Abstract
AIM: To evaluate the results of cardiac surgery in cirrhotic patients and to find the predictors of early and late mortality.
METHODS: We included 55 consecutive cirrhotic patients undergoing cardiac surgery between 1993 and 2012. Child-Turcotte-Pugh (Child) classification and Model for End-Stage Liver Disease (MELD) score were used to assess the severity of liver cirrhosis. The online EuroSCORE II calculator was used to calculate the logistic EuroSCORE in each patient. Stepwise logistic regression analysis was used to identify the risk factors for mortality at different times after surgery. Multivariate Cox proportional hazard models were applied to estimate the hazard ratios (HR) of predictors for mortality. The Kaplan-Meier method was used to generate survival curves, and the survival rates between groups were compared using the log-rank test.
RESULTS: There were 30 patients in Child class A, 20 in Child B, and five in Child C. The hospital mortality rate was 16.4%. The actuarial survival rates were 70%, 64%, 56%, and 44% at 1, 2, 3, and 5 years after surgery, respectively. There were no significant differences in major postoperative complications, and early and late mortality between patients with mild and advanced cirrhosis. Multivariate logistic regression showed preoperative serum bilirubin, the EuroSCORE and coronary artery bypass grafting (CABG) were associated with early and late mortality; however, Child class and MELD score were not. Cox regression analysis identified male gender (HR = 0.319; P = 0.009), preoperative serum bilirubin (HR = 1.244; P = 0.044), the EuroSCORE (HR = 1.415; P = 0.001), and CABG (HR = 3.344; P = 0.01) as independent risk factors for overall mortality.
CONCLUSION: Advanced liver cirrhosis should not preclude patients from cardiac surgery. Preoperative serum bilirubin, the EuroSCORE, and CABG are major predictors of early and late mortality.
Keywords: Cardiac surgery, Liver cirrhosis, Risk factor
Core tip: Patients with liver cirrhosis are considered high-risk for cardiac surgery. Information on risk factors to predict operative results was limited. We sought to evaluate the operative results of cardiac surgery in cirrhotic patients and to find the predictors of early and late mortality. Child-Turcotte-Pugh (Child) classification and Model for End-Stage Liver Disease (MELD) score were used to assess the severity of liver cirrhosis. Advanced liver cirrhosis with Child B and C and high MELD score should not preclude patients from cardiac surgery. Preoperative serum bilirubin, the EuroSCORE, and coronary artery bypass grafting are major predictors of early and late mortality.
INTRODUCTION
Patients with liver cirrhosis are considered as a high-risk population for cardiac surgery, and the surgical risk increases with the severity of liver cirrhosis[1-8]. Historically, the severity of liver cirrhosis is evaluated by the Child-Turcotte-Pugh (Child) classification and Model for End-Stage Liver Disease (MELD) score. However, the current preoperative assessment of surgical risk in cirrhotic patients undergoing cardiac surgery is imprecise. In addition, the paucity of reports in the literature makes it difficult to determine an indication for cardiac surgery in patients with liver cirrhosis. This is especially true in patients with advanced liver cirrhosis[1-8]. Therefore, it is important to find specific predictors to assess individual surgical risk before an operation in this population.
Child class and MELD score have been used to predict surgical results in cirrhotic patients undergoing cardiac surgery[5,7,9-15]. However, the small case number, short follow-up duration (< 12 mo) and lack of a multivariate analysis limited the information[1-14]. The EuroSCORE is used traditionally for predicting perioperative mortality after cardiac surgery. The purpose of this study was to evaluate the surgical results of cardiac surgery in cirrhotic patients, to find the predictors of outcomes, and to assess the relevance of Child class, the MELD score, and EuroSCORE in terms of prediction of early and late mortality. This is an update of our previously reported patients[6].
MATERIALS AND METHODS
Patients
This was a retrospective observational study of prospectively collected data. We included all consecutive cirrhotic patients undergoing cardiac surgery between 1993 and 2012 at the National Taiwan University Hospital.
