Abstract
Childhood externalizing disorders have been linked to adult affective disorders, although some studies fail to substantiate this finding. Multiple longitudinal cohort studies identifying childhood psychopathology and their association with adult psychiatric illness have been published. To examine the association between childhood externalizing symptoms or disorders and the development of adult depression across cohorts, a meta-analysis was performed. Potential studies were identified using a PubMed search through November 2013. All published, prospective, longitudinal, community-sampled cohort studies of children (≤ 13 years) with externalizing symptoms or disorders (aggression, conduct problems, oppositional defiant disorder, conduct disorder), reassessed in adulthood (≥ 18 years) for depressive disorders (major depressive disorder, depressive disorder NOS, or dysthymic disorder) were included. A random effects model was used to summarize the pooled effect sizes. Ancillary analyses considered covariates that could account for variance among studies. Ten studies representing eight cohorts of children initially assessed at age 13 or younger (N = 17,712) were included in the meta-analysis. Childhood externalizing behavior was associated with adult depressive disorders (OR = 1.52, 95% confidence interval = 1.27–1.80, p < 0.0001). Utilizing Orwin’s Fail-safe N approach, 263 studies with a mean odds ratio of 1.0 would have to be added to the analysis before the cumulative effect would become trivial. Externalizing psychopathology in childhood is associated with the development of unipolar depressive disorders in adulthood.
Keywords: depression, externalizing disorders, conduct, meta-analysis, childhood predictors
Nationwide, major depressive disorder (MDD) affects an estimated 6.6% of the population annually and 16% of the population over their lifetimes (Kessler et al., 2003). Given the frequency and severity of this major mental illness, there is significant interest in identifying predictors of depression that could guide preventive interventions. Controversy surrounds the question of whether childhood externalizing psychopathology [e.g., oppositional defiant disorder (ODD), conduct disorder (CD), externalizing behavior, aggressive behavior] predicts adult unipolar depression. Compared to conduct problems with later onset, childhood-onset conduct problems are associated with (a) higher levels of aggressive and antisocial behavior; (b) a more persistent course; (c) more cognitive, verbal, and neuropsychological deficits; (d) higher levels of comorbid conditions; and (e) greater impairment in occupational and interpersonal functioning across developmental periods (Biederman et al., 2008; Colman et al., 2009; Connor, Ford, Albert, & Doerfler, 2007; Frick & Viding, 2009; Moffitt, 1993; Moffitt & Caspi, 2001; Moffitt, Caspi, Harrington, & Milne, 2002). Thus, children with conduct problems represent a more severely affected group with a trajectory that may differ from youth whose conduct problems emerge during adolescence.
A number of longitudinal cohort studies have tested whether developmental continuity between childhood and adult diagnoses exists and whether that link is homotypic (e.g., childhood depression leads to adult depression) and/or heterotypic (e.g., childhood disruptive behavior disorders lead to adult depression). Most of these studies have focused on the trajectory from adolescence to adulthood and fewer have followed children into adulthood. Studying associations between childhood behavior and adult psychiatric disorders allows for the possibility of early identification of treatment targets and implementation of prevention strategies.
Given the controversies surrounding the predictive validity of childhood externalizing psychopathology on adult depression (see below), a meta-analysis utilizing the available large-scale, epidemiologic, longitudinal studies is needed. To our knowledge, this is the first meta-analysis examining childhood externalizing predictors of adult depression. Furthermore, our approach allowed a determination of the extent to which childhood externalizing symptoms and disorders predict the development of adult depression across samples, while taking the non-independence of studies into account. In ancillary analyses, we also considered study variables that may account for heterogeneity in effect sizes across studies.
As noted above, the literature is mixed on the question of whether there is an association between childhood externalizing psychopathology and adult depression. For example, a cohort of 1420 children from the Great Smoky Mountains Study was examined to determine if ODD and CD in childhood were associated with the development of psychopathology in early adulthood (Rowe, Costello, Angold, Copeland, & Maughan, 2010). ODD, but not CD, was associated with mood disorders in early adulthood. In a further refinement of aspects of externalizing behavior that may specifically predict depression, Stringaris and Goodman (2009) utilized data from the British Child and Adolescent Mental Health Survey, including 7912 children and adolescents aged 8–19 years who were followed for 3 years to determine if different dimensions of ODD (i.e., irritable, headstrong, hurtful) predicted psychopathology (Stringaris & Goodman, 2009). The only predictor of emotional disorders, including depression, was the irritable dimension of ODD.
In contrast, other epidemiological studies have found that children with externalizing disorders and/or behaviors are not at increased risk for developing depression as adults. For example, in the Zuid-Holland longitudinal study (N = 1580), externalizing disorders in childhood were associated with anxiety disorders but not depression in adulthood (Roza, Hofstra, van der Ende, & Verhulst, 2003). In the same cohort, Althoff et al. found that moderate aggression with attention problems in childhood was associated with the emergence of anxiety but not mood disorders in adulthood (Althoff, Verhulst, Rettew, Hudziak, & van der Ende, 2010). Similarly, among nine-year-old children from a cohort in the Northeast US (N = 354), the authors did not find an increased risk for any adult psychopathology among those with childhood externalizing disorders (Reinherz, Paradis, Giaconia, Stashwick, & Fitzmaurice, 2003). Thus, longitudinal studies addressing the trajectory from childhood externalizing behaviors to adult depression have disparate findings.
The main objective of this meta-analysis was to determine whether childhood externalizing symptoms and disorders are associated with an increased risk of developing unipolar depressive disorders in adulthood. Our primary hypothesis was that an association with adult depression would be present among children exhibiting externalizing symptoms or disorders. Although meta-analyses consider the pooled effect size across studies, there is often heterogeneity across included studies in terms of samples and design. Thus, in ancillary analyses, we considered whether differences across study methodologies might contribute to the heterogeneity of effect sizes among the studies.
Method
Search Strategies
Potential studies were identified through an initial PubMed search performed in August 2010 and an updated search in November 2013 utilizing the subject headings “cohort studies” and “mental disorders.” The search was limited to human studies published in English. To avoid omitting relevant articles, no further limitations were placed on the search. All articles obtained from the search were then manually assessed for inclusion or exclusion, based on the presence of search terms, described below, by two study investigators. In addition, the reference list of each relevant article was reviewed.
