Abstract
Background: Unmet health care needs are associated with negative health outcomes, yet there is a paucity of data on this problem among older people. Objective: To identify unmet health care needs and associated factors among older people in France. Methods: This is a cross-sectional population study of people aged 70 years or older in which 2350 respondents were interviewed in 2008–10. During a standardized interview, a nurse examined health problems, functional abilities and use of health care resources. Unmet health care needs were defined as situations in which a participant needed health care and did not receive it. Results: The mean age was 83.2 ± 7.4 years. Almost all participants reporting a chronic disease (98.6%) had consulted a physician in the previous 6 months. Unmet health care needs were found in 23.0% of the sample and mainly consisted of lack of dental care (prevalence of 17.7%), followed by lack of management of visual or hearing impairments (prevalence of 4.4% and 3.1%, respectively). Age was the main factor associated with unmet health care needs [compared with people aged 70–79: odds ratio80–89 years = 2.26 (1.70–3.03), odds ratio90 years and over = 3.85 (2.71–5.45)]. Other associated factors were regular smoking, homebound status, poor socioeconomic conditions, depression, limitations in instrumental activities of daily living and low medical density. Conclusion: Unmet health care needs affect almost one-quarter of older people in France. Efforts should be made to improve oral health and develop home care, especially for the oldest-olds.
Introduction
Unmet health care needs, defined as the difference between the health care services deemed necessary to deal with a particular health problem and the actual services received, represent a measure of access to health care. Unmet health care needs depend on the characteristics of the health care system (availability of services, waiting time before receiving care, etc.) and on the particular circumstances of the individuals seeking care (socioeconomic status, time constraints, etc.).1
France has statutory health insurance that covers almost 100% of the resident population. This insurance covers, on average, 75% of health care expenditures, but private supplementary coverage can be purchased to top up the statutory coverage up to 100%. In certain circumstances, patients are covered for 100% of the statutory charges, in particular when the insured person is suffering from 1 of 30 specified long-term illnesses.2 However, even in countries where social coverage is broad, social inequalities in health persist3,4; for example, the forfeiture of health care for economic reasons affected up to 15% of the adult population in France in 2008.5
The older people often have more complex needs compared with younger adults, due to additional disability, physical illness and social needs. A Spanish study6 suggests that unmet health care needs among older people increase the risk of dying within 5 years with an odds ratio of 1.64. Despite this worrisome result, research on the unmet needs of older people has been limited in France and elsewhere. Published studies often focus on home care and reveal lack of assistance in activities of daily living.7–11 Other studies deal with groups of elderly people with specific diseases, such as mental illnesses12 or dementia.11 Furthermore, differences between health care systems prevent useful comparisons with US13,14 and Asian15,16 studies. Indeed, there are specific limitations in access to health care in these countries, mainly due to financial issues in the USA and rurality in Asia. Even across Europe, there is substantial variation in the prevalence of unmet health care needs across countries, possibly related to the disparities in the integration of national health and social care systems.17
The increasing life expectancy across developed nations raises the issue of disparities in access to health care among older people. The purpose of the present study is to assess unmet health care needs in a sample of old people in France and identify factors associated with these unmet needs.
Methods
Study design and population
This work is part of a cross-sectional study carried out to characterize health and functional independence among people aged 70 and older. Subjects were selected at random among participants in a supplementary pension fund AG2R La Mondiale (Paris, France), with over-representation of the oldest-olds through a randomization-based sample that was stratified by age group. Recruitment took place across France from 2008 to 2010, in 21 survey areas representative of all regions and sizes of cities in mainland France. Information was collected during a 2-hour interview at home with a trained nurse. The presence of a close relative was required to confirm or complete the answers of 16.6% of the participants. The research protocol was approved by an independent ethics committee (permission n°060316).
