2 = clear (explicit action) and complete (explicit time frame); 1 = unclear or incomplete; 0 = unclear and incomplete.
2 = appropriate PWCP; 1 = appropriate pictorial warning intended for printing in cigarette packages or inappropriate PWCP (e.g., very short exposure duration or lack of an unexposed control group); 0 = inappropriate warning (not a PWCP or intended for printing in cigarette packages).
2 = pertinent and adjusted; 1 = not pertinent or unadjusted; 0 = not pertinent and unadjusted.
0–2 = very poor; 3–4 = poor; 5–6 = fair; 7–8 = good.
These articles used similar or identical data for analyses.
These articles used similar or identical data for analyses.
These articles used similar or identical data for analyses.
We summarized the findings as positive when a statistically significant effect (P < .05) was reported, regardless of the strength of the association; null when no significant effect was reported; mixed when either positive or null results were observed; and uncertain when the results available precluded a meaningful conclusion. In the text, the results were presented mostly in a narrative manner, trying to highlight the most relevant findings in context with the study limitations and strengths.
RESULTS
From the 2456 items identified, we considered 312 nonduplicate documents plus another 4 extracted from reference lists as potentially relevant to the PWCP topic. From these, we excluded 295 for various reasons, leaving 21 studies with relevant behavioral outcomes (cessation, 9; reduction, 15; and attempt, 11).25–45
Two thirds (n = 14) of the selected studies had been published within the past 5 years. Canadian and Australian data were the most frequently analyzed with 7 and 6 articles, respectively, including 3 multicountry analyses with UK and US data used as the reference because these countries have not yet implemented PWCP. Nevertheless, each of these countries also contributed 2 other studies, mostly of an experimental nature. Data from developing countries were available for Mexico, Thailand, Malaysia, and Iran. Various articles were based on similar or identical data (i.e., multicountry studies, Mexican studies, and Canadian prospective cohorts).
On the basis of the quality assessment, we considered 57% of the reviewed studies (n = 12) to be of poor or very poor quality, and only 1 could be classified as being of good quality.41 Most studies compared data at different time periods, but 4 did not specify any study period (3 being experimental). Cohorts (prospective, retrospective, survey based, and panel) were the most frequent designs, used in 9 studies, followed by pre–post and RCT designs with 5 and 4 studies, respectively. Study population, sample selection, and data collection methods varied considerably across studies, making it difficult to summarize the results. Most studies focused on adult smokers aged 18 years or older, but 3 included adolescents (aged ≥ 15 years). Twelve articles examined only 1 outcome, 4 looked at 2, and 5 investigated all 3 behavioral outcomes.
Cessation
Of the 9 articles presenting any kind of smoking cessation results, 4 used variations of cohort designs,25,27,32,37 4 were pre–post studies,26,31,40,43 and 1 was an RCT.39 Sample sizes ranged from less than 100 smokers to nearly 1000.
Two studies did not report a cessation definition,26,37 1 used an inappropriate definition (i.e., “quit smoking within 1 month”),31(p.554) 3 used stage of change toward cessation,39,43 2 used a cessation-related variable for which cessation was pooled together with reduction and attempt,25,27 and another used “reasons for having quit in ex-smokers” in the year preceding the survey.40(p.252) Only 1 study defined cessation as smoking abstinence for 1 month or more before the repeated cohort measurement from those who attempted to quit.32 The exposure assessment showed large variability. Some studies used intermediary variables such as the depth of cognitive processing,25,32 avoidance and emotional reactions,27 or salience with regard to the PWCP.32 Nearly all compared periods before and after implementation or use of PWCP in different ways, except for the RCT that directly compared pictorial with text only using computer screen warnings.39 Statistical analyses relied mainly on logistic regression with adjusted odds ratios (ORs) as a measure of association25,27,32,40 or analysis of variance using mean score comparisons,37,39,43 but 2 articles presented only cessation proportions.26,31 Logistic models were adjusted for various sociodemographic (e.g., age, gender, income, and education) and smoking behavior (e.g., daily cigarettes and smoking years) variables.27,32 Other analyses were typically unadjusted.
Results were mixed and difficult to summarize because designs, exposure, outcome definitions, and statistical measures varied much. However, we can highlight the most relevant findings looking specifically at cessation (excluding stage of change toward cessation and cessation pooled with other behavioral outcomes). The prospective Canadian cohort found no effect of PWCP cognitive processing on cessation using unadjusted quartile analyses (fourth quartile score = 1.7, 95% confidence interval [CI] = 0.37, 5.3).25 The Australian RCT showed no significant effect of pictorial warnings compared with text only at follow-up using computer screen messages once per week for 4 weeks (based on our own calculations from raw counts, 14% vs 8%; P = .65).39 The Mexican pre–post study reported an effect of PWCP compared with text only (before PWCP implementation) as a quitting reason in ex-smokers (adjusted OR = 2.44; 95% CI = 1.27, 4.72).40 Overall, the multicountry survey-based cohort study found no significant consistent adjusted effects for salience, avoiding or forgoing cigarettes, and cognitive response.32 Only 2 studies looking at cessation were of fair quality, and in both the results were null (OR = 1.74; 95% CI = 0.37–5.3 for fourth quartile exposure to cognitive processing25; no consistent statistically significant effect for PWCP’s salience, cognitive response, and forgoing or avoiding cigarettes32; Table 2.
TABLE 2—
Studies Included in the Systematic Review Exploring the Effect of the Exposure to Pictorial Warnings on Cigarette Packages on Smoking Cessation Behavior: 1993–2013
| Author, Study Area, and Study Period | Design and Sample | Outcome Definition | Exposure Assessment | Analyses | Measure and Adjustment | Main Results | Qualitya and Finding;b Remarks |
| Hammond et al.,25 southwest Ontario, CAN, 2001–2002c | Prospective cohort; n = 432 followed | ≥ 7 d abstinence (cessation-related behavior including cessation) | Depth of cognitive processing of PWCP, 9 items (5-point Likert scale), quartile exposure (cessation only), and scale (used for cessation-related behavior, which included cessation, reduction, and attempt) | Logistic regression | OR; no adjustment for cessation only (quartile analyses), adjusted for intention and attempts to quit, gender, education, daily and years smoking for pooled outcome | Q1 (Ref) | Fair, null |
| Assessment in 2002 (9 m after full PWCP implementation) | Q2: OR = 1.4 (95% CI = 0.37, 5.26) | Significant for cessation-related behavior (including cessation) adjusted analyses. | |||||
| Q3: OR = 3.0 (95% CI = 0.54, 7.65) | |||||||
| Q4: OR = 1.7 (95% CI = 0.37, 5.3) | |||||||
| Cessation-related behavior (pooled outcome); depth of cognitive processing was adjusted; OR = 1.07 (95% CI = 1.03, 1.12) | |||||||
| Christie and Etter,26 Switzerland, France, Belgium, 2001 | Pre–post; n = 393 | No cessation definition | 3 wk after baseline online survey, cig boxes with various messages were sent to smokers who used them for ∼21 d; 1 mo after getting the boxes, they filled in another questionnaire | None for cessation | Cessation proportion at follow-up; no adjustment | Cessation rate 7% after the follow-up, similar across box messages | Very poor, uncertain |
