Abstract
We systematically reviewed 12 epidemiological studies to determine whether an association exists between diet quality and patterns and mental health in children and adolescents; 9 explored the relationship using diet as the exposure, and 3 used mental health as the exposure.
We found evidence of a significant, cross-sectional relationship between unhealthy dietary patterns and poorer mental health in children and adolescents. We observed a consistent trend for the relationship between good-quality diet and better mental health and some evidence for the reverse. When including only the 7 studies deemed to be of high methodological quality, all but 1 of these trends remained.
Findings highlight the potential importance of the relationship between dietary patterns or quality and mental health early in the life span.
The role of habitual diet in the development of depressive disorders and symptoms has become a recent research focus over the past decade. Data from adult populations have indicated that better-quality diet is associated with better mental health outcomes.1–5 In fact, new meta-analyses have confirmed the inverse association between healthy diets and depression.4,5 A habitually poor diet (e.g., increased consumption of Western processed foods) is also independently associated with a greater likelihood of or risk for depression1,6,7 and anxiety.1 Although stress and depression can promote unhealthy eating, recent longitudinal studies have suggested that reverse causality is a less likely explanation for long-term associations.8
However, our understanding of these associations earlier in the life span remains unclear. To date, much of the research around this relationship has focused on dietary intake and externalizing behaviors (particularly hyperactivity). For example, poor nutritional quality is independently associated with symptoms of attention-deficit hyperactivity disorder.9 However, the relationship between dietary intake in childhood and adolescence and internalizing behaviors, which represent depressive symptoms, low mood, or anxiety, has received comparably less attention. Given that the previous literature in adults regarding diet and mental health has focused on the common mental disorders, depression and anxiety, examination of these same mental health parameters in children and adolescents is needed. In terms of what evidence is available to date, findings remain inconsistent. For example, although some studies have observed a dose–response relationship between diet quality and mental health in young adolescents,10 others have shown no significant association.11 The evidence is even less comprehensive for the relationship between dietary intake and anxiety symptoms.12
To our knowledge, no systematic reviews to date have specifically investigated the association between diet, measured using diet quality scores, dietary pattern analysis, or both and internalizing behaviors that characterize low or depressive mood and anxiety symptoms in child and adolescent populations.
METHODS
Studies considered for inclusion in this review (1) were full-text articles; (2) consisted of epidemiological cohort, case-control, and cross-sectional study designs; (3) examined associations between diet quality or patterns and internalizing disorders that encompassed depression, low mood, depressive symptoms, emotional problems, and anxiety (as distinct from externalizing disorders), assessed via self- or informant report, medical records, or the application of diagnostic measurement tools in children or adolescents who were aged 19 years or younger on enrolment (as per the United Nations13 definition); and (4) used nonclinical study samples that were population based rather than from acute or institutional settings. We included studies defining dietary patterns using either a priori or a posteriori approaches, as well as studies using proxy measures of diet quality (e.g., studies that derived a diet quality score from food frequency data).
In the absence of a standard definition of diet quality or diet patterns, we defined them as the quality of overall habitual dietary intake or the pattern of overall habitual dietary intake, as previously reported.1,14,15 Although varying in composition according to the country of origin, healthy or prudent dietary patterns are characterized by a higher intake of nutrient-dense foods, including vegetables, salads, fruits, fish, and other foods groups known to be healthful. Conversely, unhealthy patterns are characterized by a higher intake of foods with increased saturated fat, refined carbohydrates, and processed food products. We excluded studies that
1. examined individual nutrients or supplements,
2. examined the effects of preservatives on mental health,
3. examined emotional or binge eating,
4. examined dietary restraint or restriction (i.e., the restriction of calories or food consumption for the purpose of weight loss),
5. used trait-based (assessing personality) or measures of stress (as distinct from internalizing behaviors),
6. presented only univariate analyses, and
7. were published in languages other than English.
We also excluded studies that used samples in which the age range overlapped between adolescence and adulthood and studies that presented mental health data only as a composite measure (e.g., overall behavior scores as distinct from internalizing behavior scores) or as a comorbidity only. Furthermore, given that the purpose of this review was to assess whether a relationship exists between diet quality or dietary patterns and mental health (rather than examining dietary intervention effects), we also excluded studies with a randomized controlled trial design.
Search Strategy and Data Extraction
We performed the search strategy using medical, health, psychiatric, and social sciences databases (PubMed, OVID, MEDLINE, CINAHL, PsycINFO) to identify relevant literature published through August 30, 2012. We used the following search terms: (depression OR depressive disorder OR anxiety disorders OR affective symptoms OR anxi* OR mood OR internali* OR psychological symptoms OR psychological distress) AND (diet OR food habits OR dietary OR dietary patterns OR dietary quality OR western diet OR Mediterranean diet) AND (youth OR adolescen* OR child OR infant).
We also searched reference lists of relevant reviews and studies. One author (S. H.) performed the electronic search strategy, and then another author (A. O.) replicated the search. The abstracts or full-text articles of those studies deemed potentially relevant were obtained. We (A. O. and S. H.) conferred to finalize the articles to be included in the review according to the predetermined inclusion and exclusion criteria; where consensus was not reached, the senior author (F. N. J.) was consulted.
Assessment of Methodological Quality and Best-Evidence Synthesis
The heterogeneity between study definitions of dietary and internalizing symptomatology variables precluded formal meta-analysis. As such, we determined a priori that included studies would be analyzed by assessing their methodological quality and performing a best-evidence synthesis of those studies meeting quality standards.
To assess the methodological quality of the reviewed studies, we used a scoring system based on that of Lievense et al.,16 which has been used in musculoskeletal and obesity research and recently in another review article examining the relationship between dietary variables and depression in adults.15,17,18 We (S. E. Q. and S. H.) independently scored 14 items relating to the methodological quality of studies in the following areas: study population, assessment of risk factors, assessment of outcomes, study design, and data analysis (see the box on this page). If they endorsed an item, a positive score of 1 was applied; if they did not endorse the item, a score of 0 was applied. In cases in which information was missing or was insufficiently documented, the item was coded as unclear (?), and a score of 0 was subsequently applied. We calculated the total score (percentage) for each of the studies, and those subsequently deemed high quality were those with a score exceeding the mean of all the total scores. The mean score was 83.7% (range = 62.5%–100%). The scoring system is preferential to cohort studies, and this is reflected by cohort studies being eligible for a greater number of criteria (e.g., related to prospective study designs, participation and attrition rates) than case-control and cross-sectional study designs. In the case that we (S. E. Q. and S. H.) did not agree on the ratings, a co-author experienced in best evidence synthesis (S. L. B.) provided the final judgment in 1 consensus meeting.