Health and functional abilities
The health assessment took into account chronic diseases, physical functional limitations, activity restrictions as well as homebound, emotional and cognitive status. Participants reporting a chronic disease were asked to identify their problem(s) in a list of 14 chronic diseases used to monitor population health by the European Commission.18 Specific questions on physical and sensory functional limitations dealt with the ability to see newspaper print clearly, the ability to see the face of someone 4 m away clearly, the ability to hear distinctly what is said in a conversation with one other person and the ability to chew hard foods without difficulty, optionally with corrective devices (glasses, hearing devices and dentures).18 The evaluation of activity restrictions examined the five activities of daily living (ADL) included in the Katz index,19 i.e. bathing, dressing, toileting, transferring, continence and feeding, as well as instrumental activities of daily living (IADL)20 such as food preparation, the ability to use a telephone, housekeeping, shopping and the ability to manage one’s finances. Homebound status was defined as incapacity to leave the home without help. Depression was suspected in participants with a score higher than 5 to the 15-item Geriatric Depression Scale.21 Cognitive decline was defined as a Mini-Mental State Examination score of 26 or less.22
Use of health care resources
Participants were asked whether they had visited their general practitioner or a specialist during the previous 6 months and asked to identify their last visits to an ophthalmologist; an ear, nose and throat (ENT) specialist and a dentist (less than 1 year, between 1 and 5 years, more than 5 years and never).
Unmet health care needs
Unmet health care needs were defined as situations in which a participant needed health care but did not receive it. Two questions were used, the first question evaluating the need of care (‘Can you bite and chew hard foods like an apple without difficulty?’), and the second question dealing with the use of health care resources (‘When was your last visit to a dentist?’). In total, we identified four types of unmet health care need:
- Lack of ENT care: last visit to the ENT specialist more than 1 year before the interview when the participant reports hearing difficulties that prevent him/her from engaging in conversation with another person;
- Lack of visual care: last visit to the ophthalmologist more than 1 year before the interview when the participant has difficulty reading newspaper print or clearly seeing the face of someone 4 m away;
- Lack of dental care: last visit to the dentist more than 1 year before the interview when the participant reports difficulty chewing hard foods;
- Lack of management of a chronic disease: last visit to a general practitioner or specialist more than 6 months before the interview when the participant reports a chronic medical condition or a chronic health problem.
Other variables
Information was collected about the sociodemographic characteristics of participants: age, gender, former job, family situation and self-perceived economic situation. Based on the participant’s answer to the question ‘What is/was your occupation?’, we defined three professional levels: low (blue-collar workers), intermediate (intermediate white-collar workers, employees and shopkeepers) and high (high-level white-collar workers). Participants were also asked whether they were benefiting from full coverage of their health care expenditures. Regular smokers were identified by the reported use of one or more cigarette, cigar or pipe per day. Because the availability of health services is a factor contributing to unmet health care needs,23,24 medical density (number of general practitioners and specialists per 100 000 inhabitants) at the departmental level (mainland France is divided into 96 departments) was considered. Population density in the department of residence (inhabitants per km2) was also taken into account.
Statistical analysis
The prevalence of unmet health care needs was described in the whole study population, as well as in specific subgroups, i.e. among subjects presenting specific needs related to the presence of a chronic disease, a hearing impairment, a visual impairment or a dental impairment. Factors associated with unmet health care needs were identified using a multilevel logistic regression model with an individual level and a departmental level, to take into account the correlation between subjects of a same department. Indeed, the intraclass correlation coefficient obtained in empty model indicated that 5.0% of the total variance of unmet health care needs was explained by the departmental level. The variables introduced into the multivariate model were selected based on the bivariate analysis and published data. The results are presented with adjusted odds ratios (aORs) and 95% confidence intervals (CIs). Analyses were performed using Stata® software, version 12.0.