| No differences across box messages | |||||||
| Hammond et al.,27 southwest Ontario, CAN, 2001–2002c | Prospective cohort; n = 432 followed | Pooled variable: cessation-related behavior (including cessation ≥ 7 d abstinence) | Avoidance (no effort to avoid vs covering, hiding, avoiding PWCP) and emotional reaction (5-point Likert scale) for extent of fear or disgust at baseline; assessment 9 mo after full PWCP implementation | Logistic regression | OR; adjusted for daily cigarettes, smoking years, intention to quit, prior quit attempts, gender, age, education | Avoidance: AOR = 0.86 (95% CI = 0.56, 1.32) | Poor, mixed |
| Emotional reactions: AOR = 1.37 (95%CI = 1.15, 1.64) | Pooled outcome (cessation + reduction + attempt) | ||||||
| Silpasuwan et al.,31 5 regions, Thailand, 2005–2006 | Pre–post; n = 455 (including ex-smokers) | Unclear cessation definition (“quit smoking within 1 month”) | Questionnaire to assess stages of change in smoking cessation (never think to quit in 6 mo, think to quit in 6 mo, quit smoking within 1 mo, smoking relapsing) for the old text vs new PWCP warnings with 8–12 mo in between | None | Cessation proportion before and after follow-up; no adjustment | Quit within 1 mo: 23.5% (pre) vs 21.8% (post) | Poor, null |
| Of those who quit, 2.3% did because of the text warning and 2.8% because of the PWCP. | Smokers and ex-smokers mixed | ||||||
| Borland et al.,32 AUS, UK, CAN, US, 2002–2006 | Survey-based cohort; waves 1–2, 1083/2371 (quit/attempt); waves 2–3, 1176/2138; waves 3–4, 1097/1823; waves 4–5, 918/1273 | ≥ 1 mo abstinence since prior wave from those who attempted to quit; 5 waves | In relation to PWCP: salience, 2 items (noticed, read/looked last mo); cognitive response, 3 items (made think of health risk, more likely to quit, think about quitting in next 6 mo); forgoing cigarettes (ever–never); avoiding (yes–no), 4 items (covering, keep out of sight, using case, avoiding labels) | Logistic regression | OR; adjusted for age, gender, income, education, daily cigarettes, country | Point estimates: salience—waves 1–2, 0.94; waves 2–3, 0.94; waves 3–4, 1.01; waves 4–5, 1.0; cognitive—waves 2–3, 1.02; waves 3–4, 1.17;* waves 4–5, 1.02; forgoing—waves 1–2, 0.99; waves 2–3, 1.04; waves 3–4, 1.02; waves 4–5, 0.66;* avoidance—waves 1–2, 1.02; waves 2–3, 0.98; waves 3–4, 0.77;* waves 4–5, 1.18 | Fair, null |
| Only CAN and AUS had PWCP | |||||||
| Miller et al.,37 South AUS, 2005–2006 | Cohortlike; n = 152 | No cessation definition | Reasoned action approach: If text-only warnings beliefs and attitudes correlate with quit intention at baseline (2005), and intention predicts cessation at follow-up (August 2006), then higher perception of PWCP (since March 2006) at follow-up should result in more cessation. | Linear regression ANOVA paired samples | No measure; no adjustments | Attitudes and beliefs sig. relate to quit intention; intention to quit score at baseline relates to cessation at follow-up: 2.73 (80.5% still smoking) vs 3.53 (19.5% quitters; P = .01); small change in beliefs at follow-up, mostly nonsig. | Very poor, uncertain |
| Associations assessed very indirectly; marketing journal | |||||||
| Malouff et al.,39 AUS, no period reported | RCT; n = 48 followed | Stage change toward cessation: 1 = no intention, 2 = intend 6 mo, 3 = plan 30 d, 4 = action to quit (stop or decrease) | 27 exposed to text warnings only vs 29 exposed to text + PW; on computer screen once/wk for 4 wk | Two-way ANOVA | Mean stage-of-change score difference; adjusted for preexposure | Stage change (including cessation in action-to-quit stage): postexposure 2.59 (text) vs 3.04 (PW), P = .04; follow-up 2.67 (text) vs 2.92 (PW), P > .05 | Poor, null |
| Stage toward cessation assessed at baseline, end of trial (postexposure), 1 mo after (follow-up) | Cessation: intervention, 3 of 21; control, 2 of 25 (P = .65)d | Warnings on computer screen | |||||
| Thrasher et al.,40 2012, 7 cities, Mexico, 2010 and 2011 | Pre–post; quit last y: n = 106 (2010), n = 233 (2011) | Reasons for having quit among ex-smokers (“had quit in the year prior to the survey”) | Comparison between 2010 (before PWCP) and 2011 (after); the 6 PWCP (influenced decision to quit a lot) were actually shown to participants (ITC project) | GEE, logistic regression | OR; age, income, gender, education, quit intention in next 6 mo, attempt to quit in past year | AOR = 2.44 (95% CI = 1.27, 4.72) for effect of PWCP vs text as quitting reason in ex-smokers between 2010 (13% text) and 2011 (26% PWCP) | Very poor, positive |
| Measured warnings as reported reason for quitting | |||||||
| Malouff et al.,43 cities in the US, no period reported | Pre–post; n = 77 | Stage of change toward cessation | One different pictorial warning with text per week was e-mailed for 4 wk; a final questionnaire was sent 1 wk after the last warning | Pre–post ANOVA | Mean stage or score of change toward cessation; no adjustments | Stages or score of change toward cessation: higher scores at follow-up (P < .001) | Very poor, uncertain |
| Warning in computer screen |
Note. ANOVA = analysis of variance; AOR = adjusted odds ratio; CI = confidence interval; cig = cigarette(s); GEE = generalized estimating equations; ITC = International Tobacco Control; PW = pictorial warning; PWCP = pictorial warnings on cigarette packages; OR = odds ratio; Q = quartile; RCT = randomized clinical trial; sig = statistically significant.
Based on the total sum of points for study design (2 = RCT; 1 = cohort; 0 = other designs), outcome definition (2 = clear and complete; 1 = unclear or incomplete; 0 = unclear and incomplete), exposure definition (2 = appropriate PWCP; 1 = appropriate warning intended for printing or inappropriate PWCP; 0 = inappropriate warning), and statistical analyses (2 = pertinent or adjusted, 1 = not pertinent or unadjusted, 0 = not pertinent and unadjusted); studies were classified as of very poor (0–2), poor (3–4), fair (5–6), and good (7–8) quality.
According to the most relevant finding. Positive: statistically significant effect (P < .05) regardless of the association strength; null = no significantly positive effect; mixed = either positive or null results observed; and uncertain = results available precluded a meaningful conclusion.
Articles used similar or identical data for analyses.
Statistical test done by the reviewers.
*Significant on the basis of 95% CI or P < 0.05.
Reduction
Studies on reduction included 6 different types of cohorts, 4 RCTs, and 3 pre–post studies. Experimental designs included 50 to 150 smokers, whereas the cohort studies surveyed as many as 2000. Nearly all studies used different definitions for reduction. Examples of relatively clear descriptions included decreased daily cigarette consumption of at least 1 per day,25 mean daily cigarettes in the past week,39 and number of cigarettes smoked within the follow-up week.30 Other definitions related to the practice of forgoing cigarettes, such as whether the warnings stopped the smoker from having a cigarette when wanting to smoke 1 in the past month with categorical answers45 or in the past 6 months with dichotomous responses.29 Others were less specific and asked for the number of cigarettes smoked, coded as more, same, or less,36 or smoking less around others, coded dichotomously,38 but even if studies used somewhat similar definitions, the time period or coding categories differed, precluding direct comparisons. For the statistical analyses, cohort studies used adjusted logistic regression models or generalized estimating equations.25,27,29,33,44,45 Experimental and pre–post studies tended to rely on analysis of variance,39,41 the McNemar test,35,38 and the paired t test.26 Two studies presented only proportions with34 or without43 a χ2 test involved. In general, logistic models were adjusted for sociodemographic variables including gender, age, income, and education and for smoking-related factors.
