Abstract
Background
Our previous research suggested the involvement γ-aminobutyric acid (GABA), in particular the GABAB receptor subtype, in the interoceptive effects of Δ9-tetrahydrocannabinol (Δ9-THC). The aim of the present study was to determine the potential involvement of the GABAA receptor subtype by assessing the separate and combined effects of the GABAA positive allosteric modulator diazepam and Δ9-THC using pharmacologically selective drug-discrimination procedures.
Methods
Ten cannabis users learned to discriminate 30 mg oral Δ9-THC from placebo and then received diazepam (5 and 10 mg), Δ9-THC (5, 15 and 30 mg) and placebo, alone and in combination. Self-report, task performance and physiological measures were also collected.
Results
Δ9-THC functioned as a discriminative stimulus, produced subjective effects typically associated with cannabinoids (e.g., High, Stoned, Like Drug) and elevated heart rate. Diazepam alone impaired performance on psychomotor performance tasks and increased ratings on a limited number of self-report questionnaire items (e.g., Any Effect, Sedated), but did not substitute for the Δ9-THC discriminative stimulus or alter the Δ9-THC discrimination dose-response function. Similarly, diazepam had limited impact on the other behavioral effects of Δ9-THC.
Conclusions
These results suggest that the GABAA receptor subtype has minimal involvement in the interoceptive effects of Δ9-THC, and by extension cannabis, in humans.
Keywords: drug-discrimination, marijuana, subjective effects, repeated acquisition task, digit-symbol-substitution task, cardiovascular
1. INTRODUCTION
A key function of endogenous cannabinoids is to act as synaptic retrograde messengers, thereby controlling the release of other neurotransmitters, including γ-aminobutyric acid (GABA; Schlicker and Kathmann, 2001). In an initial study we probed the involvement of GABA in the interoceptive effects of Δ9-tetrahydrocannabinol (Δ9-THC) in humans by administering the GABA reuptake inhibitor tiagabine alone and in combination with Δ9-THC in subjects trained to discriminate oral Δ9-THC from placebo (Lile et al., 2012a). Tiagabine alone occasioned Δ9-THC-appropriate responding, and when combined with Δ9-THC, produced leftward/upward shifts in the dose response curves for drug-appropriate responding, subjective response and performance impairment. Comparable results were obtained in a study that employed similar methods and combined Δ9-THC with nabilone, another cannabinoid agonist (Lile et al., 2011). Taken together, these studies supported the involvement of GABA in the interoceptive and performance effects of Δ9-THC in humans.
Because tiagabine produces global elevations in GABA, the contribution of particular receptor subtypes in the cannabimimetic effects of increased GABA levels could not be determined from our prior study. A follow-up study that also used drug-discrimination and drug combination procedures was conducted to begin to isolate the receptor subtype(s) that might underlie the apparent interaction between cannabinoid and GABA systems in human behavior (Lile et al., 2012b). In that study, baclofen, a direct agonist at metabotropic GABAB receptors, produced a profile of effects that overlapped considerably with what was observed with tiagabine and nabilone when combined with Δ9-THC. Those results suggested that the enhancement of cannabinoid sensitive outcomes by tiagabine in the initial study was due, in large part, to elevated GABA increasing the activation of GABAB receptors.
The present study sought to determine if the ionotropic GABAA receptor subtype was also involved in the interoceptive and performance effects of Δ9-THC by testing Δ9-THC in combination with diazepam in human subjects trained to discriminate oral Δ9-THC. Diazepam, first marketed as Valium®, is a benzodiazepine sedative-hypnotic drug that functions as a positive allosteric modulator of GABAA receptors. A direct GABAA agonist was not used due to side effects associated with that class of drugs (e.g., dissociative hallucinations with muscimol), as well as their limited availability for use in humans. Diazepam was selected over other GABAA positive allosteric modulators because earlier preclinical work demonstrated that diazepam engendered partial drug-appropriate responding in animals trained to discriminate Δ9-THC (Barrett et al., 1995; Browne and Weissman, 1981; Järbe and Hiltunen, 1988; Mokler et al., 1986; Wiley and Martin, 1999). These Δ9-THC-like discriminative stimulus effects of diazepam appear to be mediated by its interaction with GABAA, rather than cannabinoid, receptors because the partial substitution in animals trained to discriminate Δ9-THC was blocked by the benzodiazepine antagonist flumazenil (Mokler et al., 1986) but not the inverse cannabinoid agonist/antagonist rimonabant (Wiley and Martin, 1999). There have been no prior studies that have tested diazepam in humans who have learned to discriminate Δ9-THC from placebo.
2. METHODS
2.1. Subjects
Adult men and women reporting weekly cannabis use were recruited from the local community. Potential subjects completed demographic, drug-use and medical history questionnaires, as well as medical screens. Individuals with current or past histories of Axis I disorders according to DSM-IV criteria (American Psychiatric Association, 2000), including substance dependence other than tobacco, were excluded from participating. Substance abuse was not an exclusion criterion. The Institutional Review Board of the University of Kentucky Medical Center approved the study and the informed consent document.
Ten subjects (1 black male, 4 white females and 5 white males) completed the protocol. Three additional subjects were enrolled and completed at least one session in which a drug dose was administered; two subjects failed to acquire the discrimination and another completed six sessions and then was lost to follow up. Subjects who completed the study ranged in age from 18 to 29 years (median = 22 years), in education from 10 to 16 years (median = 13), and in weight from 53 to 120 kg (median = 72 kg). All reported cannabis use (range of 2 to 7 days/week, mean = 5). Five subjects reported consuming alcohol-containing beverages on a weekly basis (range = 1-18 drinks per week). Five subjects reported daily tobacco cigarettes use (range = 1-15 cigarettes per day). Other lifetime non-medical drug use included benzodiazepines (2 subjects, no reported use in the month prior to screening), hallucinogens (three subjects, no reported use in the month prior to screening), opioids (two subjects, no reported use in the month prior to screening) and stimulants (seven subjects, with one reporting oral amphetamine use three times in the month prior to participation). During screening, subjects provided a urine sample that was assessed for recent use of amphetamine, cocaine, cannabis, methamphetamine, opioids, phencyclidine, benzodiazepines, barbiturates, methadone and 3,4-methylenedioxy-N-methamphetamine (Integrated E-Z Split Cut, Acon Laboratories, San Diego, CA); all subjects provided a urine sample positive for cannabinoids and negative for other substances prior to beginning the study.
2.2. General Procedures
Subjects were enrolled as outpatients at the University of Kentucky Residential Research Facility. They completed two drug-free practice sessions to become familiarized with the procedures prior to completing between 21 and 26 (mean = 23) experimental sessions. Study participation lasted 5 to 12 weeks (mean = 8).