Results
Study population
A total of 2350 people agreed to participate in the study (participation rate: 18.9%), including 1393 women (59.3%) and 957 men (40.7%). The main reasons for non-participation were the lack of interest in the study (28.3% of the non-participants), followed by a state of frailty (10.8%) and the refusal of a close relative (7.3%). Participation was better in low-populated areas and in departments where the population is ageing or has a lower standard of living. Characteristics of the study population are described in table 1. Briefly, the mean age was 83.2 ± 7.4 years. Almost all participants reported a chronic health problem, mainly joint problems and high blood pressure. Difficulties in activities of daily living affected 37.4% of the study population, mainly bathing and dressing (ADL) and housekeeping and shopping (IADL).
Table 1.
Characteristics of the study sample
| Characteristics | n (%) |
|---|---|
| Sociodemographic characteristics and lifestyle | |
| Gender | |
| Male | 957 (40.7) |
| Female | 1393 (59.3) |
| Age | |
| 70–79 years | 858 (36.8) |
| 80–89 years | 969 (41.6) |
| 90 years and older | 502 (21.6) |
| Living in a couple | 991 (42.2) |
| With children | 2056 (90.2) |
| Professional category | |
| High | 283 (12.1) |
| Intermediate | 1111 (47.4) |
| Low | 952 (40.6) |
| Economic situation | |
| Good | 1008 (43.5) |
| Fair | 1152 (49.7) |
| Poor | 156 (6.7) |
| Full coverage of health care expenditures | 1321 (57.1) |
| Regular tobacco smoking | 76 (3.3) |
| Health and functional abilities | |
| At least one chronic health problem or disease | 2278 (98.0) |
| Asthma | 72 (3.1) |
| Allergies | 172 (7.4) |
| Diabetes | 279 (12.0) |
| Cataract | 359 (15.5) |
| High blood pressure | 745 (32.0) |
| Heart attack | 21 (0.9) |
| Stroke | 42 (1.8) |
| Chronic bronchitis/emphysema | 214 (9.2) |
| Arthrosis/(rheumatic) arthritis | 1544 (66.0) |
| Osteoporosis | 304 (13.4) |
| Gastric or duodenal ulcer | 47 (2.0) |
| Cancer, malignant tumour | 69 (3.0) |
| Migraines/frequent headaches | 191 (8.2) |
| Chronic anxiety/depression | 435 (18.7) |
| Hearing impairment | 83 (3.6) |
| Visual impairment | 233 (10.2) |
| Difficulty chewing hard foods | 539 (23.6) |
| Need for help | |
| In IADL | 522 (22.4) |
| In ADL | 351 (15.0) |
| Homebound status | 249 (10.8) |
| Depressive symptoms | 465 (20.0) |
A large majority of the study population (n = 2243, 97.1%) had visited a general practitioner at least once during the previous 6 months, and the mean number of visits over this period was 3.9 ± 2.9. A specialist had been consulted at least once in the previous 6 months by 1449 subjects (62.7% of the sample). Ophthalmologists were widely consulted by our sample: 49.1% of the sample (n = 1137) reported a visit during the previous year and 38.5% during the previous 1–5-year period (n = 891). Only 266 subjects (11.5%) had consulted an ENT specialist during the previous year, and 1071 subjects (46.3%) reported never having seen an ENT specialist. The variable on dental care was homogeneously distributed, with one-third of the subjects having consulted a dentist during the previous year (n = 776, 33.4%), one-third having consulted a dentist between 1 and 5 years before the interview (n = 786, 33.9%) and one-third having consulted a dentist more than 5 years before (n = 710, 30.6%) or not at all (n = 49, 2.1%).
Unmet health care needs
Unmet health care needs were reported by 23.0% (95% CI: 21.3–24.7%) of the study population and prevalence increased with age, reaching 46.1% in people aged 95 and older (figure 1). The most prevalent unmet need in the study population was for dental care (17.7%); we estimated that more than three-quarters of respondents reporting difficulty chewing hard foods had not seen a dentist in the previous year (table 2). Lack of ENT care and lack of visual care were less frequent, with a prevalence of approximately 3–4% in the whole sample, but they affected a large proportion of people reporting hearing or visual limitations, 88.0% and 44.2%, respectively. Lack of contact with a medical doctor to manage a chronic disease was rare, reported by only 1.4% of the study sample.
