Abstract
Background: Evidence suggests that higher multi-morbidity rates among people with low socioeconomic status produces and maintains poverty. Our research explores the relationship between socioeconomic deprivation and multi-morbidity among Palestinian refugees in Lebanon, a marginalized and impoverished population. Methods: A representative sample of Palestinian refugees in Lebanon was surveyed, interviewing 2501 respondents (97% response rate). Multi-morbidity was measured by mental health, chronic and acute illnesses and disability. Multinomial logistic regression models assessed the association between indicators of poverty and multi-morbidities. Results: Findings showed that 14% of respondents never went to school, 41% of households reported water leakage and 10% suffered from severe food insecurity. Participants with an elementary education or less and those completing intermediate school were more than twice as likely to report two health problems than those with secondary education or more (OR: 2.60, CI: 1.73–3.91; OR: 2.47, CI: 1.62–3.77, respectively). Those living in households with water leakage were nearly twice as likely to have three or more health reports (OR = 1.88, CI = 1.45–2.44); this pattern was more pronounced for severely food insecure households (OR = 3.41, CI = 1.83–6.35). Conclusion: We identified a positive gradient between socioeconomic status and multi-morbidity within a refugee population. These findings reflect inequalities produced by the health and social systems in Lebanon, a problem expected to worsen following the massive influx of refugees from Syria. Ending legal discrimination and funding infrastructural, housing and health service improvements may counteract the effects of deprivation. Addressing this problem requires providing a decent livelihood for refugees in Lebanon.
Introduction
Social determinants such as poverty, social status and the neighbourhood environment have a formative impact on health, both producing illness and impeding care. The effect of social determinants is often most concentrated in the people at the peripheries of society. This research explores the conditions of Palestinian refugees in Lebanon, many whom were first displaced from Palestine in 1948 and remain in a marginalized state.
In 1949, the United Nations formed the United Nations Reliefs and Works Agency (UNRWA) to address the needs of Palestinians displaced across the region.1 UNRWA still carries out health, relief, education and social programs for registered refugees, though they face frequent shortfalls. This support is supplemented by charity, remittances and political and private patronage—efforts which combined still fail to address the basic needs of these communities.
Palestinian refugees have primarily settled in what are known as ‘mukhayem’ (‘camps’), which have recently experienced rapid population growth. The Bourj al Barajneh camp in Beirut (1.5 km2) accommodated 10 000 people 25 years ago, and now houses an estimated 25 000 permanent residents and at least another 5000 refugees of the Syrian conflict. Tens of thousands of refugees also live in ‘tajamooat’ (‘gatherings’), accommodating informal Palestinian communities around the country. Most Palestinian neighbourhoods have running water and closed sewage systems, with almost all dwellings built of concrete. Yet, water quality is still poor and electricity is only intermittently available, sometimes for as little as 3 hr per day. Moreover, the waste management infrastructure in many of these neighbourhoods is inadequate, leading to pest infestations and unsanitary conditions.
Social and economic conditions of Palestinian refugees
Palestinians in Lebanon face a ‘protracted mode of legal exclusion’ that restricts their labor market participation, asset ownership and mobility.2 Lebanese law prevents Palestinians from working in over 30 occupations, perhaps explaining data from a recent study, which found joblessness (defined as persons of working age who are not in school and not working) endemic for 52% of refugees surveyed.3 This legislated exclusion has led to de facto discrimination in employment and wages for Palestinian workers. A comparative study of incomes between Palestinian and Lebanese workers in Lebanon revealed that Palestinian men and women were segregated into less desirable occupational sectors and earned less for the same work across all educational and occupational categories.4
This lack of employment opportunity has influenced Palestinian views toward education. Palestinian families traditionally emphasized education as a key to social mobility;5 yet poor educational offerings available through UNRWA and a lack of job opportunities have paved the way for a staggering reversal.6 Around 40% of Palestinian refugee students do not enroll in the secondary level, a figure 10 times higher than their Lebanese counterparts.7,8 A similar trend exists among Palestinian adults, who report lower completion rates for all levels of education.3
Links between socioeconomic status and health
Population health research has convincingly associated conditions of poverty and marginalization with health problems ranging from poor self-rated health and poor mental health to chronic illness.9 Moreover, low socioeconomic status (SES) serves as an impediment to medical coverage, which may directly affect the prevalence of acute illnesses.10 These observations are supported by large population studies suggesting low SES is a determinant for all-cause mortality11 and multiple morbidities.12
Multi-morbidity is an important indicator of individual health and the need for complex health care services. Multi-morbidity is associated with greater use of inpatient and ambulatory services,13 reduced functional status14 and increased mortality rates.15 Though multi-morbidity is commonly associated with older age,13,16 there is evidence of sizeable multi-morbidity rates among middle-aged populations.12,17
The few published studies on the relationship between poverty and multiple morbidities have consistently reported strong associations between the two.12,16,18 The strongest support for this link came from Barnett et al (2012), who found a gradient relationship between multi-morbidity and socioeconomic deprivation in a study of the Scottish patient population. This association persisted in nearly all age groups and among patients diagnosed with both a mental and physical health problem. Multi-morbidity poses a dilemma for health service providers in disadvantaged communities who must contend with complex diagnoses and treatment regimes among patients who are often disadvantaged in their daily lives and in access to health services.
