Abstract
Objectives. We evaluated the relationship between dentist supply and children’s oral health and explored heterogeneity by children’s age and urbanicity.
Methods. We obtained data from the 2007 National Survey of Children’s Health (> 27 000 children aged 1–10 years; > 23 000 children aged 11–17 years). We estimated the association between state-level dentist supply and multiple measures of children’s oral health using regression analysis adjusting for several child, family, and population-level characteristics.
Results. Dentist supply was significantly related to better oral health outcomes among children aged 1 to 10 years. The odds of decay and bleeding gums were lower by more than 50% (odds ratio [OR] = 0.46; 95% CI = 0.23, 0.95) and 80% (OR = 0.18; 95% CI = 0.05, 0.76), respectively, with an additional dentist per 1000 population. The odds of a worse maternal rating of child’s dental health on a 5-category scale from poor to excellent were lower by about 50% in this age group with an additional dentist per 1000 population (OR = 0.51; 95% CI = 0.29, 0.91). We observed associations only for children in urban settings.
Conclusions. Dentist supply is associated with improved oral health for younger children in urban settings.
Children’s oral health has improved overall over the past few decades in the United States because of the introduction of fluoride into public water systems and the increased use of preventive dental care, among other factors.1 Despite this improvement, dental problems are still highly prevalent among children in the United States, and dental caries remain the leading chronic disease among children.2 Indeed 20.5% of children aged 5 to 11 years had untreated dental caries between 2005 and 2008.3 Furthermore, contrary to the overall improvement trend, the prevalence of dental caries among children aged 2–4 years has increased during the past 2 decades, from 18.0% in 1988 to 1994 to 24.0% in 1999–2004.1 These statistics create a drag on the performance of the dental health care system and highlight the need to identify and modify the pathways leading to the high prevalence of dental problems.
Limited access to dental care in many areas is thought to be among the main causes of child dental problems and disparities in children’s oral health in the United States. Both demand- and supply-side and patient- and provider-side factors can affect access to dental care. On the demand side, family demographic and socioeconomic factors (including race, socioeconomic status, oral health literacy, dental insurance, and demand for preventive care) have been found to be relevant for dental care use.4–6 On the supply side, characteristics of the dental insurance market (including reimbursement mechanisms, patient cost sharing, provider contracting, and beneficiary enrollment procedures), availability and location of dentists, and quality of dental services are also considered relevant.7,8 The Health Resources and Services Administration has designated close to 4800 geographic areas as dental care health professional shortage areas.9 Dentist shortage in these areas has been identified as a leading cause of access problems and gaps in supply and utilization of dental care.8,10,11 Nearly 50 million people in the United States live in dental professional shortage areas; 30 million of them have no access to a dentist.12,13 Dentist shortage is projected to continue and increase, particularly in rural areas.14,15
Despite its conceptually relevant role, there is little empirical assessment of the importance of dentist supply and implications of changes in the dental workforce for children’s oral health in the United States. A recent study reported a negative correlation between number of dentists relative to the size of the state’s population and proportion of children with oral health problems in the state.16 However, the association became insignificant in multivariate regression analyses. Although important, that study used only state-level data, had a fairly descriptive analysis, and did not explore heterogeneity by children’s age. To the best of our knowledge, no other published studies have evaluated the association between dentist supply and children’s oral health using a nationally representative sample of children while controlling for population and health care market characteristics that may influence both oral health and dentist supply. Specifically, not much is known about how dentist supply is related to different aspects of children’s oral health and whether any association is driven by dentist selection in locating into areas with certain population economic and demographic characteristics that in turn affect children’s oral health or by potential benefits to children’s oral health.
We evaluated the association between dentist supply and children’s oral health in a large nationally representative sample of US children. We adjusted for several child-, family-, and population-level characteristics to control as much as possible for potential confounders that are conceptually relevant for both children’s oral health and dentist location decisions. These include various child and household socioeconomic and demographic characteristics, child neighborhood conditions, state-level supply of family and general practitioners and pediatricians, and sociodemographic state-level indicators. We also explored the heterogeneity in the relationship between dentist supply and children’s oral health by child’s age—because of its importance for changes in dental health risks and interactions with the dental health care system—and by urbanicity—because of its effects on access and dentist supply and the greater concern about dentist shortage in rural areas.
METHODS
We studied a nationally representative sample of children who participated in the 2007 National Survey of Children’s Health (NSCH). The National Center for Health Statistics at the Centers for Disease Control and Prevention conducted the 2007 NSCH to provide national and state-level data on different aspects of children’s health. The NSCH used a multistage random sampling design to provide samples of children and adolescents (aged 17 years and younger) in all 50 states and the District of Columbia. In each state a sample of households was randomly selected, and in each identified household, 1 child was randomly selected. Data on several demographic, economic, health, family, and neighborhood characteristics were obtained from parents or caregivers through telephone interviews.17 The NSCH has been employed in several previous studies of children’s oral health in the United States 8,18–22 and provides the largest sample from a nationally representative survey of children with data on oral health. We limited the sample to children aged at least 1 year because this is the age for which the survey included questions about oral health and included children aged 17 years and younger. We included only children whose mother completed the study interview to reduce the chances of measurement errors and reporting inaccuracies.
