Abstract
Background
Antisocial personality disorder (AsPD) is associated with a wide range of disturbance including persistent rule-breaking, criminality, substance use, unemployment, homelessness and relationship difficulties.
Objectives
To evaluate the potential beneficial and adverse effects of psychological interventions for people with AsPD.
Search methods
Our search included CENTRAL Register of Controlled Trials, MEDLINE, EMBASE, CINAHL, PsycINFO, ASSIA, BIOSIS and COPAC.
Selection criteria
Prospective, controlled trials in which participants with AsPD were randomly allocated to a psychological intervention and a control condition (either treatment as usual, waiting list or no treatment).
Data collection and analysis
Three authors independently selected studies. Two authors independently extracted data. We calculated mean differences, with odds ratios for dichotomous data.
Main results
Eleven studies involving 471 participants with AsPD met the inclusion criteria, although data were available from only five studies involving 276 participants with AsPD. Only two studies focused solely on an AsPD sample. Eleven different psychological interventions were examined. Only two studies reported on reconviction, and only one on aggression. Compared to the control condition, cognitive behaviour therapy (CBT) plus standard maintenance was superior for outpatients with cocaine dependence in one study, but CBT plus treatment as usual was not superior for male outpatients with recent verbal/physical violence in another. Contingency management plus standard maintenance was superior for drug misuse for outpatients with cocaine dependence in one study but not in another, possibly because of differences in the behavioural intervention. However, contingency management was superior in social functioning and counselling session attendance in the latter. A multi-component intervention utilising motivational interviewing principles, the ‘Driving Whilst Intoxicated program’, plus incarceration was superior to incarceration alone for imprisoned drink-driving offenders.
Authors’ conclusions
Results suggest that there is insufficient trial evidence to justify using any psychological intervention for adults with AsPD. Disappointingly few of the included studies addressed the primary outcomes defined in this review (aggression, reconviction, global functioning, social functioning, adverse effects). Three interventions (contingency management with standard maintenance; CBT with standard maintenance; ‘Driving Whilst Intoxicated program’ with incarceration) appeared effective, compared to the control condition, in terms of improvement in at least one outcome in at least one study. Each of these interventions had been originally developed for people with substance misuse problems. Significant improvements were mainly confined to outcomes related to substance misuse. No study reported significant change in any specific antisocial behaviour. Further research is urgently needed for this prevalent and costly condition.
Medical Subject Headings (MeSH): Aggression [psychology], Antisocial Personality Disorder [*therapy], Cocaine-Related Disorders [therapy], Cognitive Therapy [methods], Psychotherapy [*methods], Randomized Controlled Trials as Topic, Reward
MeSH check words: Adult, Female, Humans, Male
BACKGROUND
Description of the condition
Antisocial personality disorder (AsPD) is one of the ten personality disorder categories in the current edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; APA 2000). DSM-IV defines personality disorder as: ‘an enduring pattern of inner experience and behaviour that deviates markedly from the expectations of the person’s culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is stable over time, and leads to distress or impairment’. General criteria for personality disorder according to DSM-IV are given in Table 1 below.
Table 1. DSM-IV general criteria for personality disorder.
|
AsPD is identified by traits that include irresponsible and exploitive behaviour, recklessness, impulsivity, high negative emotionality and deceitfulness. In order to be diagnosed with AsPD, according to the DSM-IV, a personmust fulfil criteria A, B, C and D shown in Table 2 below as well as fulfilling general criteria for a personality disorder as outlined above.
Table 2. DSM-IV diagnostic criteria for AsPD (APA 2000).
|
The focus of this review is antisocial personality disorder, although this condition is also often classified using the International Classification of Diseases - tenth edition (ICD-10; WHO 1992) as dissocial personality disorder (F60.2). AsPD and dissocial personality disorder are often used interchangeably by clinicians and they describe a very similar presentation. While there is considerable overlap between these two diagnostic systems, they differ in two respects. First, DSM-IV requires that those meeting the diagnostic criteria also show evidence of conduct disorder with onset before the age of 15 years and there is no such requirement when making the diagnosis of dissocial personality disorder using ICD-10 criteria. However, a study by Perdikouri et al (Perdikouri 2007) did not find any clinically important differences when they compared subjects meeting the full criteria for AsPD with those who otherwise fulfilled criteria for AsPD but who did not demonstrate evidence of childhood conduct disorder. Second, dissocial personality disorder focuses more on the interpersonal deficits (for example, incapacity to experience guilt, a very low tolerance of frustration, proneness to blame others) and less on antisocial behaviour. Table 3 below shows the diagnostic criteria for diagnosing dissocial personality disorder. Second, it has been argued that the criteria in ICD-10 are more reflective of the core personality traits of the antisocial with less emphasis on criminal behaviour.
Table 3. ICD-10 diagnostic criteria for dissocial personality disorder (F60.2) (WHO 1992).
|
Whilst estimates of the prevalence of AsPD in the general population vary across studies and countries, most studies report a prevalence of between 2% and 3% in the general population (Coid 2006; Moran 1999). Prevalence rates are consistently higher in men compared with women (Dolan 2009). For instance, the lifetime prevalence in two North American studies was 4.5% among men and 0.8% among women (Robins 1991) and 6.8% among men and 0.8% in women (Swanson 1994). However, two European studies found lower prevalence rates (i.e. of 1.3% in men and 0% in women (Torgensen 2001) and 1% in men and 0.2% in women (Coid 2006)). As would be expected AsPD is especially common in prison settings. In the UK prison population, the prevalence of people with AsPD has been identified as 63% in male remand prisoners, 49% in male sentenced prisoners and 31% in female prisoners (Singleton 1998).
The condition is associated with a wide range of disturbance and is associated with greatly increased rates of criminality, substance use, unemployment, homelessness and relationship difficulties. Antisocial personality disorder is generally associated with a negative long-term outcome. Many adults with AsPD are imprisoned at some point in their life. Although follow-up studies have demonstrated some improvement over time, particularly in rates of re-offending (Grilo 1998; Weissman 1993), men with AsPD who reduce their offending behaviour over time may nonetheless continue to have major problems in their interpersonal relationships (Paris 2003). Black found that men with AsPD aged less than 40 years had a strikingly high rate of premature death and obtained a value of 33 for the Standardised Mortality Rate (the age-adjusted ratio of observed deaths to expected deaths - meaning that they were 33 times more likely to die than similar males of the same age without this condition) (Black 1996). This increased mortality was due not only to an increased rate of suicide, but was also associated with reckless behaviours such as drug misuse and aggression. Follow-up studies in forensic-psychiatric settings suggest a similarly concerning picture. For example, Davies 2007 reported that 20 years after discharge from a medium secure unit almost half of the patients were reconvicted, with reconviction rates higher in those with personality order compared to mentally ill patients.
Significant comorbidity exists between AsPD and many Axis I disorders; mood and anxiety disorders are common, although the most frequent co-occurrence is with substance misuse. Men with AsPD have been found to be three to five times more likely to abuse alcohol and illicit drugs than those without the disorder (Robins 1991). The presence of personality disorder co-occurring with an Axis I condition may have a negative impact on the outcome of the latter (Newton-Howes 2006; Skodol 2005).
Description of the intervention
Psychological interventions have traditionally been the mainstay of treatment for AsPD, but the evidence upon which this is based is weak (Duggan 2007; NIHCE 2009). Psychological therapies encompass a wide range of interventions (Bateman 2004) but may be broadly classified into four main categories:
psychoanalytic psychotherapy;
cognitive behavioral;
therapeutic community; and
nidotherapy.
Traditionally, psychoanalytically-based psychological therapies held sway but latterly these have been replaced by more cognitive behavioral therapy-based approaches (Cordess 1996).
It is important to consider all relevant studies without restriction on the type of psychological therapy and to consider psychological interventions where drugs are also given as an adjunctive intervention.
How the intervention might work
Psychoanalytic therapies (which include dynamic psychotherapy, transference-focused psychotherapy, mentalisation-based therapy and group psychotherapy) aim to help the patient understand and reflect on his inner mental processes and make links between his past and his current difficulties. To our knowledge, no randomised trials have been published assessing the efficacy of dynamic psychotherapies specifically for AsPD but there are a small number of trials which examined the effectiveness of psychoanalytic therapies for personality disorder in general. Limited evidence for the efficacy of psychodynamic psychotherapy comes from Bateman 2001, Chiesa 2003, Piper 1993 and Winston 1994.
Cognitive behavioural therapy (CBT) based treatments place emphasis on encouraging the patient to challenge their core beliefs and to gain insight into how their thoughts and feeling affect their behaviour. A review of the evidence for this form of intervention concluded that “the overall evidence in favour of cognitive behavioural therapy in the treatment of personality disorder is therefore relatively slim, with much of the evidence coming from one research group, but it has involved more patients than any other form of treatment” (Bateman 2004).
Dialectical behavioural therapy (DBT) is a complex psychological intervention which was developed using some of the principles of CBT (Linehan 1993) and may help change behaviour by improving skills and the ability to contain difficult feelings. It is currently popular, but the evidence for its efficacy is less clear with some reviewers considering that its only proven benefit appears to be in the reduction of self-harm episodes (Bateman 2004). Cognitive analytic therapy (CAT) is a brief psychological therapy utilising ideas from psychodynamic psychotherapy, cognitive therapy and cognitive psychology (Denman 2001).
Therapeutic community treatments involve patients (also known as residents) not only having therapy together but also working and living together in a shared, therapeutic environment. This provides them with an opportunity to “explore intrapsychic and interpersonal problems and find more constructive ways of dealing with distress” (Campling 2001). Therapeutic community treatment is the only single treatment modality for severe personality disorder (which is likely to encompass AsPD and some other forms of personality disorder) that has been subject to a meta-analysis of randomised controlled trials. This demonstrated the effectiveness of therapeutic community treatment (Lees 1999) but several of the included studies did not specifically identify the participants as suffering from AsPD.
Nidotherapy is a formalised, planned method for achieving environmental change to minimise the effect of the patient’s disorder upon themselves and others. The effectiveness of this treatment has not yet been established. Unlike most other therapies it aims to fit the immediate environment to the patient rather than change the patient to cope in the existing environment (Tyrer 2007). Whilst the eventual outcome of nidotherapy is environmental manipulation, it may be regarded as a psychological intervention in that it relies upon first developing a psychological understanding of the person’s strengths and difficulties. From this psychological formulation there follows goal setting from which flows the necessary changes in the person’s physical and social environment (Tyrer 2005a).
Why it is important to do this review
Antisocial personality disorder is an important condition that has a considerable impact on individuals, families and society. Even by the most conservative estimate, AsPD appears to have the same prevalence in men as schizophrenia, the condition that receives the greatest attention from mental health professionals. Furthermore, AsPD is associated with significant costs, arising from emotional and physical damage to victims, damage to property, use of police time and involvement of the criminal justice system and prison services. Related costs include increased use of healthcare facilities, lost employment opportunities, family disruption, gambling and problems related to alcohol and substance misuse (Home Office 1999; Myers 1998). In one study the lifetime public services costs for a group of adults with a history of conduct disorder (of which 50% will go onto develop adult AsPD) were found to be 10 times those for a similar group without the disorder (Scott 2001).
AsPD is closely associated with criminal offending and any intervention that seeks to improve the outcome of AsPD is also likely to impact upon this offending. Aos 2001 reported that “for some crimes (especially those involving violence), the cost benefits in favour of intervention are often considerable as the costs of these types of crimes are often very high”.
Despite this, there is currently a dearth of evidence on how best to treat people diagnosed with AsPD, and to date the few reviews that have been carried out have been inconclusive and hampered by poor methodology. These issues were highlighted in Dolan and Coid’s (Dolan 1993) extensive review of the treatment of psychopathic and antisocial personality disorders. Unfortunately the challenge to produce high quality research in this area does not appear to have been fully taken up by the research community. This led a recent Review of Treatments for Severe Personality Disorder by the United Kingdom’s Home Office (Warren 2003) to wryly comment that “Despite the 1,600 copies of Dolan and Coid’s review having been purchased by clinicians, academics and institutions the methodological issues which were clearly set out in that review appear not to have been taken on board by the scientific community or those who fund research”. Similarly the recently published NICE clinical guidelines on the treatment of AsPD (NIHCE 2009, p.5) commented that there were “significant limitations to the evidence base, notably a relatively small number of randomised controlled trials (RCTs) of interventions with few outcomes in common”.
It is hoped that there will now have been additional good quality studies to address this important topic. Furthermore, a Cochrane Review of psychological treatments for AsPD will highlight areas where more work is needed and hopefully stimulate research interest.
OBJECTIVES
This review aims to evaluate the potential beneficial and adverse effects of psychological interventions for people with antisocial personality disorder.
METHODS
Criteria for considering studies for this review
Types of studies
Controlled trials in which participants have been randomly allocated to an experimental group and a control group, where the control condition is either treatment as usual, waiting list or no treatment. We included all relevant randomised controlled trials, with or without blinding of the assessors, and published in any language.
Types of participants
Men or women 18 years or over with a diagnosis of antisocial personality disorder defined by any operational criteria such as DSM-IV, or dissocial personality disorder as defined by operational criteria such as ICD-10. We included studies of people diagnosed with comorbid personality disorders or other mental health problems other than the major functional mental illnesses (i.e. schizophrenia, schizoaffective disorder or bipolar disorder). The decision to exclude persons with co-morbid major functional illness is based on the rationale that the presence of such disorders (and the possible confounding effects of any associated management or treatment) might obscure whatever other psychopathology (including personality disorder) might be present and make it more difficult to evaluate the potential effect of any intervention. We placed no restrictions on setting and included studies with participants living in the community as well as those incarcerated in prison or detained in hospital.
Types of interventions
We included studies of psychological interventions, both group and individual-based. This included, but was not limited to, interventions such as:
behaviour therapy;
cognitive analytic therapy;
cognitive behavioural therapy;
dialectical behaviour therapy;
group psychotherapy;
mentalisation-based therapy;
nidotherapy;
psychodynamic psychotherapy;
schema focused therapy;
social problem-solving therapy; and
therapeutic community treatment.
Psychological interventions were subclassified into single modality and complex psychological interventions. Single modality psychological interventions are those that only involve one specific type of intervention. Such interventions include cognitive analytic therapy and cognitive behavioural therapy. Complex psychological interventions are those that involve more than one modality of treatment (for example, group therapy plus individual therapy) and include dialectical behaviour therapy and psychodynamic psychotherapy with partial hospitalisation (Campbell 2000).
We included studies of psychological interventions where medication was given as an adjunctive intervention, but reported separately any studies where the comparison is between a psychological and a pharmacological intervention.
Studies comparing two or more different therapeutic modality groups but without a control group are not included in the review.
Types of outcome measures
Primary and secondary outcomes are listed below in terms of single constructs. We anticipated that a range of outcome measures would have been used in the studies included in the review (for example, aggression may be measured by a self-report instrument or by an external observer).
Primary outcomes
Aggression
reduction in aggressive behaviour or aggressive feelings; continuous outcome, measured through improvement in scores on the Aggression Questionnaire (AQ; Buss 1992), the Modified Overt Aggression Scale (MOAS; Malone 1994) or similar validated instrument; or as number of observed incidents.
Reconviction
measured as overall reconviction rate for the sample, or as mean time to reconviction.
Global state/functioning
continuous outcome, measured through improvement on the Global Assessment of Functioning numeric scale (GAF; APA 2000).
Social functioning
continuous outcome, measured through improvement in scores on the Social Adjustment Scale (SAS-SR; Weissman 1976), the Social Functioning Questionnaire (SFQ; Tyrer 2005b) or similar validated instrument.
Adverse events
measured as incidence of overall adverse events and of the three most common adverse events; dichotomous outcome, measured as numbers reported.
Secondary outcomes
Quality of life
self-reported improvement in overall quality of life; continuous outcome, measured through improvement in scores on the European Quality Of Life instrument (EuroQol; EuroQoL group 1990) or similar validated instrument.
Engagement with services
health-seeking engagement with services measured though improvement in scores on the Service Engagement Scale (SES; Tait 2002), or similar validated instrument.
Satisfaction with treatment
continuous outcome; measured through improvement in scores on the Client Satisfaction Questionnaire (CSQ-8; Attkisson 1982) or similar validated instrument.
Leaving the study early
measured as proportion of participants discontinuing treatment.
Substance misuse
measured as improvement on the Substance Use Rating Scale, patient version (SURSp; Duke 1994) or similar validated instrument. Where possible, drug misuse outcomes and alcohol misuse outcomes were differentiated.
Employment status
measured as number of days in employment over the assessment period.
Housing/accommodation status
measured as number of days living in independent housing/accommodation over the assessment period.
Economic outcomes
any economic outcome, such as cost-effectiveness measured using cost-benefit ratios or incremental cost-effectiveness ratios (ICERs).
Impulsivity
self-reported improvement in impulsivity; continuous outcome, measured through reduction in scores on the Barratt Impulsivity Scale (BIS; Patton 1995) or similar validated instrument.
Anger
self-reported improvement in anger expression and control; continuous outcome, measured through reduction in scores on the State-Trait Anger Expression Inventory-2 (STAXI-II; Spielberger 1999) or similar validated instrument.
Whilst acknowledging that the nature of the disorder can lead to difficulty in long-term follow up of individuals with AsPD, we aimed to report relevant outcomes without restriction on period of follow up. We aimed to divide outcomes into immediate (within six months), short-term (> 6 months to 24 months), medium term (> 24 months to five years) and long-term (beyond five years) if there were sufficient studies to warrant this.
Search methods for identification of studies
Electronic searches
The following electronic databases were searched to September 2009:
MEDLINE (from 1950);
EMBASE (from 1980);
CINAHL (from 1982);
the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2009, issue 3);
PsycINFO (from 1872);
Cochrane Schizophrenia Group’s register of trials related to forensic mental health;
ASSIA;
BIOSIS;
COPAC;
Dissertation Abstracts;
ISI-Proceedings;
ISI-SCI (Science Citation Index);
ISI-SSCI (Social Sciences Citation Index);
OpenSIGLE;
Sociological Abstracts;
ZETOC;
National Criminal Justice Reference Service Abstracts;
UK Clinical Trials Gateway*;
ClinicalTrials.gov*;
Action Medical Research*;
King’s College London (UK)*;
ISRCTN Register*;
The Wellcome Trust Register*;
NHS Trusts Clinical Trials Register*;
NHS R & D Health Technology Assessment Programme Register (HTA)*; and
NHS R & D Regional Programmes Register*.
*Searched using the meta Register of Controlled Trials (http://www.controlled-trials.com/mrct/).
Searching other resources
We searched the reference lists of included and excluded studies for additional relevant trials. We examined bibliographies of systematic review articles published in the last five years to identify relevant studies. We contacted authors of relevant studies to enquire about other sources of information and the first author of each included study for information regarding unpublished data.
Data collection and analysis
Selection of studies
Because this review is part of a larger series of reviews of personality disorders, the selection of studies was carried out in two stages. In the first stage, titles and abstracts were read independently by two review authors (JS and NH) against the inclusion criteria to identify all studies carried out with participants with personality disorder, regardless of any specific personality disorder(s) diagnosed. In the second stage, full copies of studies identified in stage one were assessed against the inclusion criteria by two review authors independently (SG and BV). This second stage assessment identified not only trials with participants diagnosed with antisocial or dissocial PD, but also trials with participants having a mix of PDs for which data on a subgroup with antisocial or dissocial PD might be available.
Studies with two treatment conditions in which the relevant participants formed a small subgroup were only included if the trial investigators randomised at least five people with antisocial or dissocial personality disorder. The rationale is that variance and standard deviation cannot be calculated in samples of two or less, and a two-condition study that randomises less than five relevant participants will have at least one arm for which variance or standard deviation cannot be calculated.
Uncertainties concerning the appropriateness of studies for inclusion in the review were resolved through consultation with a third review author (CD).
Data extraction and management
Three review authors (MF, NH and SG) extracted data independently using a data extraction form and entered data into RevMan 5 (RevMan 2008). Where data were not available in the published trial reports, we contacted the authors and asked them to supply the missing information. We made significant efforts to contact the primary trial investigator for missing data on any subgroup of participants diagnosed with AsPD where this was not published. If these data were made available to us, we included the data in the review. If data were not forthcoming, we attempted to contact at least one of the co-investigators. A reasonable length of time (eight weeks) was allowed for the investigator(s) to supply the missing data before we proceeded with the analysis.
Assessment of risk of bias in included studies
For each included study, two review authors (MF and NH) independently completed the Cochrane Collaboration’s tool for assessing risk of bias (Higgins 2008, section 8.5.1) with any disagreement resolved through consultation with a third review author (SG). We assessed the degree to which:
the allocation sequence was adequately generated (‘sequence generation’);
the allocation was adequately concealed (‘allocation concealment’);
knowledge of the allocated interventions was adequately prevented during the study (‘blinding’), whilst acknowledging that it is generally not possible to blind participants in trials of this nature;
incomplete outcome data were adequately addressed;
reports of the study were free of suggestion of selective outcome reporting; and
the study was apparently free of other problems that could put it at high risk of bias.
We allocated each domain one of three possible categories for each of the included studies: ‘Yes’ for low risk of bias, ‘No’ for high risk of bias, and ‘Unclear’ where the risk of bias was uncertain or unknown.
Measures of treatment effect
For dichotomous (binary) data, we used the odds ratio with a 95% confidence interval to summarise results within each study. The odds ratio is chosen because it has statistical advantages relating to its sampling distribution and its suitability for modelling, and because it is a relative measure and so can be used to combine studies.
For continuous data, such as the measurement of impulsiveness on a scale, we compared the mean score for each outcome as determined by a standardised tool between the two groups to give a mean difference (MD), again with a 95% confidence interval. Where possible, we made these comparisons at specific follow-up periods: (1) within the first month, (2) between one and six months, and (3) between six and 12 months. Where possible, we presented endpoint data. Where both endpoint and change data were available for the same outcomes, then we only reported the former.
We reported continuous data that are skewed in a separate table, and did not calculate treatment effect sizes to minimise the risk of applying parametric statistics to data that depart significantly from a normal distribution. We define skewness as occurring when, for a scale or measure with positive values and a minimum value of zero, the mean is less than twice the standard deviation (Altman 1996). We summarised change-from-baseline (‘change score’) data along-side endpoint data where these were available. Change-from-baseline data may be preferred to endpoint data if their distribution is less skewed, but both types may be included together in meta-analysis (Higgins 2008, page 270). Where the data were insufficient for meta-analysis, we reported the results of the trial investigators’ own statistical analyses comparing treatment and control conditions using change scores.
In any meta-analysis, we intended to use the mean difference (MD) where the same outcome measure was reported in more than one study and the standardised mean difference (SMD) if different outcome measures of the same construct had been reported.
Unit of analysis issues
(a) Cluster-randomised trials
See Table 4 for information about future updates of this review.
Table 4. Additional methods for future updates.
| Issue | Method |
|---|---|
| Cluster-randomised trials | Where trials use clustered randomisation, study investigators may present their results after appropriately controlling for clustering effects (robust standard errors or hierarchical linear models). If, however, it is unclear whether a cluster-randomised trial has used appropriate controls for clustering, we will contact the study investigators for further information. If appropriate controls were not used, we will request individual participant data and re-analysed these using multilevel models which control for clustering. Following this, effect sizes and standard errors will be meta-analysed in RevMan5 using the generic inverse method (Higgins 2008). If appropriate controls were not used and individual participant data are not available, we will seek statistical guidance from the Cochrane Methods Group and external experts as to which method to apply to the published results in attempt to control for clustering. If there is insufficient information to control for clustering, outcome data will be entered into RevMan5 using the individual as the unit of analysis, and then sensitivity analysis used to assess the potential biasing effects of inadequately controlled clustered trials (Donner 2001). |
| Missing data | The standard deviations of the outcome measures should be reported for each group in each trial. If these are not given, we will impute standard deviations using relevant data (for example, standard deviations or correlation coefficients) from other, similar studies (Follman 1992) but only if, after seeking statistical advice, to do so is deemed practical and appropriate Assessment will be made of the extent to which the results of the review could be altered by the missing data by, for example, a sensitivity analysis based on consideration of ’best-case’ and ’worst-case’ scenarios (Gamble 2005). Here, the ’best-case’ scenario is that where all participants with missing outcomes in the experimental condition had good outcomes, and all those with missing outcomes in the control condition had poor outcomes; the ’worst-case’ scenario is the converse (Higgins 2008, section 16.2.2). We will report data separately from studies where more than 50% of participants in any group were lost to follow up. Where meta-analysis is undertaken, we will assess the impact of including studies with attrition rates greater than 50% through a sensitivity analysis. If inclusion of data from this group results in a substantive change in the estimate of effect of the primary outcomes, we will not add the data from these studies to trials with less attrition and will present them separately Any imputation of data will be informed, where possible, by the reasons for attrition where these are available. We will interpret the results of any analysis based in part on imputed data with recognition that the effects of that imputation (and the assumptions on which it is based) can have considerable influence when samples are small |
| Assessment of heterogeneity | We will consider I2 values less than 30% as indicating low heterogeneity, values in the range 30% to 70% as indicating moderate heterogeneity, and values greater than 70% as indicating high heterogeneity. We will make an attempt to identify any significant determinants of heterogeneity categorised at moderate or high |
| Assessment of reporting biases | We will draw funnel plots (effect size versus standard error) to assess publication bias. Asymmetry of the plots may indicate publication bias, although they may also represent a true relationship between trial size and effect size. If such a relationship is identified, we will further examine the clinical diversity of the studies as a possible explanation (Egger 1997). |
| Data synthesis and length of follow up | We will group outcome measures by length of follow up, and use the weighted average of the results of all the available studies to provide an estimate of the effect of psychological interventions for people with antisocial personality disorder. We will use regression techniques to investigate the effects of differences in study characteristics on the estimate of the treatment effects. We will seek statistical advice before attempting meta-regression. If meta-regression is performed, it will be executed using a random-effects model |
| Subgroup analysis | We will undertake subgroup analysis to examine the effect on primary outcomes of:
|
| Sensitivity analysis | We will undertake sensitivity analyses to investigate the robustness of the overall findings in relation to certain study characteristics. A priori sensitivity analyses are planned for:
|
(b) Multi-arm trials
All eligible outcome measures for all trial arms were included in this review.
Dealing with missing data
We attempted to contact the original investigators to request any missing data and information on whether or not it can be assumed to be ‘missing at random’. For dichotomous data, we report missing data and drop-outs for each included study and report the number of participants who are included in the final analysis as a proportion of all participants in each study. We provide reasons for the missing data in the narrative summary where these are available. For missing continuous data, we provide a qualitative summary. See Table 4 for information about future updates of this review.
Assessment of heterogeneity
We aimed to assess the extent of between-trial differences and the consistency of results of any meta-analysis in three ways: by visual inspection of the forest plots, by performing the Chi2 test of heterogeneity (where a significance level less than 0.10 is interpreted as evidence of heterogeneity), and by examining the I2 statistic (Higgins 2008; section 9.5.2). The I2 statistic describes approximately the proportion of variation in point estimates due to heterogeneity rather than sampling error. See Table 4 for information about future updates of this review.
Assessment of reporting biases
See Table 4 for information about future updates of this review.
Data synthesis
We had planned to use meta-analyses to combine comparable outcome measures across studies. In carrying out meta-analysis, the weight given to each study is the inverse of the variance so that the more precise estimates (from larger studies with more events) are given more weight. See Table 4 for information about future updates of this review.
Subgroup analysis and investigation of heterogeneity
See Table 4 for information about future updates of this review.
Sensitivity analysis
See Table 4 for information about future updates of this review.
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification.
Results of the search
We carried out electronic searches over two consecutive time periods to minimise the difficulty of managing large numbers of citations. Searches to December 2006 produced in excess of 10,000 records. From inspection of titles and abstracts we identified 70 citations that appeared to describe randomised studies on psychological interventions for personality disorder. Twenty-one of these appeared to include participants with a diagnosis of antisocial or dissocial personality disorder (PD). Searches from December 2006 to September 2009 produced 6398 records. After excluding studies that focused exclusively on borderline PD, we identified 38 citations that appeared to describe randomised trials on psychological interventions for personality disorder. Twenty-seven of these had the potential to have included participants with a diagnosis of antisocial or dissocial PD. Full copies were obtained of the 48 records of studies where all or part of the sample appeared to meet diagnostic criteria for antisocial or dissocial PD.
Included studies
Of the 48 studies, we identified 11 that fully met the inclusion criteria. Ten included participants with antisocial personality disorder (under DSM criteria). One study (Tyrer 2004) included participants with dissocial personality disorder (under ICD-10 criteria). Data on participants with antisocial personality disorder (AsPD)were available for five of the 11 studies (Davidson 2009; Huband 2007; Messina 2003; Neufeld 2008; Woodall 2007) and these are summarised in this review. Data on the subgroup of participants with antisocial (or dissocial) PD from the other six studies (Ball 2005; Havens 2007; Marlowe 2007; McKay 2000; Tyrer 2004; Woody 1985) were not available at the time this review was prepared.
The 11 included studies involved a total of 14 comparisons of a psychological intervention against a relevant control condition (i.e. treatment as usual, waiting list or no treatment). There were some important differences between the studies. We summarise these differences and the main characteristics below. Further details are provided in the Characteristics of included studies table.
Only three of the included studies addressed the primary outcomes defined in this review. Two studies reported on reconviction (Marlowe 2007; Woodall 2007) and one reported on aggression (Davidson 2009).
Design
Ten of the 11 studies were parallel trials with allocation by individual participant, and one (Havens 2007) was a cluster-randomised trial where the unit of allocation was treatment site. The 10 parallel trials included one two-condition comparison (Woody 1985) and one three-condition comparison (Messina 2003) against a control group.
Sample sizes
There was some variation in sample size between studies. Overall, 411 participants with antisocial or dissocial PD were randomised in the nine trials where this allocation was reported unambiguously, with the size of sample ranging from 15 to 100 (mean 45.7; SD 24.8). However, data were available to us for only five of these trials. In these, 276 participants with antisocial or dissocial PD were randomised, and sample size ranged from 24 to 100 (mean 55.2; SD 27.6). The number of participants completing was reported in only four studies where the proportion that completed ranged from 78.8% to 100% (mean 89.1%).
Setting
Three studies were carried out in the UK (Davidson 2009; Huband 2007; Tyrer 2004); the remaining eight took place in North America (Ball 2005; Havens 2007; Marlowe 2007; Messina 2003; McKay 2000; Neufeld 2008; Woodall 2007; Woody 1985). Five were multi-centre trials: Davidson 2009 with two sites; Havens 2007 with 10 sites; Huband 2007 with five sites; Messina 2003 with two sites; and Tyrer 2004 with five sites. Nine studies took place in an outpatient or community setting, and two (Marlowe 2007; Woodall 2007) in a prison or custodial environment. None were carried out in a hospital inpatient setting.
Participants
Participants were restricted to males in three studies (Davidson 2009; McKay 2000; Woody 1985). The remaining eight studies had a mix of male and female participants. With one exception (Tyrer 2004), all studies randomised more men than women. The overall mix was 79.9% men as compared to 20.1% women. All eleven studies involved adult participants, with the mean age per study ranging between 25.1 and 43.5 years (average 34.9 years).
Eight studies focused on participants with substance misuse difficulties. For these, inclusion criteria included opioid substance dependence disorder (Neufeld 2008; Woody 1985), cocaine dependence disorder (Messina 2003; McKay 2000), sentenced for driving whilst intoxicated (Woodall 2007), recent alcohol/drug use whilst homeless (Ball 2005), sentenced for a drug-related offence (Marlowe 2007), and being an intravenous drug user (Havens 2007). The remaining three studies did not recruit participants on the basis of substance misuse. For these, the focus was on recurrent self-harm (Tyrer 2004), violence (Davidson 2009) and meeting DSM-IV criteria for (any) personality disorder (Huband 2007).
