Abstract
The human and financial costs of disasters are vast. In 2011, disasters were estimated to have cost $378 billion worldwide; disasters have affected 64% of the world’s population since 1992. Consequently, disaster risk reduction strategies have become increasingly prominent on national and international policy agendas. However, the function of health in disaster risk reduction strategies often has been restricted to emergency response.
To mitigate the effect of disasters on social and health development goals (such as risk reduction Millennium Development Goals) and increase resilience among at-risk populations, disaster strategies should assign the health sector a more all-encompassing, proactive role.
We discuss proposed methods and concepts for mainstreaming health in disaster risk reduction and consider barriers faced by the health sector in this field.
Recent decades have witnessed a growing scientific and evidence-based approach to the concept of disaster risk reduction. The United Nations Office for Disaster Risk Reduction (UNISDR) and the World Health Organization (WHO) define the term disaster as
a serious disruption of the functioning of a community or a society causing widespread human, material, economic or environmental losses which exceed the ability of the affected community or society to cope using its own resources.1
The term also describes an event that can be defined spatially and geographically that results from the interaction of an external stressor with a human community and that carries the implicit concept of nonmanageability in a local context.1
Statistics on the effects of recent disasters and their increasing global frequency are startling.2 In the past 12 years, an estimated $1.3 trillion of damage has been sustained through disasters, and in 2012, an estimated 51 million people in 16 countries required some form of humanitarian assistance.3,4 Multibillion dollar natural hazard–related disasters are becoming more common, and five of the 10 costliest disasters have occurred between 2008 and 2012.5 In 2011, disasters were estimated to have cost $378 billion, breaking the previous record of $262 billion in 2005.5 More than 1.5 billion people currently live in countries affected by fragility, conflict, or large-scale violence,6 and overall, more than 4.4 billion people—64% of the world’s population—have been affected by disasters in some way since 1992.7 As the effects of climate change become more palpable, this may be associated with a rise in the frequency of natural hazard–related disasters.8
Consequently, taking action to better mitigate hazards, prepare for disasters, and reduce their effect has assumed an increasingly prominent position on global and national agendas. Since the Buyin-Zara Earthquake in Iran in 1962, the United Nations (UN) and its member states have worked toward the development of a global disaster risk reduction strategy.9 Early milestones included the UN declaration of an International Decade for Natural Disaster Reduction in the 1990s and the launch of the Yokohama Strategy in 1994, designed to “provide guidelines for natural disaster prevention, preparedness and mitigation.”10 The process gained added momentum following the 2003 Bam Earthquake and 2004 Asian Tsunami, with efforts culminating in 2005 with the adoption by 168 countries of a 10-year strategy, the Hyogo Framework for Action. The Hyogo Framework for Action was intended to build the resilience of nations and communities to disasters through cooperation and technical assistance (see the box on the next page). In addition, since 2007, the UNISDR Global Platform has been convened on a biennial basis to review progress on the framework by international agencies, countries, institutions, and civil society actors. The platform also provides a forum to discuss and exchange views on the latest scientific and evidence-based interventions and strategies currently available to achieve those aims.12
