Abstract
We investigated the effect of propofol and fentanyl on microelectrode recording (MER) and its clinical applicability during subthalamic nucleus (STN) deep brain stimulation (DBS) surgery. We analyzed 8 patients with Parkinson's disease, underwent bilateral STN DBS with MER. Their left sides were done under awake and then their right sides were done with a continuous infusion of propofol and fentanyl under local anesthesia. The electrode position was evaluated by preoperative MRI and postoperative CT. The clinical outcomes were assessed at six months after surgery. We isolated single unit activities from the left and the right side MERs. There was no significant difference in the mean firing rate between the left side MERs (38.7±16.8 spikes/sec, n=78) and the right side MERs (35.5±17.2 spikes/sec, n=66). The bursting pattern of spikes was more frequently observed in the right STN than in the left STN. All the electrode positions were within the STNs on both sides and the off-time Unified Parkinson's Disease Rating Scale part III scores at six months after surgery decreased by 67% of the preoperative level. In this study, a continuous infusion of propofol and fentanyl did not significantly interfere with the MER signals from the STN. The results of this study suggest that propofol and fentanyl can be used for STN DBS in patients with advanced Parkinson's disease improving the overall experience of the patients.
Graphical Abstract
Keywords: Parkinson Disease, Microelectrodes, Propofol, Fentanyl, Subthalamic Nucleus, Deep Brain Stimulation
INTRODUCTION
Deep brain stimulation (DBS) of the subthalamic nucleus (STN) reduces motor disability, motor fluctuations and levodopa-induced dyskinesias (1). Intraoperative microelectrode recordings (MER) and clinical monitoring with electrical stimulation of the STN have been recommended for the accurate positioning of the electrodes in the STN (2, 3). These procedures have the STN DBS done usually under local anesthesia (LA).
It is reported that the intraoperative use of propofol can alleviate the patients' discomfort but interfere with the electrophysiological signals (4, 5, 6). However, it has not been thoroughly evaluated regarding how much it influences the electrical signals of MER during the STN DBS and the accuracy of positioning the electrodes after surgery. The purpose of this study was to investigate the influence of propofol and fentanyl on microelectrode recording and their applicability in STN DBS.
MATERIALS AND METHODS
Patients and clinical evaluation
Seventeen patients received a bilateral STN DBS operation under LA between October 2010 and June 2011 as described elsewhere (7). Eight patients whose electrical signals for MER were recorded from both sides for the comparative analysis were included in this study. The patients were evaluated with the use of the Unified Parkinson Disease Rating Scale (UPDRS), Hoehn and Yahr (H&Y) Staging, Schwab and England Activities of Daily Living (SEADL), the Short Form-36 Health Survey (SF-36), and neuropsychological tests. Evaluations were performed before surgery and 6 months after surgery. The neurological evaluations were performed by two neurologists. Patients were assessed in two conditions (off medication when the patients had taken no medication for 8 to 12 hr and on medication when the patients had experienced maximal clinical benefit 1 to 3 hr after the usual morning dose of dopaminergic treatment) before and after surgery. The levo-dopa equivalent daily dose (LEDD) was computed as described elsewhere (7). The clinical information of the eight patients with advanced Parkinson's disease (PD) who had undergone bilateral STN stimulation is summarized in Table 1.
Table 1.
Clinical findings of the 8 patients with advanced Parkinson's disease
ADL, Activities of Daily Life; LEDD, Levodopa equivalent daily dose; UPDRS, Unified Parkinson's Disease Rating Scale.
Surgical procedure
Anti-Parkinsonian drugs were tapered over two days and stopped overnight before the surgery. In all cases, a stereotactic Leksell®-G frame (Elekta Instruments AB, Stockholm, Sweden) was mounted on the head of the patients under LA. Brain images were acquired on a 1.5-T Signa system (General Electric Medical System, Milwaukee, WI, USA). The STNs were localized by a combination of direct visualization with MRI, MER, and an intraoperative stimulation technique as previously described elsewhere (7). The FSPGR 3-D sequence was used for anterior commissure (AC) - posterior commissure (PC) calculations. To better define the STN, T2 spin-echo images were obtained. Planning of STN targeting and selection of trajectories were accomplished with SurgiPlan® (Eleckta, Stockholm, Sweden). The characteristic discharge of the left STN was identified using multichannel MER by LeadPoint (Medtronic, Minneapolis, MN, USA). Additionally, a trial stimulation to assess clinical improvement was carried out before the permanent quadripolar electrodes (DBS 3389, Medtronic) were positioned in the middle of the area of discharge. Then, the same procedure was performed for right side, under the monitored anesthesia care (MAC) with continuous infusion of propofol (25 µg/kg/min) and fentanyl (25 ng/kg/min). The depth of sedation was estimated with the degree of the patients' awakening response to a loud sound and shaking as well as the response to pinching. The permanent quadripolar electrodes were positioned in the middle of the area of discharge. Then, the stereotactic frame was removed and the implantable pulse generators (IPG) (Medtronic) were then implanted in a subcutaneous pocket below the clavicle under general anesthesia in a single session. Electrical stimulation was started one day after surgery. The stimulation parameters and medications were progressively adjusted using an N'vision® programmer (Medtronic) as previously described elsewhere (7).
