Summary
Background
Magnetic resonance cholangiopancreatography is a relatively noninvasive technique of biliary and pancreatic duct imaging. MRCP technique utilizes T2-weighted sequences, in which bile is characterized by high signal intensity, whilst signal intensity of surrounding tissues is reduced.
The purpose of this publication was to assess the diagnostic value of magnetic resonance cholangiopancreatography in the diagnostics of biliary dilatation.
Material/Methods
MRCP examinations of 148 patients (48 men and 100 women; the average age was 56) performed on a 1.5T Achieva Philips device in the Provincial Hospital in Rzeszow between November 2011 and April 2013 were included in retrospective analysis. Examined group was divided into three subgroups: patients after cholecystectomy, patients with cholecystolithiasis and patients without gallbladder concretions. The definitive cause of biliary dilatation was determined mainly on the basis of MRCP and ECPW examinations, and, in individual cases, during intraoperative cholangiography and laparatomy.
Results
Signal loss corresponding to probable concretions was identified in 34 cases. In the group of patients with cholecystolithiasis the cause of biliary dilatation was usually (45%) cholelithiasis. MRCP image was typical in 4 out of 9 malignant cases. The cause of biliary dilatation was usually (20%) a neoplasm in the group of patients without gallstones. Benign causes of biliary dilatation, apart from cholelithiasis, were identified in 16 individuals, including 4 cases in which the diagnosis was identified using MRCP, whereas in the remaining 12 cases ECPW examination proved conclusive to the final diagnosis.
Conclusions
Magnetic resonance cholangiopancreatography enables reliable diagnosis of causes of biliary dilatation as long as they involve presence of gallbladder deposits and tumors. In benign causes of biliary dilatation, apart from cholelithiasis, MRCP picture is often atypical and therefore, the final identification of the cause of biliary dilatation is possible when this imagining method is combined with ERCP and additional tests.
MeSH Keywords: Cholangiopancreatography, Magnetic Resonance, Cholecystectomy, Dilatation
Background
Magnetic resonance choleangiopancreatography (MRCP) method is based on the concept of hydrography, as it visualizes the fluid contained in the biliary tract and pancreatic duct, which is why it does not require contrast. This technique utilizes T2-weighted images that generate high signal from free-flowing fluids (bile, fluid in the pancreatic duct) and low signal from fast-flowing fluid (blood within vessels) as well as the background (pancreatic and hepatic parenchyma) [1]. Although spatial resolution is usually limited, this examination usually suffices to establish the diagnosis and guide further management. MRCP may be combined with other MR sequences in various planes in order to ensure comprehensive evaluation of the liver, biliary tree and pancreas [2]. MRCP is safe and non-invasive and literature does not report complications after this examination. It may be performed in patients in poor general condition. It does not require anesthesia, which is important for people with various comorbidities. There is no exposure to ionizing radiation. However, it requires patient cooperation, which may be a drawback, particularly in a population of pediatric and elderly patients.
The goal of this publication is to establish the value of MRCP in the diagnostics of cholestasis and its causes among patients after cholecystectomy, with cholelithiasis and those without visible gallbladder deposits.
Material and Methods
Retrospective analysis was performed on the results of MRCP studies of 148 patients, including 100 women (67.5%) aged 6–90 years (mean age: 56.75 years) and 48 men (32.5%) aged 9–90 years (mean age: 55.69 years), performed between November 2011 and April 2013 at the Magnetic Resonance Facility of the No 2 Provincial Hospital in Rzeszow using a 1.5T Achieva Phillips device. Examinations were performed mostly without contrast using the following sequences: TSE/BH (T2 – ax. and cor.), FFE (T1 – ax. dual echo) FFE/e-THRIVE/BH (T1 – cor.) and sMRCP/3D (T2 – cor. and rad.). In three cases, a contrast medium was used. Clinical symptoms (jaundice, abdominal pain, vomiting) and ultrasound findings (presence of gallbladder deposits or bile duct dilatation) constituted indications for the procedure. Study group was divided into three subgroups: patients after cholecystectomy, patients with cholelithiasis and patients without gallbladder deposits. The final cause of biliary tract dilatation was established mainly based on MRCP and endoscopic retrograde choleangiopancreatography (ERCP) examinations as well as on intraoperative cholangiography and laparotomy in isolated cases, taking into consideration overall clinical picture and results of laboratory studies. Sensitivity (TPR – true positive rate), specificity (TNR – true negative rate) as well as positive predictive value (PPV) and negative predictive value (NPV) were calculated in order to assess the effectiveness of MRCP.