Research on Palestinian refugee communities in Lebanon shows similar health trends mediated by relative disadvantage. A study conducted in 2008 on chronic illness in a Palestinian refugee community found that having a family member with full-time employment halved household chances of reporting chronic illness.19 Meanwhile, a Lebanon-wide study of Palestinian communities found relationships between income and education on the one hand and chronic illness and poor mental and self-rated health on the other hand.20
The present study builds on the foundations of past research on the health of Palestinian refugees, while providing an assessment of the relationship between socioeconomic deprivation and health. Most studies of multi-morbidities focus on diverse patient or general populations. In comparison, this study assesses these outcomes among communities of refugees who are, for the most part, socially marginalized and economically deprived.
Methods
A cross-sectional survey of Palestinian refugee households in Lebanon was carried out by UNRWA and a multidisciplinary research team from the American University of Beirut (AUB). Researchers developed a questionnaire to assess household socioeconomic deprivation for Palestinian refugees in Lebanon. The Institutional Review Board at AUB approved this study.
Data and sample
The study adopted a multistage cluster sample, with households selected at random from each cluster. The research team approached 2579 households throughout 12 camps and in 20 gatherings distributed in Lebanon’s five administrative areas: the North, Central Lebanon Area, Saida, Tyre and Bekaa. Clusters were identified as distinct Palestinian refugee neighbourhoods, designated as either established camps or unofficial gatherings. Sampling frames for each neighbourhood were provided by UNRWA. Each of the 12 camps in Lebanon were sampled, while 20 gatherings were randomly selected from a total of 187 across the country, with each gathering cluster weighted based on population estimates. Within camps, a representative sample was randomly selected proportional to the population size.
The research team administered structured questionnaires during face-to-face interviews with a respondent from each of 2501 participating households (97% response rate). UNRWA social workers interviewed the person responsible for homemaking activities—generally a female—from each household. These respondents were targeted because of their involvement with homemaking and household purchases. If a homemaker was not available, any adult family member was interviewed.
Indicators
The primary study outcomes were chronic illness, acute illness, mental health and disability. Participants self-reported their health conditions, a method that is often utilized and has been validated in the literature.21–25. To measure mental health, the questionnaire included the five-item Mental Health Inventory 26,27, a scale with scores ranging from 5 to 30 and higher scores indicating good mental health. For the purpose of this study, the cut-off for poor health was taken at 19. This cut-off has been used as an indicator of poor mental health in other studies.28 The instrument also included an item on self-reported health status, an indicator strongly correlated with morbidity and mortality.29
Chronic illnesses were self-reported, answering the question, ‘Do you suffer from a chronic illness?’ Respondents answering yes could report up to four chronic illness, each being counted as an independent morbidity. Acute illnesses were self-reported with the question, ‘In the past 6 months have you suffered from an acute illness?’ while the question, ‘Do you suffer from a physical disability?’ included examples such as blindness, deafness, paralysis, amputations and inability to speak.
The primary outcome of this study is multi-morbidity measuring distinct health problems (zero, one, two, three or more), counting once for each chronic illness. Self-rated health was excluded from multi-morbidity, as it is not a health problem and is closely associated with the presence of morbidity. Associations were drawn between these health indicators and individual demographic and socioeconomic variables. SES was assessed with five measures:
Educational attainment: Measured as ‘no education or elementary school’; ‘intermediate school’; ‘secondary education or more’ including secondary school, vocational school or university.
Wealth index: Calculated using a 17-item index (including cars, computers, phones, ovens, washing machines, etc.), and households were divided into three categories (lowest, middle, highest tertile) using a principal component analysis to identify the weights of the items included in the index and the sample distribution into tertiles.30
Crowding: Calculated by dividing the number of people in a home by the number of rooms (excluding the balcony, kitchen and restrooms).
Severe food insecurity: At least one household member who in the previous 6 months did not eat for an entire day or went to sleep hungry because there was not enough food or money to buy food.