Subjects were informed that they would receive placebo, Δ9-THC and diazepam, alone or in combination, but were blind to the dose and order of administration. They were asked to abstain from illicit drugs other than cannabis, as well as over-the-counter medications, with the exception of non-steroidal anti-inflammatory analgesics, for the duration of the experiment, and any drug use on the day of experimental sessions to avoid potentially unsafe drug interactions. In addition, subjects were asked to refrain from food or caffeine intake for 4 hours prior to each experimental session, or alcohol for 12 hours prior to and following each experimental session. Subjects who smoked tobacco cigarettes were also asked to abstain from smoking the morning of each session, but were allowed to smoke a single tobacco cigarette upon arrival to the laboratory to avoid testing under conditions of nicotine withdrawal, but not again until the session had ended. There was no indication of nicotine withdrawal in these subjects.
Experimental sessions were conducted at a fixed time, Monday through Friday, and lasted approximately 7.5h; subjects participated in 1 to 5 sessions per week. At the beginning of each session, breath (Alcolyzer, AK Solutions USA, Palisades Park, NJ) and urine tests to assess drug use (described above) and pregnancy (hCG Assay, Rapid Detect, Inc., Poteau, OK) were conducted. Urine samples were negative for substances other than cannabis metabolites (i.e., 11-nor-9-carboxy-Δ9-THC) and pregnancy throughout the study, with the following exceptions. Urine toxicology screening was positive for recent opioid use in one subject and for recent amphetamine use in another subject; in both cases, the subjects were discharged from that session, but were permitted to continue study participation once a urine sample negative for all non-cannabinoid drugs was provided. At session intake, subjects also completed a modified version of the U.S. Department of Transportation Drug Evaluation and Classification Screening (walk and turn, timed one-leg balance or Romberg balance, time interval reproduction and the finger-to-nose tests; Toland and Green, 1991) and were observed by the research staff for signs of cannabis intoxication (e.g., bloodshot, glassy eyes); no cannabis intoxication was detected during intake throughout the study. Subjects were reassessed at the end of the session for possible intoxication and/or residual drug effects prior to release. In addition, subjects were required to report no further drug effects.
Subjects consumed a low-fat snack approximately 20 minutes prior to drug administration. Because of differences in the time at which peak drug concentrations were predicted to occur (Hollister et al, 1981; Hillestad et al., 1974), diazepam was administered 1 h after Δ9-THC. Data collection time points refer to Δ9-THC administration.
2.3. Drug-Discrimination Procedure
Well-established drug-discrimination procedures (e.g., Lile et al., 2009; Rush et al., 1998) were used to teach subjects to discriminate between a “Drug X” condition (i.e., 30 mg Δ9-THC) and a “Not Drug X” condition (i.e., placebo).
Sampling Phase. During two sampling sessions, subjects ingested four capsules that contained a total of 30 mg Δ9-THC. The capsules were identified by a letter code (e.g., Drug X; a unique letter code was used for each subject); subjects were not informed that the capsules contained Δ9-THC, but were instructed to associate drug effects with the letter code.
Control Phase. A control phase, lasting between 4 and 12 sessions, was conducted to determine whether subjects could discriminate 30 mg Δ9-THC from placebo. During this phase, subjects ingested capsules under double-blind conditions. The order of drug administration was random except that all subjects received each training condition, 30 mg Δ9-THC and placebo, at least twice every four sessions. Sessions were identical to the sampling phase, except subjects were not informed which drug condition (i.e., Drug X or Not Drug X) was administered until the end of the session. The criterion for having acquired the discrimination was ≥ 80% correct responding on the drug-discrimination task during the final 5-h assessment for four consecutive sessions. When a subject did not meet the control criteria within 12 sessions, they were dismissed from the study.
Test Phase. A final test phase, lasting at least 16 sessions, was conducted to test placebo, Δ9-THC (5, 15 and 30 mg) and diazepam (5 and 10 mg), alone and in combination. Each drug dose and dose combination was administered once for a total of 12 sessions. The order of drug administration was random except that an active drug dose was never administered on more than three consecutive sessions (i.e., placebo was administered at least every three sessions), and the highest dose of Δ9-THC (30 mg) and diazepam (10 mg) were not administered together before a lower dose combination was tested.
Four control sessions (i.e., 30 mg Δ9-THC or placebo) were also randomly included in the test phase to monitor drug-discrimination performance and provide feedback to subjects regarding their performance. If a subject responded incorrectly on a control session, additional control sessions were scheduled until the subject accurately identified both of the training conditions once each across consecutive sessions. Four subjects incorrectly identified the placebo condition on a single occasion and had two additional sessions (i.e., one each of 30 mg Δ9-THC and placebo) inserted into their dosing schedule. One subject only received three of these control sessions during the test phase due to a scheduling conflict.
2.4. Outcome measures
Drug discrimination was the primary outcome measure, supplemented by self-report questionnaires, performance tasks and physiological assessments. Data were collected in fixed order, immediately prior to drug administration, and 1, 2, 3, 4, 5 and 6 h after Δ9-THC administration, with the following exceptions. The drug-discrimination task was completed at only the 3 to 6 h time points because of the slow onset of the effects of Δ9-THC observed in our previous studies (e.g., Lile et al., 2013). A non-contingent Multiple-Choice Procedure was completed at the end of the 6-h assessment. Except for temperature assessments, data were collected on an Apple Macintosh computer (Apple Computer, Inc., Cupertino, CA).
2.4.1 Drug-Discrimination Task
Two circles labeled Drug X and Not Drug X and associated counters were displayed on a computer screen. Button presses increased the counter for a particular circle according to a fixed-interval 1-sec schedule for 60 s (no change-over delay). At the end of the final assessment, subjects were informed whether it was a control or a test session. During control sessions, points accumulated on the correct option were exchangeable for money at a rate of $0.21/point (up to approximately $50.00/session). During test sessions, when drugs and/or doses other than the control conditions were administered, subjects earned the average from all previous sessions in which control conditions were tested. These monetary contingencies prompted subjects to acquire points on the counters based on the presence (or absence) of the training drug cue at the time of task performance during both control and test sessions. The dependent variable for this task was the percent responding on the drug-appropriate option at the 6-h time point.
2.4.2 Subject-Rated Questionnaires
Visual Analog Scale (VAS) Subject-Rated Drug-Effect Questionnaire. Subjects rated 20 items (see Lile et al., 2012a) that assessed general “positive” (e.g., Good Effects, Like Drug) and “negative” (e.g., Bad Effects, Nauseated) drug effects, as well as items specific to cannabis intoxication (e.g., Stoned). Items were presented individually on the computer by marking a 100-unit line anchored on the extremes by “Not At All” and “Extremely”.
2.4.3 Multiple-Choice Procedure
This task provided a hypothetical assessment of the monetary value of each dose condition (Griffiths et al., 1993). Subjects made a series of nine discrete choices between the drug dose received during that session and ascending amounts of money. The dollar value increased across the choices ($0.10, 0.25, 0.50, 1.00, 2.00, 4.00, 8.00, 16.00 and 32.00). The dependent measure on the Multiple-Choice Procedure was the maximum dollar value at which subjects chose drug over money (i.e., “crossover point”).
