Abstract
Background
The Electronic Health Record (EHR) is a key component of medical informatics that is increasingly being utilized in industrialized nations to improve healthcare. There is limited information on the use of EHR in sub-Saharan Africa. This paper reviews availability of EHRs in sub-Saharan Africa.
Methods
Searches were performed on PubMed and Google Scholar databases using the terms ‘Electronic Health Records OR Electronic Medical Records OR e-Health and Africa’. References from identified publications were reviewed. Inclusion criterion was documented use of EHR in Africa.
Results
The search yielded 147 publications of which 21papers from 15 sub-Saharan African countries documented the use of EHR in Africa and were reviewed. About 91% reported use of Open Source healthcare software, with OpenMRS being the most widely used. Most reports were from HIV related health centers. Barriers to adoption of EHRs include high cost of procurement and maintenance, poor network infrastructure and lack of comfort among health workers with electronic medical records.
Conclusion
There has been an increase in the use of EHRs in sub-Saharan Africa, largely driven by utilization by HIV treatment programs. Penetration is still however very low.
Keywords: Electronic health records, Electronic Medical Records, sub-Saharan Africa
Introduction
Medical informatics is an intersection of information science, computer science and health care. It includes clinical guidelines, formal medical language, standards, and communication systems1,2. The various tools, technologies, and tactics are designed to support the progressive realization of the optimal delivery of health and medical care3,4. This field which began in the 1950’s has grown rapidly in developed countries5,6. The Electronic Health record (EHR) is a key component of medical informatics2. It provides the opportunity for health care organizations to improve the quality of patient care and safety, and also has the potential to reduce cost and improve efficiency of the workplace7. The use of electronic records has distinct advantages over paper records; these include: enabled access to medical records from remote locations, improved speed and ease of retrieval of records, avenues to flag abnormal results and the elimination of hand written prescriptions, which reduces the occurrence of prescription errors8-10. Other benefits are the simultaneous access to patient records by multiple users and the ability to perform data queries to inform decision making. These potential benefits of the EHR have enabled its wide acceptability in industrialized nations 11.
Developing countries, including sub-Saharan Africa, bear the brunt of the world’s deadliest epidemics, which include HIV/AIDS, malaria and tuberculosis12. There is a tremendous potential for the deployment of information and communication technology (ICT) to improve health care in these regions13. Access to the internet has dramatically improved in the last 10 years, and all countries in Africa now have direct access to the internet14. There is limited information on how healthcare in sub-Saharan Africa is being influenced by the current influx of ICT into the region. In order to bridge this gap, we sought to document the availability of EHR, in sub-Saharan Africa, and highlight the challenges hindering its wider adoption in the region.
Methods
Identification of publications
Searches were performed on PubMed and Google Scholar using the terms:
Electronic Medical Records AND Africa
Electronic Health Records AND Africa
E-Health AND Africa
Medical Informatics AND Africa
For countries in sub-Saharan Africa yielding no results from the search, country names were specifically included in the search terms, for example: Electronic Health Records AND Chad. References from identified publications were also reviewed.
Inclusion and exclusion criteria
Publications of interest were those on the use of EHRs in health care in Africa. Commentaries, opinions and reviews were excluded. Duplicate publications were also excluded.
Results
The search yielded 147 publications with EHR(s) related terms and the name of an African country. A total of 126 publications (86%) were excluded; of these 64 had no information on use of EHRs in an African country and 62 were duplications.
The remaining 21 articles were reviewed. These articles were from 15 African countries (Table1). Most of the publications were from Eastern and Southern Africa with Kenya having the highest number of publications (4, 19%)15-18. Two publications documented experiences in more than one country, the first in three East African countries19 and the second from ten countries20. The publication documenting experiences from 10 African countries was the ‘Drug Resources Enhancement against AIDS and Malnutrition’ (DREAM) project. This was a project of Sant’Egidio; a Christian based organization in Rome involved the fight against AIDS in sub-Saharan African. The 10 countries covered by the DREAM project are: Guinea Bissau, Republic of Guinea, Nigeria, Cameroon, Democratic Republic of Congo, Angola, Kenya, Tanzania, Malawi and Mozambique.