The National Taiwan University Hospital is a 2200-bed tertiary care hospital. It serves an urban population of 2 million as both first-line and tertiary facilities. It serves also as a referral center for other hospitals in the country with a population of 23 million. All data were collected by retrospective chart review. The local institutional medical ethics committee approved the study and waived the need for informed consent.
The diagnosis of liver cirrhosis was based on clinical history and physical stigmata consistent with cirrhosis, and findings of abdominal sonography and/or other imaging studies, which was characterized by a coarsened heterogeneous echo pattern, increased parenchymal echogenicity, and nodularity of the liver surface[6]. The severity of liver cirrhosis was graded according to the Child classification[16,17] and MELD score[18]. The online EuroSCORE II calculator (http://www.euroscore.org/calc.html) was used to calculate the logistic EuroSCORE for each patient.
Management
The details of surgical procedures and postoperative management were described previously[6]. Major postoperative complications included bleeding (profuse chest tube drainage requiring re-exploration), cardiac (postoperative mechanical circulatory support or prolonged inotropic use for more than 72 h), neurological (consciousness disturbance, seizure or stroke), pulmonary (prolonged ventilator support for more than 48 h), infectious (wound infection, bacteremia, pneumonia, or urinary tract infection), gastrointestinal (bowel ischemia or ileus), renal (acute renal failure or need of new dialysis), and hepatic (hepatic function deterioration or hepatic failure).
Data collection
Data on age, sex, medical co-morbidities, pre-surgery laboratory tests, surgical status, surgical procedure, and clinical outcome, including death and major complications, were collected retrospectively from medical records. For those patients who did not attend regular follow-up at our hospital, the information of survival data were obtained by telephone contact or from the National Death Index. The mortality rates were determined at hospital discharge, at 3 mo and annually after surgery.
Statistical analysis
Categorical variables were reported as the percentage of patients in the subgroup. The distributions of continuous variables were examined by the Shapiro-Wilk test. Continuous variables with skewed distributions were presented as medians (interquartile range, IQR). Comparison between groups was performed using the Chi-square test, Fisher’s exact test, and Mann-Whitney test. Stepwise logistic regression analysis was used to identify the risk factors for mortality at different times after surgery. Multivariate Cox proportional hazard models were applied to estimate the hazard ratios (HR) of predictors for mortality. Variables significantly associated with survival time in univariate Cox proportional hazard models and clinically important variables were included in the multivariate analyses. The concordance statistics, which are similar to the area under the receiver-operating characteristic curve (ROC), were used to assess the ability of the statistical model to predict mortality of the patients. They ranged from 0.5 (no predictive ability) to 1 (perfect predictive ability). A two-tailed P-value below 0.05 was considered significant. Stata/SE 9.0 for Windows (StataCorp LP, TX) was used for statistical analyses. The Kaplan-Meier method was used for survival curves and the survival rates between groups were compared using a log-rank test.
RESULTS
Patients
Fifty-five patients with liver cirrhosis were included. There were 43 men and 12 women, with a median age of 60 years (range, 19-84). The etiology of liver cirrhosis was viral in 32 patients, alcoholic in 13 patients, and cardiac in eight patients. Thirteen patients underwent emergency operation, and four patients had previous cardiac surgery. Sixteen patients underwent combined surgical procedures. Major postoperative complications occurred in 38 patients (69%) and included cardiac in 18 patients, infectious in 16, and renal in 14. The in-hospital mortality rate was 16.4%. The causes of in-hospital death included cardiogenic shock in four, sepsis in two, hepatic failure in one, multiple organ failure in one, and ischemic bowel disease in one. Late death occurred in 15 patients. The causes of late death included sepsis in three, hepatic failure in three, heart disease in three, stroke in two, massive gastrointestinal bleeding in one, and unknown cause in three. The actuarial survival rates were 70%, 64%, 56%, and 44% at 1, 2, 3, and 5 years after surgery, respectively. Follow-up was complete for all patients, and the median follow-up duration was 28.6 mo (IQR: 3.2-68.4).