2.4.4 Performance Tasks
These tasks were chosen because prior research has found them to be sensitive to the impairing effects of oral Δ9-THC (Hart et al., 2005; Kamien et al., 1994) and smoked cannabis (Heishman et al., 1989; Kelly et al., 1990, 1993; Wilson et al., 1994). Subjects did not receive additional compensation based on task performance.
2.4.5 Repeated Acquisition of Response Sequences Task (RA task)
During the initial acquisition component, subjects pressed 4 keys (1, 3, 7 and 9) on a numeric keypad to learn a new, randomly-determined 10-response sequence (a “chain”) for 180 s. When a correct key in the sequence was pressed, a “position” counter on the screen increased by 1. When the tenth and final key in the sequence was pressed, a “points” counter increased by one, and the position counter reset. A 60-s performance component of this task, in which the 10-response sequence remained the same across trials, followed the acquisition component. The primary dependent measures for this task were the number of chains completed (i.e., accuracy) and the total number of responses emitted (i.e., response rate).
2.4.6 Digit-Symbol-Substitution Test (DSST)
A modified version of the computerized DSST was used (McLeod et al., 1982). Briefly, subjects used a numeric keypad to enter the geometric pattern associated with one of nine patterns identified on a given trial for 90 s. The dependent measures were the number of patterns the subject entered correctly (i.e., trials correct; accuracy) and the total number of patterns entered (i.e., trials completed; response rate).
2.4.7 Time Reproduction Task
Four time periods, 3, 30, 60 and 180s were presented. Subjects responded to start a timer, and held down the response key until they believed that the interval had elapsed.
2.4.8 Physiological Indices
Heart Rate and Blood Pressure. Heart rate and blood pressure were recorded using an automated monitor (DINAMAP, Johnson and Johnson, Alexandria, TX).
2.4.9 Temperature
An infrared thermographic scanner (Derma-Temp, Exergen Corporation, Watertown, MA) was used to measure skin temperature on the tip of the index finger. An electronic thermometer was used to measure oral temperature.
2.5. Drug Administration
Across their participation, subjects received placebo, 5, 15 and 30 mg of Δ9-THC, and 5 and 10 mg of diazepam, alone and in combination. Doses of Δ9-THC were prepared by encapsulating commercially available capsules of Marinol® (Δ9-THC in sesame oil, Solvay Pharmaceuticals, Marietta, GA) in three opaque green size 00 capsules. A generic formulation of diazepam was administered in one opaque blue/white size 0 capsule. Cornstarch was used to fill the remainder of all capsules. Placebo capsules contained only cornstarch. For reference, the acute recommended Δ9-THC dosing range in adults for appetite stimulation and the prevention of nausea and vomiting is 2.5 to 20 mg (Marinol® Product Information, 2006). The recommended acute oral dosage of diazepam for the treatment of anxiety is 2-10 mg (Valium® Product Information, 2013).
2.6. Data Analyses
Data from all ten subjects were analyzed statistically. Drug-discrimination data were analyzed as percent drug-appropriate responding using two-factor, repeated-measure analysis of variance (ANOVA; JMP, SAS Institute Inc., Cary, NC) with Δ9-THC and diazepam as the factors. For the 30 mg Δ9-THC and placebo conditions, data were averaged across the sessions in which these conditions were presented during the test phase. Raw data from the self-reported drug-effect questionnaires, performance tasks and physiological measures were analyzed for each drug as the peak-effect (i.e., the mean of the maximum or minimum value observed for each subject 1 to 6 h after drug administration) using two-factor, repeated-measure ANOVA. Crossover point data from the Multiple-Choice Procedure were first subjected to a square-root transformation because of violations in the assumptions of ANOVA (i.e., monetary increments across successive choices range from $0.15 to $16.00). For all measures, effects were considered significant for p ≤ 0.05. If a main effect of Δ9-THC attained statistical significance, contrast statements were used to compare active drug doses to placebo; if a main effect of diazepam, or an interaction of Δ9-THC and diazepam, attained statistical significance, each dose of Δ9-THC alone was compared to that dose of Δ9-THC administered in combination with diazepam.
3. RESULTS
3.1. Drug-discrimination task
All subjects met the discrimination criterion in four sessions. During the final four sessions of the control phase, subjects reported an average of 0.0 (SEM = 0.0) percent Δ9-THC-appropriate responding on the drug-discrimination task during placebo sessions and 100.0 (SEM = 0.0) percent drug-appropriate responding during sessions when the training dose of Δ9-THC (i.e., 30 mg) was administered.
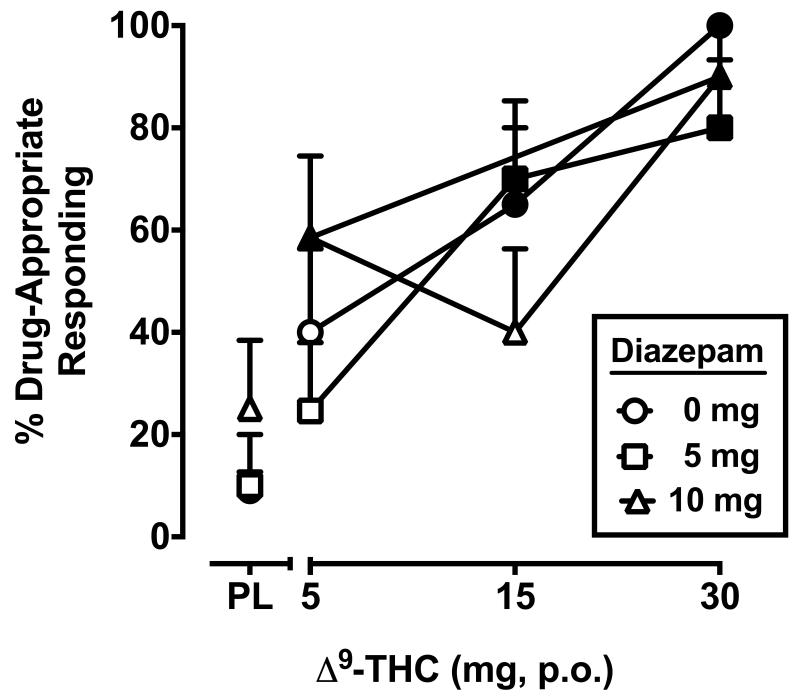
The two-factor, repeated-measure ANOVA revealed a significant main effect of Δ9-THC only (F3,27 = 27.5, p < 0.001). The separate and combined discriminative-stimulus effects of Δ9-THC and diazepam are shown in Figure 1. During the test phase, placebo and the training dose of Δ9-THC occasioned an average of 9.0 (SEM = 3.7) and 100.0 (SEM = 0.0) percent Δ9-THC-appropriate responding, respectively. Δ9-THC alone dose-dependently increased drug-appropriate responding on the drug-discrimination task. Diazepam did not occasion drug-appropriate responding alone or significantly impact the discriminative stimulus effects of Δ9-THC when combined.
