Abstract
Objectives
Most pregnant women in Burkina Faso are iron deficient and many are anemic. This study assessed women’s understanding of anemia and the role of iron in preventing and treating this condition.
Methods
A qualitative study was conducted within a randomized controlled trial of weekly iron supplementation in a rural malaria endemic area. Focus groups with women of similar age, parity, and marital status took place in 12 of 24 study villages. Two additional focus groups were conducted with female field workers. Tape-recorded transcripts were translated into French and analyzed using Framework analysis.
Results
Anemia, for which no Mooré term or traditional treatment for anemia was evident, was described in terms of blood volume. Moderate blood loss (diminished blood) could be easily replaced by eating well and was not considered serious. Massive blood loss (finished blood) was a rare, life-threatening illness. Iron tablets could increase blood volume and help women withstand massive blood loss at delivery, but for the latter, transfusion was indicated. Women had no knowledge of iron’s role and did not readily concede that iron supplements contained elemental iron. Neither adolescents nor field workers were convinced of the benefits of supplementing non-pregnant adolescents, who were incorrectly considered to be at low risk of anemia.
Conclusions
Young women’s knowledge of anemia did not provide an adequate explanatory framework to motivate anemia prevention. Improving information on the role of iron is especially important for adolescent girls who may be incorrectly considered at low risk of anemia as they have not yet experienced pregnancy.
Keywords: adolescents, perceptions, Burkina Faso, anemia, malaria, iron, iron supplementation
Introduction
Over half of all pregnant women in Africa, and more than two-thirds of pregnant women in Burkina Faso, are anemic [1]. Approaches to reduce iron deficiency include iron fortification of food, nutritional education, and treatment of geo-helminths and intestinal worm infestation [2–4]. Many causes of anemia are due to iron deficiency and pregnant women have traditionally been provided with daily iron and folic acid (IFA) tablets as part of routine antenatal care [5]. The World Health Organization (WHO) also advocates IFA supplementation for menstruating women in settings where the prevalence of anemia is above 20% [6]. This recommendation includes adolescent girls as adolescence may be the optimal time to build iron stores in readiness for pregnancy [7].
Daily IFA supplements are effective at improving the iron status of pregnant women [8] and, among non-pregnant Bangladeshi women, a nine month regimen of daily IFA improved iron stores [9]. Daily IFA, however, provides more iron than is recommended for women who are already iron replete [8] and could increase their infection risk in countries with a high prevalence of endemic infections such as malaria [10]. Such risks might be lessened by reducing the amount of iron through less frequent supplementation (the same dose given one to three times weekly). Among pregnant women, o Cochrane review reported that levels of hemoglobin concentration and iron deficiency following intermittent supplementation were not significantly different from a daily regimen [11]. Furthermore, pregnant women receiving intermittent iron were less likely to report side effects such as nausea or constipation and fewer developed high hemoglobin levels (>16 g/dl) during mid and late gestation. The data on the effectiveness, acceptability, and safety of intermittent supplementation of non-pregnant women is less clear. Another Cochrane review reported that, compared to daily supplementation, non-pregnant women receiving intermittent supplementation generally achieved similar hemoglobin concentrations, but presented with anemia more frequently [12]. Information on disease outcomes, adherence, and side effects was lacking.
Adherence to IFA is an important issue and has been difficult to achieve outside of clinical trials [13–22], not least because of the many operational problems that affect programmatic delivery. Women may also not like taking iron tablets because of gastro-intestinal side effects caused by daily iron [19]. Women who are not averse to iron tablets often do not consume the recommended amounts, which must raise the question of whether they are very concerned about their risk of anemia [13]. Anemia may be viewed as a nonurgent maternal health problem compared with other serious incapacitating illnesses with the result that non-adherence to the recommended regime seems unimportant [23]. Such lack of concern could also reflect a limited understanding of anemia and the important role of iron. Recent recommendations therefore encourage health providers to improve nutritional counselling [22].
To ensure that the health information provided to women is effective, some comprehension of how anemia is viewed in the community is required. As part of a large randomized controlled trial (RCT) of long-term (up to 18 months) weekly iron supplementation, a qualitative sub-study was conducted to assess rural Burkinabé women’s understanding of anemia and its treatment. Focus groups were conducted to determine whether, in light of their views on the causes of anemia, women viewed iron supplements as an appropriate intervention. Such information was important in terms of the research, as well as for any future anemia prevention programme requiring long-term weekly supplements for non-pregnant women.