Figure 1.
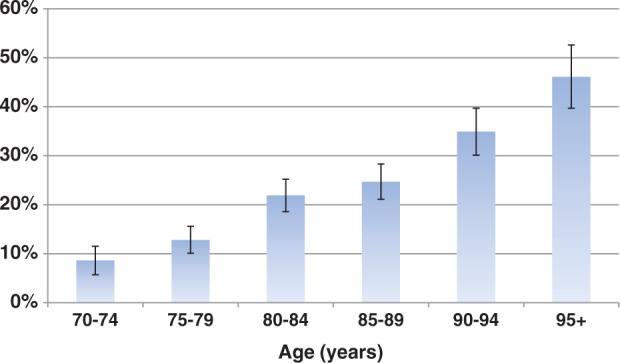
Prevalence of unmet health care needs according to age
Table 2.
Prevalence of unmet health care needs
| Types of unmet needs | Number of subjects | Prevalence in the whole sample | Prevalence in subgroups with specific needsa |
|---|---|---|---|
| Lack of management of a chronic disease | 33 | 1.4% | 1.5% |
| Lack of ENT care | 73 | 3.1% | 88.0% |
| Lack of visual care | 103 | 4.4% | 44.2% |
| Lack of dental care | 412 | 17.7% | 76.4% |
| At least one unmet health care need | 537 | 23.0% | – |
aSubgroups of subjects presenting specific needs related to the existence of a chronic disease, a hearing impairment, a visual impairment or a dental impairment.
Factors associated with unmet health care needs
Factors associated with unmet health care needs as revealed by the multivariate analysis are presented in table 3. Age was the main risk factor for unmet health care needs, independent of co-morbidities and loss of autonomy, with a more than 3-fold increase in the age group >90 years compared with the age group 70–80 years. Other strong risk factors for unmet health care needs were regular homebound status and tobacco smoking, with aOR of 1.96 and 2.70, respectively. Nevertheless, the very low prevalence of tobacco smoking in our sample (3.3%) tempers the effect of this risk factor. A poor economic situation, a low level of former employment, limitations in IADL and depressive status also increased the risk of having unmet health care needs. In contrast, living in a couple was protective against the risk of having unmet health care needs. Population density was not related to the risk of having unmet health care needs, whereas there was a negative relation with the medical density, each additional practitioner per 1000 inhabitants reducing the risk of having unmet need by 16%. Gender, full coverage of health care expenditures and the number of chronic diseases were not associated with the existence of unmet health care needs, but these variables were nevertheless kept in the model as adjustments.
Table 3.
Factors associated with unmet health care needs in the multilevel model
| Variables | Unmet health care needs (%) | aOR | 95%CI | P |
|---|---|---|---|---|
| Gender | ||||
| Female | 25.7 | 1 | ||
| Male | 19.0 | 0.96 | 0.73–1.27 | 0.786 |
| Age | ||||
| 70–79 years | 11.4 | 1 | ||
| 80–89 years | 24.3 | 2.26 | 1.70–3.03 | <0.001 |
| 90 years and older | 39.8 | 3.85 | 2.71–5.45 | <0.001 |
| Living in a couple | ||||
| No | 28.3 | 1 | ||
| Yes | 15.7 | 0.74 | 0.56–0.98 | 0.033 |
| Professional category | ||||
| High | 13.07 | 1 | ||
| Intermediate | 22.2 | 1.47 | 0.96–2.26 | 0.077 |
| Low | 26.9 | 1.61 | 1.04–2.49 | 0.032 |
| Self-perceived economic situation | ||||
| Good | 18.7 | 1 | ||
| Fair | 24.8 | 1.17 | 0.92–1.49 | 0.190 |
| Poor | 35.3 | 1.66 | 1.08–2.57 | 0.022 |
| Full coverage of health care expenditures | ||||
| No | 20.0 | 1 | ||
| Yes | 24.8 | 1.10 | 0.87–1.40 | 0.419 |
| Number of chronic diseases | ||||
| 0–1 | 18.7 | 1 | ||
| 1–3 | 24.6 | 1.21 | 0.94–1.57 | 0.137 |
| 4+ | 28.5 | 1.19 | 0.84–1.68 | 0.328 |
| Depressive symptoms | ||||
| No | 19.3 | 1 | ||
| Yes | 37.2 | 1.66 | 1.27–2.18 | <0.001 |
| Need for help | ||||
| No | 15.5 | 1 | ||
| In IADL | 32.6 | 1.50 | 1.13–2.00 | 0.005 |
| In ADL | 40.2 | 1.36 | 0.94–1.97 | 0.104 |
| Homebound status | ||||
| No | 19.6 | 1 | ||