Criteria list for the assessment of study quality (modified from Lievense et al.17)
| Study population |
| 1. Selection at uniform point C/CC/CS |
| 2. Cases and controls drawn from the same population CC |
| 3. Participation rate > 80% for cases/cohort C/CC |
| 4. Participation rate > 80% for controls CC |
| Assessment of risk factor |
| 5. Exposure assessment blinded C/CC/CS |
| 6. Exposure measured identically for cases and controls CC |
| 7. Exposure assessed according to validated measures C/CC/CS |
| Assessment of outcome |
| 8. Outcome assessed identically in studied population C/CC/CS |
| 9. Outcome reproducibly C/CC/CS |
| 10. Outcome assessed according to validated measures C/CC/CS |
| Study design |
| 11. Prospective design used C/CC |
| 12. Follow-up time > 12 months C |
| 13. Withdrawals < 20% C |
| Analysis and data presentation |
| 14. Appropriate analysis techniques used C/CC/CS |
| 15. Adjusted for at least age, and gender C/CC/CS |
Note. C = applicable to cohort studies; CC = applicable to case-control studies; CS = applicable to cross-sectional studies. Studies were scored as positive (1), negative (0), or unclear (?), and 100% represented the maximum possible score.
Our best-evidence synthesis included those studies that met high-quality standards as we have defined them. We performed the synthesis by ranking the findings across all studies into 5 levels of evidence, ranging from strong evidence, moderate evidence, limited evidence, and conflicting evidence to no evidence (Table 1). The synthesis took into account the type of study design used (i.e., strong evidence was defined by generally consistent findings in multiple high-quality cohort studies). This systematic review adhered to the guidelines outlined in the 2009 Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.19
TABLE 1—
Criteria for Ascertainment of Evidence Level for Best-Evidence Synthesis
| Level of Evidence | Criteria for Inclusion in Best Evidence Synthesis |
| Strong evidence | Generally consistent findings in multiple high-quality cohort studies |
| Moderate evidence | Generally consistent findings in 1 high-quality cohort study and > 2 high-quality case-control studies |
| Limited evidence | Generally consistent findings in single cohort study, 1 or 2 case-control studies, or multiple cross-sectional studies |
| Conflicting evidence | Inconsistent findings in < 75% of the studies |
| No evidence | No studies found |
Note. Adapted from Lievense et al.20
RESULTS
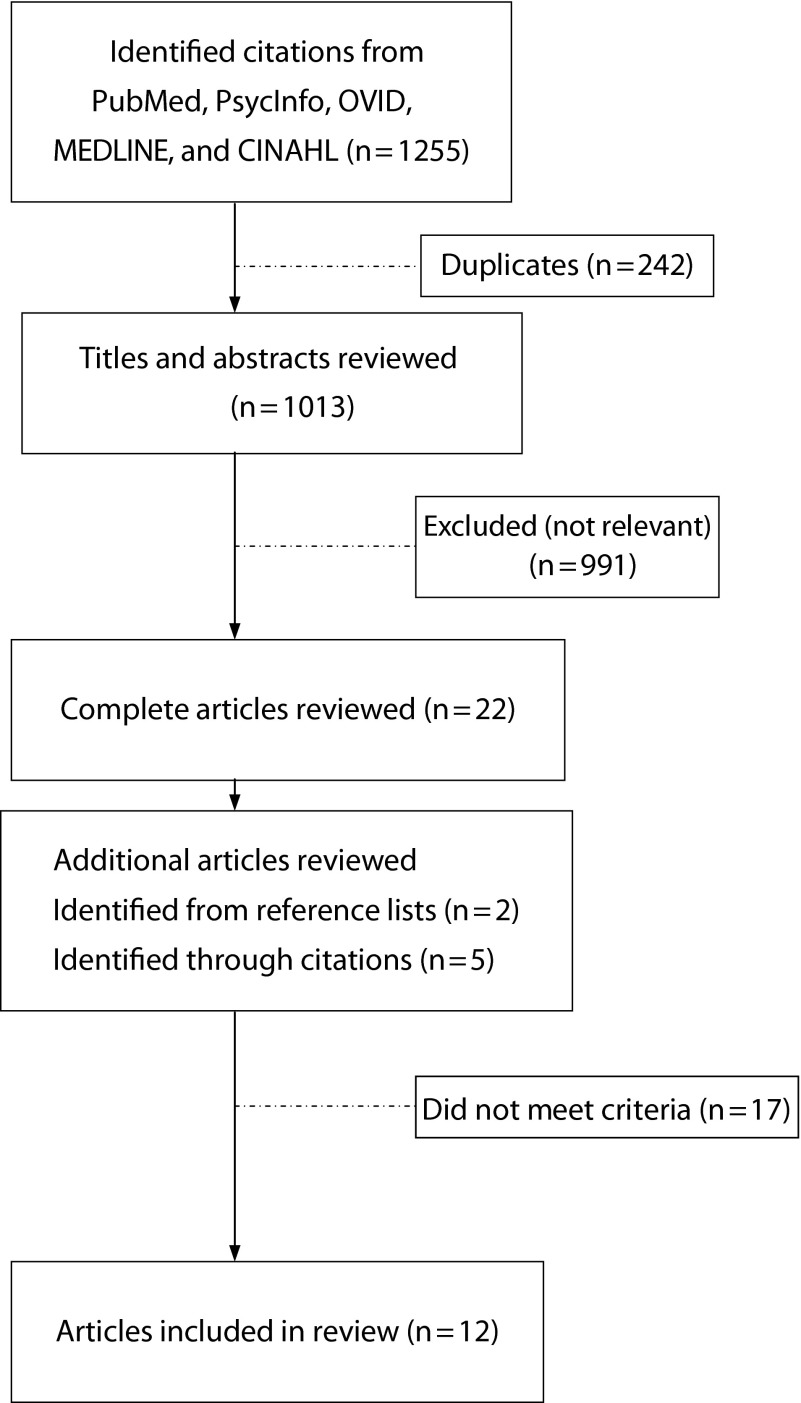
Applying the initial search strategy identified 1255 citations; we subsequently excluded 242 because of duplication, leaving 1013 potentially relevant studies. Of those, we excluded 991 on the basis of information available from the abstract and title. We obtained the full texts of the remaining 22 articles to assess eligibility. Additionally, we manually examined reference lists and citations for further relevant studies, revealing 7 new full-text articles (n = 29). On examination of the full-text articles, 14 studies did not fulfill inclusion criteria and were subsequently excluded. We (A. O. and S. H.) achieved a high level of consensus (89%); decisions surrounding the remaining articles were reached in consultation with the senior author (F. N. J). As a result, a further 3 articles were excluded (investigated stress or neuroticism or parental restrictions on foods), thus leaving 12 articles for inclusion in this review. Figure 1 displays a summary of the results of the systematic search.