Main Measures
We considered multiple oral health outcomes to capture the various aspects of oral health that are possibly sensitive to dentist supply. These outcomes were derived from maternal responses to specific questions in the survey about oral health. The first set of measures included binary indicators for whether the child has experienced decay or bleeding gums during the past 6 months, which are the main dental problems among children. We first evaluated each of these problems separately and then combined them in a binary indicator for having had either or both of these problems. Another outcome was maternal rating of the child’s dental health status on a 5-item scale. Specifically, the mothers answered the following question: “How would you describe the condition of [the child’s] teeth: excellent, very good, good, fair, or poor?” These oral health outcomes have been shown to be related to schooling problems and psychosocial well-being in this sample,19 which supports their validity.
We measured dentist supply by the number of professionally active dentists per 1000 individuals in the state in 2007; the state is the smallest identifiable geographic unit available for the NSCH. We divided by total population in the state instead of children’s population because the same dentists may see both children and adults, in which case children’s access would depend on the supply of dentists relative to the total population including children and adults. We obtained these data from the Area Resource File.23
Statistical Analysis
We evaluated the relationship between dentist supply and children’s oral health using multivariate regression models that adjusted for several potential confounding variables that are conceptually relevant for both dentist supply and child oral health. We weighted all models with the sampling probability weights and accounted for the NSCH’s complex and hierarchical sampling design. We estimated robust SEs that account for clustering (dependence) of observations within the same state. We used binary logistic regression for the dichotomous measures of child dental health problems and ordered logistic regression for the multicategory ordinal measure of maternal-rated dental health status. The regression models controlled for child and household demographic and socioeconomic characteristics and for neighborhood safety, social, and economic conditions. These factors may affect the location decisions of dentists but may also influence oral health in several ways, including through the use of dental care and household-based behaviors related to oral health such as diet and teeth brushing.20,24
We controlled for the following demographic characteristics: child’s gender, race/ethnicity, country of birth (United States vs others), numbers of children and adults in the household, and maternal age and marital status. We included the following household socioeconomic characteristics: maternal education, household income relative to federal poverty level (according to the Department of Health and Human Services’ federal poverty guidelines for 2007), and child’s health insurance coverage. We also included measures of various aspects of the neighborhood where the child lived, including physical condition (presence of litter or garbage, poorly kept or rundown housing, and availability of a library or bookmobile), safety (presence of vandalism and maternal perception of child’s safety), and social capital (people in the neighborhood helping each other, watching out for each other’s children, and counting on each other, and adults helping children if they are hurt or scared). In addition to their conceptual relevance for both dentist location decisions and parents access and use of dental care, several of these factors have been shown to be relevant for oral health, including in this sample.18,20,25 In an alternative model, we included an aggregate index of neighborhood quality derived from these variables (generated using principal component analysis), but this had no effect on the results for dentist supply (details available upon request).
In addition to the household and neighborhood factors we have described, we controlled for several state-level characteristics that may relate to both dentist supply and oral health. We included the number of active family and general practitioners and pediatricians per 1000 children in 2007, measured from the Area Resource File, because pediatric and general well-child care visits may influence dental care utilization.26 Other state-level covariates were the percentage of children in households with income less than 200% of the federal poverty level in 2007, proportion of children (up to aged 19 years) in the total population in 2007, the percentage of population living in nonmetropolitan areas (2006–2007), and the percentage of population who are uninsured (2006–2007).
The relationship between dentist supply and children’s oral health may vary with the child’s age because of changes in risk factors, including different stages of dental development, dietary and oral hygiene habits, social networks, and interactions between dentists and children.27 Previous research has shown that the relationship between oral health and children’s educational achievement and psychosocial well-being also varies with the child’s age,19 suggesting that dental care needs and effectiveness may vary with age. Therefore, we estimated all models separately for the following 2 age groups: aged 1 to 10 years, representing preschool and elementary school age, and aged 11 to 17 years, representing middle and high school age.