Child classification
There were 30 patients in Child class A, 20 in Child B, and five in Child C. Patient demographics and operative results stratified by mild (Child A) and advanced (Child B and C) liver cirrhosis are shown in Table 1. Patients with advanced liver cirrhosis were younger in age, had a lower level of preoperative blood hemoglobin, and had a lower rate of diabetes mellitus. There was no difference in preoperative EuroSCORE, operative status and types of surgical procedures. Although patients with advanced liver cirrhosis had a longer hospital stay, there were no significant differences of major postoperative complications, in-hospital mortality and late mortality rates up to 5 years between patients with mild and advanced liver cirrhosis (Table 1). As shown in Figure 1, the survival rates of patients with Child class A, B, and C 83%, 85%, 80% at hospital discharge and were 47%, 39%, 50% at 5 years after surgery.
Table 1.
Patient demographics stratified by Child-Turcotte-Pugh classification
| All patients |
Child-Turcotte-Pugh Class |
|||
| A | B and C | P value | ||
| Case number | 55 | 30 | 25 | |
| Male gender | 43 | 22 | 21 | 0.514 |
| Median age in years | 60 (51, 71) | 64.5 (56, 71) | 53 (45, 63) | 0.025 |
| Co-morbidities | ||||
| Diabetes mellitus | 15 | 13 | 2 | 0.005 |
| Hypertension | 16 | 12 | 4 | 0.075 |
| Etiology of liver cirrhosis | ||||
| Viral | 32 | 21 | 11 | 0.052 |
| Alcoholic | 13 | 7 | 6 | 0.954 |
| Cardiac | 8 | 1 | 7 | 0.018 |
| Pre-operative serum level | ||||
| Bilirubin (mg/dL) | 1.3 (0.9, 2.4) | 1.01 (0.84, 1.37) | 2.41 (1.11, 4.13) | < 0.001 |
| Albumin (g/dL) | 3.6 (3.1, 4.0) | 3.8 (3.3, 4.2) | 3.1 (2.8, 3.7) | 0.002 |
| INR | 1.2 (1.1, 1.3) | 1.14 (1.04, 1.2) | 1.3 (1.15, 1.5) | 0.001 |
| Platelet count (K/L) | 119 (91, 176) | 127.5 (94, 199) | 119 (82, 147) | 0.163 |
| Hemoglobin (g/dL) | 11.2 (9.6, 13.1) | 12.4 (11, 13.7) | 10.3 (9.4, 11.6) | 0.005 |
| Creatinine (mg/dL) | 1.2 (1.0, 1.9) | 1.2 (0.9, 1.6) | 1.2 (1, 2) | 0.762 |
| MELD Score | 11 (8, 16) | 9 (7, 11) | 15 (11, 22) | < 0.001 |
| EuroSCORE | 2.6 (1.6, 3.6) | 2.8 (2, 4.8) | 2.2 (1.5, 3.1) | 0.168 |
| Operation-related variables | ||||
| Emergency operation | 13 | 7 | 6 | 1.000 |
| CABG | 13 | 10 | 3 | 0.110 |
| OPCAB | 7 | 6 | 1 | 0.112 |
| Postoperative complications | ||||
| Bleeding | 9 | 3 | 6 | 0.273 |
| Cardiac | 18 | 8 | 10 | 0.294 |