Methods
Summary of the iron supplementation randomized trial
The RCT, including this qualitative research, was approved by the national Ethical Committee for Health Research and the Institutional Ethical Committee of Centre Muraz in Burkina Faso, and the Ethical Committees of the Liverpool School of Tropical Medicine and the University Hospital Antwerp. The RCT was conducted in Nanoro, situated 85 km from Ouagadougou, the capital city of Burkina Faso. Malaria was holoendemic with a high annual inoculation rate of infective bites. The primary objective of the RCT was to assess the safety and efficacy of weekly IFA supplementation in young women of child-bearing age living in a highly malarious area of Africa. For the main trial approximately 1700 young women (median age 16 years) were enrolled prior to their first pregnancy between April and August 2011 in 24 study villages [24]. At enrollment women were allocated to receive weekly either 60 mg iron and 2.8 mg folic acid (intervention arm) or 2.8 mg folic acid (control arm). Randomization was double blind. Supplements were given under the observation of field workers during weekly home visits. Women who remained non-pregnant continued weekly IFA for 18 months. Those who became pregnant continued weekly IFA until their first antenatal visit by the study team, after which they received daily IFA in accordance with routine antenatal care guidelines. Field workers continued weekly home visits to monitor adherence to daily IFA supplements till delivery.
The district of Nanoro was one of five districts in the centre-west health region and comprised a district hospital and 16 peripheral health centres. A demographic surveillance system covering 24 villages was set up in Nanoro in 2009 and provided the framework for study recruitment [25]. This rural population, which was reliant on subsistence farming and cattle husbandry, comprised three main ethnic groups and the predominant Mossi population was very hierarchic [23]. The local language was Mooré and the official language was French. The literacy rate was low in both men and women (about 23%). Early marriage was common, with 62% of young women aged 20–24 years being married by age 18 years [26].
Participants for the qualitative study
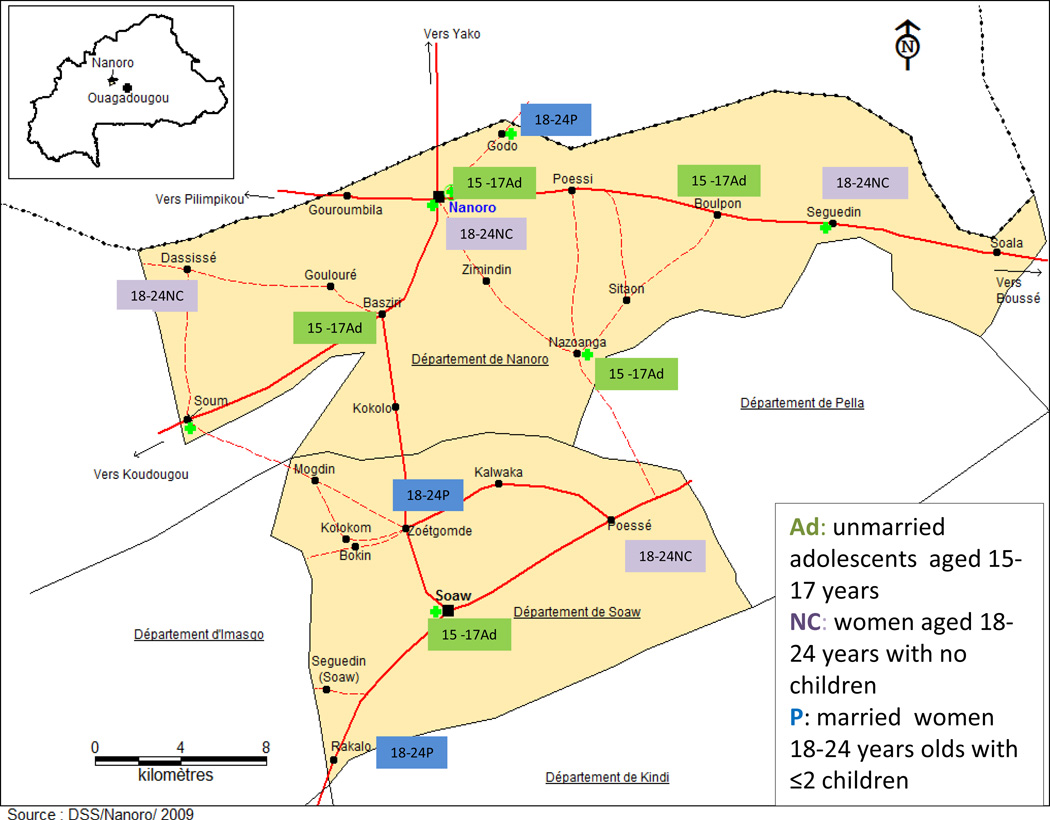
For our qualitative study there was no fixed sample size. Conducting focus groups (FG) in 12 of the study villages, which represented 50% of the sample, was judged to be adequate to elicit a representative sample of women’s views on the causes and treatment of anemia. To ensure that young women of different ages, parity and marital status were included and could readily express their views with peers of comparable status, the groups (referred to as parity groups) were constituted as follows: never-pregnant adolescents aged 15–17 years (married or unmarried) in five villages, young nulliparous women (usually married) aged 18–24 years in four different villages, and married parous women (one or two children) in three other villages. Age and parity were also characteristics likely to affect interest in, and experience of, iron supplementation. Villages were selected to ensure that FG with different parity groups were distributed in terms of distance across the study area (see Figure 1). In each village women were recruited by the local field worker who approached women on the basis of the inclusion criteria. Some of the adolescent girls attended school (notably the 15–17 year olds in the Nanoro FG), but most participants had left school early because their families could not pay fees or they had failed their exams. Parous women were not participants in the RCT, but were included in the FG. Nulliparous women were invited to take part in the RCT but field workers did not know to which trial arm any participant belonged. The field workers recruited a group of approximately 10–12 women in each of the 12 villages.