| Yes | 51.8 | 1.98 | 1.37–2.85 | <0.001 |
| Regular tobacco smoking | ||||
| No | 22.8 | 1 | ||
| Yes | 30.3 | 2.76 | 1.57–4.86 | <0.001 |
| Medical density (+1 practitioner per 1000 inhabitants) | 0.84 | 0.71–0.99 | 0.038 | |
Values in bold indicate characteristics significantly associated (p < 0.05) with the prevalence of unmet health care needs.
Discussion
Main findings
This cross-sectional population study shows that unmet health care needs may be found in almost one-quarter of the elderly population in France. Lack of dental care was the main need identified, in relation to the high prevalence of chewing problems compared with hearing and visual problems in our sample. Socioeconomic position influenced the risk of having unmet health care needs, but the main risk factors identified were advanced age and homebound status.
Strength and limitations of the study
A major strength of this study is its large random sample of recipients of a supplementary pension fund, where the over-representation of the oldest-olds improved the accuracy of estimates in extreme age groups. Definitions of unmet health care needs based on questions about forfeiting health care for various reasons (cost, illness, someone else to care for, etc.)13,14,25 focus on people’s experiences obtaining services when they needed them. Such definitions exclude people who are unaware of their health care needs, who may be numerous among the elderly. In the case of dental care, it has been found that 78% of old people consider a visit to their dentist unnecessary.26 Our assessment of unmet health care needs overcomes this problem by using separate identifications of health problems and health care use. We differentiated four types of unmet health care needs, related to chronic medical conditions, hearing, vision and dental problems, which may provide a comprehensive overview of medical problems of old people. However, we had no disease-specific data. One may fear selection effects related to the recruitment of subjects in a supplementary pension fund. Nevertheless, the source population was very large, composed of the 2 100 000 retirees who joined this supplementary pension fund, thus selection effects seem unlikely. In addition, our sampling design enabled us to represent all the French territory, and our study population was similar to the national statistics with regard to sex ratio and socioeconomic profile.27 A limitation of this analysis is its cross-sectional design. Further studies are needed to assess the consequences of unmet health care needs in terms of mortality, morbidity and autonomy.
Factors associated with unmet health care needs
The gradient observed between the prevalence of unmet health care needs and the age of subjects was previously reported in the Nepalese study by Kshetri et al.15 This finding could be due to the increasing number of health problems with age, which mechanically increases the probability of having unmet health care needs. Nevertheless, our results were adjusted for the health status of subjects, using the number of chronic diseases and reported difficulties in ADL. A form of ageism might explain part of the lack of health care among the oldest-olds: physicians, as well as the patients themselves, often disregard certain conditions that they consider inevitable results of senescence.28 Education and health literacy should play an important role here.