Health and the Hyogo Framework for Action (2005–2015): Five Priorities
| 1. Integrating health into disaster risk reduction as a national and local priority |
| • Development and implementation of coordinated multisectoral policies and strategies with sufficient resources |
| 2. Health risk assessment and early warning |
| • Assessment of risk and developing management based on hazard, vulnerability, and capacity analysis in conjunction with surveillance and monitoring of potential health threats |
| 3. Using education and information to build a culture of multilevel health and safety resilience |
| • Strengthen the knowledge, skills, and attitudes of professionals and promote healthy behaviors |
| 4. Reduction of underlying risk factors to health and health systems |
| • Includes addressing poverty, reforming health, and improving vital infrastructure and initiatives to create employment and ensure business continuity |
| 5. Emergency preparedness for effective health response and recovery at all levels |
Source. United Nations.11
HEALTH AND DISASTER RISK REDUCTION
Disasters affect the health of individuals and communities both directly and indirectly. Direct effects include death, injury, disability, and illness; indirect health effects include damage to health infrastructure (including utility services such as water, electricity, and sanitation), health systems, and service delivery. Furthermore, the economic fallout of disasters often results in the erosion of social development and hard-won health and well-being gains, including progress toward achieving Millennium Development Goal targets.13 The health effects of disasters are highly visible, but incorporating and sustaining the particular importance of health in broader disaster risk reduction strategies has remained a key challenge for the WHO, partners in national ministries of health, and the wider health community.9
Traditionally, the role of health in disaster planning has focused mostly on response to emergencies.10 This is important, but multisectoral disaster risk reduction strategies should give priority to improved health outcomes and also assign the health sector a more all-encompassing and proactive role to ensure better resilience to disasters. This will facilitate the building of local and national capacities to prevent and prepare for emergencies, strengthen primary health care at the community level, and reduce the vulnerability of at-risk populations, particularly women, children, and socially marginalized groups.9,14 By its nature, this is a multisectoral process, wherein health is a consideration in all aspects of community and national preparedness.
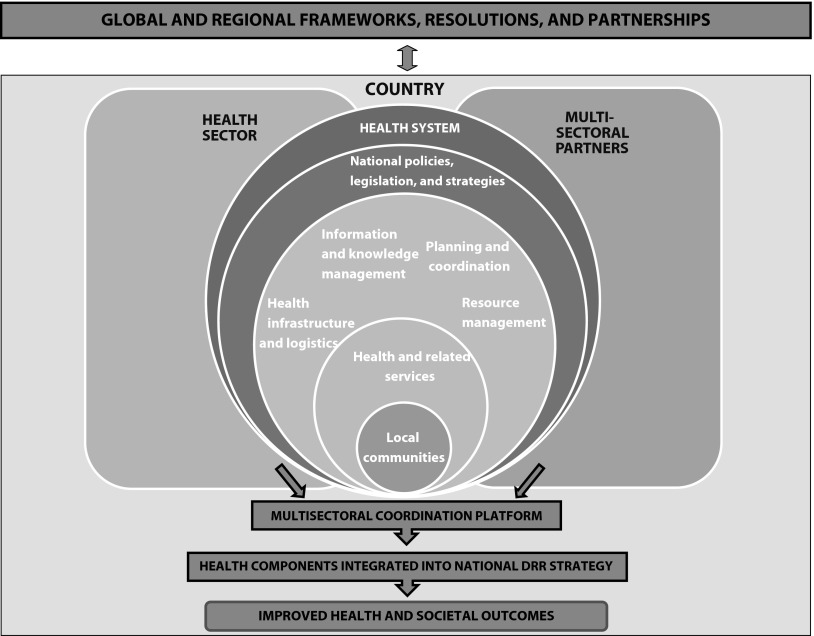
The broader role that health could play in disaster risk reduction has been considered by the UNISDR, the WHO, and a multitude of other stakeholders. This consultative and iterative process continues to evolve and encourage a common understanding. Current concepts about the role that health could potentially play in disaster risk reduction and more specifically in disaster risk management have been well described.9 In November 2012, WHO conducted a consultation to advance the development of a global framework on health emergency risk management and to improve public health preparedness. The framework seeks to communicate and foster a common understanding of the fundamental role of health in disaster risk reduction to both multisectoral partners and those within the health sector itself.15 The overarching elements of the framework discussed at the consultation are outlined in Figure 1. This includes, at its core, building country-level capability, defining the roles and responsibilities of the health sector and stakeholders, and outlining the interaction with international organizations and processes in the national disaster risk reduction strategy.
FIGURE 1—
A possible framework for health emergency and disaster risk management—a concept diagram.
Note. DRR = disaster risk reduction.