Figure 1.
Map of study area and sites where FG were conducted.
Two FG were conducted with field workers at the trial offices in Nanoro and included one of the two field workers allocated to each of the 24 study villages. Field workers, who were literate, had a primary education and were often recommended by village elders. The research team trained field workers to provide the iron/folic acid supplement at weekly home visits to women. Due to their close contact with women in the trial and their residence in the study area, field workers were very aware of community views. Information about anemia and need for the trial (read to women at recruitment and for the focus groups) is shown in Box 1. Expanded information was provided at community outreach sessions prior to the trial when village chiefs, elders and women’s groups were invited to listen and to ask questions.
Box 1 Facts provided to individual women about the need for iron supplements.
We are conducting this study to better understand anemia and malaria. Both are frequent illnesses in Burkina Faso, particularly among pregnant women. Blood is very important for health. It takes food to the different parts of the body. To make blood, the body needs iron which is found in certain foods. When a person is anemic, the blood becomes weak and cannot, for this reason, do its work correctly. Young girls are often anemic when they start menstruating and lose blood. Pregnant women are often anemic because their baby needs blood. This is why, at antenatal visits, mothers have their blood tested and are recommended to take iron tablets.
In this study we wish to give iron to young women who have never been pregnant. This is to prevent anemia and also, should they then become pregnant, they and their babies will be in better health. But it is possible that in taking iron, there may be more malaria (and other infections). That is why we are giving the iron within a study in which women will be followed up every week.
Data collection and analysis
Most FG took place before or during enrollment for the RCT, before women had begun supplementation. Women were called to a quiet location in the village and, following more detailed explanation of the objectives of the FG, individual consent and permission for the sessions to be tape-recorded were requested. FG were conducted in Mooré by a sociologist (AC) who was trained by LB. SG (the trial co-ordinator) and LB attended some of the FG for supervision and on these occasions, some of the discussions were conducted in French. The same topic guide was used for all groups. Folic acid was not discussed as it was not routinely given pre-conceptually and, although provided with iron to pregnant women, was not differentiated from iron during antenatal visits. Time was reserved at the end of the FG to answer questions and some field workers asked about folate. Saturation was deemed to have been achieved after 12 sessions when FGs with the three parity groups had been completed and initial familiarisation with the data indicated that few new concepts were emerging.
The interviews were transcribed by AC into French, checked by SG then sent to LB for preliminary manual coding. The transcripts were analysed using framework analysis, which has been specifically developed for applied or policy relevant research and ensures systematic analysis of themes across transcripts [27]. The analysis focused on women’s understanding of the causes and treatment of anemia and the importance women attached to anemia prevention. The main themes were determined a priori and were covered by the topic guide. Subthemes were defined in relation to the main themes and from issues raised by participants, as summarised in Table 1. This framework was applied to all the data and coding allowed related issues to be assigned to appropriate sub-themes within the framework, accompanied by short summaries synthesizing the data. The parity groups were each analysed separately and compared. Differences between parity groups and field workers were explored. The framework was discussed and finalized at a meeting in Burkina Faso with AC, when translation issues and meaning of local terms were also addressed. Associations between themes were explored to provide a descriptive analysis that could be used to provide immediate insight into women’s understanding of the trial and for feedback to the field team. Selected quotations were translated into English to illustrate some of the main themes and the group from which the comments originated.
Table 1.
Summary of themes and sub-themes arising from the FG topic guide
| Theme | Sub-themes |
|---|---|
| Knowledge of anemia | Local names Types Causes Malaria-associated Examples of known cases |
| Knowledge of blood | Source Disorders Quantity Role Cultural sensitivities |
| Knowledge of iron | Source of iron generally Source of iron in body Function of iron Importance of iron for women |
| Treatment of anemia | Personal experience of anemia Known cases of blood transfusion Content of iron tablets Acceptability of iron supplements Traditional treatments |
| Importance of anemia to pregnant women | Causes of anemia during pregnancy Main fears of pregnancy |
| Importance of anemia to non-pregnant women | Family’s prioritization of menstrual problems Ability to discuss menstrual problems |
Results
Views were relatively homogeneous across groups, with the main differences based on the level of detail provided. This probably reflected the fact that all the women in the parity groups were quite young (15–24 years). The youngest girls, whether married or unmarried, were less familiar with the medical concept of anemia although some biological aspects were familiar to those who were still in school. More detailed responses were given by the relatively older, parous women who had attended antenatal care and were more aware of the experiences of women in the wider community. Field workers, some of whom were older than participants, were able to provide more factual details, reflecting their training for the RCT.