In addition, because access to dental care depends on rural versus urban status, which could modify the relationship between dentist supply and oral health, we further stratified the analysis in additional models by urbanicity of the child’s area of residence. We classified the area of residence as urban or rural on the basis of whether the child lived in a metropolitan statistical area (MSA). Because the information on children’s MSA status was suppressed in the NSCH data set for 16 states, we first restricted this analysis to the states with data on MSA status. In an additional model, we imputed MSA status for children in states with missing data using the imputation procedure recommended in the NSCH documentation.16
RESULTS
The initial sample included 63 825 children aged 1 to 17 years whose mother completed the NSCH interview. For each outcome, we included only children with complete data on the outcome and covariates in the models. The final analytical sample ranged from 27 174 to 27 197 for children aged 1 to 10 years and from 23 827 to 23 902 for children aged 11 to 17 years, with the variation being because of having data on at least 1 but not all the outcomes. Descriptive statistics for the dental health outcomes, dentist supply, and model covariates are presented in Table 1. More than 17% of all children had decay, and 20% experienced either decay or bleeding gums. Dental problems were slightly more prevalent later in childhood, with about 21% of children aged 11 to 17 years experiencing decay or bleeding gums compared with 19% of younger children. About 6% of all children had their teeth reported in less than good condition (fair or poor).
TABLE 1—
Weighted Descriptive Statistics for Study Variables: National Survey of Children’s Health, United States, 2007
| Variable | Total Sample (N = 63 825), % or Mean (SD) | 1–10 y (n = 33 990), % or Mean (SD) | 11–17 y (n = 29 835), % or Mean (SD) |
| Oral health variables | |||
| Decay | 17.54 | 16.80 | 18.38 |
| Bleeding gums | 3.39 | 2.82 | 4.04 |
| Decay or bleeding gums | 19.60 | 18.57 | 20.78 |
| Self-rated oral health | |||
| Poor | 0.98 | 0.96 | 1.00 |
| Fair | 5.19 | 5.11 | 5.28 |
| Good | 19.20 | 18.46 | 20.04 |
| Very good | 24.39 | 23.39 | 25.51 |
| Excellent | 50.25 | 52.08 | 48.18 |
| Child is female | 48.53 | 47.62 | 49.56 |
| Race/ethnicity | |||
| non-Hispanic White | 59.77 | 57.32 | 62.54 |
| non-Hispanic Black | 11.81 | 10.63 | 13.14 |
| Hispanic | 20.94 | 23.33 | 18.24 |
| Other | 7.49 | 8.72 | 6.09 |
| Child born in the United States | 96.24 | 97.23 | 95.12 |
| Mother’s age | 39.48 (8.06) | 35.38 (7.02) | 44.14 (6.47) |
| Mother is married | 74.34 | 75.17 | 73.41 |
| No. of children in the household | 1.89 (0.89) | 1.99 (0.89) | 1.78 (0.88) |
| No. of adults in the household | 2.10 (0.57) | 2.07 (0.51) | 2.13 (0.63) |
| Mother’s general health is fair or poor | 10.40 | 8.54 | 12.50 |
| Mother’s education | |||
| < high school | 9.80 | 10.40 | 9.13 |
| High school graduate | 19.42 | 17.53 | 21.55 |
| > high school | 70.78 | 72.08 | 69.32 |
| Poverty level of householda | 5.76 (2.54) | 5.62 (2.60) | 5.91 (2.47) |
| Employmentb | 90.56 | 90.20 | 90.97 |
| Child insurance status | |||
| Private health insurance | 69.50 | 66.68 | 72.67 |
| Public health insurance | 22.18 | 25.51 | 18.42 |
| Uninsured | 8.33 | 7.81 | 8.90 |
| Neighborhood-level characteristics | |||
| Has library or bookmobile | 87.59 | 87.62 | 87.56 |
| Has litter or garbage on the street or sidewalk | 16.35 | 17.42 | 15.14 |
| Has poorly kept or rundown housing | 13.32 | 13.80 | 12.78 |
| Has vandalism such as broken windows or graffiti | 11.21 | 11.58 | 10.80 |
| Neighborhood feels safe | 86.00 | 84.61 | 87.58 |
| People help each other out | 88.22 | 88.05 | 88.41 |
| People watch out for each other’s children | 88.60 | 88.26 | 88.99 |
| Can count on people | 88.71 | 87.79 | 89.75 |
| Adults help if child is hurt or scared | 90.71 | 89.23 | 92.37 |
| State-level characteristics | |||
| Dentist supply: dentists/1000 population | 0.62 (0.16) | 0.62 (0.16) | 0.62 (0.16) |
| Family or general practitioners and pediatricians/1000 children | 3.08 (0.77) | 3.06 (0.77) | 3.10 (0.77) |
| % children’s population in households with income < 200% FPL | 36.16 (7.30) | 36.24 (7.33) | 36.08 (7.27) |
| % population who are children, < 19 y | 26.97 (1.87) | 27.00 (1.90) | 26.94 (1.82) |
| % population living in nonmetropolitan areas | 26.39 (18.35) | 26.08 (18.24) | 26.74 (18.45) |
| % population uninsured | 14.19 (3.98) | 14.25 (3.98) | 14.12 (3.97) |
Note. FPL = federal poverty level (from Department of Health and Human Services’ federal poverty guidelines, 2007).