FIGURE 1—
Flowchart summary of search results.
The most common reasons for exclusion were (1) “diet” defined as skipping meals, caloric control, or binge eating; (2) results taken from participants enrolled in an intervention study, community- or school-based program, or both; (3) study explored the role of stress or well-being as opposed to psychological outcomes; or (4) study investigated the impact of parental practices or attitudes related to provision of food.
Population and Design
We extracted the following key information from those articles eligible for inclusion: author, country, sample, diet measure, mental health measure, statistical presentation of results (including exposure variable), covariates, and key findings. Key characteristics of included articles are displayed in Table 2. Briefly, studies were from Australia,10,22–24,27 the United States,21,26 the United Kingdom,20 Germany,25 China,12 Canada,11 and Norway.28
TABLE 2—
Characteristics of 12 Included Studies, Grouped by Study Design, Author, and Exposure of Interest
| Author and Country | No. Participants, Sex (%), and Follow-Up Period (If Applicable) | Age at Recruitment, Years, Mean (SD) or Range | Dietary Measure | Mental Health Measure | Questionnaire Respondent |
| Cohort, prospective studies | |||||
| Wiles et al.,20 United Kingdom | 4541,a 2.5 y | 4.5b | FFQ; principal components analysis to identify junk food dietary pattern | Emotional Symptoms subscale of SDQ | Mother |
| Jacka et al.,10 Australia | 3040, 56% male, 2 y | 11–18 | Dietary questionnaire used to construct “healthy diet” score based on National Healthy Eating Guidelines, “unhealthy diet” score constructed by summing consumption of unhealthy foods | Emotional Functioning subscale of the PedsQL | Adolescent |
| McMartin et al.,11 Canada | 3757, 48% male, 3 y | 10–11 | Harvard Youth/Adolescent FFQ, overall DQI-I score (0–100), variety component score of the DQI-I | Health records of physician-diagnosed internalizing disorders (ICD-9) | Child |
| Cross-sectional studies | |||||
| Brooks et al.,21 United States | 2224, 52% male | 16.2b | Dichotomized question: “Do you eat a healthy diet?” | Frequency of feeling depressed or distressed in the past 30 d, dichotomized cutoff score ≥ 10 | Adolescents |
| Oddy et al.,22 Australia | 1324, 51.2% male | 14.1 (0.2) | CSIRO FFQ, healthy and Western dietary patterns based on factor analysis | Internalizing subscale of CBCL | Parent |
| Jacka et al.,23 Australia | 7114, 47.2% male | 11.6 (0.81) | Dietary questionnaire adapted from Amherst Health and Activity Study Adult Survey of Child Health; diet quality score divided into quintiles for unhealthy and healthy diets | SMFQ; dichotomized cutpoint score of ≥ 8 defined as symptomatic | |
| Jacka et al.,10 Australia | 3040, 56% male | 11–18 | Dietary questionnaire, healthy diet and unhealthy diet scores constructed on the basis of National Healthy Eating Guidelines | Emotional functioning subscale of the PedsQL | Adolescent |
| Robinson et al.,24 Australia | 1598,a 51.3% male | ∼14b | CSIRO FFQ; food groups: cereals and grains, fruit, dairy products, meat and meat alternatives, vegetables, and extras based on Australian dietary recommendations | Internalizing subscale of CBCL | Parent |
| Weng et al.,12 China | 5003, 52.09% male | 13.21 (0.99) | FFQ, 38 items, principal component analysis produced snack, animal, and traditional dietary patterns, divided into quintiles | DSRS (Chinese version), cutoff score of 15 defined as screening positive for depressive symptoms; SCARED (Chinese version), cutoff score of > 23 defined as screening positive for an anxiety disorder | Adolescent |
| Kohlboeck et al.,25 Germany | 3361, 62.8% male | 11.15 (0.5) | FFQ, 82 items, constructed diet quality score based on the concept of the German OMD for children and adolescents, food categories defined according to the Codex General Standard for Food Additives food category system | Emotional Symptoms subscale of SDQ | Parent |
| Fulkerson et al.,26 United States | 4734,b 50.2% male | Boys: 14.9bGirls: 14.7b | YAQ, FFQ, 149 items | Constructed 6-item scale of the following symptoms: feeling tired; having trouble sleeping; feeling unhappy, sad, depressed, hopeless, nervous or tense, worrying too much about things, stratified depressive symptom groups (low, moderate, high) | Adolescent |
| Renzaho et al.,27 Australia | 3370, 51.8% male | 4–12 | Questionnaire about fruit and vegetable consumption according to Australian Guide to Healthy eating | Emotional Symptoms subscale of SDQ | Parent or caregiver |
| Vollrath et al.,28 Norway | 42 451 | ∼1.5b | Dietary questionnaire, questionnaire consisting of 4 items based on consumption of cakes, waffles, or sweet cookies; desserts or ice cream; chocolate; and other sweets, jellybeans, or confectionary; summary score dichotomized at 85th percentile | Internalizing subscale of CBCL, 14 items; EAS, 11 items; mean score derived from 25 items of combined scales | Mother |
Note. CBCL = Child Behavior Checklist; CSIRO = Commonwealth Scientific and Industrial Research Organization; DQI-I = Diet Quality Index—International; DSRS = Depression Self-Rating Scale for Children; EAS = Emotionality Activity and Sociability Questionnaire; FFQ = Food Frequency Questionnaire; ICD-9 = International Classification of Diseases, 9th Revision; OMD = optimized mixed diet; PedsQL = Pediatric Quality of Life Inventory; SCARED = Screen for Child Anxiety Related Emotional Disorders; SDQ = Strengths and Difficulties Questionnaire; SMFQ = Short Mood and Feelings Questionnaire; YAQ = Youth and Adolescent Food Frequency Questionnaire.
Number of participants for which data are available on both mental health measure and dietary measure,
Data not provided.
Collectively, studies included 82 779 participants (Oddy et al.22 [n = 1324] and Robinson et al.24 [n = 1860] used the same data set). Data were derived predominantly from cross-sectional studies and 3 prospective cohort studies. For the latter, follow-up assessment periods ranged from 2 to 4 years. Age of participants ranged from 4.5 to 18 years in all studies (Table 2).