Results
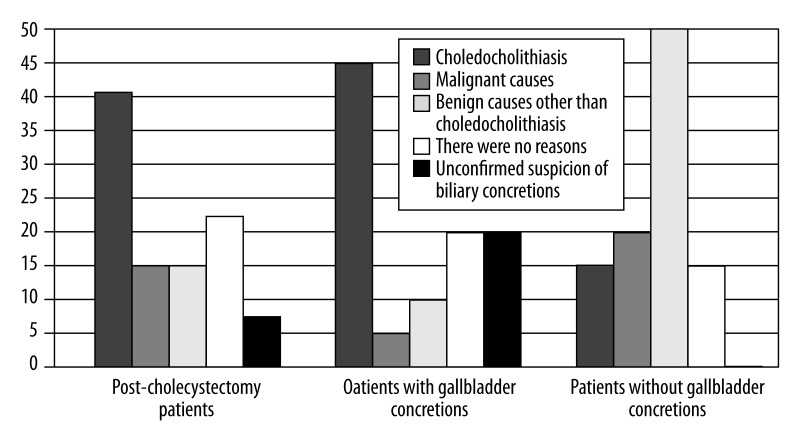
Study group included 48 patients after cholecystectomy, 55 patients with gallbladder stones and 45 patients without concretions. In the studied subgroups biliary tract dilatation was noted in 27 (56.2%), 20 (36.4%) and 20 (44.4%) subjects, respectively (Table 1). ERCP was performed in 28 patients with biliary tract dilatation (41%). In the remaining patients diagnosis was stated based on clinical picture, laboratory studies and other imaging examinations (ultrasound, computed tomography) or the cause of biliary duct dilatation was never found. Areas of signal loss raising suspicion of concretions were noted in 34 cases, while in 24 (70.6%) cases suspicion was confirmed (by ERCP in 20 cases and intraoperatively in 4 patients). The causes of biliary tree dilatation in the studied subgroups included concretions (a total of 23 cases confirmed in MRCP and ERCP) in 40.7%, 45% and 15% of cases, respectively (Figure 1). In the remaining cases (10 in total) where presence of concretions was suspected based on MRCP examinations, in 1 case suspected concretion turned out to be a malignant process, in 1 case biliary sludge was identified and in 1 one case presence of concretions was ruled out. In the remaining cases (7) ERCP was not performed for such reasons as: lack of patient consent, comorbidities or technical reasons. The most common (45%) cause of biliary tract dilatation in a subgroup of patients with biliary stones was choledocholithiasis (Figure 1). In patients with undilated biliary tract areas of signal loss demonstrated by MRCP suspected of consisting concretions were noted in 4 cases only, including 1 case where this diagnosis was ruled out and 1 confirmed case, while ERCP was not performed in 2 remaining cases. Malignant causes of biliary tract dilatation were identified in 9 (13.4%) people (1 pancreatic head tumor, 4 cases of neoplastic infiltration, 3 tumors of hepatic hilum, 1 carcinoma of the ampulla of Vater). MRCP picture was typical in 4 (44.4%) cases (Table 2). Malignancy was the most common (20%) cause of biliary tree dilatation in a subgroup of patients without cholelithiasis (Figure 1). Aside from choledocholithiasis, benign causes of biliary tract dilatation were identified in 16 (23.8) subjects (1 inflammatory tumor of pancreatic head, 5 cases of cholangitis, 1 gallbladder empyema and cholangitis, 1 case of Mirizzi syndrome, 1 case of dysfunction of the sphincter of Oddi, 1 autoimmune hepatitis, 1 primary sclerosing cholangitis, 2 cases of chronic pancreatitis, 1 case of dysfunction of the papilla of Vater, 1 biliary tree anomaly, 1 vascular band). Benign causes of biliary tract dilatation other than choledocholithiasis were identified using MRCP in 4 (25%) patients and included: chronic pancreatitis, cholecystitis and cholangitis, presence of vascular band modeling the common hepatic duct (CHD) and Mirizzi syndrome (Table 2). In the remaining 12 cases (75%) ERCP examination, laboratory studies and clinical picture played a decisive role in stating the diagnosis. Benign causes of biliary tract dilatation other than choledocholithiasis were most often (20%) diagnosed in a subgroup of patients without gallstone disease (Figure 1). No cause of biliary tract dilatation was found in 13 (19.4%) patients with biliary dilatation, mostly (22%) in a subgroup of patients who had undergone cholecystectomy in the past and in those cases ERCP was not performed for various reasons. Sensitivity and specificity as well as positive and negative predictive value of MRCP in the diagnostics of biliary tract dilatation are presented in Table 3.
