Abstract
Background
Previous laboratory studies of landing have defined landing techniques in terms of soft or stiff landings according to the degree of maximal knee flexion angle attained during the landing phase and the relative magnitude of the ground-reaction force. Current anterior cruciate ligament injury prevention programs are instructing athletes to land softly to avoid excessive strain on the anterior cruciate ligament.
Purpose
This study was undertaken to measure, describe, and compare tibiofemoral rotations and translations of soft and stiff landings in healthy individuals using biplane fluoroscopy.
Study Design
Controlled laboratory study.
Methods
The in vivo, lower extremity, 3-dimensional knee kinematics of 16 healthy adults (6 male and 10 female) instructed to land softly and stiffly in different trials were collected in biplane fluoroscopy as they performed the landing from a height of 40 cm.
Results
Average and maximum relative anterior tibial translation (average, 2.8 ± 1.2 mm vs 3.0 ± 1.4 mm; maximum, 4.7 ± 1.6 mm vs 4.4 ± 0.8 mm), internal/external rotation (average, 3.7° ± 5.1° vs 2.7° ± 4.3°; maximum, 5.6° ± 5.5° vs 4.9° ± 4.7°), and varus/valgus (average, 0.2° ± 1.2° vs 0.2° ± 1.0°; maximum, 1.7° ± 1.2° vs 1.6° ± 0.9°) were all similar between soft and stiff landings, respectively. The peak vertical ground-reaction force was significantly larger for stiff landings than for soft landings (2.60 ± 1.32 body weight vs 1.63 ± 0.73; P < .001). The knee flexion angle total range of motion from the minimum angle at contact to the maximum angle at peak knee flexion was significantly greater for soft landings than for stiff (55.4° ± 8.8° vs 36.8° ± 11.1°; P < .01).
Conclusion
Stiff landings, as defined by significantly lower knee flexion angles and significantly greater peak ground-reaction forces, do not result in larger amounts of anterior tibial translation or knee rotation in either varus/valgus or internal/external rotation in healthy individuals.
Clinical Relevance
In healthy knees, the musculature and soft tissues of the knee are able to maintain translations and rotations within a small, safe range during controlled landing tasks of differing demand. The knee kinematics of this healthy population will serve as a comparison for injured knees in future studies. It should be stressed that because the authors did not compare how the loads were distributed over the soft tissues of the knee between the 2 landing styles, the larger ground-reaction forces and more extended knee position observed during stiff landings should still be considered dangerous to the anterior cruciate ligament and other structures of the lower extremities, particularly in competitive settings where movements are often unanticipated.
Keywords: anterior cruciate ligament (ACL), kinematics, biplane fluoroscopy, prevention, landing
Seventy percent of all anterior cruciate ligament (ACL) injuries have been reported to occur during noncontact activities marked by sudden deceleration of the center of mass, as in the case of landing from a jump.9,45 Because these injuries may be preventable, considerable research has been conducted to identify factors that may reduce an individual's risk for sustaining a noncontact ACL injury. The concepts and theories developed from noncontact ACL injury studies have contributed to the development of ACL injury prevention training programs, such as the Prevent injury Enhance Performance (PEP) program.16 The implementation of ACL injury prevention programs has shown success in altering biomechanical risk factors that have been associated with ACL injury and reducing the number of noncontact ACL injuries in female athletes during competition.16,17,21,34
A key component reported in noncontact ACL injury prevention programs is the oral and instructional training to “land softly.”16,21,23 Previous laboratory studies of landing have defined landing techniques in terms of soft or stiff according to the degree of maximal knee flexion angle (KFA) attained during the landing phase.14 It has been hypothesized that stiffer landings place increased loads on the knee, and therefore subject individuals to a higher risk of ACL injury.1,6,7,25,36,39 In contrast with soft landings, stiff landings are characterized by a more extended knee position at ground contact that results in higher ground-reaction forces (GRFs)14 and a greater patellar tendon angle, defined as the angle between the patellar tendon and the long axis of the tibia.20 Large GRFs during landing can produce a large external knee flexion moment that must be overcome by an equal and opposite internal extension moment produced by the quadriceps muscles.45 A large patellar tendon angle, coupled with a large eccentric quadriceps contraction, has been suggested as a mechanism for increased anterior tibial translation that has resulted in higher ACL strain during stiff landings in both in vitro and in vivo studies.35,45
Although ACL injury prevention programs have been shown to be effective at teaching athletes to avoid stiff landings, the overall occurrence of noncontact ACL injury and surgical reconstructions remains high in both men and women.17 We believe that the inability to adequately prevent this injury is linked to the lack of understanding of the mechanisms causing it. Using traditional motion capture techniques (ie, optical-based surface marker sets), it is difficult to capture knee motion with the precision necessary to assess tibiofemoral translations. For this reason, there is limited reporting of in vivo tibiofemoral kinematics, and there are no reports describing rotation and translation differences during soft and stiff landings. Biplane fluoros-copy systems enable the precise measurement of 6 degrees of freedom kinematics of specific joints such as the knee during dynamic activities.12,19,30,31,33
The purpose of this study was to measure, describe, and compare tibiofemoral rotations and translations of soft and stiff landings using biplane fluoroscopy. Because stiff landings should generate larger GRFs and be performed with lower KFAs, we hypothesized that stiff landings would cause significantly increased anterior translation of the tibia relative to the femur when compared with soft landings.
MATERIALS AND METHODS
Drop-Landing Protocol
This study was approved by the institutional review board and all participants signed an informed consent form. All individuals had a history of participation in jumping and cutting sports, and no participant had any major injuries or surgeries to the lower limbs.