Measures of Mental Health
Table 2 displays the instruments used to measure outcome and exposure variables. We present studies in which mental health was treated as the exposure variable separately from studies exploring diet as the exposure. The most commonly used instruments to measure mental health were subscales of the Child Behavior Checklist22,24,28 and the Strengths and Difficulties Questionnaire.20,25,27 Other instruments included the Short Mood and Feelings Questionnaire (n = 1)23; the Depression Self-rating Scale for Children (n = 1)12; physician diagnosis using health records (applying the International Classification of Diseases, Ninth Revision; n = 1)11; a 6-item checklist (n = 1) consisting of symptoms of depression including feeling tired, having trouble sleeping, feeling unhappy, sad, depressed, hopeless, nervous or tense, and worrying too much about things26; the Pediatric Quality of Life Inventory (n = 1)10; and a questionnaire about frequency of feeling depressed (n = 1).21
Measures of Diet Quality and Patterns
Dietary intake was most commonly measured using variations of a Food Frequency Questionnaire (FFQ),12,20,25 including the Harvard Youth/Adolescent Questionnaire (n = 2)11,26 and the Commonwealth Scientific and Industrial Research Organization FFQ (n = 2).22,24 Other measures included a 14-item questionnaire based on the Amherst Health and Activity Study Adult Survey of Child Health Habits (n = 1),23 the German optimized mixed diet concept for children and adolescents (n = 1),25 the Australian Guide to Healthy Eating by Questionnaire (n = 2),1,27 4 questions about frequency of sweet consumption (n = 1),28 a self-report questionnaire about nutrition (n = 1),10 and the question “Do you eat a healthy diet?” (n = 1).21
Key Findings Including Data From All Studies
Key results of the 12 studies reviewed are provided in Table 3; cross-sectional and prospective analyses performed within a study are presented separately. Of the 12 studies, 9 explored the relationship between diet quality and mental health using diet as the exposure variable1,10–13, 20–25; of these 9 studies with diet as the exposure, 5 explored the relationship between dietary patterns and mental health and 3 explored the relationship between diet quality and mental health; 1 explored both diet quality, dietary patterns and mental health.25 Of those examining dietary patterns as the exposure, the majority of studies (n = 4) consistently demonstrated significant relationships between unhealthy dietary patterns and poorer mental health. Evidence of an association between healthy dietary patterns and better mental health was less consistent, with significant positive associations observed in only half of the 6 studies. Of the 5 studies exploring the association between diet quality, measured using diet quality scores, and mental health, all demonstrated a significant relationship between higher diet quality (i.e., higher intakes of healthy, nutrient-dense foods) and better mental health (Brooks et al.21 for females only). Of the 3 studies that looked specifically at the association between lower diet quality (i.e., higher intake of unhealthy foods) and poorer mental health outcomes, 2 also reported significant relationships.
TABLE 3—
Key Results of Included Articles, Including Summary, Covariates, and Methodological Quality Score
| Results |
||||
| Author | Key Results | Summary | Covariates | Quality Score, % |
| Cohort, Prospective Studies | ||||
| Wiles et al.20 | OR = 1.01 (CI = 0.94, 1.09) | No association between junk food dietary pattern at age 4.5 and emotional problems at age 7 (dietary pattern) | Sex, SDQ total difficulties or subscale score at age 4.5 y, maternal smoking, maternal age at birth of child, number of siblings, socioeconomic markers, birth weight and gestational age, maternal depression and anxiety, maternal enjoyment score, and single-parent household | 75 |
| Jacka et al.10 | C2: b = 0.11* (CI = 0.01, 0.21) | Dose–response prospective association between higher baseline healthy diet quality scores and higher PedsQL scores at 2-y follow-up (dietary quality) | Age, sex, area-level SES, dieting behaviors, BMI, physical activity, baseline PedsQL scores | 75 |
| C3: b = 0.14* (CI = 0.02,0.27) | No prospective association between higher unhealthy diet quality scores and lower PedsQL (dietary quality) after controlling for baseline mental health | |||
| C2: b = 0.05 (CI = −0.04,0.27) | ||||
| C3: b = −0.07 (CI = −0.18, 0.03) | ||||
| McMartin et al.11 | IRR = 1.09 (CI = 0.73, 1.63) | No association between “overall” DQI-I diet quality scores and rates of internalizing disorders (dietary quality) | Sex, energy intake, household income, parental marital status and education, body weight status, physical activity level, geographic area | 91.7 |
| IRR = 0.45* (CI = 0.25–0.82) | Greater “variety” component DQI-I diet quality scores associated with lower rates of internalizing disorders over 3-y follow-up period (dietary quality) | |||
| Cross-Sectional Studies | ||||
| Brooks et al.21 | Males: OR = 1.07 (CI = 0.98,1.18); | No association between a healthy diet and feeling depressed or stressed for males | Age, race | 62.5 |
| Females: OR = 0.89* (CI = 0.83,0.96) | Eating a healthy diet was associated with reduced odds of feeling depressed or stressed for females | |||
| Oddy et al.22 | b = 1.25* (CI = 0.15, 2.35) | A Western dietary pattern was associated with higher CBCL internalizing scores (dietary pattern) | Sex, total energy intake, BMI category, physical activity, screen use, family structure, family income, family functioning at age 14 and maternal education at pregnancy | 100 |
| b = 0.17 (CI = −0.54, 0.88) | No association between healthy dietary pattern and CBCL internalizing scores (dietary pattern) | |||
| Jacka et al.23 | Age, sex, physical activity, parental work and educational status, household level, SES, dieting behaviors, family conflict and poor family management, BMI, smoking, and physical activity | 75 | ||
| Unhealthy diet | Q2: OR = 1.03 (CI = 0.87, 1.22) | Dose–response association between higher unhealthy diet scores and higher odds of being depressed (SMFQ score; dietary quality) | ||
| Q3: OR = 1.22 (CI = 1.03, 1.44) | ||||
| Q4: OR = 1.29 (CI = 1.12, 1.50) | ||||
| Q5: OR = 1.79 (CI = 1.52, 2.11) | ||||
| Healthy diet | Q2: OR = 0.61 (CI = 0.45, 0.84) | Dose–response association between higher scores on healthy diet scores and lower odds of being depressed (SMFQ score; dietary quality) | ||