Poverty level represents ranges of the percentage of FPL as follows: 1 (≤ 100%), 2 (101%–133%), 3 (134%–150%), 4 (151%–185%), 5 (186%–200%), 6 (201%–300%), 7 (301%–400%), 8 (> 400%).
Anyone in the household employed at least 50 of the past 52 weeks.
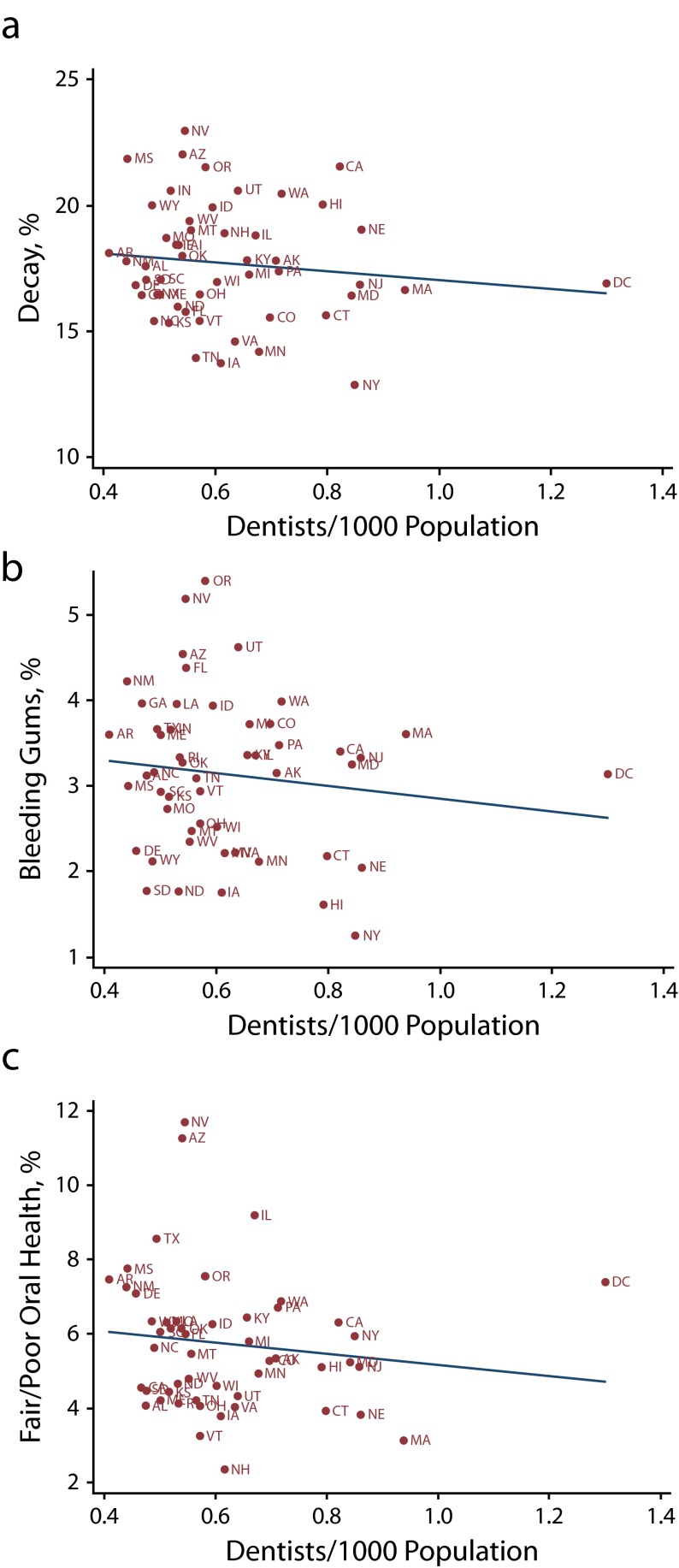
Figure 1 shows the number of dentists per capita and rates of the study oral health outcomes across states (on the basis of weighted state sample rates). There was wide geographic variation in dentist supply, with the number of dentists per 1000 population ranging from 0.41 in Arkansas to 1.30 in the District of Columbia. There were also prominent differences in outcome rates among states. For example, in New York the rates of decay, bleeding gums, and less than good oral health were 13%, 1%, and 6%, respectively, compared with 23%, 5%, and 12% in Nevada. Although unadjusted, these plots suggest a decline in the rates of the adverse oral health outcomes with increased dentist supply. Other state-level characteristics also varied substantially between states (data not shown). For example, the number of pediatricians and family and general practitioners per 1000 children ranged from 1.9 in Nevada to 5.3 in Vermont.