Exposure assessment varied a lot and included the study of concomitant interventions expected to strengthen the warning’s effect. For instance, 2 RCTs examined the impact of affirmation on the effect of warnings on daily and weekly cigarette consumption,30,41 1 retrospective-like cohort study compared the effect of PWCP with and without an antismoking media campaign,44 and a quasi-experimental study compared PWCP printed on plain or branded packs.38
As with smoking cessation, findings for reduction were mixed. Cognitive processing score in the fourth quartile only was associated with reduction (crude OR = 2.68; 95% CI = 1.21, 5.9).25 Similar reductions in the mean number of cigarettes smoked were observed between text and pictorial warning messages shown on a computer in a RCT after 4 weeks.39 The multicountry cohort showed a significant proportion forgoing after PWCP implementation in Australia. It also showed a similar increase in those forgoing after changing from text to PWCP in Australia compared with small to large text in the United Kingdom and a lower wear-out effect of PWCP in Canada compared with text only in the United Kingdom.29,33 Although neither of the 2 RCTs comparing the combined effect of affirmation and pictorial warnings led to positive findings,30,41 the experiment assessing the exposure to pictorial warnings printed on plain packages showed significant reductions for both forgoing and smoking less around others compared with warnings printed on branded packs.38 The combined effect of PWCP and media campaigns showed a significant impact, but one similar to PWCP and media alone.44 Concerning smoking reduction, 4 studies of fair quality showed positive findings,25,29,33,45 and 3 (2 of fair quality and 1 of good quality) revealed null findings (Table 3).30,39,41
TABLE 3—
Studies Included in the Systematic Review Exploring the Effect of the Exposure to Pictorial Warnings on Cigarette Packages on Smoking Reduction Behavior: 1993–2013
| Author, Study Area, and Study Period | Design and Sample | Outcome Definition | Exposure Assessment | Analyses | Measure and Adjustment | Main Results | Qualitya and Finding;b Remarks |
| Hammond et al.,25 southwest Ontario, CAN, 2001–2002c | Prospective cohort; n = 432 followed | Decreased daily cig consumption of ≥ 1/d | Depth of cognitive processing of PWCP, 9 items (5-point Likert), quartile exposure (reduction only) | Logistic regression | OR; no adjustment for reduction only (Q analyses) | Q1 (ref); Q2, OR = 1.52 (95% CI = 0.67, 3.45); Q3, OR = 1.80 (95% CI = 0.82, 3.98); Q4, OR = 2.68 (95% CI = 1.21, 5.93); 24.3% reduction at follow-up | Fair, positive |
| Reduction in Q4 only (increasing trend Q2–Q4) | |||||||
| Christie and Etter,26 Switzerland, France, Belgium, 2001 | Pre–post; n = 365 | No. cig smoked per d (unspecified period) | 3 wk after BL, online survey; 4 cig boxes (addiction, passive smoking, health risks, smell) were sent to smokers who used them for 21 d | Paired t test | Mean difference; no adjustments | Still smoking at follow-up (all boxes): mean cig/d 19.4 before vs 18.1 after, P < .01 | Poor, positive |
| 1 mo after getting the boxes, smokers filled out a questionnaire | Pre–post mean diff. in cig/d across boxes: addiction, 0; passive smoking, −2.3*; bad breath, −1.6*; health risk, −3* | 3 of 4 boxes showed reductions, short-term effect | |||||
| Hammond et al.,27 southwest Ontario, CAN, 2001–2002c | Prospective cohort; 432 followed | Cessation-related behavior (including daily reduction in cigs) | Avoidance (no vs covering, hiding, avoiding PWCP) and emotional reaction (5-point Likert scale) for extent of fear and disgust at baseline; assessment 9 mo after full PWCP implementation | Logistic regression | OR; adjusted for daily cigarettes, smoking years, intention to quit, prior quit attempts, gender, age, education | Avoidance: AOR = 0.86 (95% CI = 0.56, 1.32) | Poor, mixed |
| Emotional reactions: AOR = 1.37 (95% CI = 1.15, 1.64) | Pooled outcome | ||||||
| Hammond et al.,29 AUS, UK, CAN, US, 2002–2005 | Survey-based cohort; > 2000 per country and wave | Warning stopped smoker from having a cig when about to smoke 1 in past 6 mo (ever vs never) | CAN PWCP in January 2001–PWCP in Canada (2001, ITC standard) and AUS (2006, slightly below ITC), US–UK text only (well below ITC) | GEE | Proportion, OR; adjusted for gender, age, income, education, minority status, heaviness of smoking index, attempt to quit in past year; accounted for design effect and nonresponse. | Very similar results (patterns in figures) as in Borland et al.33 | Fair, positive |
| Waves: wave 1, 2002; wave 2, 2003; wave 3, 2004; wave 4, 2005; warnings noted 2002–2005 often or very often in last mo (%): CAN, 60%; AUS, 52%; UK, 44%; US 30% | Same as Borland et al.33 but with 1 fewer wave | ||||||
| Harris et al.,30 University of Sheffield, UK, no period reported | Experiment (RCT); BL, n = 44 SA, n = 43 C; follow-up, n = 21 SA, n = 14 C | No. cig smoked in last d of follow-up wk and in a typical d of follow-up wk (combined variable); total cigs smoked in follow-up wk | Randomized for the SA vs C groups; 4 pictorial warnings with text shown to groups | Linear regression | No. cigs/d or wk at follow-up predicted by SA; adjusted by model 1 BLrisk and model 2 interaction (BLrisk × SA) | Cig/d, SA: 0.03, model 1; −0.01, model 2 | Fair, null |
| No. cigs/d right after PWs were shown considered BLrisk | Cig/wk, SA: 0.10 (model 1); −0.15 (model 2); all coefficients nonsignificant (P > .05) | The effect of affirmation was tested rather than PWCP. | |||||
| Borland et al.,33 AUS, UK, CAN, US, 2002–2006c | Survey-based cohort; > 2000 per country and wave | Forgoing cig (ever vs never) because of the warnings (2 countries only had text) at each wave | PWCP in CAN (2001) and AUS (2006), US and UK text only; wave 1, 2002; wave 2, 2003; wave 3, 2004; wave 4, 2005; wave 5, 2006 | GEE | Proportions; weighted by age and gender, accounted for design effect and nonresponse | Before and after PWCP (waves 4–5): 10%–17% (P < .001); also sig. between wave 5 and among waves 1, 2, and 3 | Fair, positive |
| Before and after PWCP in AUS | Warning change: AUS (waves 4–5) vs UK (waves 2–3): increase of 7% in both countries (P = .98) | Sig. forgoing increase after PWCP in AUS, similar increase for recent warning change between AUS (text to PWCP) and UK (small to large text); lower PWCP wear-out effect (CAN) compared with text (UK) | |||||
| Warning change: AUS (change from text to PWCP) vs UK (change to larger text) | Wear-out: more sustained response to PWCP in CAN compared with larger text in UK,controlling for difference in implementation time | ||||||
| Wear-out effect: UK (3.5 y after larger text) vs CAN (2.5 y after PWCP) | |||||||
| Shanahan and Elliott,34 AUS, 2000 and 2008 | Repeated surveys; n = 822 in 2000, n = 670 in 2008 | Reduction in amount of tobacco smoked per d past 12 mo | Implementation of PWCP in 2006 | χ2 test | Proportions; no adjustments | Reduction 27% in 2000 vs 33% in 2008 (reported sig., no P presented) | Poor, uncertain |
| Cross-sectional surveys compared | |||||||
| Fathelrahman et al.,35 Penang State, Malaysia, 2008 | RCT; n = 140 | To what extent warning labels cause you to stop from having a cig? (0 = never, 1 = once, few times, many times) | BL assessment; after 1 wk random allocation to 5-min inspection of PWCP vs text only; final assessment of smoking reduction right after | McNemar’s test | Proportions; no adjustments | Text, 31.4 before vs 31.4% after; PWCP, 24.6 before vs 58% after (P < .001) | Poor, uncertain |
| No P for difference between groups reported. | Potential future reduction rather than reduction was assessed | ||||||