Table 1.
Examined patients divided into subgroups, patients with dilated biliary tracts are distinguished.
| Patients after cholecystectomy | Patients with gallbladder stones | Patients without gallbladder stones | |
|---|---|---|---|
| Number of examined patients | 48 | 55 | 45 |
| Number of patients with bile duct dilatation | 27 (56.2 %) | 20 (36.4 %) | 20 (44.4 %) |
Figure 1.
Causes of biliary dilatation in the examined subgroups of patients.
Table 2.
Causes of bile duct dilatation.
| Choledocholithiasis | Malignancy | Benign causes other than choledocholithiasis | |
|---|---|---|---|
| Total number | 24 | 9 | 16 |
| Diagnostic MRCP picture | 24 (100%) | 4 (44.4 %) | 4 (25%) |
Table 3.
Diagnostic value of MRCP imaging in the diagnosis of the causes of biliary dilatation.
| Causes of bile tract dilatation | TP | FP | TN | FN | S | SPEC | PPV | NPV |
|---|---|---|---|---|---|---|---|---|
| Choledocholithiasis | 23 | 3 | 24 | 0 | 100% | 88.8% | 88.4% | 100.0% |
| Malignancy | 3 | 0 | 38 | 2 | 60% | 100.0% | 100.0% | 95.0% |
| Benign causes other than choledocholithiasis | 4 | 0 | 32 | 12 | 25% | 100.0% | 100.0% | 72.7% |
Results: TP – true positive; FP – false positive; TN – true negative; FN – false negative; S – sensitivity; SPEC – specificity; PPV – positive predictive value; NPV – negative predictive value.
Discussion
Biliary tree dilatation is demonstrated with abdominal ultrasound and, less often, in computed tomography (CT) of the abdomen in both symptomatic as well as asymptomatic patients and is one of the most common reasons for referral to ERCP or MRCP. Van Hoe noted an increase in common biliary tract diameter in people over 50 years of age and estimated it at about 1 mm/decade. According to this author, this phenomenon is caused by atrophy of elastic fibers within bile duct walls [3]. In MRCP images undilated intrahepatic biliary ducts are visualized up to the point of the second division into secondary ducts, the so-called subsegmental ducts. Visualizing further divisions is the evidence of anomaly and suggests bile stasis [4]. In the studied material bile duct dilatation was noted in 56.2% of patients after cholecystectomy, 36.4% patients with cholelithiasis and 44.4% of patients without gallstones (Table 1). Choledocholithiasis is one of the most common causes of bile duct dilatation. Choledocholithiasis occurs in 15% of gallstone disease cases, up to 20% of acute cholecystitis cases and in nearly 15% of patients after cholecystectomy (mainly open procedures). Primary choledocholithiasis constitutes about 5% of choledocholithiasis cases in Western countries and secondary choledocholithiasis – about 95% of cases [5]. Biliary stones are visualized in MR imaging as areas of signal loss/foci of signal attenuation in T2-weighted images surrounded by bile, which is characterized by increased signal intensity. However, they may exhibit higher signal in T2-weighted images due to presence of bile within the stone [2]. In the studied material areas of signal loss suspected in MRCP as concretions were demonstrated only in 34 