1. Perceptions of blood, anemia and iron
a) Blood – general biological facts
Most participants knew that blood travels through veins, comes through the heart and is found in the skin. Most of them were not able to say where blood originated. A handful of better informed individuals in the non-adolescent and field worker groups noted that blood was made in the bone marrow. They described white and red blood cells as providing resistance to infection and named a few blood disorders such as vitamin B12 deficiency. Women found it difficult to estimate blood volume, and guesses varied from less than two litres to more than five. One woman described this as “everyone has blood but not in the same quantity.” [P3] With some exceptions, the view prevailed that men had more blood than women, who lost blood at menses and delivery, ate less well than men, and worked harder.
b) Cultural attributes ascribed to blood
In all groups blood was described as the key to good health because, “blood prevents sickness overwhelming you; you need strength, the strength of blood.” [Ad1] The amount of blood was critical as, “if there is not much blood in the body, it cannot circulate in all parts of the body and maintain health.” [P1] It also affected prevention and recovery from illness because, “if you have a lot of blood you can avoid many illnesses.” [FW1] Losing blood was associated with weakness and loss of power and traditionally the activities of menstruating women, who spoiled what they touched and reduced male strength, were restricted. Most of the taboos for menstruating women had been relaxed, but shedding of animal blood remained strictly a male task.
c) Notions of blood volume
The term “anemia” was rarely used, except by field workers who characterised it as “an illness due to a lack of red blood cells, but more accurately, during blood loss” [FW2]. This correlated with most women’s views of a medical condition characterised by blood being lost from the body. The local terms for lack of blood were “zi poore” and “zi kaalgo”. These terms translated respectively as “lacking or diminished blood” and “finished blood” but neither term was well defined. For example,
The blood is finished, but it isn’t finished. That’s a lack of blood.” (P2)
Most women thought that, even in acute illness, a small amount of blood was always retained although, “it would not fill a small tumbler” (¼ litre) [Ad4]. Short-lived infections that were treated and minor causes of blood loss diminished the quantity of blood, but were not a major concern. Finished blood occurred when a large amount of blood had been lost, to the point of becoming a life-threatening illness. Such patients would be pale and have lost weight and might be dizzy, trembling, unable to stand, or unconscious. Finished blood was unanimously said to be a complication of severe infection – mainly malaria, although HIV and meningitis were mentioned. In malaria, blood was lost because mosquitoes sucked blood and malaria might lead to blood in the urine or nose bleeds. If slow to resolve, it imperceptibly diminished the blood because, “the illness causes fever all the time. Thus the blood can’t avoid becoming finished.” [P3]
Another cause of finished blood was massive blood loss, as might occur in a serious accident, or at delivery. Less clear were cases of excessive menstrual bleeding. Women were clear that normal menstruation was not a cause of anemia but they did not agree on what was “normal”, either in terms of bleeding days, or cycle length. Some considered that more frequent menses might lead to anemia. The field workers referred to a condition called “kaalgo”, translated as continuous blood loss, which could have indicated menorrhagia.
“Once you get this you have blood that flows and flows……once that gets you, it never finishes.” [FW1]
As a life-threatening illness, this type of blood loss was associated with anemia.
d) The role of iron
Iron’s contribution to the maintenance of blood and all living cells was completely unknown. Few knew the source of iron itself. Asked about blacksmith’s iron, one view was as follows:
“He goes out and buys it, but we don’t know where it comes from – white people invented it.” [Ad3]
All of the women had heard of iron tablets but none believed that iron tablets contained elemental iron. Overall, they were inclined to think that the tablets contained vitamins. They could not conceive how iron got into the tablets and contested whether either tablets or iron-rich food really contained a metal. They countered that tablets could not be “iron” because they could be crushed or dissolved. It became clear that women used the term “iron” symbolically, referring to the strengthening function of the medication, “because its strength is that of iron.” [FW1] Such strength might be required if, “the illness is unyielding, like iron.” [Ad3] The conclusion was, “there’s iron and iron.” [Ad4] In other words,
“The names can be the same but the things (ie iron and iron tablets) are not the same.” [P1]
After learning about the iron content, some women became concerned that taking iron would “perforate the intestines.” [Ad4] Parous women, who had experience of antenatal iron, pointed out that iron tablets came from the white man’s country and were not harmful. Anemia iself did not appear to be viewed as an “indigenous” illness and, although women did make infusions and soups, one of the field workers [FG1] stated:
“If you are ill and have an idea you are anemic and you go to a healer, he will simply deceive you. We know of no traditional treatment that can make blood come back.”