| Q3: OR = 0.58 (CI = 0.43, 0.79) | ||||
| Q4: OR = 0.47 (CI = 0.35, 0.64) | ||||
| Q5: OR = 0.55 (CI = 0.40, 0.77) | ||||
| Jacka et al.10 | Age, sex, area level, SES, dieting behaviors, BMI, and physical activity | 75 | ||
| Healthy diet score (least healthy) | C2: b = 0.31* (CI = 0.22, 0.39) | Dose–response associations between higher healthy diet quality scores and higher PedsQL scores (dietary quality) | ||
| C3: b = 0.42* (0.31, 0.53) | ||||
| Unhealthy diet score | C2: b = −0.14* (CI = −0.23, −0.06) | Dose–response associations between higher unhealthy diet quality scores and lower PedsQL (dietary quality) | ||
| C3: b = −0.29* (CI = −0.38, −0.20) | ||||
| Robinson et al.24 | b = 0.32* (CI = 0.03, 0.60) | “Extras” food group associated with higher internalizing CBCL scores (dietary pattern) | Sex, sociodemographic factors (family income, father not at home, and maternal employment), family functioning, physical activity, screen use, smoking, alcohol, marijuana use, and early sexual activity | 87.5 |
| Vegetable food group | b = 0.14 (CI = −0.41, 0.69) | No association between the vegetable, fruit, dairy, cereal, or meat and meat alternatives food groups and internalizing CBCL scores (dietary pattern) | ||
| Fruit food group | b = 0.09 (CI = −0.39, 0.21) | |||
| Dairy food group | b = 0.11 (CI = −0.36, 0.59) | |||
| Cereal food group | b = −0.09 (CI = −0.57, 0.39) | |||
| Meat and meat alternatives food group | b = 0.01(CI = −0.62, 0.63) | |||
| Weng et al.12 | Age, sex, maternal education, paternal education, family income, BMI, physical activity | 87.5 | ||
| Snack dietary pattern and pure depression, pure anxiety, and coexisting depression and anxiety | Pure depression: | Highest tertile of snack dietary pattern associated with higher odds of pure depression, anxiety, and coexisting depression and anxiety (dietary pattern) | ||
| T2: OR = 0.98 (CI = 0.77, 1.25) | ||||
| T3: OR = 1.64* (CI = 1.30, 2.06) | ||||
| Pure anxiety: | ||||
| T2: OR = 1.38* (CI = 1.08, 1.65) | ||||
| T3: OR = 1.87* (CI = 1.51, 2.31) | ||||
| Coexisting depression and anxiety: | ||||
| T2: OR = 1.27 (CI = 1.00, 2.43) | ||||
| T3: OR = 1.93* (CI = 1.54, 2.43) | ||||
| Animal dietary pattern and pure depression, pure anxiety, and coexisting depression and anxiety | Pure depression: | Highest tertile of animal dietary pattern associated with higher odds of pure anxiety and coexisting depression and anxiety, but not pure depression (dietary pattern) | ||
| T2: OR = 1.08 (CI = 0.86, 1.37) | ||||
| T3: OR = 1.21 (CI = 0.95, 1.53) | ||||
| Pure anxiety: | ||||
| T2: OR = 1.34* (CI = 1.08, 1.65) | ||||
| T3: OR = 1.87* (CI = 1.51, 2.32) | ||||
| Coexisting depression and anxiety: | ||||
| T2: OR = 1.10 (CI = 0.88, 1.39) | ||||
| T3: OR = 1.71* (CI = 1.37, 2.15) | ||||
| Traditional dietary pattern and pure depression, pure anxiety, and coexisting depression and anxiety | Pure depression: | Highest tertile of traditional dietary pattern associated with reduced odds of pure depression and coexisting depression and anxiety, but not pure anxiety (dietary pattern) | ||
| T2: OR = 0.61* (CI = 0.49, 0.79) | ||||
| T3: OR = 0.38* (CI = 0.30, 0.49) | ||||
| Pure anxiety: | ||||
| T2: OR = 0.98 (CI = 0.79, 1.23) | ||||
| T3: OR = 0.85 (CI = 0.69, 1.04) | ||||
| Coexisting depression and anxiety: | ||||
| T2: OR = 0.74* (CI = 0.60, 0.92) | ||||
| T3: OR = 1.50* (CI = 0.39, 0.63) | ||||
| Kohlboeck et al.25 | OR = 0.89* (CI = 0.80, 0.98) | Higher diet quality score associated with lower emotional SDQ scores (dietary quality) | Sex, study center, total energy intake, parental background (education, income, single-parent family), BMI, physical activity, TV viewing or video game use | 87.5 |
| OR = 1.19* (CI = 1.08,1.32) | Increased confectionary food group associated with higher emotional SDQ scores (dietary pattern) | |||
| No association between dairy, fats and oils, fruits and vegetables, confectionary, cereals, bakery wares, meat products, egg products, or ready-to-eat savories and emotional SDQ scores (dietary pattern) | ||||
| Fulkerson et al.26 | ||||
| Daily vegetable intake | Males: 1.8 (low), 1.9, (moderate), and 1.9 (high) | No association between depressive symptoms and daily servings of vegetables or fruits for either sex (dietary pattern) | Race, grade level; all analyses stratified by sex | 100 |
| Females: 2.0 (low), 1.9 (moderate), and 2.3 (high) | ||||
| Daily fruit intake | Males: 2.3 (low), 2.2 (moderate), and 2.3 (high) | |||
| Females: 2.5 (low), 2.3 (moderate), and 2.3 (high) | ||||
| Renzaho et al.27 | Household income, family structure, child age and sex, parental educational level, language spoken at home, financial stress, food security, and social support | 87.5 | ||
| Fruit consumption | Males: b = −0.054* (CI = −0.095, −0.012) | Emotional SDQ scores associated with lower fruit consumption for males and females (dietary pattern) | ||
| Females: b = −0.064* (CI = −0.112, −0.015) | ||||
| Vegetable consumption | Males: b = −0.014 (CI = −0.054, 0.025) | Emotional SDQ scores associated with lower vegetable consumption for females but not males (dietary pattern) | ||
| Females: b = −0.050* (CI = −0.088, −0.012) | ||||
| Vollrath et al.28 | OR = 1.47* (CI = 1.32, 1.65) | Internalizing scores associated with higher consumption of sweet foods (dietary pattern) | Maternal characteristics (negative affectivity, completed education in years, duration of breastfeeding), child sex, temperament, and weight for length at 1 y | 75 |
Note. BMI = body mass index; C = category; CBCL = Child Behavior Checklist; CI = confidence interval; IRR = incident rate ratio; OR = odds ratio; PedsQL = Pediatric Quality of Life Inventory; Q = quartile; SES = socioeconomic status; SDQ = Strengths and Difficulties Questionnaire; SMFQ = Short Mood and Feelings Questionnaire; T = tertile.
*Significant results.
A paucity of available prospective studies (n = 3) investigated the association between dietary patterns or quality and mental health1,10,11,20; where evidence was available, findings were conflicting (Table 3).
When the relationship between mental health and diet quality was explored using mental health as the exposure variable, data were also limited. However, 2 of 3 of these studies (66%) demonstrated that children and adolescents with worse mental health reported significantly poorer dietary patterns.27,28 No data were available on the relationship between mental health as an exposure and its relationship to measures of healthy dietary habits.