At the heart of a resilient national health system is community-based action and primary health care. Primary health care can reduce vulnerability; chronic and preexisting conditions usually make up the largest burden of disease following an emergency.9 Community-based action is critical for the success of protecting health in emergencies because of local knowledge of risks and the capacity for immediate action. Numerous successful community-based schemes exist and have been shown to improve resilience; however, these are often not part of a coordinated national strategy or sustainable.16
A resilient and flexible health infrastructure is also essential for protecting health in disasters; health facilities should be built to withstand hazards and to remain operational. These components must be integrated into health legislation and policy. The framework also addresses the wider determinants of health, through multisectoral partners responsible for water, sanitation, nutrition, communications, logistics, and so forth. Together, these elements should feed into national disaster risk reduction management strategies. Since 2013, this emergency risk management for health framework has been incorporated as a key component into the WHO’s interim guidance on global pandemic influenza preparedness.17
INTEGRATING HEALTH INTO DISASTER RISK REDUCTION
Several national and regional initiatives have made progress toward integrating health into disaster risk reduction strategies. In Haiti, the government and UN Development Programme have coordinated actions following the 2010 earthquake to implement a national disaster risk reduction strategy via a roadmap.18 The UN stated that more than 130 countries have reported on their implementation of the international blueprint for disaster risk reduction (Hyogo Framework for Action 2005–2015), and many have applied lessons learned from Haiti.19 Following cyclones Gonu and Phet in Oman (2007, 2010), efforts have been made to strengthen national emergency risk management for health capacity by developing and implementing a pilot project led by the Ministry of Health, in collaboration with WHO and European Union support. The result has been a more integrated and multisectoral approach through the National Committee for Civil Defense, which is composed of representatives from all government departments. The committee has formed a search and rescue team, made available operational mobile hospitals, and established a coordination and communication team.20,21
Although the benefits of integrating health into disaster risk reduction strategies are widely recognized, several factors frequently prevent the full and sustained integration of health into national disaster risk reduction strategies. These factors include inadequate financing, insufficient knowledge base, complex and varied bureaucratic and governance structures within countries, and a limited interdisciplinary interaction between health and other sectors.9 The scarcity of financial and human resources—especially in low-income countries—has meant that the integration of health has had to compete for funding and visibility with priority areas such as specific vertical health programs and more general disaster risk reduction strategies.
Financing
In 2008, the WHO Global Assessment of National Health Sector Emergency Preparedness and Response found that fewer than half of national health sectors had a specific budget allocation for emergency preparedness and response.22 The Global Facility for Disaster Reduction and Recovery estimated that between 1991 and 2010, only $13.5 billion (0.45%) of the total amount of international aid ($3.03 trillion) was spent worldwide on disaster prevention and preparedness.23 The past 15 years, however, have seen the international community pay increasing attention to developing new financial solutions to help governments cope with a disaster.24
Innovative funding mechanisms, such as creating pooled funds between groups of countries or tools such as catastrophe bonds, have opened up a range of new options, especially for low-income countries. The Horn of Africa Risk Transfer for Adaptation (HARITA) Program is an example of an innovative microfinance scheme being piloted in Ethiopia. HARITA offers a holistic approach to risk management, integrating financial aspects such as risk transfer (i.e., insurance), prudent risk-taking (e.g., credit), and risk reserves (e.g., savings) alongside risk reduction activities (e.g., improved agricultural practices and conservation activities). Moreover, the HARITA Program engages local stakeholders as central participants in the design of the risk reduction package.24
Opening up the potential for optimal financing for health in disaster risk reduction strategies through innovative financing mechanisms and tools such as these should be considered at the outset of the strategic planning process. Early involvement of health economists in the planning stages of disaster risk reduction strategies could be one way to achieve this. At a global level, the relevance and value of WHO in promoting the integration of health into national disaster risk reduction strategies would be enhanced with increased focus on integrating well-laid-out financing strategies into the technical expertise it provides.