2. Replacing lost blood
a) Appropriate treatment
All groups concluded that normal menstruation, blood donation, and minor injuries in which blood loss occurred did not cause anemia because the blood “is removed and returned” [NC1] by eating well. All groups mentioned foods that should be eaten (particularly soup) or avoided, but the list was indiscriminate with regard to iron content, including fish [P1], wine [A5], beans [P2] a tree found in the Ivory Coast [FW1], boiled millet stubs and herbs, undercooked liver [FW2], and vitamins [NC3]. Finished blood could not be treated by eating well and would likely require hospitalization and blood transfusion. Indeed, “if blood has finished and you can’t buy it, you simply die.” [P2] Only one participant said she had experienced this level of blood loss, although most groups knew of children admitted to hospital for blood transfusions. Some field workers held the view that adolescents “are not often anemic” [FW1] – a view also held by adolescent girls themselves:
“It’s not a problem for them… they don’t think their blood can finish”. [Ad3]
b) Prevention of anemia
The iron tablets provided to pregnant women at the health centre were assumed to augment the volume of blood. Women were said to require more blood during pregnancy when the mother had to make extra blood for the baby and for delivery, when it would reduce the severity of any delivery hemorrhage. The priorities of the married, or about-to-be married women, were a safe pregnancy and a healthy baby and most accepted the advice of health workers that taking iron tablets contributed to improved maternal-child health outcomes, alongside other preventive measures such as reducing workload and eating nourishing foods. Iron tablets were not taken as a response to symptoms of anemia such as pallor or tiredness. Non-pregnant adolescent girls were willing to take iron supplements during the trial, not because they prevented anemia, but because they believed that “all their illness will finish. That’s what they think.” [FW1] Their parents also had this expectation:
“There are some families, when you arrive, they tell you that the tablets you are giving to their children have improved their health and they no longer get sick like before.” [FW1]
This view was reinforced by field workers [FW1] who told girls that the purpose of the tablet was, “to prevent anemia and also fight against malaria. If you have a lot of blood, you are less susceptible to malaria.”
DISCUSSION
This community’s understanding of anemia was based on literal interpretations of having “little” blood and few women felt at high risk of becoming anemic. An acknowledged need for supplementary dietary iron, mainly during pregnancy, was to some extent undermined by ignorance of why iron was important. The notion that giving iron increased blood volume and strengthened resistance to infection was positive, but this perception could be quickly undermined by infectious episodes, which are common in this area, particularly due to malaria.
Few studies discuss the detailed content of the educational messages used to describe anemia. Most research reports conclude that women need to be motivated to take iron-folate tablets [28] but focus on “benefit” messages such as “stronger” mothers and “healthier” babies and reinforce the belief that iron “increases the blood”. In a qualitative study across eight African and non-African countries, Galloway et al [29] noted that, cross-culturally, women described anemia in non-specific terms and referred to the same expected pregnancy benefits. 90% of women in those studies recognised anemia by its symptoms, described the condition as not having blood or having “weak blood”, and understood that consumption of iron tablets would “increase the blood.” Only in Honduras did respondents use the clinical term “anemia.” These messages are intended to motivate women, but as causality is barely addressed, women construct their own explanations, which are culturally specific and may either support or hinder adherence [30]. In Costa Rica, for example, mothers believed that untreated anemia in children would turn blood into water and induce leukemia [31]. These explanatory frameworks do not distinguish iron deficiency and infection as separate causes of anemia. Yet improving women’s knowledge is important. A study from Indonesia reported that maternal knowledge of anemia was associated with use of iron supplements by pregnant women and was protective against anemia in their children [32].
In Burkina Faso, where HIV prevalence is low (~2%), malaria is the most serious infectious cause of anemia. Malaria is also explained poorly to communities [33], but women attending antenatal care have been alerted to the dangers of pregnancy malaria and are encouraged to use bed nets and take intermittent preventive malaria treatment to prevent parasitemia. Schistosomiasis is uncommon locally and, although hookworm is endemic [34], women did not mention this geo-helminth as a cause of anemia. It is easy to see why malaria formed the basis of the local explanatory framework for anemia in this study and why iron deficiency anemia was seen as a relatively minor problem.
This study raises an interesting question as to what women should be told about iron in nature and in the human body. This aspect of the study was both novel and illuminating because it showed that rural women had no scientific concept of iron. Iron is a complicated topic and in health promotion the function of iron is rarely explained, as simple messages are preferred [35]. We found few reports in the literature on this topic, other than in the context of geophagy (soil-eating) which is common among pregnant women in many parts of Africa, although not in our study area [36]. Kenyan women were, to some extent, able to identify “lack of blood” as a reason for soil-eating, but the direction of causality was not fixed (ie. soil eating could be the cause or consequence of anemia) [37]. In our FGs there were mixed views on whether to tell women that the supplement contained elemental iron. Some participants thought that this would increase refusals, but others accepted, and seemed to understand, explanations given during discussions. It seems important to try and move away from the concept that iron supplements “strengthen” and “increase” blood, to a more relevant explanation of iron function and requirements. This may not increase adherence to iron interventions, but it is intrinsically important to informed decision making. A more scientific explanation of iron’s role would be especially relevant in schools, given the increasing emphasis on improving iron status of non-pregnant girls.