Best-Evidence Synthesis
When we applied criteria for the best-evidence synthesis, the mean score was 83.7% (range = 62.5%–100%, where 100% is the maximum obtainable score). Methodological quality ratings of each study are displayed in Table 3. The 7 studies exceeding the mean were subsequently included in a best-evidence synthesis. When we applied the criteria for ascertainment of evidence level for best-evidence synthesis, we deemed the level of evidence for all of these associations as limited.
DISCUSSION
Our aim was to review and synthesize the existing literature to determine whether an association exists between diet quality and mental health in childhood or adolescence, with a focus on internalizing disorders including depression, low mood, and anxiety. We observed consistent cross-sectional associations between unhealthy dietary patterns and worse mental health in childhood or adolescence. In contrast, we found inconsistent trends for the relationships between healthy diet patterns or quality and better mental health. We also found inconsistent trends for unhealthy diet quality and worse mental health. Overall, best-evidence criteria confirmed that this area had a limited level of evidence, largely attributable to a dearth of prospective and case-control data, which thereby precludes us from inferring causal associations about these relationships.
These findings add to the existing literature that has attempted to elucidate the relationship between diet quality and mental health in adult populations.6,7,15,29 To our knowledge, this is the first review of its kind in this area to focus specifically on children and adolescents. Although this review generated insufficient evidence to elucidate the directionality of the relationship, several potential explanations exist for the relationship between diet and mental health in this population.
It may be the case that children and adolescents with internalizing disorders or symptoms eat more poorly as a form of self-medication. However, it is equally as conceivable that the influence of early eating habits and nutritional intake has an important impact on affect. Indeed, there are numerous potential biological pathways by which diet quality may have an impact on mental health in children and adolescents. First, a poor quality diet that is lacking nutrient-dense foods may lead to nutrient deficiencies that have been associated with mental health issues. For example, the dietary intake of folate, zinc, and magnesium is inversely associated with depressive disorders,30 whereas dietary long-chain omega-3 fatty acids are inversely related to anxiety disorders.31
Dietary intake may also have a direct impact on various biological systems and mechanisms that underpin depression, including oxidative processes, the functioning of the immune system, and levels of salient brain proteins. For example, in patients with depression, markers of systemic inflammation are often significantly greater than in controls, which is indicative of immune system dysregulation.32 Studies have indicated that markers of inflammation are positively correlated with components of a poor diet, and a healthy diet is associated with reduced inflammation.33 The available evidence also suggests that high-fat, high-sugar diets can affect proteins that are important in brain development, such as the signaling molecule brain-derived neurotrophic factor.34 Brain-derived neurotrophic factor is often reduced in patients with depression,35 and when its synthesis is increased, symptoms of depression can improve.36 It is important to note that consistent evidence has shown that higher quality diets (i.e., those higher in nutrient-dense foods) and diets high in saturated fats and refined carbohydrates are each independently related to depression, suggesting the possibility of different operant pathways. The correlation between healthy and unhealthy dietary patterns is also weak (e.g., Jacka et al.37). However, we acknowledge that these interpretations remain speculative in view of the limited evidence for causality currently available.
Limitations
The studies acquired through the systematic search have various methodological strengths and weaknesses that might have influenced the outcomes reported. A strength of this review was the inclusion of a range of studies conducted across several countries and settings. However, the way in which diet was measured varied greatly between the studies. Many used FFQs, a common validated tool, to assess dietary quality. The FFQs were completed by the child or adolescent in some cases26 and by the primary caregiver in others.28 The Youth and Adolescent Food Frequency Questionnaire, a validated measure, was also used,26 and some studies did not use a validated tool.21 A number of these articles were secondary analyses from larger health studies (e.g., Robinson et al.24). In such studies, statistical techniques were used to score the available data to create diet-quality scores. Techniques of this kind are deemed an appropriate method to rank individuals in terms of their diet quality when available data are limited.10,23 Owing to the length and complexity of FFQs, they are not always used in health studies.
Aside from the quality of the tools used to assess diet, other issues surrounding reporting may have influenced the results obtained for habitual food intake in the reviewed articles. Studies rely on accurate reporting; however, reporting biases can occur for many reasons, including recall ability and social desirability biases,38 in which respondents are more likely to report healthier food intake as a result of knowledge about healthy eating guidelines. Reporting biases may differ between children and adults, making the comparison of results additionally challenging because FFQs were completed by the adults, or children, or both. Moreover, differential reporting might also occur in those with depressive symptoms in comparison with those without. Moreover, we acknowledge the potential influence of the file-drawer effect, in which positive studies are overrepresented in the literature because studies containing null findings remain unpublished.39
Finally, it is important to note that although many studies have taken into account many of the common confounding variables, other studies have not. For example, socioeconomic status is considered an important potential confounder that must be considered because it is associated with both diet40 and mental health.41 Several studies in this review did not take socioeconomic status into account; results from such studies should be viewed with caution because the relationships observed may possibly be explained by socioeconomic status or other related variables rather than by diet or mental health alone. Similarly, several studies did not account for physical activity. Unavoidable residual confounding may also explain the associations observed. For example, certain complex variables, such as socioeconomic status, are difficult to measure and are therefore likely to result in residual confounding. This type of confounding cannot be ruled out as an explanatory factor in the associations observed in the studies reviewed.
To our knowledge, this is the first review of its kind to explore the association between diet quality and patterns and mental health in children and adolescents. Findings from the cross-sectional studies included in this review highlight the potential importance of the relationship between dietary patterns or quality and the mental health of young people; however, we acknowledge that further studies that contribute to a stronger level of evidence are required. We recommend that the relationships between both poor diet and poorer mental health and good diet and better mental health be examined using longitudinal study designs. Moreover, the need for studies explicating specific biological mechanisms of action, as well as data from well-designed randomized controlled trials to support or refute direct biologically causal relationships, is clear.42
Conclusions
Despite a paucity of data, our findings highlight the potential importance of the relationship between dietary patterns or quality and mental health early in the life span. Prospective and intervention studies are now required to improve the level of evidence. Given that the average age of onset for anxiety and mood disorders is 6 years and 13 years, respectively,43 the potential for early intervention using strategies targeted at improving dietary intake at a population level may be of substantial public health benefit. However, this would require policy action to improve the global food environment.44
Acknowledgments
A. O’Neil, S. L. Brennan, and F. N. Jacka are recipients of National Health and Medical Research Council (NHMRC) Fellowships (1052865, 1012472, and 628912). L. J. Williams is the recipient of an NHMRC Career Development Award and was supported by an Alfred Deakin Postdoctoral Fellowship while undertaking this work. M. Berk is supported by an NHMRC Senior Principal Research Fellowship (1059660).