| Pulmonary | 11 | 7 | 4 | 0.736 |
| Gastrointestinal | 2 | 1 | 1 | 1.000 |
| Hepatic | 12 | 4 | 8 | 0.114 |
| Renal | 14 | 6 | 8 | 0.309 |
| Neurological | 7 | 3 | 4 | 0.689 |
| Infectious | 16 | 8 | 8 | 0.665 |
| ICU stay in days | 3 (2, 13) | 3 (2, 7.5) | 3 (2, 16) | 0.368 |
| Hospital stay in days | 17 (12, 36) | 13.5 (10, 32) | 27 (16, 41) | 0.042 |
| Mortality | ||||
| In-hospital | 9 (16.4%) | 5 (16.7%) | 4 (16%) | 1.000 |
| 3-mo | 10 | 5 | 5 | 0.750 |
| 1-yr | 15 | 6 | 9 | 0.136 |
| 2-yr | 17 | 8 | 9 | 0.391 |
| 3-yr | 18 | 9 | 9 | 0.890 |
| 5-yr | 20 | 10 | 10 | 0.709 |
| Follow-up duration (mo) | 28.6 (3.2, 68.4) | 31.4 (5.6, 64.3) | 22.8 (3.0, 62.4) | 0.697 |
Continuous variables were expressed as the median (interquartile range). CABG: Coronary artery bypass grafting; ICU: Intensive care unit; INR: International normalized ratio; MELD: Model for end-stage liver disease; OPCAB: Off-pump coronary artery bypass surgery; WBC: White blood cell count.
Figure 1.
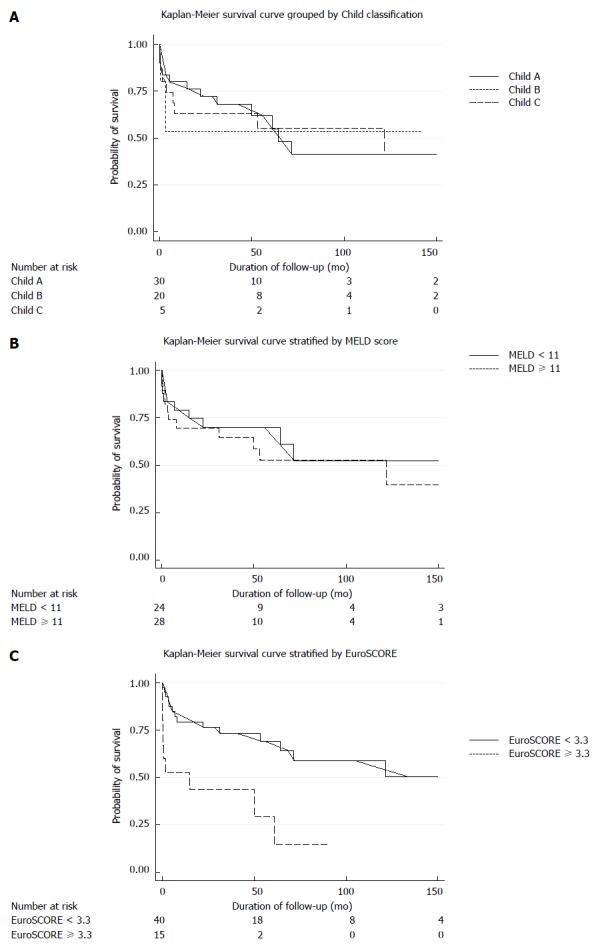
Stratified Kaplan-Meier survival curves. A: Child-Turcotte-Pugh class A, B and C; B: Model for End-Stage Liver Disease score; C: EuroSCORE. Comparison between groups by log-rank test. MELD: Model for End-Stage Liver Disease.
Logistic regression
As shown in Table 2, we used univariate and multivariate stepwise logistic regression to identify independent predictors for early and late mortality. Patient data were compared between survivors and non-survivors at the time points of hospital discharge, 3 mo, 1 year, 2 years, 3 years and 5 years after surgery. Variables listed in Table 1 were included in the analysis. In Table 2, only variables with statistically significant odds ratios for mortality in multivariate analysis are listed. Among them, the preoperative level of serum bilirubin, the EuroSCORE and the procedure of coronary artery bypass grafting (CABG) were independent risk factors for early and late mortality. The Child class and MELD score were not. The predicting value of serum bilirubin was significant at 1 year, 2 years, 3 years and 5 years after operation. The predictive value of the EuroSCORE was significant at hospital discharge, 3 mo, 1 year, and 2 years after surgery. CABG also affected the mortality at 3 mo, 3 years and 5 years after surgery. The odds ratios of the EuroSCORE decreased gradually with time (Table 2).