Only two of the 11 studies focused exclusively on participants with a diagnosis of antisocial PD (Davidson 2009; Neufeld 2008). For the remaining nine, participants with antisocial or dissocial PD formed a subgroup. The size of this antisocial subgroup ranged from 15 to 52 participants, representing 3.1% to 46.1% respectively of the total sample (mean 28.5%). Data on the antisocial subgroup were available to us for only three (Huband 2007; Messina 2003; Woodall 2007) of these nine studies.
The precise definition of antisocial personality disorder and the method by which it was assessed varied between the studies. Six used DSM-IV criteria and made assessments using the Structured Clinical Interview for DSM Axis II disorders (SCID-II) (Davidson 2009; Havens 2007; Messina 2003), an ‘antisocial PD interview’ developed by the investigators from the SCID-II (Marlowe 2007), the International Personality Disorder Examination (Huband 2007), or the Personality Disorder Questionnaire (Ball 2005). Three studies used DSM-III-R criteria and assessed using the SCID-II (McKay 2000; Neufeld 2008), or the Diagnostic Interview Schedule (Woodall 2007). One earlier study used DSM-III criteria and made assessments using the Schedule for Affective Disorders & Schizophrenia and the Maudsley Personality Inventory (Woody 1985). One study used ICD-10 criteria and assessed using the PAS-Q (Tyrer 2004).
Ethnicity of participants was not always reported. Where it was, the proportion of the sample described by the investigators as either ‘white’ or ‘Caucasian’ ranged from 7% to 67% per study. The total number of white participants randomised expressed as a proportion of total randomised was 58% for those studies where this information was available. Taking just the studies from which data could be extracted for participants with antisocial or dissocial PD, the proportion of the sample described as either ‘white’ or ‘Caucasian’ ranged from 31% to 67% per study. Overall, 63% of all participants randomised were described as neither ‘white’ nor ‘Caucasian’.
Interventions
The following types of interventions were represented: behaviour therapy, cognitive behaviour therapy, schema therapy, and social problem-solving therapy. Interventions that were group-based may have included elements of group psychotherapy, depending on how group psychotherapy is defined. None of the 11 studies evaluated psychodynamic psychotherapy, therapeutic community treatment, dialectical behaviour therapy, cognitive analytic therapy, mentalisation-based therapy or nidotherapy.
Eleven different psychological interventions were compared to a control condition. Full details are provided in the Characteristics of included studies table but can be summarised as follows and in Table 5 below.
Table 5. Details of the psychological interventions examined in the 11 included studies.
| Intervention | Description |
|---|---|
|
CBT + standard maintenance
Messina 2003 |
CBT is a structured intervention based on behavioural principles with positive verbal reinforcement of decreased or no use of illicit drugs, or for prosocial behaviour). Comprises 48 group sessions of 90 minutes (three per week for 16 weeks) with typically four to eight participants in each group. Participants continue on standard maintenance treatment (including methadone, mean 72 mg/day) |
|
Supportive-expressive psychotherapy + standard maintenance
Woody 1985 |
Supportive-expressive psychotherapy is an analytically-oriented focal psychotherapy. Standard maintenance is an individual counselling intervention focused on providing external services rather than dealing with intra-psychic processes, plus methadone maintenance |
|
Dual-focus schema therapy
Ball 2005 |
Dual focus schema therapy is a 24-week manual-guided individual therapy that integrates symptom-focused relapse prevention coping skills techniques with schema-focused techniques for early maladaptive schemas and coping styles |
|
Contingency management + standard maintenance
Neufeld 2008 Messina 2003 |
Neufeld 2008: Contingency-based behavioural programme is a highly structured contingency-based, adaptive treatment protocol comprising counselling sessions and behavioural interventions. Drug abstinence and counselling attendance are rewarded by greater control over methadone management with negative reinforcers being a reduction in methadone dosage and control of the dosage. Standard maintenance comprises standard methadone substitution treatment with two individual counselling sessions per week with bi-weekly reviews; negative drug screens are rewarded with methadone take home doses Messina 2003: Contingency management + standard maintenance comprises a brief meeting (two to five minutes) with a contingency management technician. Clean urine specimens are rewarded with vouchers of escalating value (to a maximum of $1277. 50 if drug-free for the 16 weeks of the trial) and with praise/encouragement. Positive samples result in the vouchers being with-held but the participant is not rebuked or punished. Participants continue on standard maintenance treatment (including metha-done, mean 62 mg/day) |
|
Individualised relapse prevention aftercare
McKay 2000 |
Individualised relapse prevention is a manualised modular intervention for substance users in the maintenance phase of recovery. Risky situations are identified and improved coping responses encouraged. Clients receive one individual relapse prevention session and one group session per week for up to 20 weeks |
|
Strengths-based case management
Havens 2007 |
Strengths-based case management includes engagement, strengths assessment, personal case planning, and resource acquisition. Services provided by case managers include advice on referrals to health and social services, and on transportation and employment |
|
Optimal judicial supervision
(Marlowe 2007) |
Optimal (’matched’) schedule of court hearings in which frequency of court attendance is matched with risk, so that high-risk offenders (those with AsPD and a history of drug treatment) attend with greater frequency. Group sessions were psychoeducational and covered a range of topics including relapse prevention strategies |
|
’Driving Whilst Intoxicated program’ + incarceration
Woodall 2007 |
The ’Driving Whilst Intoxicated program’ is non-confrontational and utilises a psychoeducational approach on the harmful effects of alcohol, stress management, and a work release programme for those in employment. It also incorporated culturally appropriate elements (71% of participants were native American). The programme was delivered whilst participants were subject to 28 days incarceration |
|
CBT + treatment as usual
Davidson 2009 Tyrer 2004 |
Davidson 2009: CBT involves a cognitive formulation of the individual’s problems (to promote engagement) and therapy focusing on beliefs about self and others that impair social functioning. Individuals were offered 15 or 30 sessions of CBT (to determine the optimal ’dose’) and therapist adherence/competence was assessed for a random selection (30%) of sessions by audio recording and found to be ”within competent range”. Tyrer 2004: Manual-assisted cognitive behaviour therapy (MACT) is a treatment for self-harming behaviour where participants are provided with a booklet based on CBT principles plus an offer of five plus two booster sessions of CBT in the first three months |
|
Social problem-solving therapy with psychoeducation
Huband 2007 |
An individual psychoeducation programme followed by 16 weekly group-based problem-solving sessions (lasting approximately two hours) based on the ’Stop and Think!’ method. Groups start with no more than eight participants in each and are single gender. |
Single modality interventions focused on substance misuse difficulties
CBT + standard maintenance (Messina 2003 for outpatients with cocaine dependence; Woody 1985 for male outpatients with opioid dependence, but with no data available for the AsPD subgroup).
Supportive-expressive psychotherapy + standard maintenance (Woody 1985 for male outpatients with opioid dependence, but with no data available for the AsPD subgroup).
Dual-focus schema therapy (Ball 2005 for homeless adults with substance abuse, but with no data available for the AsPD subgroup).
Complex interventions focused on substance misuse difficulties
Contingency management + standard maintenance (Neufeld 2008 and Messina 2003, both for outpatients with cocaine dependence).
Contingency management + CBT + standard maintenance (Messina 2003 for outpatients with cocaine dependence).
Individualised relapse prevention aftercare (McKay 2000 for male outpatients with cocaine dependence, but with no data available for the AsPD subgroup).
Strengths-based case management (Havens 2007 for intravenous drug-using outpatients, but with no data available for the AsPD subgroup).
Optimal judicial supervision (Marlowe 2007 for adult drug court offenders, but with no data available for the AsPD subgroup).
‘Driving Whilst Intoxicated program’ + incarceration (Woodall 2007 for incarcerated drink-driving offenders with AsPD).
Single modality interventions not focused on substance misuse difficulties
CBT + treatment as usual (Davidson 2009 for male outpatients with AsPD and recent verbal/physical violence; Tyrer 2004 for outpatients with recurrent self-harm, but with no data available for the dissocial PD subgroup).
Social problem-solving therapy with psychoeducation (Huband 2007 for community-living adults with personality disorder and an AsPD subgroup).
It is important to note that participants allocated to the experimental condition in these studies commonly received some degree of treatment as usual in addition to the intervention under evaluation. It could be argued that the presence of such ‘treatment’ requires single modality interventions to be reclassified as complex. For example, standard maintenance for participants with opioid dependence commonly includes counselling sessions in addition to methadone maintenance, which could be seen as introducing an additional CBT component. We have, however, chosen to regard single modality interventions as uncontaminated by any ‘treatment as usual’ providing that similar ‘treatment as usual’ forms the control condition.
The duration of the interventions (excluding the very short intervention described by Havens 2007) ranged between four and 52 weeks (mean 23.5 weeks; median 24 weeks). Seven studies followed up participants beyond the end of the intervention period by, on average, 30.9 weeks (range four to 104 weeks).
Control conditions
The inclusion criteria required a control condition that was either treatment as usual, waiting list or no treatment (see Types of studies). We considered that all 11 studies had a control condition that could be described as treatment as usual (TAU). This decision was straightforward for six of the 11 studies, as follows. For Davidson 2009 and Tyrer 2004 it was clear that TAU simply comprised whatever treatment the participants would have received had the trial not taken place. For Huband 2007, treatment as usual pertained whilst on a wait-list for the intervention under evaluation. Treatment as usual was incarceration in Woodall 2007, passive referral in Havens 2007 and standard (‘unmatched’) schedule court hearings in Marlowe 2007.
For the remaining five studies, all of which focused on participants with substance misuse difficulties, we were forced to consider carefully whether the control condition was treatment as usual or an intervention in its own right. In each case we concluded that the control condition could properly be described as TAU because it represented what a treatment-seeking participant with similar substance misuse problems would normally experience had the trial not taken place. The control conditions for these five studies can be summarised:
Ball 2005: up to three sessions per week of group counselling and psychoeducation sessions plus standard methadone maintenance where appropriate, which the trial investigators described as ‘standard group substance abuse counselling’.
Messina 2003: one counselling session per fortnight, standard methadone maintenance, case management visits and medical care, which the trial investigators described as ‘methadone maintenance only’.
Neufeld 2008: two individual counselling sessions per week with standard methadone maintenance treatment, which the trial investigators described as ‘standard methadone substitution treatment’.
Woody 1985: standard drug counselling, which the investigators described as ‘a standard individual counselling intervention focused on providing external services rather than dealing with intra-psychic processes’, plus standard methadone maintenance.
McKay 2000: two group therapy sessions per week based on addictions-counselling and 12-step recovery practices, which the trial investigators described as ‘standard continuing care treatment’.
Outcomes
Primary outcomes
One study included self-reported aggression as an outcome: Davidson 2009 summarised the number of participants reporting any incident of physical or verbal aggression, as measured with the MacArthur Community Violence Screening Instrument (MCVSI) interview, plus additional questions on four other behaviours (shouting angrily at others; threatening harm to others; causing damage to property; self-harm).
Two studies included reconviction as an outcome: Woodall 2007 reported drink-driving reconviction using data from the New Mexico State Citation Tracking System, and Marlowe 2007 assessed re-arrests and convictions using state criminal justice databases (although with no data available for the subgroup with AsPD).
Adverse effects, which are generally reported only rarely in studies of psychological interventions, were mentioned only by Marlowe 2007 where the investigators noted the absence of any study-related adverse events.
Four studies included self-reported social functioning as an outcome. Both Davidson 2009 and Huband 2007 reported mean scores on the Social Functioning Questionnaire (SFQ). Neufeld 2008 reported composite scores on the family/social domain of the Addiction Severity Index (ASI), and Ball 2005 reported scores using the same measure but with no data available for the subgroup with AsPD. The ASI is a semi-structured interview designed to assess problem severity in seven areas commonly affected by substance misuse difficulties, one of which is termed the family/social domain. Investigators obtained composite scores for this domain ranging from zero to 1.0 and based on problems reported in the last 30 days. Other domains relevant to this review are those concerning alcohol use, drug use and employment problems (see paragraph below on secondary outcomes).
There were five studies that did not report on any of the primary outcomes defined in the protocol for this review (Havens 2007; McKay 2000; Messina 2003; Tyrer 2004; Woody 1985); of these, only Messina 2003 had data available for participants with AsPD.
Secondary outcomes
Studies varied widely in their choice of secondary outcomes. Seven reported on leaving the study early, measuring this as the proportion of participants discontinuing treatment before endpoint. Three had data available for participants with AsPD (Davidson 2009; Messina 2003; Neufeld 2008). The remaining four had no data available for the AsPD subgroup (Ball 2005; Marlowe 2007; McKay 2000; Woody 1985). The mean number of continuing care sessions attended was additionally reported by McKay 2000. Only Davidson 2009 examined satisfaction with treatment as an outcome: the investigators used a semi-structured interview to enquire about ‘satisfaction with taking part in study’ and rated responses on a Likert scale from 1 to 7.
One study considered employment status: Neufeld 2008 reported mean composite scores on the employment domain of the Addiction Severity Index (ASI).
One study (Huband 2007) measured self-reported impulsivity using mean scores on the Barratt Impulsiveness Scale (BIS).
Economic outcomes were considered by two studies: Davidson 2009 examined the total cost per participant of healthcare, social care and criminal justice services measured using case records and the Client Service Receipt Inventory (CSRI); Tyrer 2004 calculated as total costs per participant, including costs incurred by all service-providing sectors and productivity losses resulting from time off work due to illness, although with no data available for the subgroup with dissocial PD.
Two studies included a self-reported measure of anger: Davidson 2009 provided mean scores on the NOVACO Scale and Provocation Inventory (NAS-PI), and Huband 2007 provided mean anger expression index scores using the State-Trait Anger Expression Inventory (STAXI-2).
To aid interpretation, ‘substance misuse’ was considered as two separate outcomes (see section on Differences between protocol and review). Substance misuse (drugs) was examined in six studies using the drug use domain of the Addiction Severity Index (ASI) (Marlowe 2007; McKay 2000; Neufeld 2008; Woody 1985), using the Cocaine Relapse Interview (CRI) (McKay 2000), and through urinalysis (Marlowe 2007; McKay 2000, Messina 2003; Neufeld 2008). Substance misuse (alcohol) was examined by three studies using the alcohol use domain of the Addiction Severity Index (Neufeld 2008), using the Alcohol Use Disorders Identification Test (AUDIT) (Davidson 2009), and via the Form 90 (a time-line follow-back self-report method to assess drinking over the previous 90 days) and the Drinker Inventory of Consequences (DrInC-2R) (Woodall 2007). In addition, Woodall 2007 reported the frequency of drink-driving in 30 days prior to arrest, or in previous 30 days, measured via questionnaire.
The outcome of engagement with services was considered only by Havens 2007 where the investigators report numbers entering into drug addiction treatment services as a key outcome, although with no data available for the AsPD subgroup.
No study reported on quality of life.
Other relevant outcomes
Psychiatric symptoms were measured in several studies: depression scores were reported using the Beck Depression Inventory (BDI) by Woody 1985; both anxiety and depression using the Hospital Anxiety and Depression Rating Scale (HADS) by Davidson 2009; or generally using the Symptoms Checklist (SCL90) (Woody 1985) or the Brief Symptom Inventory (BSI) (Ball 2005). Huband 2007 reported on shame using the Experience of Shame Scale (ESS), on dissociation using the Dissociative Experiences Scale (DES), and on social problem-solving ability via Social Problem Solving Inventory-Revised (SPSI-R). Ball 2005 reported on interpersonal problems via the Inventory of Interpersonal Problems (IIP), on severity of PD via the Personality Diagnostic Questionnaire (PDQ), and on schemas via scores on Early Maladaptive Schema Questionnaire-Research (EMSQ-R). Davidson 2009 reported on schemas using the Brief Core Schema Scales (BCSS). Tyrer 2004 reported number of completed suicides and frequency of self-harm episodes via the Parasuicide History Interview (PHI). Finally, therapy retention was measured as total weeks in treatment (Ball 2005), as adherence to counselling sessions (Neufeld 2008) or as the proportion therapeutically transferred over to routine care due to poor/partial treatment response in response to ongoing drug use or poor attendance to scheduled services (Neufeld 2008).
Studies awaiting classification
We identified three studies of psychological treatments for samples with a mixture of personality disorders where it remains unclear whether a subgroup of participants with a diagnosis of antisocial or dissocial PD had been included (Berget 2008; Evans 1999; Linehan 2006). Clarification has been sought from the trial investigators but no further information was available at the time this review was prepared. Details are provided in the Characteristics of studies awaiting classification table. These may be summarised as follows.
Berget 2008 compared animal-assisted therapy with a control condition in individuals with psychiatric disorders, and may have recruited a subgroup with dissocial PD since 22 of the 90 participants had a disorder diagnosed under sections F60-69 in ICD-10 (disorders of adult personality and behaviour).
Evans 1999 compared manualised cognitive therapy with treatment as usual in adults with recent self-harm and cluster B personality disturbance. The investigators may have recruited a subgroup with dissocial PD since, although formal Axis II diagnoses are not reported, all participants scored on the Personality Assessment Schedule at least to the level of personality disturbance within the flamboyant cluster of ICD-10.
Linehan 2006 compared DBT and community treatment by experts for adults with suicidal behaviour and BPD, and may have recruited a subgroup with AsPD since 11 of the 101 participants (10.9%) had at least one other cluster B personality disorder.
Excluded studies
The remaining 34 studies that failed to meet all inclusion criteria were categorised as excluded studies. Fifteen were excluded because on close inspection, and following translation into English and contact with the investigators where necessary, it became clear that the sample did not include a subgroup with antisocial or dissocial PD. A further six were excluded because there were less than five participants with antisocial or dissocial PD for reasons that are now explained in the Selection of studies section. Five were excluded because participants had not been allocated at random, and a further six because of lack of a relevant control condition. One study was excluded because it was a trial of assessment rather than of psychological treatment, and one because a proportion of the sample had bipolar disorder. Reasons for exclusion of each of these 34 studies are given in the Characteristics of excluded studies table.
We paid particular attention to five of the excluded studies (described in seven separate reports) that compared one psychological treatment against another. Each was excluded because there was no control condition that could be regarded as treatment as usual, waiting list or no treatment. Although none of these studies focused exclusively on AsPD, and none provided data on their AsPD subgroup, each reported information that we considered would be of interest to a clinician who was seeking treatment options for clients with AsPD. Because of this, we have summarised briefly the characteristics of each of these five studies and conclusions drawn by the trial investigators in the Discussion section.
Risk of bias in included studies
There was considerable variation in how the included studies were reported. We attempted to contact the investigators wherever the available trial reports provided insufficient information for decisions to be made about the likely risk of bias, and were successful in respect of four studies.
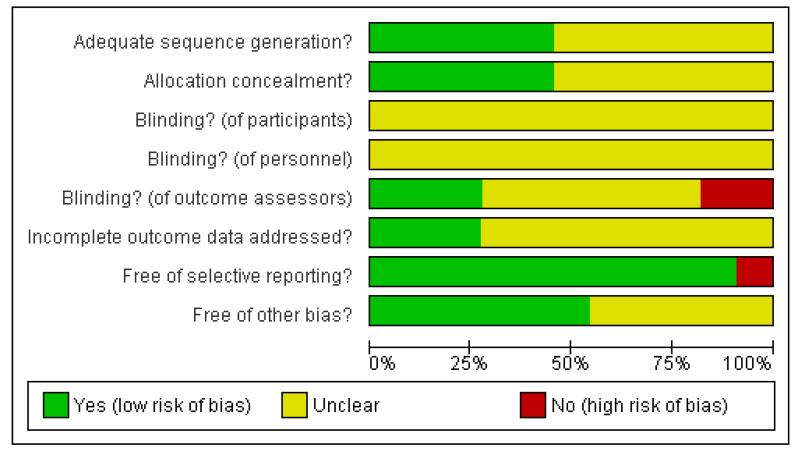
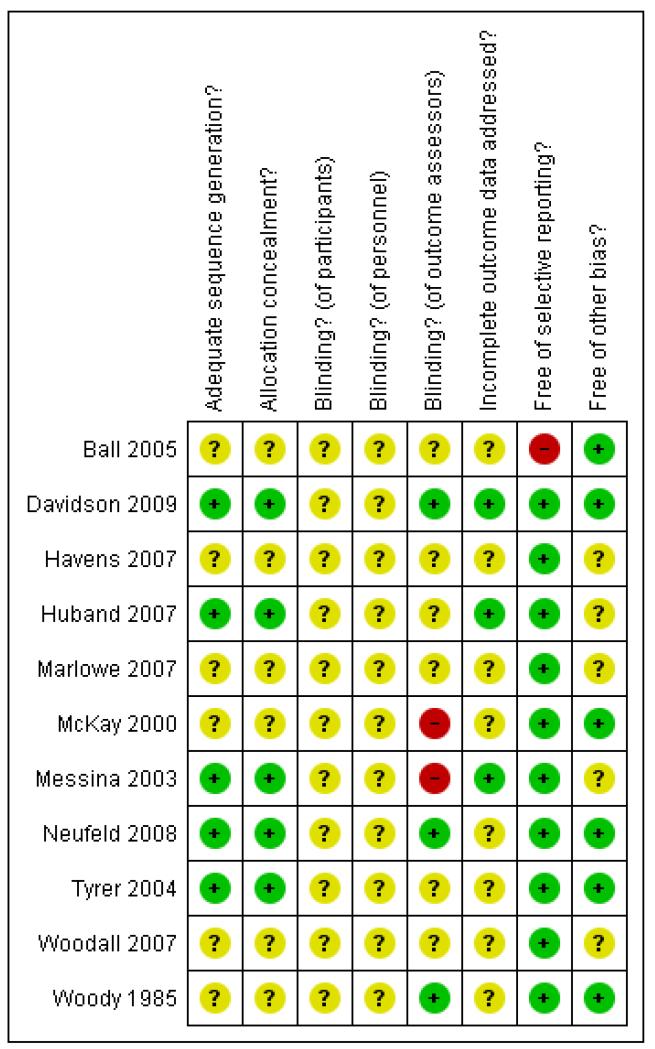
We summarise below the risk of bias for the 11 included studies. Studies with data that could be extracted for the antisocial or dissocial PD subgroup (n = 5) are summarised separately from those for which data were unavailable (n = 6). This allows the reader to make a separate judgement about possible bias associated with the quantitative data from which conclusions are drawn in this review. Full details of our assessment of the risk of bias in each case are tabulated within the Characteristics of included studies section. Graphical summaries of methodological quality are presented as Figure 1 and Figure 2.
Figure 1.
Methodological quality graph: review authors’ judgements about each methodological quality item presented as percentages across all included studies.
Figure 2.
Methodological quality summary: review authors’ judgements about each methodological quality item for each included study.
Allocation
With data (five studies)
We considered the generation of allocation sequence to be adequate in three studies where allocation was by random numbers which were computer-generated (Davidson 2009; Huband 2007) or derived from a table (Messina 2003), and in one study where the toss of coin was used (Neufeld 2008). We classified adequacy of sequence generation as ‘unclear’ in the remaining study (Woodall 2007) where the investigators reported that participants had been allocated at random but provided no further information on how this had been achieved. We considered concealment of the allocation sequence adequate for Davidson 2009, Huband 2007, Neufeld 2008 and Messina 2003 where we considered that there was sufficient evidence that the person enrolling participants could not have foreseen assignment. We classified adequacy of sequence concealment as ‘unclear’ in the remaining study (Woodall 2007) because the information available was insufficient to allow a judgment to be made.
Without data (six studies)
We classified adequacy of sequence generation as adequate for Tyrer 2004 (computer-generated random numbers) but ‘unclear’ for the remaining five studies. In each case the investigators reported that participants had been allocated at random but provided no further information on how this had been achieved. We considered concealment of the allocation sequence adequate for Tyrer 2004. We classified adequacy of sequence concealment as ‘unclear’ in the remaining five studies, again because the information available was insufficient to allow a judgement to be made.
Blinding
We judged that blinding of participants and personnel involved in the delivery of the intervention was not practical in the design of trials of psychological interventions summarised in this review.
With data (five studies)
We considered adequacy of blinding of outcome assessors to be adequate in two studies (Davidson 2009; Neufeld 2008) and that it was unlikely that this blind could have been broken. In Messina 2003 the outcome assessors were not blinded. We classified two studies as ‘unclear’ because the information available was insufficient to allow a judgment to be made (Huband 2007; Woodall 2007).
Without data (six studies)
We judged adequacy of blinding of outcome assessors adequate for Woody 1985, not adequate for McKay 2000 and ‘unclear’ in the remaining four studies where there was insufficient information to allow a judgement to be made.
Incomplete outcome data
With data (five studies)
We judged none to have adequately addressed incomplete outcome data. We classified all five as ‘unclear’ because, although numbers balanced approximately between treatment conditions, the reasons for attrition were not available. This generally arose because participants failed to complete endpoint measures without providing a reason. Two of these five studies reported undertaking an intention-to-treat analysis for at least one primary or secondary outcome (Davidson 2009; Huband 2007) and three provided analysis only for those participants classed by the investigators as ‘completers’ (Messina 2003; Neufeld 2008; Woodall 2007).
Without data (six studies)
We classed all six studies as ‘unclear’ because it was not possible, in the absence of data from the subgroup with antisocial or dissocial PD, to judge the extent and nature of any missing data, and whether the reasons for such missing data balance across intervention groups.
The overall proportion of missing data (treatment and control conditions combined) varied significantly between studies. Missing data rates for the five studies with data were calculated as number with endpoint scores in comparison with number randomised and ranged from 8.3% to 29.2% (mean 18.0%; SD 7.8%; median 17.3%). Mean rates by type of intervention, calculated similarly, were as follows: CBT 18.2% (two studies); contingency management plus standard maintenance 13.0% (two studies); social problem-solving therapy with psychoeducation 29.2% (one study); DWI program with incarceration 17.3% (one study). These percentages should be regarded with caution for studies where the sample size is small.
Selective reporting
With data (five studies)
We judged that all five studies appeared to have reported on all the measures they set out to use and at all time scales in as far as could be discerned from the published reports without access to the original protocols.
Without data (six studies)
We classified all six studies as ‘unclear’ because it was not possible, in the absence of data from the subgroup with antisocial or dissocial PD, to judge whether there was selective reporting of any relevant data.
Other potential sources of bias
With data (five studies)
Messina 2003 report providing a reduction of $40 per month (representing a discount of between 22% and 29%) in the cost of methadone maintenance treatment as an incentive for participation in the study. Review authors classed this as ‘unclear’ because of uncertainty whether this could have introduced bias. We judged the remaining four studies free of other potential sources of bias.
Without data (six studies)
We classed Marlowe 2007 as ‘unclear’ because of uncertainty about possible risk of bias from diagnosis of AsPD using an ‘antisocial personality disorder interview’ derived from SCID-II by the trial investigators but with no information on its validation. Havens 2007 was classed as ‘unclear’ because, as the trial investigators acknowledged, selection bias may have been present because only those completing the one-month follow up were eligible for psychiatric assessment and participants in the case management arm were significantly less likely to have been followed up. We judged the remaining four studies free of other potential sources of bias.
Effects of interventions
Comparison 1. Contingency management + standard maintenance versus standard maintenance alone
Two studies were included in this comparison: Neufeld 2008 (outpatients with AsPD and opioid dependence; six months treatment; n = 100) and Messina 2003 (outpatients with cocaine dependence; AsPD subgroup; 16 weeks treatment; n = 26).
1.1 Social functioning
Neufeld 2008 report data indicating a statistically significant difference between treatment and control conditions in (adjusted) composite family/social domain scores via the Addiction Severity Index at six months favouring treatment (MD −0.08; 95% CI −0.14 to −0.02, P = 0.005, Analysis 1.3). This analysis is based on summary data of completers supplied by the trial investigators and derived from a mixed regression model that included time-specific random effects and an interaction term (see Table 1).
1.2 Leaving the study early
Both Neufeld 2008 and Messina 2003 provide data on leaving the study early. Meta-analysis of data from these two studies indicates no statistically significant difference between treatment and control conditions (OR 0.59; 95% CI 0.28 to 1.24, P = 0.16, I2 = 0%; P value for heterogeneity 0.69, Analysis 1.2).
1.3 Substance misuse (drugs)
Messina 2003 report data indicating a statistically significant difference between treatment and the control condition in numbers with cocaine-negative specimens by week 17 (OR 8.56; 95% CI 1.33 to 54.95, P = 0.02, Analysis 1.4), by week 26 (OR 11.67; 95% CI 1.53 to 89.12, P = 0.01, Analysis 1.5), and by week 52 (OR 10.00; 95% CI 1.44 to 69.26, P = 0.02, Analysis 1.6), favouring treatment in each case. Messina 2003 also report skewed summary data (see Table 2) indicating a statistically significant greater mean number of cocaine-negative specimens for the treatment compared to the control condition by 16 weeks (P < 0.05; two-way ANOVA with Tukey-Kramer post-hoc test; analysis of completers by the trial investigators). The trial investigators conclude that “ … patients with AsPD were more likely to abstain from cocaine use during treatment than patients without AsPD. The strong treatment effect for AsPD patients was primarily due to the contingency management condition. Regression analyses showed that AsPD remained significantly related to contingency management treatment responsivity while controlling for other factors”. (Abstract, p.320, Messina 2003). Neufeld 2008 report data indicating no statistically significant difference between treatment and control conditions in (adjusted) mean composite drug domain scores via the Addiction Severity Index at six months (data presented graphically; hierarchical regression model with variables at one, two, three and six months including condition, time, time-by-condition interaction and polydrug use at baseline; analysis of completers by the trial investigators, see Table 1). Neufeld 2008 also report summary data (see Table 3) indicating no statistically significant difference between treatment and control conditions at six months for overall percentage of opioid-negative urine specimens (OR 1.31; 95% CI 0.71 to 2.42, P = 0.39), of cocaine-negative urine specimens (OR 1.59; 95% CI 0.86 to 2.96, P = 0.14), of sedative-negative urine specimens (OR 1.82; 95% CI 0.72 to 4.42, P = 0.18) and of negative urine specimens for any drug (OR 1.70; 95% CI 0.94 to 3.07, P = 0.08), each being an analysis of completers carried out by the trial investigators.
1.4 Substance misuse (alcohol)
Neufeld 2008 report data indicating no statistically significant difference between treatment and control conditions in (adjusted) mean composite alcohol domain scores via the Addiction Severity Index at six months (data presented graphically; hierarchical regression model with variables at one, two, three and six months including condition, time, time-by-condition interaction and polydrug use at baseline; analysis of completers by the trial investigators, see Table 1).
1.5 Employment status
Neufeld 2008 report data indicating no statistically significant difference between treatment and control conditions in (adjusted) mean composite employment domain scores via the Addiction Severity Index at six months (data presented graphically; hierarchical regression model with variables at one, two, three and six months including condition, time, time-by-condition interaction and polydrug use at baseline; analysis of completers by the trial investigators, see Table 1).
1.6 Other outcomes
Neufeld 2008 report summary data (see Table 4) indicating a greater, statistically significant, overall number of counselling sessions attended in proportion to the total number of sessions offered for treatment compared to the control condition by six months (OR 4.00, 95% CI 2.39 to 6.70, P < 0.0001; analysis of completers by the trial investigators). The trial investigators concluded that “subjects in the experimental group had significantly better counselling attendance … compared to the control group. The experimental intervention increased attendance in subjects with low and high levels of psychopathy and with and without other psychiatric co-morbidity.” (Abstract, p.101, Neufeld 2008).