Whereas published studies often point to the cost of health care as the main reason for unmet health care needs,13,14 we observed a stronger effect of other factors, such as regular tobacco smoking, homebound status and depression, as compared with socioeconomic factors. The increased risk of having unmet health care needs among regular smokers compared with people who never smoked or former smokers probably indicates the poor health-seeking behaviour of smokers, consistent with a denial of the adverse health effects of smoking previously shown among US elders.29 But again, smokers were a marginal group in our sample. Homebound status is an indicator of poor mobility and poor social participation. It was shown to be an independent predictor of 2-year mortality and disability. Among the reasons that could explain this excess mortality, it was suggested that homebound status may limit contacts with the health care system and finally make health problems worsen.30,31 The present study confirms this hypothesis by showing that homebound people are more likely to have unmet health care needs compared with non-homebound people. Depression may also lead to poor use or misuse of health care resources, as it can reduce adherence to treatments, and be associated with an unhealthy lifestyle and inactivity.32
Nevertheless, we still confirm the role played by socioeconomic factors. A poor self-perceived economic situation and a low-level former job were factors increasing the risk of having unmet health care needs with aOR of 1.66 and 1.61, respectively. While full coverage of health care expenditures was expected to be associated with a lower prevalence of unmet health care needs, we did not observe any significant relationship. Such a result may be explained by the nature of unmet health care needs: they were mainly lack of dental care, which is poorly covered by France’s statutory health insurance.
Potential consequences of unmet health care needs
The analysis of the literature shows that poor dental health is related to increased morbidity and mortality33 and poor quality of life.34 An inability to chew hard foods may restrict the intake of red meat and foods rich in fibre,35,36 resulting in constipation, vitamin deficiency and denutrition.33 Denutrition is considered a gateway to frailty.37 French health authorities therefore recommend an annual dental consultation for the elderly.38 We nevertheless observed that 17.7% of the study population had not met with their dentist, even though they had difficulty chewing hard foods. In supplementary analyses, we observed a significant relationship between difficulty chewing hard foods and involuntary weight loss in the past 6 months, with an odds ratio of 1.46 (95% CI: 1.04–2.07) after adjusting for gender, age, co-morbidities and limitations in daily activities. Various interventions to improve seniors’ access to dental care could be proposed, such as the use of mobile services to provide dental care in the home39 or the development of gerontological networks through which medical and paramedical staffs providing home care could alert authorities when a patient needs dental care. A French study39 also suggests that general practitioners should take advantage of their strategic position to promote dental care among their elderly patients. Considering the number of patients, family caregivers and physicians who may disregard dental care, a public health campaign would be helpful.
In conclusion, our results underscore the scope of unmet health care needs among older people, especially with regard to dental health. The oldest-olds are the most affected by unmet health care needs. Further studies are required to better assess the consequences of unmet health care needs in this growing segment of the population. Public health policy should already promote better access to care for older people and fight against any form of ageism.
Funding
This work was supported by AG2R La Mondiale (staffing, data management) and the Versailles Saint Quentin University (data analysis).
Conflicts of interest: Data analyses were performed by the Laboratoire Santé Environnement Vieillissement (EA2506), which is a university team independent from AG2R La Mondiale.
Key points.
The lengthening of life in industrialized countries raises the issue of access to health care among older people. Unmet health care needs, defined as situations in which someone who needed health care did not receive it, represent a measure of access to health care.
This cross-sectional population study shows that unmet health care needs may be found in 23.0% of people aged 70 and older in France. Lack of dental care was the main need identified (prevalence of 17.7%).
Whereas published studies often point to the cost of health care as the main reason for unmet health care needs, we observed a stronger effect of other factors, particularly age and homebound status.
Efforts should be made to develop home care and improve oral health, especially for the oldest-olds, using mobile health care services, gerontological networks and public health campaigns.
Acknowledgements
In addition to our sources of funding, we would like to thank Jean-Pierre AUDRAN for his involvement in setting up the study, Isabelle REMY for her logistical support and Frédéric SIMOES DA GAMA for his contribution to data management.
References
- 1. Institut canadien d’information sur la santé (ICIS). Les soins de santé au Canada 2001. Ottawa, Institut canadien d’information sur la santé 2001 (cited 2012). Available at: https://secure.cihi.ca/estore/productFamily.htm?locale=fr&pf=PFC105&lang=fr&media=0.
