Abstract
Purpose
To study the reliability of a Non-Instrumented Walk Test in individuals with Parkinson's disease (PD).
Method
Thirty individuals (21 Males) with PD were studied. Their mean age was 68.90 ± 9.28 years. The average time since diagnosis was 8.75 ± 5.68 years. The reliability of the manual Non-Instrumented Walk Test was studied while “OFF” and “ON” dopaminergic medication. Subjects walked at their self-selected, usual speed during a Non-Instrumented Walk Test and while walking on a computerized instrumented walkway. Intraclass correlation coefficients (ICCs) were calculated and means were compared for three gait parameters as measured by the two methods.
Results
During “OFF” medication testing, ICCs between the Non-Instrumented Walk Test and the instrumented measures for gait speed, cadence and stride length were 0.96 (p < 0.0005), 0.72 (p = 0.001) and 0.97 (p < 0.0005), respectively. During “ON” medication testing, the ICCs were 0.96 (p < 0.0005), 0.86 (p < 0.0005) and 0.96 (p < 0.0005), respectively. The means of the non-instrumented measures tended to be lower than those obtained on the instrumented walkway.
Conclusions
The Non-Instrumented Walk Test is a quick, simple and inexpensive gait evaluation for individuals with PD. The method is sufficiently reliable to be used clinically in this population during different medication cycles.
Keywords: GAITRite, medication status, Non-Instrumented Walk Test, Parkinson's disease, reliability
Introduction
Gait disturbance is one of the clinical hallmarks of Parkinson's disease (PD) and a frequent cause of disability and impairment. The PD gait pattern is characterized by reduced speed, short stride lengths, shuffling steps and, occasionally, freezing episodes [1]. Gait evaluation in individuals with PD is crucial in clinical settings. Gait measurement approaches including paper imprint methods [2], electronic foot switches [3], video-based systems [4,5] and a three-dimensional motion analysis system [6] have been used for gait evaluation.
Laboratory-based quantitative gait measures are expensive, time consuming and labor intensive and they require technical expertise [3–6]. These measures are burdensome in clinical applications, where quick and simple methods are more suitable [7]. A simple timed walk test can be used to measure certain gait parameters and may provide a way to quickly obtain quantitative gait evaluation in routine clinical assessments [7]. However, it is not known if a Non-Instrumented Walk Test is a reliable way to estimate gait speed, cadence and stride length in individuals with PD.
In clinical practice, clinicians often perform mobility evaluations in individuals with PD during different medication states depending on the time of the evaluation. Therefore, we performed this study during poorest performance (“OFF” medication) and during peak performance (“ON” medication) to establish the correlation of the two methods of gait measure in the extremes of the medication states. Therefore, the primary aim of this study was to determine the reliability of gait parameters measured by the Non-Instrumented Walk Test while “OFF” and “ON” dopaminergic medication in individuals with PD.
To date, no study has examined the correlation of gait parameters calculated from a non-instrumented, timed walk test compared to the parameters measured by a computerized walkway. It was hypothesized that a non-instrumented, timed walk test would be highly correlated with gait parameters measured by a computerized walkway when testing while “OFF” and “ON” dopaminergic medication. A secondary aim was to compare the means of the gait parameters as measured by the two methods to determine whether there was any consistent bias.
Materials and methods
Subjects
Thirty individuals with idiopathic PD were recruited from movement disorder outpatient clinics in the Houston area. They all had gait or balance impairment or had fallen. Their Hoehn and Yahr stages were between 2 and 3 [8]. All subjects were able to stand and walk independently. No subject had visual or hearing deficits that would interfere with the walking test. Subjects were excluded if they had clinically significant musculoskeletal problems in their back, hips, knees or ankles that currently interfered with walking.
All subjects received levodopa therapy for PD. None of them had had stereotactic brain surgery or deep brain stimulation. Subjects were screened for cognitive impairment with the Neurobehavioral Cognitive Status Examination (Cognistat) [9]. The Unified Parkinson Disease Rating Scale (UPDRS) [10] was used to assess disease severity of the subjects.