Variability
Another significant barrier to the integration of health into disaster risk reduction strategies is the natural variability of disasters and the countries that they affect. Disasters affect a wide range of social, ecological, and physical systems, and in many of the world’s most resource-poor countries, they overwhelm their coping capacities and hinder long-term development as resources are funneled to disaster response and reconstruction efforts (95% of humanitarian finance).25,26 Between 1970 and 1999, 90% of deaths in disasters were climate related, and with the frequency of climate change events increasing, some regions are expected to experience more extreme events, such as unseasonal floods, droughts, storms, and cyclones.25,27 Within countries, natural geographic variations also mean that some areas may be more at risk than others (e.g., coastal regions to floods and cyclones). Apart from the natural and geographic variations between countries and communities, differences in governance and political structures further complicate strategy development.28
Consequently, generalizing effective strategies between countries, communities, and different disaster scenarios can be problematic. A flexible approach is therefore essential, and greater focus must be placed on the integration of health into disaster risk reduction strategies at a local level, including in small, rural municipalities and informal settlements with local governance linked to national efforts. Furthermore, attention should be given to situations in which different sectors such as the agricultural and engineering industries are engaged in working on methods to reduce the effect of disasters; these may not be recognized in health-based disaster risk reduction strategies.28 Examples of effective schemes showing how services can be tailored to meet the environmental needs of local communities include the application of a regional Hospital Safety Index in Latin American countries. With more than half of the 16 000 hospitals in Latin America and the Caribbean located in areas at high risk for disasters, this index—developed with the Pan American Health Organization—helps health facilities assess their safety by predicting the likelihood of a hospital or health facility continuing to function in emergencies on the basis of structural and functional factors. The Pan American Health Organization played a critical role in facilitating collaboration between countries and showed the value of a regional approach, incorporating cross-sectoral local expertise and needs. Recent disasters have galvanized similar activities elsewhere: Pakistan, Nepal, and some Caribbean island states are now committed to building safer, more resilient hospitals as part of a national disaster risk reduction strategy.29,30
Variability in processes relating to accountability and transparency can also pose challenges. Although the international Hyogo Monitor attempts to gauge this element in its progress reports, results are based on government submissions and are therefore subjective. With no objective external evaluation, reports are often overly positive as a result.28 One approach used to address this challenge is to arrange external peer reviews to assess progress toward Hyogo Framework for Action implementation. The United Kingdom was the first to undertake such a peer review. However, the process of external peer review could be expensive and time-consuming.31 Practical solutions to some of these recurring difficulties could include encouraging partnerships between communities and countries with similar circumstances and the development of a central repository of community and country case studies describing methods and outcomes of initiatives that have integrated health into disaster risk reduction strategies. This repository ideally would be open access and use a standardized reporting template. International organizations such as the WHO could play a valuable role in hosting and developing such a resource.
Multisectoral Cooperation
The multisectoral nature of health in disaster risk reduction strategies means that developing new methods of cooperation and coordination between stakeholders remains a continuing concern and constant challenge. In the past, there has been a lack of collaboration at an international level. For example, climate change adaptation and disaster risk reduction communities have had limited interactions, even though it is widely recognized that both parties have key areas of convergence and that improved dialogue could result in more resilient, better integrated strategies for disaster risk reduction.26 In addition, there have been repeated calls for mainstreaming of disaster risk reduction, closer integration of public policy frameworks, greater multiple stakeholder dialogue, partnerships, and collaboration, all of which are current pertinent issues.32–34 Some success has occurred in this regard with countries such as India and Morocco aligning their national disaster risk reduction strategy with Millennium Development Goal targets. In India, the Desert Development Programme and Drought Prone Area Programme are both linked to Millennium Development Goal 7, and in Morocco, the National Action Programme to combat desertification aims to incorporate a strategy to eradicate poverty (Millennium Development Goal 1).35 Meanwhile, the WHO’s 2013 Pandemic Influenza Risk Management: WHO Interim Guidance provides a good example of how health and disaster risk management structures are being more closely joined at a global level and how multisectoral links are being encouraged in security planning. Pandemic risk management is considered as “a whole-of-government responsibility” in which “all ministries should work with the Ministry of Health within the national coordination system to ensure a consistent approach to preparedness.” The guidance also recommends involving civil society and the private business sector in pandemic preparedness planning and national committees.17
Developing a cadre of appropriately trained personnel with sufficient multisectoral working experience is a key component for dealing with concerns around intersectoral collaboration. Intersectoral and interdisciplinary secondments of staff can be used to achieve this as can postgraduate training programs that bridge knowledge streams between disciplines, such as the “One Health” approach to animal, human, and environmental health.36 To be effective, however, these measures have to be complemented with adequately repeated training courses and multisectoral disaster risk reduction exercises. The inevitably intermittent nature of disasters and the often high turnover and part-time role of staff in these sectors are factors that contribute to the risk of a rapid dilution of skills and experience.