Table 2.
Risk factors for death by stepwise logistic regression at different times after operation: odds ratios with P value < 0.05
| In-hospital | 3 mo | 1 yr | 2 yr | 3 yr | 5 yr | |
| Patient number | 55 | 55 | 50 | 47 | 41 | 36 |
| Death | 9 | 10 | 15 | 17 | 18 | 20 |
| Mortality rate (%) | 16.4 | 18.2 | 30 | 36.2 | 43.9 | 55.6 |
| Bilirubin | 1.86 (1.11-3.14) | 1.83 (1.05-3.20) | 1.74 (1.04-2.89) | 1.87 (1.02-3.42) | ||
| EuroSCORE | 2.17b (1.32-3.59) | 1.92b (1.19-3.09) | 1.68 (1.10-2.58) | 1.57 (1.04-2.37) | ||
| CABG | 7.14 (1.12-45.58) | 9.00 (1.71-47.48) | 10.62 (1.64-68.84) |
Data are expressed as odds ratio (95%CI).
P < 0.01 vs control. CABG: Coronary artery bypass grafting.
Survival
The survival rates stratified by the Child class, MELD score and EuroSCORE are shown in Figures 1A-C. Patients with preoperative EuroSCORE > 3.3 had a significant improved survival rates after operation (Figure 1C). However, the MELD score > 11 (Figure 1B) and advanced liver cirrhosis (Child class B and C) (Figure 1A) were not significant risk factors for mortality at any time point after surgery.
Cox regression
We used the Cox proportional hazard models for risk factor analysis with regard to time. The variables listed in Table 1 were included in the analysis. Univariate analysis revealed five risk factors and only four of them were independent in multivariate analysis (Table 3). Multivariate analysis identified male gender, preoperative level of serum bilirubin, the EuroSCORE, and CABG as the independent predictors for early and late mortality.
Table 3.
Risk factor for death by Cox hazard proportional models-hazard ratios
| Crude | Full model | Reduced model | |
| Male gender | 0.30b (0.13-0.68) | 0.26b (0.10-0.69) | 0.32b (0.14-0.75) |
| Bilirubin | 1.26a (1.03-1.55) | 1.22 (0.96-1.55) | 1.24a (1.01-1.54) |
| EuroSCORE | 1.44b (1.22-1.71) | 1.46b (1.18-1.81) | 1.42b (1.15-1.74) |
| Multiple procedures | 2.53a (1.08-5.91) | 1.31 (0.51-3.37) | |
| CABG | 2.90a (1.25-6.75) | 4.05b (1.47-11.20) | 3.34b (1.33-8.38) |
P < 0.05;
P < 0.01 vs control. CABG: Coronary arteries bypass grafting.
ROC
In a comparison of Child class, MELD score and EuroSCORE, we found that the Child classification was the least relevant to surgical outcome, with a ROC area of 0.5034, followed by 0.5307 for the MELD score. The ROC area of the EuroSCORE was 0.6008, and that of the serum level of bilirubin was 0.6237. The EuroSCORE was the most significant risk determinant for cardiac surgery in cirrhotic patients, rather than the Child classification and MELD score. The ROC area of the EuroSCORE in Cox model was 0.7151, and the concordance statistics was 0.804, indicating that the EuroSCORE predicted surgical mortality better than the other scores.