| Heydari et al.,36 Tehran, Iran, 2008–2009 | Pre–post; n = 1590 | No. of cig and consumption coded as “more, same, less” | Participants surveyed in 2008 (before PWCP), follow-up 9 mo after PWCP implementation | Wilcoxon (smoking rate); χ2 test | Proportions, mean difference; stratified by gender, age, and time of first cigarette in the morning | “No sig. decrease in rate of smoking” (mean difference = 0.179; P = .86); 7.6% smoked less, 12% smoked more after PWCP compared with 2008 | Poor, null |
| Negative results reported | |||||||
| Moodie et al.,38 Glasgow, Scotland, UK, 2010 | Quasi- experimental; n = 48 | Forgoing cig; smoking less around others (yes–no responses) | Half of the participants used plain packs (with PWCP) for 2 wk and then branded packs (with PWCP) for other 2 wk; the other half vice versa | McNemar’s test | Proportions; no adjustments | Measure, plain vs branded: forgoing—I, 15% vs 4%; II, 20% vs 0.6%; III, 19% vs 6%;* IV, 30% vs 9%.* Smoke less around others—I, 33% vs 11%;* II, 37% vs 10%; III, 46% vs 13%;* IV, 44% vs 7%* | Poor, positive |
| Four measurements (2 per wk): I, II, III, IV | The effect of plain package was tested rather than PWCP | ||||||
| Malouff et al.,39 AUS, no period reported | RCT; 48 followed | Cigs smoked yesterday (mean daily cig in past wk) | 27 exposed to text only vs 29 exposed to text and PW; on computer screen once per week for 4 wk; stage toward cessation at baseline, end of trial (post exposure), 1 mo after (follow-up) | Two-way ANOVA | No. cigarettes smoked yesterday; adjusted for preexposure | Cigs smoked yesterday: post exposure, 5.86 (text) vs 6.60 (PW) P > .05; follow-up, 5.29 (text) vs 5.22 (PW), P > .05 (similar results for mean daily cigs in past wk) | Fair, null |
| Narrow definition for reduction | |||||||
| Zhao et al.,41 mid-Atlantic university, US, no period reported | RCT; n = 91 | Daily cigs smoked in 7 d after intervention using diary (data changed into smoking behavior index by tallying the total no. of cig during the 7 d) | 3 groups: 1, no PWCP, no affirmation; 2, PWCP only; 3, affirmation (protecting an image of integrity, morality, adequacy), followed by PWCP | ANOVA | Mean difference; stratified by daily vs occasional smokers | Similar mean smoking index across the 3 groups (P = .56) | Good, null |
| BL data on daily vs occasional smoking | Mean smoking index between daily vs occasional smokers similar in 3 groups (P = .96) | No difference between daily vs occasional smokers | |||||
| Malouff et al.,43 cities in the US, no period reported | Pre–post; n = 78 | No. cig smoked in previous 24 h and wk | Different PW warning and text/wk e-mailed for 4 wk; assessment 1 wk after last warning; perceived distress and usefulness of warning as mediator factors | Pre–post ANOVA, correlation | Mean difference, r between warning distress and usefulness score and cigs (prior 24 h or wk); no adjustments | Mean pre vs post: cig/d, 11.5 vs 8.9, P < .05; cig/wk, 77.4 vs 58.2, P < .05 | Poor, positive |
| cig/wk: distress r = −.25 (P < .05); usefulness r = −.34, (P > .05); cig/d: nonsig | Warning in computer screen | ||||||
| Thrasher et al.,44 Mexico, 2010–2012 | Retrospective-like cohort; 1765 | Health warnings (text and pictorial) “make smokers stop when about to smoke” (refraining yes–no) during the previous mo | Exposure (recall of having seen): PWCP (September 25, 2010), media campaign (only October 2010), PWCP and media (none); warnings were actually shown to assess recall | Logistic regression | OR; adjusted for age, gender, income, civil status, education, smoking intensity, quit intention, exposure to PWCP and media | AOR (95% CI; refrained %): None as Ref (11%), PWCP, 2.55 (1.43, 4.57; 23%); media, 2.13 (1.23, 3.69; 22%); PWCP + media, 2.51 (1.46, 4.31; 24%) | Poor, positive |
| Data collected from October 17, 2010–November 30, 2012 | Similar to media, and PWCP and media; variable duration of exposure, based on cross-sectional data | ||||||
| Yong et al.,45 Thailand and Malaysia, 2005–2008 | Survey-based cohort; n = ∼2000 per wave and country | Warnings stopped smoker from having a cig when wanting to smoke 1 in past m (forgoing never, once, few times, many times) | Wave 1: 2005, before PWCP in T and M | Logistic regression, GEE | OR; adjusted for age, gender, education, cohort, urban vs rural, income, ethnicity, daily vs nondaily smoking, number cigs/d, cigarette type | Change in forgoing cig over time between T and M (Ref): waves 2–1, 2.59 (P < .001); waves 3–2, 1.49 (P < .05); waves 3–1, 3.86 (P < .001) | Fair, positive |
| Wave 2: July–September 2006, 14–18 m after PWCP in T; August 2006–March 2007 in M (only text; control country) | 62%–73% noticed PWCP in T vs 57%–54% text in M; low retention, replenishment needed | ||||||
| Wave 3: 2008 in T and M |
Note. ANOVA = analysis of variance; AOR = adjusted odds ratio; AUS = Australia; BL = baseline; BLrisk = baseline risk; C = control; CAN = Canada; CI = confidence interval; cig = cigarette(s); GEE = generalized estimating equations; ITC = International Tobacco Control; M = Malaysia; PW = pictorial warning; PWCP = pictorial warnings on cigarette packages; OR = odds ratio; Q = quartile; RCT = randomized clinical trial; SA = self-affirmation; sig = statistically significant; T = Thailand.
Based on the total sum of points for study design (2 = RCT; 1 = cohort; 0 = other designs), outcome definition (2 = clear and complete; 1 = unclear or incomplete; 0 = unclear and incomplete), exposure definition (2 = appropriate PWCP; 1 = appropriate warning intended for printing or inappropriate PWCP; 0 = inappropriate warning), and statistical analyses (2 = pertinent or adjusted; 1 = not pertinent or unadjusted; 0 = not pertinent and unadjusted); studies were classified as of very poor (0–2), poor (3–4), fair (5–6), and good (7–8) quality.
According to the most relevant finding. Positive: statistically significant effect (P < .05) regardless of the association strength; null = no significantly positive effect; mixed = either positive or null results observed; and uncertain = results available precluded a meaningful conclusion.
Articles used similar or identical data for analyses.
*Significant on the basis of 95% CI or P < 0.05.
Attempt
Of the 11 articles looking at attempt, 9 also investigated reduction, cessation, or both. The articles included 5 cohort studies, 3 pre–post studies, 2 repeated surveys, and 1 RCT. Sample sizes ranged from 48 smokers in the RCT39 to more than 2000 in a multicountry cohort.32 Various definitions were used, such as any attempt to quit that lasted 24 hours or more within the past month26 or past 3 months25,27 or within the period before the cohort wave under study32,40; an attempt to quit in the past 642 or 12 months28,40,44; or a quitting period of at least 1 month during the past year.34
Adjusted regression modeling was the more frequent method of statistical analysis, though 2 studies used a simple χ2 test to compare proportions,26,34 and 1 displayed only the proportion of smokers who attempted to quit at different survey periods without statistical comparisons.28
The Canadian cohort panel was the most relevant study, focusing only on quit attempt and showing that significantly higher proportions attempted to quit compared with those not exposed among all smokers and among daily smokers using various time-dependent definitions.42
Attempt to quit results were mixed. Although cognitive processing of PWCP had no effect on the basis of quartile exposure25 or when compared with text-only warnings,40 significant associations of cognitive response to PWCP were reported in a cohort.32 Recall of having seen PWCP significantly increased the likelihood of a quit attempt, but not when it occurred in addition to a media campaign.44 Exposure to various types of PWCP for 3 weeks resulted in no increase in quit attempt proportions after 1 month, regardless of the warning message involved.26 The 4 studies with fair quality looking at attempt to quit showed positive, mixed, null, or uncertain results, respectively (Table 4).