Figure 1.
Separate and combined effects of Δ9-THC and diazepam on Δ9-THC-appropriate responding on the drug-discrimination task. Filled symbols indicate values that are significantly different from placebo. The x-axis represents the Δ9-THC dose in mg; PL denotes placebo. Data points show means of 10 subjects. Uni-directional brackets indicate 1 SEM.
3.2. Subject Ratings
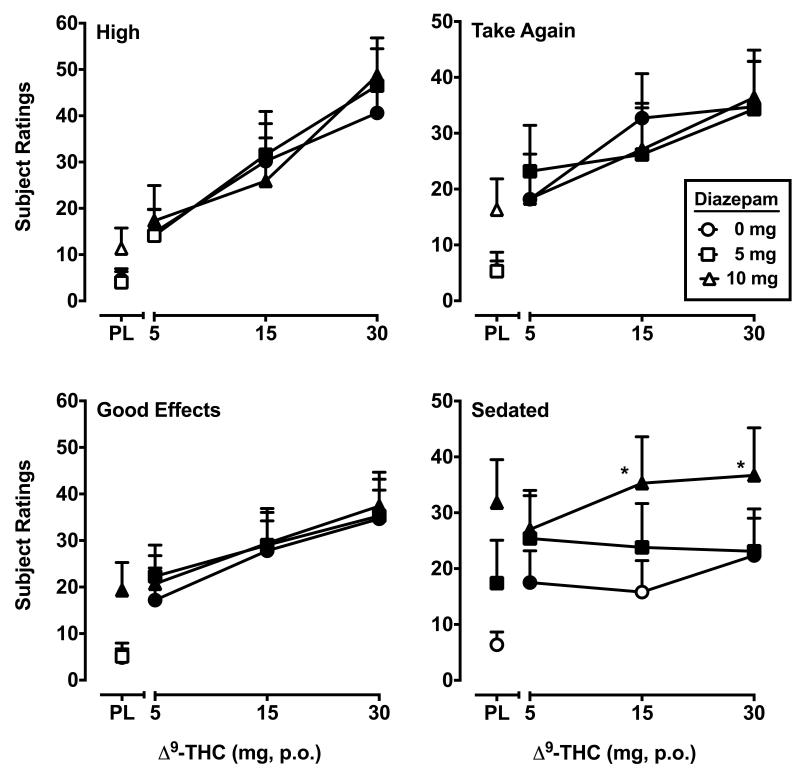
Significant main effects of only Δ9-THC (F’s3,27 = 3.2-22.0, p’s ≤ 0.05) were detected for eleven VAS items: Good Effects, Bad Effects, High, Like Drug, Stimulated, Take Again, Hungry, Thirsty, Stoned, Forgetful, Confused/Difficulty Concentrating. In general Δ9-THC produced orderly increases in subject ratings on these items as a function of dose and diazepam did not modify the subject-rated effects of Δ9-THC when combined. For three of the measures, pairwise comparisons revealed that ratings of Good Effects, Like Drug and Stoned were significantly increased by 10 mg dose of diazepam alone relative to placebo. A main effect of diazepam was observed for the questionnaire item Sedated (F2,18 = 8.3, p < 0.01), with both doses of diazepam increasing ratings on this item and producing parallel, upward shifts in the Δ9-THC dose response function. The data from VAS items Good Effects, High, Take Again and Sedated are presented in Figure 2. Main effects of both Δ9-THC (F3,27 = 19.0, p < 0.001) and diazepam (F2,18 = 5.2, p < 0.05) were detected for the item Any Effect. The high dose of diazepam (10 mg) and all Δ9-THC doses increased ratings of Any Effect, but the response to Δ9-THC was not changed by concurrent diazepam administration. An interaction between Δ9-THC and diazepam (F6,54 = 2.5, p < 0.05) was found for the item Pay For. As with Any Effect, the 10 mg dose of diazepam and all Δ9-THC doses increased ratings of Pay For, but the response to Δ9-THC was not altered by concurrent diazepam administration. Interactions between Δ9-THC and diazepam were also detected for Shaky/Jittery and Nauseated (F’s6,54 = 2.2, 2.3, p’s < 0.05). Responses to these items were of lower magnitude (less than approximately 20 out of 100 on a VAS) with the interaction stemming from an enhancement of the lowest dose of Δ9-THC by diazepam.
Figure 2.
Peak (maximum value) Visual Analog Scale ratings for Δ9-THC and diazepam, alone and in combination, on the drug-effect questionnaire items High, Take Again, Good Effect and Sedated. Asterisks indicate combinations of Δ9-THC and diazepam that are significantly different from that dose of Δ9-THC alone. All other details are as in Figure 1.
3.3. Multiple-Choice Procedure
Significant main effects of Δ9-THC (F3,27 = 4.2, p < 0.05) were observed for crossover point. Δ9-THC alone increased crossover point at the 15 mg ($1.60 ± 0.78; mean ± SEM) and 30 mg ($1.88 ± 0.72) doses relative to placebo ($0.05 ± 0.04). Diazepam doses did not increase crossover point when administered alone and failed to significantly influence crossover points for Δ9-THC when administered in combination.
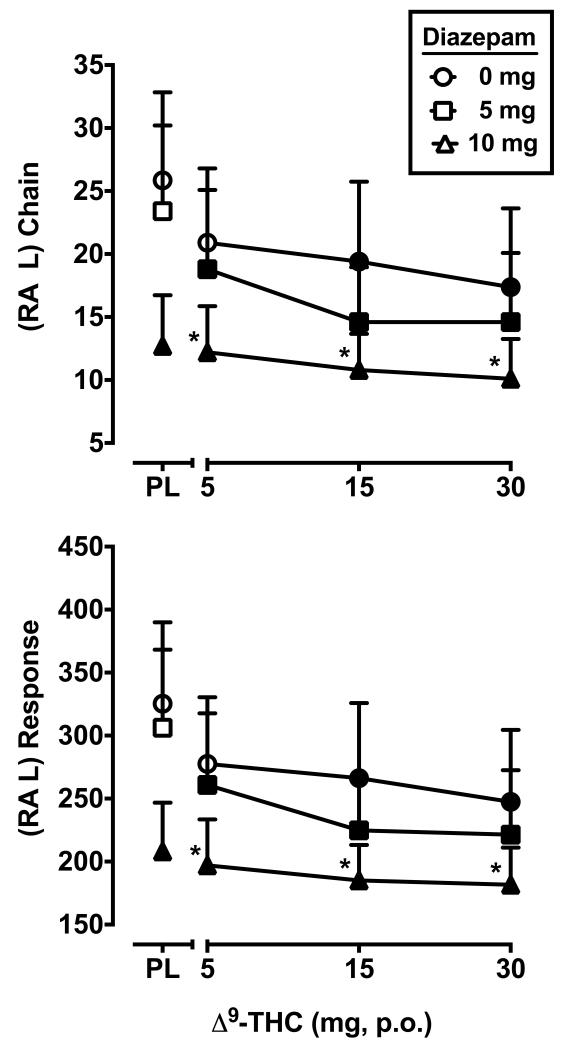
3.4. Performance
Main effects of Δ9-THC (F3,27 = 3.3, p < 0.05) and diazepam (F2,18 = 8.5, p < 0.01) were found for the number of chains completed (i.e., accuracy) on the acquisition component of the RA task. Main effects of Δ9-THC (F3,27 = 3.3, p < 0.05) and diazepam (F2,18 = 8.5, p < 0.01) were also found for the total number of responses emitted (i.e., rate) on this task component. For these outcomes, performance was impaired by the 15 and 30 mg doses of Δ9-THC, as well as the 10 mg dose of diazepam, relative to placebo. In combination, diazepam doses produced downward, parallel shifts of the Δ9-THC dose-response function, with statistically significant reductions in performance following administration of 10 mg diazepam + each active dose of Δ9-THC, relative to those doses of Δ9-THC alone. The effects of Δ9-THC and diazepam on rate and accuracy on the acquisition component of the RA task are presented in Figure 3.