DISCUSSION
In this study, we investigated the predictive factors of early and late mortality in cirrhotic patients undergoing cardiac surgery. The in-hospital mortality was 16.4% in the total cohort of 55 cirrhotic patients undergoing cardiac surgery. The early and late mortality identified in this study was comparable with other published reports[1-14]. We found a significantly higher risk for in-hospital, 3 mo, 1 year, 2 years and 3 years mortality in patients with a high EuroSCORE. Surprisingly, Child class and MELD score failed to predicted either early or late mortality. The Kaplan-Meier survival curves further confirmed the predictive role of the EuroSCORE, but not Child class and MELD score. We further identified preoperative level of serum bilirubin and the CABG procedure as independent predictors of overall mortality.
Risk prediction
Several specific scores, such as the EuroSCORE, exist to assess the risk of operative mortality in cardiac surgery. However, the presence and/or severity of liver cirrhosis have not been included in established models of predicting cardiac surgical risk. In patients with liver cirrhosis, specific scores are needed to evaluate the surgical risk.
Many medical tools are used beyond their original intended scope, and often become the standard of care in their new application. The Child score and Child classification were originally designed to predict results after surgery for portal hypertension in patients with liver cirrhosis. It has been used to predict operative mortality in cirrhotic patients after abdominal surgery. The MELD score was originally designed to prioritize organ allocation in patients awaiting liver transplantation, and it has been shown to reflect the 3-mo mortality in patients with end-stage liver cirrhosis. Both Child class and MELD score have been used to predict the results of cardiac surgery in patients with liver cirrhosis[5,7,9-14]. The general consensus is that cardiac surgery can be performed safely in patients with Child class A liver cirrhosis and in selected patients with Child class B liver cirrhosis, but is not recommended in patients with Child class C liver cirrhosis[1-5,7-15]. However, the variables used in Child score were not the result of objective systematic analysis, but rather emerged from clinical experience of small case numbers. Clinicians must determine subjectively the degree of encephalopathy and ascites. The Child score, therefore, is prone to inter-observer variation. On the other hand, the MELD score consists of three objective variables: serum international normalized ratio, total bilirubin, and creatinine levels. The MELD score uses objective parameters and is easy to calculate. The majority of previous studies have demonstrated equivalence or superiority of MELD to Child class in predicting risk[5,10,12,14]. However, other investigators did not agree[7,12,13].
In this study, we used univariate and multivariate logistic regression and Cox regression analysis to determine which scores or variables were most predictive of early and late mortality. The calculated EuroSCORE was highly statistically significant. Serum bilirubin and CABG were also statistically significant. Notably, Child class and MELD score were not significant in our statistical analysis. The EuroSCORE evaluated several different risk factors, including patient-related, cardiac-related and operation-related factors. Our results showed that preoperative cardiac function and the type of surgical procedure were the critical contributors to postoperative mortality.
Advanced liver cirrhosis
Except for our previous report in 2005[6], all other studies in the literature recommended that cardiac surgery is not performed in patients with advanced liver cirrhosis, especially in Child class C[1-5,7-15], because the perioperative mortality rate was 75%-100%. Although there has been a gradual improvement of the operative results in patients with Child class B liver cirrhosis, no improvement was observed in patients with Child class C liver cirrhosis[7]. However, some patients with Child class C liver cirrhosis were facing life-threatening diseases, such as infective endocarditis and severe heart failure, and no therapeutic option other than a cardiac surgical procedure was available. Cardiac surgery should be performed immediately. In this study, we demonstrated that cardiac surgery can be performed safely in patients with advanced liver cirrhosis, even in Child class C liver cirrhosis or with the MELD score > 11. The rates of major postoperative complications and mortality were not significantly increased. The results of the current study do not mean that the severity of liver cirrhosis has no impact on surgical risk and outcome for cardiac surgery in this patient group. The current study and the published literature suggest that advanced liver cirrhosis alone should not preclude patients from cardiac surgery. Rather, other predictors, including patient-related, cardiac-related and procedure-related factors, should be taken into consideration in risk stratification. In addition, the EuroSCORE might provide be better at predicting postoperative mortality than the Child class or MELD score.