Water leakage in the home: Measured with questions asking about water damage to the walls and roofs. Answers were categorized as ‘yes’ or ‘no’.
The independent demographic variables included in the logistic regression were age (continuous), gender and geographic location (Beirut or periphery to the capital).
Demographic and SES variables were run in logistical regressions with each of the five health indicators. No multicolinearity was found among the measures. A multinomial regression model was then conducted for multiple health problems (zero, one, two, three or more health outcomes) taking the category ‘no poor health outcomes’ as a baseline reference. Odds ratios and 95% confidence intervals were calculated.
Furthermore, data were compiled into two graphs, one depicting the relationship between SES deprivation, multi-morbidities and self-rated health, while the other indicates the relationship between SES deprivation, multi-morbidities and age. Statistical analysis was conducted using Stata 10. Two-stage sampling [weight, clustered primary sampling unit (PSU)] has been adjusted for.
Results
The average age of respondents was 47, with 82% female participants to 18% male. In total, 333 (14%) of respondents never went to school, 686 (29%) attained elementary school only, 895 (38%) attained intermediate school and another 246 (10%) attained secondary school. Eighty-one respondents (3%) had vocational training, and only 149 (6%) went to university. Reflecting families’ inabilities to maintain upkeep of their homes, 41% of respondents reported water leakage. Respondents reported an average household crowding level of 1.76 persons per room, and 10% of respondents lived in families suffering from severe food insecurity. Table 1 shows the demographic characteristics of the study population and response to the main socioeconomic variables in the study and health outcomes.
Table 1.
Socio-demographic characteristics, determinants of poverty and health outcomes for Palestinian refugees living in Lebanese camps, N = 2501, 2010
| Respondent (N = 2501) | n | % |
|---|---|---|
| Demographic characteristics | ||
| Age | ||
| Mean (min–max) | 46.6 (14–87) | SD (15.90) |
| Gender | ||
| Male | 443 | 18.09 |
| Female | 2006 | 81.91 |
| Geographic location | ||
| Peripheriesa | 1952 | 78.05 |
| Capital Beirut | 549 | 21.95 |
| Determinants of poverty | ||
| Education | ||
| Elementary or less | 1019 | 42.64 |
| Intermediate | 895 | 37.45 |
| Secondary or more | 476 | 19.92 |
| Water leaking from walls and roofs | ||
| No water leakage | 1453 | 58.64 |
| Water leakage | 1025 | 41.36 |
| Wealth index | ||
| Lowest | 809 | 33.21 |
| Middle | 810 | 33.25 |
| Highest | 817 | 33.54 |
| Mean (min–max) | 5.86 (0–14) | SD. 2.20 |
| Crowding | ||
| Mean (min–max) | 1.76 (0.12–12) | SD. 1.03 |
| Severe food insecurity | ||
| No | 2249 | 89.92 |
| Yes | 252 | 10.08 |
| Health of respondent | ||
| Number of chronic illness | ||
| None | 1182 | 48.11 |
| One | 610 | 24.83 |
| Two | 463 | 18.84 |
| Three | 143 | 5.82 |
| Four | 59 | 2.40 |
| Prevalence of acute illness in the past 6 months | ||
| No | 1728 | 70.33 |
| Yes | 729 | 29.67 |
| Prevalence disability | ||
| No | 2338 | 96.13 |
| Yes | 94 | 3.87 |
| Mental health | ||
| Good | 1074 | 43.25 |
| Poor | 1409 | 56.75 |
| Self-rated health | ||
| Good | 1716 | 69.11 |
| Poor | 767 | 30.89 |
| Number of health outcomes (multiple chronic, acute, disability and mental) | ||
| Zero | 489 | 20.17 |
| One | 678 | 27.97 |
| Two | 571 | 23.56 |
| Three or more | 686 | 28.30 |
a: Peripheries include: North Lebanon, Bekaa, South Lebanon and Tyre.
The study findings on health outcomes showed that 52% (n = 1275) of the respondents reported suffering from a chronic illness (including hypertension, diabetes, back pain, asthma and heart problems), 729 (30%) reported suffering from an acute illness (including influenza, diarrheal diseases, food poisoning, infections, tonsillitis and others) in the past 6 months, and 94 (4%) reported living with a physical disability. In total, 1409 respondents (57%) reported poor mental health and 767 (31%) perceived their health as poor. Concerning multi-morbidity, 678 (28%) reported only one health problem, 571 (24%) reported two health problems and 686 (28%) reported three or more health problems. Only 489 (20%) reported no health problems.