Neufeld 2008 report data indicating no statistically significant difference between treatment and control conditions in the proportion of participants transferred due to poor or partial treatment response by six months (OR 0.42; 95% CI 0.17 to 1.04, P = 0.04, Analysis 1.1).
Comparison 2. CBT + standard maintenance versus standard maintenance alone
Two studies were included in this comparison: Messina 2003 (outpatients with cocaine dependence; AsPD subgroup; 16 weeks treatment; n = 27) and Woody 1985 (male outpatients with opioid dependence; 24 weeks treatment; n = 50; no data available for control condition for the AsPD subgroup).
2.1 Leaving the study early
Messina 2003 report data indicating no statistically significant difference between treatment and control conditions for leaving the study early (OR 0.38; 95% CI 0.03 to 4.87, P = 0.46, Analysis 4.1). Woody 1985 provide data on leaving the study early, but with no data for the AsPD subgroup.
2.2 Substance misuse (drugs)
Messina 2003 report data indicating no statistically significant difference between treatment and control conditions in numbers with cocaine-negative specimens by week 17 (OR 2.72; 95% CI 0.48 to 15.47, P = 0.26, Analysis 4.2) and by week 26 (OR 5.60; 95% CI 0.81 to 38.51, P = 0.08, Analysis 4.3).
However, Messina 2003 also report data indicating a statistically significant difference between treatment and control conditions in numbers with cocaine-negative specimens by week 52 (OR 8.00; 95% CI 1.13 to 56.79, P = 0.04, Analysis 4.4), favouring treatment, plus skewed summary data (see Table 5) indicating a statistically significant difference in mean number of cocaine-negative specimens between treatment and control conditions by 16 weeks (P < 0.05; two-way ANOVA with Tukey-Kramer post-hoc test; analysis of completers by the trial investigators), again favouring treatment.
Woody 1985 provide data on drug domain scores via the Addiction Severity Index, but with no data for the AsPD subgroup.
2.3 Other outcomes
Woody 1985 provide data on psychiatric symptoms via scores on the SCL-90 and on depression via scores on the Beck Depression Inventory, but with no data for the AsPD subgroup.
Comparison 3. Contingency management + CBT + standard maintenance versus standard maintenance alone
One study was included in this comparison: Messina 2003 (outpatients with cocaine dependence; AsPD subgroup; 16 weeks treatment; n = 19).
3.1 Leaving the study early
Messina 2003 report data indicating no statistically significant difference between treatment and control conditions in leaving the study early (OR 0.28; 95% CI 0.01 to 6.72, P = 0.43, Analysis 5.1).
3.2 Substance misuse (drugs)
Messina 2003 report data indicating no statistically significant difference between treatment and control conditions in numbers with cocaine-negative specimens by week 17 (OR 3.11; 95% CI 0.41 to 23.39, P = 0.27, Analysis 5.2) and by week 26 (OR 7.00; 95% CI 0.69 to 70.74, P = 0.10, Analysis 5.3).
However, Messina 2003 also report data indicating a statistically significant difference between treatment and control conditions in numbers with cocaine-negative specimens by week 52 (OR 16.00; 95% CI 1.09 to 234.25, P = 0.04, Analysis 5.4), favouring treatment, plus skewed summary data (see Table 6) indicating a statistically significant difference in mean number of cocaine-negative specimens between treatment and control conditions by 16 weeks, again favouring treatment (P < 0.05; two-way ANOVA with Tukey-Kramer post-hoc test; completer analysis by the trial investigators).
Comparison 4. CBT + treatment as usual versus treatment as usual
Two studies were included in this comparison: Davidson 2009 (male outpatients with AsPD and recent verbal/physical violence; six and 12 months treatment; n = 52) and Tyrer 2004 (outpatients with recurrent self-harm; dissocial PD subgroup; up to seven treatment sessions; n = 15; no data available).
4.1 Aggression
Davidson 2009 report data indicating no statistically significant difference between treatment and control conditions at 12 months in number reporting any act of verbal aggression (OR 1.25; 95% CI 0.40 to 3.94, P = 0.70, Analysis 2.2) or of physical aggression (OR 0.92; 95% CI 0.28 to 3.07, P = 0.90, Analysis 2.4).
Davidson 2009 report data indicating no statistically significant difference between treatment and control conditions from baseline to endpoint at 12 months in the change (reduction) in number reporting any act of verbal aggression (OR 0.94; 95% CI 0.29 to 3.00, P = 0.92, Analysis 2.3) or of physical aggression (OR 1.20; 95% CI 0.40 to 3.62, P = 0.75, Analysis 2.5). The trial investigators observed, however, that “incidents of any acts of verbal or physical aggression decreased in both groups over the year of the study”. (p.574).
4.2 Social functioning
Davidson 2009 report data indicating no statistically significant difference between treatment and control conditions in mean Social Functioning Questionnaire (SFQ) scores at 12 months (MD −1.60; 95% CI −5.21 to 2.01, P = 0.39, Analysis 2.6).
4.3 Satisfaction with treatment
Davidson 2009 report data indicating no statistically significant difference between treatment and control conditions in mean scores for satisfaction with taking part in the study (MD 0.70; 95% CI −0.22 to 1.62, P = 0.14, Analysis 2.1).
4.4 Leaving the study early
Davidson 2009 report data indicating no statistically significant difference between treatment and control conditions for leaving the study early by three months (OR 0.63; 95% CI 0.19 to 2.13, P = 0.46, Analysis 2.7), by six months (OR 0.96; 95% CI 0.31 to 2.96, P = 0.94, Analysis 2.8), by nine months (OR 1.84; 95% CI 0.61 to 5.57, P = 0.28, Analysis 2.9), or by 12 months (OR 0.88; 95% CI 0.23 to 3.33, P = 0.84, Analysis 2.10).
4.5 Substance misuse (alcohol)
Davidson 2009 report skewed summary data (see Table 7) indicating no statistically significant difference between treatment and control conditions at 12 months for mean AUDIT overall scores (P = 0.08; mean difference in change from baseline 4.1, 95% CI −0.6 to 8.9; LOCF by the trial investigators) and for mean AUDIT total unit scores at 12 months (P = 0.88; mean difference in change from baseline 0.6, 95% CI −7.6 to 8.8; intention-to treat-analysis by the trial investigators in each case).
4.6 Economic outcomes
Davidson 2009 provide data on the total cost of health, social work and criminal justice services received over 12 months, and the average cost per participant for NHS services alone over 12 months (see Table 8) but with no statistics. Tyrer 2004 provide the total costs per patient over one year for the whole sample, but with no data for the dissocial PD subgroup.
4.7 Anger
Davidson 2009 report data indicating no statistically significant difference between treatment and control conditions at 12 months in mean Novaco Anger Scale scores (MD −1.30; 95% CI −13.97 to 11.37, P = 0.84, Analysis 2.11) or in mean Novaco Provocation Inventory scores (MD −2.60; 95% CI −11.51 to 6.31, P = 0.57, Analysis 2.12).
4.8 Other outcomes
Davidson 2009 report data indicating no statistically significant difference between treatment and control conditions at 12 months in mean HADS anxiety scores (MD −0.30; 95% CI −2.70 to 2.10, P = 0.81, Analysis 2.13) or in mean Hospital Anxiety and Depression Rating Scale (HADS) depression scores (MD −1.30; 95% CI −4.38 to 1.78, P = 0.41, Analysis 2.14).
Davidson 2009 report skewed summary data (see Table 9) indicating no statistically significant difference between treatment and control conditions for mean BCSS (Brief Core Schema Scales) scores at 12 months on the self-as-positive subscale (P = 0.89; mean difference in change from baseline −0.2, 95% CI −3.6 to 3.1), the self-as-negative subscale (P = 0.64; mean difference in change from baseline −0.8, 95% CI −4.3 to 2.7), the others-as-positive subscale (P = 0.10; mean difference in change from baseline −2.6, 95% CI −5.8 to 0.5) and the others-as-negative subscale (P = 0.15; mean difference in change from baseline −2.4, 95% CI −5.8 to 0.9; intention-to treat-analysis by the trial investigators in each case). Tyrer 2004 provide data on number of completed suicides for the whole sample and on frequency of self-harm episodes via the Parasuicide History Interview, but with no data for the dissocial PD subgroup. The trial investigators conclude for the sample as a whole ‘Although the results showed no significant difference between those repeating self-harm in the manual-assisted CBT group (39%) compared with the TAU group (46%) (P = 0.20), the treatment was cost-effective [10% cheaper than TAU] and the frequency of self-harm episodes was fewer [50%] in the manual-assisted CBT group.’ (Abstract, p.102).
Comparison 5. Social problem-solving therapy with psychoeducation versus treatment as usual
One study was included in this comparison: Huband 2007 (community living adults with personality disorder; AsPD subgroup; 24 weeks treatment; n = 24). The trial investigators, while providing data on the AsPD subgroup, noted that their trial was not designed to have sufficient power to detect significant change in subgroups of this size, and also that 20 of the 24 had at least one other Axis II diagnosis.
5.1 Social functioning
Huband 2007 report data indicating no statistically significant difference between treatment and control conditions in mean Social Functioning Questionnaire scores at six months (MD −1.60; 95% CI −5.43 to 2.23, P = 0.41, Analysis 3.1).
5.2 Leaving the study early
Huband 2007 report data indicating no statistically significant difference between treatment and control conditions for leaving the study early (OR 1.19; 95% CI 0.20 to 6.99, P = 0.85, Analysis 3.7).
5.3 Impulsivity
Huband 2007 report data indicating no statistically significant difference between treatment and control conditions in mean Barrett Impulsiveness Scale scores at six months (MD 6.58; 95% CI −4.81 to 17.97, P = 0.26, Analysis 3.4).
5.4 Anger
Huband 2007 report data indicating no statistically significant difference between treatment and control conditions in mean anger expression index scores on the State-Trait Anger Expression Inventory at six months (MD −1.74; 95% CI −12.64 to 9.16, P = 0.75, Analysis 3.3).
5.5 Other outcomes
Huband 2007 report data indicating no statistically significant difference between treatment and control conditions at six months in mean SPSI social problem-solving ability scores (MD 0.18; 95% CI −2.57 to 2.93, P = 0.90, Analysis 3.2), in mean ESS shame scores at six months (MD 14.64; 95% CI −12.70 to 41.98, P = 0.29, Analysis 3.5) and in mean DES dissociation scores at six months (MD 4.30; 95% CI −21.19 to 29.79, P = 0.74, Analysis 3.6).
Comparison 6. ‘Driving Whilst Intoxicated program’ + incarceration versus treatment as usual (incarceration alone)
One study was included in this comparison: Woodall 2007 (incarcerated drink-driving offenders with AsPD; 28 days treatment; n = 52).
6.1 Reconviction
Woodall 2007 report data indicating no statistically significant difference between treatment and control conditions in reconviction for drink-driving (Cox regression of re-arrest rates) over 24 months (HR 0.56; 95% CI −0.19 to 1.31, P = 0.15, Analysis 6.1). The trial investigators concluded that “although non-significant, AsPD participants in the treatment group were considerably less likely to be re-arrested for DWI than AsPD participants in the control group” (p.985, col 1).
6.2 Substance misuse (alcohol)
Woodall 2007 provide descriptive and graphical summaries (p.983, col 1) of analyses of self-reported alcohol use using the Form90 measure. These showed a statistically significant difference between treatment and control conditions (group × AsPD × time interaction) over the 24-month period for both total standard ethyl-alcohol consumption units and number of drinking days, favouring treatment in each case (P < 0.05; omnibus test; repeated measures ANOVA, mixed factorial design with Geisser-Greenhouse adjustment; analysis of completers by the trial investigators). A similar analysis for average blood alcohol content did not indicate statistically significant differences (P = 0.052).
The trial investigators concluded that “participants randomized to receive the first offender incarceration and treatment [DWI] program reported greater reductions in alcohol consumption from baseline levels when compared with participants who were only incarcerated. AsPD participants reported heavier and more frequent drinking but showed significantly greater decline in drinking from intake to post-treatment assessments.” (Abstract, p.974, Woodall 2007).
6.3 Other outcomes
Woodall 2007 report skewed summary data indicating no statistically significant difference between treatment and control conditions for mean number of days driving after drinking in past 30 days (see Table 10) and for mean number of days driving after five or more drinks in past 30 days (see Table 11) at six, 12 and 24 months post incarceration (P values not provided, but not significant for the group-by-time interaction; ANOVA mixed factorial design; completer analysis by the trial investigators). However, the trial investigators report a significant overall main effect of time for the whole sample (P < 0.001), “indicating a decline in self-reported drinking and driving from intake to post-incarceration assessments” (p.982, col 2) and a “significant AsPD-by-time interaction (P < 0.001) resulting from the fact that, contrary to expectations, the AsPD participants showed a greater improvement over time than the non-AsPD participants on both these self-reports of drinking and driving.” (p.982, col 2).
Comparison 7. Optimal judicial supervision versus treatment as usual (standard judicial supervision)
One study was included in this comparison: Marlowe 2007 (adults drug offenders supervised by pre-adjudication court; AsPD subgroup; average nine months treatment; n = unknown; no data available). This study compares optimal (‘matched’) judicial supervision with standard judicial supervision (treatment as usual) in adult drug court offenders. Trial investigators used diagnosis of AsPD as one criterion for assignment to high (rather than low) risk category, but no data was available for the AsPD subgroup. Marlowe 2007 provide data on reconviction (to 24 months post-admission), substance misuse (drugs) (self-report via the Addiction Severity Index, and drug screen by urinalysis), leaving the study early and adverse events (descriptively only; “no study-related adverse event was reported to date” (p.56, col 1)), but with no data for the AsPD subgroup.
The trial investigators conclude …“high risk participants graduated [from the program] at a higher rate, provided more drug-negative urine specimens at 6 months post-admission, and reported significantly less drug use and alcohol intoxication at 6 months post-admission when they were matched to bi-weekly hearings [i.e. optimal judicial supervision] as compared to the usual schedule of hearings [i.e. standard judicial supervision].” (Abstract, p.S4, Marlowe 2007).
Comparison 8. Supportive-expressive psychotherapy + standard maintenance versus standard maintenance alone
One study was included in this comparison: Woody 1985 (male outpatients with opioid dependence; AsPD subgroup; 24 weeks treatment; n = 50; no data available). The trial investigators report on AsPD subgroup with data for the experimental condition, but not for control condition for the AsPD subgroup. Woody 1985 provide data on leaving the study early, substance misuse (drugs) (self-report via the Addiction Severity Index), psychiatric symptoms (scores on the SCL90), and depression (scores on the BDI), but with no data for the AsPD subgroup in the control condition. Trial investigators conclude “Those with opiate dependence plus AsPD alone improved only on ratings of drug use. Patients with opiate dependence alone or with opiate dependence plus depression improved significantly and in many areas. Opiate-dependent patients with AsPD plus depression responded almost as well as those with only depression. AsPD alone is a negative predictor of psychotherapy outcome, but the presence of depression appears to be a condition that allows the patient to be amenable to psychotherapy, even though the behavioural manifestations of sociopathy are present.” (Abstract, p.1081, Woody 1985).
Comparison 9. Dual-focus schema therapy versus treatment as usual
One study was included in this comparison: Ball 2005 (homeless adults with substance abuse; AsPD subgroup; 24 weeks treatment; n = 24; no data available). This study describes an RCT comparing dual-focus schema therapy with treatment as usual (TAU) in homeless substance abusers.
Ball 2005 provide data on leaving the study early, therapy retention (as total weeks in treatment), therapy utilisation (number weeks in which sessions attended), psychiatric symptoms (via the Brief Symptom Inventory (BSI)), early maladaptive schemas (scores on the Early Maladaptive Schema Questionnaire-Research (EMSQ-R)), interpersonal problems (scores on the Inventory of Interpersonal Problems (IIP)) and social/family functioning (via the Addiction Severity Index (ASI)) for the whole sample, but with no data for the AsPD subgroup.
Trial investigators concluded “Overall, there was greater utilization of individual dual-focus schema therapy than standard group substance abuse counselling [i.e. treatment as usual]. However, clients with more severe personality disorder symptoms demonstrated better utilization of standard group substance abuse counselling than dual-focus schema therapy.” (Abstract, p.371, Ball 2005).
Comparison 10. Case management versus treatment as usual (passive referral)
One study was included in this comparison: Havens 2007 (intravenous drug-using outpatients; AsPD subgroup; four weeks treatment; n = unknown; no data available). This study describes a cluster RCT and compares participants with and without AsPD. Havens 2007 provide data on engagement with services (as entry into treatment) for the whole sample, but with no data for the AsPD subgroup.
The trial investigators concluded for the whole sample “In a multivariate intention-to-treat model (i.e. ignoring the amount of case management actually received), those randomised to case management were more likely to enter treatment within 7 days. Additional ‘as treated’ analyses revealed that participants who received 30 min or more of case management within 7 days were 33% more likely to enter treatment and the active ingredient of case management was provision of transportation.” (Abstract, p. 225, Strathdee 2006).
Additionally, investigators concluded “Compared to those without AsPD, intravenous drug users with comorbid AsPD who spent 25 or more minutes with their case manager prior to their treatment entry date were 3.51 times more likely to enter treatment than those receiving less than 5 minutes, adjusting for interventions status, race, and treatment site (98% confidence interval 1.04 to 11.89). Providing case management services to intravenous drug users with comorbid AsPD may facilitate treatment entry and reduce negative consequences of drug abuse.” (Abstract, p.267, Havens 2007).
Comparison 11. Individualised relapse prevention versus treatment as usual (standard continuing care treatment)
One study was included in this comparison: McKay 2000 (male outpatients with cocaine dependence; AsPD subgroup; 20 weeks treatment; n = 46; no data available). McKay 2000 provide data on substance misuse (self-report via the Addiction Severity Index (ASI) and the Cocaine Relapse Interview, and drug screen by urinalysis) for the whole sample, but with no data for the AsPD subgroup.
The trial investigators concluded that “a diagnosis of AsPD was not a predictor of differential response to the two continuing care interventions in the study. However, AsPD patients had worse medical and psychiatric problem severity than non-AsPD patients at entrance to continuing care and during follow-up. These results suggest that cocaine patients with AsPD who are in the continuing care phase of outpatient rehabilitation might benefit from additional medical and psychiatric treatment services.” (Abstract, p.287, McKay 2000).
DISCUSSION
As described in the introduction, antisocial personality disorder (AsPD) is a prevalent condition associated with considerable personal and societal adverse consequences. It also has major negative economic consequences as it is associated with poor occupational productivity and increased criminal justice costs. Consequently, one might expect that the identification of interventions that might reduce this impact would be a research priority. Unfortunately, the conclusion of this review is similar to many that preceded it in that there is little good quality evidence as to what might (or might not) be effective for this condition. As only 11 studies could be included in the review, the first point to make therefore is how few studies there were to consider.
The second refers to the design and methodological quality of the few studies that could be included. Disappointingly few of the included studies addressed the primary outcomes defined in this review. While the underlying personality structure of AsPD comprises dissociate traits such as impulsivity, lack of remorse and irritability, its most common behavioural manifestation is persistent rule-breaking. Although the focus on behaviour, rather than on the underlying personality structure, has been frowned upon by some commentators (e.g. Livesley 2007), we argue that persistent rule-breaking is akin to a final common pathway manifestation of the underlying personality structure. If one accepts this argument, it is disappointing that only two of the included studies (Marlowe 2007; Woodall 2007) had reconviction as their primary outcome. Another (Davidson 2009) used self-reported aggression. In the light of the important adverse cost consequences of the condition and likely need for complex and expensive interventions, it was also disappointing that only two studies (Davidson 2009; Tyrer 2004) considered the economic impact of their intervention.
Furthermore, the majority of the included studies were trials to reduce substance misuse. As many within the sample of substance misusers also satisfied criteria for AsPD, there was an opportunity to report on these separately. Hence, strictly speaking, these were not interventions for AsPD; rather, they were interventions to reduce substance misuse in a sample, some of whom also satisfied criteria for AsPD. While these studies were not without their limitations, there is evidence that contingency management is effective in reducing substance misuse in this population. While this finding is similar to the recent NICE guidance on opioid detoxification (NIHCE 2007) in general, it suggests that this principle of intervention is also effective in those with AsPD.
Summary of main results
A proportion of the quantitative data available from the studies included in this review met our criteria for skewed data as described in the section on Measures of treatment effect. Consequently, in the absence of raw data from the trial investigators, we have presented all skewed data as Additional tables and have reported statistics on comparisons between conditions as calculated by the trial investigators rather than performing our own analysis. We did not carry out any synthesis of primary or secondary outcome data via meta-analysis (other than for the outcome of leaving the study early) because (a) data for an outcome was available from only one study, or (b) we wanted to minimise the risk of applying parametric statistics to skewed data that was not normally distributed. The summaries that follow below are therefore essentially descriptive. The focus of this review is relatively broad since it seeks evidence on effectiveness of any psychological intervention in the treatment of antisocial or dissocial personality disorder. We found considerable differences between the studies in terms of participants, size of sample, intervention modality and choice of outcome measures.
We found only three interventions (contingency management with standard maintenance; CBT with standard maintenance; ‘Driving Whilst Intoxicated program’ with incarceration) which were effective, compared to the control condition, in terms of improvement in at least one outcome in at least one study. Each of these interventions had been developed for people with substance misuse problems. No study reported significant change in any specific antisocial behaviour, such as offending, aggression or impulsivity.
Contingency management + standard maintenance was superior to standard maintenance alone on family/social domain scores on the Addiction Severity Index in outpatients with opioid dependence (Neufeld 2008) at end of treatment at six months.
Contingency management + standard maintenance was superior to standard maintenance alone on numbers with cocaine-negative urine specimens in outpatients with cocaine dependence (Messina 2003) at end of treatment at 16 weeks, and also at weeks 17, 26 and 52 of follow up.
Contingency management + standard maintenance was superior to standard maintenance alone on proportion of counselling sessions attended in outpatients with opioid dependence (Neufeld 2008) at end of treatment at six months.
CBT + standard maintenance was superior to standard maintenance alone on numbers with cocaine-negative urine specimens in outpatients with cocaine dependence (Messina 2003) at end of treatment at 16 weeks, and also at week 52 of follow up.
Contingency management + CBT + standard maintenance was superior to standard maintenance alone on numbers with cocaine-negative urine specimens in outpatients with cocaine dependence (Messina 2003) at end of treatment at 16 weeks, and also at weeks 17, 26 and 52 of follow up.
‘Driving Whilst Intoxicated program’ + incarceration was superior to treatment as usual (incarceration alone) on number of drinking days and on total standard ethyl-alcohol consumption units in prisoners sentenced for driving whilst intoxicated (Woodall 2007) at 24 months.
For the ‘contingency management’ intervention, two studies produced contrasting results in terms of drug misuse (Messina 2003 and Neufeld 2008). The Addiction Severity Index (ASI) results in Section 1.10 a: Substance misuse (drugs) and in Section 1.10b: Substance misuse (alcohol) favoured the intervention over control in the Messina 2003 study but not the Neufeld 2008 study. However, contingency management was superior in terms of social functioning and counselling session attendance in Neufeld 2008. These differences may have arisen because of differences in the nature of the behavioural intervention. Both studies describe ‘contingency management’, but the positive reinforcements available in the Messina study for participants who stayed drug-free seem considerably more attractive. For example, a participant in the Messina study who managed to stay drug-free for the whole 16 weeks of the trial could earn redeemable vouchers worth a total of $1277. In contrast, the positive reinforcement in the Neufeld 2008 trial comprised greater control over methadone clinic attendance and dosage in reward for drug abstinence and attendance at counselling sessions.
A note on the five excluded trials that compared one psychological intervention against another
We excluded five studies (described in seven separate reports) that compared one psychological treatment against another because there was no control condition that could be regarded as treatment as usual, waiting list or no treatment. Although none of these five studies focused exclusively on AsPD, and none provided data on their AsPD subgroup, each reported information that we consider to be of interest to a clinician seeking treatment options for this client group. Because of this, we now summarise briefly the characteristics of each of these five studies and the conclusions drawn by the trial investigators.
-
Ball 2007 conducted a randomised trial comparing dual-focus schema therapy (DFST) with 12-step facilitation therapy (12FT) in 30 opioid-dependent outpatients who were receiving methadone maintenance. The investigators note that DFST focuses on achievable goals such as improving self-esteem, relationships and exposure to substance abuse, but does seek to achieve full remission. Both therapies were manual-guided and were delivered for six months. All participants had at least one DSM-IV personality disorder diagnosed using the SCID-II.
AsPD was the most common diagnosis (n = 19) followed by borderline, avoidant and dependant personality disorder (PD), although the trial investigators did not report results from the AsPD subgroup separately. For the whole sample, the investigators report no significant differences between the two therapies on retention, utilisation or reduction in psychiatric symptoms or psychosocial impairment. However, participants allocated to DFST showed more rapid decrease in the frequency of substance use over six months in comparison with those allocated to 12FT. DFST was also associated with a stronger therapeutic alliance between therapists and participants, whereas 12FT showed a better reduction of dysphoric affect.
Easton 2007 describe a study aggregating results of two controlled trials: Carroll 2004 in outpatients with cocaine dependence, and Carroll 1998 in outpatients with cocaine and alcohol dependence. The first trial (Carroll 2004) randomised to four conditions to allow comparison between CBT and interpersonal therapy (IPT), both with and without disulfiram. The other trial (Carroll 1998) involved five conditions: CBT plus disulfiram, 12-step facilitation plus disulfiram, supportive psychotherapy plus disulfiram, CBT plus no medication and 12-step facilitation plus no medication. Treatment duration was 12 weeks in each case. Both trials had a subgroup with AsPD (pooled n = 79), although neither study nor Easton 2007 analyse results from the AsPD subgroup separately. Carroll 2004 report that, for their whole sample (of which 41% had AsPD), those allocated to CBT reduced their cocaine use significantly more than those allocated to IPT. Carroll 1998 report that, for their whole sample (of which 25% had AsPD), those allocated to CBT and 12-step facilitation significantly reduced their cocaine use over time compared with the supportive psychotherapy condition. Taking the results of the two trials together, there were no significant differences between participants with and without criminal justice involvement in frequency of substance use during treatment or the one-year follow up (Easton 2007).
Longabaugh 1994 conducted a randomised trial comparing CBT with relationship enhancement therapy for 229 outpatients with alcohol abuse problems. Treatment was for 20 sessions in each case and was completed in four to six months. A subgroup (n = 48) met criteria for DSM-III AsPD via the Diagnostic Interview Schedule, of which 31 were used in the investigators’ analysis. At 13 to 18 months following start of treatment, the investigators report that participants with AsPD averaged more abstinent days than those without AsPD. In addition, participants with AsPD who were allocated to CBT drank less per drinking day than did either those without AsPD who were allocated to CBT or those with AsPD allocated to relationship enhancement therapy. The investigators conclude that, irrespective of drinking index, participants with AsPD responded poorly with high post-treatment support for abstinence, whereas those without AsPD responded better with support.
Vinnars 2005 compared manualised supportive-expressive dynamic psychotherapy with non-manualised community-delivered dynamic psychotherapy for 156 outpatients with any DSM-IV personality disorder, assessed using the SCID-II. A small subgroup (n = 12) met criteria for AsPD, although the investigators did not analyse these data separately. For the whole sample, investigators report global level of functioning as improved in both treatment conditions. They also report decreases in number of participants fulfilling criteria for a PD diagnosis, PD severity, and psychiatric symptoms, but with no significant difference in effect between treatments. The investigators conclude that manualised supportive-expressive psychotherapy was as effective as non-manualised community-delivered psychodynamic therapy conducted by experienced clinicians. Vinnars 2007 and Vinnars 2009 report further analysis of data from the same trial, exploring significant predictors of reduction in psychiatric symptoms and in personality pathology. No additional information on the small AsPD subgroup is provided. For the whole sample, the investigators found both treatments equally effective at reducing personality pathology and the largest improvement was found in quality of object relations.
Findings from these five excluded trials (importantly, with no specific data from the AsPD subgroup), suggest that CBT may be more effective than interpersonal therapy, and dual-focus schema therapy may be more effective than 12-step facilitation therapy for those with opioid dependency, and also that CBT may be more effective than relationship enhancement therapy for those with alcohol dependency.
Overall completeness and applicability of evidence
The evidence obtained from the included studies is relevant to the review question, but is incomplete for the following reasons:
Although 11 different psychological interventions were compared, none of the studies evaluated psychodynamic psychotherapy, therapeutic community treatment, dialectical behaviour therapy, cognitive analytic therapy, mentalisation-based therapy or nidotherapy.
The majority of studies did not primarily focus on the treatment of antisocial personality disorder, and in only two recruited samples did all participants have this diagnosis.
Eight studies focused on participants with substance misuse difficulties. Although drug/alcohol misuse is often relevant to people with AsPD, having a substance abuse problem is not part of the diagnostic criteria for AsPD.
The findings in two studies may not fully generalise to the population of interest: the sample in Woodall 2007 was drawn mainly from a Native American community; Marlowe 2007 found that women were significantly over-represented in their sample, and that individuals with more severe drug problems and less severe criminal histories were significantly more likely to have participated.
Quality of the evidence
We identified 11 studies that met the criteria for inclusion in this review, involving a total of 411 participants with AsPD. Of these, only five provided usable data, involving 276 participants with AsPD. We judged the overall quality of the evidence from these trials to be relatively poor for the following reasons:
The review relies on data from only five of the 11 included studies, despite attempts to contact the trial investigators for information on the AsPD subgroups.
The study samples were heterogeneous; they encompassed, for example, both prisoners and outpatients. In addition, AsPD was diagnosed under three similar but not identical rubrics (DSM-III, DSM-III-R, and DSM-IV).
Where the completion rate was reported, it was high (mean 89.1%). This may be misleading because of the custodial element of some interventions. For example, Woodall 2007 had a 100% completion rate which might be expected given that one component of the intervention was incarceration.
There was inconsistency in the way primary and secondary outcomes were measured and reported.
The authors consider that the body of evidence summarised in this review is insufficient to allow any conclusion to be drawn about the use of psychological interventions in the treatment of antisocial personality disorder.
Potential biases in the review process
We were aware of a potential for bias that might be seen as arising because two of the review authors (CD and NH) were investigators in one of the studies included in this review (Huband 2007). We minimised this risk by ensuring that neither author took part in the extraction of data or in summarising the risk of bias for this trial. When it became necessary to request additional data from this study’s lead investigator, correspondence was handled via the Cochrane Developmental, Psychosocial and Learning Problems Group in Bristol. These requests were referred by NH to the trial’s research committee who responded via Cochrane in Bristol.
Agreements and disagreements with other studies or reviews
The most relevant recent review with which to compare our findings is that carried out in the development of the NICE clinical guideline on antisocial personality disorder (NIHCE 2009). In reporting their systematic review, the NICE guideline authors observed that there had been little formal development of psychological interventions specifically for the treatment of AsPD, whereas there had been “very considerable development of interventions aimed at reducing offending behaviour” (NIHCE 2009, section 7.2.1, p.191). In recognition of this, they chose to consider not only interventions which targeted AsPD itself, but also those which targeted the symptoms or behaviours associated with the diagnosis (such as anger, impulsivity and aggression) as well as interventions specifically for offenders regardless of diagnosis. The review described by NIHCE 2009 thus is much broader than our current review which focuses solely on studies of participants with a diagnosis of antisocial or dissocial PD.
Although the two reviews identified the same four studies targeting treatment of AsPD (Davidson 2009) and treatment of comorbid disorder in people with AsPD (Messina 2003; McKay 2000; Woody 1985), there were several differences.
The current review identified one study (Neufeld 2008) that was a later and more complete summary of the trial initially reported by Brooner 1998 which was included in the NICE review.