Inclusion and Exclusion Criteria
For the purposes of this meta-analysis, childhood externalizing psychopathology is defined as diagnoses of ODD or CD, or dimensional ratings consistent with disruptive behaviors, specifically externalizing, aggression, hostile behavior, or conduct problems. Although attention-deficit/hyperactivity disorder (ADHD) often co-occurs with ODD and CD, the identified cohort studies did not explicitly identify or control for ADHD among child participants. Thus, this meta-analysis, like the primary source publications, does not distinguish between adult depression attributable to childhood ADHD symptoms versus other externalizing psychopathology. For the outcome, adult depression was defined as MDD, depressive disorder not otherwise specified, or dysthymic disorder. Studies that combined adult anxiety and depressive disorders, or that considered the broader construct of “internalizing” disorders, were excluded. Adult diagnoses of bipolar disorder (Type I, II, or NOS) were not examined, as they are outside of the scope of this meta-analysis.
Prospective, longitudinal cohort studies were included if they were published in peer-reviewed journals, assessed community- or epidemiologically-sampled participants aged 13 years or younger for disruptive behavior disorders or symptoms, and reassessed these participants for current depressive symptoms or disorders at 18 years of age or older. Age 13 was selected to delineate childhood because several studies included a multiple cohort design and data were combined at the initial childhood wave such that age ranges often extended to age 13 (e.g., age 10–13; see Table 1). Given the need to include as many studies as possible and the developmental similarity of 13- to 10-year-olds, studies that included youth up to age 13 were included. However, given that childhood onset conduct problems are often defined as occurring prior to age 10 (e.g., DSM criteria), we conducted an ancillary analysis in which we considered only data points derived from youth age 10 or younger. Similarly, most studies combined 18-year-olds into groups with individuals in their twenties; thus, we selected 18 to delineate adulthood. Articles including only clinically referred samples or cohorts of families were excluded. Only studies identifying children with mental illness utilizing standardized, well-established, reliable, and valid diagnostic instruments, behavior checklists, or rating scales were included, although no studies were found to have utilized non-standard assessments; therefore, none were excluded for this reason. In all studies, initial pediatric assessments, which comprised the predictors for later psychopathology, primarily consisted of behavior checklists, whereas adult follow-up visits focused on diagnosing specific disorders. Specifically, diagnoses in adulthood were made according to a validated semi-structured/structured interview with a qualified interviewer, with the exception of one study that utilized self-report on a validated questionnaire (Huesmann, Dubow, & Boxer, 2009). Studies that did not evaluate childhood externalizing symptoms or disorders, or where diagnoses were applied retrospectively, were excluded.
Table 1.
Characteristics of studies included in the meta-analysis.
| Study (Cohort) | N | Sex | Base-line Age | Follow- Up Age | Baseline Assessment | (Number) and Description of Baseline Variables | Follow-up Assessment |
|---|---|---|---|---|---|---|---|
| Clark et. al, 2007 (National Child Development Study; NCDS) | 9,377 | M/F | 7y and 11y | 23y, 33y, 42y | Teacher rated Bristol Social Adjustment Guide | (2) Teacher-reported externalizing problems at 7y and 11y | Self-report based on the previous week on the Malaise Inventory, Revised Clinical Interview Schedule using ICD-10 criteria |
| Copeland et al., 2009 (Great Smoky Mountains) | 1,420 | M/F | 9–12y | 19–21y | Parent report on the Child Behavior Checklist, parent and youth report on Child and Adolescent Psychiatric Assessment | (2) ODD and CD based on combined parent and youth report | Self-report based on the previous three months on the Young Adult Psychiatric Assessment using DSM-IV criteria |
| Rowe et al., 2010 (Great Smoky Mountains) | 1,420 | M/F | 9y, 11y, 13y | 19y, 21y | Parent report on the Child Behavior Checklist, parent and youth report on Child and Adolescent Psychiatric Assessment | (3) ODD, CD, and ODD+CD based on combined parent and youth report | Self-report based on the previous three months on the Young Adult Psychiatric Assessment using DSM-IV criteria |
| Sourander et al., 2005 (Finnish Boy to a Man) | 2,712 | M | 8y | 18–23y | Teacher report on Rutter B2 scale, Parent report on Rutter A2 scale, Self-report on the Child Depression Inventory and Psychosomatic Scale | (2) Parent-reported conduct problems, teacher- reported conduct problems | Self-report of current psychiatric illness at military health exams/interviews in 1999, 2002, or 2004 using ICD-10 criteria |
| Sourander et al., 2007 (Finnish Boy to a Man) | 2,556 | M | 8y | 18–23y | Teacher report on Rutter B2 scale, Parent report on Rutter A2 scale, Self-report on the Child Depression Inventory and Psychosomatic Scale | (1) Conduct problems based on combined parent and teacher reports | Self-report of current psychiatric illness at military health exams/interviews in 1999, 2002, or 2004 using ICD-10 criteria |
| Reinherz et al., 1999 (Community in Northeast US) | 375 | M/F | 6–9y | 18y, 21y, 26y | Teacher rated Preschool Behavior Questionnaire | (1) Teacher-reported hostile behavior | Self-report of symptoms occurring between 18 and 26 years on the Diagnostic Interview Schedule, v III-R, using DSM-III-R criteria |