Multi-morbidities were strongly correlated with socioeconomic variables in the adjusted multinomial model (table 2). Participants with an elementary education or less and those completing intermediate school were more than twice as likely to report two health problems than those with secondary education or more (OR: 2.60, CI: 1.73–3.91; OR: 2.47, CI: 1.62–3.77, respectively), while people with an elementary education or less were more likely to report three health outcomes or more (OR: 1.83, CI: 1.12–2.99).
Table 2.
Adjusted multinomial model of the association between demographic and poverty determinants and the number of health outcomesb among Palestinian Refugees living in Lebanese camps, N = 2501, 2010
| Respondent (N = 2288) | One poor health outcomec (n = 678; 28%) |
Two poor health outcomesc (n = 571; 24%) |
Three or more poor health outcomesc (n = 686; 28%) |
|||
|---|---|---|---|---|---|---|
| Adjusted RR (95% CI) | P-value* | Adjusted RR (95% CI) | P-value* | Adjusted RR (95% CI) | P-value* | |
| Age | 1.02 (1.01–1.03) | 0.00 | 1.05 (1.04–1.07) | 0.00 | 1.10 (1.08–1.11) | 0.00 |
| Gender | ||||||
| Male | 1 | 1 | 1 | |||
| Female | 1.17 (0.85–1.61) | 0.33 | 1.16 (0.83–1.64) | 0.38 | 1.33 (0.94–1.87) | 0.10 |
| Education | ||||||
| Secondary or more | 1 | 1 | 1 | |||
| Intermediate | 1.28 (0.86–1.93) | 0.23 | 2.47 (1.62–3.77) | 0.00 | 1.32 (0.81–2.17) | 0.27 |
| Never went - Elementary | 1.22 (0.81–1.82) | 0.35 | 2.60 (1.73–3.91) | 0.00 | 1.83 (1.12–2.99) | 0.02 |
| Water leaking from walls and roofs | ||||||
| No water leakage | 1 | 1 | 1 | |||
| Water leakage | 1.30 (0.98–1.72) | 0.07 | 1.16 (0.90–1.50) | 0.24 | 1.88 (1.45–2.44) | 0.00 |
| Wealth index | ||||||
| Highest | 1 | 1 | 1 | |||
| Middle | 1.19 (0.90–1.57) | 0.23 | 1.16 (0.88–1.53) | 0.31 | 1.50 (1.02–2.01) | 0.04 |
| Lowest | 1.49 (1.08–2.06) | 0.02 | 1.80 (1.23–2.63) | 0.00 | 2.14 (1.48–3.09) | 0.00 |
| Crowding index | 1.20 (1.00–1.44) | 0.048 | 1.21 (1.04–1.41) | 0.01 | 1.27 (1.02–1.57) | 0.03 |
| Geographic location | ||||||
| Peripheriesa | 1 | 1 | 1 | |||
| Capital - Beirut | 1.64 (1.05–2.54) | 0.03 | 1.74 (1.22–2.48) | 0.00 | 3.61 (2.40–5.42) | 0.00 |
| Severe food insecurity | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 2.44 (1.37–4.37) | 0.00 | 1.97 (0.96–4.01) | 0.06 | 3.41 (1.83–6.35) | 0.00 |
a: Peripheries include: North Lebanon, Bekaa, South Lebanon and Tyre.
b: The health outcome is a composite of: having one or multiple chronic illnesses, acute illness, disability and poor mental health.
c: The baseline reference is: No poor health outcome (n = 489; 20%).
*Bold values: statistical significant associations (P < 0.05).
Our analysis identified strong distinctions between Palestinians living in the capital city Beirut and those living in periphery areas. Refugees living in Beirut were 64% more likely to have one poor health report than those outside the capital, nearly twice as likely to have two health problems (OR: 1.74, CI: 1.22–2.48), and over three times as likely to have three or more health outcomes (OR: 3.61, CI: 2.40–5.42) than those without health reports. Findings for crowding showed a similar trend, with crowded households 21% (OR: 1.21, CI: 1.04–1.41) more likely to report two poor health outcomes and 27% (OR: 1.27, CI: 1.02–1.57) more likely to report three health problems than homes without crowding.
Water leakage in the home was also significantly associated with multi-morbidity. Respondents living in households with water leakage were nearly twice as likely to have three or more health reports (OR: 1.88, CI: 1.45–2.44) than the baseline. This pattern was more pronounced among respondents living in households with severe food insecurity. Those reporting severe food insecurity in the past 6 months were over twice as likely to report one health outcome, and more than three times as likely to report three or more health problems (OR: 3.41, CI: 1.83–6.35).