Analysis of microelectrode recordings
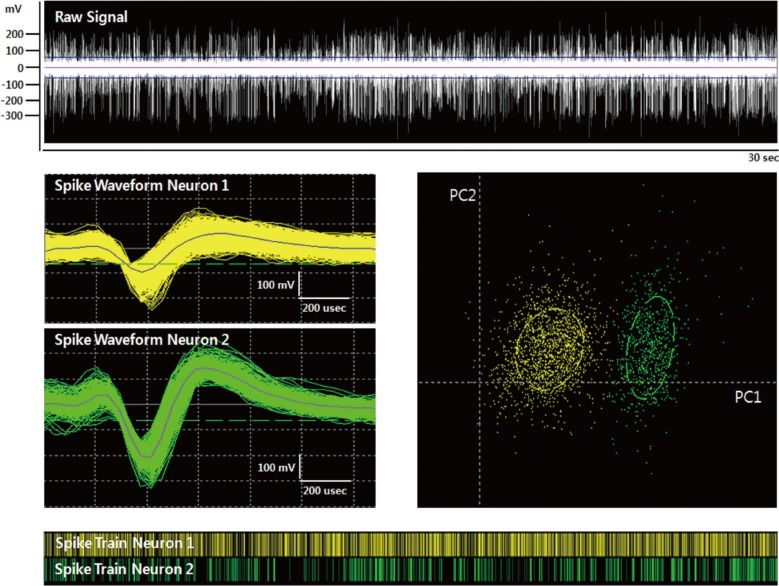
The MER signals along the finally selected trajectories were selected for the analysis. Each MER signal was band-pass filtered at 500-5,000 Hz with a gain 10,000 and was sampled at a rate of 24 kHz. Only an MER signal having stable single/multiunit activity that was clearly over the amplitude of the background noise baseline was selected and a threshold was applied to detect spikes. We isolated a total of 78 single unit activities under LA and 66 single unit activities under MAC. Spike sorting for a single unit was performed using the Offline Sorter software (Offline Sorter, Plexon, TX, USA). Principal components were calculated for unsorted waveforms and the waveforms were assigned to the clusters using the expectation-maximization algorithm based on the T-distribution method (Fig. 1). Two statistical parameters, the J3 statistic and the Davies-Bouldin (DB) validity, were used to examine sorting quality statistics between classified clusters. A high value for the J3 statistic and a low value for the DB validity indicate that the clusters are compact and well-separated.
Fig. 1.
A sorted single unit on microelectrode recording. This figure demonstrates a sorted single unit. The expectation-maximization algorithm was applied to raw signal (white) for getting isolated unit waveforms (green) from noise signal (yellow). Top, raw spiking activity; middle left, unit waveforms (green) and isolated form noise (yellow); middle right, isolated unit and noise on a principle component plot (x-axis, PC1;y-axis, PC2); bottom, raster trace of unit events (green) and noise events (yellow) over a selected time period.
Image fusion of preoperative MRI and postoperative CT
For all patients 3-D spiral stereotactic CT scans (64-channel Brilliance CT, Philips, Eindhoven, the Netherlands) with a 1-mm slice thickness were taken at an immediate postoperative period and one month after bilateral STN stimulation to localize the electrodes by image fusion with the preoperative MRI by using mutual information techniques as previously described elsewhere (7). With CT-MRI image fusion, the electrode positions were plotted on the human brain atlas of Schaltenbrand and Wharen (8).
Statistical analysis
The data for the aforementioned variables were presented as the mean±standard deviation. To examine the effect of anesthesia and the pattern on the mean firing rate and the effect of different combinations of anesthesia and the pattern on the mean firing rate, analysis of variance (ANOVA) was performed.
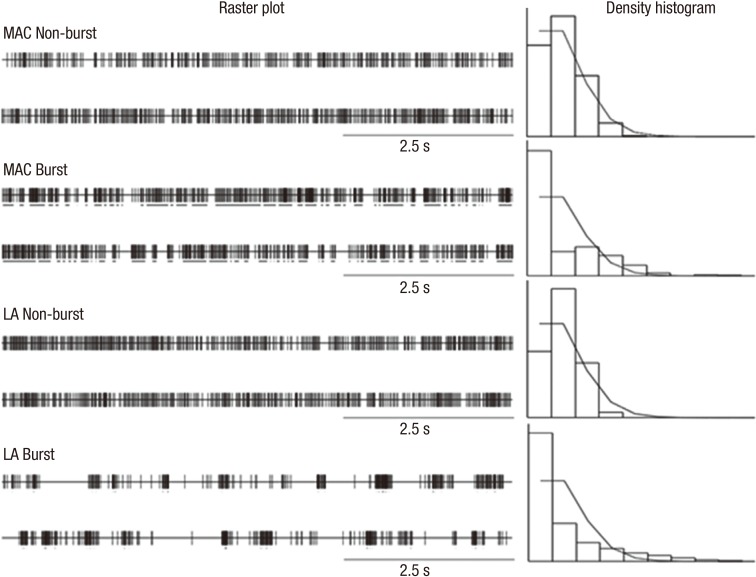
Single unit activity was classified as non-burst (tonic, irregular), or as a burst discharge pattern using the method of the previous study (9). The discharge density histogram was estimated from each 30-sec spike train containing at least 300 spikes. A tonic discharge pattern was characterized by a quasi-normal density distribution histogram. An irregular discharge pattern was characterized by a Poisson distribution, and a burst discharge pattern was tested with the chi-square test from a Poisson distribution with a mean of 1.0 and characterized by a significant different distribution histogram (P<0.05), a significantly positive skewness (P<0.05) of the density distribution histogram and a minimum of four spikes per burst (Fig. 2).