cases, including 24 (70.6%) confirmed cases (20 in ERCP and 4 intraoperatively). In one case only concretion was identified in undilated biliary tract. The most common (45%) cause of biliary duct dilatation was choledocholithiasis in a subgroup of patients with gallbladder stones (Figure 1). Literature contains discrepancies regarding sensitivity and specificity of MRCP in detection of choledocholithiasis. Moon et al. determined sensitivity of MRCP at 80% and specificity at 83% [6]. Zidi et al. also assessed the role of MRCP in diagnosis of choledocholithiasis. Among 45 patients with bile stones MRCP visualized concretions in 28 cases only (sensitivity – 57%, specificity – 100%) [7]. Such low sensitivity could be due to the presence of minute concretions less than 3 mm in diameter. As also noted by other authors, small concretions may be overlooked in MRCP [6,8]. In their publication Calvo et al. emphasize that small concretions (3–5 mm) may pose a problem for those who evaluate MRCP, particularly if they become impacted [9]. On the other hand, according to Becker et al., MRCP allows for detection of stones as little as 2 mm in diameter, also in patients with undilated bile ducts [10]. In the analyzed cases the smallest concretion was 2 mm and the largest 30 mm in diameter. The majority of concretions detected in the biliary tract were 8–12 in diameter (Figure 2A, 2B). In our material sensitivity of MRCP in detection of concretions in dilated biliary tract was high and amounted to 100% with specificity of 88.8% and PPV and NPV values 88.4% and 100% respectively (Table 3). High sensitivity probably resulted from relatively easy visualization of areas of signal loss within dilated bile ducts. Single-shot fast spin-echo sequences in T2-weighted images were considered superior in detection of gallstones, as most gallstones are isointense in T1-weighted images [11]. In an in vitro study, Ukaji et al. demonstrated that hyperintense signal from biliary concretions in T1-weighted images is produced by the presence of metal ions with paramagnetic properties that shorten T1 relaxation time of water protons [12]. T2-weighted imaging indirectly detects gallstones through imaging of corresponding areas of signal loss, which is associated with several diagnostic pitfalls. Areas of intraductal signal loss caused by presence of neoplasms, thrombi or gas bubbles (pneumobilia) may mimic gallstones and are difficult to differentiate. On the other hand, small concretions located in peripapillary region may be omitted in T2-weighted imaging due to the absence of surrounding bile, thus lack of signal loss [13]. This is why Hong-Ming et al. recommend to routinely combine 3D fast spoiled gradient-echo technique in T1-weighted images and single-shot fast spin-echo in T2-weighted images for magnetic resonance imaging of gallstones [14].
Figure 2.
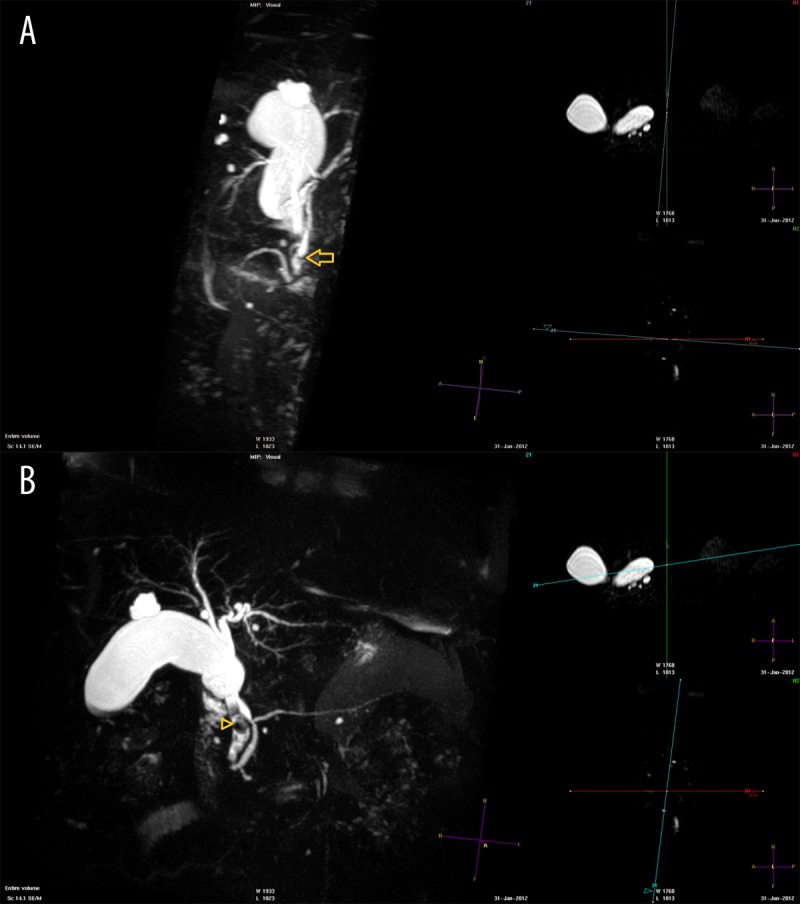
MRCP (A, B). Low origin of elongated cystic duct (arrow). Short common bile duct. Dilated common hepatic duct with signal loss equivalent to concretions (arrowhead). Liver cysts.