Equipment and measures
The GAITRite system (GAITRite, CIR Systems Inc., Havertown, PA), is a 5-m, computerized instrumented walkway containing sensor pads encapsulated in a roll-up carpet. While the subject walks, the system continuously scans the sensors to detect pressures, and transfers the information to the computer for calculating, recording and storing gait characteristics. The parameters of interest were gait speed, cadence and stride length.
A stop watch with 0.04 s/h accuracy was used to time the Non-Instrumented Walk Test (ACCUSPLIT Pro Survivor – A601X Stopwatch, Livermore, CA).
Walking protocol
The study used a within-subjects design to assess the reliability of gait speed, cadence and stride length of the Non-Instrumented Walk Test compared to the same parameters obtained by the instrumented walkway. These three parameters are those most used clinically to evaluate the effect of a treatment. They are also measures that can be performed simply by one tester.
All subjects read and signed an approved consent form prior to participation. Usual speed was tested while “OFF” and “ON” dopaminergic medication on the same day. For “OFF” medication testing, the subjects were tested in the morning after abstaining from their dopaminergic medication overnight. The wash-out period was at least 12 h in the “OFF” medication state. They were assessed by a neurologist with the UPDRS Motor section III for “OFF” status prior to performing the walking test. After walking on the computerized mat at their self-selected, usual speed, the subjects took a few minutes break and walked at their usual speed for 500 cm (5 m) on the floor in the laboratory. One tester timed their walk with a stop watch and counted the number of steps to complete the 5-m walking course. All subjects wore a gait belt during the walking tests and were closely guarded by a research assistant for safety. There was no evidence in the literature regarding the influence of wearing the gait belt on gait performance in persons with PD. All subjects in the study wore the belt during both testing methods, thus minimizing any influence of the belt on the results.
After completing the two walk tests in the “OFF” medication state, the subjects were observed while they took their morning dose of their usual dopaminergic medication in the laboratory. Once the subjects reported that they felt “ON”, which was approximately 45 min to 1 h after taking the medication, the same neurologist obtained the UPDRS motor scores again. Then, the subjects followed the same walking protocol as they did in the “OFF” medication condition.
Verbal instruction for each walk test was given before the subject started walking. No instruction was given after the subject started walking in order to prevent any influence of verbal cueing on gait performance. The verbal instruction for the walking tests was “Walk down the mat/course at your usual, comfortable walking speed.” Subjects were instructed to start walking a few steps before reaching the GAITRite walkway or the 5-m overground testing course and again after finishing the walkway or the course, to allow for acceleration and deceleration.
Gait speed, cadence and stride length were studied because the three parameters could be manually calculated using the time and number of steps that were manually measured during the Non-Instrumented Walk Test. Gait speed (cm/s), cadence (steps/min) and average stride length (cm) during the GAITRite Test were recorded and correlated with the corresponding gait parameters measured during the Non-Instrumented Walk Test.
From the Non-Instrumented Walk Test, gait speed (centimeters per second) was calculated by dividing the 500-cm distance by the time in seconds to complete the walking course. Cadence was calculated by dividing the number of steps by the walking time to complete the 500-cm distance. Average stride length (centimeters per stride) was not directly measured. It was calculated by dividing the 500-cm distance by the number of steps to complete the course, and then multiplying by two.
Formulas used to calculate the gait parameters of the Non-Instrumented Walk Test were:
Gait speed (cm/s) = 500 cm/Time (s)
Cadence (steps/min) = (Number of steps × 60)/Time (s)
Stride length (cm) = (500 cm/Number of steps) × 2
Statistical analysis
Demographic data was descriptively summarized. All analysis was performed using SPSS version 19.0. The Intraclass Correlation Coefficient [ICC (3, 1)] was used to calculate the reliability of gait parameters measured by the Non-Instrumented Walk Test compared with those obtained by the GAITRite. Paired Student's t-tests were used to determine if significant differences existed between the means of the gait parameters measured by the GAITRite and the Non-Instrumented Walk Test. Parameters of interest were gait speed, cadence and stride length. Data collection was performed by the same personnel throughout the study. The significance level was set at p < 0.05.