Figure 3.
Peak number of chains completed and total responses on the repeated acquisition task (minimum value) for Δ9-THC and diazepam, alone and in combination. All other details are as in Figure 1.
With respect to the performance component of the RA task, main effects were found only for diazepam (F2,18 = 4.8, p < 0.05) and only for the number of chains completed. For this outcome, performance was impaired relative to placebo (90.8 ± 9.1) following administration of 30 mg Δ9-THC alone (78.7 ± 10.0), 5 mg (78.2 ± 9.3) and 10 mg of diazepam (79.7 ± 10.0) alone, and at every dose of Δ9-THC when combined with 10 mg diazepam (70.0 ± 12.5, 73.5 ± 9.7 and 77.8 ± 9.6, in ascending Δ9-THC dose order).
For the DSST, significant main effects of diazepam were detected for the number of trials completed (rate; F2,18 = 26.2, p < 0.001) and the number of correct trials (accuracy; F2,18 = 27.8, p < 0.001). Overall, 10 mg diazepam impaired performance on this task when administered alone and in combination with active Δ9-THC doses, whereas the 5 mg dose of diazepam reduced rate and accuracy on the DSST only when combined with the highest Δ9-THC doses. More specifically, when placebo was administered, subjects completed 80.0 ± 3.7 trials and were correct on 73.8 ± 2.8 of those trials. The 10 mg dose of triazolam alone reduced rate to 69.7 ± 5.3 trials and accuracy to 60.4 ± 4.9 trials. Rate and accuracy on the DSST were also decreased when 10 mg diazepam was combined with 5 mg Δ9-THC (63.2 ± 4.5 and 54.7 ± 5.6 trials), 15 mg Δ9-THC (67.3 ± 4.8 and 59.5 ± 3.4 trials) and 30 mg Δ9-THC (69.1 ± 5.2 and 59.8 ± 5.5 trials). Finally, 5 mg diazepam impaired performance when combined with 15 mg Δ9-THC (rate = 69.9 ± 4.0, accuracy = 62.0 ± 4.1 trials) and 30 mg Δ9-THC (accuracy = 65.8 ± 3.2 trials).
Neither Δ9-THC or diazepam affected reproduction of time for any interval (data not shown).
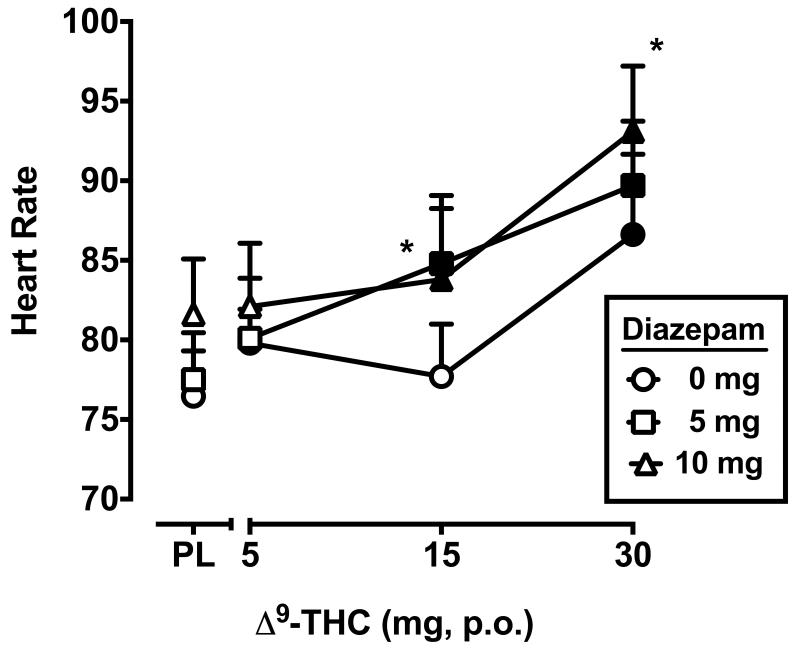
3.5. Heart Rate, Blood Pressure and Temperature
Significant main effects of Δ9-THC (F3,27 = 12.8, p < 0.001) and diazepam (F2,18 = 7.0, p < 0.01) were observed for heart rate, as illustrated in Figure 4. When administered separately, only Δ9-THC (30 mg) increased heart rate. When combined with the 15 mg dose of Δ9-THC, 5 and 10 mg diazepam significantly elevated heart rate relative to placebo, and 5 mg diazepam + 15 mg Δ9-THC significantly elevated heart rate relative to 15 mg Δ9-THC alone. An interaction between Δ9-THC and diazepam (F6,54 = 2.6, p < 0.05) was detected for systolic blood pressure; however, only a single dose combination (30 mg Δ9-THC + 5 mg diazepam) increased blood pressure compared to placebo. Diastolic blood pressure and temperature were not impacted by Δ9-THC or diazepam (data not shown).
Figure 4.
Peak heart rate (maximum value) for Δ9-THC and diazepam, alone and in combination. All other details are as in Figure 1.