The in vivo lower extremity, 3-dimensional, knee kinematics of 6 men (height, 181.8 ± 9.5 cm; body mass, 81 ± 11 kg; body mass index [BMI], 24.8 ± 1.7 kg/m2; age, 29.7±7.9 years) and 10 women (height, 167.8 ± 7.1 cm; body mass, 57 ± 4 kg; BMI, 20.1 ± 1.4 kg/m2; age, 26.7 ± 6.7 years) instructed to land softly and stiffly were collected as they performed the landing from a 40-cm height (Figure 1). The instructions for executing both the soft and stiff landings were given using verbal cues. Participants were told to “land erect as possible” and “with little bending at the knee and hip” during stiff landings, and “land as quietly as possible” and “use your legs as shock absorbers” during soft landings. An unloaded knee extension trial was collected following the landing trials to be referenced to the landing data. The individuals were seated with their knee in 90° of flexion. They were then asked to slowly extend their knee to 0° of flexion while fluoroscopy data were collected. The 2 landing styles were collected in random order between participants. The knee extension trial was always collected after the landing trials were completed. Comparisons between the 2 landing styles were made throughout the entire landing range of motion using the motion analysis system. Because of the constraints imposed by the limited field of view of the fluoroscopy system, analysis was done over the first 100 milliseconds from ground contact or until peak knee flexion was observed.
Figure 1.
Participant at approximately the point of maximum knee flexion while landing from a drop landing from a height of 40 cm in the biplane fluoroscopy system.
Surface Marker Motion Analysis Data Capture
Traditional surface marker motion capture techniques were used to collect kinematic and kinetic data simultaneously with fluoroscopy data. Ten cameras (Motion Analysis Corporation, Santa Rosa, California) were used positioned at ~36° intervals around the performance area and sampled at 240 Hz. The 3-dimensional kinematics of each trial were captured by securing 53 retroreflective spherical markers (10-mm diameter) to anatomic landmarks on each subject reported previously to produce a standard Helen Hayes marker set with a configuration of 3 markers per segment.8 All force values and all joint moments were scaled to body weight and Newton-meter per kilogram of body mass, respectively.
Biplane Fluoroscopy System
The biplane fluoroscopy system was composed of 2 commercially available BV Pulsera c-arms with 30-cm image intensifiers (Philips Medical Systems, Best, the Netherlands), which were modified under appropriate US Food and Drug Administration guidelines. To capture the high-speed nature of the landing motion, 2 coupled high-speed, high-resolution (1024 × 1024) digital cameras (Phantom V5.1, Vision Research, Wayne, New Jersey) with frame rates up to 1000 frames per second were interfaced with the image intensifiers of the fluoroscopy systems using a custom-built interface.
Biplane Fluoroscopy System Calibration
Fluoroscopy systems tend to have significant image distortion that must be corrected for accurate measurements. Image distortion was corrected by imaging an accurately machined aluminum plate with 406 holes placed 15 mm apart arranged in a square pattern, placed directly in front of the image intensifier. The transformation from the distorted image to the corrected image was calculated and applied to all subsequent images using Model-Based RSA (roentgen stereophotogrammetric analysis) software (Medis Specials, BV, Leiden, the Netherlands).
To determine the focus position of the 2 fluoroscopy systems, a 15-cm3 calibration cube enclosing 15 tantalum markers was positioned inside the 24-cm3 3-dimensional capture volume. The precise relative positions of the markers within the cube were obtained using Model-Based RSA. Radiographic images of the foam cube were acquired with the biplane fluoroscopy system, and the precise focus position was determined using a nested optimization algorithm. The inner optimization loop determined the error of the best match of the cube markers given a focus position; the outer optimization loop searched for the focus position that minimized the matching error from the inner optimization loop. The relative positions of the 2 fluoroscopy systems were based on the cube position in the 2 views of the individual fluoroscopy systems.15,41
Collection of In Vivo Landing Data Using Biplane Fluoroscopy
The in vivo biplane fluoroscopy data collection for the landing motion consisted of 2 parts: (1) obtaining a static CT scan of the knee joint and (2) collecting biplane fluoroscopy data during the drop-landing trials simultaneously with standard surface marker–based motion capture.
To obtain accurate 3-dimensional geometric descriptions of the bones in the knee, a supine, high-resolution static CT scan of the knee (approximately 12 cm above and below the joint line) utilizing an Aquilion 64 scanner (Toshiba America Medical Systems, Tustin, California) was obtained. The sequence of images from the scan, representing slices of 0.5-mm thickness with a resolution of 512 × 512 pixels (ie, voxel size of ~0.7 × 0.7 × 0.5 mm), were obtained using the standard 120-kVp and 200-mA bone reconstruction technique. Commercial software (Mimics, Materialize, Inc, Ann Arbor, Michigan) was used to extract the bone contours from the CT images and to reconstruct the 3-dimensional geometry of the femur, tibia/fibula, and the patella. These 3-dimensional geometries were then ready to be used in Model-Based RSA for the 3-dimensional position and orientation (pose) estimation of the knee in the dynamic biplane fluoroscopy images.
Biplane fluoroscopy data were collected for 1.0 second for each landing at 500 frames per second with a shutter speed of 1/2000 second. The x-ray generators were operated in radiographic mode at 60 mA and approximately 60 kV. The pose of the femur and tibia/fibula during landing was determined for each frame by semiautomatically extracting (automatically detected, manually assigned) both the inner and outer bony contours of the femur and tibia/fibula from the biplane fluoroscopy images. Subsequently, a fully automatic 6 degrees of freedom optimization algorithm that has been previously described28 was used to determine the position and orientation, which optimally matched the detected contours with the projected contours from the imported bone geometries (Figure 2). The origin of the femoral coordinate system was placed between the medial and lateral femoral condyles on the center line of a cylinder fitted to the medial and lateral posterior condyles. The medial-lateral (ML) axis of the femur was determined as the line through the long axis of this cylinder. The superior-inferior (SI) axis was aligned to the posterior line of the femur, and an anterior-posterior (AP) axis was determined as the cross-product of the ML and SI axes. The tibial coordinate system was defined by the position of the tibia at full extension in the knee extension trial. At maximum knee extension, the femoral coordinate system was copied, with the duplicate coordinate system representing the tibia (Figure 3).41 Using these coordinate systems, knee kinematics were calculated using methods described by Grood and Suntay.18
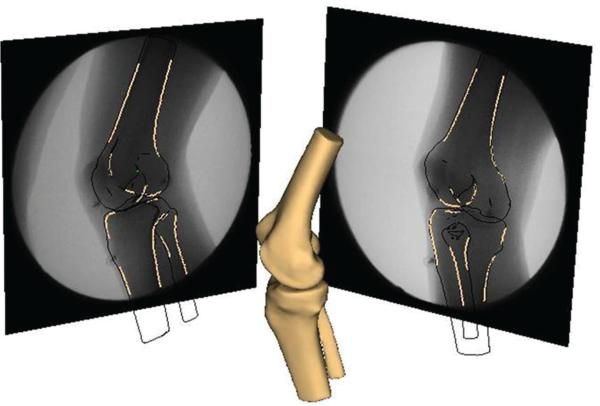
Figure 2.