TABLE 4—
Studies Included in the Systematic Review Exploring the Effect of the Exposure to Pictorial Warnings on Cigarette Packages on Attempt to Quit Smoking: 1993–2013
| Author, Study Area, and Study Period | Design and Sample | Outcome Definition | Exposure Assessment | Analyses | Measure and Adjustment | Main Results | Quality,a Finding,b and Remarks |
| Hammond et al.,25 southwest Ontario, CAN, 2001–2002c | Prospective cohort; n = 432 | Any attempt to quit smoking that lasted ≥ 24 h in 3 mo follow-up | Depth of cognitive processing of PWCP, 9 items (5-point Likert scale), Q exposure (reduction only) | Logistic regression | OR; no adjustment for attempt only (Q analyses) | 23.1% attempted at follow-up | Fair, null |
| Q1, Ref; Q2, OR = 1.21 (95% CI = 0.44, 3.36); Q3, 1.28 (0.46, 3.50); Q4, 1.37 (0.50, 3.70) | Increasing trend from Q2–Q4 of PWCP cognitive processing on attempt in nonadjusted quartile analyses | ||||||
| Christie and Etter,26 Switzerland, France, Belgium, 2001 | Pre–post; n = 365 | ≥ 1 quit attempt lasting ≥ 24 h in prior 4 wk (yes–no) | 3 wk after online survey 4 cig boxes (addiction, passive smoking, health risks, smell) were sent to smokers who used them ∼21 d; evaluation 1 mo after getting the boxes | χ2 test | Proportions; no adjustments | Pre–post change, quit attempt proportion, 27% vs 22%, P > .05; pre–post difference across boxes: passive smoking, −1%; health risk, −7%; bad breath, +2%; addiction, −15%* | Poor, null |
| Addiction even decreased attempt proportion sig. after exposure | |||||||
| Hammond et al.,27 southwest Ontario, CAN, 2001–2002c | Prospective cohort; n = 432 followed | Cessation-related behavior (including attempt lasting ≥ 24 h in past 3 mo) | Avoidance (no vs covering, hiding, avoiding PWCP) and emotional reaction (Likert scale) for extent of fear and disgust at BL; assessment 9 mo after full PWCP implementation | Logistic regression | OR; adjusted for daily cigarettes, smoking years, intention to quit, prior quit attempts, gender, age, education | Avoidance: AOR = 0.86 (95% CI = 0.56, 1.32) | Poor, mixed |
| Emotional reactions: AOR = 1.37 (95% CI = 1.15, 1.64) | Pooled outcome | ||||||
| Environics Research Group Ltd.,28 CAN, 2000–2004 | Repeated survey; n = 1002 smokers | Times stopped smoking ≥ 24h in past y | Implementation of PWCP in January 2001; all brands in June 2001 | None | Proportion; no adjustments | 2000 (before PWCP), 60%; 2001 (1 y after), 60%; 2002, 67%; 2003, 67%; 2004, 65% | Fair, uncertain—report |
| Borland et al.,32 AUS, UK, CAN, US, 2002–2006 | Survey-based cohort; wk 1–2 2371/6525 (attempt/total), wk 2–3 2138/5257, wk 3–4 1823/4439, wk 4–5 1273/3993 | Attempt to quit for ≥ 24 h since prior wave since previous wave out of the total | In relation to PWCP: salience, 2 items (noticed, read, or looked past month); cognitive response, 3 items (made think of health risk, more likely to quit, think about quitting in next 6 mo); forgoing cigs (ever–never); avoiding (yes–no); 4 items (covering, keep of sight, using case, avoid labels) | Logistic regression | OR; adjusted for age, gender, income, country, education, daily cig, baseline quit intention | Point estimates in 4 waves: | Fair, mixed |
| salience—waves 1–2, 1.02; waves 2–3, 0.96; waves 3–4, 0.97; waves 4–5, 0.97; cognitive—waves 2–3, 1.28;* waves 3–4, 1.14;* waves 4–5, 1.16; forgoing—waves 1–2, 1.38;* waves 2–3, 1.23;* waves 3–4, 1.42;* waves 4–5, 1.30;* avoidance—waves 1–2, 1.17*; waves 2–3, 1.09; waves 3–4, 1.03;* waves 4–5, 1.03 | Only CAN and AUS had PWCP | ||||||
| Shanahan and Elliott,34 AUS, 2000 and 2008 | Repeated survey; n = 822 in 2000, n = 670 in 2008; smokers | Tried to give up and have been successful for ≥ 1 mo or < 1 mo in past y | Implementation of PWCP in 2006 | χ2 test | Proportions; no adjustments | For ≥ 1 mo: 18% in 2000 vs 24% in 2008 (sig) | Poor, positive |
| For < 1 mo: 21% in 2000 vs 26% in 2008 (sig) | Cross-sectional surveys compared | ||||||
| Malouff et al.,39 AUS, no period reported | RCT; n = 48 followed | Stage change toward cessation (includes “action to quit such as stopping or decreasing use”) | 27 exposed to text-only vs 29 exposed to text + PW; on computer screen once per week for 4 wk; stage toward cessation at baseline, end of trial (post exposure), 1 mo after (follow-up) | Two-way ANOVA | Mean stage-of-change score difference; adjusted for preexposure | Stage change (including action-to- quit stage): postexposure, 2.59 (text) vs 3.04 (PW), P = .04; follow-up, 2.67 (text) vs 2.92 (PW), P > .05 | Poor, mixed |
| Unclear whether attempt was included in “action to quit” | |||||||
| Azagba and Sharaf,42 CAN,1998–2008 | Cohort panel; n = 1459 (6269 person-years) | Smokers tried to quit in past 6 mo (yes–no) | 3 exposure definitions: positive to PWCP (started January 2001) if (1) ≥ July 2001, (2) ≥ December 2001, (3) January–December 2001 | GEE (population-averaged marginal effects of PCWC) | Proportion, OR; adjusted for gender, age, education, income, marital and immigration status, job, residence, smoking bans, price, nicotine dependence | Attempt: 1998, 30.1%; 2000, 34.6%; 2002, 40.2%; 2004, 33.1%; 2006, 34.6%; 2008, 29.6% | Fair, positive |
| Scale 0–1 (January–June = 0, July = 0.1, August = 0.3, September = 0.5, October = 0.7, November = 0.9, December = 1.0) | All, ≥ July 2001, OR = 1.32 (95% CI 1.18, 1.49); January–December 2001, OR = 1.33 (95% CI 1.18, 1.49) | Population average effect rather than individual | |||||
| Daily smokers: ≥ December 2001, OR = 1.33 (95% CI 1.17, 1.50); January–December 2001, OR = 1.33 (95% CI 1.17, 1.50) | |||||||
| Thrasher et al.,44 Mexico, 2010–2012 | Retrospective-like cohort; n = 1765 | Attempt to quit in previous year, but after PWCP was implemented | Exposure (recall of having seen): PWCP (introduced September 25, 2010), media (only October 2010), PWCP + media (none); warnings were shown to assess recall (data collected from October 17, 2010–November 30, 2012) | Logistic regression | Proportion, OR; adjusted for age, income, civil status, education, gender, quit intention, smoking intensity, PWCP or media exposure | OR (95% CI; % attempt during study period): no recall of exposure, Ref (6%); PWCP, 4.23 (2.05, 8.69; 17%); media, 1.85 (0.81, 4.21; 9%), PWCP and media, 1.63 (0.75, 3.54; 9%) | Poor, positive |
| No effect of media, or PWCP and media; variable duration of exposure, based on cross-sectional data |
Note. ANOVA = analysis of variance; AOR = adjusted odds ratio; AUS = Australia; BL = baseline; BLrisk = baseline risk; C = control; CAN = Canada; CI = confidence interval; cig = cigarette(s); GEE = generalized estimating equations; ITC = International Tobacco Control; PW = pictorial warning; PWCP = pictorial warnings on cigarette packages; OR = odds ratio; Q = quartile; RCT = randomized clinical trial; SA = self-affirmation; sig = statistically significant.
Based on the total sum of points for study design (2 = RCT, 1 = cohort, 0 = other designs), outcome definition (2 = clear and complete, 1 = unclear or incomplete, 0 = unclear and incomplete), exposure definition (2 = appropriate PWCP, 1 = appropriate warning intended for printing or inappropriate PWCP, 0 = inappropriate warning), and statistical analyses (2 = pertinent or adjusted, 1 = not pertinent or unadjusted, 0 = not pertinent and unadjusted); studies were classified as of very poor (0–2), poor (3–4), fair (5–6), and good (7–8) quality.
According to the most relevant finding. Positive: statistically significant effect (P < .05) regardless of the association strength; null = no significantly positive effect; mixed = either positive or null results observed; and uncertain = results available precluded a meaningful conclusion.
Articles used similar or identical data for analyses.
*Significant on the basis of 95% CI or P < 0.05.