| Mason et al., 2004 (Seattle Social Development Project) | 765 | M/F | 10–11y | 21y | Parent, Teacher and self- report on the Child Behavior Checklist | (5) Child self-reported conduct problems, parent- reported oppositional symptoms and conduct problems, teacher-reported oppositional symptoms and conduct problems | Self-report based on the previous 12 months on a modified version of the Diagnostic Interview Schedule using DSM-III criteria |
| Althoff et al., 2010 (Zuid-Holland Longitudinal Study) | 1,576 | M/F | 4–16y (Mean age 9.9 y ± 3.7 y) | 24.5 ± 3.8 y/o | Parent report on the Child Behavior Checklist | (2) Parent-reported aggressive behavior and externalizing symptoms | Self-report based on the previous 12 months on the Composite International Diagnostic Interview using DSM-IV criteria and three sections of the Diagnostic Interview Schedule |
| Huesmann et al., 2009 (Columbia County Longitudinal Study) | 523 | M/F | 8y | 19y, 30y, 48y | Classroom based peer nominations of aggressive behavior | (2) Peer nominated childhood limited aggression and life-course persistent aggression | Self-report based on the previous week on the Brief Symptom Inventory |
| Fergusson et al., 2013 (Christchurch Health and Development Study) | 964 | M/F | 6–10y | 18–30y | Parent and Teacher report on the Rutter Behavior Questionnaire | (1) Conduct problems based on combined parent and teacher reports | Self-report of current symptoms on the Composite International Diagnostic Interview using DSM-IV criteria |
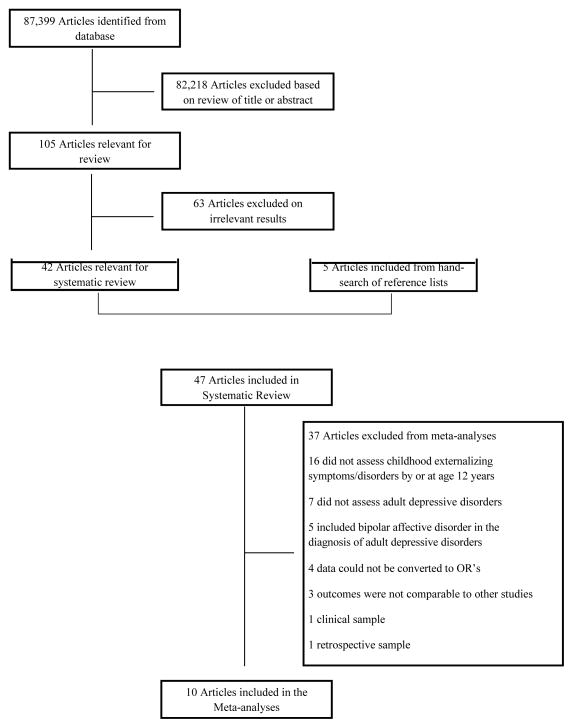
Selection of Studies for the Meta-Analysis
The search returned 87,399 articles, for which the title and/or abstract were reviewed for relevance. Following this review, 105 articles remained, which were assessed for relevant outcomes. Sixty-three articles were excluded because depression outcomes were not reported. The reference sections of the remaining 42 studies were assessed for other potentially relevant articles, which yielded 5 additional studies to include in the systematic review. Of the remaining 47 references, 37 were excluded based on exclusion criteria (Figure 1). This resulted in 10 studies appropriate for inclusion (Althoff, et al., 2010; Clark, Rodgers, Caldwell, Power, & Stansfeld, 2007; Copeland, Shanahan, Costello, & Angold, 2009; Fergusson, Boden, & Horwood, 2013; Huesmann, et al., 2009; Mason et al., 2004; Reinherz, Giaconia, Hauf, Wasserman, & Silverman, 1999; Rowe, et al., 2010; Sourander & Helstela, 2005; Sourander et al., 2007), presented in Table 1.
Figure 1.
Review and selection of articles describing longitudinal studies.
Characteristics of Studies for the Meta-Analysis
Information about participants in each study is presented in Table 1. These ten published reports each provided one or more predictors, resulting in a total of 21 data points for the meta-analysis (M=2.10, SD=1.20, range=1–5 data points per study; across the 8 cohorts, M=2.62, SD=1.60). Strategies for addressing the non-independence across contributed data points are presented below. In total, across the studies, 17,712 unique participants were included in the meta-analysis.
Data Extraction
For the 21 data points, outcomes representing the impact of childhood externalizing problems on adult unipolar mood disorders were presented as odds ratios (ORs) with 95% confidence intervals (CIs) for 18 data points, and as an independent sample t-test that was converted to an OR for the meta-analysis for three data points. Data were extracted in six areas to address the primary research question and to account for heterogeneity among studies and their respective effect sizes: (1) assessment strategy (checklist, interview), informant (parent, teacher, youth), and externalizing symptoms (ODD, CD, externalizing, aggression, or conduct problems) in childhood; (2) assessment strategy, informant, and mood disorder symptoms or diagnosis at adult follow-up; (3) whether and type of participant characteristics controlled (child sex, family SES); (4) whether baseline levels of externalizing (ADHD or different externalizing symptoms than predictor) or internalizing (depressive, anxiety, or internalizing) symptoms were controlled; (5) ages at baseline and follow-up, and years between baseline and follow-up assessments; and (6) geographic origin of the sample (US or other).
Covariates of Interest
We used the extracted data to create covariates that were hypothesized a priori to explain heterogeneity or variance in effect sizes. For the initial assessment of externalizing behaviors, we considered two informant variables (parent informant: yes/no, other informant (child or teacher): yes/no). We coded whether childhood externalizing behaviors were indexed by symptoms (externalizing, aggression, hostile behavior, conduct problems) or diagnoses (ODD, CD). We also considered (yes/no) whether studies controlled for (a) demographic variables or (b) internalizing symptoms in childhood (depression, anxiety, internalizing). Although we considered ages at baseline and follow-up, as well as duration to follow-up, many studies used a multiple cohort design and thus included ranges of ages (e.g., 9–13 years at baseline, 18–21 at follow-up; see Table 1). Thus, there was not a specific value that we could include in a meta-regression for many studies. To address this issue, we used a categorical coding system for time between baseline assessment and initial follow-up, which led to the creation of 4 variables: 2 based on time since initial assessment (follow-up at > 12 years and > 15 years), and 2 based on individuals’ age at follow-up (> 23 years and > 30 years). Type of assessment at follow up was examined (interview vs. behavioral checklist), but informant was not included because all studies assessed the index individuals at follow-up. Given that gender was treated differently across studies and only two studies explicitly examined sex differences, we were unable to consider sex in the covariate analyses. Finally, we also coded whether cohorts were from the US or not (e.g., European or New Zealand).