The current review identified two additional studies with data that were not included in the NICE review (Huband 2007; Woodall 2007).
NIHCE 2009 considered three additional studies that were excluded from the current review: Wolwer 2001 on cognitive behavioural therapy (CBT) versus coping skills training versus treatment as usual (TAU) in alcohol dependence, which we excluded because too few participants had AsPD; Hesselbrock 1991 on hospitalisation for alcohol dependence, which we excluded because it was not a randomised trial and had no control condition; and Vannoy 2004 on anger-management versus waiting list TAU in offenders, which we excluded because no participant had AsPD.
NIHCE 2009 additionally considered a further 21 studies of treatments for offending behaviour in young people (n = 11), in adults (n = 5) and in offenders with substance misuse problems (n = 5). These studies would not have been eligible for inclusion in the current review because the participants had no formal diagnosis of antisocial or dissocial PD.
In their conclusions, NIHCE 2009 considered that the evidence for the psychological treatment of antisocial personality disorder was limited to one community trial, that the quality of the evidence was low to moderate, and that the limited economic evidence from that trial suggested that CBT may not be cost-saving in the short term. They considered, however, that there was modest evidence for the effectiveness of cognitive and behavioural interventions, primarily delivered in groups, in reducing offending for adults with substance misuse problems, and that this effect has been found in variety of settings including institutional, outpatient and probation settings.
The current review concludes that good quality evidence favouring any psychological intervention for AsPD is virtually non-existent, but that contingency management appears to be effective for those that have AsPD comorbid with substance misuse difficulties.
AUTHORS’ CONCLUSIONS
Implications for practice
The results from this review are that there is insufficient trial evidence to justify using any psychological intervention for those with a diagnosis of AsPD. We acknowledge, however, that ‘absence of evidence is not evidence of absence of effect’ and that this is a group with complex needs that may present to healthcare professionals for help with their difficulties. Professionals will therefore have to rely on their clinical experience in responding, but recognise that good quality evidence supporting whatever intervention is chosen is virtually non-existent. Clinicians should also recognise the difficulty of retaining this group in treatment so that data showing that contingency management is effective for those with AsPD and substance misuse suggest that rewarding them may overcome their treatment-resistant characteristics.
Implications for research
Studies with positive findings reported here require replicating to confirm apparent efficacy. Given the very few studies that could be considered in this review, there is clearly an imperative to conduct well-designed trials using psychological approaches. Given the poor evidence base, we recognise that these initial trials are almost inevitably going to be of an active treatment against treatment as usual, rather than the more desirable investigation of one active treatment against another. A major problem in carrying out such a trial in the community is that this is a notoriously difficult group to retain in treatment, as they tend to be treatment-rejecting rather than treatment-seeking (NIHCE 2009). However, this caveat does not apply to those in prison where there is a large number of individuals incarcerated with AsPD. If this were the population chosen, then reconviction on release ought to be the outcome as this is, unfortunately, a relatively common outcome in many with AsPD with approximately two-thirds of those being released from prison reoffending within two years (Home Office 1999; ONS 2004). Hence we recommend that reconviction is chosen as the primary outcome in such a trial, preferably in conjunction with an economic evaluation. If there was a consensus on a single outcome measured across studies, then it would be possible to make cross study comparisons, a task that is difficult to perform at the moment because of the wide range of outcomes and outcome measures that are used.
PLAIN LANGUAGE SUMMARY.
Psychological treatments for people with antisocial personality disorder
Antisocial personality disorder is a condition that leads to persistent rule-breaking, criminality, and drug or alcohol misuse. It causes a great deal of hardship for the person concerned, as well as for the person’s immediate family and society in general. This review systematically examines the evidence for the effectiveness of psychological treatments used to help people with antisocial personality disorder.
We considered 11 studies, but were unable to draw any firm conclusions from the evidence available. Although several studies looked at treatments to reduce drug or alcohol misuse in people with antisocial personality disorder, few studies focused on treating the disorder itself. Only three studies reported outcome measures that were originally defined in the review protocol as being of particular importance in this disorder (reconviction and aggression). Nonetheless, there was some evidence that a type of treatment known as contingency management (which provides rewards for progress in treatment) could help people with antisocial personality disorder to reduce their misuse of drugs or alcohol.
Further research is urgently needed to clarify which psychological treatments are effective for people with this disorder. This research is best carried out using carefully designed clinical trials. Such trials should focus on the key features of antisocial personality disorder. To be informative, they need to be carried out with samples of participants of sufficient size.
ACKNOWLEDGEMENTS
We gratefully acknowledge: Jo Abbott (Cochrane Developmental, Psychosocial and Learning Problems Group) for running the electronic searches, Renate Reniers for translation of a paper from Dutch, and Cathy Bennett for advice and helpful comments on an early draft of this review.
SOURCES OF SUPPORT
Internal sources
Nottinghamshire Healthcare NHS Trust, UK.
German Federal Ministry of Education and Research, grant no. 01KG0812, Germany.
External sources
NHS Cochrane Collaboration Programme Grant Scheme, UK.
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: homeless adults with substance abuse difficulties and personality disorder Sex: (for whole sample; see note 1) 49/52 (94%) male; 3/52 (6%) female Age: (for whole sample; see note 1) mean 38.3 (SD 10.4) years; range 19 to 57 years Unit of allocation: individual participant Number randomised: 52 (for sample as a whole; no details for AsPD subgroup (see note 1) Number completing: no details for AsPD subgroup (see note 1) Setting: outpatient; single site; urban; USA (Manhattan) Inclusion criteria: at least 18 years old; alcohol or drug use in past 30 days; diagnosis of PD (DSM-IV; PDQ, see note 2); able to read and comprehend consents and assessments; willingness to be a research participant Exclusion criteria: acute schizophrenia; bipolar disorder; organic syndrome; acute violence or suicidality; incarceration pending; actively participating in counselling at another substance abuse or mental health clinic whilst in active treatment phase Ethnicity: (for whole sample; see note 1) white (23%); Hispanic (26%); African American (49%) Baseline characteristics: (for whole sample; see note 1) never married (58%); currently married (4%); separated/divorced (33%); high school education (67%); essentially unemployed for prior 3 years (26%); some full-time or part-time work in prior 3 years (49%); alcohol as primary misuse substance (50%); illicit drugs as primary misuse substance (50%); average age of diagnosis onset for alcohol abuse 23.5 (SD 7.8, median 22) years; average age of diagnosis onset for drug abuse 21.0 (SD 5.8, median 19) years; Cluster A PD diagnosis (88%); Cluster B PD diagnosis (74%); Cluster C PD diagnosis (85%); no period of stable living arrangements over last 3 years (27%) |
|
| Interventions | Two conditions: dual focus schema therapy/treatment as usual
Details of conditions: DFST is individual psychotherapy focused on PD and substance abuse relapse prevention. Is a 24-week manual-guided individual therapy that integrates symptom-focused relapse prevention coping skills techniques for interpersonal, affective and craving experiences, and schema-focused techniques for early maladaptive schemas and coping styles and is delivered weekly TAU is standard group substance abuse counselling as normally provided at the drop-in centre where clients are typically offered a total of 3 opportunities per week to attend group psychoeducation and counselling sessions Duration of intervention: 24 weeks Duration of trial: 9 months Length of follow up: 3 months following end of treatment (although investigators report ”successful follow up in the sample proved to be extraordinarily difficult to achieve”, p.374, col 1) |
|
| Outcomes |
Primary outcomes
Social functioning: mean scores on the Addiction Severity Index (ASI) social/family domain Secondary outcomes Leaving the study early: proportion of participants discontinuing treatment Other outcomes Therapy retention: total weeks in treatment Therapy utilisation: number weeks in which sessions attended Severity of PD: scores on the Personality Diagnostic Questionnaire (PDQ, see note 2) Psychiatric symptoms: mean scores on the Brief Symptom Inventory (BSI) Early maladaptive schemas: mean scores on the Early Maladaptive Schema Questionnaire - Research (EMSQ-R) Interpersonal problems: means scores on the Inventory of Interpersonal Problems (IIP) |
|
| Notes |
|
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Investigators report ”after completion of baseline assessments, subjects were randomly allocated to 1 of 2 study treatments” (p.374, col. 1) but no further details were reported. Clarification about method of sequence generation has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Allocation concealment? | Unclear | Insufficient information to allow a judgement to be made. Clarification about method of allocation concealment has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Blinding? of participants |
Unclear | In a study such as this full blinding is difficult to achieve because participants would be aware whether or not that they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants |
| Blinding? of personnel |
Unclear | In a study such as this full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study |
| Blinding? of outcome assessors |
Unclear | Insufficient information to allow a judgement to be made. Clarification about blinding of outcome assessors has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Incomplete outcome data addressed? All outcomes |
Unclear | The trial investigators note significant missing data for PDQ scores ”because of a major computer malfunction, the personality disorder profiles of 16 of the participants could not be recovered” (p. 373, col 1). Although review authors consider this could have introduced bias for one outcome (severity of PD), this was not one of the primary or secondary outcomes addressed in this review. Unclear whether there are missing outcome data for the AsPD subgroup and, if so, whether the numbers of and reasons for such missing data balance across intervention groups. Review authors unable to make a judgement unless data from AsPD subgroup become available |
| Free of selective reporting? | No | Investigators do not report endpoint or follow-up data for 3 outcomes, measured with the Early Maladaptive Schema Questionnaire, the Inventory of Interpersonal Problems and the Addiction Severity Index |
| Free of other bias? | Yes | The study appeared to be free of other sources of bias |
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: male outpatients with AsPD and recent verbal/physical violence Sex: all male Age: mean 37.9 (SD 10.4) years Unit of allocation: individual participant Number randomised: 52 (n = 25 CBT + TAU; n = 27 TAU only) Number completing: 41 (n = 20 CBT + TAU; n = 21 TAU only) at 12 months Setting: outpatient; multi-site (2 sites); urban; UK (Glasgow and London) Inclusion criteria: male; aged 18 to 65 years; diagnosis of AsPD (DSM-IV; SCID); living in community; endorsement of at least one item on MacArthur Community Violence Screening Instrument (MCVSI); interviewed in 6 months prior to baseline; able to provide written informed consent Exclusion criteria: currently receiving a systematic psychological therapy; insufficient knowledge of English to participate/understand; diagnosis of psychosis (schizophrenia or bipolar-affective disorder); currently receiving in-patient treatment (see note 1) Ethnicity: 35/52 (67%) white Baseline characteristics: 51/52 (98%) reported verbal aggression in previous six months; 45/52 (87%) reported physical aggression against others in previous 6 months; mean 4. 9 (SD 20.4) days in psychiatric hospital in previous 12 months; mean age at first contact with psychiatric services 19.8 (SD 12.5) years; mean age at first trouble with law 14.3 (SD 7.6) years; mean total Drug and Alcohol Screening Test (DAST) score 5.7 (SD 4.4); mean age at leaving school 15.6 (SD 1.4) years; mean number of months in work during last 5 years 16.5 (SD 22.9) months; 38/52 (73%) unemployed at entry into study; 37/52 (71%) assessed as at least below average literacy on Test of Word Reading Efficacy |
|
| Interventions | Two conditions: cognitive behavioural therapy plus treatment as usual/treatment as usual
Details of conditions: CBT intervention defined as ”structured, time-limited, psychosocial intervention developed to treat those with borderline and antisocial personality disorder within National Health Service settings”. Participants were encouraged to engage in treatment through a cognitive formulation of their problems. The therapy focuses on beliefs about self and others that impair social functioning. CBT was delivered by 7 therapists who had relevant experience and training and who were supported with weekly case supervision. Therapist adherence/competence was assessed for a random selection (30%) of sessions by audio recording and found to be ”within competent range”. In treatment as usual (TAU) ”All participants received whatever treatment they would have received had the trial not taken place” Duration of intervention: 6 months or 12 months (see note 2). Participants who were randomised to CBT+TAU were further randomly allocated to treatment over either 6 months as 15 × 1-hour sessions (n = 12) or 12 months as 30 × 1-hour sessions (n = 13) Duration of trial: 12 months (see note 2) Length of follow up: participants were not followed up beyond end of trial at 12 months |
|
| Outcomes |
Primary outcomes
Aggression: number reporting incidents of physical aggression; number reporting incidents of verbal aggression Social functioning: mean scores on Social Functioning Questionnaire (SFQ) Secondary outcomes Leaving the study early: proportion of participants discontinuing treatment Anger: mean scores on Novaco Anger Scale and Provocation Inventory (NAS-PI) Satisfaction with treatment: satisfaction with taking part in study (via questionnaire) Substance misuse (alcohol): scores on AUDIT questionnaire Economic outcomes: costs per patient Other outcomes Depression: mean scores on Hospital Anxiety and Depression Rating Scale (HADS) Anxiety: mean scores on Hospital Anxiety and Depression Rating Scale (HADS) Shame: mean BCSS shame scores |
|
| Notes |
|
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Web-based system used to generate the allocation sequence with stratification by centre. Trial investigators report: ”randomisation schedule was constructed using the method of randomised permuted blocks of size four. Randomisation was conducted using a web-based system”. After contacting the investigators (telephone conversation between SG and Prof Davidson on 14 August 2009), review authors judge that an appropriate computer-generated randomisation method was used for random sequence generation |
| Allocation concealment? | Yes | Investigators report: ”the randomisation schedules were generated by the study data centre … and kept securely and confidentially by the trial coordinator at the study coordinating centre in Glasgow. The trial coordinator informed the referring agent of the result of the randomisation immediately and in writing, and then contacted the CBT therapists in each area with the participants details so that CBT could be initiated”. Review authors judge that concealment achieved by use of central allocation so that participants and any investigator enrolling participants could not foresee assignment |
| Blinding? of participants |
Unclear | In a study such as this full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants |
| Blinding? of personnel |
Unclear | In a study such as this full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study |
| Blinding? of outcome assessors |
Yes | Investigators report: ”the research assistants on each site carried out all the assessments at 3-monthly intervals until the participant exited the trial (after 12 months) and were blind to allocation”. Review authors judge that blinding of outcome assessors was adequate and that it was unlikely that this blinding could have been broken |
| Incomplete outcome data addressed? All outcomes |
Yes | Number missing varied across the 4 time points for all outcomes, although at each time point the numbers missing were approximately balanced across the groups. At the final time point (i.e. endpoint at 12 months) there were 5/25 (20%) missing from the CBT group and 6/27 (22%) missing from the TAU group. Reasons for missing data (and any differences in the reasons between groups) are not reported. Feedback from trial investigators (telephone conversation between SG and Prof Davidson on 14 August 2009) confirmed that missing data occurred where clients declined to participate and did not attend. Although no further information is available on why these clients declined to participate, review authors considered the reasons for non-participation were reasonably likely to be balanced across the treatment conditions |
| Free of selective reporting? | Yes | Investigators noted that three additional behaviours were assessed (’shouting angrily at others’; ’threatening to harm others’; ’causing damage to property’), but the published report does not appear to fully report the results of these besides noting that ”overall, no differences were found between those randomised to CBT or TAU on any of the measures at 12-month follow-up”. However, feedback from trial investigators (telephone conversation between SG and Prof Davidson on 14 August 2009) confirmed that ’shouting angrily at others’ and ’threatening to harm others’ were reported together as ’verbal aggression’, and that ’causing damage to property’ was included in outcome ’number reporting any act of physical aggression’ |
| Free of other bias? | Yes | Review authors judge study to be free of other forms of bias despite the analysis being partial rather than true intention-to-treat |
| Methods | Design: cluster-randomised controlled trial | |
| Participants |
Participants: intravenous drug users (subgroup with AsPD) attending an outpatient needle exchange programme Sex: 68% male (whole sample including non-AsPD) Age: median 38 years (whole sample including non-AsPD) Unit of allocation: site (see note 1) Number randomised: 10 sites, 254 participants (whole sample including non-AsPD) (breakdown by treatment condition not supplied) Number completing: 162 (n = 74 intervention group; n = 88 control group) (whole sample including non-AsPD; see note 2) Setting: outpatient; multi-site (10 sites); urban; USA (Baltimore) Inclusion criteria: diagnosis of AsPD (DSM-IV, SCID-II); intravenous drug user participating in the Baltimore needle exchange programme Exclusion criteria: none reported Ethnicity: (whole sample including non-AsPD) 76% black Baseline characteristics: 19% current major depressive disorder; 14% current generalised anxiety disorder; Addiction Severity Index mean score 0.23; 28% HIV positive; 31% had entered opiate agonist treatment |
|
| Interventions | Two conditions: strengths-based case management/control
SBCM activities included engagement, strengths assessment, personal case planning, and resource acquisition. Services provided by case managers included referrals to health and social services, transportation and employment Control condition was passive referral or SBCM of 0 to 4 minutes duration Duration of intervention: median treatment duration of SBCM was 25 minutes Duration of trial: one month Length of follow up: one month Dose adjustment: n/a |
|
| Outcomes |
Primary outcomes
None Secondary outcomes Engagement with services: entry into treatment |
|
| Notes |
|
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | No information given. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Allocation concealment? | Unclear | No information given. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Blinding? of participants |
Unclear | In a study such as this full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants |
| Blinding? of personnel |
Unclear | In a study such as this full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study |
| Blinding? of outcome assessors |
Unclear | Insufficient information to allow a judgement to be made. Clarification about blinding of outcome assessors has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Incomplete outcome data addressed? All outcomes |
Unclear | Unclear whether there are missing outcome data for the AsPD subgroup and, if so, whether the numbers of and reasons for such missing data balance across intervention groups. Review authors unable to make a judgement unless data from AsPD subgroup become available |
| Free of selective reporting? | Yes | Review authors judge that the published report includes all expected outcomes, including those that were pre-specified |
| Free of other bias? | Unclear | There is the possibility of bias arising from baseline imbalance in that the median age of first injection (of drugs) was greater in the control group than in the intervention group |
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: community living adults with personality disorder Sex: (for AsPD subgroup; see note 1) 18 male; 6 female Age: (for AsPD subgroup; see note 1) mean 34.4 (SD 8.4) years Unit of allocation: individual participant Number randomised: (for AsPD subgroup) 24 (13 intervention, 11 control) Number completing: not reported; used Last Observation Carried Forward (LOCF) Setting: outpatient; 5 sites; urban and rural; UK (East Midlands) Inclusion criteria: presence of at least one personality disorder (DSM-IV; IPDE); age 18 to 65 years; literacy and cognitive functioning sufficient to allow engagement with the intervention; able to provide written informed consent Exclusion criteria: major functional psychosis Ethnicity: no information on ethnicity reported for AsPD subgroup Baseline characteristics: (for the entire sample including non-AsPD participants) 49/176 (27.8%) visited Accident and Emergency (A + E) for any reason in the previous 6 months; 25/176 (14.2%) visited A + E due to self-harm in the previous 6 months; 21/176 (11.9%) psychiatric hospital admission in the previous 6 months; mean number of contacts with a psychiatrist/month in the last 6 months 0.21 (intervention) and 0.27 (control group); mean number of contacts with other mental health staff/month in the last 6 months 0.63 (intervention) and 0.83 (control group) (for the AsPD subgroup; see note 1) 4/24 (16.7%) AsPD as the only personality disorder; 20/24 (83.3%) AsPD comorbid with at least one other personality disorder |
|
| Interventions | Two conditions: brief individual psychoeducation plus problem-solving group sessions/treatment as usual
Details of conditions: participants in the intervention condition attended an individual psychoeducation programme where they learned about personality disorder and nature of own personality disorder diagnosis. This followed by 16 weekly group-based problem-solving sessions (lasting approximately 2 hours) based on the ’Stop and Think!’ method. Each group was facilitated by 2 facilitators, experienced in working with patients with personality disorder. Groups started with no more than 8 participants in each and were single gender. In TAU, participants were placed on a waiting list Duration of intervention: mean 24 (range 21 to 28) weeks Duration of trial: mean 24 (range 21 to 28) weeks Length of follow up: none |
|
| Outcomes |
Primary outcomes
Social functioning: scores on Social Functioning Questionnaire (SFQ) Secondary outcomes Anger: scores on State-Trait Anger Expression Inventory-2 (STAXI-2) Impulsivity: scores on Barrett Impulsivity Scale (BIS) Other outcomes Social problem-solving ability: mean scores on the Social Problem Solving Inventory -Revised (SPSI-R) Shame: mean scores on the Experience of Shame Scale (ESS) Dissociation: mean scores on the Dissociative Experiences Scale (DES) |
|
| Notes | 1. 24 (13.6%) of all 176 participants in the sample had AsPD. Of these 13 were allocated to intervention and 11 to control conditions. Data from this AsPD subgroup supplied by trial investigators | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Research investigators describe a block randomisation procedure using computer-generated random numbers provided by an independent statistician. Review authors judge this adequate to minimise bias |
| Allocation concealment? | Yes | Allocation codes pre-sealed into identical, sequentially numbered, opaque envelopes that were opened in sequence by research staff with trial coordinator masked to allocations. Review authors consider it unlikely that participants or any investigator enrolling participants could foresee assignment |
| Blinding? of participants |
Unclear | In a study such as this full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants |
| Blinding? of personnel |
Unclear | In a study such as this full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study |
| Blinding? of outcome assessors |
Unclear | Outcome measures were self-report questionnaires completed by participants who were not blind to their own allocation status and were scored by research assistants who could have been aware of this allocation status in some cases. In view of this uncertainty, review authors consider a judgement of ’unclear’ to be appropriate as some possibility of bias remains |
| Incomplete outcome data addressed? All outcomes |
Yes | Data from the AsPD subgroup supplied by trial investigators indicate that at the end of the trial 4 of 13 (30.8%) were missing from the intervention condition and 3 of 11 (27.3%) were missing from the TAU condition (all outcomes). Reasons for missing data (and any differences in the reasons between conditions) are not available. Feedback from trial investigators confirmed that missing data occurred where clients declined to complete endpoint questionnaires. Although no further information is available on why these clients declined to participate in this task, review authors considered the reasons for missing data were reasonably likely to be balanced across the treatment conditions |
| Free of selective reporting? | Yes | Review authors judge that the published report includes all expected outcomes, including those that were pre-specified |
| Free of other bias? | Unclear | Trial investigators note that outcomes were based on measurements at just two time points (baseline and endpoint) so may be open to bias from those participants in either very optimistic or pessimistic state of mind. They also note that 20 of 24 (83. 3%) participants had at least one other personality disorder. There is also the possibility of bias arising from baseline imbalance in that those in the intervention group were significantly more likely to have had psychiatric hospitalisation at some time in their life in comparison with the controls (although they were not significantly more likely to have been hospitalised in the previous 6 months) |
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: adults charged with a drug-related offence and admitted to a pre-adjudication court Sex: (for whole sample; see note 1) 75% male; 25% female Age: (for whole sample; see note 1) mean 25.1 (SD 8.4) years Unit of allocation: individual participant Number randomised: 279 for sample as a whole; no details for AsPD subgroup (see note 1) Number completing: no details for AsPD subgroup (see note 1) Setting: outpatient; single site; urban; USA (Wilmington, Delaware) Inclusion criteria: at least 18 years old; admitted to a misdemeanour (pre-adjudication) drug court located in Wilmington, Delaware, USA; having plead guilty to the initial charge (the plea of guilty is held in abeyance pending graduation or termination from the programme); charged with possession or consumption of cannabis, possession of drug paraphernalia, possession of hypodermic syringes, or driving under the influence; resident in New Castle County, Delaware or committed his/her offence there Exclusion criteria: having a history of a violent offence involving serious injury to a victim or use of a deadly weapon Ethnicity: (for whole sample; see note 1) white (60%); African American (35%) Baseline characteristics: (for whole sample; see note 1) unmarried (94%); employed (66%); currently abusing cannabis (68%); currently abusing alcohol to intoxication (47%); currently abusing stimulants or cocaine (14%), opiates (13%) or hallucinogens (3%) |
|
| Interventions | Two conditions: optimal (’matched’) schedule of court hearings/standard (’unmatched’) schedule court hearings
Details of conditions: optimal (’matched’) schedule of court hearings in which frequency of court attendance is matched with risk, so that high-risk offenders (those with AsPD and a history of drug treatment) attend with greater frequency. Group sessions were psychoeducational and covered a range of topics including relapse prevention strategies. Minimum requirements for graduation from the programme were attending at least 12 weekly group counselling sessions, providing at least 14 consecutive weekly drug-negative urine specimens, remaining arrest-free, obeying programme rules and paying a $200 court fee Standard (’unmatched’) schedule court hearings required attendance every 4 to 6 weeks Duration of intervention: minimum 14 weeks, although clients require on average approximately 9 months to satisfy all the conditions for graduation Duration of trial: 15 months (9 months to graduation plus 6 months post-discharge) Length of follow up: 6 months post-discharge |
|
| Outcomes |
Primary outcomes
Reconviction: as recorded in Criminal Justice System databases up to 24 months post admission to programme Adverse events: ”no study-related adverse event was reported to date” (p.56, col 1) Secondary outcomes Substance misuse (drugs): data from Addiction Severity Interview, including days of drug use, days any drug use, days alcohol intoxication; any criminal activity; drug screen by urinalysis Substance misuse (alcohol): days alcohol intoxication from ASI Leaving the study early: proportion of participants discontinuing treatment |
|
| Notes |
|
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | No information given. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Allocation concealment? | Unclear | No information given. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Blinding? of participants |
Unclear | In a study such as this full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants |
| Blinding? of personnel |
Unclear | In a study such as this full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study |
| Blinding? of outcome assessors |
Unclear | Insufficient information to allow a judgement to be made. Clarification about blinding of outcome assessors has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Incomplete outcome data addressed? All outcomes |
Unclear | Unclear whether there are missing outcome data for the AsPD subgroup and, if so, whether the numbers of and reasons for such missing data balance across intervention groups. Review authors unable to make a judgement unless data from AsPD subgroup are available |
| Free of selective reporting? | Yes | Review authors judge that the published report includes all expected outcomes, including those that were pre-specified |
| Free of other bias? | Unclear | Review authors unable to judge unless data from the AsPD subgroup become available. It is important to note, however, that the diagnosis of AsPD was via an ‘antisocial personality disorder interview’ derived from SCID-II by the trial investigators, but with no evidence that this has been validated. This may have introduced bias |
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: male outpatients with cocaine dependence Sex: all male Age: (for AsPD subgroup; see note 1) mean 41.2 (SD 6.8) years Unit of allocation: individual participant Number randomised: (for AsPD subgroup) 46 (no details on numbers randomised to each condition; see note 1) Number completing: no details for AsPD subgroup (see note 1) Setting: outpatient; single sites; urban; USA (Philadelphia) Inclusion criteria: male; diagnosis of cocaine dependence (DSM-IIIR; SCID); cocaine use in the 6 months before entrance into the IOP (see note 2); willingness to participate in research; literacy at approximately the fourth-grade level; not homeless Exclusion criteria: history of psychotic disorder requiring antipsychotic medication; current severe dementia Ethnicity: (for AsPD subgroup) African-American 89.1%; white 6.5%; other 4.3%; currently married 28.3%; separated/divorced 60.9%; never married 10.9% Baseline characteristics: (for AsPD subgroup; see note 1) veterans 100%; in education for a mean of 12.6 (SD 1.5) years; lifetime alcohol dependence 84.8%; lifetime major depression 46.7%; mean duration regular cocaine use 7.9 (SD 5.6) years; mean duration of regular drinking 17.6 (9.1) years |
|
| Interventions | Two conditions: individualised relapse prevention/treatment as usual
Details of conditions: IRP is a manualised modular intervention developed for substance users who are in the maintenance phase of recovery. Modules deal with identifying risky situations in the past, self-monitoring current risky situations, learning to anticipate further risky situations, and improving coping responses in these situations. Clients allocated to the IRP condition received 1 individual relapse prevention session and 1 group session per week for up to 20 weeks Participants in the TAU condition received standard continuing care comprising 2 group therapy sessions per week where the orientation was a mix of addictions counselling and 12-step recovery practices Duration of intervention: mean 20 weeks Duration of trial: 17 months Length of follow up: follow up at 3, 6 and 12 months following treatment |
|
| Outcomes |
Primary outcomes
None Secondary outcomes Substance misuse (drugs): data from Addiction Severity Interview and Time-Line Follow-Back, including days of drug use, days any drug use, any criminal activity; data from the Cocaine Relapse Interview; drug screen by urinalysis Substance misuse (alcohol): days alcohol intoxication from ASI Leaving the study early: proportion of participants discontinuing treatment; mean number of continuing care sessions attended Other outcomes None |
|
| Notes |
|
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Trial investigators report: ”An urn randomization procedure was used…which balanced the groups on five potential prognostic factors (marital status, employment status, race, site of initial treatment, and completion of the IOP within the standard 4-week period)”. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Allocation concealment? | Unclear | Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Blinding? of participants |
Unclear | In a study such as this full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants |
| Blinding? of personnel |
Unclear | In a study such as this full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study |
| Blinding? of outcome assessors |
No | Outcome assessors not blinded. Trial investigators report: ”Baseline and follow-up interviews were conducted by research personnel who had received extensive training in the use of the assessment instruments…these interviewers had not been informed of the study hypotheses but they had been informed of treatment condition” (McKay 1997, p.781, col 1). |
| Incomplete outcome data addressed? All outcomes |
Unclear | Unclear whether there are missing outcome data for the AsPD subgroup and, if so, whether the numbers of and reasons for such missing data balance across intervention groups. Review authors unable to make a judgement unless data from AsPD subgroup are available |
| Free of selective reporting? | Yes | Review authors judge that the published report includes all expected outcomes, including those that were pre-specified |
| Free of other bias? | Yes | The study appeared to be free of other sources of bias. In terms of baseline imbalance, a significantly lower percentage of those in the intervention group were married compared to the controls, but as the groups were equivalent on percentages of those living with a romantic partner for 2 years or more the risk of bias from this source was judged not to be significant |
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: cocaine-dependent outpatients (with AsPD subgroup) receiving methadone maintenance treatment Sex: (for AsPD subgroup) 34/48 (71%) male; 14/48 (29%) female Age: (for AsPD subgroup) mean 43.5 (SD 8.1) years Unit of allocation: individual participant Number randomised: 48 (n = 14 CBT; n = 15 CM; n = 7 CM + CBT; n = 12 MM only) Number completing: 44 at 17 weeks; 41 at 26 weeks; 41 at 52 weeks Setting: outpatient, multi-site (2 sites), urban, USA (Los Angeles) Inclusion criteria: cocaine dependence (DSM-IV); receiving methadone maintenance treatment at 1 of 2 clinics for at least 90 days; urine sample testing positive for cocaine use during month prior to study enrolment; antisocial personality disorder (DSM-IV, SCID-II) for AsPD subgroup Exclusion criteria: alcohol or benzodiazepine dependence requiring withdrawal medication; received specific treatment for cocaine dependency in past 30 days; court mandated to treatment Ethnicity: (for AsPD subgroup) 31% white; 21% black; 48% Hispanic/other Baseline characteristics: described by investigators as having ”relatively low motivation”; 60% had completed at least 12 years of schooling; 13% had been in steady employment over last 3 years; self-reported drug/alcohol use in the 30 days prior to admission to the study was: 60% alcohol use, 35% alcohol use to intoxication, 27% marijuana use, 79% heroin use, 31% other opiate use, 96% cocaine use and 8% amphetamine use |
|
| Interventions | Four conditions: cognitive behavioural therapy/contingency management/CBT + contingency management /standard maintenance
Details of conditions: CBT + standard maintenance comprised 48 group sessions of 90 minutes (3 per week for 16 weeks) with typically 4 to 8 participants in each group. Format of sessions was: topic introduced, worksheet read out, discussion of relevance of topic to participants, participants reported their own use of illicit drugs since the last session (with positive verbal reinforcement of decreased or no use of illicit drugs, or for prosocial behaviour), participants described a behavioural plan for the time upto the next session (with positive verbal reinforcement of activities based on the CBT principles presented in the group). Participants continued on standard maintenance treatment (including methadone, mean 72 mg/day) In CM + standard maintenance, participants required to provide 3 urine samples each week and briefly meet (2 to 5 minutes) with a contingency management technician. If urine sample negative for stimulants, participants given a voucher of escalating value and praise/encouragement. Voucher rewards could be increased by subsequent negative samples to a maximum (if the participant was drug-free for all of the 16 week trial) of redeemable vouchers worth $1,277.50. If urine sample positive, voucher was withheld but participant not rebuked/punished. Participants continued on standard maintenance treatment (including methadone, mean 62 mg/day) In CBT + CM + standard maintenance, participants received all 3 interventions. Participants continued on standard maintenance treatment (including methadone, mean 68 mg/day) In standard maintenance only, participants continued on methadone maintenance treatment (mean 71 mg/day) with daily clinic visits for methadone, twice-monthly counselling sessions, plus medical care and case management visits as required Duration of intervention: 16 weeks Duration of trial: 52 weeks (16 week intervention + 36 weeks of follow up) Length of follow up: participants were followed up at weeks 17, 26 and 52 (i.e. weeks 1, 10 and 36 following end of intervention) Dose adjustment: none |