CONCLUSIONS
As a global community, our aim is to be as prepared as we possibly can be, given our constraints of knowledge, resources, and competing priorities, for the disasters that will inevitably afflict us. Thus, integrating health into disaster risk reduction is a global health priority and should feature increasingly in high-level policy discussions such as the current debates around the formulation of a successor framework to the Hyogo Framework for Action and the post-2015 Sustainable Development Goals.37 Agreement on a comprehensive process framework for integrating health into disaster risk reduction would help accelerate and sustain the progress already being made. Increasing the visibility and understanding of this concept within the health sector and with other partners in disaster risk reduction is a key first step in that process.
Acknowledgments
We would like to thank Virginia Murray.
References
- 1. World Health Organization. Definitions: emergencies. Available at: http://www.who.int/hac/about/definitions/en. August 2008. Accessed June 25, 2013.
- 2.Maurice J. Mitigating disasters—a promising start. Lancet. 2013;381(9878):1611–1613. doi: 10.1016/s0140-6736(13)61008-9. [DOI] [PubMed] [Google Scholar]
- 3. United Nations Office for Disaster Risk Reduction (UNISDR). The economic and human impact of disasters in the last 12 years. 2012. Available at: http://www.unisdr.org/files/25831_20120318disaster20002011v3.pdf. Accessed April 25, 2014.
- 4.Amos V. Under-secretary-general for humanitarian affairs and emergency relief coordinator [press briefing]. Geneva, Switzerland: United Nations Office for the Coordination of Humanitarian Affairs; 2011. Cited in UNHCR. Integrating sexual and reproductive health into health emergency and disaster risk management. 2012. Available at: http://www.unhcr.org/5077d9349.pdf. Accessed July 31, 2014.
- 5. Counting the cost of calamities. The Economist. January 14, 2012. Available at: http://www.economist.com/node/21542755. Accessed August 1, 2013.
- 6.The World Bank. World Development Report 2011: Conflict, Security, and Development. Washington, DC: The International Bank for Reconstruction and Development/The World Bank; 2011; Available at: http://siteresources.worldbank.org/INTWDRS/Resources/WDR2011_Full_Text.pdf. Accessed April 25, 2014. [Google Scholar]
- 7. United Nations Office for Disaster Risk Reduction (UNISDR). Impacts of disasters since the 1992 Rio de Janeiro Earth Summit. December 14, 2012. Available at: http://www.preventionweb.net/files/27162_infographic.pdf. Accessed June 26, 2013.
- 8. University of Copenhagen. Key messages from the Congress. March 12, 2009. Available at: http://news.ku.dk/all_news/2009/congress_key_messages. Accessed August 9, 2011.
- 9. World Health Organization. Disaster risk management for health: overview. May 2011. Available at: http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1296686244041. Accessed April 25, 2014.