Malignant causes of dilatation (a total of 9 cases) in studied subgroups constituted 14.8%, 5% and 20% (Figure 1) of cases, respectively. MRCP picture unequivocally corresponded to malignant etiology in 4 cases (Table 2) (pancreatic head tumor, two tumors of hepatic hilum and infiltration of common bile duct). Contrast medium was administered in three of these four studies. Contrast medium was not used in any of the five remaining cases of biliary tract dilatation due to malignancy. In three cases of malignancy MRCP raised only a suspicion of a neoplastic process, which was later confirmed. MRCP image unequivocally corresponded to a malignant cause in another 4 cases (Table 2) (pancreatic head tumor, 2 tumors of hepatic hilum and common bile duct infiltration). Typical features of pancreatic head tumor noted in MRCP include sudden obstruction of the lumen of intrapancreatic segment of common bile duct and a “double duct sign” related to concomitant dilatation of the pancreatic duct. Obstructed or narrowed segment is usually of medium length, has irregular margins and transverse sequences demonstrate a presence of a pathological mass within pancreatic head, weakly hyperintense in T2-weighted images and strongly hypointense in T1-weighted images following intravenous administration of contrast medium [3,11]. In the studied material pancreatic head tumor was visible as a poorly demarcated area with somewhat heterogeneous and slightly increased signal in T2-weighted images. Pancreatic duct was 1.5 mm in diameter and modeled into an arch from the anterior side. Common hepatic duct was dilated to 13.5 mm. Common biliary duct was narrowed to 2 mm. In the peripheral form of intrahepatic cholangiocarcinoma MRCP picture demonstrates segmental obstruction or narrowing of duct lumen, presence of intraductal mass presenting as loss of signal within the lumen, proximal ductal dilatation away from the infiltrated site. Adjuvant gradient echo T1-weighted sequences with contrast demonstrate signal enhancement following intravenous administration of contrast medium (low tumor signal in overview T1-weighted sequences compared to normal liver parenchyma), central changes persisting also in the delayed phase [3,15,16]. Extrahepatic form of cholangiocarcinoma usually develops from the middle part of common bile duct. Signal from the infiltration is usually weakly hyperintense in T2-weighted images. Above the lesion biliary tree dilatation is observed. Klatskin tumor usually develops from the proximal part of common hepatic duct. In MRCP projection sequences we observe segmental duct narrowing, usually 1–3 cm in diameter, with smooth or irregular internal margins. There are often areas of signal loss within duct lumen. Transverse images show a high-signal (well demarcated forms with high mucin content) or intermediate-signal mass (fibrous forms) within liver hilum. In adjuvant sequences we observe heterogeneous signal enhancement after intravenous administration of contrast with dominance in the delayed phase [17]. There were 3 cases of Klatskin tumor in the studied material. The picture was typical in two cases. In the first case MRI picture was concordant with the above description (Figure 3A, 3B), while ERCP showed a tight, organic narrowing at the level of common bile duct and common hepatic duct. In the second case MRCP showed dilatation of extra- and intrahepatic biliary tracts and loss of lumen signal from the confluence of right and left hepatic duct. In case of a tumor of the liver hilum and carcinoma of the papilla of Vater MRCP examination, laboratory studies and ERCP did not unequivocally indicate a malignant cause of dilatation, which was identified in later studies. In the first one of these cases MRI showed only slight common hepatic duct dilatation and loss of signal from the proximal part of common biliary duct, which was related to the presence of post-cholecystectomy clips. CT image was unequivocal in this case, while ERCP demonstrated biliary duct obstruction at the level of cystic duct stump. In the end (intraoperatively), tumor of liver hilum was diagnosed. In case of carcinoma of papilla of Vater MRCP showed slight dilatation of main stems of intrahepatic bile ducts, extrahepatic bile ducts and pancreatic duct (Figure 4). However, the examination was performed after evacuation of concretions and bile duct dilatation was thought to be related to recent procedure. Further CT study prompted a suspicion of obstruction at the level of papilla of Vater, which was confirmed by ERCP examination (egzophytic lesion within the papilla). Sensitivity of MRCP in detection of malignant causes of biliary tract dilatation in the studied material amounted to 60% with specificity of 100% (Table 3). Relatively low sensitivity could be due to lack of contrast administration in most of these examinations (6/9).
Figure 3.