This study was conducted in the context of a clinical trial, which may have generated responses that would not be typical of non-intervention villages. Lack of knowledge is, however, likely to be more pronounced in non-intervention areas. Considerable efforts were made by the study team to provide accurate information but reaching non-parous adolescents is challenging. Cultural norms dictate modesty and shyness when discussing menses or pregnancy, so frank discussions between girls and field workers can be difficult. In Burkina Faso, adolescent participation during health promotion campaigns is also regulated and restricted [38] so girls’ opportunity to hear information first-hand is limited. In general, health workers, who share community views of the adolescent’s low status, are less assiduous in their care of this group [39–40]. As regards other factors affecting women’s responses, the FG were initiated before and shortly after recruitment finished. At this early stage, negative views on supplements should not have influenced women’s views. Importantly, the research provided an opportunity to actively improve communication about iron supplements during the trial. For this reason, qualitative analyses early during trial implementation can provide an immediate insight into factors impairing adherence and intervention compliance.
Conclusion
Clinicians and health providers are being encouraged to counsel women at high risk of anemia in order to reduce the many adverse outcomes associated with this condition. They will need to provide a clearer definition of anemia and guard against reinforcing lay explanations of the beneficial outcomes expected from iron supplements. One suggestion from this study is better clarity on how iron is taken up and used in the body, and why even a small lack of iron can have detrimental effects that should be addressed before they become life threatening and require blood transfusion. These concepts would seem to be central to any of the anemia control strategies that are currently recommended.
Acknowledgements
This research was funded by the National Institute of Child Health and Human Development (NICHD) and the NIH Office of Dietary Supplements (ODS) as a component of NIH grant 1U01HDO61234-01A1 (Long term weekly iron and folic acid supplementation and malaria risk in early pregnancy: a randomized controlled trial). LB is funded by the Max Elstein Trust.
REFERENCES
- 1.de Benoist B, McLean E, Egli I, Cogswell M, editors. World Health Organisation. Worldwide Prevalence of Anaemia 1993–2005. WHO Global Data Base on Anaemia. Geneva, Switzerland: 2008. [Google Scholar]
- 2.Sanou D, Turgeon-O'Brien H, Desrosiers T. Nutrition intervention and adequate hygiene practices to improve iron status of vulnerable preschool Burkinabe children. Nutrition. 2010;26:68–74. doi: 10.1016/j.nut.2009.05.017. [DOI] [PubMed] [Google Scholar]
- 3.Ouédraogo HZ, Traoré T, Zèba; AN, Dramaix-Wilmet M, Hennart P, Donnen P. Effect of an improved local ingredient-based complementary food fortified or not with iron and selected multiple micronutrients on Hb concentration. Public Health Nutrition. 2010;13:1923–1930. doi: 10.1017/S1368980010000911. [DOI] [PubMed] [Google Scholar]
- 4.Rohner F, Zimmermann MB, Amon RJ, Vounatsou P, Tschannen AB, N’Goran EK, Nindjin C, Cacou MC, Té-Bonlé MD, Aka H, Sess DE, Utzinger J, Hurrell RF. In a randomized controlled trial of iron fortification, anthelmintic treatment, and intermittent preventive treatment of malaria for anemia control in Ivorian children, only anthelmintic treatment shows modest benefit. Journal of Nutrition. 2010;140:635–641. doi: 10.3945/jn.109.114256. [DOI] [PubMed] [Google Scholar]
- 5.Pena-Rosas JP, Viteri FE. Effects and safety of preventive oral iron or iron and folic acid supplementation for women during pregnancy (Review) The Cochrane Library. 2009;(Issue 4) doi: 10.1002/14651858.CD004736.pub3. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Geneva: 2011. Guideline: Intermittent iron and folic acid supplementation in menstruating women. Available at: http://whqlibdoc.who.int/publications/2011/9789241502023_eng.pdf. [PubMed] [Google Scholar]
- 7.Lynch SR. The potential impact of iron supplementation during adolescence on iron status in pregnancy. Journal of Nutrition. 2000;130(S2 Suppl):448S–451S. doi: 10.1093/jn/130.2.448S. [DOI] [PubMed] [Google Scholar]
- 8.Beard JL. Effectiveness and strategies of iron supplementation during pregnancy. American Journal of Clinical Nutrition. 2000;71(Suppl):1288S–1294S. doi: 10.1093/ajcn/71.5.1288s. [DOI] [PubMed] [Google Scholar]