- 2.Chevreul K, Durand-Zaleski I, Bahrami S, et al. France: health system review. Health Syst Trans. 2010;12:1–291. [PubMed] [Google Scholar]
- 3.van Doorslaer E, Masseria C, Koolman X Group OECD Health Equity Research Group. Inequalities in access to medical care by income in developed countries. CMAJ. 2006;174:177–83. doi: 10.1503/cmaj.050584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sirven N, Or Z. The Individual and the Welfare State: Life Histories in Europe. Springer Berlin Heidelberg: Disparities in Regular Health Care Utilisation in Europe. pp. 241–54. [Google Scholar]
- 5. Comptes nationaux de la santé 2010 (cited 2012). Available at: http://www.drees.sante.gouv.fr/IMG/pdf/comptes_nationaux_sante_2010.pdf.
- 6.Alonso J, Orfila F, Ruigomez A, et al. Unmet health care needs and mortality among Spanish elderly. Am J Public Health. 1997;87:365–70. doi: 10.2105/ajph.87.3.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allen SM, Mor V. The prevalence and consequences of unmet need. Contrasts between older and younger adults with disability. Med Care. 1997;35:1132–48. doi: 10.1097/00005650-199711000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Kennedy J. Unmet and undermet need for activities of daily living and instrumental activities of daily living assistance among adults with disabilities: estimates from the 1994 and 1995 disability follow-back surveys. Med Care. 2001;39:1305–12. doi: 10.1097/00005650-200112000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Otero A, de Yebenes MJ, Rodriguez-Laso A, Zunzunegui MV. Unmet home care needs among community-dwelling elderly people in Spain. Aging Clin Exp Res. 2003;15:234–42. doi: 10.1007/BF03324504. [DOI] [PubMed] [Google Scholar]
- 10.Casado BL, van Vulpen KS, Davis SL. Unmet needs for home and community-based services among frail older Americans and their caregivers. J Aging Health. 2011;23:529–53. doi: 10.1177/0898264310387132. [DOI] [PubMed] [Google Scholar]
- 11.Gaugler JE, Kane RL, Kane RA, Newcomer R. Unmet care needs and key outcomes in dementia. J Am Geriatr Soc. 2005;53:2098–105. doi: 10.1111/j.1532-5415.2005.00495.x. [DOI] [PubMed] [Google Scholar]
- 12.Futeran S, Draper BM. An examination of the needs of older patients with chronic mental illness in public mental health services. Aging Mental Health. 2012;16:327–34. doi: 10.1080/13607863.2011.628978. [DOI] [PubMed] [Google Scholar]
- 13.Shi L, Stevens GD. Vulnerability and unmet health care needs. The influence of multiple risk factors. J Gen Int Med. 2005;20:148–54. doi: 10.1111/j.1525-1497.2005.40136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diamant AL, Hays RD, Morales LS, et al. Delays and unmet need for health care among adult primary care patients in a restructured urban public health system. Am J Public Health. 2004;94:783–9. doi: 10.2105/ajph.94.5.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kshetri DB, Smith WC. Self-reported health problems, health care utilisation and unmet health care needs of elderly men and women in an urban municipality and a rural area of Bhaktapur District of Nepal. Aging Male. 2011;14:127–31. doi: 10.3109/13685538.2010.502272. [DOI] [PubMed] [Google Scholar]
- 16.Li H, Tracy MB. Family support, financial needs, and health care needs of rural elderly in China: a field study. J Cross Cult Gerontol. 1999;14:357–71. doi: 10.1023/a:1006607707655. [DOI] [PubMed] [Google Scholar]
- 17.Bien B, McKee KJ, Dohner H, et al. Disabled older people's use of health and social care services and their unmet care needs in six European countries. Eur J Public Health. 2013 doi: 10.1093/eurpub/cks190. [DOI] [PubMed] [Google Scholar]