Study limitation
Although our study population was larger than most previous reports[1-9,11-13], this study was still limited by the relatively small case number and its retrospective nature. However, this study provided important information. First, our study included an analysis of late outcome, up to 5 years. Second, we found that the EuroSCORE was valid for predicting overall mortality. Child class and MELD scores were not good enough to predict early and late outcome after cardiac surgery in patients with liver cirrhosis. Further validation of the EuroSCORE in large datasets is required.
In conclusion, advanced liver cirrhosis with Child B and C and high MELD score should not preclude patients from cardiac surgery. Preoperative levels of serum bilirubin, EuroSCORE, and CABG were major predictors of early and late mortality.
COMMENTS
Background
The current preoperative assessment of surgical risk in cirrhotic patients undergoing cardiac surgery is imprecise. The paucity of reports in the literature makes it difficult to determine an indication for cardiac surgery in patients with liver cirrhosis. Therefore, it is important to find specific predictors to assess individual surgical risk before surgery in this population.
Research frontiers
Except for their previous report in 2005, all other studies in the literature recommended that cardiac surgery is not performed for patients with advanced liver cirrhosis, especially in Child class C, because the perioperative mortality rate was 75%-100%. Although there has been a gradual improvement of the surgical results in patients with Child class B liver cirrhosis, no improvement was observed in patients with Child class C liver cirrhosis.
Innovations and breakthroughs
In this study, the authors used univariate and multivariate logistic regression and Cox regression analysis to determine which scores or variables were most predictive of early and late mortality.
Applications
The purpose of this study was to evaluate the surgical results of cardiac surgery in cirrhotic patients, to find the predictors of outcomes, and to assess the relevance of Child class, the Model for End-Stage Liver Disease (MELD) score, and EuroSCORE in terms of prediction of early and late mortality. This is an update of our patients reported previously.
Peer review
The author found that the MELD score and Child classification had no influence on patient survival; however, strikingly, the mortality rate of this cohort was 16%, which is very high for the age group of the patients.
Footnotes
P- Reviewer: Firstenberg FS, Hirose H, Won M, Zhu X S- Editor: Qi Y L- Editor: Stewart G E- Editor: Zhang DN
References
- 1.Klemperer JD, Ko W, Krieger KH, Connolly M, Rosengart TK, Altorki NK, Lang S, Isom OW. Cardiac operations in patients with cirrhosis. Ann Thorac Surg. 1998;65:85–87. doi: 10.1016/s0003-4975(97)00931-4. [DOI] [PubMed] [Google Scholar]
- 2.Bizouarn P, Ausseur A, Desseigne P, Le Teurnier Y, Nougarede B, Train M, Michaud JL. Early and late outcome after elective cardiac surgery in patients with cirrhosis. Ann Thorac Surg. 1999;67:1334–1338. doi: 10.1016/s0003-4975(99)00226-x. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan M, Cimen S, Kut MS, Demirtas MM. Cardiac operations for patients with chronic liver disease. Heart Surg Forum. 2002;5:60–65. [PubMed] [Google Scholar]
- 4.Hayashida N, Shoujima T, Teshima H, Yokokura Y, Takagi K, Tomoeda H, Aoyagi S. Clinical outcome after cardiac operations in patients with cirrhosis. Ann Thorac Surg. 2004;77:500–505. doi: 10.1016/j.athoracsur.2003.06.021. [DOI] [PubMed] [Google Scholar]