- 9.Khambalia AZ, O’Connor DL, Macarthur C, Depuis A, Zlotkin SH. Periconceptual iron supplementation does not reduce anemia or improve iron status among pregnant women in rural Bangladesh. American Journal of Clinical Nutrition. 2009;90:1295–1302. doi: 10.3945/ajcn.2009.28350. [DOI] [PubMed] [Google Scholar]
- 10.Brabin L, Brabin BJ, Gies S. Influence of iron status on risk of maternal or neonatal mortality with an emphasis on developing countries. Nutrition Reviews. 2013;71:528–540. doi: 10.1111/nure.12049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peña Rosas JP, De-Regil LM, Dowswell T, Viteri FE. Intermittent oral iron supplementation during pregnancy (Review) The Cochrane Library. 2012;(Issue 7) doi: 10.1002/14651858.CD009997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fernández-Gaxiola AC, De-Regil LM. Intermittent iron supplementation for reducing anaemia and its associated impairments in menstruating women. The Cochrane Library. 2011;(Issue 12) doi: 10.1002/14651858.CD009218.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Titaley CR, Dibley MJ, Roberts CL, Agho K. Combined iron/folic acid supplements and malaria prophylaxis reduce neonatal mortality in 19 sub-Saharan countries. American Journal of Clinical Nutrition. 2010;92:235–243. doi: 10.3945/ajcn.2009.29093. [DOI] [PubMed] [Google Scholar]
- 14.Ogundipe O, Hoyo C, Ostbye T, Oneko O, Manongi R, Lie R, Daltveit AK. Factors associated with prenatal folic acid and iron supplementation among 21,889 pregnant women in Northern Tanzania: a cross-sectional hospital-based study. BioMed Central Public Health. 2012;12:481. doi: 10.1186/1471-2458-12-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kulkarni B, Christian P, LeClerq SC, Khatry SK. Determinants of compliance to antenatal micronutrient supplementation and women’s perceptions of supplement use in rural Nepal. Public Health Nutrition. 2009;13:82–90. doi: 10.1017/S1368980009005862. [DOI] [PubMed] [Google Scholar]
- 16.Mumtaz Z, Shahab S, Butt N, Rab A, DeMuynck A. Daily iron supplementation is more effective that twice weekly iron supplementation in pregnant women in Pakistan in a randomized double-blind clinical trial. Journal of Nutrition. 2000;130:2697–2702. doi: 10.1093/jn/130.11.2697. [DOI] [PubMed] [Google Scholar]
- 17.Christian P, West KP, Khatry SK, Leclerq SC, Pradhan EK, Katz J, Shrestha SR, Sommer A. Effects of maternal micronutrient supplementation on fetal loss and infant mortality. American Journal of Clinical Nutrition. 2003;78:1194–1202. doi: 10.1093/ajcn/78.6.1194. [DOI] [PubMed] [Google Scholar]
- 18.Zeng L, Dibley MJ, Cheng Y, Dang S, Chang S, Kong L, Yan H. Impact of micronutrient supplementation during pregnancy on birthweight, duration of gestation and perinatal mortality in rural western China: double blind cluster randomised controlled trial. British Medical Journal. 2008;337:1211–1215. doi: 10.1136/bmj.a2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ekström E-CM, Kavishe FP, Habicht J-P, Frongillo EA, Rasmussen KM, Hemed L. Adherence to iron supplementation during pregnancy in Tanzania: determinants and hematological consequences. American Journal of Clinical Nutrition. 1996;64:368–374. doi: 10.1093/ajcn/64.3.368. [DOI] [PubMed] [Google Scholar]
- 20.Chakma T, Rao PV, Meshram PK. Factors associated with high compliance/feasibility during iron and folic acid supplementation in a tribal area of Madhya Pradesh, India. Public Health Nutrition. 2013;16:377–380. doi: 10.1017/S1368980012002704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zavaleta N, Caulfield LE, Figueroa A, Chen P. Patterns of compliance with prenatal iron supplementation among Peruvian women. Maternal and Child Nutrition. 2012 doi: 10.1111/j.1740-8709.2012.00407.x. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Victora CG, Barros FC, Assunção MC, Restrepo-Méndez MC, Matijasevich A, Martorell R. Scaling up maternal nutrition programs to improve birth outcomes: a review of implementation issues. Food and Nutrition Bulletin. 2012;33(2 Suppl):S6–S26. doi: 10.1177/15648265120332S102. [DOI] [PubMed] [Google Scholar]
- 23.Nikiema B, Haddad S, Potvin L. Women bargaining to seek healthcare: norms, domestic practices, and implications in rural Burkina Faso. World Development. 2008;36:608–624. [Google Scholar]
- 24.Protocol 10PRT/6932: Malaria risk prior to and during early pregnancy in nulliparous women receiving longterm weekly iron and folic acid supplementation (WIFS): a non-inferiority randomised controlled trial (WCT01210040) Report available at: www.thelancet.com/protocol-reviews/10PRT6932.