FIGURE 1—
State-level prevalence of oral health indicators in children aged 1–17 years vs number of dentists per 1000 population for (a) decay, (b) bleeding gums, and (c) fair/poor oral health: National Survey of Children’s Health, United States, 2007.
Note. District of Colombia (DC) is shown separately on the graph. The linear (unadjusted) relationship between each outcome and dentist supply estimated using ordinary least squares is shown as a solid line on each panel.
Table 2 reports the regression results as odds ratios (ORs) and 95% confidence intervals (CIs) for dentist supply, adjusting for all model covariates listed in Table 1 (regression results for all covariates are available as a supplement to this article at http://www.ajph.org). Dentist supply was significantly (at least at P < .05) related to better oral health among children aged 1 to 10 years on all oral health outcomes. The association was sizeable in all specifications. The odds of decay and bleeding gums were lower by more than 50% (OR = 0.46; 95% CI = 0.23, 0.95) and 80% (OR = 0.18; 95% CI = 0.05, 0.76), respectively, with an additional dentist per 1000 population. Similarly, the odds of a worse oral health rating on the 5-category scale from poor to excellent in the ordered logit model were lower by about 50% in this age group (OR = 0.51; 95% CI = 0.29, 0.91). By contrast, dentist supply was not significantly related to oral health for older children (11–17 years). Furthermore, the relationship was of the opposite (unexpected) sign (albeit insignificant) compared with the younger age group for decay (both alone and when combined with bleeding gums) and maternal-rated dental health with relatively large ORs but also wide intervals.
TABLE 2—
Association Between State-Level Dentist Supply and Children’s Oral Health (by Child’s Age Group): National Survey of Children’s Health, United States, 2007
| Aged 1–10 Years |
Aged 11–17 Years |
|||
| Variable | No. | OR (95% CI) | No. | OR (95% CI) |
| Decay | 27 180 | 0.46* (0.23, 0.95) | 23 838 | 1.78 (0.76, 4.17) |
| Bleeding gums | 27 197 | 0.18* (0.05, 0.76) | 23 877 | 0.79 (0.15, 4.27) |
| Decay or bleeding gums | 27 174 | 0.38** (0.19, 0.76) | 23 827 | 1.56 (0.69, 3.52) |
| Self-rated oral healtha | 27 179 | 0.51* (0.29, 0.91) | 23 902 | 1.24 (0.70, 2.23) |
Note. CI = confidence interval; OR = odds ratio.
Estimated from an ordered logit model for predicting a worse rating on a 5-category scale (poor, fair, good, very good, and excellent).
*P ≤ .05; **P ≤ .01.
When stratified further by rural versus urban status, dentist supply was significantly related to better oral health only among children aged 1 to 10 years living in an MSA (Table 3 and supplemental data available at http://www.ajph.org; analysis was limited to 35 states with nonimputed MSA status). Among those children, the odds of decay and bleeding gums were lower by 70% (OR = 0.30; 95% CI = 0.12, 0.77) and almost 90% (OR = 0.12; 95% CI = 0.02, 0.80), respectively, with an additional dentist per 1000 population. Likewise, the odds of worse maternal rating of the child’s dental health on the 5-category scale were lower by more than 50% in this group (OR = 0.41; 95% CI = 0.20, 0.82). On the other hand, there was no significant association between dentist supply and oral health among children aged 1 to 10 years living outside an MSA, and the associations were of the unexpected direction for decay and maternal-rated oral health. Similarly, there was no significant association for children aged 11 to 17 years in either MSA or non-MSA areas. The results were very similar when imputing MSA status for children living in states with suppressed MSA data in the NSCH (detailed results available upon request).
TABLE 3—
Association Between State-Level Dentist Supply and Children’s Oral Health (by Child’s Age Group and Rural vs Urban Status): National Survey of Children’s Health, United States, 2007
| Within an MSA, Aged 1–10 Years |
Outside an MSA, Aged 1–10 Years |
Within an MSA, Aged 11–17 Years |
Outside an MSA, Aged 11–17 Years |
|||||
| Variable | No. | OR (95% CI) | No. | OR (95% CI) | No. | OR (95% CI) | No. | OR (95% CI) |
| Decay | 14 984 | 0.30* (0.12, 0.77) | 4086 | 1.60 (0.24, 10.72) | 12 474 | 1.91 (0.69, 5.27) | 3817 | 2.02 (0.43, 9.50) |
| Bleeding gums | 14 998 | 0.12* (0.02, 0.80) | 4051 | 0.48 (0.03, 8.24) | 12 492 | 0.85 (0.11, 6.80) | 3825 | 0.11 (0.01, 1.50) |
| Decay or bleeding gums | 14 981 | 0.24** (0.10, 0.59) | 4087 | 1.48 (0.24, 9.34) | 12 467 | 1.67 (0.63, 4.44) | 3819 | 1.34 (0.30, 5.93) |
| Self-rated oral healtha | 14 982 | 0.41* (0.20, 0.82) | 4085 | 1.56 (0.39, 6.30) | 12 506 | 1.22 (0.60, 2.49) | 3832 | 0.90 (0.28, 2.92) |
Note. CI = confidence interval; OR = odds ratio.