Table 1.
Summary of publications on the use of electronic medical records in sub-Saharan Africa
| Publications | Country | Software | Setting |
|---|---|---|---|
| Identification of losses to follow-up in a community based antiretroviral therapy clinic in South Africa using a computerized pharmacy tracking system30 | South Africa | Open Source (iDART) | HIV care |
| Leapfrogging paper-based records using handheld technology: experience from Western Kenya15 | Kenya | Open Source | Home based care |
| Innovative approaches to application of information technology in disease surveillance and prevention in Western Kenya16 | Kenya | Open Source | Injury surveillance |
| The Mosoriot medical record system: design and implementation of an outpatient electronic record system in rural Kenya17 | Kenya | Open Source | Tertiary care |
| “Talkin’ about a revolution”: How electronic health records can facilitate the scale-up of HIV care and treatment and catalyze primary care in resource-constrained settings18 | Kenya | Open Source (Open MRS) | HIV care |
| Experience with implementing electronic health records in three East African countries19 | Kenya, Tanzania & Uganda. | Open Source (Open MRS) | HIV care |
| Combining vital events registration, verbal autopsy and electronic medical records in rural Ghana for improved health service delivery10 | Ghana | Open Source (MGV-net) | Vital registration |
| Implementing OpenMRS for patient monitoring in an HIV/AIDS care and treatment program in rural Mozambique34 | Mozambique | Open Source (Open MRS) | HIV care |
| Using electronic medical records in HIV care in rural Rwanda35 | Rwanda | Open Source | HIV Care |
| Rapid deployment of electronic medical records in rural Rwanda32 | Rwanda | Open Source (Open MRS) | HIV care |
| Experience implementing OpenMRS to support maternal and reproductive health in Northern Nigeria23 | Nigeria | Open Source (Open MRS) | Maternal & reproductive health |
| The computer in a Nigerian teaching Hospital: First year experience45 | Nigeria | Open Source | Tertiary care center |
| Experience implementing a point-of-care electronic medical record system for primary care in Malawi22 | Malawi | Open Source (Open MRS) | Primary care center |
| A global approach to the management of EMR (electronic medical records) of patients with HIV/AIDS in sub-Saharan Africa: the experience of Dream Software20 | Guinea Bissau, Republic of Guinea, Nigeria, Cameroon, Republic of Congo, Kenya, Angola Mozambique, Malawi, Tanzania | Open Source (DREAM Software) | HIV care |
| Expanding an electronic medical record to support community health worker and nutritional support programs in rural Rwanda36 | Rwanda | Open Source | HIV care |
| Hybrid data capture for monitoring patients on highly active antiretroviral therapy (HAART) in urban Botswana31 | Botswana | Open Source | HIV care |
| Designing and implementing an electronic health record system in primary care in sub-Saharan Africa: a case study from Cameroon24 | Cameroon | MEDCAD | Primary care |
| An electronic medical record system for ambulatory care of HIV-infected patients in Kenya33 | Kenya | Open Source (Open MRS) | HIV care |
| Enumeration of non-communicable disease in rural South Africa by electronic data linkage and capture–recapture techniques25 | South Africa | Open Source | Primary care |
| Open Source challenges for Hospital Information System (HIS) in a developing country: a pilot project in Mali26 | Mali | Open Source | Tertiary care |
| Assessment of data quality of and staff satisfaction with an electronic health record system in a developing country (Uganda): a qualitative and quantitative comparative study44 | Uganda | Open Source (Open MRS) | Primary care |
The use of open source healthcare software was documented in 95.2% (20/21) of publications, with 47.6% (10/21) of publications being from HIV-related treatment programs. Open Medical Records System (OpenMRS) was the most popularly used open source health software and was used in 60% (6/10) of centers involved in HIV care and 27% (3/11) of non-HIV related programs.