4. DISCUSSION
4.1. Drug discrimination
The present study found no evidence of overlap in the discriminative-stimulus effects of diazepam and Δ9-THC. These results contrast with previous research that demonstrated partial substitution of diazepam for the Δ9-THC discriminative-stimulus in rats and monkeys (Barrett et al., 1995; Browne and Weissman, 1981; Järbe and Hiltunen, 1988; Mokler et al., 1986; Wiley and Martin, 1999). Full substitution was not observed with diazepam in those studies, but the partial substitution was replicated, whereas multiple drugs across several pharmacological classes have generally failed to produce Δ9-THC-like discriminative-stimulus effects under similar conditions (Barrett et al., 1995; Browne and Weissman, 1981). However, Δ9-THC did not occasion drug-appropriate responding in animals trained to discriminate diazepam demonstrating that the partial cross-generalization was asymmetrical (Järbe and Hiltunen, 1988; Wiley and Martin, 1999). In addition, the benzodiazepines chlordiazepoxide and midazolam failed to produce Δ9-THC-appropriate responding under conditions in which diazepam partially substituted (Barrett et al., 1995). In humans, triazolam also did not occasion Δ9-THC-like discriminative-stimulus effects, up to doses that impaired psychomotor performance (Lile et al., 2009). Together, these results indicate that there is minimal involvement of GABAA in the interoceptive cue produced by Δ9-THC, and that shared discriminative stimulus effects between Δ9-THC and benzodiazepines are limited to diazepam and only under certain training conditions and in non-human species.
4.2. Abuse potential of diazepam in cannabis users
Of the benzodiazepines, diazepam is considered to have a relatively high potential for abuse (Griffiths and Johnson, 2005). In addition, experimental assessment of the abuse potential of diazepam has demonstrated that individual differences such as sensation seeking status and alcohol use history can increase the likelihood that diazepam will produce “positive” subject-rated effects or be self-administered in the laboratory (de Wit et al., 1986; Kelly et al, 2009). Similarly, cannabis use history has been associated with a greater propensity to diazepam self-administration (Chutuape and de Wit, 1994), so it might have been predicted that diazepam would have produced robust positive subject-rated effects in the present study. In contrast, only a single VAS item reflective of abuse potential, Pay For, emerged as significant in the analysis (i.e., interaction between diazepam and Δ9-THC), with the effects of diazepam limited to an increase in ratings at the 10 mg dose alone. Pairwise comparisons also revealed that the 10 mg dose of diazepam increased ratings of Good Effects, Like Drug and Stoned relative to placebo without impacting the response Δ9-THC, though no statistically significant effects were found for the diazepam factor in the ANOVAs for those items. Significant main effects of diazepam were also found for the VAS items Sedated and Any Effect, as well as for several performance measures (see below), indicating that behaviorally relevant doses were tested. Although not directly compared, the minimal signal for abuse potential of diazepam in these subjects relative to the positive response to Δ9-THC on multiple self-report items and a hypothetical multiple choice procedure is suggestive of a preference for Δ9-THC over diazepam, consistent with cannabis as their drug of choice. Furthermore, these results suggest that benzodiazepines would have limited abuse potential if used as a therapeutic in cannabis dependent patients.
4.3. Side effects of diazepam and diazepam-cannabinoid combinations
Of the few VAS items for which an effect of diazepam was apparent, Sedated showed a diazepam-dose-dependent upward shift in subject ratings regardless of Δ9-THC dose, suggesting that ratings of Sedated could be attributed in large part to diazepam. In addition, diazepam significantly impaired psychomotor task performance on the DSST and the performance and acquisition components of the RA task. Δ9-THC also impaired performance when administered alone, though only for the acquisition component of the RA task, and the parallel downward shifts in performance on that task with concurrent diazepam administration suggest that impairment also was largely due to diazepam. These findings are consistent with the well-documented sedative and performance impairing effects of benzodiazepines in general, and diazepam specifically, observed in previous studies. When combined with Δ9-THC, diazepam significantly elevated heart rate above what was observed with Δ9-THC alone; three of the ten subjects met criteria for tachycardia (>100 bpm) when Δ9-THC was administered alone and only at the highest (i.e., 30 mg dose), whereas 1-3 subjects exceeded 100 bpm at every combination of active Δ9-THC and diazepam. Worth noting, however, is that no additional symptoms (e.g., blurry vision, sweating) indicative of a more serious cardiovascular problem were observed when tachycardia occurred. Although combinations of diazepam and Δ9-THC were generally well tolerated, caution and awareness of possible additive effects on heart rate and sedation/impairment is warranted in situations in which these drugs might be combined or when benzodiazepines would be indicated in cannabis users on an outpatient basis.
4.4 Limitations
Limitations of the present methodology have been described in detail previously (Lile et al., 2012a) and include the use of illicit drugs having short durations of action that might have been missed by toxicology screening and variability in cannabis use during outpatient participation. In addition, the present study used a staggered dosing procedure to account for anticipated differences in the onset of peak effects for Δ9-THC and diazepam. If the effects of Δ9-THC onset more rapidly than diazepam, however, the ability of diazepam to influence the discriminative-stimulus effects of Δ9-THC might have been reduced. To evaluate this possibility, the VAS item Any Effect was considered as a drug discrimination proxy measure that was assessed at all session time points, and the time-to-peak effects (TTP; omitting subject data from sessions in which a “0” rating was reported at all time points) for both drugs was calculated. The average TTP across active Δ9-THC only sessions (i.e., 5, 15 and 30 mg alone) was 3.1 h, whereas the average TTP across active diazepam sessions (i.e., 5 and 10 mg alone) was 2.6 h. Therefore, the difference in the time-to-peak effect was not as large as anticipated (i.e., 1 h), which might have impacted the results from the drug discrimination measure. However, important to emphasize is that the data from the final session time point (i.e., 6 h after Δ9-THC administration) were used for analysis of drug discrimination results. This strategy was adopted because the onset of action for orally administered Δ9-THC is highly variable (Lile et al., 2013). In addition, subjects are instructed that they can change their mind when reporting whether they received the Drug or Not Drug condition based on what they think each time the task is presented throughout the session. Thus, the use of this instruction set and analysis of the final hour drug discrimination data should have minimized the impact that variability in the onset of action for Δ9-THC alone and in combination with diazepam might have had on the drug discrimination results.
4.5. Role of GABAA in cannabinoid effects
As noted, when evaluated using similar procedures, the cannabinoid agonist nabilone, as well as the GABA reuptake inhibitor tiagabine and the GABAB agonist baclofen, produced overlapping behavioral effects with Δ9-THC and enhanced Δ9-THC effects. Together, those results suggest that GABA is involved in the behavioral effects of Δ9-THC, and by extension cannabis, and that the shared effects of tiagabine and Δ9-THC was due, in large part, to elevated GABA increasing the activation of GABAB receptors. In contrast, the present results do not support the involvement of GABAA in the discriminative-stimulus and subject-rated effects of Δ9-THC in cannabis users. Worth noting, however, is that there are similarities in some of the other behavioral effects of benzodiazepines such as diazepam and cannabinoid agonists. For example, diazepam produced a positive signal on three of the four tests included in the “tetrad” traditionally used to assess cannabinoid activity in rodents, specifically catalepsy, locomotor activity and antinociception (Wiley and Martin, 2003). As demonstrated here and elsewhere, rates of behavior on performance tasks are reduced in humans following administration of Δ9-THC or diazepam (e.g., Evans et al., 1996; Kelly et al., 1993). In addition, impairment of learning and memory processes is a well-characterized effect of GABAA positive allosteric modulators and cannabinoids (reviewed in Greenblatt, 1992; Ranganathan and D’Souza, 2006). A last example is that cannabinoids function as anxiolytics under certain conditions and doses, a main therapeutic indication of GABAA positive allosteric modulators (e.g., Glass et al., 1981; Witkin et al., 2005). Whether the behavioral similarities between GABAA positive allosteric modulators and cannabinoids are due to direct interactions between these neurotransmitter systems or through distinct neural mechanisms has received little attention and further research in this area would be informative.