Estimated from an ordered logit model for predicting a worse rating on a 5-category scale (poor, fair, good, very good, and excellent).
*P ≤ .05; **P ≤ .01.
DISCUSSION
We examined the relationship between dentists supply and children’s oral health in a large and nationally representative sample of children aged 1 to 17 years. We found a large and significant association among children aged 1 to 10 years, for whom the risks of dental problems and worse dental health rating (by the mother) on a 5-category poor to excellent scale decreased by nearly 50% with an additional dentist per 1000 population. This finding indicates that the supply of dentists contributes to geographic variation in oral health among younger children.
One mechanism behind this finding could be that a low availability of dental providers limits access and use of dental services, which in turn has consequences for children’s oral health. However, further evidence for this pathway is needed because previous studies have examined only the relationship between dentist supply and preventive care but not treatment. Furthermore, these previous analyses have produced mixed results. Using the 2007 NSCH, Lin et al. found a significant positive association between dentist-to-population ratio and use of preventive dental care for children aged 5 to 17 years.8 However, 2 other studies using the 2003 NSCH did not find a significant relationship between preventive dental care use and dentist supply at county28 or state levels.29
We evaluated the relationship between dentist supply and use of preventive dental care sample using the same sample inclusion criteria and regression model (including covariates) we used for oral health outcomes but found nonsignificant results. However, we were able to find a positive association between dentist supply and preventive dental care use for children aged 5 to 17 years when using a set of covariates that is closer to that in Lin et al.’s study.8 The excluded covariates were maternal age and marital status, household employment status, neighborhood quality characteristics, and certain state-level characteristics (pediatricians and general practitioners per 1000 children, percentage of population who are children, and percentage of state population in nonmetropolitan areas).
When we stratified by child’s rural versus urban status, this association was only significant for children living in MSAs. Therefore, the lack of a significant association between dentist supply and preventive dental care in our main model is owing to controlling for many more relevant covariates that may confound this association if excluded. It was not possible to assess the relationship between dentist supply and other (nonpreventive) dental care services using the NSCH, which does not include those measures. Evaluating this question in other data sets, such as Medicaid claims, that provide these data is an important future research question.
The observed heterogeneity by rural versus urban status suggests that any potential benefits from greater dentist supply are not uniform across rural and urban areas and that simply increasing the number of dentists in the state would not be enough on its own to dramatically change the oral health of younger children in rural areas. Larger distances to dental care providers (with higher transportation cost), lower rates of dental insurance coverage in rural areas,28,30 and the limited availability of dentists within rural areas could partly explain our results; these factors would limit access to dental care services for children in rural areas even if the number of dentists at the state level is high.
Our state-level measure of total dentists per 1000 population combined dentists in rural and urban areas because children may obtain services outside the geographic areas where they reside. However, this combined measure may be less relevant for children in rural areas because of the greater concentration of dentists in urban areas. To evaluate whether our results are driven by this measurement, we reestimated the models for children outside an MSA, measuring dentist supply only on the basis of the population and dentists in rural counties, and found insignificant results (data available as a supplement to this article at http://www.ajph.org). More work is needed to understand the sources of the observed heterogeneity by rural versus urban status.
The lack of a significant association for older children (aged 11–17 years) suggests that other factors may mitigate the relationship between dentist supply and oral health for this age group. We compared the relationship between child’s oral health and model covariates by age group (data available as a supplement to this article at http://www.ajph.org) and found some notable differences for certain sociodemographic characteristics. Maternal age, number of children in the household, and child’s country of birth (United States vs others) were significantly associated with oral health among children aged 1 to 10 years but not among those aged 11 to 17 years. Likewise, the number of active family and general practitioners and pediatricians per 1000 children showed a positive (unexpected direction) and significant relationship with oral health problems and worse maternal rating of child’s dental health for children 11 to 17 years, but these were not significant for younger children.
These differences suggest changing influences and risk factors for child oral health by age; their role in modifying the relationship between dentist supply and oral health is worth exploring in future research. There were no systematic differences between the 2 age groups in the associations of other model covariates with the dental health outcomes. Other factors, including parenting, diet, dental hygiene, and child’s activities and social networks, also change and modify oral disease risks later in childhood and in adolescence. Such factors are not captured in the NSCH and should be explored in other data sets that have these measures.