A. O’Neil, M. Berk, and F. N. Jacka have received project funding from Meat and Livestock Australia. M. Berk has received grant and research support from the National Institutes of Health, Cooperative Research Centre, Simons Autism Foundation, Cancer Council of Victoria, Stanley Medical Research Foundation, Medical Benefits Fund, NHMRC, Beyond Blue, Rotary Health, Geelong Medical Research Foundation, Bristol Myers Squibb, Eli Lilly, Glaxo SmithKline, Organon, Novartis, Mayne Pharma, and Servier; has been a speaker for Astra Zeneca, Bristol Myers Squibb, Eli Lilly, Glaxo SmithKline, Janssen Cilag, Lundbeck, Merck, Pfizer, Sanofi Synthelabo, Servier, Solvay, and Wyeth; and served as a consultant to Astra Zeneca, Bristol Myers Squibb, Eli Lilly, Glaxo SmithKline, Janssen Cilag, Lundbeck Merck, and Servier. F. N. Jacka has received grant and research support from the Brain and Behaviour Research Institute, NHMRC, Australian Rotary Health, Geelong Medical Research Foundation, Ian Potter Foundation, Eli Lilly, and The University of Melbourne and has been a paid speaker for Sanofi-Synthelabo, Janssen Cilag, Servier, Pfizer, Health Ed, Network Nutrition, and Eli Lilly. L. J. Williams has received grant and research support from Eli Lilly, Pfizer, The University of Melbourne, Deakin University, and NHMRC.
Human Participant Protection
Institutional review board approval was not needed because data were obtained from secondary sources.
References
- 1.Jacka FN, Pasco JA, Mykletun A et al. Association of Western and traditional diets with depression and anxiety in women. Am J Psychiatry. 2010;167(3):305–311. doi: 10.1176/appi.ajp.2009.09060881. [DOI] [PubMed] [Google Scholar]
- 2.Akbaraly TN, Brunner EJ, Ferrie JE, Marmot MG, Kivimaki M, Singh-Manoux A. Dietary pattern and depressive symptoms in middle age. Br J Psychiatry. 2009;195(5):408–413. doi: 10.1192/bjp.bp.108.058925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sánchez-Villegas A, Delgado-Rodríguez M, Alonso A et al. Association of the Mediterranean dietary pattern with the incidence of depression: The Seguimiento Universidad de Navarra/University of Navarra follow-up (sun) cohort. Arch Gen Psychiatry. 2009;66(10):1090–1098. doi: 10.1001/archgenpsychiatry.2009.129. [DOI] [PubMed] [Google Scholar]
- 4.Lai JS, Hiles S, Bisquera A, Hure AJ, McEvoy M, Attia J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am J Clin Nutr. 2014;99(1):181–197. doi: 10.3945/ajcn.113.069880. [DOI] [PubMed] [Google Scholar]
- 5.Psaltopoulou T, Sergentanis TN, Panagiotakos DB, Sergentanis IN, Kosti R, Scarmeas N. Mediterranean diet, stroke, cognitive impairment, and depression: a meta-analysis. Ann Neurol. 2013;74(4):580–591. doi: 10.1002/ana.23944. [DOI] [PubMed] [Google Scholar]
- 6.Sánchez-Villegas A, Verberne L, De Irala J et al. Dietary fat intake and the risk of depression: the SUN Project. PLoS One. 2011;6(1) doi: 10.1371/journal.pone.0016268. e16268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sánchez-Villegas A, Toledo E, De Irala J et al. Fast-food and commercial baked goods consumption and the risk of depression. Public Health Nutr. 2012;15(3):424–432. doi: 10.1017/S1368980011001856. [DOI] [PubMed] [Google Scholar]
- 8.Le Port A, Gueguen A, Kesse-Guyot E et al. Association between dietary patterns and depressive symptoms over time: a 10-year follow-up study of the GAZEL cohort. PLoS One. 2012;7(12) doi: 10.1371/journal.pone.0051593. e51593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Egmond-Fröhlich AW, Weghuber D, de Zwaan M. Association of symptoms of attention-deficit/hyperactivity disorder with physical activity, media time, and food intake in children and adolescents. PLoS ONE. 2012;7(11) doi: 10.1371/journal.pone.0049781. e49781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jacka FN, Kremer PJ, Berk M et al. A prospective study of diet quality and mental health in adolescents. PLoS One. 2011;6(9) doi: 10.1371/journal.pone.0024805. e24805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McMartin S, Kuhle S, Kirk S, Veugelers P, Colman I. The association between diet quality and internalizing disorders in children. Am J Epidemiol. 2011;173:S289–S289. [Google Scholar]
- 12.Weng TT, Hao JH, Qian QW et al. Is there any relationship between dietary patterns and depression and anxiety in Chinese adolescents? Public Health Nutr. 2012;15(4):673–682. doi: 10.1017/S1368980011003077. [DOI] [PubMed] [Google Scholar]
- 13.UNICEF. The State of the World’s Children 2011. New York, NY: UNICEF USA; 2011. [Google Scholar]
- 14.Chatzi L, Melaki V, Sarri K et al. Dietary patterns during pregnancy and the risk of postpartum depression: the mother-child “Rhea” cohort in Crete, Greece. Public Health Nutr. 2011;14(9):1663–1670. doi: 10.1017/S1368980010003629. [DOI] [PubMed] [Google Scholar]
- 15.Quirk SE, Williams LJ, O’Neil A et al. The association between diet quality, dietary patterns and depression in adults. BMC Psychiatry. 2013;13:175. doi: 10.1186/1471-244X-13-175. doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lievense A, Bierma-Zeinstra S, Verhagen A, Verhaar J, Koes B. Influence of work on the development of osteoarthritis of the hip: a systematic review. J Rheumatol. 2001;28(11):2520–2528. [PubMed] [Google Scholar]
- 17.Lievense AM, Bierma-Zeinstra SM, Vergahen AP, van Baar ME, Verhaar JAN, Koes BW. Influence of obesity on the development of osteoarthritis of the hip: a systematic review. Rheumatology (Oxford) 2002;41(10):1155–1162. doi: 10.1093/rheumatology/41.10.1155. [DOI] [PubMed] [Google Scholar]
- 18.Brennan SL, Pasco JA, Urquhart DM, Oldenburg B, Wang Y, Wluka AE. Association between socioeconomic status and bone mineral density in adults: a systematic review. Osteoporos Int. 2011;22(2):517–527. doi: 10.1007/s00198-010-1261-y. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wiles NJ, Northstone K, Emmett P, Lewis G. Junk food diet and childhood behavioural problems: results from the ALSPAC cohort. Eur J Clin Nutr. 2009;63(4):491–498. doi: 10.1038/sj.ejcn.1602967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brooks TL, Harris SK, Thrall JS, Woods ER. Association of adolescent risk behaviors with mental health symptoms in high school students. J Adolesc Health. 2002;31(3):240–246. doi: 10.1016/s1054-139x(02)00385-3. [DOI] [PubMed] [Google Scholar]