DISCUSSION
The results of this systematic review showed that evidence concerning the effect of PWCP on smoking behavior is inconclusive, in contrast with previous reviews reporting a significant impact on smokers’ intention to quit.7,10,46,47 These results are in line with the notion that turning the intention to quit smoking into actual and sustained behavioral change is an outcome more difficult to attain and demonstrate with formal tests of effectiveness in evaluation research.
In fact, during this review we also identified articles looking at intention to quit and found nearly 20 studies approaching this issue in different ways,7,10,25,26,28,30,31,33–35,37,39,41,43,46–49 11 of which reported positive findings.7,10,25,26,34,35,40,41,43,46,47 The fact that two thirds of the studies dealing with behavioral outcomes were published within the past 5 years indicates the growing interest in examining the effects of PWCP on smokers.
Among the few countries that conducted studies on behavioral outcomes, Canada provided the largest number of studies. This country not only pioneered using PWCP in 2001, but it was also the only 1 fully complying with International Tobacco Control standards.5 Canada has been collecting data systematically to assess the short- and long-term trends in smoking rates, resulting in one third of the selected articles included in this review.25,27–29,32,33,42 Australia has also produced relevant results on the topic.37,39 Limited evidence from developing countries came from studies conducted in Mexico,40,44 Thailand,31,45 Malaysia,35 and Iran.36
The methodological heterogeneity of the studies was so large that two articles could seldom be compared with one another. This heterogeneity concerned first and foremost the definition of the outcomes. For example, reduction was defined in terms of cigarette consumption (daily, weekly, past 24 hours, past week), as forgoing cigarettes (yes or no; never, once, few times, many times) in various time periods (past month, 6 months, 12 months), or by using different categorical definitions (smoking more, same, or less; smoking less around others as dichotomous variable). The variability in terms of exposure measurement, study design and population, and statistical analysis and adjustments was also very large.
Being a smoker was an eligibility criterion. However, 1 study overtly combined ex-smokers,31 and another seemed to include ex-smokers in the analysis.40 This finding was particularly difficult to interpret because the study outcomes could only occur among a smoking population.
Study quality was generally low. For instance, in 3 articles relevant to cessation no definition was given26,37 or it was unclear.31 Some studies also did not provide an association measure.26,28,31,43 Thus, the results should be contextualized with the poor methodological quality of the studies, adding to the limitations in their interpretation.
Some studies assessed PWCP exposure using intermediary indicators. For instance, authors used the understanding of PWCP (i.e., cognitive processing)25,32,37,40 or the emotional reaction (i.e., fear, disgust) and avoidance behavior27 as measures of exposure. Although 2 of these studies were of fair methodological quality, the lack of an actual comparison with a nonexposed group and the fact that they mainly assessed the short-term effect of PWCP makes questionable the value of the findings observed, which were null in these studies for the cessation outcome.
In 4 studies, it was not possible to disentangle the effects of PWCP on specific behavioral indicators because the outcomes were combined.25,27,39,43 For instance, 2 studies used scales to measure the stage of change toward smoking cessation,39,43 including the precontemplation, contemplation, action, and maintenance phases, rather than using the behavioral outcomes separately. These were included in the action phase, making it impossible to discriminate the effect on the specific outcomes under study. Similarly, 2 other studies pooled attempt, reduction, and cessation into 1 outcome, precluding separate analyses.25,27
Some studies looked at the combined effect of PWCP along with another intervention. Although these studies aimed to examine the effect of this other intervention rather than the sole effect of PWCP, we decided to include them because they compared a combined PWCP with a PWCP-only intervention. For instance, 2 studies tested the notion that an intervention to protect the person’s image of integrity, morality, and adequacy (i.e., self-affirmation) along with the exposure to PWCP would enhance the warning’s impact on behavior (i.e., more favorable message response).30,41 Yet, the results of these fairly well-conducted studies showed similar effects of PWCP on reduction and attempt to quit smoking regardless of the self-affirmation intervention.
Another study examined the combined effects of recalling PWCP and a media campaign (TV or radio),44 showing positive effects on smoking reduction—though similar to a media campaign alone or combined with PWCP—and attempt to quit; we classified this study as being of poor quality.
Tobacco industry representatives have expressed doubts concerning the added value of pictorial warnings to inform consumers about the risks of smoking and their effect on behavior.19 The argument is that text-only warnings might have a similar effect without having to “harass” smokers. In this regard, we identified various studies comparing text only and PWCP, using different approaches. Results differed depending on the outcome assessed.
Three studies indirectly assessed the difference between warnings for cessation: a Mexican pre–post study found a positive effect of PWCP over text as reason for quitting,40 an Australian RCT using computer-based messages only allowed a comparison of the proportions of those quitting smoking with no significant differences after 1 month follow-up,39 and a study from Thailand showed similar effects before (text only) and after the implementation of PWCP.31 We classified all 3 studies as being of poor or very poor quality.
For reduction, data that compared Canada, Australia, the United Kingdom, and the United States showed higher forgoing of cigarettes with PWCP,33 which also had a lesser wear-out effect. Similar results were seen for a study comparing Thailand (PWCP) with Malaysia (text only).45 Conversely, 2 studies showed no differences in cigarettes smoked before (text only) and after implementation of PWCP.34,36 Mixed results were also reported for attempt with a Mexican pre–post study showing no effect,44 contrasting with Australian surveys showing a higher proportion after PWCP implementation.34
Although studies looking at plain tobacco packs have suggested that removing the branding from the pack can reduce the demand for smoking,50–52 so far the evidence concerning behavior change has been very limited. In this review, we identified only 1 study comparing the effect of PWCP printed on a plain cigarette package with that of standard branded packages, with PWCP leading to significant forgoing of cigarettes; however, the study was relatively small, and individuals could receive more than £40 for their participation over 4 weeks, leading to potential bias.38
Nearly all studies examined the combined effect of different pictorial warnings, but 2 tried to discriminate between those producing higher and lower impact on behavior.26,40 The Mexican study found no effect on attempt across the 6 PWCP examined,40 but the Swiss study found that cigarette boxes depicting passive smoking, bad breath, and health risks were related to reduced smoking, as those showing addiction messages were with attempt to quit smoking.26
That warning messages need to rotate and be updated periodically as the effect of the messages wears away with time has been discussed.5 In this review, we identified only 1 study assessing the wear-out effect (about 3 years after implementation) on behavior.33 This study showed a higher impact on forgoing cigarettes for the PWCP implemented in Canada than for the larger text warnings introduced in the United Kingdom, after controlling for differences in implementation times.
Not all studies used actual cigarette packages displaying the pictorial warnings; some used alternative means such as computer screenshots presented in a laboratory setting41 or sent through e-mail39,43 and photographs already used40,44 or for possible use on cigarette packs.44 Although these types of warnings differed from the real branded cigarette packs with pictorial warnings printed on their surface, we believe that these substitutes mimicked well the logic of the PWCP. In most cases, the reason for not using the actual PWCP was logistical because it was difficult to contact individuals periodically to deliver the exposure.
Effect on Smoking Rates
The evidence concerning the impact of PWCP on smoking rates at the population level was beyond the scope of this review. However, for the sake of completeness, we include a perusal of 8 studies included in this review and presenting results on this issue. Three studies presented similar data from Canada,28,42,53 1 was a report from Australia comparing the prevalence of current smokers before and after the implementation of PWCP,34 and 2 were simulation studies of tobacco control policies, including PWCP, to forecast effects on smoking prevalence up to 2040.54,55 The simulation exercises were conducted in Finland and the Netherlands, 2 countries that to date have not implemented PWCP. The remaining 2 studies compared surveys from 245 or 356 countries with and without PWCP implementation in different years. However, only the Canadian and to some extent the Australian data were useful in assessing population trends in smoking prevalence. The decreasing trends observed in Canada (from 26.8% in 2000, 1 year before PWCP, to 21.4% in 2008) and in Australia (from 20% in 2000, 6 years before PWCP, to 17% in 2008) could be attributed to the implementation of various policies, such as regulations concerning advertising and packaging, higher taxes, and bans on smoking in public places, besides PWCP.
