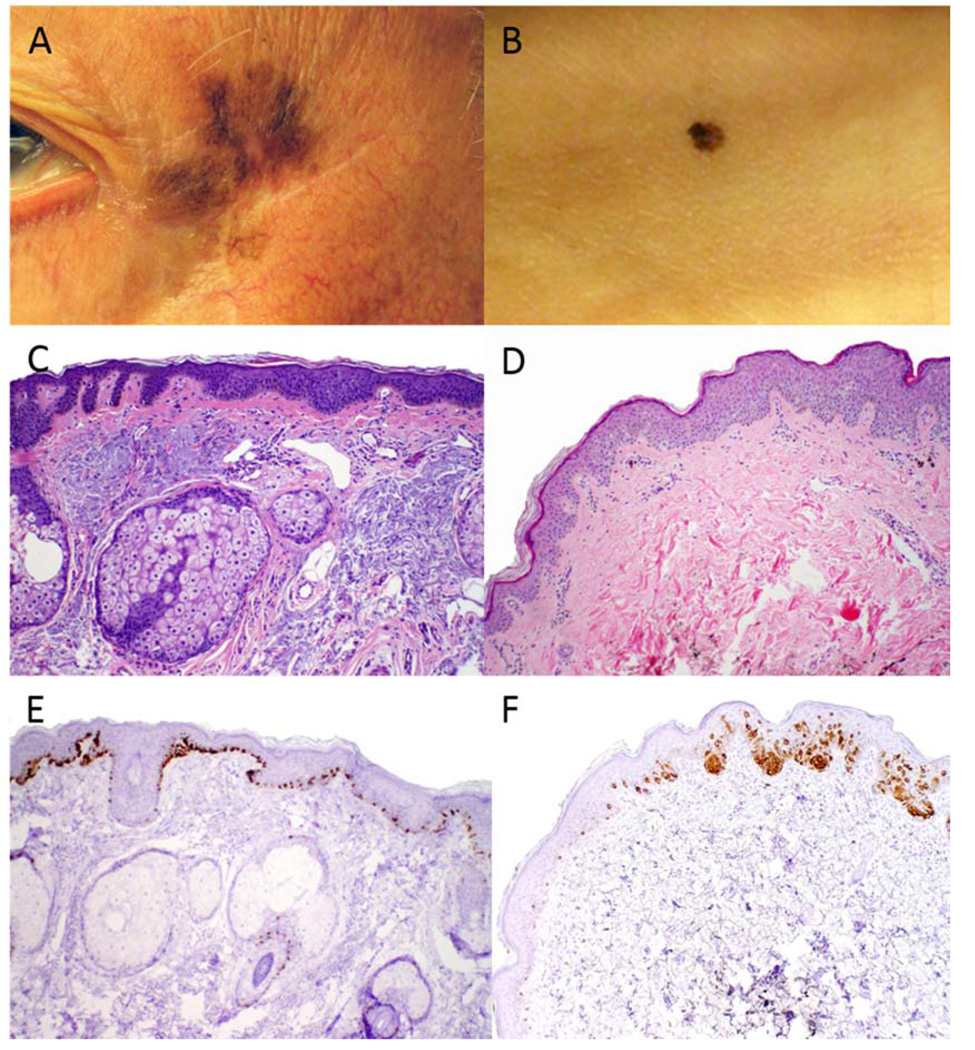
To the Editor: The lentigo maligna (LM) subtype of melanoma-in-situ (MIS) develops on chronically sun-exposed skin, with indistinct clinical margins corresponding to single melanocytes trailing along the epidermal-dermal junction (Figure 1A,C,E). Alternatively, the less common non-lentiginous MIS (non-LM MIS) typically occurs in more sun-protected areas with distinct clinical margins corresponding to sharp transition from malignant to normal melanocytes histologically (Figure 1B,D,F).
Fig 1.
Clinical and histologic photographs of LM and non-LM-MIS. A, Clinical lesion of LM and B, Clinical lesion of non-LM-MIS contrast the relatively indistinct versus distinct clinical margins in these subtypes of MIS. C, Histology of LM demonstrates the lentiginous melanocytic pattern and presence on sun-damaged skin. D, Histology of non-LM-MIS demonstrates the non-lentiginous melanocytic pattern and presence on non-sun-damaged skin. E, Immunohistochemical labeling with Melan-A in LM demonstrates an increased number of melanocytes trailing off at the edge of the lesion, making it difficult to discern from atypical melanocytic hyperplasia. F, Melan-A staining in non-LM-MIS demonstrates sharp demarcation of melanocyte density. These distinct histologic patterns account for the clinically indistinct margins observed in LM (A) versus the clinically distinct margins observed in non-LM-MIS (B). All photomicrographs taken at 100× original magnification.
Treatment of MIS has historically been surgical excision with 5-mm margins, however a footnote added in the recent NCCN guidelines indicates that some MIS (i.e. LM) require greater margins to ensure removal and prevent local recurrence.1 Based on their review of MIS lesions treated by Mohs surgery and finding that 14% required a margin of > 6 mm for histologic clearance, Kunishige et al.2 recommended 9-mm margins for standard excision of MIS. Appropriate surgical margins for non-LM MIS using standard excision technique have not been rigorously defined,3 and treating all MIS with 9-mm excisional margins as proposed2 may lead to larger than necessary excisions for non-LM MIS. We initiated an IRB-approved study (RONMIST: Review of non-lentiginous melanoma-in-situ lesions treated) to determine histologic margins and recurrence rates of non-LM-MIS treated by standard excision at our institution.