The review also showed an increase in the number of publications between 1992, when the first article was published, and 2010 (Figure 1).
Figure 1.
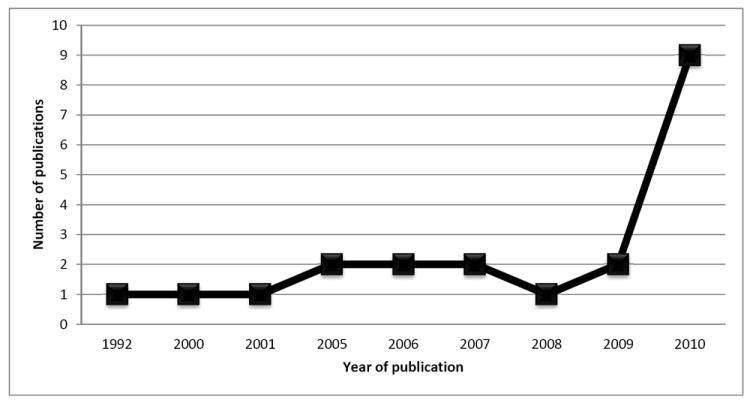
Chart showing publications on the use of electronic medical records in sub-Saharan Africa
The major documented challenge to the establishment of EHR was the high cost of set-up and maintenance. This was due to poor existing infrastructure, frequent power outages and network failure. In facilities with EHRs, use was sub-optimal because of the need for parallel entry of data to paper and computer which increased the work-load of over-stretched staff. Despite these challenges, some authors have documented benefits of the use of EHR in sub-Saharan Africa; these include greater data accuracy, improved timeliness, availability of routine reports and reduced data duplication21-25.
Discussion
The implementation of Clinical Information Systems has been identified as an important component of improving health care, and the degree of adoption of technologies in health care has been shown to correlate with reduction of complications and mortalities in hospitals26-28. Although African nations are still lagging behind developed countries in the availability and use of EHRs29, this review shows that there has been an appreciable increase in the availability and utilization of EHRs in Africa over the last decade. This increase has been driven by collaboration between African institutions and international collaborators mostly in the area of HIV/AIDS treatment and care18,20,30-36.
The influx of EHRs in sub-Saharan Africa has been facilitated by several factors, key factors being the increased availability of personal computers12 and increased access to internet. Internet access in Africa has grown by 2,357.3% from 2000 to 2010. This however represents only 10% of the population, far behind the 30% world average coverage37. Although the internet is present in all 54 African countries, access is often concentrated in urban centers, with no access in most rural centers where over 80% of the population reside. This inequitable distribution has affected the realization of the full benefits of EHRs in sub-Saharan Africa.
To set up an EHR system is capital intensive38,39 and thus beyond the reach of most health providers in sub-Saharan Africa. Few African countries have the manpower and skills to develop the required infrastructure and the cost of commercial software packages is exorbitant. The emergence of Open Source Software has however enhanced the opportunity of several African countries to gain access to EHRs, and this was observed in the review15-20,22,30-35. The acquisition of Open Sources is less expensive and provides opportunities for adaptation for local use40.
Few studies have audited the use of EHRs in sub-Saharan Africa41,42. Expectedly, results have been as conflicting as those from developing countries. Several publications have documented benefits of the use of EHRs in Africa including greater data accuracy, improved timeliness and availability of routine reports21,22,24. A review by Foster et al 43 however showed that more effort is still required to optimize the benefits of EHRs in developing countries.
Despite the successful introduction of EHRs in sub-Saharan Africa so far, it has not been without challenges. Most EHRs are sustained by funding from international partnerships raising questions about the sustainability of these systems by the host institutions. Poor infrastructure also increases the cost to set up and maintain the systems. Specifically there have been reports of power outages and network breakdowns; the need for parallel data entry also contributed to overload of work for the limited health staff44,45.
A potential limitation of this review is the restriction of the search to published literature. This may exclude experiences from centers not documented in scholarly publications. Also striking is the dearth of publications from Francophone countries. Although the search through English literature may contribute to this, the paucity of use of EHRs in Francophone sub-Saharan Africa has been previously documented26.