Delayed Smoking Initiation
A possible added value of PWCP has been purported with regard to preventing or delaying smoking initiation among adolescents and young adults. In our broad literature search, we did not find any publication specifically looking at this issue. However, 2 experimental studies with adolescents reported decreased intention to smoke after exposure to PWCP compared with no warning57 or text warning.58 However, an undergraduate thesis reported that the way in which the pictorial warnings messages are framed (i.e., gain vs loss) had no effect on the intention to smoke among high school students.48
Conclusions
Until now, studies assessing the effect of PWCP on cessation, reduction, and attempt to quit smoking have been very limited in amount and quality and therefore have provided no clear evidence regarding the question of effectiveness of pictorial warning on smoking behavior. Of the 21 articles that were included in this review, very few would have been selected had we used more strict criteria such as are used in systematic reviews assessing the effect of an intervention.21
Irrespective of study quality, the reported findings were generally null or conflicting for any explored outcome. In fact, the proportions of studies showing null results for cessation, reduction, and attempt to quit smoking were 44.4%, 26.6%, and 27.2%, respectively. The corresponding proportions of positive results were 11.1%, 53.3%, and 27.2%, respectively; the remaining studies presented mixed or uncertain results.
Although the evidence for or against the use of these warnings is insufficient, evidence so far suggests that if PWCP have an effect on behavior, it would be modest compared with other tobacco control policies. It should be borne in mind that tobacco control efforts do not usually rely on a single intervention but on a comprehensive strategy of which PWCP would be just a part. Determining the single impact of PWCP on behavior would require studies based on strong methodological designs, preferably with longer follow-up periods.
Acknowledgments
We acknowledge the critical comments and valuable suggestions made by the reviewers.
Human Participant Protection
No protocol approval was necessary because data were obtained from secondary sources.
References
- 1.Bala MM, Strzeszynski L, Cahill K. Mass media interventions for smoking cessation in adults. Cochrane Database Syst Rev. 2013;2013(6) doi: 10.1002/14651858.CD004704.pub2. CD004704. [DOI] [PubMed] [Google Scholar]
- 2.Mackay J, Eriksen M, Shafey O. The Tobacco Atlas. 2nd ed. Brighton, UK: American Cancer Society; 2006. [Google Scholar]
- 3.Hoek J, Maubach N, Gendall P. Effects of cigarette on-pack warning labels on smokers’ perceptions and behaviour. Borderless Consumption: Asia Pacific Advances in Consumer Research. Vol. 7. In: Craig Lees M, Gregory G, editors. Sydney, New South Wales, Australia: Association for Consumer Research; 2006. pp. 173–180. [Google Scholar]
- 4.Aftab M, Kolben D, Lurie P. International cigarette labelling practices. Tob Control. 1999;8(4):368–372. doi: 10.1136/tc.8.4.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hammond D. Waterloo, Ontario, Canada: Tobacco Labelling Resource Centre; 2009. Tobacco Labelling and Packaging Toolkit: A Guide to FCTC Article 11. [Google Scholar]
- 6.Hammond D. Health warning messages on tobacco products: a review. Tob Control. 2011;20(5):327–337. doi: 10.1136/tc.2010.037630. [DOI] [PubMed] [Google Scholar]
- 7.Rooke S, Malouff JM, Copeland J. Effects of repeated exposure to a graphic smoking warning image. Curr Psychol. 2012;31(3):282–290. [Google Scholar]
- 8.O’Hegarty M, Pederson LL, Nelson DE et al. Reactions of young adult smokers to warning labels on cigarette packages. Am J Prev Med. 2006;30(6):467–473. doi: 10.1016/j.amepre.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 9.Hammond D, Fong GT, McNeill A, Borland R, Cummings KM.Effectiveness of cigarette warning labels in informing smokers about the risks of smoking: findings from the International Tobacco Control (ITC) Four Country Survey Tob Control 200615suppl 3iii19–iii25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cantrell J, Vallone DM, Thrasher JF et al. Impact of tobacco-related health warning labels across socioeconomic, race and ethnic groups: results from a randomized Web-based experiment. PLoS ONE. 2013;8(1):e52206. doi: 10.1371/journal.pone.0052206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.White V, Webster B, Wakefield M. Do graphic health warning labels have an impact on adolescents’ smoking-related beliefs and behaviours? Addiction. 2008;103(9):1562–1571. doi: 10.1111/j.1360-0443.2008.02294.x. [DOI] [PubMed] [Google Scholar]
- 12.Craig L, Sansone N, Sansone G . The International Tobacco Control Policy Evaluation Project: Health Warnings on Tobacco Packages: ITC Cross-Country Comparison Report. Waterloo, Ontario, Canada: University of Waterloo; 2012. [Google Scholar]
- 13.World Health Organization. History of the WHO Framework Convention on Tobacco Control. Available at: http://www.who.int/fctc/about/history/en. Accessed September 30, 2013.
- 14.World Health Organization. WHO Framework Convention on Tobacco Control 2003. Available at: http://www.who.int/fctc/text_download/en. Accessed September 30, 2013.
- 15.International Tobacco Control Policy Evaluation Project. About ITC. Available at: http://www.itcproject.org/about. Accessed September 30, 2013.
- 16.Bansal-Travers M, Hammond D, Smith P, Cummings KM. The impact of cigarette pack design, descriptors, and warning labels on risk perception in the US. Am J Prev Med. 2011;40(6):674–682. doi: 10.1016/j.amepre.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wakefield M, Morley C, Horan JK, Cummings KM. The cigarette pack as image: new evidence from tobacco industry documents. Tob Control. 2002;11(suppl 1):I73–I80. doi: 10.1136/tc.11.suppl_1.i73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schoenbaum M. Do smokers understand the mortality effects of smoking? Evidence from the Health and Retirement Survey. Am J Public Health. 1997;87(5):755–759. doi: 10.2105/ajph.87.5.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.RJ Reynolds Tobacco Co. v. US Food and Drug Administration, 696 F.3d 1205, 1214 (DC Cir 2012) Available at: http://www.cadc.uscourts.gov/internet/opinions.nsf/4C0311C78EB11C5785257A64004EBFB5/$file/11-5332-1391191.pdf. Accessed September 30, 2013.
- 20.Champion VL, Skinner CS. The health belief model. In: Glanz K, Rimer B, Viswanath K, editors. Health Behaviour and Health Education: Theory, Research, and Practice. San Francisco, CA: Jossey-Bass; 2008. pp. 45–65. [Google Scholar]
- 21.Liberati A, Altman DG, Tetzlaff J et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339 doi: 10.1136/bmj.b2700. b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Current cigarette smoking among adults—United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(44):889–894. [PubMed] [Google Scholar]
- 23.Melvin CL, Tucker P. Measurement and definition for smoking cessation intervention research: the smoke-free families experience. Smoke-Free Families Common Evaluation Measures for Pregnancy and Smoking Cessation Projects Working Group. Tob Control. 2000;9(suppl 3):III87–III90. doi: 10.1136/tc.9.suppl_3.iii87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Estabrooks PA, Gaglio B, Morse EF et al. Defining and understanding success at smoking reduction: a mixed-methods study. Addict Behav. 2010;35(12):1113–1119. doi: 10.1016/j.addbeh.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hammond D, Fong GT, McDonald PW, Cameron R, Brown KS. Impact of the graphic Canadian warning labels on adult smoking behaviour. Tob Control. 2003;12(4):391–395. doi: 10.1136/tc.12.4.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Christie D, Etter J. Utilization and impact of cigarette pack covers illustrated with antismoking messages. Eval Health Prof. 2004;27(2):107–118. doi: 10.1177/0163278704264050. [DOI] [PubMed] [Google Scholar]
- 27.Hammond D, Fong GT, McDonald PW, Brown KS, Cameron R. Graphic Canadian cigarette warning labels and adverse outcomes: evidence from Canadian smokers. Am J Public Health. 2004;94(8):1442–1445. doi: 10.2105/ajph.94.8.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Environics Research Group Limited. The health effects of tobacco and health warning messages on cigarette packages—survey of adults and adult smokers. Available at: http://www.smoke-free.ca/warnings/WarningsResearch/POR-04-19%20Final%20Report%205552%20Adult%20wave%209.pdf. Accessed September 30, 2013.