Results
Subject characteristics
Our sample consisted of 21 men and nine women who were community-dwelling individuals with PD. Their mean age was 68.90 (9.28) years. The time since diagnosis was 8.75 (5.68) years. The means of the UPDRS motor score during the “OFF” and “ON” medication states were 29.97 (11.17) and 20.70 (8.34), respectively. The average HY stage was 2.45 (0.36). All subjects were receiving dopaminergic treatment (carbidopa/ levodopa or carbidopa/levodopa/entacapone). Twenty-three subjects usually walked without a walking device, three subjects walked with a cane and four subjects walked with a wheeled walker; however, all subjects were able to complete the walking tests without any assistive device.
Reliability of the GAITRite Test and the Non-Instrumented Walk Test
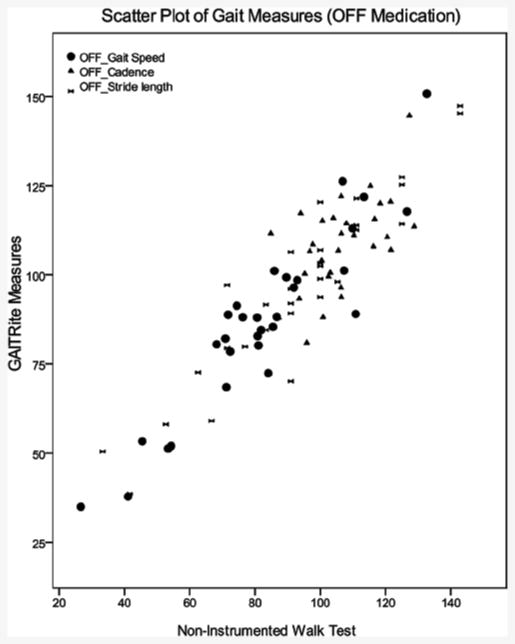
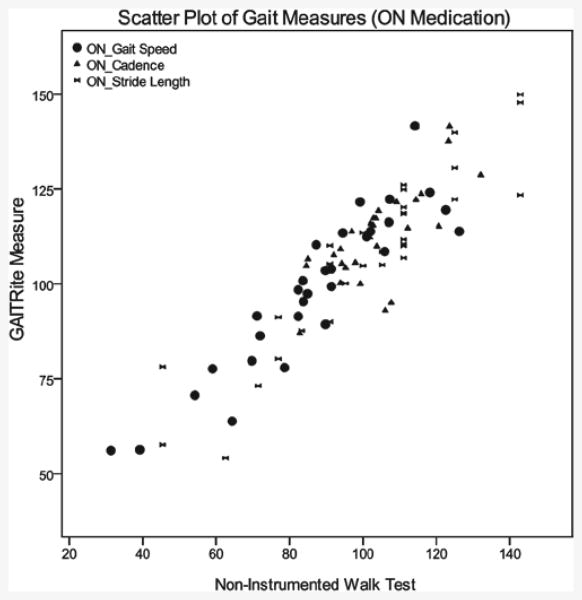
Based on the ICCs, gait speed and stride length from the Non-Instrumented Walk Test were highly correlated with the same measures from the GAITRite both “OFF” (gait speed, ICC = 0.96; stride length, ICC = 0.97) and “ON” medication states (gait speed, ICC = 0.96, stride length, ICC = 0.96). Cadence measured during the Non-Instrumented Walk Test was moderately correlated with cadence measured by the GAITRite during “OFF” medication testing (ICC = 0.72), but showed good correlation during “ON” medication testing (ICC = 0.86) (Table I). Scatter plot of the gait variables measured by the two methods were displayed in Figures 1 and 2.
Table I.
Intraclass correlation coefficient of gait parameters from GAITRite and Non-Instrumented Walk Tests While “OFF” and “ON” dopaminergic medication.
| N = 30 | ICC (3,1) | 95% CI |
|---|---|---|
| OFF medication testing | ||
| Gait speed (cm/s) | 0.96 | 0.92–0.98* |
| Cadence (step/min) | 0.72 | 0.41–0.87* |
| Stride length (cm) | 0.97 | 0.93–0.99* |
| ON medication testing | ||
| Gait speed (cm/s) | 0.96 | 0.91–0.98* |
| Cadence (step/min) | 0.86 | 0.69–0.93* |
| Stride length (cm) | 0.96 | 0.92–0.98* |
All significant levels p < 0.05.