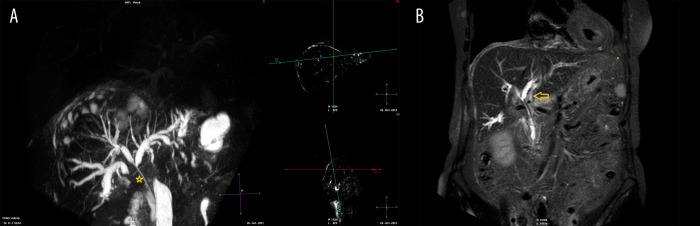
MRI. (A) MRCP. (B) T2-weighted image, coronal plane. Tumor of hepatic hilum. Prosthesis in the biliary tract. Dilated intra- and extrahepatic biliary ducts. Lack of signal in the distal sections of intrahepatic biliary tract, common hepatic duct as well as the proximal part of common bile duct (asterisk). A nondemarcated area of neoplastic infiltration around the prosthesis, within hepatic hilum and in the adjacent liver parenchyma (arrow).
Figure 4.
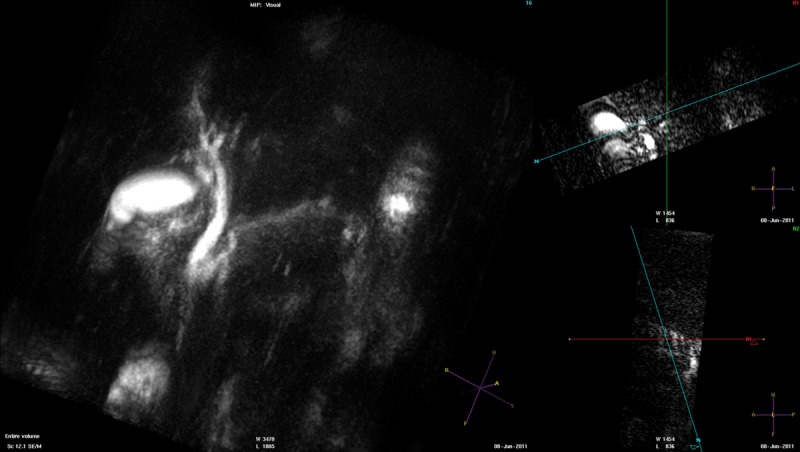
MRCP. Carcinoma of the ampulla of Vater. Dilated intra- and extrahepatic biliary tract as well as pancreatic duct.
Benign causes of biliary tract dilatation other than choledocholithiasis (16 cases altogether) constituted respectively 14.8%, 10% and 50% of the study subgroups (Figure 1). In bacterial cholangitis we observe only slight dilatation of bile tracts in the initial phase of illness, while irregular margins of external duct walls, loss of lumen signal due to the presence of biliary stones, sludge or pus as well as intrahepatic abscesses (irregular areas with signal similar to bile) communicating with the biliary tree are visualized at later stages [4]. In the studied material such picture was not observed in MRCP examination. No case of cholangitis was unequivocally identified based on MRCP examination. These studies were performed without administration of contrast. On the other hand, in cases of bile duct dilatation due to chronic pancreatitis, cholecystitis and cholangitis, as well as presence of a vascular band modeling common hepatic duct and Mirizi syndrome MRCP was typical in our material (4 cases) (Table 2). MRI examination visualized significantly enlarged, kinked gallbladder with unthickened wall and dilated main intrahepatic biliary stems. However, common biliary and common hepatic ducts were not visualized (Figure 5). In cholelithiasis and cholangitis (confirmed intraoperatively) MRCP examination showed irregular thickening of gallbladder wall with numerous areas of signal loss typical of concretions and an irregular fluid collection constricting and modeling the duodenum, as well as dilated intrahepatic bile ducts. The following features suggest fibrotic changes in MRCP examinations: short segment of stenosis in the biliary duct, smooth margins of the stricture and absence of pathological masses near the stenotic segment in transverse images [15]. In 4 cases of postinflammatory scarring that caused biliary tract dilatation MRCP picture was uncharacteristic, as it was in the remaining 8 cases (1 inflammatory tumor of pancreatic head (Figure 6A, 6B), 1 cholangitis, 1 dysfunction of sphincter of Oddi, 1 autoimmune hepatitis, 1 case of primary sclerosing cholangitis, 1 chronic pancreatitis, 1 case of dysfunction of papilla of Vater, 1 bile duct anomaly). ERCP examination and other (laboratory and imaging) studies proved to be complementary to the final diagnosis. In case of sphincter of Oddi dysfunction, which was demonstrated in ERCP examination and was supported by overall clinical picture, MRCP examination showed dilatation of extrahepatic bile tracts and narrowing of proximal common bile duct without pancreatic duct dilatation. The picture was similar in dysfunction of papilla of Vater caused by its anatomical location within a recess (Figure 7A, 7B). Sensitivity of MRCP in detection of benign causes of biliary tract dilatation other than choledocholithiasis in the studied material was low and amounted to 25% with specificity of 100% (Table 3).