- 29.Hammond D, Fong GT, Borland R et al. Text and graphic warnings on cigarette packages: findings from the International Tobacco Control Four Country Study. Am J Prev Med. 2007;32(3):202–209. doi: 10.1016/j.amepre.2006.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harris PR, Mayle K, Mabbott L, Napper L. Self-affirmation reduces smokers’ defensiveness to graphic on-pack cigarette warning labels. Health Psychol. 2007;26(4):437–446. doi: 10.1037/0278-6133.26.4.437. [DOI] [PubMed] [Google Scholar]
- 31.Silpasuwan P, Yaowaluk N, Viwatwongkasem C et al. Potential effectiveness of health warning labels among employees in Thailand. J Med Assoc Thai. 2008;91(4):551–558. [PubMed] [Google Scholar]
- 32.Borland R, Yong HH, Wilson N et al. How reactions to cigarette packet health warnings influence quitting: findings from the ITC Four-Country survey. Addiction. 2009;104(4):669–675. doi: 10.1111/j.1360-0443.2009.02508.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borland R, Wilson N, Fong GT et al. Impact of graphic and text warnings on cigarette packs: findings from four countries over five years. Tob Control. 2009;18(5):358–364. doi: 10.1136/tc.2008.028043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shanahan P, Elliott D. Evaluation of the Effectiveness of the Graphic Health Warnings on Tobacco Product Packaging 2008. Canberra, Australian Capital Territory, Australia: Australian Government Department of Health and Ageing; 2009. [Google Scholar]
- 35.Fathelrahman AI, Omar M, Awang R et al. Impact of the new Malaysian cigarette pack warnings on smokers’ awareness of health risks and interest in quitting smoking. Int J Environ Res Public Health. 2010;7(11):4089–4099. doi: 10.3390/ijerph7114089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heydari GR, Ramezankhani A, Talischi F. The impacts of cigarette packaging pictorial warning labels on smokers in the city of Tehran. Tanaffos. 2011;10(1):40–47. [PMC free article] [PubMed] [Google Scholar]
- 37.Miller CL, Hill DJ, Quester PG, Hiller JE. The impact of Australia’s new graphic cigarette packet warnings on smokers’ beliefs and attitudes. AMJ. 2011;19(3):181–188. [Google Scholar]
- 38.Moodie C, Mackintosh AM, Hastings G, Ford A. Young adult smokers’ perceptions of plain packaging: a pilot naturalistic study. Tob Control. 2011;20(5):367–373. doi: 10.1136/tc.2011.042911. [DOI] [PubMed] [Google Scholar]
- 39.Malouff JM, Schutte NS, Rooke SE, MacDonell G. Effects on smokers of exposure to graphic warning images. Am J Addict. 2012;21(6):555–557. doi: 10.1111/j.1521-0391.2012.00284.x. [DOI] [PubMed] [Google Scholar]
- 40.Thrasher JF, Perez-Hernandez R, Arillo-Santillan E, Barrientos-Gutierrez I. Towards informed tobacco consumption in Mexico: effect of pictorial warning labels in smokers. Salud Publica Mex. 2012;54(3):242–253. [PMC free article] [PubMed] [Google Scholar]
- 41.Zhao X, Peterson EB, Kim W, Rolfe-Redding J. Effects of self-affirmation on daily versus occasional smokers’ responses to graphic warning labels. Communic Res. 2012 Epub ahead of print November 9, 2012. [Google Scholar]
- 42.Azagba S, Sharaf MF. The effect of graphic cigarette warning labels on smoking behavior: evidence from the Canadian experience. Nicotine Tob Res. 2013;15(3):708–717. doi: 10.1093/ntr/nts194. [DOI] [PubMed] [Google Scholar]
- 43.Malouff JM, Emmerton AJ, Schutte NS. Changes in smoking level after viewing graphic cigarette warnings: preliminary findings. Am J Addict. 2013;22(4):388–390. doi: 10.1111/j.1521-0391.2013.12040.x. [DOI] [PubMed] [Google Scholar]
- 44.Thrasher JF, Murukutla N, Perez-Hernandez R et al. Linking mass media campaigns to pictorial warning labels on cigarette packages: a cross-sectional study to evaluate effects among Mexican smokers. Tob Control. 2013;22(e1):e57–e65. doi: 10.1136/tobaccocontrol-2011-050282. [DOI] [PubMed] [Google Scholar]
- 45.Yong HH, Fong GT, Driezen P et al. Adult smokers’ reactions to pictorial health warning labels on cigarette packs in Thailand and moderating effects of type of cigarette smoked: findings from the International Tobacco Control Southeast Asia Survey. Nicotine Tob Res. 2013;15(8):1339–1347. doi: 10.1093/ntr/nts241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brennan E, Durkin SJ, Cotter T, Harper T, Wakefield MA. Mass media campaigns designed to support new pictorial health warnings on cigarette packets: evidence of a complementary relationship. Tob Control. 2011;20(6):412–418. doi: 10.1136/tc.2010.039321. [DOI] [PubMed] [Google Scholar]
- 47.Nonnemaker J, Farrelly M, Kamyab K, Nusey A, Mann N. Experimental Study of Graphic Cigarette Warning Labels. Rockville, MD: Food and Drug Administration, Center for Tobacco Products; 2010. [Google Scholar]
- 48.Goodall CE. Modifying Smoking Behavior Through Public Service Announcements and Cigarette Package Warning Labels: A Comparison of Canada and the United States [senior honors thesis] Columbus, OH: Ohio State University; 2005. [Google Scholar]
- 49.Romer D, Peters E, Strasser AA, Langleben D. Desire versus efficacy in smokers’ paradoxical reactions to pictorial health warnings for cigarettes. PLoS ONE. 2013;8(1):e54937. doi: 10.1371/journal.pone.0054937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hoek J, Wong C, Gendall P, Louviere J, Cong K. Effects of dissuasive packaging on young adult smokers. Tob Control. 2011;20(3):183–188. doi: 10.1136/tc.2010.037861. [DOI] [PubMed] [Google Scholar]
- 51.White CM, Hammond D, Thrasher JF, Fong GT. The potential impact of plain packaging of cigarette products among Brazilian young women: an experimental study. BMC Public Health. 2012;12:737. doi: 10.1186/1471-2458-12-737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hammond D. “Plain packaging” regulations for tobacco products: the impact of standardizing the color and design of cigarette packs. Salud Publica Mex. 2010;52(suppl 2):S226–S232. doi: 10.1590/s0036-36342010000800018. [DOI] [PubMed] [Google Scholar]
- 53.Gospodinov N, Irvine IJ. Global health warnings on tobacco packaging: evidence from the Canadian experiment. Top Econ Anal Policy. 2004;4(1) Article 30. [Google Scholar]
- 54.Levy DT, Blackman K, Currie LM, Levy J, Clancy L. SimSmokeFinn: how far can tobacco control policies move Finland toward tobacco-free 2040 goals? Scand J Public Health. 2012;40(6):544–552. doi: 10.1177/1403494812456635. [DOI] [PubMed] [Google Scholar]
- 55.Nagelhout GE, Levy DT, Blackman K et al. The effect of tobacco control policies on smoking prevalence and smoking-attributable deaths. Findings from the Netherlands SimSmoke tobacco control policy simulation model. Addiction. 2012;107(2):407–416. doi: 10.1111/j.1360-0443.2011.03642.x. [DOI] [PubMed] [Google Scholar]
- 56.Thrasher JF, Villalobos V, Szklo A et al. Assessing the impact of cigarette package health warning labels: a cross-country comparison in Brazil, Uruguay and Mexico. Salud Publica Mex. 2010;52(suppl 2):S206–S215. doi: 10.1590/s0036-36342010000800016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Golmier I, Chebat JC, Gelinas-Chebat C. Can cigarette warnings counterbalance effects of smoking scenes in movies? Psychol Rep. 2007;100(1):3–18. doi: 10.2466/pr0.100.1.3-18. [DOI] [PubMed] [Google Scholar]
- 58.Veer E, Rank T. Warning! The following packet contains shocking images: the impact of mortality salience on the effectiveness of graphic cigarette warning labels. J Consum Behav. 2012;11(3):225–233. [Google Scholar]