Statistical Analysis
We performed a meta-analysis using published (for 18 data points) or calculated (for three data points) ORs and 95% CIs to estimate the precision of the mean for all included studies using Comprehensive Meta-analysis Version 2 (Biostat, Englewood, NJ, n.d.) software. Because the studies included in the meta-analysis varied in methodology and design, a random-effects model was calculated. Multiple predictors and studies drawn from the same cohort were included and accounted for by calculating (a) effect sizes for each cohort, and then (b) an overall effect size. Specifically, effect sizes and variances first were computed for each of the 21 predictors. Next, we calculated a weighted mean for each of the eight cohorts. Weights were based on the inverse of the total variance associated with each of the 21 data points. Last, we computed a weighted mean of the effect sizes for each of the eight cohorts, which were based on within-cohort error and between-cohort variance, to produce an overall summary effect (Borenstein, Hedges, Higgisn, & Rothestein, 2009).
Statistical stability of the results was measured in two ways. First, each study was individually excluded from the analysis and the pooled OR and 95% CI were recalculated. If an individual study contributed heavily to the pooled OR, a change in the magnitude or significance of the pooled OR would be observed. Second, given the possibility of publication bias (i.e., significant findings are more likely to be published), we also calculated Orwins’ Fail-safe N (Borenstein, et al., 2009), which provides an index of the number of studies with a mean OR of 1.0 needed to make the overall effect size trivial (e.g., defined as an OR of 1.01).
Following determination of the combined effect size across studies, we considered heterogeneity or observed variance across studies, indexed by tau, a metric that is sensitive to the unit of measurement and acts as the standard deviation of the summary effect, and l2, which provides an index of the proportion of observed variability that reflects “real” differences among studies (Borenstein, et al., 2009; Higgins, Thompson, Deeks, & Altman, 2003). To explore the impact of the selected covariates on this observed variability among studies, we conducted ancillary, subgroup analyses to determine effect sizes (ORs) for each level of the categorical variable (e.g., separately for studies that do and do not use parent report, or that do and do not control for background variables). For these analyses, ORs and associated p-values were calculated for each level of the categorical variable (Borenstein, et al., 2009). We then examined the Q statistic, which is based on the weighted sum of squares for each level of the covariate and thus provides an index of dispersion (Borenstein, et al., 2009), to determine whether the magnitude of prediction differed between the levels of the covariates. Given that the covariate analyses were hypothesis-generating and based on 8 cohorts, we report differences that were marginally significant (p < .10) for these analyses.
Results
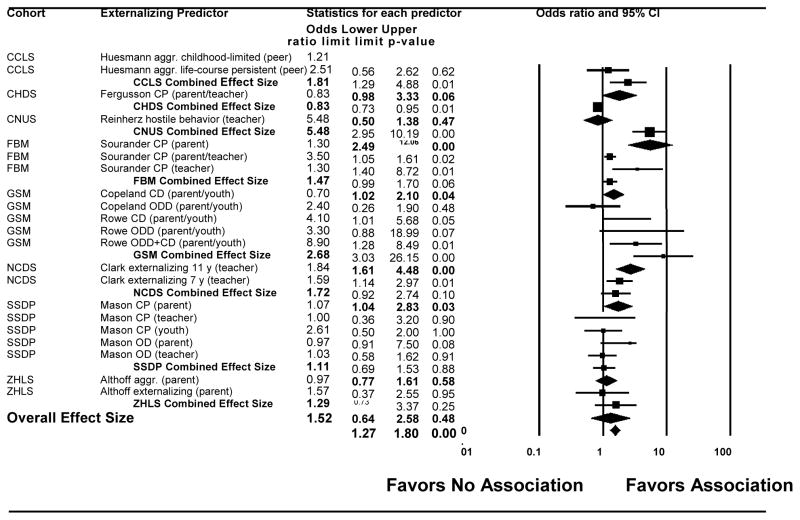
The ten studies included in the meta-analysis represented eight cohorts and 17,712 individuals who underwent assessments in both childhood and adulthood. Across the 21 data points generated within these 8 cohorts, 6 studies and 4 cohorts reported significant findings for prediction from childhood externalizing symptoms to adult unipolar depressive disorders. When all 21 data points were considered together, children who manifested externalizing behaviors were more likely to develop depressive disorders as adults than children who did not demonstrate such symptoms (Figure 2; OR = 1.52, 95% CI = 1.27–1.80, p = 0.000). Results remained significant (OR = 1.45, 95% CI=1.18–1.79, p < .001) when the meta-analysis was limited to children aged 10 and under (vs. 13 and under, the criterion used for the primary analysis). The first column in Figure 2 represents the cohort; the second represents the 21 individual data points. Effect sizes for each of the 21 outcomes are represented by a square and the lines bisecting the square correspond to the CIs. Effect sizes were combined within cohort. Summary statistics for each cohort are presented in rows below their respective data points, with relevant statistics in bold and diamonds in Figure 2.
Figure 2.
Childhood externalizing symptoms as predictors of adult depressive disorders. Boxes reflect weights of individual predictors. Effect sizes were combined within cohorts; combined effect sizes are in bold and represented by diamonds. NCDS = National Child Development Study, CNUS = Community in Northeast US, FBM = Finnish Boy to Man, GSM = Great Smoky Mountains, SSDP = Seattle Social Development Project, ZHLS = Zuid-Holland Longitudinal Study, CCLS = Columbia County Longitudinal Study, CHDS = Christchurch Health and Development Study, aggr. = aggression, CI = confidence interval, CP = conduct problems, OD = oppositional defiant symptoms.
The overall variance of these results was large (l2 = 78.93), suggesting heterogeneity among studies in the magnitude of prediction and that approximately 79% of the variance could be accounted for by covariates. Removal of any individual study from the analysis did not affect the prediction to adult depressive disorders (ORs with each individual study removed ranged from 1.50–1.71, M=1.63, SD=0.06; all ps< 0.001). Using the respective effect sizes for these 21 data points, defining a trivial effect size as an OR of 1.01, and a threshold of p < 0.05, Orwin’s Fail-safe N was 263, indicating that there would have to be 263 studies with a mean OR of 1.0 added to the meta-analysis before the cumulative effect would become trivial.