An image of the reconstructed tibia/fibula and femur. Contours of bony landmarks were detected on each radiograph and a fully automatic 6 degrees of freedom optimization algorithm was used to determine the position and orientation that optimally matched the detected contours with the projected contours from the imported bone geometries.
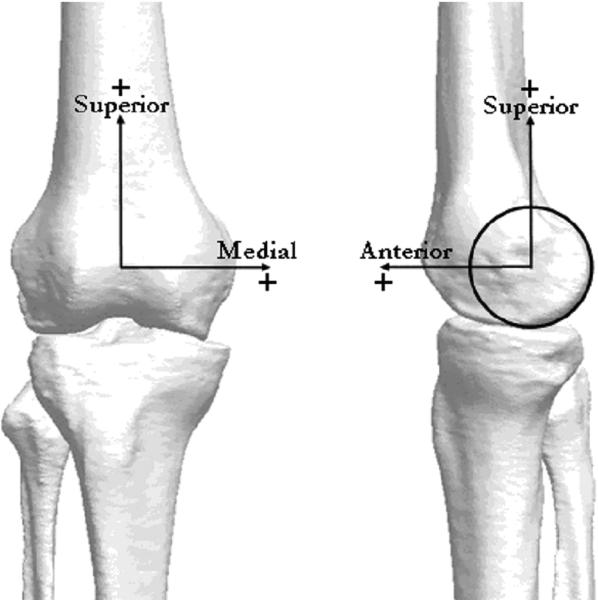
Figure 3.
The femoral and tibial coordinate system used to calculate tibiofemoral translations and rotation. A cylinder was fitted to the medial and lateral posterior femoral condyles and the origin of the femoral coordinate system was placed between the medial and lateral femoral condyles on the center line of this cylinder. The tibial coordinate system was defined by the position of the tibia at full extension in the knee extension trial. At maximum knee extension, the femoral coordinate system was copied, with the duplicate coordinate system representing the tibia.
Fluoroscopy kinematic data obtained during landing were referenced to the unloaded knee extension fluoroscopy trial data by subtracting the knee extension data from the landing data at the same flexion angles to obtain “relative” kinematic data. For example, anterior tibial translation data from the unloaded knee extension trial was subtracted from anterior tibial translation data during a stiff landing at the same KFA to yield relative anterior tibial translation measures.
Referencing to the passive motion of the knee collected during a low-load activity such as knee extension, in which the ACL is generally taut but not overly strained,1,5 is important for studying the change in kinematics when loads are applied. Referencing to a low-load task has been used previously during cadaver and in vivo investigations and has been reported to reduce intrasubject variability and produce more consistent comparisons of the changes in knee kinematics that occur during activity.26,41 Specifically, internal-external rotation and AP translation of the tibia relative to the femur are coupled to KFA because of the geometry of the articular surfaces and the soft tissue restraints in the knee. By referencing data to kinematics measured at each flexion angle of the low-load knee extension, this bias was removed. Relative kinematics presented here are those associated specifically with the forces applied to the lower limb during these 2 landing tasks.
Biplane Fluoroscopy System Accuracy
The biplane fluoroscopy system was validated using standard validation techniques.4,24,27 Tantalum beads were placed in 3 cadaveric knee specimens (5 beads per bone) and the specimens were dropped from a height of 40 cm within the biplane fluoroscopy system. This was done during a morning testing session and then repeated 4 hours later in an afternoon testing session. A total of 24 frames were selected from the image sequences during the morning testing session and afternoon testing session. The beads and bones were tracked independently using the same bone-tracking methods as described in this study. The bead coordinate systems were registered to the femur and tibia/fibula coordinate systems and subsequently the knee kinematics based on the bead data were determined. Bias and precision representing the mean and standard deviation of the difference between the bone tracking and the bead tracking was calculated from the 24 frames.3 The average bias and precision was 0.3° ± 0.6°, 0.4° ± 0.5°, and 0.3° ± 0.6° for flexion-extension, varus-valgus, and internal-external rotations, respectively. The average bias and precision was 0.3 ± 0.4 mm, 0.4 ± 0.4 mm, and 0.3 ± 0.4 mm for AP, ML, and distraction-compression translations, respectively. These values were consistent with previously reported studies using similar biplane fluoroscopy technology.2,4,32,41
Statistical Analysis
To analyze the effects of landing type and gender on marker-based and biplane fluoroscopic variables, univariate 2-way (gender × landing type) analyses of variance were used with landing type as a repeated measure. This statistical analysis was completed for each kinematic and kinetic variable with α = .05. All statistical analyses were completed with SPSS software (SPSS, an IBM Company, Chicago, Illinois). We recognize that more study participants would have been necessary to show a sex difference. Our previous power analysis using these data indicated that we would have needed more than 500 participants in each group to identify differences between males and females. The primary purpose of this study was to examine the link between landing style and anterior tibial translation in a general population.