- 18.Robine JM, Jagger C, Euro RG. Creating a coherent set of indicators to monitor health across Europe: the Euro-REVES 2 project. Eur J Public Health. 2003;13(3 Suppl):6–14. doi: 10.1093/eurpub/13.suppl_1.6. [DOI] [PubMed] [Google Scholar]
- 19.Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 20.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- 21.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 22.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 23.Diwan S, Moriarty D. A conceptual framework for identifying Unmet health care needs of community dwelling elderly. J Appl Gerontol. 1995;14:47–63. [Google Scholar]
- 24.Chaix B, Boelle PY, Guilbert P, Chauvin P. Area-level determinants of specialty care utilization in France: a multilevel analysis. Public Health. 2005;119:97–104. doi: 10.1016/j.puhe.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 25.Sanmartin C, Berthelot JM, Ng E, Murphy K, Blackwell DL, Gentleman JF, et al. Comparing health and health care use in Canada and the United States. Health Affairs. 2006;25:1133–42. doi: 10.1377/hlthaff.25.4.1133. [DOI] [PubMed] [Google Scholar]
- 26.Chiappelli F, Bauer J, Spackman S, et al. Dental needs of the elderly in the 21st century. Gen Dent. 2002;50:358–63. [PubMed] [Google Scholar]
- 27. National Institute of Statistics and Economic Studies (INSEE) (cited 2012). Available at: http://www.insee.fr/
- 28.Eymard AS, Douglas DH. Ageism among health care providers and interventions to improve their attitudes toward older adults: an integrative review. J Gerontol Nurs. 2012;38:26–35. doi: 10.3928/00989134-20120307-09. [DOI] [PubMed] [Google Scholar]
- 29.Ruchlin HS. An analysis of smoking patterns among older adults. Med Care. 1999;37:615–9. doi: 10.1097/00005650-199906000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Herr M, Latouche A, Ankri J. Homebound status increases death risk within two years in the elderly: results from a national longitudinal survey. Arch Gerontol Geriatr. 2013;56:258–64. doi: 10.1016/j.archger.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 31.Cohen-Mansfield J, Shmotkin D, Hazan H. The effect of homebound status on older persons. J Am Geriatr Soc. 2010;58:2358–62. doi: 10.1111/j.1532-5415.2010.03172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Taleb M, Rouillon F, Hegerl U, et al. Programmes against depression. Encephale. 2006;32:9–15. doi: 10.1016/s0013-7006(06)76132-2. [DOI] [PubMed] [Google Scholar]
- 33.Papas AS, Palmer CA, Rounds MC, Russell RM. The effects of denture status on nutrition. Spec Care Dentist. 1998:1817–25. doi: 10.1111/j.1754-4505.1998.tb01354.x. [DOI] [PubMed] [Google Scholar]
- 34.Petersen PE, Bourgeois D, Ogawa H, et al. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83:661–9. [PMC free article] [PubMed] [Google Scholar]
- 35.Atchison KA, Gift HC. Perceived oral health in a diverse sample. Adv Dent Res. 1997;11:272–80. doi: 10.1177/08959374970110021001. [DOI] [PubMed] [Google Scholar]
- 36.Marcenes W, Steele JG, Sheiham A, Walls AW. The relationship between dental status, food selection, nutrient intake, nutritional status, and body mass index in older people. Cad Saude Publica. 2003;19:809–16. doi: 10.1590/s0102-311x2003000300013. [DOI] [PubMed] [Google Scholar]
- 37.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–56. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 38. Prévention bucco-dentaire chez les personnes âgées. Direction Générale de la Santé 2006 (cited 2012). Available at: http://www.sante.gouv.fr/IMG/pdf/Prevention_bucco-dentaire_chez_les_personnes_agees.pdf.
- 39.British Society for disability and oral health BSDH. The development of standards for domiciliary dental services: Guidelines and recommendations. 2000 (cited 2012) doi: 10.1111/j.1741-2358.2000.00119.x. Available at: http://www.bsdh.org.uk/guidelines/domicil.pdf. [DOI] [PubMed] [Google Scholar]