|
| Outcomes |
Primary outcomes
None Secondary outcomes Leaving the study early: proportion of participants discontinuing post-treatment follow up Substance misuse (drugs): cocaine use by urinalysis |
|
| Notes |
|
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Information received from trial investigators (email received 19 October 2009) confirms that a random numbers table was used to prepare numbered sealed envelopes. Review authors judge this adequate to minimise bias |
| Allocation concealment? | Yes | Information received from trial investigators (email received 19 October 2009) confirms that allocation codes were sealed within envelopes that were opened in turn at each site at time of allocation. Only the principal investigator and project co-ordinator had access to these envelopes. Review authors consider it unlikely that participants or any investigator enrolling participants could foresee assignment |
| Blinding? of participants |
Unclear | In a study such as this full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants |
| Blinding? of personnel |
Unclear | In a study such as this full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study |
| Blinding? of outcome assessors |
No | Information received from trial investigators (email received 19 October 2009) confirms that outcome assessors were not blinded to participant allocation. This may have introduced bias |
| Incomplete outcome data addressed? All outcomes |
Yes | The actual number of participants with AsPD failing to complete treatment (at 17 weeks) and to provide data relating to the key outcome (substance misuse - cocaine, by urinalysis) was broadly balanced between the treatment conditions (1/14 for CBT condition; 1/15 for the CM condition, 0/7 for the CBT + CM condition, and 2/12 for the control (SM) condition) |
| Free of selective reporting? | Yes | Study protocol is not available but it seems clear that the published report includes all expected outcomes. No evidence of selective reporting. All prospectively stated outcomes are reported |
| Free of other bias? | Unclear | Trial investigators acknowledge the presence of other psychiatric disorders in the sample; review authors did not judge this to introduce a significant risk of bias. However, whilst all participants were paying for their methadone maintenance treatment (either $140 or $180/month depending upon centre), they received a discount of $40/month for participating in the study. Prior to the introduction of this incentive only 4 subjects had volunteered for the study after 60 days of recruitment. Review authors were unclear whether this payment would introduce bias |
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: outpatients with AsPD and opioid dependency Sex: 77/100 (77%) male; 33/100 (33%) female Age: mean 39 (SD = 7.1) years Unit of allocation: individual participant Number randomised: 100 (n = 51 experimental group; n = 49 control group) Number completing: 86 (n = 42 experimental group; n = 44 control group) Setting: outpatient, single site, urban, USA (Baltimore) Inclusion criteria: antisocial personality disorder (DSM-III-R; SCID-II); opioid dependence (DSM-III-R; SCID-I) Exclusion criteria: pregnancy; bipolar disorder; schizophrenia Ethnicity: 40/100 (40%) Caucasian Baseline characteristics: all participants recruited from local addiction treatment program; 75/100 (75%) were new admissions to the programme and 25/100 (25%) were already in treatment and responding poorly; 12/100 (12%) married; 34/100 (34%) employed; mean 10.7 (SD 2.1) years in education; 72/100 (72%) income less than $500 per month; all participants met criteria for both lifetime and current opioid use disorder (includes both dependence and abuse); 95/100 (95%) met criteria for lifetime cocaine use disorder and 49/100 (49%) current cocaine use disorder; 82/100 (82%) met criteria for lifetime alcohol use disorder and 18/100 (18%) current alcohol use disorder; 58/100 (58%) met criteria for lifetime sedative use disorder and 11/100 (11%) current sedative use disorder; 74/100 (74%) met criteria for lifetime cannabis use disorder and 12/100 (12%) current cannabis use disorder; 41/100 (41%) met criteria for lifetime other stimulants use disorder and 0/100 (0%) current other stimulants use disorder; 38/100 (38%) met criteria for lifetime hallucinogen use disorder and 1/100 (1%) current hallucinogen use disorder; 35/100 (35%) met criteria for lifetime axis I diagnosis and 25/100 (25%) current axis I diagnosis; 28/100 (28%) met criteria for axis II diagnosis (presumably other than AsPD); 46/100 (46%) met criteria for any axis I or II diagnosis |
|
| Interventions | Two conditions: contingency-based behavioural programme/standard maintenance
Details of conditions: The contingency-based behavioural programme is a highly structured contingency-based, adaptive treatment protocol. It is based on counselling sessions and behavioural interventions of rewarding/punishing participants with greater/lesser control over their methadone maintenance based on their compliance with counselling attendance and drug abstinence. Participants gained greater control over methadone clinic attendance and dosage in reward for drug abstinence and attendance at counselling sessions. Negative reinforcers were reduction in methadone dosage and staff determining when and what dosage administered, or being given split dosing Standard maintenance comprised standard methadone substitution treatment in which participants started at methadone dosage of 55 mg/day and attended 2 individual counselling sessions per week. Methadone dosage reviewed every 2 weeks and changes determined clinically. Methadone doses also monitored monthly to ensure it remained comparable to mean dose in experimental group. Methadone take home doses could be earned but only after 12 weeks of consecutive illicit drug negative urine samples and participants could not select the specific day of the week on which they received take home methadone Duration of intervention: 6 months Duration of trial: 7 months (initial 4-week baseline evaluation period followed by 6 months of randomised treatment) Length of follow up: none Dose adjustment: dose of methadone was adjusted according to protocol as determined by group membership (see above) |
|
| Outcomes |
Primary outcomes
Social functioning: mean scores on the Addiction Severity Index (ASI) social/family domain Secondary outcomes Leaving the study early: proportion of participants discontinuing treatment Substance misuse (drugs): drug-related problem severity (adjusted mean ASI composite scores); urinalysis Substance misuse (alcohol): mean ASI scores Employment status: mean ASI employment domain scores Engagement with services: adherence to counselling sessions Other outcomes Proportion transferred due to poor/partial treatment response |
|
| Notes | - | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Information received from trial investigators (email to NH received 17 November 2009) confirmed that sequence generation was by coin toss |
| Allocation concealment? | Yes | Information received from trial investigators (email to NH, received 17 November 2009) indicated that the nature of the allocation process was such that allocation status could not have been predicted or foreseen by the participants or any investigator enrolling participants |
| Blinding? of participants |
Unclear | In a study such as this full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants |
| Blinding? of personnel |
Unclear | In a study such as this full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study |
| Blinding? of outcome assessors |
Yes | Information received from trial investigators (email to NH, received 17 November 2009) confirmed that the laboratory technicians who tested the urines were not privy to the study design or group assignment, that the data entry people who collated attendance did not know the assignment of the patient, and that the research staff who collected the ASI questionnaire data over the course of the study did not know which arm of the study the patient was assigned. Review authors judge that blinding of outcome assessors was adequate and that it was unlikely that this blinding could have been broken |
| Incomplete outcome data addressed? All outcomes |
Unclear | For urinalysis results, 31% of data missing from experimental group and 33% of data missing from control group. Investigators report that missing data were equally distributed across study conditions, but reasons were not given. For ASI results, 9/51 (18%) data missing from experimental group and 5/49 (10%) missing from control group. Review authors unable to judge whether reasons for missing data differ substantially across the groups or if reasons for missing outcome data are likely to be related to true outcome. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Free of selective reporting? | Yes | Review authors judge that the published report includes all expected outcomes, including those that were pre-specified |
| Free of other bias? | Yes | The study appeared to be free of other sources of bias. Investigators comment that presence of therapeutic transfer procedure may have reduced drug abuse in order to avoid transfer to a more intensive routine treatment allocation, although investigators report that this drop-out rate is comparable to other studies of opioid-dependent subjects |
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: patients with recurrent self-harm presenting at hospital emergency departments Sex: for whole sample: 154 male; 326 female Age: for whole sample: mean 31.0 (SD 11.0) years Unit of allocation: individual participant Number randomised: 480 for sample as a whole; no details for dissocial PD subgroup (see note 1) Number completing: no details for dissocial PD subgroup (see note 1) Setting: outpatient; 5 sites; urban; UK (Glasgow, Edinburgh, Nottingham, West London, South London) Inclusion criteria: recent episode of self-harm and presenting at hospital emergency department; at least 1 previous episode of self-harm; willing to provide written consent Exclusion criteria: requiring inpatient psychiatric treatment after self-harm episode; primary diagnosis of substance dependence; psychotic or bipolar disorder Ethnicity: no information provided Baseline characteristics: (for whole sample; see note 1) any personality disorder (ICD-10; PAS-Q) (42.1%); paranoid PD (7.5%); schizoid PD (1.0%); dissocial PD (3.1%); impulsive PD (12.9%); borderline PD (14.0%); histrionic PD (6.7%); anankastic PD (4.0%); anxious PD (14.2%); dependent PD 11.3%) |
|
| Interventions | Two conditions: manual-assisted cognitive behaviour therapy/treatment as usual
Details of conditions: in MACT, participants were allocated a therapist from the existing services and previously trained in MACT according to a pre-planned rota arrangement. Each was sent a 70-page booklet and offered up to 7 treatment sessions In TAU, participants were seen by another designated therapist and offered the standard treatment in the area concerned or the continuation of current therapy Duration of intervention: up to 7 treatment sessions (total duration not specified) Duration of trial: one year Length of follow up: 6 months and 12 months post-treatment |
|
| Outcomes |
Primary outcomes
Social functioning: scores on the Social Functioning Questionnaire (SFQ) Global functioning: scores on the Global Assessment of Functioning (GAF) Quality of life: scores on the EuroQOL Secondary outcomes Economic outcomes: total costs per patient over one year Other outcomesFrequency of self-harm episodes: via Parasuicide History Interview (PHI) Anxiety and depressive symptoms (HADS) Number of completed suicides |
|
| Notes |
|
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Trial investigators report that ”The Stata software was used to generate allocation using randomly permuted blocks…” (Tyrer 2003, p.60). Review authors judge that an appropriate computer-generated randomisation method was used for random sequence generation |
| Allocation concealment? | Yes | Participants were randomly allocated by telephone or fax from the trial’s co-ordinating centre. Review authors judge that concealment was achieved by use of central allocation so that neither participants nor any investigator enrolling participants could foresee assignment |
| Blinding? of participants |
Unclear | In a study such as this full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding? of personnel |
Unclear | In a study such as this full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study |
| Blinding? of outcome assessors |
Unclear | Insufficient information to allow a judgement to be made. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Incomplete outcome data addressed? All outcomes |
Unclear | Unclear whether there are missing outcome data for the dissocial PD subgroup and, if so, whether the numbers of and reasons for such missing data balance across intervention groups. Review authors unable to make a judgement unless data from dissocial PD subgroup become available |
| Free of selective reporting? | Yes | Review authors judge that the published report includes all expected outcomes, including those that were pre-specified |
| Free of other bias? | Yes | The study appeared to be free of other sources of bias |
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: incarcerated drink-driving offenders with AsPD sentenced to a Driving While Intoxicated (DWI) treatment programme Sex: (AsPD subgroup) 45/52 (87%) male; 7/52 (13%) female Age: (AsPD subgroup) mean 26.5 (SD 7.9) years Unit of allocation: individual participant Number randomised: 52 (n = 36 intervention group; n = 16 control group) Number completing: 52 (n = 36 intervention group; n = 16 control group) Setting: prison, single site, USA (New Mexico) Inclusion criteria: court-defined first offenders sentenced to the Driving While Intoxicated (DWI) treatment programme whilst in prison; diagnosis of AsPD (DSM-III-R, Diagnostic Interview Schedule) Exclusion criteria: none reported Ethnicity: (AsPD subgroup) 37/52 (71%) Native American; 12/52 (23%) Non-Hispanic white; 3/52 (6%) Hispanic or other Baseline characteristics: 42/52 (89%) met DSM-III-R criteria for alcohol dependency using the Diagnostic Interview Schedule; mean DrinC score = 23.8 (SD 9.9); mean number of days drinking in past 30 days = 9.2 (SD 8.4) days; mean number of days in last 30 days when had drank and then driven = 3.9 (SD 5.3) days; mean number of drinks per drinking day = 5.9 (SD 5.1); mean number of days with 5 or more drinks = 5.9 (SD 6.9); mean number of days driving after 5 or more drinks = 2.9 (SD 4.3); Form 90 measures of drinking over past 90 days: total standard ethyl-alcohol consumption (SEC) = 328.0 (SD 431.3), drinking days = 25.7 (SD 26.3), mean blood alcohol content (BAC) = 0.043 (SD 0.058) |
|
| Interventions | Two conditions: ’Driving Whilst Intoxicated
program’ + incarceration/incarceration only
Details of conditions: In the DWI condition, the programme was non-confrontational and utilised motivational interviewing principles. Components included: alcohol use, abuse and dependence; health and nutrition; psychological effects of alcohol; drinking and driving awareness; stress management; goal setting and action planning for the future; family issues and alcohol; domestic violence; HIV/AIDS prevention; work release programme for those in employment. Also incorporated culturally appropriate elements such as sweat lodges and talking circles (71 % of participants were native American). The DWI programme was delivered whilst participants were subject to 28 days incarceration The control condition was 28 days incarceration Duration of intervention: 28 days Duration of trial: 25 months (1 month of intervention and 24 months of follow up) Length of follow up: 6, 12 and 24 months Dose adjustment: n/a |
|
| Outcomes |
Primary outcomes
Reconviction: recidivism data Secondary outcomes Substance misuse (alcohol): number of drinks, number of drinking days and mean blood alcohol content; mean number of days driving after drinking in past 30 days; mean number of days driving after 5 or more drinks in past 30 days (via Form 90 and DrInc-2R questionnaires) Other outcomes None |
|
| Notes | - | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | No information provided. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Allocation concealment? | Unclear | No information provided. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Blinding? of participants |
Unclear | In a study such as this full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants |
| Blinding? of personnel |
Unclear | In a study such as this full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study |
| Blinding? of outcome assessors |
Unclear | Insufficient information to allow a judgement to be made. Clarification about blinding of outcome assessors has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Incomplete outcome data addressed? All outcomes |
Unclear | For the outcome of self-reported drink-driving behaviour, data missing for 6/36 (17%) of the intervention group and for 3/16 (19%) of control group. Although these numbers appear similar, reasons for this missing data are not provided. For the outcome of alcohol use, the amount of missing self-report data is not reported but review authors judge it reasonable to assume that the above figures also apply to this as it was measured similarly. For the outcome of drink-driving recidivism, it is unclear what numbers of missing data occurred in AsPD subgroup, although for entire sample missing data on this item reported as 31/305 (10%). Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Free of selective reporting? | Yes | Study protocol is not available but it seems clear that the published report includes all expected outcomes. No evidence of selective reporting. All prospectively stated outcomes are reported |
| Free of other bias? | Unclear | In terms of baseline imbalance, the intervention group were significantly more likely to have histories of drinking and driving in comparison with the controls, although it is unclear if this applied to the AsPD subgroup |
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: methadone-maintained male outpatients with AsPD and opioid dependence (see note 1) Sex: all male Age: (for whole sample, see note 1) mean 29 (SD 6) years Unit of allocation: individual participant Number randomised: 50 with AsPD (breakdown by treatment group not available, see note 1) Number completing: not available (see note 1) Setting: outpatient; single site; urban; USA (Philadelphia) Inclusion criteria: male; aged 18 to 55 years; meeting Food and Drug Administration requirements for methadone maintenance treatment; had been receiving methadone for at least 2 weeks but not more than 6 months during their current treatment episode; subgroup met DSM-III criteria for AsPD (obtained via MPI and SADS) Exclusion criteria: psychosis; persistent or clinically significant organic brain syndrome; serious medical, legal or personal problems that would require movement from local area within 1 year Ethnicity: (for whole sample, see note 1) black (62%); white (38%) Baseline characteristics: (for whole sample, see note 1) lifetime major depressive disorder (35%); lifetime anxiety disorder, any (20%); lifetime alcoholism (19%); antisocial personality disorder (45%) |
|
| Interventions | Three conditions: supportive-expressive psychotherapy + standard maintenance/cognitive behavioural therapy + standard maintenance/standard maintenance only
Details of conditions: SE is an analytically-oriented focal psychotherapy. CBT is cognitive behavioural psychotherapy. Standard maintenance is an individual counselling intervention focused on providing external services rather than dealing with intra-psychic processes, plus methadone maintenance Duration of intervention: 24 weeks Duration of trial: 28 weeks Length of follow up: participants were not followed up after the end of treatment |
|
| Outcomes |
Primary outcomes
None Secondary outcomes Leaving the study early: proportion of participants discontinuing treatment Substance misuse (drugs): data from the Addiction Severity Interview Other outcomes Psychiatric symptoms: mean scores on the SCL90 Depression: mean scores on the Beck Depression Inventory (BDI) |
|
| Notes |
|
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Trial investigators report: ”Patients were randomly assigned to three treatment conditions…”(p.1082, col 1). No further information given. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Allocation concealment? | Unclear | No information provided. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared |
| Blinding? of participants |
Unclear | In a study such as this full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants |
| Blinding? of personnel |
Unclear | In a study such as this full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study |
| Blinding? of outcome assessors |
Yes | Trial investigators report: ”Addiction Severity Interviews were done by independent technicians who were not part of the treatment staff and were not aware of patients group assignments” (p.1082, col 2). Review authors judge that blinding of outcome assessors was adequate for this outcome and that it was unlikely that this blinding could have been broken |
| Incomplete outcome data addressed? All outcomes |
Unclear | Unclear whether there are missing outcome data for the AsPD control condition and, if so, whether the numbers of and reasons for such missing data balance across intervention groups. Review authors unable to make a judgement unless data from AsPD control condition become available |
| Free of selective reporting? | Yes | Review authors judge that the published report includes all expected outcomes, including those that were pre-specified |
| Free of other bias? | Yes | The study appeared to be free of other sources of bias. Review authors note that although participants were not paid for attending sessions, they could receive up to $55 for completing all the measures required over the course of the project. The case for this is argued in the paper. Review authors consider that this is unlikely to have introduced a source of bias |
ASI = Addiction Severity Index; AsPD = antisocial personality disorder; AUDIT = Alcohol Use Disorders Identification Test; BCSS = Brief Core Schema Scales; BIS = Barratt Impulsivity Scale; CBT = cognitive behavioural therapy; CM = contingency management; DAST = Drug and Alcohol Screening Test; DES = Dissociative Experiences Scale; DFST = dual-focus schema therapy; ESS = Experience of Shame Scale; GAF = Global Assessment of Functioning; HADS = Hospital Anxiety and Depression Rating Scale; IOP = Intensive Outpatient Program; IRP = individualised relapse prevention; MACT= manual-assisted cognitive behaviour therapy; PD = personality disorder; PDQ = Personality Diagnostic Questionnaire; QOL = quality of life; SBCM = strengths-based case management; SCID = Structured Clinical Interview for DSM; SD = standard deviation; SFQ= Social Functioning Questionnaire; TAU = treatment as usual
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abbass 2008 | Randomised trial comparing intensive short-term dynamic psychotherapy with TAU in outpatients. Excluded because only one participant had an AsPD diagnosis |
| Arnevik 2009 | Randomised trial comparing short-term day-hospital psychotherapy and outpatient individual psychotherapy for adults with personality disorders. Excluded because diagnosis of AsPD was an exclusion criterion, and because there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Bagby 2008 | Analyses the aggregated results of 2 randomised trials comparing CBT and pharmacotherapy for adults with major depression. Excluded because diagnosis of AsPD was an exclusion criterion, and because there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Ball 2007 | Randomised trial comparing dual-focus schema therapy with 12-step facilitation therapy in opioid dependent outpatients. Excluded because there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Chiesa 2003 | Prospective study comparing 2 specialist psychosocial interventions (therapeutic community-based inpatient treatment and step-down). Excluded because participants not randomised |
| Colom 2004 | Randomised trial comparing a group psychoeducation intervention with a non-structured control intervention in patients with PD and bipolar disorder. Only 2 participants had an AsPD diagnosis. Excluded because participants had bipolar disorder in addition to AsPD |
| Daughters 2008 | Study examining the interactive effects of court-mandated treatment and AsPD on treatment drop-out in a sample of male substance users who were receiving residential substance-abuse treatment. Excluded because participants were not randomised, and there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Easton 2007 | Study aggregating results from two RCTs (Carroll 1998; Carroll 2004) to compare CBT, interpersonal psychotherapy, 12-step facilitation therapy, supportive psychotherapy and disulfiram in outpatients with alcohol and cocaine dependence. Both trials had a subgroup with AsPD. Excluded because neither trial had a control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Fournier 2008 | Randomised trial comparing antidepressants with cognitive therapy in patients with and without PD. Excluded because no participants had an AsPD diagnosis (email from investigators confirming this received 3 June 2009) . Placebo control condition only in the follow up of treatment responders |
| Hesselbrock 1991 | Outcome study of inpatients with alcohol dependency. Excluded because participants were not randomised |
| Kallert 2007 | Randomised trial comparing acute day hospital care with inpatient care. Excluded because no participants had an AsPD diagnosis (email from investigators confirming this received 2 June 2009) |
| Kelly 2009 | Randomised trial comparing individual problem-solving treatment, group sessions on depression prevention and treatment as usual on large pan-European sample of adults with depressive disorder (the ODIN study). Investigators report that 30.9% (n = 93) of the 301 participants who were fully assessed met criteria for at least one PD, but do not report on specific PDs. Excluded because no AsPD subgroup was identified and because a proportion of the sample had a diagnosis of bipolar disorder |
| Kool 2003 | Randomised trial comparing psychodynamic supportive therapy plus pharmacotherapy with pharmacotherapy for depressive disorder in depressed patients with and without AsPD. Excluded because only 4 participants had an AsPD diagnosis (email from investigators to J. Dennis sent 29 May 2009) |
| Kool 2007 | Randomised trial comparing psychodynamic supportive therapy plus pharmacotherapy with pharmacotherapy alone for depressive disorder in depressed patients with and without AsPD (article in Dutch). Excluded because only 3 participants had an AsPD diagnosis |
| Liberman 1981 | Randomised trial comparing BT with insight-oriented therapy for repeated suicide attempters. Excluded because no participants had an AsPD diagnosis and there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Longabaugh 1994 | Randomised trial comparing CBT and relationship enhancement therapy for alcohol abusers. Investigators report 48 of 229 participants recruited had AsPD. Excluded because there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Lynch 2007 | Randomised trial comparing medication plus a DBT-based intervention with medication only in older adults with comorbid PD and depression. Excluded because only 1 participant had an AsPD diagnosis |
| Messina 2002 | Study comparing 2 therapeutic community treatments. PD assessed using MCMI-II. Excluded because the participants were not randomised and there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Milrod 2007 | Randomised trial comparing psychodynamic psychotherapy with relaxation for individuals with panic disorder. Excluded because no participants had an AsPD diagnosis, and there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Mortberg 2007 | Randomised trial comparing group cognitive therapy, individual cognitive therapy and TAU in outpatients with social phobia. Investigators used the SCID-II screener but made no formal diagnostic assessment of PD. Excluded because no indication that any participant had an AsPD diagnosis |
| Muran 2009 | Randomised trial comparing CBT, brief relational therapy and short-term dynamic psychotherapy in fee-paying outpatients. Excluded because the primary inclusion criterion was a diagnosis of Cluster C PD or PDNOS, with no indication of any AsPD subgroup. In addition, there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Petersen 2008 | Randomised trial comparing a specialised psychotherapeutic day-treatment programme with a waiting list control condition for adults with personality disorder. Excluded because a diagnosis of AsPD was an exclusion criterion |
| Sloane 1976 | Randomised trial comparing psychoanalytically-oriented psychotherapy, behaviour therapy and wait-list controls in outpatients. Excluded because diagnosis of AsPD not attempted |
| Springer 1995 | Randomised trial comparing DBT-derived CBT group therapy with discussion control group for inpatients with PD, assessed using MCMI-II. Excluded because no indication that any participant had an AsPD diagnosis |
| Tyrer 2009 | Randomised trial of early versus late assessment of dangerous and severe personality disorder in a sample of prisoners. Excluded because there was no psychological treatment in either allocated condition |
| Vannoy 2004 | Randomised trial comparing anger management with a waiting list control condition. Excluded because no AsPD subgroup |
| Vera 2008 | Study describing a cognitive behavioural group treatment for adults with OCD symptoms plus comorbid personality disorder. Excluded because there was no random allocation and no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Vinnars 2005 | Randomised trial comparing manualised supportive-expressive psychotherapy with non-manualised community-delivered psychotherapy. Excluded because there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Vinnars 2007 | Reports further analysis of data from the trial described by Vinnars 2005, exploring for significant predictors of reduction in psychiatric symptoms. No additional information on the small AsPD subgroup is provided. Excluded because there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Vinnars 2009 | Reports further analysis of data from the trial described by Vinnars 2005, exploring for reductions in personality pathology. No additional information on the small AsPD subgroup is provided. Excluded because there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Weertman 2007 | Randomised trial comparing present-focused and past-focused cognitive therapy in outpatients. Excluded because no participants had an AsPD diagnosis, and there was no control condition that could be classified as either treatment as usual, waiting list or no treatment |
| Winston 1994 | Randomised trial comparing brief adaptive psychotherapy with short-term dynamic psychotherapy and with waiting list controls in outpatients. Excluded because no AsPD subgroup (trial excluded participants with history of violent behaviour or destructive impulse control problems) |
| Wolwer 2001 | Randomised trial comparing CBT and coping skills training against treatment as usual in outpatients with alcohol dependency. Excluded because only 10 participants had an AsPD diagnosis. Review authors judged the number randomised to each of the 3 conditions was too small for extraction of means and SDs for each condition |
| Zorn 2007 | Randomised trial comparing schema focused emotional behaviour therapy and classical social skills training. Excluded because no participants had an AsPD diagnosis |
AsPD = antisocial personality disorder; BT = behaviour therapy; CBT = cognitive behavioural therapy; OCD = obsessive-compulsive disorder; PD = personality disorder; PDNOS = personality disorder not otherwise specified; RCT = randomised controlled trial; TAU = treatment as usual
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Design: parallel randomised controlled trial |
| Participants |
Participants: adult psychiatric inpatients and outpatients with various diagnoses (see note 1) Sex: (for whole sample) 59 women; 31 men Age: (for whole sample) mean 34.7 (SD 10.7), range 18 to 58 years Unit of allocation: individual participant Number randomised: for whole sample, 90 (n = 60 intervention group; n = 30 control group); data not extractable for any AsPD subgroup (see note 1) Number completing: data not extractable for any AsPD subgroup (see note 1) Setting: community; 15 sites (farms); rural; Oslo (Norway) Inclusion criteria: adults currently receiving psychiatric care (both inpatients and outpatients) Exclusion criteria: aged less than 18 years; acute psychotic disorder; mental retardation; serious drug addiction; being in a job during the 6 months prior to start of intervention Ethnicity: no information Baseline characteristics: (for whole sample, see note 1) current inpatients 14/90 (15.5%); current outpatients 76/90 (84.5%); ill for more than 5 years (> 50%); treated in psychiatric institutions for > 3 years (72%); receiving daily medication (83%) |
| Interventions | Two conditions: animal-assisted therapy plus treatment as usual/treatment as usual
TAU comprised ’standard therapy’ and stable medical treatment Duration of intervention: 12 weeks Duration of trial: 9 months Length of follow up: participants were followed up for 6 months after end of treatment |
| Outcomes |
Primary outcomes
None Secondary outcomes Leaving the study early: proportion of participants discontinuing treatment Quality of life: scores on the Quality of Life Scale (QOLS-N) Other outcomes Self-efficacy: scores on the Generalised Self-Efficacy Scale Coping ability: scores on the Coping Strategies Scale |
| Notes |
|
| Methods | Design: parallel randomised controlled trial |
| Participants |
Participants: individuals with recent self-harm episode and personality disturbance within ICD-10 ’flamboyant’ cluster (see note 1) Sex: mixed (breakdown not provided, although treatment groups similar in terms of male:female ratio) Age: range 16 to 50 years Unit of allocation: individual participant Number randomised: for whole sample, 34 (n = 18 intervention group; n = 16 control group; data not extractable for any AsPD subgroup (see note 1) Number completing: data not extractable for any AsPD subgroup (see note 1) Setting: outpatient; 2 sites; urban; UK (London) Inclusion criteria: aged 16 to 50 years; recent episode of self-harm; at least one other episode of self-harm in past 12 months; minimum score of personality disturbance (i.e. one level below personality disorder) within the ICD-10 flamboyant cluster (antisocial, histrionic or emotionally unstable) on the Personality Assessment Schedule (PAS) Exclusion criteria: primary ICD-10 diagnosis within the organic (F0), alcohol or drug dependence (F1) or schizophrenia (F2) groups Ethnicity: no details given Baseline characteristics: (for whole sample, see note 1) groups very similar in age, sex ratio, marital status and employment with no important differences in baseline assessments apart from SFQ scores (MACT mean 11.9; TAU mean 15.6) |
| Interventions | Two conditions: brief manual assisted cognitive behavioural therapy (MACT)/treatment as usual (TAU)
Details of conditions: MACT lasted 2 to 6 sessions, with first chapter of manual given by therapists and remaining 5 chapters sent by post. TAU was standard psychiatric treatment Duration of intervention: between 2 and 6 sessions Duration of trial: to 6 months post-treatment Length of follow up: participants were followed up for 6 months after end of treatment |
| Outcomes |
Primary outcomes
Social functioning: scores on the Social Functioning Questionnaire Secondary outcomes Leaving the study early: proportion of participants discontinuing treatment Economic outcomes: cost of care Other outcomes Time to next parasuicidal act, rate of parasuicidal acts per month, anxiety/depression symptoms |
| Notes |
|
| Methods | Design: parallel randomised controlled trial |
| Participants |
Participants: women with recent suicidal and self-injurious behaviours meeting criteria for BPD (see note 1) Sex: all female Age: mean 29.3 (SD 7.5) years Unit of allocation: individual participant Number randomised: for whole sample, 101 (n = 52 intervention group; n = 49 control group); data not extractable for any AsPD subgroup (see note 1) Number completing: data not extractable for any AsPD subgroup (see note 1) Setting: outpatient; single site; urban; USA (Washington) Inclusion criteria: aged 18 to 45 years; meeting criteria for BPD (DSM-IV, IPDE); current or past suicidal behaviour (2 suicide attempts or self-injuries in past 5 years, with at least 1 in past 8 weeks) Exclusion criteria: lifetime diagnosis of schizophrenia, schizoaffective disorder, bipolar disorder, psychotic disorder, psychotic disorder not otherwise specified, mental retardation; seizure disorder requiring medication; a mandate to treatment; needing primary treatment for another debilitating condition Ethnicity: (for whole sample, see note 1) white (87%), African American (4%), Asian American (2%), native American (1%), other (5%) Baseline characteristics: (for whole sample, see note 1) single, divorced or separated (87.2%); median number suicide attempts in past 5 years 1.0 (IQR 0.5 to 4.0); median number self-injuries in past 5 years 10.0 (IQR 2.0 to 47.0) ; college graduate (23.8%); current major depressive disorder (72.3%); current anxiety disorder (78.2%); current substance use disorder (29.7%); current eating disorder (23.8%); current panic disorder (40.6%); comorbid Cluster A personality disorder (3.0%); comorbid Cluster B personality disorder other than BPD (10.9%), Cluster C PD (25. 7%) |
| Interventions | Two conditions: dialectical behaviour therapy (DBT)/community treatment by experts (CTBE)
Duration of intervention: 12 months Duration of trial: 12 months Length of follow up: participants were followed up for 12 months after end of treatment |
| Outcomes |
Primary outcomes
None Secondary outcomes Leaving the study early: proportion of participants discontinuing treatment Other outcomes Number and severity of self-harm incidents; level of suicidal ideation, reasons for living, depression |
| Notes |
|
AAT = animal-assisted therapy; AsPD = antisocial personality disorder; BPD = borderline personality disorder; CTBE = community treatment by experts; DBT = dialectical behaviour therapy; IQR = inter-quartile range; MACT= manual-assisted cognitive behaviour therapy; SD = standard deviation; SFQ = Social Functioning Questionnaire; TAU = treatment as usual
DATA AND ANALYSES
Comparison 1. Contingency management plus standard maintenance versus standard maintenance alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Other: proportion transferred to routine care due to poor treatment response (high = poor); by 6 months | 1 | 100 | Odds Ratio (M-H, Fixed, 95% CI) | 0.42 [0.17, 1.04] |
| 2 Leaving the study early | 2 | 127 | Odds Ratio (M-H, Fixed, 95% CI) | 0.59 [0.28, 1.24] |
| 3 Social functioning: mean family/social domain scores (high = poor); ASI; at 6 months | 1 | 83 | Mean Difference (IV, Fixed, 95% CI) | −0.08 [−0.14, −0.02] |
| 4 Substance misuse (drugs): numbers with cocaine-negative specimens; at 17 weeks | 1 | 24 | Odds Ratio (M-H, Fixed, 95% CI) | 8.56 [1.33, 54.95] |
| 5 Substance misuse (drugs): numbers with cocaine-negative specimens; at 26 weeks | 1 | 22 | Odds Ratio (M-H, Fixed, 95% CI) | 11.67 [1.53, 89.12] |
| 6 Substance misuse (drugs): numbers with cocaine-negative specimens; at 52 weeks | 1 | 24 | Odds Ratio (M-H, Fixed, 95% CI) | 10.0 [1.44, 69.26] |
Comparison 2. CBT plus TAU versus TAU.