RESULTS
The absolute knee kinematics are presented in Table 1. Average and maximum absolute internal rotation were significantly greater for soft landings than stiff (maximum, 18.9° ± 5.3° vs 15.4° ± 6.4°; P < .0001; average, 15.3° ± 5.7° vs 12.3° ± 6.7°; P < .001). Maximum absolute valgus angle was significantly greater for soft landings than for stiff (2.3° ± 2.3° vs 1.0° ± 1.9°; P < .01).
TABLE 1.
Absolute Knee Kinematics From the Biplane Fluoroscopy System for Soft and Stiff Landingsa
| Soft | Stiff | |
|---|---|---|
| AvgKFA, degb | 56.8 (12.7) | 39.8 (14.5) |
| MaxAntTibTr, mm | 6.70 (2.91) | 6.45 (2.44) |
| AvgAntTibTr, mm | 4.76 (2.38) | 4.49 (2.44) |
| MaxInt/ExtRot, degb | 18.87 (5.28) | 15.43 (6.38) |
| AvgInt/ExtRot, degb | 15.31 (5.68) | 12.30 (6.71) |
| MaxVar/Val, degb | 2.33 (2.26) | 1.04 (1.93) |
| AvgVar/Val, degb | 0.20 (1.66) | –0.32 (1.77) |
AvgKFA, average knee flexion angle; MaxAntTibTr, maximum amount of anterior tibial translation; AvgAntTibTr, average amount of anterior tibial translation; MaxInt/ExtRot, maximum internal/external rotation angle: (+) external, (–) internal; AvgInt/ExtRot, average internal/external rotation angle: (+) external, (–) internal; MaxVar/Val, maximum varus/valgus angle: (+) valgus, (–) varus; AvgVar/Val, average varus/valgus angle: (+) valgus, (–) varus.
Significantly different between landing styles for all participants (P < .05).
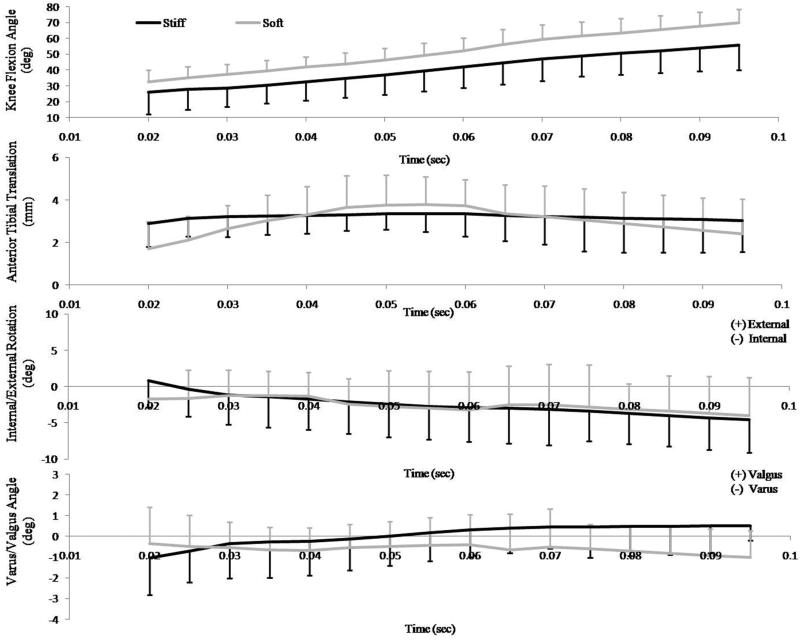
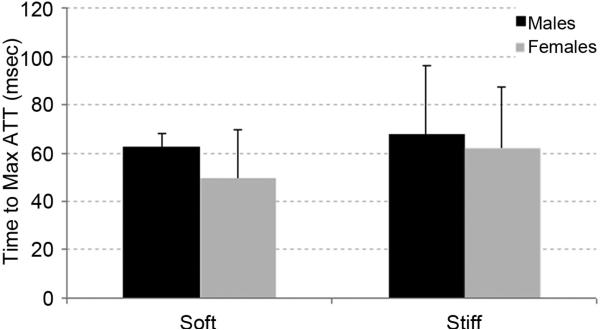
Table 2 describes normalized fluoroscopy data for soft and stiff landing styles. There was no significant difference in the average and maximum relative anterior tibial translation (average, 2.8 ± 1.2 mm vs 3.0 ± 1.4 mm; maximum, 4.7 ± 1.6 mm vs 4.4 ± 0.8 mm), internal/external rotation (average, 3.7° ± 5.1° vs 2.7° ± 4.3°; maximum, 5.6° ± 5.5° vs 4.9° ± 4.7°), and varus/valgus rotation (average, 0.2° ± 1.2° vs 0.2° ± 1.0°; maximum, 1.7° ± 1.2° vs 1.6° ± 0.9°) between soft and stiff landings, respectively (Table 2) (Figure 4). No significant gender or landing type and gender interaction effects were noted for these variables (Table 2). Additionally, there were no significant differences or gender interaction between landing style for time to maximum anterior tibial translation (Figure 5).
TABLE 2.