4.6. GABAA ligands as medications for cannabis-use disorders
In part, this and our previous studies that assessed GABAergic compounds alone and in combination with Δ9-THC in cannabis users were undertaken in an effort to reveal neurobiological targets for future medications development efforts to manage cannabis-use disorders. To the extent that drugs that produce comparable interoceptive effects to Δ9-THC would be valuable as pharmacotherapies for cannabis-use disorders, diazepam does not appear to be a useful candidate. In addition, benzodiazepines, particularly diazepam, have the potential to be abused and have sedative and performance impairing side effects that could impact the safety of patients and others, as described above. Further, cessation from chronic benzodiazepine administration has been associated with a withdrawal syndrome that can include more serious signs such as seizures (Owen and Tyrer, 1983). However, it is possible that GABAA positive allosteric modulators with limited abuse potential and improved safety profiles such as zolpidem could address some of the complaints associated with cannabis abstinence thought to contribute to continued use (e.g., anxiety and difficulty sleeping) and research in this area is ongoing (Vandrey et al., 2011). Given the need for effective medications for cannabis-use disorders, research incorporating a variety of pharmacological approaches based on different theories of promoting cannabis abstinence is worthy of consideration.
Highlights.
- Diazepam shares discriminative stimulus effects with Δ9-THC in animals.
- This study tested diazepam in humans trained to discriminate Δ9-THC.
- Diazepam did not substitute for the Δ9-THC discriminative stimulus.
- Diazepam did not alter the Δ9-THC discrimination dose-response function.
- GABAA has minimal involvement in the interoceptive effects of Δ9-THC in humans.
Acknowledgements
We appreciate the pharmacy services of Dr. Steve Sitzlar of the University of Kentucky Investigational Drug Service. We also thank Shanna Babalonis, Beth Eaves, Cleeve Emurian, Lauren Hayden, Sarah Ingebrand, Jaclyn Miller, Glenn Robbins and Sheila Rutherford for expert technical assistance.
Role of Funding Source This research and the preparation of this manuscript were supported by grants awarded to Dr. Joshua Lile (National Institute on Drug Abuse grants K02 DA031766 and R01 DA025605) as well as the University of Kentucky Center for Clinical and Translational Science (National Center for Advancing Translational Sciences grant UL1TR000117). These funding sources had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest There are no conflicts of interest to declare.
Contributors Drs. Lile, Kelly and Hays designed the study. Dr. Lile wrote the protocol; managed literature searches and summaries of previous related work; undertook the statistical analysis and graphical representation of the data; and wrote the first draft of the manuscript. Dr. Hays provided medical management and oversight. All authors contributed to and have approved the final manuscript.
REFERENCES
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. Fourth edition, Text revision American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Barrett RL, Wiley JL, Balster RL, Martin BR. Pharmacological specificity of delta 9-tetrahydrocannabinol discrimination in rats. Psychopharmacology. 1995;118:419–424. doi: 10.1007/BF02245942. [DOI] [PubMed] [Google Scholar]
- Browne RG, Weissman A. Discriminative stimulus properties of delta 9-tetrahydrocannabinol: mechanistic studies. J. Clin. Pharmacol. 1981;21:S227–34. doi: 10.1002/j.1552-4604.1981.tb02599.x. [DOI] [PubMed] [Google Scholar]
- Chutuape MA, de Wit H. Relationship between subjective effects and drug preferences: ethanol and diazepam. Drug Alcohol Depend. 1994;34:243–251. doi: 10.1016/0376-8716(94)90163-5. [DOI] [PubMed] [Google Scholar]
- de Wit H, Uhlenhuth EH, Johanson CE. Individual differences in the reinforcing and subjective effects of amphetamine and diazepam. Drug Alcohol Depend. 1986;16:341–360. doi: 10.1016/0376-8716(86)90068-2. [DOI] [PubMed] [Google Scholar]
- Evans SM, Griffiths RR, de Wit H. Preference for diazepam, but not buspirone, in moderate drinkers. Psychopharmacology (Berl) 1996;123:154–163. doi: 10.1007/BF02246172. [DOI] [PubMed] [Google Scholar]
- Glass RM, Uhlenhuth EH, Hartel FW, Schuster CR, Fischman MW. Single-dose study of nabilone in anxious volunteers. JClin Pharmacol. 1981;21:S383–96. doi: 10.1002/j.1552-4604.1981.tb02618.x. [DOI] [PubMed] [Google Scholar]
- Greenblatt DJ. Pharmacology of benzodiazepine hypnotics. J Clin Psychiatry. 1992;53:7–13. [PubMed] [Google Scholar]
- Griffiths RR, Johnson MW. Relative abuse liability of hypnotic drugs: a conceptual framework and algorithm for differentiating among compounds. J Clin Psychiatry. 2005;66:31–41. [PubMed] [Google Scholar]
- Griffiths RR, Troisi JR, II, Silverman K, Mumford GK. Multiple-choice procedure: An efficient approach for investigating drug reinforcement in humans. Behav. Pharmacol. 1993;4:3–13. [PubMed] [Google Scholar]
- Hart CL, Haney M, Vosburg SK, Comer SD, Foltin RW. Reinforcing effects of oral Delta9-THC in male marijuana smokers in a laboratory choice procedure. Psychopharmacology (Berl) 2005;181:237–243. doi: 10.1007/s00213-005-2234-2. [DOI] [PubMed] [Google Scholar]
- Heishman SJ, Stitzer ML, Yingling JE. Effects of tetrahydrocannabinol content on marijuana smoking behavior, subjective reports and performance. Pharmacol. Biochem. Behav. 1989;34:173–179. doi: 10.1016/0091-3057(89)90369-9. [DOI] [PubMed] [Google Scholar]
- Hillestad L, Hansen T, Melsom H, Drivenes A. Diazepam metabolism in normal man. I. Serum concentrations and clinical effects after intravenous, intramuscular and oral administration. Clin Pharmacol Ther. 1974;16:479–84. [PubMed] [Google Scholar]