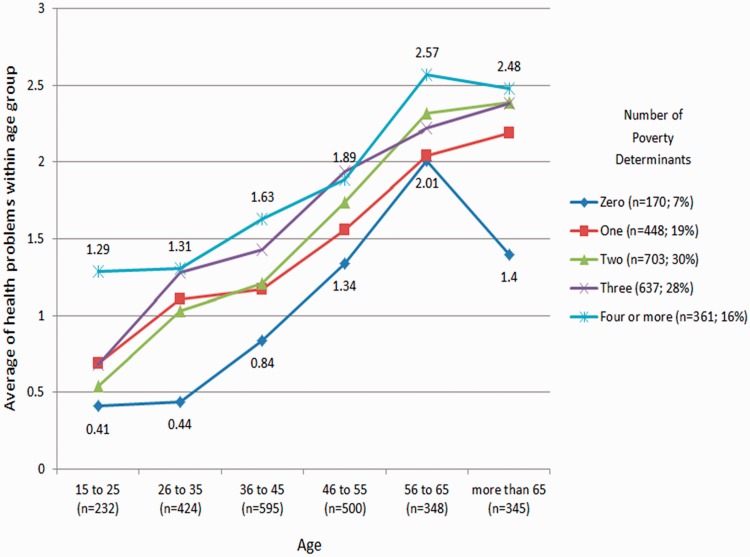
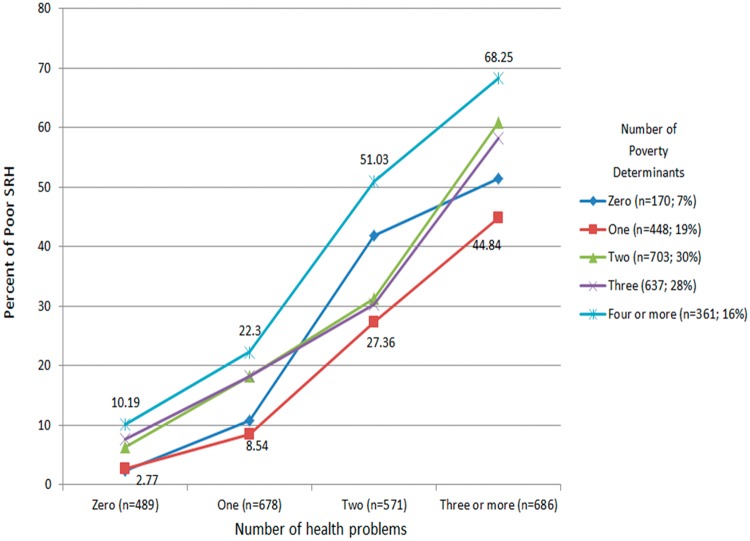
Additional analysis revealed that multi-morbidity was correlated with greater degrees of socioeconomic disadvantage. So while the average number of health problems increased with age in all socioeconomic categories, the most disadvantaged grouping had the highest average health problems in all age categories and the highest socioeconomic grouping had the lowest averages in all age categories (figure 1). A similar pattern was observed when crossing multi-morbidity and self-rated health (figure 2). Those in the lowest socioeconomic group were substantially more likely than respondents with higher SES to report poor self-rated health in all morbidity categories.
Figure 1.
The association of age with the number of health problems and determinants of poverty. (a) Health problems include multiple chronic illness, acute illness, mental illness and disability. (b) Poverty determinants include 1. Educational level (below secondary determined low educational level); 2. Wealth Index (the lowest half determine poor assets); 3. Crowding (above the median = 1.67 people per room was determined as crowded); 4. Water leakage in the household (determined poor condition); and 5. Severe food insecurity (based on the definition provided in the methods)
Figure 2.
The association of self-rated heath with the number of health problems and determinants of poverty. (a) Health problems include multiple chronic illness, acute illness, mental illness and disability. (b) Poverty determinants include 1. Educational level (below secondary determined low educational level); 2. Wealth Index (the lowest half determine poor assets); 3. Crowding (above the median = 1.67 people per room was determined as crowded); 4. Water leakage in the household (determined poor condition); and 5. Severe food insecurity (based on the definition provided in the methods)
Discussion
Our study adds to the mounting evidence of greater multi-morbidity among the poor.12,16,18 The findings reported here demonstrate the inequalities that our health and social systems produce. The correlation between multi-morbidity and poverty indicators highlights a gradient effect of SES on overall health and well-being. This likely reflects dimensions of Palestinian refugees’ social exclusion and economic marginalization, as well as gaps in the aid and social services meant to serve them. Unfortunately, there is no panacea to improve the legal, social and economic status of Palestinians.