Normalized Knee Kinematics for Both Genders and the Total Subject Group From the Biplane Fluoroscopy System for Soft and Stiff Landingsa
| Soft |
Stiff |
|||||
|---|---|---|---|---|---|---|
| Males | Females | Total (N = 16) | Males | Females | Total (N = 16) | |
| AvgKFA, degb | 54.7 (7.9) | 50.2 (7.7) | 56.8 (12.7) | 32.9 (14.1) | 34.7 (12.9) | 39.8 (14.5) |
| MaxAntTibTr, mm | 4.6 (1.3) | 4.7 (1.9) | 4.7 (1.6) | 4.3 (0.8) | 4.5 (0.9) | 4.4 (0.8) |
| AvgAntTibTr, mm | 3.0 (1.6) | 2.8 (1.3) | 2.8 (1.2) | 2.7 (1.6) | 2.8 (0.8) | 3.0 (1.4) |
| MaxInt/ExtRot, deg | 5.9 (7.1) | 5.3 (4.7) | 5.6 (5.5) | 5.6 (6.0) | 5.6 (4.1) | 4.9 (4.7) |
| AvgInt/ExtRot, deg | 4.0 (6.9) | 4.3 (3.3) | 3.7 (5.1) | 3.1 (5.8) | 3.2 (3.3) | 2.7 (4.3) |
| MaxVar/Val, deg | 1.8 (0.9) | 1.7 (0.9) | 1.7 (1.2) | 1.6 (0.9) | 1.6 (0.9) | 1.6 (0.9) |
| AvgVar/Val, deg | 0.1 (1.2) | 0.3 (1.0) | 0.2 (1.2) | 0.4 (1.0) | 0.1 (1.0) | 0.20 (1.0) |
AvgKFA, average knee flexion angle; MaxAntTibTr, maximum amount of anterior tibial translation; AvgAntTibTr, average amount of anterior tibial translation; MaxInt/ExtRot, maximum internal/external rotation angle: (+) external, (–) internal; AvgInt/ExtRot, average internal/external rotation angle: (+) external, (–) internal; MaxVar/Val, maximum varus/valgus angle: (+) valgus, (–) varus; AvgVar/Val, average varus/valgus angle: (+) valgus, (–) varus.
Significantly different between landing styles for all participants (P < .05).
Figure 4.
Normalized flexion angle, anterior tibial translation, and internal/external rotation angle versus time for soft and stiff landings.
Figure 5.
Time to maximum anterior tibial translation (ATT) compared between soft and stiff landings and males and females. There were no significant differences between the 2 landings or between gender.
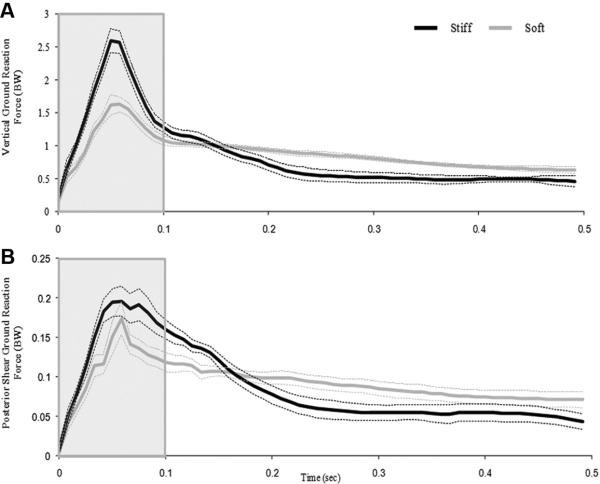
Peak vertical GRFs were significantly larger for stiff landings than soft landings (2.60 ± 1.32 body weight vs 1.63 ± 0.73; P < .001) (Figure 6A). However, there was no significant difference between the peak shear component of the GRF between soft and stiff landings (Figure 6B). The KFA total range of motion from the minimum angle at contact to the maximum angle at peak knee flexion was significantly greater for soft landings than for stiff (55.4° ± 8.8° vs 36.8° ± 11.1°; P < .01) even though KFA at contact differed by only a little more than 5° (15.0° ± 4.7° vs 9.6° ± 6.2°; P < .05). Peak knee extension moments were significantly greater for stiff landings than for soft landings (2.05 ± 0.58 N m/kg vs 1.75 ± 0.39 N m/kg; P < .05) (Table 3). There was no difference between peak knee abduction moment between the soft and stiff landings (9.9 ± 5.5 N m vs 9.4 ± 6.5 N m/kg) but when knee abduction moment was normalized to body weight, women had significantly greater peak abduction moments than men during both soft and stiff landings (Table 3). We did not observe any non-normalized peak knee abduction moments that would be considered at risk (soft range, 2.4 to 17.6 N·m; stiff range, –1.9 to 20.0 N·m).
Figure 6.
A, the mean and standard deviation of the vertical ground-reaction force during soft and stiff landings versus time. Stiff landings are shown in black and soft landings in gray. The boxed area indicates the portion of the landing phase that was captured in the biplane fluoroscopy system. B, the mean and standard deviation of the posterior shear ground-reaction force during soft and stiff landings versus time.
TABLE 3.
Knee Flexion Angle, Forces, and Moments During Soft and Stiff Landings for Both Genders and the Total Study Groupa
| Soft |
Stiff |
|||||
|---|---|---|---|---|---|---|
| Males | Females | Total (N = 16) | Males | Females | Total (N = 16) | |
| KFArom, degb | 54.4 (6.9) | 56.0 (11.0) | 55.4 (8.8) | 34.1 (8.0) | 39.3 (10.2) | 36.8 (11.1) |
| ContactKFA, degb | 14.1 (4.3) | 16.3 (7.7) | 15.0 (4.7) | 8.2 (7.1) | 12.1 (6.1) | 9.6 (6.2) |
| PVGRF, BWb | 1.57 (0.26) | 1.77 (0.21) | 1.63 (0.73) | 2.51 (0.56) | 2.91 (0.61) | 2.60 (1.32) |
| PSGRF, BWb | –0.19 (0.05) | –0.24 (0.06) | –0.22 (0.06) | –0.18 (0.07) | –0.21 (.08) | –0.19 (0.07) |
| PExtMoment, N·m/kgb | 1.67 (0.39) | 1.76 (0.41) | 1.75 (0.39) | 2.04 (0.41) | 2.03 (0.47) | 2.05 (0.58) |
| PAbdMoment, Nm/kgc | 0.097 (0.067) | 0.22 (0.15) | 0.20 (0.15) | 0.078 (0.098) | 0.24 (0.15) | 0.21 (0.17) |
KFArom, total knee flexion angle range of motion from minimum to maximum; ContactKFA, knee flexion angle at the point of contact; PVGRF, peak vertical ground-reaction force; BW, body weight; PSGRF, peak shear ground-reaction force; PExtMoment, peak knee extension moment; PAbdMoment, peak knee abduction moment.