Conclusion
The availability of EHR in sub-Saharan Africa has increased over the last decade, mostly driven by international efforts at stemming the HIV/AIDS epidemic. Based on the current literature, most countries in sub-Saharan Africa, particularly Francophone countries, are however being left behind in the progress towards EHR adoption. Government institutions in sub-Saharan Africa also appear to be slow in implementing EHR and other appropriate ICTs which are required to improve healthcare on the continent.
Acknowledgments
MOA was supported by NIH through a Fogarty International Center grant D43TW007995. The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the Fogarty International Center or the National Institutes of Health. The authors gratefully acknowledge the assistance of Pamela Shaw in retrieving relevant materials for this review.
References
- 1.Coiera E. Medical informatics. BMJ. 1995;310:1381–6. doi: 10.1136/bmj.310.6991.1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hayrinen K, Saranto K, Nykanen P. Definition, structure, content, use and impacts of electronic health records: A review of the research literature. Int J Med Inf. 2008;77:291–304. doi: 10.1016/j.ijmedinf.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Goldstein DE. Medical informatics 20/20 : quality and electronic health records through collaboration, open solutions, and innovation. Sudbury, Mass.: Jones and Bartlett Publishers; 2007. [Google Scholar]
- 4.Millman A, Lee N, Kealy K. ABC of the Medical Computing Internet. BMJ. 1995;311:440. doi: 10.1136/bmj.311.7002.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haux R. Health information systems -- past, present, future. Int J Med Inf. 2006;75:268–81. doi: 10.1016/j.ijmedinf.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 6.Haux R. Individualization, globalization and health - about sustainable information technologies and the aim of medical informatics. Int J Med Inf. 2006;75:795–808. doi: 10.1016/j.ijmedinf.2006.05.045. [DOI] [PubMed] [Google Scholar]
- 7.Jha AK, DesRoches CM, Campbell EG, et al. Use of Electronic Health Records in U.S. Hospitals. New England Journal of Medicine. 2009;360:1628–38. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 8.Gaylin DS, Moiduddin A, Mohamoud S, Lundeen K, Kelly JA. Public Attitudes about Health Information Technology, and Its Relationship to Health Care Quality, Costs, and Privacy. Health Services Research. 2011:920–38. doi: 10.1111/j.1475-6773.2010.01233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenhalgh T, Hinder S, Stramer K, Bratan T, Russell J. Adoption, non-adoption, and abandonment of a personal electronic health record: case study of HealthSpace. BMJ. 341 doi: 10.1136/bmj.c5814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ohemeng-Dapaah S, Pronyk P, Akosa E, Nemser B, Kanter A. Combining vital events registration, verbal autopsy and electronic medical records in rural Ghana for improved health services delivery. stud Health Technol Inform. 2010;160:416–20. [PubMed] [Google Scholar]
- 11.Black AD, Car J, Pagliari C, et al. The Impact of eHealth on the Quality and Safety of Health Care: A Systematic Overview. PLoS Med. 2011;8:e1000387. doi: 10.1371/journal.pmed.1000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ajuwon G. Computer and internet use by first year clinical and nursing students in a Nigerian teaching hospital. BMC Medical Informatics and Decision Making. 2003;3:10. doi: 10.1186/1472-6947-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marques ET, Jr, Maciel Filho R, August PN. Overcoming health inequity: potential benefits of a patient-centered open-source public health infostructure. Cad Saude Publica. 2008;24:547–57. doi: 10.1590/s0102-311x2008000300008. [DOI] [PubMed] [Google Scholar]