- 10. International Decade for Natural Disaster Reduction (IDNDR). Yokohama Strategy and Plan of Action for a Safer World: Guidelines for Natural Disaster Prevention, Preparedness and Mitigation. World Conference on Natural Disaster Reduction; May 23–27, 1994; Yokohama, Japan. Available at: http://www.preventionweb.net/files/8241_doc6841contenido1.pdf. Accessed December 13, 2013.
- 11.United Nations. Hyogo Framework for Action 2005-2015: Building the Resilience of Nations and Communities to Disasters. 2005. Available at: http://www.refworld.org/docid/42b98a704.html. Accessed June 20, 2013. [Google Scholar]
- 12.United Nations Office for Disaster Risk Reduction (UNISDR) About the global platform for disaster risk reduction. 2013. Available at: http://www.preventionweb.net/globalplatform/2013/about. Accessed June 25, 2013.
- 13.World Health Organization. Integrating sexual and reproductive health into health emergency and disaster risk management. Available at: http://www.who.int/hac/techguidance/preparedness/SRH_policybrief/en. 2012. Accessed April 21, 2014.
- 14.Redwood-Campbell L, Abrahams J. Primary health care and disasters—the current state of the literature: what we know, gaps and next steps. Prehosp Disaster Med. 2011;26(3):184–191. doi: 10.1017/S1049023X11006388. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Consultation on the Health Emergency Risk Management Framework and Improving Public Health Preparedness: Meeting Report, WHO Headquarters, Geneva, Switzerland, 21–23 November 2012. Geneva, Switzerland: World Health Organization; 2013. Available at: http://apps.who.int/iris/bitstream/10665/78359/1/WHO_HSE_HEA_HSP_2013.1_eng.pdf. Accessed December 13, 2013. [Google Scholar]
- 16. International Strategy for Disaster Reduction (ISDR). Building Disaster Resilient Communities: Good Practices and Lessons Learned. 2007. Available at: http://www.unisdr.org/files/596_10307.pdf. Accessed April 20, 2014.
- 17. World Health Organization. Pandemic Influenza Risk Management: WHO Interim Guidance. Geneva, Switzerland: World Health Organization; 2013. Available at: http://www.who.int/influenza/preparedness/pandemic/GIP_PandemicInfluenzaRiskManagementInterimGuidance_Jun2013.pdf. Accessed April 24, 2013.
- 18. United Nations Development Programme. Rebuilding Haiti. 2014. Available at: http://www.undp.org/content/undp/en/home/ourwork/crisispreventionandrecovery/projects_initiatives/crisis_in_haiti. Accessed April 20, 2014.
- 19. United Nations Office for Disaster Risk Reduction (UNISDR). Haitian earthquake boosted global commitment to disaster risk reduction. January 12, 2012. Available at: http://www.unisdr.org/archive/24593. Accessed April 26, 2014.
- 20. Public Health England in collaboration with World Health Organization and the Ministries of Health of New Zealand and Oman. Country experiences in strengthening emergency risk management for health: key factors for success. Report presented at: United Nations Office for Disaster Risk Reduction Fourth Global Platform; 2013; Geneva, Switzerland.
- 21. National Committee for Civil Defence. NCCD accomplishments. Available at: http://www.nccd.gov.om/english/about_project.asp. Accessed April 23, 2014.