Significantly different between landing styles for all participants (P < .05).
Significantly different between genders for the same landing style (P < .05).
DISCUSSION
Our hypothesis that stiff landings would produce significantly increased anterior tibial translation when compared with soft landings in healthy knees was not supported. Stiff landings produced significantly greater GRFs and knee extension moments, but did not cause increased amounts of anterior tibial translation or knee rotation in either varus/valgus or internal/external rotation when compared with soft landings in healthy individuals under these testing conditions. Previous literature has predicted that reduced KFA13,40 and the combination of reduced knee flexion and increased GRF38 may place greater stress on the ACL, increasing the risk of injury. While the current study did not estimate the loads on the ACL, the results illustrate that more complex interactions are responsible for producing excessive amounts of translation and rotation in the knee during dynamic activities. The neuromuscular control of knee kinematics in a healthy population appears to be capable of compensating for the increased demand of stiffer landings caused by significantly higher GRFs without resulting in greater translation or rotation of the tibia relative to the femur when compared to soft landings. It is possible that when landing in a controlled, safe manner such as that which was completed in the current study, athletes are able to manipulate the timing and level of muscular activation to control tibiofemoral kinematics in response to changes in external load (ie, GRF). However, it should be stressed that because we did not compare how the loads were distributed over the soft tissues of the knee between the 2 landing styles, the larger GRFs and more extended knee position observed during stiff landings should still be considered dangerous to the ACL and other structures of the lower extremities particularly in competitive settings where movements are often unanticipated.
In addition to the similarities found between knee kinematics during soft and stiff landings, both tasks exhibited relatively low magnitudes of anterior tibial translation. This result again points to the ability of musculature and soft tissues to keep translations of the knee within a small, safe range during controlled tasks. Peak vertical GRF and peak knee extension moment were significantly greater for stiff landings compared with soft landings. This is attributable to the fact that soft landings allow the vertical GRF to be dissipated over a larger knee flexion range of motion than the stiff landings. Despite the differences in vertical GRF and knee extension moment, the 2 landing styles did not produce a significant difference between the peak shear component of the GRF.
To our knowledge, there have not been any studies that have reported 6 degrees of freedom tibiofemoral kinematic measurements during landing outside of our laboratory.41 However, our results are somewhat similar to those reported for walking. Two recent studies calculated 6 degrees of freedom translations and rotations of the knee during walking.30,31 Li et al31 measured knee kinematics for a single individual while walking at 1.5, 2.0, 2.5, and 3.0 m/s. Results showed anterior tibial translation to range from approximately 5 mm during midstance to 22.5 mm at toe-off, with no kinematic differences observed between the tested walking speeds. A study by Kozanek et al30 also used biplane fluoroscopy to measure knee kinematics during gait of 8 healthy individuals at 1.5 m/s. Similar to Li et al, maximum anterior tibial translation was approximately 4 mm near midstance, and maximum posterior tibial translation was approximately 2.5 mm near toe-off. In the present study, maximum absolute anterior tibial translation was 6.4 ± 2.4 mm and 6.7 ± 2.9 mm for stiff and soft landings, respectively. The subtle increase in anterior tibial translation with relation to previously reported walking data may be expected, because external forces are approximately 2 to 3 times larger in landing tasks than walking.37 Alternatively, differences in translation data between this and previous studies may in part be attributable to differing tibial and femoral coordinate systems. In both the Li et al and Kozanek et al reports, kinematic variables were calculated as translations of the femur with respect to the tibia. In the current study, translations were calculated as movements of the tibia with relation to the femur as described by Grood and Suntay.18 Thus the differing methods of translation calculation, as well as task differences, may explain the small differences in observed tibial translation between studies.
Our in vivo dynamic measurements of anterior tibial translation during landing were less than that commonly measured statically in vivo using the KT-1000 arthrometer (MedMetric, San Diego, California). The KT-1000 arthrometer is commonly used to measure static displacement of the tibia with respect to the femur in vivo. A study by Daniel et al11 measured anterior tibial translation of 240 normal knees using the KT-1000 arthrometer as 20 lb of anterior force was applied to the tibia. The average anterior translation of the knee when relaxed was 7.2 (±1.9) mm. Investigators also measured tibial translation when the quadriceps were active and found an average of 5.2 mm of anterior tibial translation. Numerous cadaveric studies have been completed to determine the relationship between translation and ACL strain in vitro.29,42-44 For example, Woo et al44 reported that normal knees could experience up to 13.6 ± 0.8 mm of anterior tibial translation to occur before ACL rupture. These studies support the findings of our current investigation, because absolute tibial translations during soft and stiff landings were within the normal range of tibial translations measured by in vitro work, and were reasonably similar to KT-1000 arthrometer measurements taken when the quadriceps are active.
In the current study, verbal cues were used to instruct participants on how to land “soft” and “stiff.” This method of instruction was chosen because verbal instructions have been reported to effectively reduce the number of noncontact ACL injuries when combined with balance and strength training.21,34 Further, these oral instructions were reported to reduce knee abduction angle and GRF, while increasing absorption time and peak KFA for landings.23 These adaptations have been suggested to reduce the risk of ACL injury, and have been shown to be effective even without balance and strength training.10
We recognize some limitations of the current study. First, participants landed in a controlled laboratory setting. Therefore, they did not experience a true “in-game” scenario in which ACL injuries generally occur. We selected a vertical drop-landing task because a version of this movement is what has been utilized to screen individuals for noncontact ACL injury risk with notable successes.22 We acknowledge that these 2 landing styles did not produce a significant difference between the peak shear component of the GRF. The shear component of the GRF during dynamic movements has been shown to affect knee joint stability by increasing the shear joint reaction force on the proximal end of the tibia.37 In addition, no real-time feedback was provided to participants discriminating between soft and stiff landings. Rather, each participant was given verbal cues and took several practice jumps for each landing style before data were collected. This method of guidance was chosen to match the methodology of previous ACL injury prevention programs in which athletes were trained to land more softly. Finally, this sample of athletes did not employ landing styles that display high valgus knee angles or high abduction knee moments. Follow-up studies should test males and females who would be identified as “at risk” for ACL injury because of their abnormal frontal plane landing mechanics.