- 14.Bukachi F, Pakenham-Walsh N. Information Technology for Health in Developing Countries*. Chest. 2007;132:1624–30. doi: 10.1378/chest.07-1760. [DOI] [PubMed] [Google Scholar]
- 15.Were MC, Kariuki J, Chepng’eno V, et al. Leapfrogging paper-based records using handheld technology: experience from Western Kenya. Stud Health Technol Inform. 2010;160:525–9. [PubMed] [Google Scholar]
- 16.Odero W, Rotich J, Yiannoutsos CT, Ouna T, Tierney WM. Innovative approaches to application of information technology in disease surveillance and prevention in Western Kenya. J Biomed Inform. 2007;40:390–7. doi: 10.1016/j.jbi.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 17.Hannan TJ, Rotich JK, Odero WW, et al. The Mosoriot medical record system: design and initial implementation of an outpatient electronic record system in rural Kenya. Int J Med Inform. 2000;60:21–8. doi: 10.1016/s1386-5056(00)00068-x. [DOI] [PubMed] [Google Scholar]
- 18.Braitstein P, Einterz RM, Sidle JE, Kimaiyo S, Tierney W. “Talkin’ about a revolution”: How electronic health records can facilitate the scale-up of HIV care and treatment and catalyze primary care in resource-constrained settings. J Acquir Immune Defic Syndr. 2009;52(Suppl 1):S54–7. doi: 10.1097/QAI.0b013e3181bbcb67. [DOI] [PubMed] [Google Scholar]
- 19.Tierney WM, Achieng M, Baker E, et al. Experience implementing electronic health records in three East African countries. Stud Health Technol Inform. 2010;160:371–5. [PubMed] [Google Scholar]
- 20.Nucita A, Bernava GM, Bartolo M, et al. A global approach to the management of EMR (electronic medical records) of patients with HIV/AIDS in sub-Saharan Africa: the experience of DREAM software. BMC Med Inform Decis Mak. 2009;9:42. doi: 10.1186/1472-6947-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tierney WM, Rotich JK, Hannan TJ, et al. The AMPATH medical record system: creating, implementing, and sustaining an electronic medical record system to support HIV/AIDS care in western Kenya. Stud Health Technol Inform. 2007;129:372–6. [PubMed] [Google Scholar]
- 22.Waters E, Rafter J, Douglas GP, Bwanali M, Jazayeri D, Fraser HS. Experience implementing a point-of-care electronic medical record system for primary care in Malawi. Stud Health Technol Inform. 2010;160:96–100. [PubMed] [Google Scholar]
- 23.Thompson A, Castle E, Lubeck P, Makarfi P. Experience implementing OpenMRS to support maternal and reproductive health in Nothern Nigeria. stud Health Technol Inform. 2010;160:332–6. [PubMed] [Google Scholar]
- 24.Kamadjeu R, Tapang E, Moluh R. Designing and implementing an electronic health record system in primary care practice in sub-Saharan Africa: a case study from Cameroon. Inform Prim Care. 2005;13:179–86. doi: 10.14236/jhi.v13i3.595. [DOI] [PubMed] [Google Scholar]
- 25.Gill G, Scott B, Beeching N, Wilkinsom D, Ismail A. Enumeration of non-communicable disease in rural South Africa by electronic data linkage and capture- recapture techniques. Trop Med Int Health. 2001;6:435–41. doi: 10.1046/j.1365-3156.2001.00722.x. [DOI] [PubMed] [Google Scholar]
- 26.Bagayoko C-O, Dufour J-C, Chaacho S, Bouhaddou O, Fieschi M. Open source challenges for hospital information system (HIS) in developing countries: a pilot project in Mali. BMC Medical Informatics and Decision Making. 2010;10:22. doi: 10.1186/1472-6947-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amarasingham R, Plantinga L, Diener-West M, Gaskin D, Powe N. Clinical information technologies and inpatient outcomes. A multiple hospital study. Arch Int Med. 2009;169:108–14. doi: 10.1001/archinternmed.2008.520. [DOI] [PubMed] [Google Scholar]
- 28.Scott R. e-Records in health--Preserving our future. Int J of Med Inf. 2007;76:427–31. doi: 10.1016/j.ijmedinf.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 29.Kumar S, Aldrich K. Overcoming barriers to electronic medical record (EMR) implementation in the US healthcare system: A comparative study. Health Informatics Journal. 2010;16:306–18. doi: 10.1177/1460458210380523. [DOI] [PubMed] [Google Scholar]