To explore whether the covariates could account for some of the variability among the effect sizes for each of the 21 data points, we conducted ancillary analyses where separate OR and p values were calculated for each level of the categorical covariates. Because studies within cohorts often differed in these covariates, these supplementary analyses considered the 21 data points independently. Despite the large total number of participants, because only 21 data points from 8 cohorts were considered, these results are intended to be hypothesis-generating as opposed to identifying conclusively reasons for heterogeneity among studies. For one covariate, the magnitude of the ORs differed at a trend level among the levels of each covariate. Specifically, studies that applied dimensional (symptom-based) approaches to describing externalizing behavior in childhood had a significant prediction to depression in adulthood (n=16/21, OR=1.47, p=.003), whereas those studies that used categorical (ODD, CD) approaches also had a significant, but marginally stronger, prediction to adult depressive disorders (n=5/21, OR=2.72, p=.001; index of group difference: Q = 3.50, p=.06). All other comparisons between the different levels of each covariate were not significant (parent vs. non-parent informant, U.S vs non-U.S sample, time gap between evaluations, age at initial evaluation and follow-up, control for internalizing and externalizing symptoms vs. not controlling for either internalizing or externalizing symptoms; all Qs < 2.08, all ps > .15). Results of all covariate analyses are reported in Supplementary Table 1.
Discussion
Although efforts to understand the etiology of depressive disorders have focused on numerous possible childhood risk factors, previous research has been mixed in terms of the magnitude and significance of a link between childhood externalizing symptoms or disorders and the development of adult depression. Such knowledge has important implications for prevention, intervention, and etiological models, yet we know of no systematic efforts to quantitatively combine previous findings to clarify associations between childhood externalizing symptoms and adult depression. The goals of this meta-analysis were to address these mixed findings by determining whether there is developmental continuity between childhood externalizing disorders and adult depression across eight large, longitudinal samples followed from childhood into adulthood; to ascertain the magnitude of this association; and, as an ancillary strategy, to explore whether methodological differences across studies (i.e., covariates) might account for the heterogeneity in effect sizes across cohorts.
The findings of this meta-analysis confirm that among community-based samples, childhood externalizing symptoms and disorders predict unipolar depressive symptoms and disorders in adulthood. Specifically, compared to children without externalizing behaviors, those with such behaviors were approximately 1.5 times more likely to develop depression as adults. This finding supports previous reports indicating the existence of heterotypic development of psychiatric disorders across the lifespan (Burke, Loeber, Lahey, & Rathouz, 2005; Capaldi, 1992; Costello, Mustillo, Erkanli, Keeler, & Angold, 2003; Fergusson, Boden, & Horwood, 2007; Fischer, Barkley, Smallish, & Fletcher, 2002; Hofstra, van der Ende, & Verhulst, 2002; Loeber & Farrington, 1994; Moffitt et al., 2007; Pine, Cohen, Gurley, Brook, & Ma, 1998; Roza, et al., 2003; Woodward & Fergusson, 1999; Zoccolillo, 1992). Given that this is the first meta-analysis examining the association between childhood externalizing psychopathology and adult depression, the present results extend this more general finding of heterotypic continuity to these specific conditions that are common and impairing, but not often considered jointly.
Several lines of research lend support to the developmental relation between early externalizing problems and later depression reported here. Existing explanatory models for this trajectory posit that disruptive behavior in childhood may lead to developmental “failures” in domains in which youth strive to be successful (e.g., poor family and peer relations, academic underperformance). These repeated failures might then contribute to depression (Drabick, 2009; Drabick, Gadow, & Sprafkin, 2006; Patterson & Capaldi, 1990). Thus, interventions that minimize childhood behavior problems and associated interpersonal and academic difficulties could mitigate risk for adult depressive disorders. Indeed, there is some evidence that such a preventive approach can be successful, even when depressive symptoms are not a target of such preventive interventions. For example, Stormshak and colleagues reported that the Family Check-Up, a family-centered intervention designed to prevent youth behavior problems and improve adjustment, predicted not only improved self-regulation among youth, but also decreased depressive symptoms prospectively (Stormshak, Fosco, & Dishion, 2010). Similarly, among families who participated in the Adolescent Transitions Program, a prevention program that focuses on parenting factors related to adolescent behavior problems, intervention youth were less likely to exhibit depressive symptoms than youth whose families did not receive the intervention (Connell & Dishion, 2008). Last, in a study examining the effects of Parent Management Training, although improved parenting led to reductions in child behavior problems, these effects were mediated by reductions in boys’ depressive symptoms (DeGarmo, Patterson, & Forgatch, 2004). Thus, though not a proximal target of these family-based interventions for youth behavior problems, several studies indicate that intervening with child behavior problems is associated with attenuated risk for subsequent depressive symptoms.
The affective instability seen in childhood externalizing disorders also has been conceptualized as a possible contributing mechanism to later life mood disorders (Burke, et al., 2005; Capaldi, 1992; Capaldi & Stoolmiller, 1999). Specifically, Stringaris found that after a 20-year follow-up, chronic irritability in adolescence predicted MDD and dysthymia at age 33 (Stringaris, Cohen, Pine, & Leibenluft, 2009). Similarly, in the Great Smoky Mountains Study, adolescent irritability was predictive of MDD and dysthymia at 20 year follow-up even after controlling for baseline behavioral and emotional disorders (Rowe, et al., 2010). Because of a lack of specific assessment of irritability in most of the longitudinal studies included in this meta-analysis, we are unable to directly test hypotheses about irritability as a specific mediator of adult depression. We were also unable to test associations between ODD, which has an irritable dimension, and adult depression specifically, because few studies identified categorical diagnoses (e.g., ODD) in their baseline assessments, and only Rowe et al. considered ODD dimensions as well. However, based on previous work (Bank, Duncan, Patterson, & Reid, 1993; Costello, et al., 2003; Rowe, et al., 2010; Stringaris & Goodman, 2009), we speculate that irritability, commonly seen in childhood externalizing disorders, may serve as a risk factor or mediate the transition to subthreshold depression and eventually MDD, possibly through shared genetics (Stringaris, Zavos, Leibenluft, Maughan, & Eley, 2012). Finally, given that mood and anxiety disorders are highly co-morbid and that the studies in this meta-analysis did not control for adult anxiety symptoms/disorders, it is possible that childhood externalizing disorders may predict general adult affective instability, including anxiety symptoms, rather than isolated depressive disorders.