Comparison 3. Social problem-solving therapy with psychoeducation versus TAU.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Social functioning: mean social functioning scores (high = poor); SFQ; at 6 months | 1 | 17 | Mean Difference (IV, Fixed, 95% CI) | −1.60 [−5.43, 2.23] |
| 2 Other: social problem-solving ability; mean overall scores (high = good); SPSI; at 6 months | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 0.18 [−2.57, 2.93] |
| 3 Anger: mean anger expression index scores (high = poor); STAXI-2; at 6 months | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | −1.74 [−12.64, 9.16] |
| 4 Impulsivity: mean impulsiveness scores (high = poor); BIS; at 6 months | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | 6.58 [−4.81, 17.97] |
| 5 Other: shame; mean overall shame scores (high = poor); ESS; at 6 months | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | 14.64 [−12.70, 41. 98] |
| 6 Other: dissociation; mean dissociation scores (high = poor); DES: at 6 months | 1 | 13 | Mean Difference (IV, Fixed, 95% CI) | 4.30 [−21.19, 29.79] |
| 7 Leaving the study early | 1 | 24 | Odds Ratio (M-H, Fixed, 95% CI) | 1.19 [0.20, 6.99] |
Comparison 4. CBT plus standard maintenance versus standard maintenance alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Leaving the study early | 1 | 26 | Odds Ratio (M-H, Fixed, 95% CI) | 0.38 [0.03, 4.87] |
| 2 Substance misuse (drugs): numbers with cocaine-negative specimens; at 17 weeks | 1 | 23 | Odds Ratio (M-H, Fixed, 95% CI) | 2.72 [0.48, 15.47] |
| 3 Substance misuse (drugs): numbers with cocaine-negative specimens; at 26 weeks | 1 | 22 | Odds Ratio (M-H, Fixed, 95% CI) | 5.60 [0.81, 38.51] |
| 4 Substance misuse (drugs): numbers with cocaine-negative specimens; at 52 weeks | 1 | 22 | Odds Ratio (M-H, Fixed, 95% CI) | 8.0 [1.13, 56.79] |
Comparison 5. Contingency management plus CBT plus standard maintenance versus standard maintenance alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Leaving the study early | 1 | 19 | Odds Ratio (M-H, Fixed, 95% CI) | 0.28 [0.01, 6.72] |
| 2 Substance misuse (drugs): numbers with cocaine-negative specimens; at 17 weeks | 1 | 17 | Odds Ratio (M-H, Fixed, 95% CI) | 3.11 [0.41, 23.39] |
| 3 Substance misuse (drugs): numbers with cocaine-negative specimens; at 26 weeks | 1 | 15 | Odds Ratio (M-H, Fixed, 95% CI) | 7.0 [0.69, 70.74] |
| 4 Substance misuse (drugs): numbers with cocaine-negative specimens; at 52 weeks | 1 | 15 | Odds Ratio (M-H, Fixed, 95% CI) | 16.0 [1.09, 234.25] |
Comparison 6. ’Driving Whilst Intoxicated program’ plus incarceration versus incarceration alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Reconviction: reconviction for drink-driving; Cox regression of rearrest rates; at 24 months | 1 | Hazard Ratio (Fixed, 95% CI) | 0.56 [−0.19, 1.31] |
Analysis 1.1. Comparison 1 Contingency management plus standard maintenance versus standard maintenance alone, Outcome 1 Other: proportion transferred to routine care due to poor treatment response (high = poor); by 6 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 1 Contingency management plus standard maintenance versus standard maintenance alone
Outcome: 1 Other: proportion transferred to routine care due to poor treatment response (high = poor); by 6 months
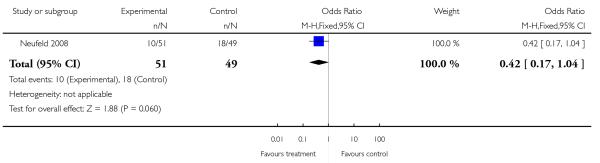
|
Analysis 1.2. Comparison 1 Contingency management plus standard maintenance versus standard maintenance alone, Outcome 2 Leaving the study early.
Review: Psychological interventions for antisocial personality disorder
Comparison: 1 Contingency management plus standard maintenance versus standard maintenance alone
Outcome: 2 Leaving the study early
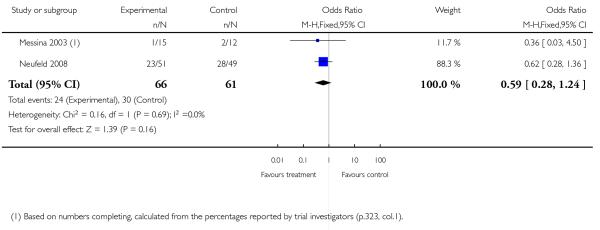
|
Analysis 1.3. Comparison 1 Contingency management plus standard maintenance versus standard maintenance alone, Outcome 3 Social functioning: mean family/social domain scores (high = poor); ASI; at 6 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 1 Contingency management plus standard maintenance versus standard maintenance alone
Outcome: 3 Social functioning: mean family/social domain scores (high = poor); ASI; at 6 months
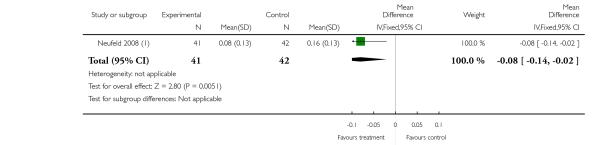
|
(1) From summary data supplied by the trial investigators (adjusted means from mixed regression model, including time-specific random effects and an interaction term). SDs calculated from SEs by review authors as described in the Cochrane Handbook (sections 7.7.3.3 and 16.1.3.1) assuming equal SDs for each group. Estimated SDs were comparable with those reported in broadly similar studies.
Analysis 1.4. Comparison 1 Contingency management plus standard maintenance versus standard maintenance alone, Outcome 4 Substance misuse (drugs): numbers with cocaine-negative specimens; at 17 weeks.
Review: Psychological interventions for antisocial personality disorder
Comparison: 1 Contingency management plus standard maintenance versus standard maintenance alone
Outcome: 4 Substance misuse (drugs): numbers with cocaine-negative specimens; at 17 weeks
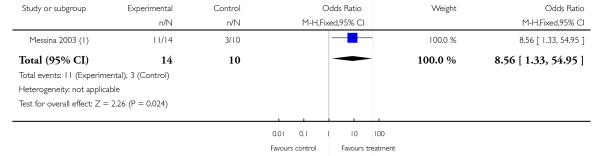
|
|
|
Analysis 1.5. Comparison 1 Contingency management plus standard maintenance versus standard maintenance alone, Outcome 5 Substance misuse (drugs): numbers with cocaine-negative specimens; at 26 weeks.
Review: Psychological interventions for antisocial personality disorder
Comparison: 1 Contingency management plus standard maintenance versus standard maintenance alone
Outcome: 5 Substance misuse (drugs): numbers with cocaine-negative specimens; at 26 weeks
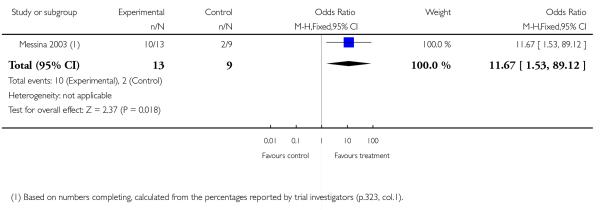
|
Analysis 1.6. Comparison 1 Contingency management plus standard maintenance versus standard maintenance alone, Outcome 6 Substance misuse (drugs): numbers with cocaine-negative specimens; at 52 weeks.
Review: Psychological interventions for antisocial personality disorder
Comparison: 1 Contingency management plus standard maintenance versus standard maintenance alone
Outcome: 6 Substance misuse (drugs): numbers with cocaine-negative specimens; at 52 weeks
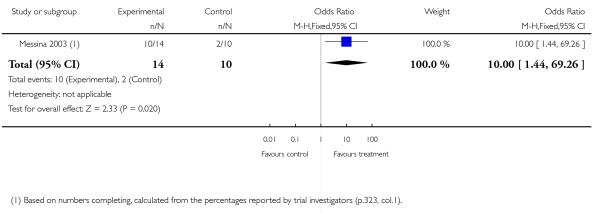
|
Analysis 2.1. Comparison 2 CBT plus TAU versus TAU, Outcome 1 Satisfaction with treatment: satisfaction with taking part in the study (high = good); at 12 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 1 Satisfaction with treatment: satisfaction with taking part in the study (high = good); at 12 months
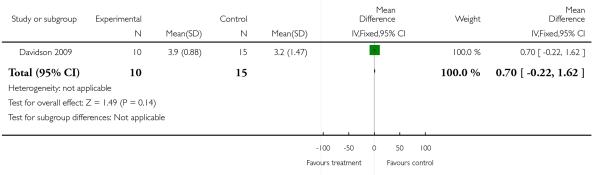
|
Analysis 2.2. Comparison 2 CBT plus TAU versus TAU, Outcome 2 Aggression: number reporting any act of verbal aggression; MCVSI interview; at 12 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 2 Aggression: number reporting any act of verbal aggression; MCVSI interview; at 12 months
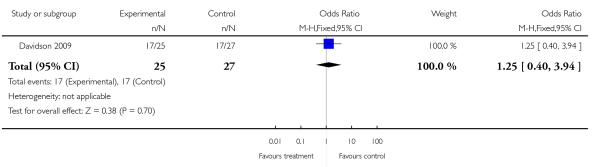
|
Analysis 2.3. Comparison 2 CBT plus TAU versus TAU, Outcome 3 Aggression: change in number reporting any act of verbal aggression (high = good); MCVSI interview; baseline to endpoint at 12 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 3 Aggression: change in number reporting any act of verbal aggression (high = good); MCVSI interview; baseline to endpoint at 12 months
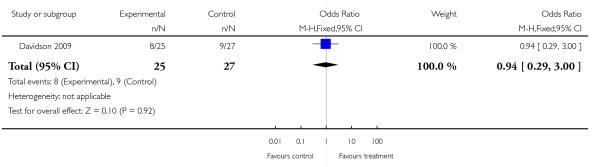
|
Analysis 2.4. Comparison 2 CBT plus TAU versus TAU, Outcome 4 Aggression: number reporting any act of physical aggression; MCVSI interview; at 12 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 4 Aggression: number reporting any act of physical aggression; MCVSI interview; at 12 months
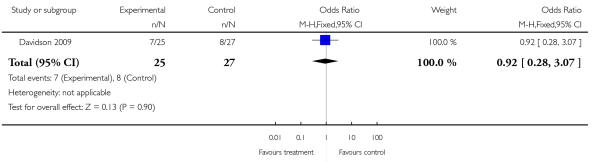
|
Analysis 2.5. Comparison 2 CBT plus TAU versus TAU, Outcome 5 Aggression: change in number reporting any act of physical aggression (high = good); baseline to endpoint at 12 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 5 Aggression: change in number reporting any act of physical aggression (high = good); baseline to endpoint at 12 months
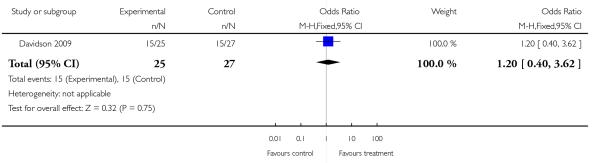
|
Analysis 2.6. Comparison 2 CBT plus TAU versus TAU, Outcome 6 Social functioning: mean SFQ scores (high = poor); at 12 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 6 Social functioning: mean SFQ scores (high = poor); at 12 months
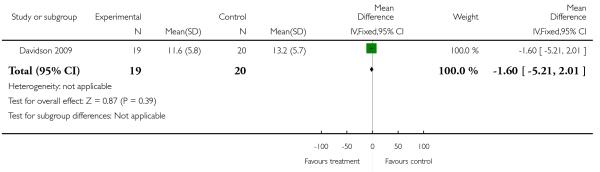
|
Analysis 2.7. Comparison 2 CBT plus TAU versus TAU, Outcome 7 Leaving the study early; by 3 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 7 Leaving the study early; by 3 months
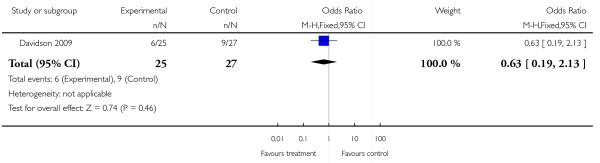
|
Analysis 2.8. Comparison 2 CBT plus TAU versus TAU, Outcome 8 Leaving the study early; by 6 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 8 Leaving the study early; by 6 months
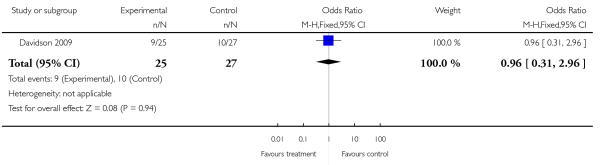
|
Analysis 2.9. Comparison 2 CBT plus TAU versus TAU, Outcome 9 Leaving the study early; by 9 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 9 Leaving the study early; by 9 months
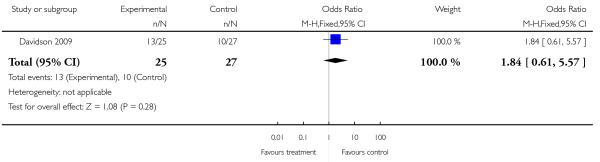
|
Analysis 2.10. Comparison 2 CBT plus TAU versus TAU, Outcome 10 Leaving the study early; by 12 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 10 Leaving the study early; by 12 months
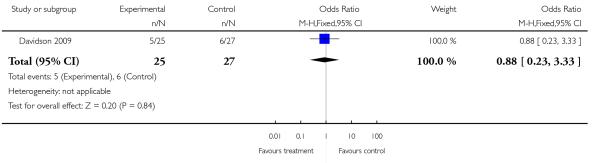
|
Analysis 2.11. Comparison 2 CBT plus TAU versus TAU, Outcome 11 Anger: mean Novaco Anger Scale scores (high = poor); at 12 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 11 Anger: mean Novaco Anger Scale scores (high = poor); at 12 months
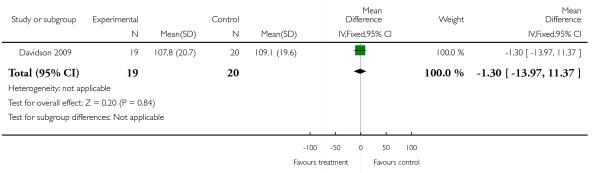
|
Analysis 2.12. Comparison 2 CBT plus TAU versus TAU, Outcome 12 Anger: mean Novaco Provocation Inventory scores (high = poor); at 12 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 12 Anger: mean Novaco Provocation Inventory scores (high = poor); at 12 months
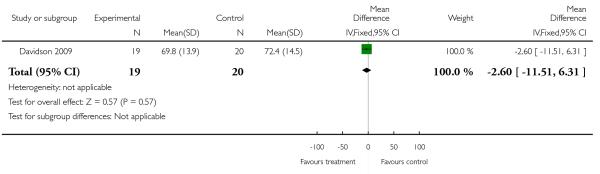
|
Analysis 2.13. Comparison 2 CBT plus TAU versus TAU, Outcome 13 Other: anxiety; mean HADS score (high = poor); at 12 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 13 Other: anxiety; mean HADS score (high = poor); at 12 months
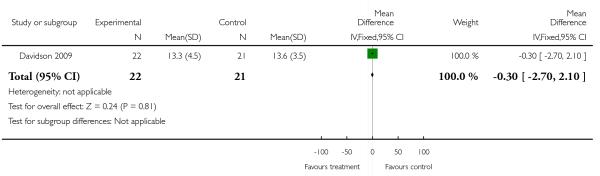
|
Analysis 2.14. Comparison 2 CBT plus TAU versus TAU, Outcome 14 Other: depression; mean HADS score (high = poor); at 12 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 2 CBT plus TAU versus TAU
Outcome: 14 Other: depression; mean HADS score (high = poor); at 12 months
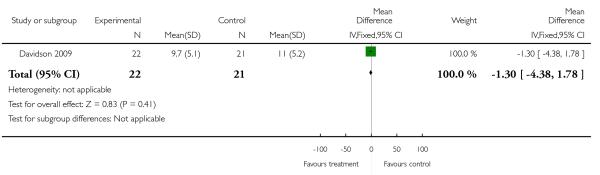
|
Analysis 3.1. Comparison 3 Social problem-solving therapy with psychoeducation versus TAU, Outcome 1 Social functioning: mean social functioning scores (high = poor); SFQ; at 6 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 3 Social problem-solving therapy with psychoeducation versus TAU
Outcome: 1 Social functioning: mean social functioning scores (high = poor); SFQ; at 6 months
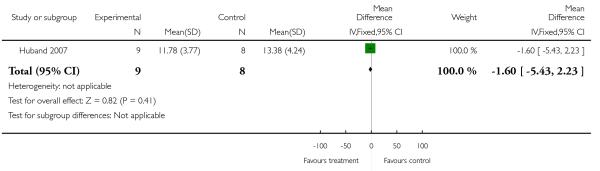
|
Analysis 3.2. Comparison 3 Social problem-solving therapy with psychoeducation versus TAU, Outcome 2 Other: social problem-solving ability; mean overall scores (high = good); SPSI; at 6 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 3 Social problem-solving therapy with psychoeducation versus TAU
Outcome: 2 Other: social problem-solving ability; mean overall scores (high = good); SPSI; at 6 months
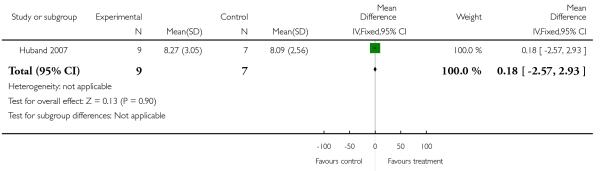
|
Analysis 3.3. Comparison 3 Social problem-solving therapy with psychoeducation versus TAU, Outcome 3 Anger: mean anger expression index scores (high = poor); STAXI-2; at 6 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 3 Social problem-solving therapy with psychoeducation versus TAU
Outcome: 3 Anger: mean anger expression index scores (high = poor); STAXI-2; at 6 months
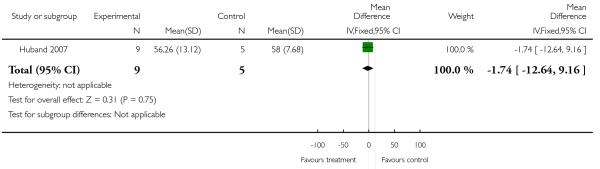
|
Analysis 3.4. Comparison 3 Social problem-solving therapy with psychoeducation versus TAU, Outcome 4 Impulsivity: mean impulsiveness scores (high = poor); BIS; at 6 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 3 Social problem-solving therapy with psychoeducation versus TAU
Outcome: 4 Impulsivity: mean impulsiveness scores (high = poor); BIS; at 6 months
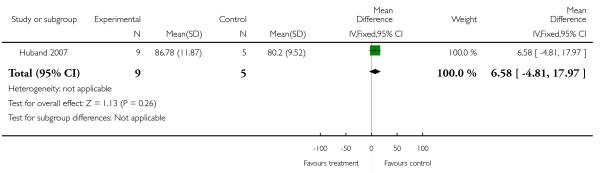
|
Analysis 3.5. Comparison 3 Social problem-solving therapy with psychoeducation versus TAU, Outcome 5 Other: shame; mean overall shame scores (high = poor); ESS; at 6 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 3 Social problem-solving therapy with psychoeducation versus TAU
Outcome: 5 Other: shame; mean overall shame scores (high = poor); ESS; at 6 months
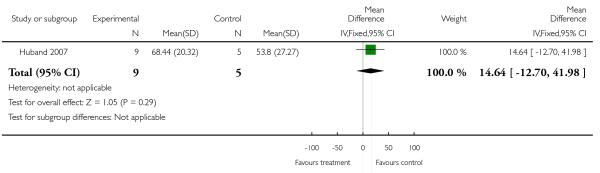
|
Analysis 3.6. Comparison 3 Social problem-solving therapy with psychoeducation versus TAU, Outcome 6 Other: dissociation; mean dissociation scores (high = poor); DES: at 6 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 3 Social problem-solving therapy with psychoeducation versus TAU
Outcome: 6 Other: dissociation; mean dissociation scores (high = poor); DES: at 6 months
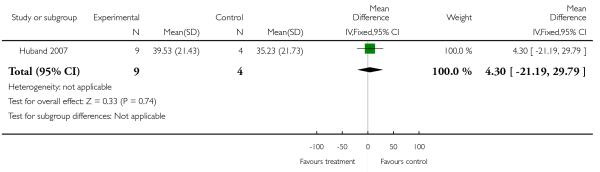
|
Analysis 3.7. Comparison 3 Social problem-solving therapy with psychoeducation versus TAU, Outcome 7 Leaving the study early.
Review: Psychological interventions for antisocial personality disorder
Comparison: 3 Social problem-solving therapy with psychoeducation versus TAU
Outcome: 7 Leaving the study early
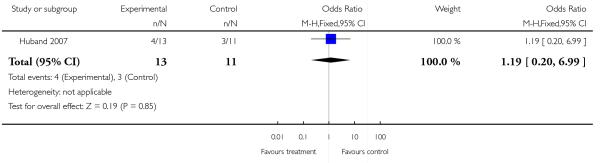
|
Analysis 4.1. Comparison 4 CBT plus standard maintenance versus standard maintenance alone, Outcome 1 Leaving the study early.
Review: Psychological interventions for antisocial personality disorder
Comparison: 4 CBT plus standard maintenance versus standard maintenance alone
Outcome: 1 Leaving the study early
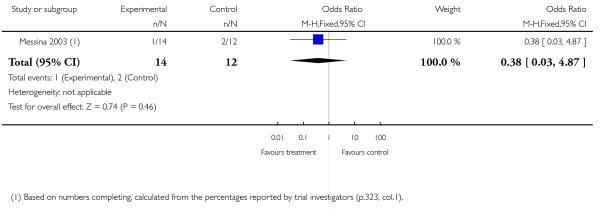
|
Analysis 4.2. Comparison 4 CBT plus standard maintenance versus standard maintenance alone, Outcome 2 Substance misuse (drugs): numbers with cocaine-negative specimens; at 17 weeks.
Review: Psychological interventions for antisocial personality disorder
Comparison: 4 CBT plus standard maintenance versus standard maintenance alone
Outcome: 2 Substance misuse (drugs): numbers with cocaine-negative specimens; at 17 weeks
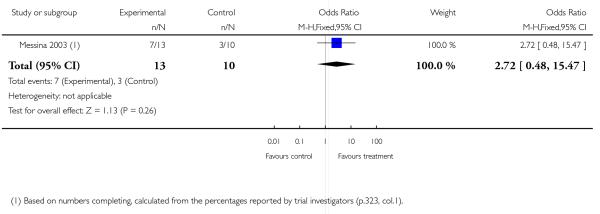
|
Analysis 4.3. Comparison 4 CBT plus standard maintenance versus standard maintenance alone, Outcome 3 Substance misuse (drugs): numbers with cocaine-negative specimens; at 26 weeks.
Review: Psychological interventions for antisocial personality disorder
Comparison: 4 CBT plus standard maintenance versus standard maintenance alone
Outcome: 3 Substance misuse (drugs): numbers with cocaine-negative specimens; at 26 weeks
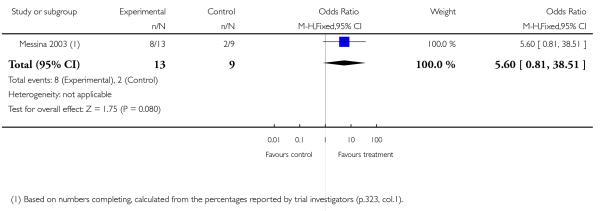
|
Analysis 4.4. Comparison 4 CBT plus standard maintenance versus standard maintenance alone, Outcome 4 Substance misuse (drugs): numbers with cocaine-negative specimens; at 52 weeks.
Review: Psychological interventions for antisocial personality disorder
Comparison: 4 CBT plus standard maintenance versus standard maintenance alone
Outcome: 4 Substance misuse (drugs): numbers with cocaine-negative specimens; at 52 weeks
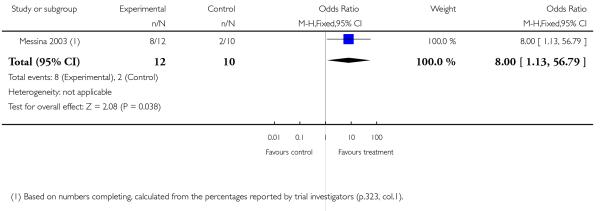
|
Analysis 5.1. Comparison 5 Contingency management plus CBT plus standard maintenance versus standard maintenance alone, Outcome 1 Leaving the study early.
Review: Psychological interventions for antisocial personality disorder
Comparison: 5 Contingency management plus CBT plus standard maintenance versus standard maintenance alone
Outcome: 1 Leaving the study early
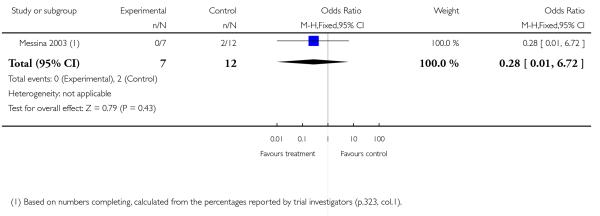
|
Analysis 5.2. Comparison 5 Contingency management plus CBT plus standard maintenance versus standard maintenance alone, Outcome 2 Substance misuse (drugs): numbers with cocaine-negative specimens; at 17 weeks.
Review: Psychological interventions for antisocial personality disorder
Comparison: 5 Contingency management plus CBT plus standard maintenance versus standard maintenance alone
Outcome: 2 Substance misuse (drugs): numbers with cocaine-negative specimens; at 17 weeks
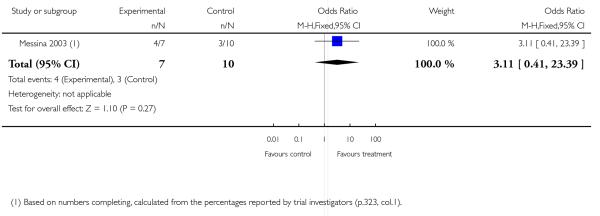
|
Analysis 5.3. Comparison 5 Contingency management plus CBT plus standard maintenance versus standard maintenance alone, Outcome 3 Substance misuse (drugs): numbers with cocaine-negative specimens; at 26 weeks.
Review: Psychological interventions for antisocial personality disorder
Comparison: 5 Contingency management plus CBT plus standard maintenance versus standard maintenance alone
Outcome: 3 Substance misuse (drugs): numbers with cocaine-negative specimens; at 26 weeks
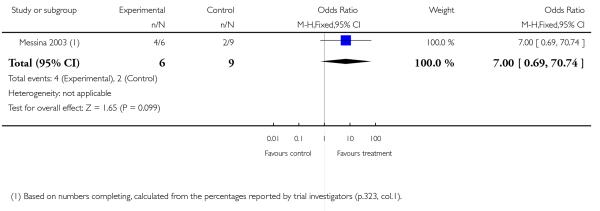
|
Analysis 5.4. Comparison 5 Contingency management plus CBT plus standard maintenance versus standard maintenance alone, Outcome 4 Substance misuse (drugs): numbers with cocaine-negative specimens; at 52 weeks.
Review: Psychological interventions for antisocial personality disorder
Comparison: 5 Contingency management plus CBT plus standard maintenance versus standard maintenance alone
Outcome: 4 Substance misuse (drugs): numbers with cocaine-negative specimens; at 52 weeks
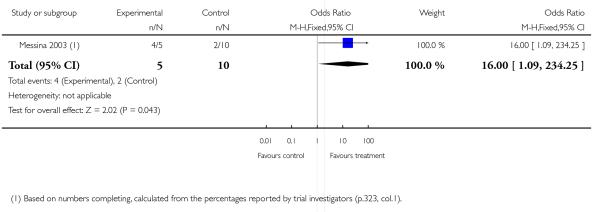
|
Analysis 6.1. Comparison 6 ‘Driving Whilst Intoxicated program’ plus incarceration versus incarceration alone, Outcome 1 Reconviction: reconviction for drink-driving; Cox regression of rearrest rates; at 24 months.