- 22.Oddy WH, Robinson M, Ambrosini GL et al. The association between dietary patterns and mental health in early adolescence. Prev Med. 2009;49(1):39–44. doi: 10.1016/j.ypmed.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 23.Jacka FN, Kremer PJ, Leslie ER et al. Associations between diet quality and depressed mood in adolescents: results from the Australian Healthy Neighbourhoods Study. Aust N Z J Psychiatry. 2010;44(5):435–442. doi: 10.3109/00048670903571598. [DOI] [PubMed] [Google Scholar]
- 24.Robinson M, Kendall GE, Jacoby P et al. Lifestyle and demographic correlates of poor mental health in early adolescence. J Paediatr Child Health. 2011;47(1-2):54–61. doi: 10.1111/j.1440-1754.2010.01891.x. [DOI] [PubMed] [Google Scholar]
- 25.Kohlboeck G, Sausenthaler S, Standl M et al. Food intake, diet quality and behavioral problems in children: results from the GINI-plus/LISA-plus studies. Ann Nutr Metab. 2012;60(4):247–256. doi: 10.1159/000337552. [DOI] [PubMed] [Google Scholar]
- 26.Fulkerson JA, Sherwood NE, Perry CL, Neumark-Sztainer D, Story M. Depressive symptoms and adolescent eating and health behaviors: a multifaceted view in a population-based sample. Prev Med. 2004;38(6):865–875. doi: 10.1016/j.ypmed.2003.12.028. [DOI] [PubMed] [Google Scholar]
- 27.Renzaho AMN, Kumanyika S, Tucker KL. Family functioning, parental psychological distress, child behavioural problems, socio-economic disadvantage and fruit and vegetable consumption among 4-12 year-old Victorians, Australia. Health Promot Int. 2011;26(3):263–275. doi: 10.1093/heapro/daq054. [DOI] [PubMed] [Google Scholar]
- 28.Vollrath ME, Tonstad S, Rothbart MK, Hampson SE. Infant temperament is associated with potentially obesogenic diet at 18 months. Int J Pediatr Obes. 2011;6(2-2):e408–e414. doi: 10.3109/17477166.2010.518240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sanhueza C, Ryan L, Foxcroft DR. Diet and the risk of unipolar depression in adults: systematic review of cohort studies. J Hum Nutr Diet. 2013;26(1):56–70. doi: 10.1111/j.1365-277X.2012.01283.x. [DOI] [PubMed] [Google Scholar]
- 30.Jacka FN, Maes M, Pasco JA, Williams LJ, Berk M. Nutrient intakes and the common mental disorders in women. J Affect Disord. 2012;141(1):79–85. doi: 10.1016/j.jad.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 31.Jacka FN, Pasco JA, Williams LJ, Meyer BJ, Digger R, Berk M. Dietary intake of fish and PUFA, and clinical depressive and anxiety disorders in women. Br J Nutr. 2013;109(11):2059–2066. doi: 10.1017/S0007114512004102. [DOI] [PubMed] [Google Scholar]
- 32.Irwin MR, Miller AH. Depressive disorders and immunity: 20 years of progress and discovery. Brain Behav Immun. 2007;21(4):374–383. doi: 10.1016/j.bbi.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 33.Esposito K, Marfella R, Ciotola M et al. Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA. 2004;292(12):1440–1446. doi: 10.1001/jama.292.12.1440. [DOI] [PubMed] [Google Scholar]
- 34.Molteni R, Barnard R, Ying Z, Roberts C, Gomez-Pinilla F. A high-fat, refined sugar diet reduces hippocampal brain-derived neurotrophic factor, neuronal plasticity, and learning. Neuroscience. 2002;112(4):803–814. doi: 10.1016/s0306-4522(02)00123-9. [DOI] [PubMed] [Google Scholar]
- 35.Bocchio-Chiavetto L, Bagnardi V, Zanardini R et al. Serum and plasma BDNF levels in major depression: a replication study and meta-analyses. World J Biol Psychiatry. 2010;11(6):763–773. doi: 10.3109/15622971003611319. [DOI] [PubMed] [Google Scholar]
- 36.Brunoni AR, Lopes M, Fregni F. A systematic review and meta-analysis of clinical studies on major depression and BDNF levels: implications for the role of neuroplasticity in depression. Int J Neuropsychopharmacol. 2008;11(8):1169–1180. doi: 10.1017/S1461145708009309. [DOI] [PubMed] [Google Scholar]
- 37.Jacka FN, Cherbuin J, Anstey K, Butterworth P. Dietary patterns and depressive symptoms over time: examining the relationships with socioeconomic position, health behaviours and cardiovascular risk. PLoS One. 2014;9(1) doi: 10.1371/journal.pone.0087657. e87657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hebert JR, Clemow L, Pbert L, Ockene IS, Ockene JK. Social desirability bias in dietary self-report may compromise the validity of dietary intake measures. Int J Epidemiol. 1995;24(2):389–398. doi: 10.1093/ije/24.2.389. [DOI] [PubMed] [Google Scholar]
- 39.Song F, Parekh S, Hooper L et al. Dissemination and publication of research findings: an updated review of related biases. Health Technol Assess. 2010;14(8) doi: 10.3310/hta14080. iii, ix–xi, 1–193. [DOI] [PubMed] [Google Scholar]
- 40.Brennan SL, Henry MJ, Nicholson GC, Kotowicz MA, Pasco JA. Socioeconomic status, obesity and lifestyle in men: the Geelong Osteoporosis Study. J Mens Health. 2010;7(1):31–41. [Google Scholar]
- 41.Williams LJ, Brennan SL, Henry MJ et al. Area-based socioeconomic status and mood disorders: cross-sectional evidence from a randomly selected cohort of adult women. Maturitas. 2011;69(2):173–178. doi: 10.1016/j.maturitas.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 42.Jacka FN, Mykletun A, Berk M. Moving towards a population health approach to the primary prevention of common mental disorders. BMC Med. 2012;10(1):149. doi: 10.1186/1741-7015-10-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Merikangas KR, He JP, Burstein M et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jacka FN, Sacks G, Berk M, Allender S. Food policies for physical and mental health. BMC Psychiatry. 2014;14:132. doi: 10.1186/1471-244X-14-132. [DOI] [PMC free article] [PubMed] [Google Scholar]