Figure 1.
Scatter plot of gait measure during “OFF” medication.
Figure 2.
Scatter plot of gait measure during “ON” medication.
Comparison of mean gait parameters from the GAITRite and from the Non-Instrumented Walk Test during “OFF” and “ON” medication states
During “OFF” medication testing, gait speed was significantly faster as measured by the GAITRite compared to gait speed as measured during the Non-Instrumented Walk Test (Table II). There was no significant difference in cadence or stride length between the two methods of measurement (Table II). During “ON” medication testing, gait speed was faster, cadence was greater and stride length was longer as measured by the GAITRite compared with the Non-Instrumented Walk Test (Table II).
Table II.
Comparison of mean gait parameters from GAITRite and Non-Instrumented Walk Tests While “OFF” and “ON” dopaminergic medication.
| N = 30 | Non-Instrumented | ||
|---|---|---|---|
| GAITRite | Walk Test | p value | |
| OFF medication testing | |||
| Gait speed (cm/s) | 86.79 ± 25.44 | 82.47 ± 24.29 | 0.018 |
| Cadence (step/min) | 108.35 ± 12.83 | 106.43 ± 11.34 | 0.361 |
| Stride length (cm) | 96.53 ± 25.96 | 93.24 ± 26.47 | 0.062 |
| ON medication testing | |||
| Gait speed (cm/s) | 98.55 ± 20.90 | 86.81 ± 22.77 | <0.0005 |
| Cadence (step/min) | 111.69 ± 12.12 | 102.76 ± 12.22 | <0.0005 |
| Stride length (cm) | 107.34 ± 23.31 | 101.47 ± 25.10 | 0.002 |
Discussion
The aim of the study was to assess whether gait variables obtained from a manual timed test in individuals with PD would be comparable to those measured by the GAITRite during two medication states (“ON” and “OFF”). Therefore, we performed this study during poorest performance (“OFF” medication) and during peak performance (“ON” medication) to establish the correlation of the two methods of gait measure in the extremes of the medication states.
This study demonstrated several new findings. First our results demonstrated that gait speed and stride length as measured by the non-instrumented timed walk test were highly correlated with the corresponding gait parameters from the GAITRite in both medication states. Cadence measured from the two methods demonstrated only medium correlation in the “OFF” state, but fairly high correlation in the “ON” state.
Second, mean values of gait speed, cadence and stride length measured by the Non-Instrumented Walk Test were significantly lower than those measured by the GAITRite, especially during “ON” medication testing. The results indicated that a simple timed walk test might be an acceptable inexpensive quick evaluation in individuals with PD for both medication states. The timed walk test and the calculation can be used in routine clinical evaluation of gait in individuals with PD. However, clinicians should be cognizant of the underestimation of gait parameters from the timed walk test and the differences related to the medication status of the patients. The bias of the two methods is consistent since the ICCs were good even if the means were lower.
This underestimation of gait parameters suggests the presence of methodological bias in the gait parameters measured during the Non-Instrumented Walk Test (i.e. significant differences between mean values of gait speed, cadence and stride length during “ON” medication status, and gait speed during “OFF” medication status). Interestingly, more bias was found during the “ON” medication testing. This may occur because the speed is faster and the number of steps per minute is greater making it more difficult for the rater to accurately assess the parameters. This could be a concern in the clinical assessment of gait in persons with PD when comparing performance during different medication states.
A stopwatch used to measure walking time (i.e., from start to finish lines) required the tester to press the start button of the timer when the subject began his/her walking at the start line and press the stop button at the finish line, which might introduce potential error in temporal measures due to some latency in starting and stopping the stopwatch. The computerized, quantitative gait analysis system of the GAITRite may have eliminated the potential manual error and step counting error inherent in timed, Non-Instrumented Walk Tests, because the electronic sensors immediately received and transferred signals once the subject stepped onto the mat.