Review: Psychological interventions for antisocial personality disorder
Comparison: 6 ‘Driving Whilst Intoxicated program’ plus incarceration versus incarceration alone
Outcome: 1 Reconviction: reconviction for drink-driving; Cox regression of rearrest rates; at 24 months
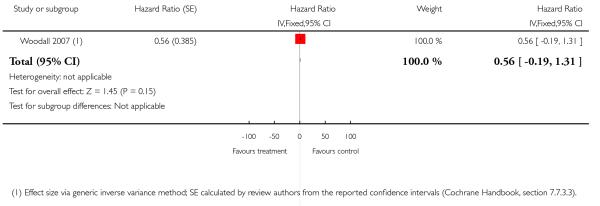
|
ADDITIONAL TABLES
Table 1. Comparison 1: Contingency management + standard maintenance versus standard maintenance alone: Addiction Severity Index scores.
| Study | Outcome | Adjusted mean(Exp) | SE(Exp) | Adjusted mean(Cntrl) | SE(Cntrl) | Difference of least square means over months 1 to 6 | df | P value | Notes |
|---|---|---|---|---|---|---|---|---|---|
| Neufeld 2008 | Family/social domain scores | 0.08 | 0.02 | 0.16 | 0.02 | −0.09 | 81 | 0.005 | Favours treatment |
| Neufeld 2008 | Employment domain scores | 0.72 | 0.04 | 0.72 | 0.04 | 0.006 | 81 | 0.91 | Favours neither condition |
| Neufeld 2008 | Alcohol domain scores | 0.02 | 0.01 | 0.04 | 0.01 | −0.02 | 81 | 0.17 | Favours neither condition |
| Neufeld 2008 | Drug domain scores | 0.16 | 0.01 | 0.19 | 0.01 | −0.03 | 81 | 0.09 | Favours neither condition |
Summary data supplied by the trial investigators. Adjusted means obtained from mixed regression model which included time-specific random effects and an interaction term.
Table 2. Comparison 1: Contingency management + standard maintenance versus standard maintenance alone: cocaine abstinence (skewed data).
| Study | Outcome | n(Exp) | Mean(Exp) | SD(Exp) | n(Cntrl) | Mean(Cntrl) | SD(Cntrl) | Statistic | Notes |
|---|---|---|---|---|---|---|---|---|---|
| Messina 2003 | Number cocaine-negative specimens; by 16 weeks (see note 1) | 15 | 39.4 | 11.4 | 12 | 9.3 | 11.3 | P < 0.05 (Two- way ANOVA; Tukey-Kramer post-hoc test; no further details) | Favours treatment |
1. Outcome is mean number of cocaine-negative specimens per participant; n(EXp) and n(Cntrl) are numbers reported as randomised to each condition.
Table 3. Comparison 1: Contingency management + standard maintenance versus standard maintenance alone: percentage drug-negative specimens.
| Study | Outcome | Experimental group | Control group | Statistic | Notes |
|---|---|---|---|---|---|
| Neufeld 2008 | P ercentage opioid-negative specimens; at 6 months | 80.5% | 73.7% | OR 1.31 (95% CI 0.71 to 2.42; P = 0.393) | Favours neither condition |
| Neufeld 2008 | Percentage cocaine-negative specimens; at 6 months | 77.3% | 66.7% | OR 1.59 (95% CI 0.86 to 2.96; P = 0.139) | Favours neither condition |
| Neufeld 2008 | Percentage sedative-negative specimens; at 6 months | 96.2% | 90.8% | OR 1.82 (95% CI 0. 715 to 4.42; P = 0.184) | Favours neither condition |
| Neufeld 2008 | Percentage (any) drug-negative specimens; at 6 months | 68.7% | 54.2% | OR 1.70 (95% CI 0.94 to 3.07; P = 0.081) | Favours neither condition |
Statistics provided by trial investigators; data relate to proportion of specimens that are negative, rather than proportion of participants who provided negative specimens.
Table 4. Comparison 1: Contingency management + standard maintenance versus standard maintenance alone: attendance at counselling sessions.
| Study | Outcome | Experimental group | Control group | Statistic | Notes |
|---|---|---|---|---|---|
| Neufeld 2008 | Number counselling sessions attended in proportion to total number of sessions offered; by 6 months | 83.2% (1285/1545) | 53.4% (897/1679) | OR 4.00 (95% CI 2. 39 to 6.70; P < 0. 0001) Statistics provided by trial investigators | Favours treatment |
T hese data relate to the counselling sessions attended, and not to the numbers of participants who attended.
Table 5. Comparison 2: CBT + standard maintenance versus standard maintenance alone: cocaine abstinence (skewed data).
| Study | Outcome | n(Exp) | Mean(Exp) | SD(Exp) | n(Cntrl) | Mean(Cntrl) | SD(Cntrl) | Statistic | Notes |
|---|---|---|---|---|---|---|---|---|---|
| Messina 2003 | Number cocaine-negative specimens; by 16 weeks (see note 1) | 14 | 24.8 | 15.6 | 12 | 9.3 | 11.3 | P < 0.05 (T wo-way ANOVA; Tukey-Kramer post-hoc test) | Favours treatment |
1. Outcome is mean number of cocaine-negative specimens per participant; n(Exp) and n(cntrl) are numbers reported as randomised to each condition.
Table 6. Comparison 3: Contingency management + CBT + standard maintenance versus standard maintenance alone: cocaine abstinence (skewed data).
| Study | Outcome | n(Exp) | Mean(Exp) | SD(Exp) | n(Cntrl) | Mean(Cntrl) | SD(Cntrl) | Statistic | Notes |
|---|---|---|---|---|---|---|---|---|---|
| Messina 2003 | Number cocaine-negative specimens; by 16 weeks (see note 1) | 7 | 37.7 | 13.3 | 12 | 9.3 | 11.3 | P < 0.05 (T wo-way ANOVA; Tukey-Kramer post-hoc test) | Favours treatment |
1. Outcome is mean number of cocaine-negative specimens per participant; n(Exp) and n(cntrl) are numbers reported as randomised to each condition.
Table 7. Comparison 4: CBT + TAU versus TAU: alcohol abuse scores (skewed data).
| Study | Outcome | CBT(baseline)
Mean (SD) |
n | CBT(last)
Mean (SD) |
n | Difference (95% CI) |
TAU(baseline) | n | TAU(last value) | n | Difference (95% CI) |
Comparison of difference (95% CI) |
Notes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Davidson 2009 | AUDIT scores (high = poor); at 12 months | 8.2 (6. 8) | 25 | 5.9 (7. 6) | 19 | 4.1 (0.5 to 7.7) P = 0.03 | 11.1 (5. 9) | 27 | 11.0 (9. 4) | 20 | 0.3 (−3.1 to 3. 7) P = 0.85 | 4.1 (−0.6 to 8. 9) P = 0.08 | Favours neither condition LOCF analysis (see note 1) |
| Davidson 2009 | AUDIT total units scores (high = poor); at 12 months | 8.4 (9. 1) | 24 | 7.9 (10.0) | 18 | 2.7 (−2.8 to 8.2) P = 0.31 | 15.7 (12.4) | 26 | 10.7 (14. 7) | 20 | 5.5 (−1.7 to 12. 8) P = 0.12 | 0.6 (−7.6 to 8. 8) P = 0.88 | Favours neither condition LOCF analysis (see note 1) |
1. Trial investigators have used a Last Observation Carried Forward procedure (i.e. endpoint scores based on last available value).
CBT = cognitive behavioural therapy; LOCF = last observation carried forward; TAU = treatment as usual
Table 8. Comparison 4: CBT + TAU versus TAU: costs of services received.
| Study | Outcome | Experimental (CBT) (n = 25) | Control (TAU) (n = 27) | Statistic |
|---|---|---|---|---|
| Davidson 2009 | T otal cost of health, social work and criminal justice services received; over 12 months | £38,004 | £31,097 | No statistic available |
| Davidson 2009 | A verage cost per participant for NHS services alone; over 12 months | £1295 | £1133 | No statistic available |
CBT = cognitive behavioural therapy; TAU = treatment as usual
Table 9. Comparison 4: CBT + TAU versus TAU: schema scores; at 12 months (skewed data).
| Study | Outcome | CBT(baseline)
Mean (SD) |
n | CBT(last)
Mean (SD) |
n | Difference (95% CI) |
TAU(baseline) | n | TAU(last value) | n | Difference (95% CI) |
Comparison of difference (95% CI) |
Notes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Davidson 2009 | BCSS self-as-positive belief scores; at 12 months | 8.6 (5. 7) | 25 | 8.8 (6. 3) | 19 | 0.2 (−1.9 to 2.4) P = 0.84 | 7.8 (6. 1) | 27 | 7.2 (6.8) | 20 | −0.1 (−3.0 to 2. 7) P = 0.92 | −0.2 (−3.6 to 3. 1) P = 0.89 | Favours neither condition LOCF analysis (see note 1) |
| Davidson 2009 | BCSS self-as-negative belief scores; at 12 months | 8.6 (5. 5) | 25 | 7.7 (6. 7) | 19 | 2.2 (−0.4 to 4.8) P = 0.09 | 10.1 (6. 6) | 27 | 8.6 (6.1) | 20 | 0.5 (−2.1 to 3. 1) P = 0.68 | −0.8 (−4.3 to 2. 7) P = 0.64 | Favours neither condition LOCF analysis (see note 1) |
| Davidson 2009 | BCSS others-as-positive belief scores; at 12 months | 9.3 (6. 1) | 25 | 9.6 (6. 4) | 19 | −0.4 (−3.0 to 2.2) P = 0.74 | 6.6 (4. 4) | 27 | 5.6 (4.4) | 20 | 1.2 (−1.0 to 3. 4) P = 0.28 | −2.6 (−5.8 to 0. 5) P = 0.10 | Favours neither condition LOCF analysis (see note 1) |
| Davidson 2009 | BCSS others-as-negative belief scores; at 12 months | 12.9 (7.4) | 25 | 11.9 (8.2) | 19 | 0.2 (−1.7 to 2.1) P = 0.82 | 11.8 (7. 1) | 27 | 9.1 (5.3) | 20 | 2.4 (−0.7 to 5. 6) P = 0.12 | −2.4 (−5.8 to 0. 9) P = 0.15 | Favours neither condition LOCF analysis (see note 1) |
1. Trial investigators have used a Last Observation Carried Forward procedure (i.e. endpoint scores based on last available value).
BCSS = Brief Core Schema Scales ; CBT = cognitive behavioural therapy; LOCF = last observation carried forward; TAU = treatment as usual
Table 10. Comparison 6: ’Driving Whilst Intoxicated program’ + incarceration versus incarceration alone: days drink driving, self-reported (skewed data).
| Study | Outcome | n(Exp) | Mean(Exp) | SD(Exp) | n(Cntrl) | Mean(Cntrl) | SD(Cntrl) | Statistic |
|---|---|---|---|---|---|---|---|---|
| Woodall 2007 | D ays driving after drinking in past 30 days; self-reported; at 6 months | 30 | 0.83 | 3.70 | 13 | 0.69 | 2.50 | Favours neither condition Completer analysis (see note 1) |
| Woodall 2007 | D ays driving after drinking in past 30 days; self-reported; at 12 months | 30 | 0.63 | 1.69 | 13 | 0.46 | 0.88 | Favours neither condition Completer analysis (see note 1) |
| Woodall 2007 | Days driving after drinking in past 30 days; self-reported; at 24 months | 30 | 0.67 | 1.75 | 13 | 0.38 | 0.38 | Favours neither condition Completer analysis (see note 1) |
| Woodall 2007 | Days driving after drinking in past 30 days; self-reported; mean improvement over baseline; at 24 months | 30 | 4.26 | 6.32 | 13 | 3.03 | 4.08 | Favours neither condition Completer analysis (see note 1) |
1. Trial investigators report a significant overall main effect of time (P < 0.001), ”indicating a decline in self-reported drinking and driving from intake to post-incarceration assessments” (p.982, col 2) and a significant AsPD-by-time interaction (P < 0.001) ”resulting from the fact that the AsPD participants showed a greater improvement over time than the non-AsPD participants” (p.982, col 2), but that the group-by-time interaction was not significant (ANOVA, mixed factorial design).
Table 11. Comparison 6: ’Driving Whilst Intoxicated program’ + incarceration versus incarceration alone: days driving after five or more drinks, self-reported (skewed data).
| Study | Outcome | n(Exp) | Mean(Exp) | SD(Exp) | n(Cntrl) | Mean(Cntrl) | SD(Cntrl) | Statistic |
|---|---|---|---|---|---|---|---|---|
| Woodall 2007 | Days driving after 5 or more drinks in past 30 days; self-reported; at 6 months | 30 | 0.87 | 3.73 | 13 | 0.08 | 0.28 | Favours neither condition Completer analysis (see note 1) |
| Woodall 2007 | Days driving after 5 or more drinks in past 30 days; self-reported; at 12 months | 30 | 0.57 | 1.63 | 13 | 0.38 | 0.77 | Favours neither condition Completer analysis (see note 1) |
| Woodall 2007 | Days driving after 5 or more drinks in past 30 days; self-reported; at 24 months | 30 | 0.50 | 1.25 | 13 | 0.31 | 0.63 | Favours neither condition Completer analysis (see note 1) |
| Woodall 2007 | Days driving after 5 or more drinks in past 30 days; self-reported; mean improvement over baseline; at 24 months | 30 | 3.02 | 4.93 | 13 | 2.28 | 4.22 | Favours neither condition Completer analysis (see note 1) |
1. Trial investigators report a significant overall main effect of time (P < 0.001), ”indicating a decline in self-reported drinking and driving from intake to post-incarceration assessments” (p.982, col 2) and a significant AsPD-by-time interaction (P < 0.001) ”resulting from the fact that the AsPD participants showed a greater improvement over time than the non-AsPD participants” (p.982, col 2), but that the group-by-time interaction was not significant (ANOVA, mixed factorial design).
Appendix 1. MEDLINE search strategy
We searched MEDLINE 1950 to 11 September 2009 using the following terms:
exp Personality Disorders/
exp Antisocial Personality Disorder/
exp Borderline Personality Disorder/
exp Compulsive Personality Disorder/
exp Dependent Personality Disorder/
exp Histrionic Personality Disorder/
exp Hysteria/
exp Paranoid Personality Disorder/
exp Passive-Aggressive Personality Disorder/
exp Schizoid Personality Disorder/
exp Schizotypal Personality Disorder/
((asocial$ or antisocial$ or dissocial$ or psychopath$ or sadist$ or sociopath$) adj2 person$).tw.
psychopath.tw.
sociopath$.tw.
(moral adj2 insanity).tw.
(DSM and (axis and II)).tw.
or/1-16
randomized controlled trial.pt.
controlled clinical trial.pt.
randomized controlled trials.sh.
random allocation.sh.
double blind method.sh.
single-blind method.sh.
or/18-23
(animal not human).sh.
24 not 25
clinical trial.pt.
exp clinical trials/
(clin$ adj25 trial$).ti,ab.
((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).ti,ab.
Placebos.sh.
placebo$.ti,ab.
random$.ti,ab.
research design.sh.
or/27-34
35 not 25
36 not 26
comparative study.sh.
exp evaluation studies/
follow up studies.sh.
prospective studies.sh.
(control$ or prospectiv$ or volunteer$).ti,ab.
or/38-42
43 not 25
44 not (26 or 37)
26 or 37 or 45
17 and 46
Appendix 2. ASSIA search strategy
We searched Applied Social Sciences Index and Abstracts (1987 to September 2009) using the following terms:
((personality near disorder*) or ((antisocial* near disorder*) or (avoidant* near disorder*) or (bordeline* near disorder*)) or ((dependent* near disorder*) or (histrionic* near disorder*) or (narcissistic* near disorder*)) or ((obsessive* near disorder*) or (compulsive* near disorder*) or (paranoid* near disorder*)) or (((passive* near disorder*) or (aggress* near disorder*) or (sadomasochistic* near disorder*)) or (schizo* near disorder*)) or (((passive* and disorder*) or (aggress* and disorder*) or (sadomasochistic* and disorder*)) or ((schizo* and disorder*) or (paranoid* and disorder*) or (compulsive* and disorder*)) or ((obsessive* and disorder*) or (narcissistic and disorder*) or (histrionic* and disorder*))) or (((personality and disorder*) or (antisocial* and disorder*) or (avoidant* and disorder*)) or ((borderline* and disorder*) or (dependent* and disorder*)))) and ((AB=randomi* or TI=randomi*) or (DE=(randomi?ed controlled trials) or AB=(double* blind*) or TI=(double* blind*)) or (DE=(double blind studies) or (single* near blind*)))
Appendix 3. BIOSIS search strategy
We searched BIOSIS (1985 to 16 September 2009) using the following terms:
((((al: ((personality and disorder))) or al: ((antisocial and behaviour))) or al: ((antisocial and behavior)) or (((al: ((self and defeating))) or al: ((parano* and person*))) or al: ((gender and identity)) or ((al: ((asocial or antisocial* or dissocial* or psychopath* or sadist* or sociopath*))) and al: ((person*)) and or (al: ((moral and insanity)) or ((al: ((psychopath* or sociopath* or dissocial* or sadis* or schizotypal self-defeating or borderline or avoidant or dependent or depressive))) and al: (person*) or ((al: ((histrionic or multi-impulsive or multiple or narcissistic or passive-aggressive))) and al: (person*) and ((al: ((randomi* or crossover or random-assignment))) or al: (((singl* or doubl* or tripl*or trebl*) and (mask* or blind*)))
Appendix 4. COPAC search strategy
We searched the Consortium of University Research Libraries joint catalogue in September 2009 using the following terms:
randomi* OR ((double OR single OR triple OR treble) and blind) OR prospective OR (clinical and trial)
We then downloaded results into a Procite5 database and searched again using the terms:
(antisocial* OR asocial* OR avoidant OR borderline OR dependent OR depressive OR dissocial OR dissocial* OR histrionic OR moral OR multi-impulsive OR multiple* OR narcissistic OR parano* OR passive-aggressive OR psychopath* OR sadis* OR schizotypal OR self-defeating OR sociopath*)
Appendix 5. CENTRAL search strategy
We searched CENTRAL 2009, Issue 3, using the following terms:
[(antisocial-personality-disorder*:me OR personality-disorders*:me OR sexual-and-gender-disorders*:me OR multiple-personality-disorder*:me OR paraphilias*:me) OR (multi-impulsive and personality) OR (parano* NEAR person*) OR (asocial* NEAR person) OR (dissocial* NEAR person) OR (psychopath* NEAR person) OR (sadist* NEAR person) OR (sociopath* NEAR person*) OR (moral NEAR insanity) OR ((personality and disorder*) and ((((avoidant OR multiimpulsive) OR narcissistic) OR self-defeating) OR personality)]
Appendix 6. CINAHL search strategy
We searched CINHAL 1982 to September 2009 using the following terms:
exp Personality Disorders/
exp Antisocial Personality Disorder/
exp Borderline Personality Disorder/
exp Compulsive Personality Disorder/
exp Dependent Personality Disorder/
exp Impulse Control Disorders/
exp Passive-Aggressive Personality Disorder/
(histrionic$ adj2 person$).tw.
(parano$ adj2 person$).tw.
(schizo$ adj3 person$).tw.
((asocial$ or antisocial$ or dissocial$ or psychopath$ or sadist$ or sociopath$) adj2 person$).tw.
psychopath.tw.
sociopath.tw.
(moral adj2 insanity).tw.
dyssocial.tw.
(DSM and (Axis and II)).tw.
or/1-16
randomi$.mp. [mp=title, subject heading word, abstract, instrumentation]
clin$.mp. [mp=title, subject heading word, abstract, instrumentation]
trial$.mp. [mp=title, subject heading word, abstract, instrumentation]
(clin$ adj3 trial$).mp. [mp=title, subject heading word, abstract, instrumentation]
singl$.mp. [mp=title, subject heading word, abstract, instrumentation]
doubl$.mp. [mp=title, subject heading word, abstract, instrumentation]
tripl$.mp. [mp=title, subject heading word, abstract, instrumentation]
trebl$.mp. [mp=title, subject heading word, abstract, instrumentation]
mask$.mp. [mp=title, subject heading word, abstract, instrumentation]
blind$.mp. [mp=title, subject heading word, abstract, instrumentation]
(22 or 23 or 24 or 25) and (26 or 27)
crossover.mp. [mp=title, subject heading word, abstract, instrumentation]
random$.mp. [mp=title, subject heading word, abstract, instrumentation]
allocate$.mp. [mp=title, subject heading word, abstract, instrumentation]
assign$.mp. [mp=title, subject heading word, abstract, instrumentation]
(random$ adj3 (allocate$ or assign$)).mp.
Random Assignment/
exp Clinical Trials/
exp Meta Analysis/
33 or 29 or 28 or 21 or 18 or 34 or 35 or 36
17 and 37
Appendix 7. EMBASE search strategy
We searched EMBASE (1980 to 37th week 2009) using the following terms:
exp Personality Disorder/
exp Borderline State/
exp Character Disorder/
exp Compulsive Personality Disorder/
exp DELUSION/
exp Dependent Personality Disorder/
exp DEPERSONALIZATION/
exp JEALOUSY/
exp KLEPTOMANIA/
exp Multiple Personality/
exp NARCISSISM/
exp PSYCHOPATHY/
exp SCHIZOIDISM/
exp SOCIOPATHY/
(antisoci$ adj2 person$).tw.
(aggres$ adj2 person$).tw.
(border$ adj2 person$).tw.
histrion$ person$.tw.
paranoid person$.tw.
(passive adj2 aggressive).tw.
((asocial$ or antisocial$ or dissocial$ or psychopath$ or sadist$ or sociopath$) adj person$).tw.
(moral adj2 insan$).tw.
dyssocial.tw.
(DSM and (Axis and II)).tw.
or/1-24
clin$.tw.
trial$.tw.
(clin$ adj3 trial$).tw.
singl$.tw.
doubl$.tw.
trebl$.tw.
tripl$.tw.
blind$.tw.
mask$.tw.
((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
randomi$.tw.
random$.tw.
allocat$.tw.
assign$.tw.
(random$ adj3 (allocat$ or assign$)).tw.
crossover.tw.
41 or 40 or 36 or 35 or 28
exp Randomized Controlled Trial/
exp Double Blind Procedure/
exp Crossover Procedure/
exp Single Blind Procedure/
exp RANDOMIZATION/
43 or 44 or 45 or 46 or 47 or 42
25 and 48
Appendix 8. NATIONAL CRIMINAL JUSTICE REFERENCE SERVICE ABSTRACTS search strategy
We searched NCJRS 1970 to July 2008 using the phrase:
(randomi* OR double blind) and (antisocial* OR asocial* OR avoidant OR borderline OR dependent OR depressive OR dissocial OR dissocial* OR histrionic OR moral OR multiimpulsive OR multiple* OR narcissistic OR parano* OR passiveaggressive OR psychopath* OR sadis* OR schizotypal OR selfdefeating OR sociopath*)
Appendix 9. PsycINFO search strategy
We searched PsycINFO 1872 to 2nd week September 2009 using the following terms:
Personality Disorders/
exp Antisocial Personality Disorder/
exp Avoidant Personality Disorder/
exp Borderline Personality Disorder/
exp Dependent Personality Disorder/
exp Histrionic Personality Disorder/
exp Narcissistic Personality Disorder/
exp Obsessive Compulsive Personality Disorder/
exp Paranoid Personality Disorder/
exp Passive Aggressive Personality Disorder/
exp Sadomasochistic Personality/
exp Schizoid Personality Disorder/
exp Schizotypal Personality Disorder/
(personality adj disorders).tw.
(antisocial adj personality).tw.
(avoidant adj personality).tw.
(borderline adj personality).tw.
(dependent adj personality).tw.
(histrionic adj (personality and disorder)).tw.
(narcissistic adj personality).tw.
(obsessive adj (compulsive and personality)).tw.
(paranoid adj personality).tw.
(passive adj (aggressive and personality)).tw.
(sadomasochistic adj personality).tw.
(schizoid adj personality).tw.
(schizotypal adj personality).tw.
or/1-26
randomi$.tw.
singl$.tw.
doubl$.tw.
trebl$.tw.
tripl$.tw.
blind$.tw.
mask$.tw.
(or/29-32) adj3 (or/33-34)
clin$.tw.
trial$.tw.
(clin$ adj3 trial$).tw.
placebo$.tw.
exp PLACEBO/
crossover.tw.
exp Treatment Effectiveness Evaluation/
exp Mental Health Program Evaluation/
random$.tw.
assign$.tw.
allocate$.tw.
(random$ adj3 (assign$ or allocate$)).tw.
27 or 35 or 38 or 39 or 40 or 41 or 42 or 43 or 47
27 and 48
Appendix 10. SIGLE search strategy
We searched SIGLE 1980 to April 2006 using the following terms:
((randomisation) OR (randomised) OR (randomisee) OR (randomises) OR (randomize) OR (randomized) OR (randomly) OR ((double AND blind) OR double-blind OR double* blind* OR randomi?ed controlled trials)) AND ((psychopath* OR sociopath* OR dissocial OR sadis* OR schizotypal OR selfdefeating OR borderline OR avoidant OR dependent OR depressive OR histrionic OR multi-impulsive OR multiple OR narcissistic OR passive-aggressive) AND (person*) OR (antisocial AND behaviour) OR (personality AND disorder*) OR (gender AND identity) OR (parano* AND person*) OR (self AND defeating) OR ((asocial* OR antisocial* OR dissocial* OR psychopath* OR sadist* OR sociopath*) AND person*) OR (moral AND insanity))
Appendix 11. SOCIOLOGICAL ABSTRACTS search strategy
We searched SOCIOLOGICAL ABSTRACTS 1963 to September 2009 using the following terms:
((personality near disorder*) or ((antisocial* near disorder*) or (avoidant* near disorder*) or (bordeline* near disorder*)) or ((dependent* near disorder*) or (histrionic* near disorder*) or (narcissistic* near disorder*)) or ((obsessive* near disorder*) or (compulsive* near disorder*) or (paranoid* near disorder*)) or (((passive* near disorder*) or (aggress* near disorder*) or (sadomasochistic* near disorder*)) or (schizo* near disorder*)) or (((passive* and disorder*) or (aggress* and disorder*) or (sadomasochistic* and disorder*)) or ((schizo* and disorder*) or (paranoid* and disorder*) or (compulsive* and disorder*)) or ((obsessive* and disorder*) or (narcissistic and disorder*) or (histrionic* and disorder*))) or (((personality and disorder*) or (antisocial* and disorder*) or (avoidant* and disorder*)) or ((borderline* and disorder*) or (dependent* and disorder*)))) and ((AB=randomi* or TI=randomi*) or (DE=(randomi?ed controlled trials) or AB= (double* blind*) or TI=(double* blind*)) or (DE=(double blind studies) or (single* near blind*)))
Appendix 12. WEB OF SCIENCE search strategy
We searched the Web of Science 1981 to 12 September 2009 using the following terms:
(double blind OR randomi*) AND ((passive-aggressive OR psychopath* OR sociopath* OR dissocial OR sadis* OR schizotypal OR self-defeating OR borderline OR avoidant OR dependent OR depressive OR parano* OR asocial* OR antisocial* OR dissocial* OR psychopath* OR sadist* OR sociopath* OR histrionic OR multi-impulsive OR multiple* OR narcissistic) AND personality*) OR ((moral AND insanity) OR (self AND defeating) OR (gender AND identity) OR (personality AND disorder) OR (antisocial AND behaviour))
HISTORY
Protocol first published: Issue 1, 2009
Review first published: Issue 6, 2010
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
The review differs from the original protocol in four ways:
An additional restriction was added to the Selection of studies section to apply to studies where participants with antisocial or dissocial personality disorder formed a small subgroup. This required that studies included in the review should have randomised at least five people with antisocial or dissocial personality disorder. The rationale is that variance and standard deviation cannot be calculated in samples of two or less, and so a two-condition study randomising less than five (relevant) participants will have at least one arm for which standard deviation cannot be calculated.
The outcome of substance misuse (as specified a priori in the section on Secondary outcomes in the protocol) was modified so that a reader would find it easier to differentiate drug misuse outcomes from alcohol misuse outcomes. It has been replaced by two separate categories: substance misuse (drugs) and substance misuse (alcohol).
Skewed data are reported in separate tables as specified in the original protocol (see Measures of treatment effect). However, where the trial investigators provide results of their own statistical analysis on such data, we report their results descriptively within the section on Effects of interventions.
Where investigators did not provide standard deviations for a continuous outcome, these were calculated where possible from standard errors, confidence intervals, t-values, F values or P values using the method described in the Cochrane Handbook for Systematic Reviews of Interventions, section 7.7.3.3 (Higgins 2008)).
The review omits six analyses specified in the original protocol because of insufficient data (see Table 4). These were:
subgroup analysis of effect on primary outcomes of comorbid diagnosis, setting, category of intervention, and whether group-based or individual-based;
sensitivity analysis to investigate the robustness of findings concerning concealment of allocation, blinding of outcome assessors, and extent of drop-outs;
assessment of the extent to which the results of the review could be altered by the missing data by sensitivity analysis based on consideration of ‘best-case’ and ‘worst-case’ scenarios;
sensitivity analysis of the impact of including studies with high attrition rates (25% to 50%);
drawing of funnel plots of effect size versus standard error to assess for possible publication bias; and
grouping of outcome measures by length of follow up.
Footnotes
DECLARATIONS OF INTEREST
Conor Duggan: Chair, UK National Institute of Clinical Excellence Committee on antisocial personality disorder; advisor to a current randomised controlled trial of schema focused therapy at Ashworth High Secure Hospital, UK; investigator in a completed randomised controlled trial of social problem-solving therapy plus psychoeducation for people with personality disorder (Huband 2007).
Nick Huband: investigator in a completed randomised controlled trial of social problem-solving therapy plus psychoeducation for people with personality disorder (Huband 2007); because this study was included in this review, NH and CD excluded themselves from data extraction and summarising the risk of bias for this trial.
Klaus Lieb: Chair, Department of Psychiatry and Psychotherapy, University Medical Center, Mainz; advisor to a planned randomised controlled trial of inpatient schema therapy in patients with personality disorders.