Often, meta-analyses do not account for the methodological heterogeneity across the included studies, thus precluding consideration of why previous findings may be mixed and consequently limiting the interpretation of the results. In the present meta-analysis, 79% of the variance could be explained by differences among the studies in terms of sample, study design, and other potential covariates. The method of characterizing externalizing disorders influenced the degree of association between childhood externalizing behavior and adult depression. In exploratory analyses, we found a trend such that, when DSM diagnoses were used to define externalizing disorders, the prediction to adult depression was marginally stronger than when dimensional, symptom-based approaches were employed, though both strategies resulted in significant prediction to adult depressive disorders. Previous research indicates that childhood externalizing behaviors conceptualized dimensionally are associated with adult depression (Angold, Costello, Farmer, Burns, & Erkanli, 1999; Brotman et al., 2006; Drabick, 2009; Stringaris, et al., 2009), suggesting that defining childhood behavior using both dimensional and categorical conceptualizations of children’s behavior problems may be useful for clarifying the trajectories from childhood externalizing behavior to adult depressive disorders (Drabick, 2009).
An important issue to consider in examining these longitudinal outcomes is that most of the studies (6/8 cohorts; 17/21 data points) did not control for the possible impact of co-occurring childhood depression on adult depression outcomes. This omission is of concern for the present findings given that childhood internalizing symptoms such as depression have been shown to predict depression in adulthood. Thus, given the co-occurrence of internalizing and externalizing symptoms among youth (Burke, et al., 2005; Capaldi, 1992; Drabick, et al., 2006), it is possible that adult depression among children with externalizing psychopathology may actually reflect homotypic continuity from their childhood internalizing symptoms rather than heterotypic continuity from their externalizing symptoms or disorders. These data do not allow us to rule out this possibility at this time. However, we suggest that childhood internalizing symptoms are unlikely to account completely for our findings for three reasons. First, although childhood internalizing symptoms were not controlled in most of the studies considered in the present meta-analysis, homotypic continuity for internalizing symptoms often was considered. Findings drawn from the cohorts considered in this meta-analysis indicate that childhood internalizing symptoms were predictors of adult depression across only half of these samples (Supplementary Table 2). It is important to note that this lack of consistent prediction should not be interpreted as a general lack of evidence for homotypic continuity for depression. Our cohorts were not necessarily representative of typical or depressed pediatric samples, as we only selected children who had been assessed for externalizing disorders. Second, when we compare the small number of studies that did control for childhood internalizing symptoms when predicting adult depression (4/21 data points; OR=1.57, p =0.115) to those that did not control for childhood depression (17/21 data points; OR= 1.65, p = 0.000), we find that the magnitude of these predictions was not significantly different (Q value =0.03, p=0.87; Supplementary Table 1). Thus, prediction from studies that did and did not control for childhood depression among the included studies in this meta-analysis was similar in magnitude, suggesting that whether depression was controlled, externalizing symptoms predicted adult depressive disorders. Third, depression typically has its onset after puberty and consequently occurs in a relatively small subset (0%–8.4%) of children (ages 9–13) with CD or ODD (Angold, Costello, & Erkanli, 1999). Thus, in childhood, there is only a small proportion of youth who meet criteria for depressive disorders and comorbid externalizing psychopathology, and it is unlikely that these children with comorbid conditions drive our findings. In sum, although our conclusions are limited by the fact that most studies did not control for childhood internalizing symptoms in examining prediction to adult depression, other evidence suggests that childhood internalizing symptoms are unlikely to account completely for the association we report between childhood externalizing symptoms and adult depression.
The studies included in this meta-analysis used varying informants, rating scales and interviews, sample demographics, analytic designs, and follow-up assessments. Although the chosen covariates illustrated differential associations with adult depressive disorders, several other factors that were not examined may affect the associations seen in this study. Specifically, the magnitude of the association between childhood externalizing behaviors and adult depression may be underestimated secondary to selection bias and study attrition. Families and children with disadvantaged backgrounds, who may be at higher risk for externalizing disorders at baseline, are more likely to be lost at follow-up. We chose to exclude clinical samples, as well as studies comprised of families with identified genetic risk for developing unipolar depression (i.e., offspring of depressed parents), which may also have resulted in our underestimating the magnitude of the association between childhood externalizing disorders and adult depression. Finally, sex differences were not uniformly addressed by the studies used in this meta-analysis, and sex therefore was not examined as a moderator.
Despite the fact that our analysis is probably conservative in terms of our inclusion criteria, Orwin’s Fail-safe N demonstrated that 263 studies with a mean OR of 1.0 would be needed to make the overall effect size trivial. We did not omit studies that utilized data from the same cohort, which enabled us to increase the number of data points that we could examine but also led to a reduction in power to test covariates because of the resulting nested design of the meta-analysis. However, when each study was systematically removed from the meta-analysis, the magnitude of the association stayed remarkably similar. Thus, expanding our inclusion criteria would have led to greater power to test covariates that account for heterogeneity in effect sizes, but would have altered the types of conclusions that could be drawn from these data. Future research that includes a greater number of cohorts and/or uses less stringent inclusion criteria would provide greater power to test potential covariates and moderators. However, despite the relatively small number of studies utilized here, the data are drawn from prospective, epidemiological and community-based studies that include a total of 17,712 participants. In addition, the sampling design of many studies required our use of categorical covariates, which further limited our power to test covariates. Although this limitation stemmed from the lack of dimensional variables in the original studies, future research that includes dimensional covariates and meta-regression could permit greater power for tests designed to account for variability in effect sizes across studies.