- 25.Derra K, Rouamba E, Kazienga A, Ouedraogo S, Tahita MC, Sorgho H, Valea I, Tinto H. Profile: Nanoro Health and Demographic Surveillance System. International Journal of Epidemiology. 2012;41:1293–1301. doi: 10.1093/ije/dys159. [DOI] [PubMed] [Google Scholar]
- 26.Institut National de la Statistique et de la Démographie (INSD) and Macro International, Inc. Enquête Démographique et de Santé, Burkina Faso 1998–1999. Calverton, Maryland: Macro International Inc; 2000. [Google Scholar]
- 27.Ritchie J, Lewis J. Qualitative Research Practice. London: Sage; 2003. [Google Scholar]
- 28.Moore M, Riono P, Pariani S. A qualitative investigation of factors influencing use of iron folate tablets by pregnant women in West Java: a summary of findings; MotherCare Working Paper 13, John Snow Inc; Virginia USA. 1991. [Google Scholar]
- 29.Galloway R, Dusch E, Elder L, Achadi E, Grajeda R, Hurtado E, Favin M, Kanani S, Marsaban J, Meda N, Moore KM, Morison L, Raina N, Rajaratnam J, Rodriguea J, Stephen C. Women’s perceptions of iron deficiency and anemia prevention and control in eight developing countries. Social Science and Medicine. 2002;55:529–544. doi: 10.1016/s0277-9536(01)00185-x. [DOI] [PubMed] [Google Scholar]
- 30.Nagata JM, Gatti LR, Barg FK. Social determinants of iron supplementation among women of reproductive age: a systematic review of qualitative data. Maternal and Child Nutrition. 2012;8:1–18. doi: 10.1111/j.1740-8709.2011.00338.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jefferds MD. Concepts of iron deficiency and public health measures in rural Costa Rica. Social Science and Medicine. 2002;55:1143–1156. doi: 10.1016/s0277-9536(01)00254-4. [DOI] [PubMed] [Google Scholar]
- 32.Souganidis ES, Sun K, de Pee S, Kraemer K, Rah J-H, Moench-Pfanner R, Sari M, Bloem MW, Semba RD. Relationship of maternal knowledge of anemia with maternal and child anemia and health-related behaviours targeted at anemia among families in Indonesia. Maternal and Child Health Journal. 2012;16:1913–1925. doi: 10.1007/s10995-011-0938-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pell C, Straus L, Andrew EVW, Menaca A, Pool R. Social and cultural factors affecting interventions for malaria in pregnancy in Africa: a systematic review of the qualitative research. PLoS One. 2011;6(Issue 7) doi: 10.1371/journal.pone.0022452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nacoulma EW, Sakande J, Ouermi A, Tieno H, Drabo YJ. Causes of iron-deficiency anaemia in the internal medicine department of the national teaching hospital of Ouagadougou. Sante. 2008;18:223–225. [Article in French] [PubMed] [Google Scholar]
- 35.Loevinsohn BP. Health education interventions in developing countries: a methodological review of published articles. International Journal of Epidemiology. 1990;19:788–794. doi: 10.1093/ije/19.4.788. [DOI] [PubMed] [Google Scholar]
- 36.Njiru H, Elchalal U, Paltiel O. Geophagy during pregnancy in Africa: a literature review. Obstetrical and Gynecological Survey. 2011;66:452–459. doi: 10.1097/OGX.0b013e318232a034. [DOI] [PubMed] [Google Scholar]
- 37.Geissler PW, Prince RJ, Levene M, Poda C, Beckerleg SE, Mutemi W, Shulman CE. Perceptions of soil-eating and anaemia among pregnant women on the Kenyan coast. Social Science and Medicine. 1999;48:1069–1079. doi: 10.1016/s0277-9536(98)00409-2. [DOI] [PubMed] [Google Scholar]
- 38.Grietens KP, Gies S, Coulibaly SO, Ky C, Somda J, Toomer E, Ribera JM, D’Alessandro U. Bottlenecks for high coverage of intermittent preventive treatment in pregnancy: the case of adolescent pregnancies in Burkina Faso. PloS ONE. 2010;5(Issue 8) doi: 10.1371/journal.pone.0012013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Msyamboza K, Savage E, Kalanda G, Kazembe P, Gies S, D’Alessandro U, Brabin BJ. Trends in pregnancy outcomes in Malawian adolescents receiving antimalarial and hematinic supplements. Acta Obstetetricia et Gynecologica. 2010;89:1011–1016. doi: 10.3109/00016349.2010.487892. [DOI] [PubMed] [Google Scholar]
- 40.Ejidokun OO. Community attitudes to pregnancy anaemia, iron and folate supplementation in urban and rural Lagos, south-western Nigeria. Midwifery. 2000;16:89–95. doi: 10.1054/midw.1999.0196. [DOI] [PubMed] [Google Scholar]