Not all Palestinians in Lebanon are poor, yet the majority has low SES and lives in marginalized neighbourhoods. A recent meta-analysis found that neighbourhoods with low SES had increased mortality rates for all area residents regardless of individual SES.31 Improving the neighbourhood environment of Palestinian communities may be one of the more achievable means to improve health outcomes.
Yet Lebanese law prohibits new construction in the camps that house these refugees. Beyond these prohibitions, there are other hurdles (i.e. lack of effective development planning bodies) while resource limitations impede possible infrastructural and environmental improvements. It is in the interest of Lebanese policymakers to work with Palestinian officials toward community revitalization.
Multi-morbidity and health care systems
Our main findings suggest a need to tailor health care regimes for Palestinian refugees with multi-morbidity in mind. Barnett et al.12 suggest that patients with both a mental health problem and chronic condition require the most complex health regimes, needs that most primary and tertiary care centers are unprepared to meet. Mental illness especially complicates self-management aspects of chronic illness, and many physical health care providers have minimal mental health training to guide their response. Over 33% of respondents in this study reported both a mental health problem and at least one chronic condition. This is a clear warning sign given the limited resources dedicated to psychological support in Palestinian refugee communities.
The high prevalence of multi-morbidity among Palestinian refugees in Lebanon is likely to be costly for care-providing organizations like UNRWA and the Palestinian Red Crescent Society (PRCS). A recent report suggested that, in the UK, comorbidities pairing mental illness with a physical ailment increase the cost of care by 45% and could be responsible for at least 12% of health expenditures for long-term care.32 To address this issue, the report suggests primary and tertiary care providers better integrate psychological support resources into health services, improve early identification of mental illness and carry out preventive measures for those already suffering from chronic physical conditions. Another recommendation made by O’Neill et al.33 is for the incorporation of gerontological training into primary care and wider access to geriatric specialist care for people with multi-morbidities.
Though these reforms might better the wellness of Palestinian refugees, achieving even modest improvements present a tall order. The most obvious constraint is resource limitations that only additional international funding can address. UNRWA receives most of its funding from foreign governments and is underfunded as is. Yet, the more salient obstacle is the fragmentation of care provision at all levels of the health system.
Mental health services are provided by a variety of organizations, including UNRWA and a plethora of non-governmental organizations. Primary care is as diversely sourced, while tertiary care is funded and provided by the PRCS, paid out of pocket by patients at private Lebanese hospitals or funded by UNRWA and provided at Lebanese hospitals. This fragmentation requires any successful reform to coordinate multiple institutions that have little historical grounds, common necessity or financial incentive compelling them. On the face of these obstacles, UNRWA could pilot a small-scale ‘mental health and multi-morbidity’ training program for care providers at one of their larger primary care clinics. With success, the project may be scaled up to other centers across the country.
Limitations
The cross-sectional design of our study limited our ability to establish causality, and does not provide insight into how poverty produces multi-morbidity over the life course. There were also several limitations to our measurements of poverty and multi-morbidity, which may have affected our findings. The sample is representative of at-home adults, the majority being women, and not all refugees living in camps and gatherings in Lebanon. Although each component of the deprivation scale showed independent correlations with multi-morbidity, some were more strongly related than others.
Another limitation was the use of self-reported data, which leaves the potential for recall bias or misdiagnosis. To minimize these issues, our research team used lay descriptions of illnesses in the questionnaire and had UNRWA social workers who were familiar with the study participants to conduct the survey. Additionally, the standard of crowding we used was not externally validated. The sample’s median was used as opposed to a local or international standard so that we could identify variations from within the community. It is likely, for example, had we used the Canadian Crowding Index question (‘does your home require one or more additional rooms’) all respondents would have answered ‘yes’.
Conclusion
The literature on social determinants of health has tended to highlight inequalities between the poor and the affluent, yet in developing countries and especially refugee communities ‘poor’ is the norm. This article makes a strong case that research into health and poverty must magnify the spectrum of deprivation that exists within such marginalized communities, hence highlighting the need to reaffirm international commitment to health and poverty alleviation as basic human rights.
Palestinian refugees in Lebanon face an ever-evolving regional political landscape, which has unfortunately defined their health, life and death for three-quarters of a century. Recent events in neighbouring Syria have had perilous implications for health systems serving Palestinians in Lebanon. An estimated 80 000 Palestinians have fled to Lebanon from Syria since late 2012.34 This has put additional burden on an already under-resourced physical, social, economic and health infrastructure. With no clear end in sight to the Syrian conflict and no timeframe of return for these twice-displaced refugees, health systems in Lebanon will continue to strain.