- 22.World Health Organization. Global Assessment of National Health Sector Emergency Preparedness and Response. Geneva, Switzerland: World Health Organization; 2008; Available at: http://www.who.int/hac/about/Global_survey_inside.pdf. Accessed February 23, 2014. [Google Scholar]
- 23.Kellett J, Caravani A.Financing Disaster Risk Reduction: A 20 Year Story of International Aid London, UK: Overseas Development Institute and Global Facility for Disaster Reduction and Recovery; September 2013Available at: http://www.odi.org/publications/7452-climate-finance-disaster-risk-reduction. Accessed July 31, 2014 [Google Scholar]
- 24.The World Bank. Innovation in Disaster Risk Financing for Developing Countries: Public and Private Contributions. March 2011. Available at: http://www.gfdrr.org/sites/gfdrr.org/files/DRFI_WRC_Paper_FINAL_April11.pdf. Accessed January 22, 2014. [Google Scholar]
- 25.IPCC (Intergovernmental Panel on Climate Change) Climate Change 2001: IPCC Third Assessment Report. Working Group II Impacts, Adaptation and Vulnerability. Cambridge, UK: Cambridge University Press; 2001. [Google Scholar]
- 26.Thomalla F, Downing T, Spanger-Siegfried E, Han G, Rockstrom J. Reducing hazard vulnerability: towards a common approach between disaster risk reduction and climate adaptation. Disasters. 2006;30(1):39–48. doi: 10.1111/j.1467-9523.2006.00305.x. [DOI] [PubMed] [Google Scholar]
- 27.Kellett J, Sweeney H. Analysis of Financing Mechanisms and Funding Streams to Enhance Emergency Preparedness. Development Initiatives; 2011. Cited in Harris K. Background Note: Finance for Emergency Preparedness: Links to Resilience. London, UK: Overseas Development Institute; January 2013. Available at: http://www.preventionweb.net/files/globalplatform/entry_bg_paper∼8214.pdf. Accessed June 26, 2013.
- 28.Mitchell T, Wilkinson E. Disaster risk management in post-2015 policy frameworks: forging a more resilient future. Briefing Paper; Issue 75. June 2012. Available at: http://www.odi.org/publications/6663-disaster-risk-management-sustainable-development-policy-post2015. Accessed April 2, 2014.
- 29. Pan American Health Organization. Emergency Preparedness and Disaster Relief: What is the hospital safety index? Available at: http://www.paho.org/disasters/index.php?option=com_content&view=category&layout=blog&id=907&Itemid=884. Accessed October 23, 2013.
- 30.United Nations Office for Disaster Risk Reduction (UNISDR) 2008-2009 World Disaster Reduction Campaign: Hospitals Safe From Disasters; Reduce Risk, Protect Health Facilities, Save Lives. Available at: http://www.unisdr.org/2009/campaign/pdf/wdrc-2008-2009-information-kit.pdf. Accessed October 23, 2013. [Google Scholar]
- 31.United Nations Office for Disaster Risk Reduction (UNISDR), European Commission (EC), OECD. 2013 United Kingdom Peer Review – Building Resilience to Disasters: Implementation of the Hyogo Framework for Action (2005-2015) 2013. Available at: http://www.unisdr.org/files/32996_32996hfaukpeerreview20131.pdf. Accessed July 31, 2014. [Google Scholar]
- 32.United Nations Office for Disaster Risk Reduction (UNISDR) Geneva, Switzerland: May 21–23, 2013. Chair’s summary presented at: Fourth Session of the Global Platform for Disaster Risk Reduction. [Google Scholar]
- 33.Oxley MC. A “people-centred principles-based” post-Hyogo framework to strengthen the resilience of nations and communities. Int J Disaster Risk Reduction. 2013;4:1–9. [Google Scholar]
- 34. Intergovernmental Panel on Climate Change (IPCC). Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaption: A Special Report of Working Groups I and II of the IPCC. Field CB, Barros V, Stocker TF, et al. eds. Cambridge, UK, and New York, NY: Cambridge University Press; 2012.
- 35.United Nations Office for Disaster Risk Reduction (UNISDR) Summary of country practices and examples. 2005. Available at: http://www.unisdr.org/2005/mdgs-drr/summary-countries.htm. Accessed April 24, 2014.
- 36. The One Health Initiative. Available at: http://www.onehealthinitiative.com/about.php. Accessed April 22, 2014.
- 37. Sustainable Development 2015: advocacy toolkit: influencing the post-2015 development agenda. Available at: http://www.sustainabledevelopment2015.org/index.php/about/timeline. Accessed November 1, 2013.