Most commercially available gait evaluation equipment is labor intensive, time consuming, expensive and technologically sophisticated. Paper imprint methods require testers to chalk or ink subjects' soles and heels to make an imprint as they walked along a paper walkway. Footfall imprints are subsequently measured with a measuring tape [2]. For the foot switch method, foot switches tethering the subject to a recording device are attached to the subject's heels to record footfalls electronically [3,11]. Three-dimensional motion analysis systems are complicated, require specific technical skills and excessive preparation time for attaching reflective markers, setting-up and calibrating multi-camera system [6].
These methods require tremendous effort and are too labor intensive to apply routinely in clinical settings, where a quick gait evaluation performed by one clinician is often preferred. In addition, some systems (i.e. 3-dimensional motion analysis system) provided extraneous data that might not be useful or meaningful for a clinical evaluation. The hand-held stopwatch and step counting used during the Non-Instrumented Walk Test in this study could be performed simply by one tester and provide reasonably reliable gait variables including gait speed, cadence and stride length. These three parameters are those most used clinically to evaluate the effect of a treatment, especially in persons with PD [12,13].
Based on our literature search, this is the first study to demonstrate the correlation between a manual timed test and step counting method of gait evaluation in individuals with PD during “OFF” and “ON” medication states. Gait measures from paper imprint methods, video-based analysis systems and foot switch methods were previously reported to be highly correlated with the GAITRite measures [5,11,14].
When performing mobility assessments for individuals with PD, it is important to perform them in both the “OFF” and “ON” medication phases, so that the full spectrum of impaired mobility can be documented. Rehabilitation interventions may be more effective if they are tailored to the patient's changing mobility status during different medication phases [15].
This gait evaluation can be a very useful adjunct to observational or subjective gait assessment in clinic, rehabilitation and community settings for individuals with PD. This simple and straightforward calculation as described above can be used for a quick gait evaluation and provides quantitative assessment to determine whether there are any changes from certain interventions, or to document gait impairment. However, clinicians should be cognizant that the manual method of gait measurement was less sensitive than the GAITRite. Our results showed that the three gait variables from the manual timed test method were significantly lower than those from the GAITRite.
Limitations
There are some limitations of the study to be addressed. Our sample consisted of individuals with diagnosed idiopathic PD with mild to moderate severity who reported either gait or balance impairment or falls as a result of PD. Their gait performance might be different from individuals with PD who do not have gait and balance impairments or who never fall.
Only one tester was involved in this study to minimize the variation of testing performance between raters. Therefore, we were unable to determine inter-rater reliability, and this might limit the generalizability of the findings.
Cadence calculated from the Non-Instrumented Walk Test during “OFF” medication status had only a moderate correlation with cadence measured by the GAITRite. Clinicians should be cautious when performing evaluations of cadence by this method.
Despite these limitations, we believe that our study provides quantitative evidence establishing the concurrent reliability of the Non-Instrumented Walk Test for gait evaluation in individuals with PD in both non-medicated and medicated states. Our results are useful and encourage the use of this gait measure clinically, which is quick and easy to administer in both clinical and community settings. However, if change over time is of interest, using the same method with the same tester and during the same medication state is important.
Conclusions
In summary, gait evaluation using a manually timed test together with step counting and a simple calculation of gait parameters could be incorporated into clinical evaluations to quantitate Parkinsonian gait, and might be adequately substituted for more sophisticated gait measurement systems, such as GAITRite or electronic footswitch systems.
Implications for Rehabilitation.
The Non-Instrumented Walk Test in individuals with PD is reliable.
Results supported the use of the measure. This simple walk test is quick and easy to administer in both clinical and community settings.
Acknowledgments
We thank Mr. Angel Fernandez and Steven P. Rivas for their assistance with data collection and the subjects for their time and effort.
Declaration of Interest: This work was supported by the National Institute for Neurological Disorders and Stroke, K12 HD055929 and the National Institute of Health, R01 HD051844.