In conclusion, kinematic variables often associated with ACL injury, which included anterior tibial translation, valgus angle, and internal rotation angle, were not different between soft and stiff landings in healthy individuals. The results of this study demonstrate the ability of the musculature and soft tissues around the knee joint to keep translations and rotations of the knee within a small, safe range during controlled tasks of differing demand.
ACKNOWLEDGMENT
The authors thank Andrea North, Elizabeth Hageman, and Nicole Pinwell for help with the data collection and the reduction process. Medis Specials is acknowledged for the use of the Model-Based RSA software. Support from the NIH (see conflict of interest statement) is gratefully acknowledged.
This study was funded in part by the Steadman Philippon Research Institute and the National Institutes of Health (grant no. AR39683). The Steadman Philippon Research Institute is a 501(c)(3) nonprofit institution supported financially by private donations and corporate support from the following entities: Smith & Nephew Endoscopy, Arthrex, Siemens Medical Solutions USA, Saucony, OrthoRehab, Ossur Americas, Alignmed LLC, and Opedix.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding
REFERENCES
- 1.Ahmed AM, Hyder A, Burke DL, Chan KH. In-vitro ligament tension pattern in the flexed knee in passive loading. J Orthop Res. 1987;5(2):217–230. doi: 10.1002/jor.1100050208. [DOI] [PubMed] [Google Scholar]
- 2.Anderst W, Zauel R, Bishop J, Demps E, Tashman S. Validation of three-dimensional model-based tibio-femoral tracking during running. Med Eng Phys. 2009;31(1):10–16. doi: 10.1016/j.medengphy.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ASTM E177-08. Standard Practices for Use of the Terms Precision and Bias in ASTM Test Methods. ASTM International; West Conshohocken, PA: 2008. [Google Scholar]
- 4.Bey MJ, Zauel R, Brock SK, Tashman S. Validation of a new model-based tracking technique for measuring three-dimensional, in vivo glenohumeral joint kinematics. J Biomech Eng. 2006;128(4):604–609. doi: 10.1115/1.2206199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beynnon BD, Fleming BC, Johnson RJ, Nichols CE, Renstrom PA, Pope MH. Anterior cruciate ligament strain behavior during rehabilitation exercises in vivo. Am J Sports Med. 1995;23(1):24–34. doi: 10.1177/036354659502300105. [DOI] [PubMed] [Google Scholar]
- 6.Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 7.Chappell JD, Creighton RA, Giuliani C, Yu B, Garrett WE. Kinematics and electromyography of landing preparation in vertical stop-jump: risks for noncontact anterior cruciate ligament injury. Am J Sports Med. 2007;35(2):235–241. doi: 10.1177/0363546506294077. [DOI] [PubMed] [Google Scholar]
- 8.Collins TD, Ghoussayni SN, Ewins DJ, Kent JA. A six degrees-of-freedom marker set for gait analysis: repeatability and comparison with a modified Helen Hayes set. Gait Posture. 2009;30(2):173–180. doi: 10.1016/j.gaitpost.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 9.Conn JM, Annest JL, Gilchrist J. Sports and recreation related injury episodes in the US population, 1997-99. Inj Prev. 2003;9(2):117–123. doi: 10.1136/ip.9.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cowling EJ, Steele JR, McNair PJ. Effect of verbal instructions on muscle activity and risk of injury to the anterior cruciate ligament during landing. Br J Sports Med. 2003;37(2):126–130. doi: 10.1136/bjsm.37.2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daniel DM, Stone ML, Sachs R, Malcom L. Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med. 1985;13(6):401–407. doi: 10.1177/036354658501300607. [DOI] [PubMed] [Google Scholar]
- 12.de Asla RJ, Wan L, Rubash HE, Li G. Six DOF in vivo kinematics of the ankle joint complex: application of a combined dual-orthogonal fluoroscopic and magnetic resonance imaging technique. J Orthop Res. 2006;24(5):1019–1027. doi: 10.1002/jor.20142. [DOI] [PubMed] [Google Scholar]
- 13.Decker MJ, Torry MR, Wyland DJ, Sterett WI, Richard Steadman J. Gender differences in lower extremity kinematics, kinetics and energy absorption during landing. Clin Biomech (Bristol, Avon) 2003;18(7):662–669. doi: 10.1016/s0268-0033(03)00090-1. [DOI] [PubMed] [Google Scholar]
- 14.Devita P, Skelly WA. Effect of landing stiffness on joint kinetics and energetics in the lower extremity. Med Sci Sports Exerc. 1992;24(1):108–115. [PubMed] [Google Scholar]
- 15.Garling EH, Kaptein BL, Geleijns K, Nelissen RG, Valstar ER. Marker configuration model-based roentgen fluoroscopic analysis. J Biomech. 2005;38(4):893–901. doi: 10.1016/j.jbiomech.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 16.Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36(8):1476–1483. doi: 10.1177/0363546508318188. [DOI] [PubMed] [Google Scholar]
- 17.Granan LP, Bahr R, Steindal K, Furnes O, Engebretsen L. Development of a national cruciate ligament surgery registry: the Norwegian National Knee Ligament Registry. Am J Sports Med. 2008;36(2):308–315. doi: 10.1177/0363546507308939. [DOI] [PubMed] [Google Scholar]
- 18.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105(2):136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 19.Hanson GR, Suggs JF, Freiberg AA, Durbhakula S, Li G. Investigation of in vivo 6DOF total knee arthroplasty kinematics using a dual orthogonal fluoroscopic system. J Orthop Res. 2006;24(5):974–981. doi: 10.1002/jor.20141. [DOI] [PubMed] [Google Scholar]