Our findings have important implications for policymakers. The decline in dentist workforce and potential future shortage may have negative consequences for the oral health of younger children, highlighting the need for policy initiatives that facilitate and promote the demand for and supply of dental education and training such as through laws related to school accreditation, licensing, and educational loans. However, the findings also indicate that whereas policies to increase dentist relocation into rural areas are important to increase access, they may not be sufficient alone because demand-side constraints such as distance and cost (in part because of the lack of dental care coverage) may still limit the use of dental care. The observed association between state-level variation in dentists and child oral health outcomes may partly reflect variation in the supply of other dental professionals, such as dental hygienists.
Evaluating the role and capacity of these dental professionals in providing basic preventive dental care and the effects of their supply on child dental health would shed light on potential alternative supply-side initiatives and policies to improve oral health outcomes, especially in rural areas, and should be considered in future research. Finally, our study identifies early childhood as a more sensitive period to dentist supply than is adolescence, supporting the need for early access to dental care and suggesting that policies that improve access early in life are particularly important for child oral health. However, again, future research is needed to identify the factors behind the depreciation in the association between dentist supply and oral health later in childhood.
Our study has several strengths, including the large and nationally representative sample, controlling for several conceptually relevant variables, evaluating multiple dental health outcomes, and exploring heterogeneity by child age and urbanicity. There are some limitations that warrant discussion and highlight future research directions. Even though we controlled for many potential confounders, we were able to estimate only associations and not causal effects. The cross-sectional design of the NSCH prevented us from evaluating oral health trajectories and how dental health outcomes specific to a child vary with dentist supply over time.
The lack of microlevel geographic data on dentist location and distance to children limited our measurement of dentist supply to the state level; such data would help accurately capture the availability of dentists at the child level, including distance to the nearest dentist. Finally, clinical measures of oral health may be more accurate than are mother-reported measures. Other data sets that could address these limitations and that should be considered in future research are the Medicaid enrollment and claim files, although at the cost of not being nationally representative. Nonetheless, Medicaid data would be helpful in further understanding the role of dental supply factors in the oral health of a large and disadvantaged group of children in the United States.
Acknowledgments
The authors thank Fred Ullirch, research specialist at the University of Iowa, for assistance with the Area Resource File data.
Human Participant Protection
No protocol approval was necessary because the study used existing publicly available data without personal identifiers.
References
- 1.Tomar SL, Reeves AF. Changes in the oral health of US children and adolescents and dental public health infrastructure since the release of the Healthy People 2010 objectives. Acad Pediatr. 2009;9(6):388–395. doi: 10.1016/j.acap.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: National Institute of Dental and Craniofacial Research; 2000. [Google Scholar]
- 3.Dye BA, Li X, Beltran-Aguilar ED. Selected oral health indicators in the United States, 2005–2008. NCHS Data Brief. 2012;(96):1–8. [PubMed] [Google Scholar]
- 4.Yu SM, Bellamy HA, Kogan MD, Dunbar JL, Schwalberg RH, Schuster MA. Factors that influence receipt of recommended preventive pediatric health and dental care. Pediatrics. 2002;110(6):e73. doi: 10.1542/peds.110.6.e73. [DOI] [PubMed] [Google Scholar]
- 5.Edelstein BL, Chinn CH. Update on disparities in oral health and access to dental care for America’s children. Acad Pediatr. 2009;9(6):415–419. doi: 10.1016/j.acap.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 6.Wehby G, Jones M, Momany E, Kuthy R, Carter K, Damiano P. Returns of early dental health prevention: the case of comprehensive oral evaluation. Presented at the American Public Health Association Meeting; October 27–31, 2012; San Francisco, CA.
- 7.Liao C-C, Ganz ML, Jiang H, Chelmow T. The impact of the public insurance expansions on children’s use of preventive dental care. Matern Child Health J. 2010;14(1):58–66. doi: 10.1007/s10995-008-0432-3. [DOI] [PubMed] [Google Scholar]
- 8.Lin M, Sappenfield W, Hernandez L et al. Child- and state-level characteristics associated with preventive dental care access among US children 5–17 years of age. Matern Child Health J. 2012;16(suppl 2):320–329. doi: 10.1007/s10995-012-1099-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. U.S. Department of Health and Human Services. Shortage designation: health professional shortage areas. Available at: http://www.hrsa.gov/shortage. Accessed May 13, 2014.