Figure 5.
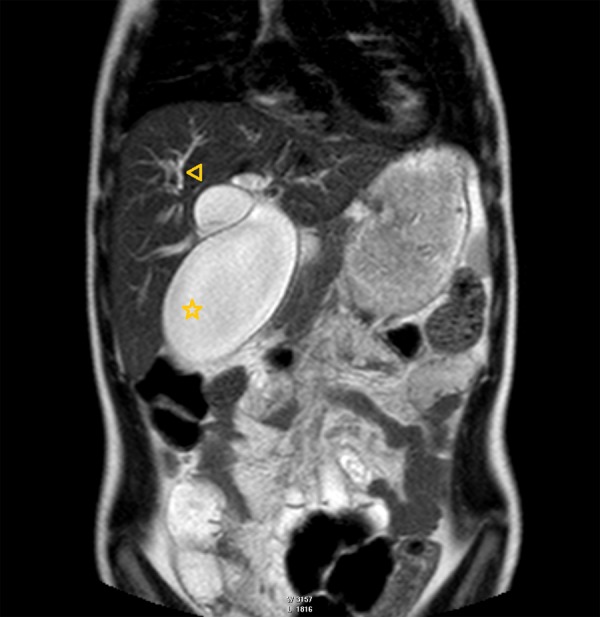
MRI. T2-weighted image, frontal plane. Mirizzi syndrome. Markedly enlarged, kinked gallbladder (asterisk). Main intrahepatic biliary trunks dilated (arrowhead).
Figure 6.
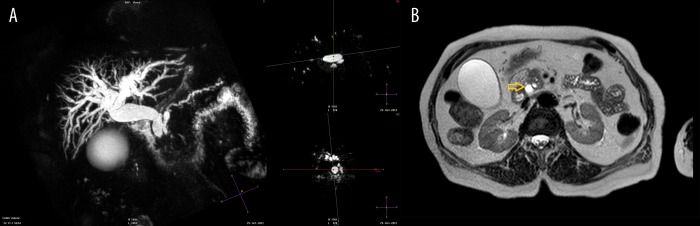
MRI. (A) MRCP. (B) T2-weighted image, transverse plane. Inflammatory tumor of the head of pancreas. Dilated intra- and extrahepatic biliary tract (arrow). Irregularly enlarged pancreatic duct with dilated secondary ducts.
Figure 7.
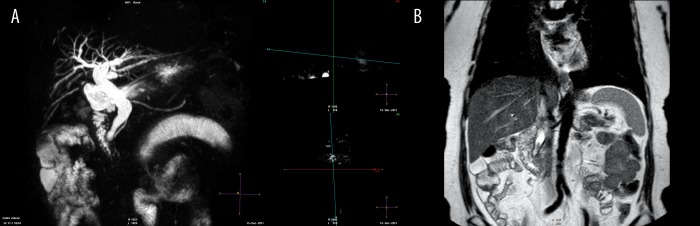
MRI. (A) MRCP. (B) T2-weighted image, coronal plane. Dysfunction of the ampulla of Vater due to its anatomical location – ampullary diverticulum. Dilated intra- and extrahepatic biliary tract. Pancreatic duct not dilated.
Conclusions
The majority of areas of signal loss suspicious of concretions demonstrated in MRCP were confirmed by ERCP.
In case of cholecystectomy patients with biliary tract dilatation, particularly with gallstones, MRCP together with basic MRI sequences without contrast administration appear to be sufficient to determine the cause of bile duct dilatation.
In patients without cholelithiasis and with bile duct dilatation broadening the MRCP diagnostics to include additional sequences and contrast administration seems reasonable.
If malignant cause of bile duct dilatation is not revealed in MRCP examination, ERCP should be the next step in establishing proper diagnosis.