To our knowledge, this is the first meta-analysis examining the link between childhood externalizing disorders and adult depression. This report contributes to the already existing data suggesting that depressive psychopathology may develop in a heterotypic fashion. Intuitively, researchers and clinicians alike are likely to assume that childhood internalizing disorders precede adult internalizing disorders. The findings from the present analyses suggest that our understanding of the developmental trajectory of depression should be expanded to encompass early life externalizing problems. In addition, those children with externalizing behavior and a family history of depression may be at particularly high risk to develop depression (Beardslee, Gladstone, & O’Connor, 2012), suggesting potential risk profiles to consider in future research. Our work suggests that children with externalizing disorders should be observed closely for the emergence of depression in adolescence, in addition to adult manifestations of externalizing behavior such as antisocial personality disorder or substance use disorders. This conceptualization of childhood externalizing disorders could inform depression prevention programs and decisions made by agencies who fund clinical and research programming. Further research is needed to determine mechanisms that underlie this association, so that targets for prevention and treatment can be better tailored.
Supplementary Material
Results of covariate analyses. “N for present/yes” indicates the number of data points with the particular variable present (e.g., “Informant: parent” indicates 13 data points included data from which the parent was the informant); “OR for present/yes” is the odds ratio (OR) for which the particular variable predicts adult depression (e.g., data points with parents as informants are 1.613 times more likely to predict depression than studies without parents as informants); p is the relevant p value associated with the OR, indicating significance at p < .05. “N and OR for absent” represents the same information, except for data points where the particular variable is absent (e.g., studies that did not use parents as informants).
The relation between childhood depression (and/or internalizing symptoms) and adult depression from the community- and epidemiological-based cohorts considered in the meta-analysis.
Acknowledgments
This research was partially supported by grants from the National Institute of Mental Health (K01MH0737 to DD; Intramural Research Program to EL) and the National Institutes of Drug Abuse (K12 DA000357 for LH’s effort). The authors would like to thank Mr. Michael Tonzi for administrative assistance and Dr. Michael Borenstein for statistical consultation.
References
- Althoff RR, Verhulst FC, Rettew DC, Hudziak JJ, van der Ende J. Adult outcomes of childhood dysregulation: A 14-year follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:1105–1116. doi: 10.1016/j.jaac.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Angold A, Costello EJ, Farmer EM, Burns BJ, Erkanli A. Impaired but undiagnosed. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:129–137. doi: 10.1097/00004583-199902000-00011. [DOI] [PubMed] [Google Scholar]
- Bank L, Duncan T, Patterson GR, Reid J. Parent and teacher ratings in the assessment and prediction of antisocial and delinquent behaviors. J of Personality. 1993;61:693–709. doi: 10.1111/j.1467-6494.1993.tb00787.x. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Gladstone TR, O’Connor EE. Developmental risk of depression: Experience matters. Child and Adolescent Psychiatric Clinics of North America. 2012;21:261–278. vii. doi: 10.1016/j.chc.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Dolan C, Hughes S, Mick E, Monuteaux MC, Faraone SV. The long-term longitudinal course of oppositional defiant disorder and conduct disorder in ADHD boys: findings from a controlled 10-year prospective longitudinal follow-up study. Psychological Medicine. 2008;38:1027–1036. doi: 10.1017/S0033291707002668. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgisn JPT, Rothestein HR. Introduction to Meta-analysis. Chichester: Wiley; 2009. [Google Scholar]
- Brotman MA, Schmajuk M, Rich BA, Dickstein DP, Guyer AE, Costello EJ, Leibenluft E. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biological Psychiatry. 2006;60:991–997. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. Journal of Child Psychology and Psychiatry. 2005;46:1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- Capaldi DM. Cooccurrence of Conduct Problems and Depressive Symptoms in Early Adolescent Boys. A 2-Year Follow-up at Grade-8. Development and Psychopathology. 1992;4:125–144. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Stoolmiller M. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: III. Prediction to young-adult adjustment. Development and Psychopathology. 1999;11:59–84. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Clark C, Rodgers B, Caldwell T, Power C, Stansfeld S. Childhood and adulthood psychological ill health as predictors of midlife affective and anxiety disorders: the 1958 British Birth Cohort. Archives of General Psychiatry. 2007;64:668–678. doi: 10.1001/archpsyc.64.6.668. [DOI] [PubMed] [Google Scholar]
- Colman I, Murray J, Abbott RA, Maughan B, Kuh D, Croudace TJ, Jones PB. Outcomes of conduct problems in adolescence: 40 Year follow-up of national cohort. British Medical Journal. 2009;338:a2981. doi: 10.1136/bmj.a2981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell AM, Dishion TJ. Reducing depression among at-risk early adolescents: three-year effects of a family-centered intervention embedded within schools. Journal of Family Psychology: Journal of the Division of Family Psychology of the American Psychological Association. 2008;22:574–585. doi: 10.1037/0893-3200.22.3.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor DF, Ford JD, Albert DB, Doerfler LA. Conduct disorder subtype and comorbidity. Annals of Clinical Psychiatry: Official Journal of the American Academy of Clinical Psychiatrists. 2007;19:161–168. doi: 10.1080/10401230701465269. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry. 2009;66:764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- DeGarmo DS, Patterson GR, Forgatch MS. How do outcomes in a specified parent training intervention maintain or wane over time? Prevention Science: The official Journal of the Society for Prevention Research. 2004;5:73–89. doi: 10.1023/b:prev.0000023078.30191.e0. [DOI] [PubMed] [Google Scholar]
- Drabick DA. Can a Developmental Psychopathology Perspective Facilitate a Paradigm Shift toward a Mixed Categorical-Dimensional Classification System? Clinical Psychology: A publication of the Division of Clinical Psychology of the American Psychological Association. 2009;16(1):41–49. doi: 10.1111/j.1468-2850.2009.01141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drabick DA, Gadow KD, Sprafkin J. Co-occurrence of conduct disorder and depression in a clinic-based sample of boys with ADHD. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2006;47:766–774. doi: 10.1111/j.1469-7610.2006.01625.x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Recurrence of major depression in adolescence and early adulthood, and later mental health, educational and economic outcomes. British Journal of Psychiatry. 2007;191:335–342. doi: 10.1192/bjp.bp.107.036079. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Childhood self-control and adult outcomes: results from a 30-year longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:709–717. e701. doi: 10.1016/j.jaac.2013.04.008. [DOI] [PubMed] [Google Scholar]