From the University of Utah Dermatology dermatopathology (1990–2010) and Huntsman Cancer Institute Melanoma Program (2000–2010) databases, we identified 268 unique cases reported as non-LM-MIS. Matching biopsy and excision slides were obtained for 81 cases, which were reviewed in blinded fashion by board-certified dermatopathologists (KLD, SRF, ARB) to assess accuracy of initial diagnosis and confirm non-LM MIS. Only 36 biopsies were confirmed as non-LM MIS (Table I). Among the excluded cases, most (40/45) were deemed LM and not non-LM MIS. The biopsy margins were positive in only 16 specimens (11 shaves, 5 punches), and in none of the 6 excisional biopsies. Only 3 of the 16 (19%) biopsy specimens with positive margins demonstrated residual melanoma on re-excision, and none of the specimens with negative biopsy margins demonstrated residual tumor on re-excision. The average histologic excisional margin was 3.80 mm (range 0.2 – 6.5 mm). While our practice is to excise these lesions with 5-mm margins, our data suggests that often the clinical margins are < 5 mm even after normal shrinkage (approximately 15%) from formalin processing is accounted for. The average margin of clearance was 4.38 mm (range 1.30 – 7.75 mm).
Table I.
Histologic margin assessment of non-LM-MIS cases in this study.
| Cases screened by dermatopathologists | 81 |
| Confirmed cases of non-LM-MIS | 36 |
| Biopsy technique | Shave (18), punch (12), excisional (6) |
| Average excisional margin a | 3.80 mm (range 0.2–6.5) |
| Average margin of clearance b | 4.38 mm (range 1.30–7.75) |
Measured from residual melanoma in situ or edge of the scar in the excision specimen.
Sum of clear biopsy margin and excisional margin.
As summarized in Table II, these lesions were confined to the trunk or extremities and had a median size of 7 mm (range 2–18). Of 34 patients with confirmed follow-up (0.5 to 18 years, median 6.6 years), none had clinical evidence of recurrence. Follow-up times were short for some patients who were seen shortly after surgery and then never returned for additional follow-up.
Table II.
Demographic and clinical information for patients with non-LM-MIS in this study.
| Number of patients included a | 36 |
| Gender | F:M ratio = 3:1 |
| Median age at diagnosis | 44.9 years (range 10.4–77.7) |
| Tumor sites | Head and Neck (0) Shoulder (4) Chest (2) Abdomen (2) Back (8) Arm (6) Leg (11) Foot (3) |
| Median lesion size b | 7 mm (range 2–18) |
| Number of patients with clinical f/u | 34 (94%) |
| Number of patients with clinical recurrence | 0 |
| Median f/u time c | 6.6 years (range 0.5–18.3) |
No patients had more than one non-LM MIS lesion.
Determined from biopsy and excision pathology reports.
Follow-up length was determined from the date of excision to the most recent follow-up visit where clinical recurrence was documented.
Most prior studies of MIS did not distinguish between LM and non-LM MIS subtypes. In response to our correspondence,3 Kunishige et al.4 re-analyzed a subset of their cases and reported that 17 of 91 (19%) “other MIS” (non-LM) cases required > 6-mm margins for histologic clearance. A possible explanation for this discrepancy in margin requirements between their study and ours is that some of their “other MIS” lesions may have been LM rather than non-LM MIS. Distinguishing between these two entities on frozen sections is problematic due to freeze artifact, and they do not appear to have re-reviewed permanent paraffin-embedded sections to confirm diagnoses as we did in the present study. We were able to distinguish clearly between these two MIS subtypes upon histologic examination. Our results are consistent with a recent study by Akhtar et al.5 in which 192 cases of MIS (62% were non-LM MIS) were examined; no recurrence of non-LM MIS lesions was found and most were excised with margins of 2–5 mm.
In conclusion, LM and non-LM MIS are distinct entities clinically, histologically, and molecularly – thus their optimal treatment is not the same. Based on our findings, we suggest that 5-mm margins are adequate for standard excision of lesions clinically and histologically consistent with non-LM MIS.
Acknowledgements
D.G. is supported by the Department of Dermatology, the Huntsman Cancer Foundation, and the National Institutes of Health.
We thank Carolyn Ross and Patricia Tibolla for help in identifying cases from databases and obtaining histologic slides for review.
Abbreviations
- LM
lentigo maligna
- MIS
melanoma-in-situ
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: None declared.
References
- 1.Coit DG, Andtbacka R, Anker CJ, Bichakjian CK, Carson WE, 3rd, Daud A, et al. Melanoma, version 2.2013: featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2013;11:395–407. doi: 10.6004/jnccn.2013.0055. [DOI] [PubMed] [Google Scholar]
- 2.Kunishige JH, Brodland DG, Zitelli JA. Surgical margins for melanoma in situ. J Am Acad Dermatol. 2012;66:438–444. doi: 10.1016/j.jaad.2011.06.019. [DOI] [PubMed] [Google Scholar]
- 3.Grossman D, Duffy KL, Bowen GM. Surgical margins for melanoma in situ. J Am Acad Dermatol. 2012;67:1068–1069. doi: 10.1016/j.jaad.2012.04.046. [DOI] [PubMed] [Google Scholar]
- 4.Kunishige JH, Brodland DG, Zitelli JA. Larger surgical margins are required for lentigo maligna and other melanoma in situ. J Am Acad Dermatol. 2012;67:1069–1071. [Google Scholar]
- 5.Akhtar S, Bhat W, Magdum A, Stanley PR. Surgical excision margins for melanoma in situ. J Plast Reconstr Aesthet Surg. 2014;67:320–323. doi: 10.1016/j.bjps.2013.11.014. [DOI] [PubMed] [Google Scholar]