The deprivation faced by Palestinian refugees in Lebanon has been the unfortunate reality of most refugees and stateless persons in the country. Indeed, since World War I, Lebanon has hosted several persecuted communities and populations, victims of conflicts in the region. In the past decade alone, the small country has seen an influx of Iraqi refugees, who also live in precarious conditions,35 followed by an unprecedented flow of Syrian refugees. These displaced people are equal to 25% of Lebanon’s population today. In a country prone to political and economic instability and with an already ailing infrastructure, provision of resources to refugees by the Lebanese state is perhaps an unrealistic expectation. In the meantime, international organizations have been assigned to cater refugee needs. Yet, with serious constraints on funding and a growing list of demands from multiple refugee groups, international agencies such as UNRWA and UNHCR cannot cope anymore on their own. The international community must be more proactive, increasing their funding and support to the organizations providing relief. This will go a long way in guaranteeing short-term security and stability for refugees in Lebanon, while conflicts in the region continue to evolve.
Funding
The European Union SC-A-33/R082/000.
Conflicts of interest: None declared.
Key points.
This research is the first to analyse associations between socioeconomic deprivation and multiple morbidities in the Middle East and among a refugee population.
Mounting evidence suggests higher multi-morbidity rates among people with low SES. Our study found a positive gradient between socioeconomic determinants of deprivation and multi-morbidity among Palestinian refugees in Lebanon.
The study findings reflect basic inequalities produced by health and social systems, especially legal discrimination and underdevelopment affecting refugee communities.
Ending legal discrimination and funding infrastructural, housing and health service improvements may counteract the effects of deprivation. Addressing this problem requires providing a decent livelihood for refugees in Lebanon.
Acknowledgements
The authors thank UNRWA for commissioning this survey and the European Union for providing financial support. The authors also thank the fieldworkers for helping with the data collection, and Robert Habib and Marwan Khawaja for commenting on earlier drafts of this article.
References
- 1.UNRWA. United Nations relief and works agency for Palestine refugees in the near east–An overview. Available at: http://www.unrwa.org/Accessed (21 November 2012, date last accessed) [Google Scholar]
- 2.Hanafi S, Chaaban J, Seyfert K. Social exclusion of Palestinian refugees in Lebanon: reflections on the mechanisms that cement their persistent poverty. Refugee Survey Quarterly. 2012;31:34–53. [Google Scholar]
- 3.Chaaban J, Ghattas H, Habib R, et al. Socio-economic survey of Palestinian refugees in Lebanon. Report published by the American University of Beirut (AUB) and the United Nations Relief and Works Agency for Palestine Refugees in the Near East (UNRWA), 2012. [Google Scholar]
- 4.Abdulrahim S, Khawaja M. The cost of being Palestinian in Lebanon. J Ethn Migr Stud. 2011;37:151–66. [Google Scholar]
- 5.Chatty D, Hundt GL. Children of Palestine: Experiencing Forced Migration in the Middle East. Canada: Berghahn Books; 2005. [Google Scholar]
- 6.Tiltnes AA. Falling behind: a brief on the living conditions of Palestinian refugees in Lebanon. Norway: Fafo Report, 2005. [Google Scholar]
- 7.UNICEF. Palestinian Central Bureau of Statistics (PCBS), Survey on child labour (7–17 years) in Palestinian refugee camps and gatherings in Lebanon, September 2009. Jordan: Preliminary Report, 2009. [Google Scholar]
- 8.UNICEF. Multiple Indicator Survey (MICS) – Round 4: Final report on Palestinian camps and Gatherings in Lebanon 2011. Ramallah – Palestine [in Arabic]. Available at: http://www.childinfo.org/files/MICS4_Lebanon-Palestinians_FinalReport_2011_Ar.pdf (21 October 2013, date last accessed) [Google Scholar]
- 9.Marmot M. Social determinants of health inequalities. Lancet. 2005;365:1099–104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 10.Adda J, Chandola T, Marmot M. Socio-economic status and health: causality and pathways. J Econometrics. 2003;112:57–63. [Google Scholar]
- 11.Galobardes B, Lynch JW, Smith GD. Is the association between childhood socioeconomic circumstances and cause-specific mortality established? Update of a systematic review. J Epidemiol Community Health. 2008;62:387–90. doi: 10.1136/jech.2007.065508. [DOI] [PubMed] [Google Scholar]