References to studies included in this review
- Ball 2005 {published data only} .Ball SA, Cobb-Richardson P, Connolly AJ, Bujosa CT, O’Neall TW. Substance abuse and personality disorders in homeless drop-in center clients: symptom severity and psychotherapy retention in a randomized clinical trial. Comprehensive Psychiatry. 2005;46(5):371–9. doi: 10.1016/j.comppsych.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Davidson 2009 {published data only} .Davidson KM, Tyrer P, Tata P, Cooke D, Gumley A, Ford I, et al. Cognitive behaviour therapy for violent men with antisocial personality disorder in the community: an explanatory randomized controlled trial. Psychological Medicine. 2009;39:569–77. doi: 10.1017/S0033291708004066. [DOI] [PubMed] [Google Scholar]
- Havens 2007 {published data only} .*; Havens JR, Cornelius LJ, Ricketts EP, Latkin CA, Bishai D, Lloyd JJ, et al. The effect of a case management intervention on drug treatment entry among treatment-seeking injection drug users with and without comorbid antisocial personality disorder. Journal of Urban Health. 2007;84(2):267–71. doi: 10.1007/s11524-006-9144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Ricketts EP, Huettner S, Cornelius L, Bishai D, Havens JR, et al. Facilitating entry into drug treatment among injection drug users referred from a needle exchange program: results from a community-based behavioral intervention trial. Drug and Alcohol Dependence. 2006;83:225–32. doi: 10.1016/j.drugalcdep.2005.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huband 2007 {published data only} .Huband N, McMurran M, Evans C, Duggan C. Social problem-solving plus psychoeducation for adults with personality disorder: pragmatic randomised controlled trial. British Journal of Psychiatry. 2007;190:307–13. doi: 10.1192/bjp.bp.106.023341. [DOI] [PubMed] [Google Scholar]
- Marlowe 2007 {published data only} .Marlowe DB, Festinger DS, Dugosh KL, Lee PA, Benasutti KM. Adapting judicial supervision to the risk level of drug offenders: discharge and 6-month outcomes from a prospective matching study. Drug and Alcohol Dependence. 2007;88(Suppl 2):S4–S13. doi: 10.1016/j.drugalcdep.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay 2000 {published data only} .*; McKay JR, Alterman AI, Cacciola JS, Mulvaney FD, O’Brien CH. Prognostic significance of antisocial personality disorders in cocaine-dependent patients entering continuing care. Journal of Nervous & Mental Disease. 2000;188:287–96. doi: 10.1097/00005053-200005000-00006. [DOI] [PubMed] [Google Scholar]
- McKay JR, Alterman AI, Cacciola JS, Rutherford MJ, O’Brian CP, Koppenhaver J. Group counselling vs. individualized relapse prevention aftercare following intensive outpatient treatment for cocaine-dependence: initial results. Journal of Consulting and Clinical Psychology. 1997;65:778–88. doi: 10.1037//0022-006x.65.5.778. [DOI] [PubMed] [Google Scholar]
- Messina 2003 {published data only} .Messina N, Farabee D, Rawson R. Treatment responsivity of cocaine-dependent patients with antisocial personality disorder to cognitive-behavioral and contingency management interventions. Journal of Consulting & Clinical Psychology. 2003;71(2):320–30. doi: 10.1037/0022-006x.71.2.320. [DOI] [PubMed] [Google Scholar]
- Neufeld 2008 {published data only} .Brooner RK, Kidorf M, King VL, Stoller K. Preliminary evidence of good treatment response in antisocial drug abusers. Drug and Alcohol Dependence. 1998;49:249–60. doi: 10.1016/s0376-8716(98)00018-0. [DOI] [PubMed] [Google Scholar]
- *; Neufeld KJ, Kidorf MS, Kolodner K, King VL, Clark M, Brooner RK. A behavioral treatment for opioid-dependent patients with antisocial personality. Journal of Substance Abuse Treatment. 2008;34:101–11. doi: 10.1016/j.jsat.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrer 2004 {published data only} .Tyrer P, Tom B, Byford S, Schmidt U, Jones V, Davidson K, et al. Differential effects of manual assisted cognitive behavior therapy in the treatment of recurrent deliberate self-harm and personality disturbance: the POPMACT study. Journal of Personality Disorders. 2004;18(1):102–16. doi: 10.1521/pedi.18.1.102.32770. [DOI] [PubMed] [Google Scholar]
- Woodall 2007 {published data only} .Woodall WG, Delaney HD, Kunitz SJ, Westerberg VS, Zhao H. A randomized trial of a DWI intervention program for first offenders: intervention outcomes and interactions with antisocial personality disorder among a primarily American-Indian sample. Alcoholism, Clinical and Experimental Research. 2007;31(6):974–87. doi: 10.1111/j.1530-0277.2007.00380.x. [DOI] [PubMed] [Google Scholar]
- Woody 1985 {published data only} .Luborsky L, McLellan AT, Woody GE, O’Brien CP, Auerbach A. Therapist success and its determinants. Archives of General Psychiatry. 1985;42:602–11. doi: 10.1001/archpsyc.1985.01790290084010. [DOI] [PubMed] [Google Scholar]
- Woody GE, McLellan AT, Luborsky L, O’Brien CP. Sociopathy and psychotherapy outcome. Archives of General Psychiatry. 1985;42(11):1081–6. doi: 10.1001/archpsyc.1985.01790340059009. [DOI] [PubMed] [Google Scholar]
- Woody GE, McLellan AT, Luborsky L, O’Brien CP, Beck AT, Blaine J, et al. Psychotherapy for opiate addicts. Archives of General Psychiatry. 1983;40:639–45. doi: 10.1001/archpsyc.1983.04390010049006. [DOI] [PubMed] [Google Scholar]
- Woody GE, McLellan AT, Luborsky L, O’Brien CP, Blaine J, Fox S, et al. Severity of psychiatric symptoms as a predictor of benefits from psychotherapy: the Veterans Administration-Penn study. American Journal of Psychotherapy. 1984;141:1172–7. doi: 10.1176/ajp.141.10.1172. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Abbass 2008 {published data only} .Abbass A, Sheldon A, Gyra J, Kalpin A. Intensive short-term dynamic psychotherapy for DSM-IV personality disorders: a randomized controlled trial. Journal of Nervous & Mental Disease. 2008;196(3):211–6. doi: 10.1097/NMD.0b013e3181662ff0. [DOI] [PubMed] [Google Scholar]
- Arnevik 2009 {published data only} .Arnevik E, Wilberg T, Urnes O, Johansen M, Monsen JT, Karterud S. Psychotherapy for personality disorders: short-term day hospital psychotherapy versus outpatient individual therapy - a randomized controlled study. European Psychiatry. 2009;24(2):71–8. doi: 10.1016/j.eurpsy.2008.09.004. [DOI] [PubMed] [Google Scholar]
- Bagby 2008 {published data only} .Bagby RM, Quilty LC, Segal ZV, McBride CC, Kennedy SH, Costa PT. Personality and differential treatment response in major depression: a randomized controlled trial comparing cognitive-behavioural therapy and pharmacotherapy. Canadian Journal of Psychiatry. 2009;53(6):361–70. doi: 10.1177/070674370805300605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball 2007 {published data only} .Ball SA. Comparing individual therapies for personality disordered opioid dependent patients. Journal of Personality Disorders. 2007;21(3):305–21. doi: 10.1521/pedi.2007.21.3.305. [DOI] [PubMed] [Google Scholar]
- Chiesa 2003 {published data only} .Chiesa M, Fonagy P. Psychosocial treatment for severe personality disorder: 36 month follow-up. British Journal of Psychiatry. 2003;183:356–62. doi: 10.1192/bjp.183.4.356. [DOI] [PubMed] [Google Scholar]
- Colom 2004 {published data only} .Colom F, Vieta E, Sanchez-Moreno J, Martinez-Aran A, Torrent C, Reinares M, et al. Psychoeducation in bipolar patients with comorbid personality disorders. Bipolar Disorders. 2004;6(4):294–8. doi: 10.1111/j.1399-5618.2004.00127.x. [DOI] [PubMed] [Google Scholar]
- Daughters 2008 {published data only} .Daughters SB, Stipelman BA, Sargeant MN, Schuster R, Bornovalova MA, Lejuez CW. The interactive effects of antisocial personality disorder and court-mandated status on substance abuse treatment dropout. Journal of Substance Abuse Treatment. 2008;34(2):157–64. doi: 10.1016/j.jsat.2007.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easton 2007 {published data only} .Easton CJ, Babuscio T, Carroll KM. Treatment retention and outcome among cocaine-dependent patients with and without active criminal justice involvement. Journal of the American Academy of Psychiatry and the Law. 2007;35(1):83–91. [PubMed] [Google Scholar]
- Fournier 2008 {published data only} .Fournier JC, DeRubeis RJ, Shelton RC, Gallop R, Amsterdam JD, Hollon S. Antidepressant medications v. cognitive therapy in people with depression with or without personality disorder. British Journal of Psychiatry. 2008;192(2):124–9. doi: 10.1192/bjp.bp.107.037234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesselbrock 1991 {published data only} .M Hesselbrock. Gender comparison of antisocial personality disorder and depression in alcoholism. Journal of Substance Abuse. 1991;3:205–19. doi: 10.1016/s0899-3289(05)80037-9. [DOI] [PubMed] [Google Scholar]
- Kallert 2007 {published data only} .Kallert TW, Priebe S, McCabe R, Kiejna A, Rymaszewska J, Nawka P, et al. Are day hospitals effective for acutely ill psychiatric patients? A European multicenter randomized controlled trial. Journal of Clinical Psychiatry. 2007;68(2):278–97. doi: 10.4088/jcp.v68n0214. [DOI] [PubMed] [Google Scholar]
- Kelly 2009 {published data only} .Kelly BD, Nur UA, Tyrer P, Casey P. Impact of severity of personality disorder on the outcome of depression. European Psychiatry. 2009;24(5):322–6. doi: 10.1016/j.eurpsy.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Kool 2003 {published data only} .Kool S, Dekker J, Duijsens IJ, Jonghe F, Puite B. Efficacy of combined therapy and pharmacotherapy for depressed patients with and without personality disorders. Harvard Review of Psychiatry. 2003;11(3):133–41. doi: 10.1080/10673220303950. [DOI] [PubMed] [Google Scholar]
- Kool 2007 {published data only} .Kool S, Schoevers R, Duijsens IJ, Peen J, Van AAlst G, De Jonghe F, et al. Treatment of depressive disorder and comorbid personality pathology: combined therapy versus pharmacotherapy [Dutch] Tijdschrift voor Psychiatrie. 2007;49(6):361–72. [PubMed] [Google Scholar]
- Liberman 1981 {published data only} .Liberman RP, Eckman T. Behavior therapy vs insight-oriented therapy for repeated suicide attempters. Archives of General Psychiatry. 1981;38:1127–30. doi: 10.1001/archpsyc.1981.01780350060007. [DOI] [PubMed] [Google Scholar]
- Longabaugh 1994 {published data only} .Longabaugh R, Rubin A, Malloy P, Beattie M, Clifford PR, Noel N. Drinking outcomes of alcohol abusers diagnosed as antisocial personality disorder. Alcoholism: Clinical & Experimental Research. 1994;18(4):778–85. doi: 10.1111/j.1530-0277.1994.tb00040.x. [DOI] [PubMed] [Google Scholar]
- Lynch 2007 {published data only} .Lynch TR, Cheavens JS, Cukrowicz KC, Thorp SR, Bronner L, Beyer J. Treatment of older adults with comorbid personality disorder and depression: a dialectical behavior therapy approach. International Journal of Geriatric Psychiatry. 2007;22(2):131–43. doi: 10.1002/gps.1703. [DOI] [PubMed] [Google Scholar]
- Messina 2002 {published data only} .Messina NP, Wish ED, Hoffman JA, Nemes S. Antisocial personality disorder and TC treatment outcomes. American Journal of Drug and Alcohol Abuse. 2002;28(2):197–212. doi: 10.1081/ada-120002970. [DOI] [PubMed] [Google Scholar]
- Milrod 2007 {published data only} .Milrod BI, Leon AC, Barber JP, Markowitz JC, Graf E. Do comorbid personality disorders moderate panic-focused psychotherapy? An exploratory examination of the American Psychiatric Association practice guideline. Journal of Clinical Psychiatry. 2007;68(6):885–91. doi: 10.4088/jcp.v68n0610. [DOI] [PubMed] [Google Scholar]
- Mortberg 2007 {published data only} .Mortberg E, Bejerot S, Wistedt AA. Temperament and character dimensions in patients with social phobia: patterns of change following treatments? Psychiatry Research. 2007;152(1):81–90. doi: 10.1016/j.psychres.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Muran 2009 {published data only} .Muran JC, Safran JD, Gorman BS, Samstag LW, Eubanks-Carter C, Winston A. The relationship of early alliance ruptures and their resolution to process and outcome in three time-limited psychotherapies for personality disorders. Psychotherapy: Theory, Research, Practice, Training. 2009;46(2):233–48. doi: 10.1037/a0016085. [DOI] [PubMed] [Google Scholar]
- Petersen 2008 {published data only} .Petersen B, Toft J, Christensen NB, Foldager L, Munk-Jorgensen P, Lien K, et al. Outcome of a psychotherapeutic programme for patients with severe personality disorders. Nordic Journal of Psychiatry. 2008;62(6):450–6. doi: 10.1080/08039480801984271. [DOI] [PubMed] [Google Scholar]
- Sloane 1976 {published data only} .Sloane RB, Staples FR, Cristol AH, Yorkston NJ, Whipple K. Patient characteristics and outcome in psychotherapy and behavior therapy. Journal of Consulting and Clinical Psychology. 1976;44(3):330–9. doi: 10.1037//0022-006x.44.3.330. [DOI] [PubMed] [Google Scholar]
- Springer 1995 {published data only} .Springer T, Lohr NE, Buchtel HA, Silk KR. A preliminary report of short-term cognitive-behavioral group therapy for inpatients with personality disorders. Journal of Psychotherapy Practice and Research. 1995;5(1):57–71. [PMC free article] [PubMed] [Google Scholar]
- Tyrer 2009 {published data only} .Tyrer P, Cooper S, Rutter D, Seivewright H, Duggan C, Maden T, et al. The assessment of dangerous and severe personality disorder: lessons from a randomised controlled trial linked to qualitative analysis. Journal of Forensic Psychiatry and Psychology. 2009;20(1):132–46. [Google Scholar]
- Vannoy 2004 {published data only} .Vannoy SD, Hoyt WT. Evaluation of an anger therapy intervention for incarcerated adult males. Journal of Offender Rehabilitation. 2004;39:39–57. [Google Scholar]
- Vera 2008 {published data only} .Vera L, Mirabel-Sarron C, Ba K. Cognitive and behavioral therapy of obsessive and compulsive troubles with associated personality troubles: group therapy. Annales Medico-Psychologiques. 2008;166(8):673–6. [Google Scholar]
- Vinnars 2005 {published data only} .Vinnars B, Barber JP, Noren K, Gallop R, Weinryb RM. Manualized supportive-expressive psychotherapy versus nonmanualized community-delivered psychodynamic therapy for patients with personality disorders: bridging efficacy and effectiveness. American Journal of Psychiatry. 2005;162(10):1933–40. doi: 10.1176/appi.ajp.162.10.1933. [DOI] [PubMed] [Google Scholar]
- Vinnars 2007 {published data only} .Vinnars B, Barber JP, Noren K, Thormahlen B, Gallop R, Lindgren A, et al. Who can benefit from time-limited dynamic psychotherapy? A study of psychiatric outpatients with personality disorders. Clinical Psychology and Psychotherapy. 2007;14(3):198–210. [Google Scholar]
- Vinnars 2009 {published data only} .Vinnars B, Thormahlen B, Gallop R, Noren K, Barber JP. Do personality problems improve during psychodynamic supportive-expressive psychotherapy? Secondary outcome results from a randomized controlled trial for psychiatric outpatients with personality disorders. Psychotherapy: Theory, Research, Practice, Training. 2009;46(3):362–75. doi: 10.1037/a0017002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weertman 2007 {published data only} .Weertman A, Arntz A. Effectiveness of treatment of childhood memories in cognitive therapy for personality disorders: a controlled study contrasting methods focusing on the present and methods focusing on childhood memories. Behaviour Research & Therapy. 2007;45(9):2133–43. doi: 10.1016/j.brat.2007.02.013. [DOI] [PubMed] [Google Scholar]
- Winston 1994 {published data only} .Winston A, Laikin M, Pollack J, Samstag LW, McCullough L, Muran JC. Short-term psychotherapy of personality disorders. American Journal of Psychiatry. 1994;151(2):190–4. doi: 10.1176/ajp.151.2.190. [DOI] [PubMed] [Google Scholar]
- Wolwer 2001 {published data only} .Wolwer W, Burtscheidt W, Redner C, Schwarz R, Gaebel W. Out-patient behaviour therapy in alcoholism: impact of personality disorders and cognitive impairments. Acta Psychiatrica Scandinavica. 2001;103:30–7. doi: 10.1034/j.1600-0447.2001.00149.x. [DOI] [PubMed] [Google Scholar]
- Zorn 2007 {published data only} .Zorn P, Roder V, Muller DR, Tschacher W, Thommen M. Schema Focused Emotive Behavioural Therapy (‘SET’): a randomised controlled trial on patients with cluster B and C personality disorders. Verhaltenstherapie. 2007;17(4):233–41. [Google Scholar]
References to studies awaiting assessment
- Berget 2008 {published data only} .Berget B, Ekeberg O, Braastad BO. Animal-assisted therapy with farm animals for persons with psychiatric disorders: effects on self-efficacy, coping ability and quality of life, a randomized controlled trial. Clinical Practice and Epidemiology in Mental Health. 2008;4(9):1–7. doi: 10.1186/1745-0179-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans 1999 {published data only} .Evans K, Tyrer P, Catalan J, Schmidt U, Davidson K, Dent J, et al. Manual-assisted cognitive-behaviour therapy (MACT): a randomized controlled trial of a brief intervention with bibliotherapy in the treatment of recurrent deliberate self-harm. Psychological Medicine. 1999;29(1):19–25. doi: 10.1017/s003329179800765x. [DOI] [PubMed] [Google Scholar]
- Linehan 2006 {published data only} .Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomised controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry. 2006;63(7):757–66. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
Additional references
- Altman 1996 .Altman DG, Bland JM. Detecting skewedness from summary information. BMJ. 1996;313(7066):1200. doi: 10.1136/bmj.313.7066.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aos 2001 .Aos S, Phipps P, Barnoski R, Leib R. The comparative costs and benefits of programs to reduce crime. Washington State Institute for Public Policy; Olympia, WA: 2001. http://www.wa.gov/wsipp. [Google Scholar]
- APA 2000 .American Psychiatric Association . DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders: Text Revision. American Psychiatric Association; Arlington, Virginia, USA: 2000. [Google Scholar]
- Attkisson 1982 .Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning. 1982;5:233–7. doi: 10.1016/0149-7189(82)90074-x. [DOI] [PubMed] [Google Scholar]
- Bateman 2001 .Bateman P, Fonagy P. Treatment of borderline personality disorder with psychoanalytically orientated partial hospitalisation: an 18 month follow-up. American Journal of Psychiatry. 2001;158:36–42. doi: 10.1176/appi.ajp.158.1.36. [DOI] [PubMed] [Google Scholar]
- Bateman 2004 .Bateman AW, Tyrer P. Psychological treatment for personality disorders. Advances in Psychiatric Treatment. 2004;10:378–88. [Google Scholar]
- Black 1996 .Black DW, Baumgard CH, Bell SE, Kao C. Death rates in 71 men with antisocial personality disorder: A comparison with general population mortality. Psychosomatics. 1996;37(2):131–6. doi: 10.1016/S0033-3182(96)71579-7. [DOI] [PubMed] [Google Scholar]
- Brooner 1998 .Brooner RK, Kidorf M, King VL, Stoller K. Preliminary evidence of good treatment response in antisocial drug abusers. Drug and Alcohol Dependence. 1998;49:249–60. doi: 10.1016/s0376-8716(98)00018-0. [DOI] [PubMed] [Google Scholar]
- Buss 1992 .Buss AH, Perry M. The Aggression Questionnaire. Journal of Personality and Social Psychology. 1992;63:452–9. doi: 10.1037//0022-3514.63.3.452. [DOI] [PubMed] [Google Scholar]
- Campbell 2000 .Campbell M, Fitzpatrick R, Haines A, Kinmouth AL, Sandercock P, Spiegelhalter D, et al. A framework for the design and evaluation of complex interventions to improve health. BMJ. 2000;321:694–6. doi: 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campling 2001 .Campling P. Therapeutic communities. Advances in Psychiatric Treatment. 2001;7:365–72. [Google Scholar]
- Carroll 2004 .Carroll KM, Fenton LR, Ball SA, Nich C, Frankforter TL, Shi J, et al. Efficacy of disulfiram and cognitive behavior therapy in cocaine-dependent outpatients. Archives of General Psychiatry. 2004;61:264–72. doi: 10.1001/archpsyc.61.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll 1998 .Carroll KM, Nich C, Ball SA, McCance E, Rounsavile BJ. Treatment of cocaine and alcohol dependence with psychotherapy and disulfiram. Addiction. 1998;93(5):713–28. doi: 10.1046/j.1360-0443.1998.9357137.x. [DOI] [PubMed] [Google Scholar]
- Chiesa 2003 .Chiesa M, Fonagy P, Holmes J. Psychosocial treatment for severe personality disorder: a 36 month follow-up. British Journal of Psychiatry. 2003;183:356–62. doi: 10.1192/bjp.183.4.356. [DOI] [PubMed] [Google Scholar]
- Coid 2006 .Coid J, Yang M, Tyrer P, Roberts A, Ullrich S. Prevalence and correlates of personality disorder in Great Britain. British Journal of Psychiatry. 2006;188:423–31. doi: 10.1192/bjp.188.5.423. [DOI] [PubMed] [Google Scholar]
- Cordess 1996 .Cordess C, Cox M. Forensic psychotherapy: Crime, psychodynamics and the offender patient. Vol. 2. Jessica Kingsley; London: 1996. [Google Scholar]
- Davies 2007 .Davies S, Clarke M, Hollin C, Duggan C. Long-term outcomes after discharge from medium secure care: a cause for concern. British Journal of Psychiatry. 2007;191:70–4. doi: 10.1192/bjp.bp.106.029215. [DOI] [PubMed] [Google Scholar]
- Denman 2001 .Denman C. Cognitive analytic therapy. Advances in Psychiatric Treatment. 2001;7:243–56. [Google Scholar]
- Dolan 1993 .Dolan B, Coid J. Psychopathic and anti-social personality disorders: treatment and research Issues. Gaskell; London: 1993. [Google Scholar]
- Dolan 2009 .Dolan M, Völlm B. Antisocial personality disorder and psychopathy in women: a literature review on the reliability and validity of assessment instruments. International Journal of Law and Psychiatry. 2009;32(1):2–9. doi: 10.1016/j.ijlp.2008.11.002. [DOI] [PubMed] [Google Scholar]
- Donner 2001 .Donner A, Piaggio G, Villar J. Statistical methods for the meta-analysis of cluster randomization trials. Statistical Methods in Medical Research. 2001;10(5):325–38. doi: 10.1177/096228020101000502. [DOI] [PubMed] [Google Scholar]
- Duggan 2007 .Duggan C, Huband N, Smailagic N, Ferriter M, Adams C. The use of psychological treatments for people with personality disorder: a systematic review of randomized controlled trials. Journal of Personality and Mental Health. 2007;1:95–125. [Google Scholar]
- Duke 1994 .Duke PJ, Pantelis C, Barnes TRE. South Westminster Schizophrenia Survey. Alcohol use and its relationship to symptoms, tardive dyskinesia and illness onset. British Journal of Psychiatry. 1994;164:630–6. doi: 10.1192/bjp.164.5.630. [DOI] [PubMed] [Google Scholar]
- Egger 1997 .Egger M, Davey-Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EuroQoL group 1990 .EuroQoL Group EuroQoL: a new facility for measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- Follman 1992 .Follmann D, Elliot P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. Journal of Clinical Epidemiology. 1992;45(7):769–93. doi: 10.1016/0895-4356(92)90054-q. [DOI] [PubMed] [Google Scholar]
- Gamble 2005 .Gamble C, Hollis S. Uncertainty method on best-worst case analysis in a binary meta-analysis. Journal of Clinical Epidemiology. 2005;58(6):579–88. doi: 10.1016/j.jclinepi.2004.09.013. [DOI] [PubMed] [Google Scholar]
- Grilo 1998 .Grilo CM, McGlashan TH, Oldham JM. Course and stability of personality disorders. Journal of Practical Psychiatry and Behavioural Health. 1998;4:61–75. [Google Scholar]
- Higgins 2008 .Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0. The Cochrane Collaboration; [accessed 1 April 2008]. 2008. Available from www.cochrane-handbook.org. [Google Scholar]
- Home Office 1999 .Home Office . Reconviction of offenders sentenced or discharged from prison in 1994, England and Wales: Home Office Statistical Bulletin 5/99. Home Office; London: 1999. [Google Scholar]
- Huband 2007 .Huband N, McMurran M, Evans C, Duggan C. Social problem-solving plus psychoeducation for adults with personality disorder: pragmatic randomised controlled trial. British Journal of Psychiatry. 2007;190:307–13. doi: 10.1192/bjp.bp.106.023341. [DOI] [PubMed] [Google Scholar]
- Lees 1999 .Lees J, Manning N, Rawlings B. Therapeutic effectiveness: a systematic international review of therapeutic community treatment for people with personality disorder and mentally disordered offenders (CRD report 17) University of York NHS Centre for Reviews and Dissemination; York: 1999. [Google Scholar]
- Linehan 1993 .Linehan MM. The skills training manual for treating borderline personality disorder. Guilford Press; New York: 1993. [Google Scholar]
- Livesley 2007 .Livesley W. A framework for integrating dimensional and categorical classifications of personality disorder. Journal of Personality Disorders. 2007;21(2):199–224. doi: 10.1521/pedi.2007.21.2.199. [DOI] [PubMed] [Google Scholar]
- Malone 1994 .Malone RP, Luebbert RP, Pena-Ariet M, Biesecker K, Delaney MA. The Overt Aggression Scale in the study of lithium in aggressive conduct disorder. Psychopharmacology Bulletin. 1994;30:215–8. [PubMed] [Google Scholar]
- McKay 1997 .McKay JR, Alterman AI, Cacciola JS, Rutherford MJ, O’Brian CP, Koppenhaver J. Group counselling vs. individualized relapse prevention aftercare following intensive outpatient treatment for cocaine-dependence: initial results. Journal of Consulting and Clinical Psychology. 1997;65:778–88. doi: 10.1037//0022-006x.65.5.778. [DOI] [PubMed] [Google Scholar]
- Moran 1999 .Moran P. The epidemiology of antisocial personality disorder. Social Psychiatry and Psychiatric Epidemiology. 1999;34(5):231–42. doi: 10.1007/s001270050138. [DOI] [PubMed] [Google Scholar]
- Myers 1998 .Myers MG, Stewart DG, Brown SA. Progression from conduct disorder to antisocial personality disorder following treatment for adolescent substance abuse. American Journal of Psychiatry. 1998;155:479–85. doi: 10.1176/ajp.155.4.479. [DOI] [PubMed] [Google Scholar]
- Newton-Howes 2006 .Newton-Howes G, Tyrer P, Johnson T. Personality disorder and the outcome of depression: meta-analysis of published studies. British Journal of Psychiatry. 2006;188:13–20. doi: 10.1192/bjp.188.1.13. [DOI] [PubMed] [Google Scholar]
- NIHCE 2007 .National Institute of Health and Clinical Excellence . Drug misuse: opioid detoxification (NICE Guideline 52) National Institute of Health and Clinical Excellence; London: [accessed 29 October 2009]. 2007. www.nice.org.uk/CG52. [Google Scholar]
- NIHCE 2009 .National Institute of Health and Clinical Excellence . Antisocial personality disorder: treatment, management and prevention (NICE Guideline 77) National Institute of Health and Clinical Excellence; London: [(accessed 29/10/2009)]. 2009. www.nice.org.uk/CG77. [Google Scholar]
- ONS 2004 .ONS . Social Trends 34. Office of National Statistics; London: 2004. [Google Scholar]
- Paris 2003 .Paris J. Personality Disorders Over Time: Precursors, Course, and Outcome. American Psychiatric Publishing; Arlington, VA: 2003. [DOI] [PubMed] [Google Scholar]
- Patton 1995 .Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology. 1995;51(6):768–74. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Perdikouri 2007 .Perdikouri M, Rathbone G, Huband N, Duggan C. A comparison of adults with antisocial personality traits with and without childhood conduct disorder. Annals of Clinical Psychiatry. 2007;19(1):17–23. doi: 10.1080/10401230601163501. [DOI] [PubMed] [Google Scholar]
- Piper 1993 .Piper WE, Rosie JS, Azim HF. A randomised trial of psychiatric day treatment for patients with affective and personality disorders. Hospital and Community Psychiatry. 1993;44:757–63. doi: 10.1176/ps.44.8.757. [DOI] [PubMed] [Google Scholar]
- RevMan 2008 .The Nordic Cochrane Centre, The Cochrane Collaboration . Review Manager (RevMan). 5.0. The Nordic Cochrane Centre, The Cochrane Collaboration; Copenhagen: 2008. [Google Scholar]
- Robins 1991 .Robins LN, Tipp J, Przybeck T. Antisocial personality. In: Robins LN, Regier DA, editors. Psychiatric disorders in America. Free Press; New York: 1991. [Google Scholar]
- Scott 2001 .Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ. 2001;323:191–5. doi: 10.1136/bmj.323.7306.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singleton 1998 .Singleton N, Melzer H, Gatward R. Psychiatric morbidity among prisoners in England and Wales. HM Stationery Office; London: 1998. [Google Scholar]
- Skodol 2005 .Skodol AE, Oldham JM, Bender DS, Dyck IR, Stout RL, Morey LC, et al. Dimensional representations of DSM-IV personality disorders: relationships to functional impairment. American Journal of Psychiatry. 2005;162(10):1919–25. doi: 10.1176/appi.ajp.162.10.1919. [DOI] [PubMed] [Google Scholar]
- Spielberger 1999 .Spielberger CD. STAXI-2: State-Trait Anger Expression Inventory-2. Psychological Assessment Resources, Inc.; Odessa, FL: 1999. [Google Scholar]
- Strathdee 2006 .Strathdee SA, Ricketts EP, Huettner S, Cornelius L, Bishai D, Havens JR, et al. Facilitating entry into drug treatment among injection drug users referred from a needle exchange program: results from a community-based behavioral intervention trial. Drug and Alcohol Dependence. 2006;83:225–32. doi: 10.1016/j.drugalcdep.2005.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson 1994 .Swanson MC, Bland RC, Newman SC. Epidemiology of psychiatric disorders in Edmonton: antisocial personality disorders. Acta Psychiatrica Scandinavica. Supplementum. 1994;376:63–70. [PubMed] [Google Scholar]
- Tait 2002 .Tait L, Birchwood M, Trower P. A new scale (SES) to measure engagement with community mental health services. Journal of Mental Health. 2002;11(2):191–8. doi: 10.1080/09638230020023570-2. [DOI] [PubMed] [Google Scholar]
- Torgensen 2001 .Torgensen S. Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Archives of General Psychiatry. 2001;58:590–6. doi: 10.1001/archpsyc.58.6.590. [DOI] [PubMed] [Google Scholar]
- Tyrer 2003 .Tyrer P, Jones V, Thompson S, Catalan J, Schmidt U, Davidson K, et al. Service variation in baseline variables and prediction of risk in a randomised controlled trial of psychological treatment in repeated parasuicide: the POPMACT Study. International Journal of Social Psychiatry. 2003;49(1):58–69. doi: 10.1177/0020764003049001148. [DOI] [PubMed] [Google Scholar]
- Tyrer 2005a .Tyrer P, Bajaj P. Nidotherapy: making the environment do the work. Advances in Psychiatric Treatment. 2005;11:232–8. [Google Scholar]
- Tyrer 2005b .Tyrer P, Nur U, Crawford M. The Social Functioning Questionnaire: a rapid and robust measure of perceived functioning. International Journal of Social Psychiatry. 2005;51:265–75. [PubMed] [Google Scholar]
- Tyrer 2007 .Tyrer P, Kramo K, Miloseka K, Seivewright H. The place for nidotherapy in psychiatric practice. Psychiatric Bulletin. 2007;31:1–3. [Google Scholar]
- Warren 2003 .Warren F, McGauley G, Norton K, Dolan R, Preedy-Fayers K, Pickering A, et al. [accessed 30/11/2009];Review of treatments of severe personality disorder. 2003 http://www.homeoffice.gov.uk/rds/pdfs2/rdsolr3003.pdf. Home Office Online Report 30/03.
- Weissman 1976 .Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry. 1976;33:1111–15. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Weissman 1993 .Weissman MM. The epidemiology of personality disorders: a 1990 update. Journal of Personality Disorders. 1993;(Suppl):44–62. [Google Scholar]
- WHO 1992 .World Health Organization (WHO) The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. WHO; Geneva: 1992. [Google Scholar]
- Winston 1994 .Winston A, Laikin M, Pollack J. Short-term dynamic psychotherapy of personality disorders. American Journal of Psychiatry. 1994;15:190–4. doi: 10.1176/ajp.151.2.190. [DOI] [PubMed] [Google Scholar]
- *Indicates the major publication for the study