- 20.Herzog W, Read LJ. Lines of action and moment arms of the major force-carrying structures crossing the human knee joint. J Anat. 1993;182(Pt 2):213–230. [PMC free article] [PubMed] [Google Scholar]
- 21.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 22.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 23.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24(6):765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 24.Hurschler C, Seehaus F, Emmerich J, Kaptein BL, Windhagen H. Comparison of the model-based and marker-based roentgen stereo-photogrammetry methods in a typical clinical setting. J Arthroplasty. 2009;24(4):594–606. doi: 10.1016/j.arth.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 25.Huston LJ, Vibert B, Ashton-Miller JA, Wojtys EM. Gender differences in knee angle when landing from a drop-jump. Am J Knee Surg. 2001;14(4):215–220. [PubMed] [Google Scholar]
- 26.Ishibashi Y, Rudy TW, Livesay GA, Stone JD, Fu FH, Woo S. The effect of anterior cruciate ligament graft fixation site at the tibia on knee stability: evaluation using a robotic testing system. Arthroscopy. 1997;13:177–182. doi: 10.1016/s0749-8063(97)90152-3. [DOI] [PubMed] [Google Scholar]
- 27.Kaptein BL, Valstar ER, Stoel BC, Reiber HC, Nelissen RG. Clinical validation of model-based RSA for a total knee prosthesis. Clin Orthop Relat Res. 2007;464:205–209. [PubMed] [Google Scholar]
- 28.Kaptein BL, Valstar ER, Stoel BC, Rozing PM, Reiber JH. Evaluation of three pose estimation algorithms for model-based roentgen stereophotogrammetric analysis. Proc Inst Mech Eng H. 2004;218(4):231–238. doi: 10.1243/0954411041561036. [DOI] [PubMed] [Google Scholar]
- 29.Kennedy JC, Hawkins RJ, Willis RB, Danylchuck KD. Tension studies of human knee ligaments. Yield point, ultimate failure, and disruption of the cruciate and tibial collateral ligaments. J Bone Joint Surg Am. 1976;58(3):350–355. [PubMed] [Google Scholar]
- 30.Kozanek M, Hosseini A, Liu F, et al. Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech. 2009;42(12):1877–1884. doi: 10.1016/j.jbiomech.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li G, Kozanek M, Hosseini A, Liu F, Van de Velde SK, Rubash HE. New fluoroscopic imaging technique for investigation of 6DOF knee kinematics during treadmill gait. J Orthop Surg Res. 2009;4:6. doi: 10.1186/1749-799X-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li G, Van de Velde SK, Bingham JT. Validation of a non-invasive fluoroscopic imaging technique for the measurement of dynamic knee joint motion. J Biomech. 2008;41(7):1616–1622. doi: 10.1016/j.jbiomech.2008.01.034. [DOI] [PubMed] [Google Scholar]
- 33.Li G, Wan L, Kozanek M. Determination of real-time in-vivo cartilage contact deformation in the ankle joint. J Biomech. 2008;41:128–136. doi: 10.1016/j.jbiomech.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 34.Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 35.Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GA, Slauterbeck JL. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13:930–935. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]
- 36.McNair PJ, Marshall RN, Matheson JA. Important features associated with acute anterior cruciate ligament injury. N Z Med J. 1990;103(901):537–539. [PubMed] [Google Scholar]
- 37.McNitt-Gray JL. Kinetics of the lower extremities during drop landings from three heights. J Biomech. 1993;26(9):1037–1046. doi: 10.1016/s0021-9290(05)80003-x. [DOI] [PubMed] [Google Scholar]
- 38.Pflum MA, Shelburne KB, Torry MR, Decker MJ, Pandy MG. Model prediction of anterior cruciate ligament force during drop-landings. Med Sci Sports Exerc. 2004;36(11):1949–1958. doi: 10.1249/01.mss.0000145467.79916.46. [DOI] [PubMed] [Google Scholar]
- 39.Sell TC, Ferris CM, Abt JP, et al. Predictors of proximal tibia anterior shear force during a vertical stop-jump. J Orthop Res. 2007;25(12):1589–1597. doi: 10.1002/jor.20459. [DOI] [PubMed] [Google Scholar]
- 40.Shelburne KB, Pandy MG, Torry MR. Comparison of shear forces and ligament loading in the healthy and ACL-deficient knee during gait. J Biomech. 2004;37(3):313–319. doi: 10.1016/j.jbiomech.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 41.Torry MR, Shelburne KB, Peterson DS, et al. Knee kinematic profiles during drop landings: a biplane fluoroscopy study. Med Sci Sports Exerc. 2011;43(3):533–541. doi: 10.1249/MSS.0b013e3181f1e491. [DOI] [PubMed] [Google Scholar]
- 42.Trent PS, Walker PS, Wolf B. Ligament length patterns, strength, and rotational axes of the knee joint. Clin Orthop Relat Res. 1976;117:263–270. [PubMed] [Google Scholar]
- 43.Woo SL, Adams DJ. The tensile properties of human anterior cruciate ligament (ACL) and ACL graft tissues. In: Daniel DM, Akeson W, O'Connor J, editors. Knee Ligaments: Structure, Function, Injury, and Repair. Raven Press; New York, NY: 1990. pp. 279–290. [Google Scholar]
- 44.Woo SL, Hollis JM, Adams DJ, Lyon RM, Takai S. Tensile properties of the human femur-anterior cruciate ligament-tibia complex: the effects of specimen age and orientation. Am J Sports Med. 1991;19(3):217–225. doi: 10.1177/036354659101900303. [DOI] [PubMed] [Google Scholar]
- 45.Yu B, Garrett WE. Mechanisms of non-contact ACL injuries. Br J Sports Med. 2007;41(Suppl 1):i47–i51. doi: 10.1136/bjsm.2007.037192. [DOI] [PMC free article] [PubMed] [Google Scholar]