- 10.Krause D, Frate DA, May WL. Demographics and distribution of dentists in Mississippi: a dental work force study. J Am Dent Assoc. 2005;136(5):668–677. doi: 10.14219/jada.archive.2005.0241. [DOI] [PubMed] [Google Scholar]
- 11.Chi DL, Momany ET, Kuthy RA, Chalmers JM, Damiano PC. Preventive dental utilization for Medicaid-enrolled children in Iowa identified with intellectual and/or developmental disability. J Public Health Dent. 2010;70(1):35–44. doi: 10.1111/j.1752-7325.2009.00141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gehshan S, Mijic M. Getting help for children: the need to expand the dental workforce. J Calif Dent Assoc. 2011;39(7):481–490. [PubMed] [Google Scholar]
- 13.Bazargan N, Chi DL, Milgrom P. Exploring the potential for foreign-trained dentists to address workforce shortages and improve access to dental care for vulnerable populations in the United States: a case study from Washington State. BMC Health Serv Res. 2010;10:336. doi: 10.1186/1472-6963-10-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuthy RA, McKernan SC, Hand JS, Johnsen DC. Dentist workforce trends in a primarily rural state: Iowa: 1997–2007. J Am Dent Assoc. 2009;140(12):1527–1534. doi: 10.14219/jada.archive.2009.0105. [DOI] [PubMed] [Google Scholar]
- 15. US Department of Health and Human Services. Oral health workforce. Available at: http://www.hrsa.gov/publichealth/clinical/oralhealth/workforce.html. Accessed July 10, 2013.
- 16.Bailit H, D’Adamo J. State case studies: improving access to dental care for the underserved. J Public Health Dent. 2012;72(3):221–234. doi: 10.1111/j.1752-7325.2012.00346.x. [DOI] [PubMed] [Google Scholar]
- 17.Blumberg SJ, Foster EB, Frasier AM et al. Design and operation of the National Survey of Children’s Health, 2007. Vital Health Stat 1. 2012;(55):1–149. [PubMed] [Google Scholar]
- 18.Guarnizo-Herreño CC, Wehby GL. Explaining racial/ethnic disparities in children’s dental health: a decomposition analysis. Am J Public Health. 2012;102(5):859–866. doi: 10.2105/AJPH.2011.300548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guarnizo-Herreño CC, Wehby GL. Children’s dental health, school performance, and psychosocial well-being. J Pediatr. 2012;161(6):1153–1159. doi: 10.1016/j.jpeds.2012.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iida H, Rozier RG. Mother-perceived social capital and children’s oral health and use of dental care in the United States. Am J Public Health. 2013;103(3):480–487. doi: 10.2105/AJPH.2012.300845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fisher-Owens SA, Isong IA, Soobader MJ et al. An examination of racial/ethnic disparities in children’s oral health in the United States. J Public Health Dent. 2013;73(2):166–174. doi: 10.1111/j.1752-7325.2012.00367.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bell JF, Huebner CE, Reed SC. Oral health need and access to dental services: evidence from the National Survey of Children’s Health, 2007. Matern Child Health J. 2012;16(suppl 1):S27–S34. doi: 10.1007/s10995-012-0992-0. [DOI] [PubMed] [Google Scholar]
- 23. US Department of Health and Human Services. Area Resource File [database]. Washington, DC; 2007.
- 24.Dorri M, Sheiham A, Watt RG. Modelling the factors influencing general and oral hygiene behaviours in adolescents. Int J Paediatr Dent. 2010;20(4):261–269. doi: 10.1111/j.1365-263X.2010.01048.x. [DOI] [PubMed] [Google Scholar]
- 25.Bramlett MD, Soobader M-J, Fisher-Owens SA et al. Assessing a multilevel model of young children’s oral health with national survey data. Community Dent Oral Epidemiol. 2010;38(4):287–298. doi: 10.1111/j.1600-0528.2010.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chi DL, Momany ET, Jones MP et al. Relationship between medical well baby visits and first dental examinations for young children in Medicaid. Am J Public Health. 2013;103(2):347–354. doi: 10.2105/AJPH.2012.300899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harris R, Nicoll AD, Adair PM, Pine CM. Risk factors for dental caries in young children: a systematic review of the literature. Community Dent Health. 2004;21(suppl 1):71–85. [PubMed] [Google Scholar]
- 28.Liu J, Probst JC, Martin AB, Wang JY, Salinas CF. Disparities in dental insurance coverage and dental care among US children: the National Survey of Children’s Health. Pediatrics. 2007;119(suppl 1):S12–S21. doi: 10.1542/peds.2006-2089D. [DOI] [PubMed] [Google Scholar]
- 29.Lewis CW, Johnston BD, Linsenmeyar KA, Williams A, Mouradian W. Preventive dental care for children in the United States: a national perspective. Pediatrics. 2007;119(3):e544–e553. doi: 10.1542/peds.2006-1958. [DOI] [PubMed] [Google Scholar]
- 30.Skillman SM, Doescher MP, Mouradian WE, Brunson DK. The challenge to delivering oral health services in rural America. J Public Health Dent. 2010;70(suppl 1):S49–S57. doi: 10.1111/j.1752-7325.2010.00178.x. [DOI] [PubMed] [Google Scholar]