- 5.Suman A, Barnes DS, Zein NN, Levinthal GN, Connor JT, Carey WD. Predicting outcome after cardiac surgery in patients with cirrhosis: a comparison of Child-Pugh and MELD scores. Clin Gastroenterol Hepatol. 2004;2:719–723. doi: 10.1016/s1542-3565(04)00296-4. [DOI] [PubMed] [Google Scholar]
- 6.Lin CH, Lin FY, Wang SS, Yu HY, Hsu RB. Cardiac surgery in patients with liver cirrhosis. Ann Thorac Surg. 2005;79:1551–1554. doi: 10.1016/j.athoracsur.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 7.Filsoufi F, Salzberg SP, Rahmanian PB, Schiano TD, Elsiesy H, Squire A, Adams DH. Early and late outcome of cardiac surgery in patients with liver cirrhosis. Liver Transpl. 2007;13:990–995. doi: 10.1002/lt.21075. [DOI] [PubMed] [Google Scholar]
- 8.An Y, Xiao YB, Zhong QJ. Open-heart surgery in patients with liver cirrhosis. Eur J Cardiothorac Surg. 2007;31:1094–1098. doi: 10.1016/j.ejcts.2007.01.042. [DOI] [PubMed] [Google Scholar]
- 9.Morisaki A, Hosono M, Sasaki Y, Kubo S, Hirai H, Suehiro S, Shibata T. Risk factor analysis in patients with liver cirrhosis undergoing cardiovascular operations. Ann Thorac Surg. 2010;89:811–817. doi: 10.1016/j.athoracsur.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 10.Thielmann M, Mechmet A, Neuhäuser M, Wendt D, Tossios P, Canbay A, Massoudy P, Jakob H. Risk prediction and outcomes in patients with liver cirrhosis undergoing open-heart surgery. Eur J Cardiothorac Surg. 2010;38:592–599. doi: 10.1016/j.ejcts.2010.02.042. [DOI] [PubMed] [Google Scholar]
- 11.Gundling F, Seidl H, Gansera L, Schuster T, Hoffmann E, Kemkes BM, Eichinger B, Gansera B, Schepp W, Schmidtler F. Early and late outcomes of cardiac operations in patients with cirrhosis: a retrospective survival-rate analysis of 47 patients over 8 years. Eur J Gastroenterol Hepatol. 2010;22:1466–1473. doi: 10.1097/MEG.0b013e32834059b6. [DOI] [PubMed] [Google Scholar]
- 12.Vanhuyse F, Maureira P, Portocarrero E, Laurent N, Lekehal M, Carteaux JP, Villemot JP. Cardiac surgery in cirrhotic patients: results and evaluation of risk factors. Eur J Cardiothorac Surg. 2012;42:293–299. doi: 10.1093/ejcts/ezr320. [DOI] [PubMed] [Google Scholar]
- 13.Macaron C, Hanouneh IA, Suman A, Lopez R, Johnston D, Carey WW. Safety of cardiac surgery for patients with cirrhosis and Child-Pugh scores less than 8. Clin Gastroenterol Hepatol. 2012;10:535–539. doi: 10.1016/j.cgh.2011.12.030. [DOI] [PubMed] [Google Scholar]
- 14.Arif R, Seppelt P, Schwill S, Kojic D, Ghodsizad A, Ruhparwar A, Karck M, Kallenbach K. Predictive risk factors for patients with cirrhosis undergoing heart surgery. Ann Thorac Surg. 2012;94:1947–1952. doi: 10.1016/j.athoracsur.2012.06.057. [DOI] [PubMed] [Google Scholar]
- 15.Modi A, Vohra HA, Barlow CW. Do patients with liver cirrhosis undergoing cardiac surgery have acceptable outcomes? Interact Cardiovasc Thorac Surg. 2010;11:630–634. doi: 10.1510/icvts.2010.241190. [DOI] [PubMed] [Google Scholar]
- 16.Child CG III, Turcott JG. Surgery and portal hypertension. In: Child CG III, editor. The liver and portal hypertension. Philadelphia, PA: Saunders; 1964. pp. 50–58. [Google Scholar]
- 17.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 18.Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, TerBorg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2001;34:215–216. doi: 10.1053/he.2000.5852. [DOI] [PubMed] [Google Scholar]