References
- 1.Pedersen SW, Oberg B, Larsson LE, Lindval B. Gait analysis, isokinetic muscle strength measurement in patients with Parkinson's disease. Scand J Rehabil Med. 1997;29:67–74. [PubMed] [Google Scholar]
- 2.Sekiya N, Nagasaki H, Ito H, Furuna T. Optimal walking in terms of variability in step length. J Orthop Sports Phys Ther. 1997;26:266–272. doi: 10.2519/jospt.1997.26.5.266. [DOI] [PubMed] [Google Scholar]
- 3.Baker PA, Hewison SR. Gait recovery pattern of unilateral lower limb amputees during rehabilitation. Prosthet Orthot Int. 1990;14:80–84. doi: 10.3109/03093649009080327. [DOI] [PubMed] [Google Scholar]
- 4.Wall JC, Scarbrough J. Use of a multimemory stopwatch to measure the temporal gait parameters. J Orthop Sports Phys Ther. 1997;25:277–281. doi: 10.2519/jospt.1997.25.4.277. [DOI] [PubMed] [Google Scholar]
- 5.Cutlip RG, Mancinelli C, Huber F, DiPasquale J. Evaluation of an instrumented walkway for measurement of the kinematic parameters of gait. Gait Posture. 2000;12:134–138. doi: 10.1016/s0966-6362(00)00062-x. [DOI] [PubMed] [Google Scholar]
- 6.Mirek E, Rudzinska M, Szczudlik A. The assessment of gait disorders in patients with Parkinson's disease using the three-dimensional motion analysis system Vicon. Neurol Neurochir Pol. 2007;41:128–133. [PubMed] [Google Scholar]
- 7.Chien SL, Lin SZ, Liang CC, Soong YS, Lin SH, Hsin YL, Lee CW, Chen SY. The efficacy of quantitative gait analysis by the GAITRite system in evaluation of parkinsonian bradykinesia. Parkinsonism Relat Disord. 2006;12:438–442. doi: 10.1016/j.parkreldis.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Hoehn MM, Yahr MD. Parkinsonism: onset, progression and mortality. Neurology. 1967;17:427–442. doi: 10.1212/wnl.17.5.427. [DOI] [PubMed] [Google Scholar]
- 9.Oehlert ME, Hass SD, Freeman MR, Williams MD, Ryan JJ, Sumerall SW. The Neurobehavioral Cognitive Status Examination: accuracy of the “screen-metric” approach in a clinical sample. J Clin Psychol. 1997;53:733–737. doi: 10.1002/(sici)1097-4679(199711)53:7<733::aid-jclp11>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 10.Fahn S, Elton RL . Members of the UPDRS Development Committee. Unified Parkinson's Disease Rating Scale. In: Fahn S, Marsden CD, Calne DB, Goldstein M, editors. Recent Developments in Parkinson's Disease. Vol. 2. Florham Park: Macmillan Health Care Information; 1987. [Google Scholar]
- 11.Beauchet O, Herrmann FR, Grandjean R, Dubost V, Allali G. Concurrent validity of SMTEC footswitches system for the measurement of temporal gait parameters. Gait Posture. 2008;27:156–159. doi: 10.1016/j.gaitpost.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 12.Vokaer M, Azar NA, de Beyl DZ. Effects of levodopa on upper limb mobility and gait in Parkinson's disease. J Neurol Neurosurg Psychiatr. 2003;74:1304–1307. doi: 10.1136/jnnp.74.9.1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Sullivan SB. Parkinson's disease. In: O'Sullivan SB, Schmitz TJ, editors. Physical Rehabilitation. 5th. Philadelphia, PA: F.A. Davis Co.; 2007. p. 870. [Google Scholar]
- 14.McDonough AL, Batavia M, Chen FC, Kwon S, Ziai J. The validity and reliability of the GAITRite system's measurements: A preliminary evaluation. Arch Phys Med Rehabil. 2001;82:419–425. doi: 10.1053/apmr.2001.19778. [DOI] [PubMed] [Google Scholar]
- 15.Morris S, Morris ME, Iansek R. Reliability of measurements obtained with the Timed “Up & Go” test in people with Parkinson disease. Phys Ther. 2001;81:810–818. doi: 10.1093/ptj/81.2.810. [DOI] [PubMed] [Google Scholar]