- Hollister LE, Gillespie HK, Ohlsson A, Lindgren JE, Wahlen A, Agurell S. Do plasma concentrations of delta 9-tetrahydrocannabinol reflect the degree of intoxication? J. Clin. Pharmacol. 1981;21:171S–177S. doi: 10.1002/j.1552-4604.1981.tb02593.x. [DOI] [PubMed] [Google Scholar]
- Järbe TU, Hiltunen AJ. Limited stimulus generalization between delta 9-THC and diazepam in pigeons and gerbils. Psychopharmacology. 1988:328–331. doi: 10.1007/BF00174684. [DOI] [PubMed] [Google Scholar]
- Kamien JB, Bickel WK, Higgins ST, Hughes JR. The effects of delta 9-tetrahydrocannabinol on repeated acquisition and performance of response sequences and on self-reports in humans. Behav. Pharmacol. 1994;5:71–78. doi: 10.1097/00008877-199402000-00008. [DOI] [PubMed] [Google Scholar]
- Kelly TH, Delzer TA, Martin CA, Harrington NG, Hays LR, Bardo MT. Performance and subjective effects of diazepam and d-amphetamine in high and low sensation seekers. Behav Pharmacol. 2009;20:505–517. doi: 10.1097/FBP.0b013e3283305e8d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly TH, Foltin RW, Emurian CS, Fischman MW. Performance-based testing for drugs of abuse: dose and time profiles of marijuana, amphetamine, alcohol and diazepam. J. Anal. Toxicol. 1993;17:264–272. doi: 10.1093/jat/17.5.264. [DOI] [PubMed] [Google Scholar]
- Kelly TH, Foltin RW, Fischman MW. Multidimensional behavioral effects of marijuana. Prog. Neuropsychopharmacol. Biol. Psychiatry. 1990;14:885–902. doi: 10.1016/0278-5846(90)90075-r. [DOI] [PubMed] [Google Scholar]
- Lile JA, Kelly TH, Charnigo RJ, Stinchcomb AL, Hays LR. Pharmacokinetic and pharmacodynamic profile of supratherapeutic oral doses of Δ(9) -THC in cannabis users. J Clin Pharmacol. 2013;53:680–90. doi: 10.1002/jcph.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lile JA, Kelly TH, Hays LR. Substitution profile of the cannabinoid agonist nabilone in humans discriminating Δ9-THC. Clin. Neuropharmacol. 2010;33:235–242. doi: 10.1097/WNF.0b013e3181e77428. [DOI] [PubMed] [Google Scholar]
- Lile JA, Kelly TH, Hays LR. Separate and combined effects of the cannabinoid agonists nabilone and Δ9-THC in humans discriminating Δ(9)-THC. Drug Alcohol Depend. 2011;116:86–92. doi: 10.1016/j.drugalcdep.2010.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lile JA, Kelly TH, Hays LR. Separate and combined effects of the GABA reuptake inhibitor tiagabine and Δ9-THC in humans discriminating Δ(9)-THC. Drug Alcohol Depend. 2012a;122:61–69. doi: 10.1016/j.drugalcdep.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lile JA, Kelly TH, Hays LR. Separate and combined effects of the GABAB agonist baclofen and Δ9-THC in humans discriminating Δ(9)-THC. Drug Alcohol Depend. 2012b;126:216–223. doi: 10.1016/j.drugalcdep.2012.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lile JA, Kelly TH, Pinsky DJ, Hays LR. Substitution profile of Δ9-tetrahydrocannabinol, triazolam, hydromorphone and methylphenidate in humans discriminating Δ9-tetrahydrocannabinol. Psychopharmacology. 2009;203:241–250. doi: 10.1007/s00213-008-1393-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marinol® Product Information. Solvay Pharmaceuticals Inc.; 2006. [Google Scholar]
- McLeod DR, Griffiths RR, Bigelow GE, Yingling JE. An automated version of the Digit Symbol Substitution Test (DSST) Behav. Res. Methods Instrument. 1982;14:463–466. [Google Scholar]
- Mokler DJ, Nelson BD, Harris LS, Rosecrans JA. The role of benzodiazepine receptors in the discriminative stimulus properties of delta 9-tetrahydrocannabinol. Life Sci. 1986;38:1581–1589. doi: 10.1016/0024-3205(86)90497-2. [DOI] [PubMed] [Google Scholar]
- Owen RT, Tyrer P. Benzodiazepine dependence. A review of the evidence. Drugs. 1983;25:385–398. doi: 10.2165/00003495-198325040-00003. [DOI] [PubMed] [Google Scholar]
- Ranganathan M, D’Souza DC. The acute effects of cannabinoids on memory in humans: a review. Psychopharmacology (Berl) 2006;188:425–44. doi: 10.1007/s00213-006-0508-y. [DOI] [PubMed] [Google Scholar]
- Rush CR, Kollins SH, Pazzaglia PJ. Discriminative-stimulus and participant-rated effects of methylphenidate, bupropion and triazolam in d-amphetamine trained humans. Exp. Clin. Psychopharmacol. 1998;6:32–44. doi: 10.1037//1064-1297.6.1.32. [DOI] [PubMed] [Google Scholar]
- Schlicker E, Kathmann M. Modulation of transmitter release via presynaptic cannabinoid receptors. Trends Pharmacol Sci. 2001;22:565–572. doi: 10.1016/s0165-6147(00)01805-8. [DOI] [PubMed] [Google Scholar]
- Toland SL, Green W. DRE field testing of drug impaired drivers. In: Watts V, editor. The Effects of Drugs on Human Performance and Behavior: Drugs and Driving/Drugs in the Workplace. American Academy of Forensic Sciences; 1991. [Google Scholar]
- Valium® Product Information. Genentech, Inc.; 2013. [Google Scholar]
- Vandrey R, Smith MT, McCann UD, Budney AJ, Curran EM. Sleep disturbance and the effects of extended-release zolpidem during cannabis withdrawal. Drug Alcohol Depend. 2011;117:38–44. doi: 10.1016/j.drugalcdep.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiley JL, Martin BR. Effects of SR141716A on diazepam substitution for delta 9-tetrahydrocannabinol in rat drug discrimination. Pharmacol Biochem Behav. 1999;64:519–522. doi: 10.1016/s0091-3057(99)00130-6. [DOI] [PubMed] [Google Scholar]
- Wiley JL, Martin BR. Cannabinoid pharmacological properties common to other centrally acting drugs. Eur J Pharmacol. 2003;471:185–93. doi: 10.1016/s0014-2999(03)01856-9. [DOI] [PubMed] [Google Scholar]
- Wilson WH, Ellinwood EH, Mathew RJ, Johnson K. Effects of marijuana on performance of a computerized cognitive-neuromotor test battery. Psychiatry Res. 1994;51:115–125. doi: 10.1016/0165-1781(94)90031-0. [DOI] [PubMed] [Google Scholar]
- Witkin JM, Tzavara ET, Nomikos GG. A role for cannabinoid CB1 receptors in mood and anxiety disorders. Behav Pharmacol. 2005;16:315–31. doi: 10.1097/00008877-200509000-00005. [DOI] [PubMed] [Google Scholar]