- Fischer M, Barkley RA, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: self-reported psychiatric disorders, comorbidity, and the role of childhood conduct problems and teen CD. Journal of Abnormal Child Psychology. 2002;30:463–475. doi: 10.1023/a:1019864813776. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Viding E. Antisocial behavior from a developmental psychopathology perspective. Developmental Psychopathology. 2009;21:1111–1131. doi: 10.1017/S0954579409990071. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analysis. British Medical Journal. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofstra MB, van der Ende J, Verhulst FC. Child and adolescent problems predict DSM-IV disorders in adulthood: a 14-year follow-up of a Dutch epidemiological sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:182–189. doi: 10.1097/00004583-200202000-00012. [DOI] [PubMed] [Google Scholar]
- Huesmann LR, Dubow EF, Boxer P. Continuity of aggression from childhood to early adulthood as a predictor of life outcomes: Implications for the adolescent-limited and life-course-persistent models. Aggressive Behavior. 2009;35:136–149. doi: 10.1002/ab.20300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) The Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Loeber R, Farrington DP. Problems and solutions in longitudinal and experimental treatment studies of child psychopathology and delinquency. Journal of Consulting Clinical Psychology. 1994;62:887–900. doi: 10.1037//0022-006x.62.5.887. [DOI] [PubMed] [Google Scholar]
- Mason WA, Kosterman R, Hawkins JD, Herrenkohl TI, Lengua LJ, McCauley E. Predicting depression, social phobia, and violence in early adulthood from childhood behavior problems. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:307–315. doi: 10.1097/00004583-200403000-00012. [DOI] [PubMed] [Google Scholar]
- Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychological Review. 1993;100:674–701. [PubMed] [Google Scholar]
- Moffitt TE, Caspi A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Developmental Psychopathology. 2001;13:355–375. doi: 10.1017/s0954579401002097. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: follow-up at age 26 years. Developmental Psychopathology. 2002;14:179–207. doi: 10.1017/s0954579402001104. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, Poulton R. Depression and generalized anxiety disorder: cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Archives of General Psychiatry. 2007;64:651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Capaldi DM. Risk and Protective Factors in the Development of Psychopathology. New York: Cambridge University Press; 1990. [Google Scholar]
- Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry. 1998;55:56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Reinherz HZ, Giaconia RM, Hauf AM, Wasserman MS, Silverman AB. Major depression in the transition to adulthood: Risks and impairments. Journal of Abnormal Psychology. 1999;108:500–510. doi: 10.1037//0021-843x.108.3.500. [DOI] [PubMed] [Google Scholar]
- Reinherz HZ, Paradis AD, Giaconia RM, Stashwick CK, Fitzmaurice G. Childhood and adolescent predictors of major depression in the transition to adulthood. The American Journal of Psychiatry. 2003;160:2141–2147. doi: 10.1176/appi.ajp.160.12.2141. [DOI] [PubMed] [Google Scholar]
- Rowe R, Costello EJ, Angold A, Copeland WE, Maughan B. Developmental pathways in oppositional defiant disorder and conduct disorder. Journal of Abnormal Psychology. 2010;119:726–738. doi: 10.1037/a0020798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roza SJ, Hofstra MB, van der Ende J, Verhulst FC. Stable prediction of mood and anxiety disorders based on behavioral and emotional problems in childhood: a 14-year follow-up during childhood, adolescence, and young adulthood. American Journal of Psychiatry. 2003;160:2116–2121. doi: 10.1176/appi.ajp.160.12.2116. [DOI] [PubMed] [Google Scholar]
- Sourander A, Helstela L. Childhood predictors of externalizing and internalizing problems in adolescence. A prospective follow-up study from age 8 to 16. European Child and Adolescent Psychiatry. 2005;14:415–423. doi: 10.1007/s00787-005-0475-6. [DOI] [PubMed] [Google Scholar]
- Sourander A, Jensen P, Davies M, Niemela S, Elonheimo H, Ristkari T, Almqvist F. Who is at greatest risk of adverse long-term outcomes? The Finnish From a Boy to a Man study. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1148–1161. doi: 10.1097/chi.0b013e31809861e9. [DOI] [PubMed] [Google Scholar]
- Stormshak EA, Fosco GM, Dishion TJ. Implementing Interventions with Families in Schools to Increase Youth School Engagement: The Family Check-Up Model. School Mental Health. 2010;2:82–92. doi: 10.1007/s12310-009-9025-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult outcomes of youth irritability: a 20-year prospective community-based study. American Journal of Psychiatry. 2009;166:1048–1054. doi: 10.1176/appi.ajp.2009.08121849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris A, Goodman R. Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:404–412. doi: 10.1097/CHI.0b013e3181984f30. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Zavos H, Leibenluft E, Maughan B, Eley TC. Adolescent irritability: phenotypic associations and genetic links with depressed mood. American Journal of Psychiatry. 2012;169:47–54. doi: 10.1176/appi.ajp.2011.10101549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward LJ, Fergusson DM. Childhood peer relationship problems and psychosocial adjustment in late adolescence. Journal of Abnormal Child and Adolescent Psychology. 1999;27:87–104. doi: 10.1023/a:1022618608802. [DOI] [PubMed] [Google Scholar]
- Zoccolillo M. Co-occurrence of conduct disorder and its adult outcomes with depressive and anxiety disorders: A review. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:547–556. doi: 10.1097/00004583-199205000-00024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Results of covariate analyses. “N for present/yes” indicates the number of data points with the particular variable present (e.g., “Informant: parent” indicates 13 data points included data from which the parent was the informant); “OR for present/yes” is the odds ratio (OR) for which the particular variable predicts adult depression (e.g., data points with parents as informants are 1.613 times more likely to predict depression than studies without parents as informants); p is the relevant p value associated with the OR, indicating significance at p < .05. “N and OR for absent” represents the same information, except for data points where the particular variable is absent (e.g., studies that did not use parents as informants).
The relation between childhood depression (and/or internalizing symptoms) and adult depression from the community- and epidemiological-based cohorts considered in the meta-analysis.