- 30.Nglazi MD, Kaplan R, Wood R, Bekker LG, Lawn SD. Identification of losses to follow-up in a community-based antiretroviral therapy clinic in South Africa using a computerized pharmacy tracking system. BMC Infect Dis. 2010;10:329. doi: 10.1186/1471-2334-10-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bussmann H, Wester CW, Ndwapi N, et al. Hybrid data capture for monitoring patients on highly active antiretroviral therapy (HAART) in urban Botswana. Bulletin of the World Health Organization. 2006;84:127–31. doi: 10.2471/blt.04.019307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Allen C, Manyika P, Jazayeri D, Rich M, Lesh N, Fraser H. Rapid deployment of electronic medical records for ARV rollout in rural Rwanda. AMIA Annu Symp Proc. 2006:840. [PMC free article] [PubMed] [Google Scholar]
- 33.Siika AM, Rotich JK, Simiyu CJ, et al. An electronic medical record system for ambulatory care of HIV-infected patients in Kenya. International Journal of Medical Informatics. 2005;74:345–55. doi: 10.1016/j.ijmedinf.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 34.Manders EJ, Jose E, Solis M, Burlison J, Nhampossa JL, Moon T. Implementing OpenMRS for patient monitoring in an HIV/AIDS care and treatment program in rural Mozambique. Stud Health Technol Inform. 2010;160:411–5. [PubMed] [Google Scholar]
- 35.Amoroso CL, Akimana B, Wise B, Fraser HS. Using electronic medical records for HIV care in rural Rwanda. Stud Health Technol Inform. 2010;160:337–41. [PubMed] [Google Scholar]
- 36.Allen C, Manyika P, Ufitamahoro E, et al. Expanding an electronic medical record to support community health worker and nutritional support programs in rural Rwanda. AMIA Annu Symp Proc. 2007:860. [PubMed] [Google Scholar]
- 37.Internet World Stats. Internet usage and population statistics for Africa. [Febuary 19, 2011]; at http://www.internetworldstats.com/stats1.htm.
- 38.Cusack CM. Electronic Health Records and Electronic Prescribing: Promise and Pitfalls. Obstetrics and Gynecology Clinics of North America. 2008;35:63–79. doi: 10.1016/j.ogc.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 39.Zlabek JA, Wickus JW, Mathiason MA. Early cost and safety benefits of an inpatient electronic health record. Journal of the American Medical Informatics Association. doi: 10.1136/jamia.2010.007229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Seebregts CJ, Mamlin BW, Biondich PG, et al. The OpenMRS Implementers Network. International Journal of Medical Informatics. 2009;78:711–20. doi: 10.1016/j.ijmedinf.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 41.Yogeswaran P, Wright G. EHR implementation in South Africa: how do we get it right? Stud Health Technol Inform. 2010;160:396–400. [PubMed] [Google Scholar]
- 42.Tomasi E, Facchini LA, Maia MdFS. Health information technology in primary health care in developing countries: a literature review. Bulletin of the World Health Organization. 2004;82:867–74. [PMC free article] [PubMed] [Google Scholar]
- 43.Forster M, Bailey C, Brinkhof MW, et al. Electronic medical record systems, data quality and loss to follow-up: survey of antiretroviral therapy programmes in resource-limited settings. Bull World Health Organ. 2008;86:939–47. doi: 10.2471/BLT.07.049908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ndira SP, Rosenberger KD, Wetter T. Assessment of data quality of and staff satisfaction with an electronic health record system in a developing country (Uganda): a qualitative and quantitative comparative study. Methods Inf Med. 2008;47:489–98. [PubMed] [Google Scholar]
- 45.Daini O, Korpela M, Ojo J, Soriyan H. MEDIFO. Amsterdam: 1992. The computer in a Nigerian teaching hospital: First year experience; pp. 230–5. [Google Scholar]