- 12.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 13.Salisbury C, Johnson L, Purdy S, et al. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2011;61:e12–21. doi: 10.3399/bjgp11X548929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kadam UT, Croft PR. Clinical multimorbidity and physical function in older adults: a record and health status linkage study in general practice. Fam Pract. 2007;24:412–9. doi: 10.1093/fampra/cmm049. [DOI] [PubMed] [Google Scholar]
- 15.Gijsen R, Hoeymans N, Schellevis FG, et al. Causes and consequences of comorbidity: a review. J Clin Epidemiol. 2001;54:661–74. doi: 10.1016/s0895-4356(00)00363-2. [DOI] [PubMed] [Google Scholar]
- 16.Walker AE. Multiple chronic diseases and quality of life: patterns emerging from a large national sample, Australia. Chronic Illn. 2007;3:202–18. doi: 10.1177/1742395307081504. [DOI] [PubMed] [Google Scholar]
- 17.Van Oostrom SH, Picavet HSJ, Van Gelder BM, et al. Multimorbidity and comorbidity in the Dutch population-data from general practices. BMC Public Health. 2012;12:715. doi: 10.1186/1471-2458-12-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mercer SW, Watt GC. The inverse care law: clinical primary care encounters in deprived and affluent areas of Scotland. Ann Fam Med. 2007;5:503–10. doi: 10.1370/afm.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zabaneh JE, Watt GC, O'Donnell CA. Living and health conditions of Palestinian refugees in an unofficial camp in the Lebanon: a cross-sectional survey. J Epidemiol Commun Health. 2008;62:91–7. doi: 10.1136/jech.2006.054338. [DOI] [PubMed] [Google Scholar]
- 20.Al-Madi Y, Bashour N, Jacobsen LB, et al. Difficult past, Uncertain Future: living conditions among Palestinian refugees in camps and gatherings in Lebanon. Norway: Fafo Report, 2003;409. [Google Scholar]
- 21.Martin L, Leff M, Caloge N, et al. Validation of self-reported chronic conditions and health services in a managed care population. Am J Prev Med. 2000;18:215–8. doi: 10.1016/s0749-3797(99)00158-0. [DOI] [PubMed] [Google Scholar]
- 22.Schneider AL, Pankow JS, Heiss G, Selvin E. Validity and reliability of self-reported diabetes in the atherosclerosis risk in communities study. Am J Epidemiol. 2012;176:738–43. doi: 10.1093/aje/kws156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Habib RR, Mahfoud Z, Fawaz M, et al. Housing quality and ill health in a disadvantaged urban community. Public Health. 2009;123:174–81. doi: 10.1016/j.puhe.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 24.Habib RR, Yassin N, Ghanawo J, et al. Double jeopardy: assessing the association between internal displacement, housing quality and chronic illness in a low-income neighborhood. J Public Health. 2011;19:171–82. doi: 10.1007/s10389-010-0368-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gunn JM, Darshini RA, Densley K, et al. The association between chronic illness, multimorbidity and depressive symptoms in an Australian primary care cohort. Soc Psychiatry Psychiatr Epidemiol. 2012;47:175–84. doi: 10.1007/s00127-010-0330-z. [DOI] [PubMed] [Google Scholar]
- 26. WHO. EUROHIS: Developing Common instruments for health surveys. In: Nosikov A, Gudex C, editors. Biomedical and Health Research, Amsterdam, Netherlands Vol. 57. 2003.
- 27.Veit CT, Ware JE., Jr The structure of psychological distress and well-being in general populations. J Consult Clin Psychol. 1983;51:730–42. doi: 10.1037//0022-006x.51.5.730. [DOI] [PubMed] [Google Scholar]
- 28.Stillman S, McKenzie D, Gibson J. Migration and mental health: evidence from a natural experiment. J Health Econ. 2009;28:677–87. doi: 10.1016/j.jhealeco.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 29.Jylha M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69:307–16. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 30.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–32. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 31.Meijer M, Rohl J, Bloomfield K, Grittner U. Do neighborhoods affect individual mortality? A systematic review and meta-analysis of multilevel studies. Soc Sci Med. 2012;74:1204–12. doi: 10.1016/j.socscimed.2011.11.034. [DOI] [PubMed] [Google Scholar]
- 32.Naylor C, Parsonage M, McDaid D, et al. Long-term Conditions and Mental Health. The cost of Co-morbidities. London: King’s Fund; 2012. [Google Scholar]
- 33.O'Neill D, Cherubini A, Michel JP. Epidemiology of multimorbidity. Lancet. 2012;380:1383. doi: 10.1016/S0140-6736(12)61795-4. [DOI] [PubMed] [Google Scholar]
- 34.ANERA. REPORT. Palestinian Refugees from Syria in Lebanon. Available at: http://www.anera.org/refugeereport/ (12 December 2013, date last accessed) [Google Scholar]
- 35.Chaaban J, Seyfert K, Salti N, Makkaoui G. Poverty and livelihoods among UNHCR registered refugees in Lebanon. Refugee Survey Quarterly. 2013;32:24–49. [Google Scholar]