References
- 1.Herman-Sucharska I, Urbanik A. Cholangiopankreatografia rezonansu magnetycznego – nowa metoda diagnostyczna w schorzeniach drzewa żółciowo-trzustkowego. Gastroenterol Pol. 2001;8:373–77. [in Polish] [Google Scholar]
- 2.Federle MP. Drogi żółciowe-wprowadzenie. In: Federle MP, Jeffrey RB, Woodword PJ, et al., editors. Diagnostyka obrazowa. Jama brzuszna. III-2. MediPage; Warszawa: 2013. pp. 2–5. [in Polish] [Google Scholar]
- 3.Van Hoe L, Vanbeckevoort D, Van Steenbergen W. Atlas of cross-sectional and projective MR cholangio-pancreatography. Springer-Verlag; Berlin Heidelberg: 2006. pp. 56–410. [Google Scholar]
- 4.Herman-Sucharska I, Urbanik A, Karcz D, et al. Biliary stenosis in the radiologist’s eyes: A review. Pol J Radiol. 2006;71(3):103–19. [Google Scholar]
- 5.Serafin Z, Lasek W. Kamica dróg żółciowych. In: Leszczyński S, Pilch-Kowalczyk J, editors. Diagnostyka Obrazowa. Układ Trawienny. Wydawnictwo Lekarskie PZWL; Warszawa: 2012. pp. 477–80. [in Polish] [Google Scholar]
- 6.Moon JH, Cho YD, Cha SW, et al. The Detection of Bile Duct Stones in Suspected Biliary Pancreatitis: comparison of MRCP, ERCP and Intraductal US. Am J Gastroenterol. 2005;100:1051–57. doi: 10.1111/j.1572-0241.2005.41057.x. [DOI] [PubMed] [Google Scholar]
- 7.Zidi SH, Prat F, Le Guen O, et al. Use of magnetic resonance cholangiography in the diagnosis of choledocholithiasis: prospective comparison with a reference imaging method. Gut. 1999;44:118–22. doi: 10.1136/gut.44.1.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fulcher AS. Magnetic resonance cholangiopancreatography: is it becoming the study of choice for evaluating obstructive jaundice? J Clin Gastroenterol. 2004;38:887–90. doi: 10.1097/00004836-200411000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Calvo MM, Bujanda L, Calderon A, et al. Role of magnetic resonance cholangiopancreatography in patients with suspected choledocholithiasis. Mayo Clin Proc. 2002;77:422–28. doi: 10.4065/77.5.422. [DOI] [PubMed] [Google Scholar]
- 10.Becker CD, Grossholz M, Becker M, et al. Choledocholithiasis and bile duct stenosis: diagnostic accuracy of MR cholangiopancreatography. Radiology. 1997;205:523–30. doi: 10.1148/radiology.205.2.9356639. [DOI] [PubMed] [Google Scholar]
- 11.Chan YL, Lam WW, Metreweli C, et al. Detectability and appearance of bile duct calculus on MR imaging of the abdomen using axial T1- and T2-weighted sequences. Clin Radiol. 1997;52:351–55. doi: 10.1016/s0009-9260(97)80129-8. [DOI] [PubMed] [Google Scholar]
- 12.Ukaji M, Ebara M, Tsuchiya Y, et al. Diagnosis of gallstone composition in magnetic resonance imaging in vitro analysis. Eur J Radiol. 2002;41:49–56. doi: 10.1016/s0720-048x(01)00420-x. [DOI] [PubMed] [Google Scholar]
- 13.Baillie J, Paulson EK, Vitellas KM. Biliary imaging: a review. Gastroenterology. 2003;124:1686–99. doi: 10.1016/s0016-5085(03)00390-1. [DOI] [PubMed] [Google Scholar]
- 14.Hong-Ming T, Xi-Zhang L, Chiung-Yu C, et al. MRI of gallstones with different compositions. Am J Roentgenol. 2004;182:1513–19. doi: 10.2214/ajr.182.6.1821513. [DOI] [PubMed] [Google Scholar]
- 15.Herman-Sucharska I. Praca doktorska po tytułem: Przydatność cholangiopankreatografii rezonansu magnetycznego w nowoczesnej diagnostyce obrazowej i kompleksowe opracowanie symptomatologii MR schorzeń układu żółciowego. Biblioteka Jagiellońska, Główna Biblioteka Medyczna; Krakó: 2000. [in Polish] [Google Scholar]
- 16.Van Beers BE, Gallez B, Pringot J. Contrast-enhanced MR imaging of the liver. Radiology. 1997;203(2):297–306. doi: 10.1148/radiology.203.2.9114076. [DOI] [PubMed] [Google Scholar]
- 17.Guthrie JA, Ward J, Robinson PJ. Hilar cholangiocarcinomas: T2-weighted spin echo and gadolinium-enhanced FLASH MR imaging. Radiology. 1996;201:347–51. doi: 10.1148/radiology.201.2.8888221. [DOI] [PubMed] [Google Scholar]