Fig. 2.
Burst discharge patterns on microelectrode recording. This figure shows results of burst discharge patterns under the MAC and the LA conditions. Spike discharge in left column and discharge density histogram in right column with/without burst discharge patterns in MAC and LA.
Paired and unpaired t-tests were used for the comparison of means and Fisher's exact test for the comparison of variables measured at the baseline before surgery and 6 months after surgery. P values of 0.05 were considered to indicate statistical significance. All statistical analyses were used in SAS statistical software (Version 9.0).
Ethics statement
This study was approved by the institutional review board of the Seoul National University Hospital (IRB No. H-1402-057-555). Informed consent was exempted by the board.
RESULTS
The demographics in Table 1 show that the eight patients of this cohort study group were similar to those in our previous studies regarding age, sex ratio, age of onset of PD, duration of PD and preoperative levodopa equivalent dosage (7). There were no perioperative complications.
Results of MER analysis
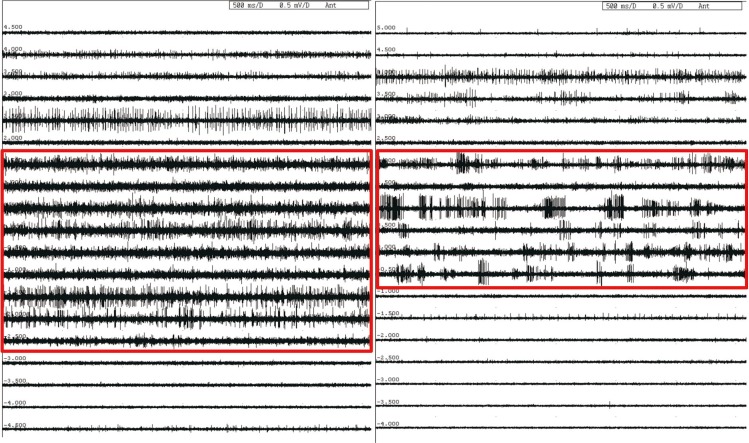
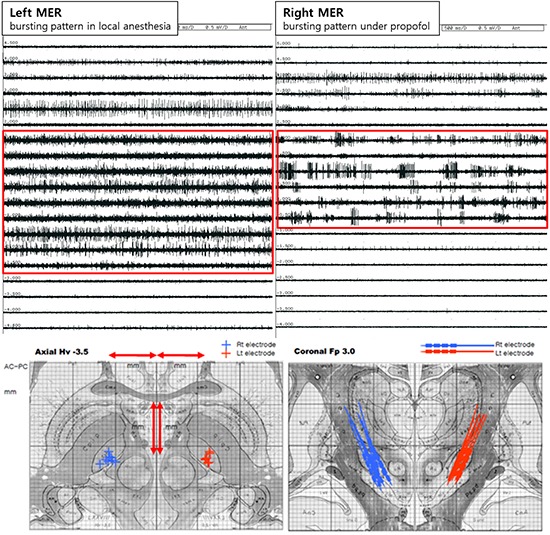
The typical STN bursting pattern and widening of the signal background noise baseline could be identified by the interaoperative MER under LA. A typical bursting pattern in MAC could be also identified, whereas the signal background noise baseline seemed to be slightly reduced (Fig. 3). The mean firing rates were 38.7±16.8 spikes/sec for LA, and 35.5±17.2 spikes/sec for MAC. There was no significant difference in mean firing rate between the LA and MAC conditions (P=0.256).
Fig. 3.
Typical bursting patterns (see the boxes). The typical bursting patterns are demonstrated according to anesthetic methods. Left column, bursting pattern in LA; Right column, bursting pattern in MAC.
The recorded neuronal discharge exhibited two types of discharge pattern. The majority of the single unit STN neurons under LA had a burst discharge pattern (52.6%), and the remainder exhibited a non-burst discharge pattern (47.4%). In the case of the MAC, the majority of the single unit STN neurons exhibited a burst discharge pattern (75.4%), and the non-bursting activity had an irregular discharge pattern (24.6%). The relative proportion of these discharge patterns differed significantly between the LA and MAC (P=0.006).
Since the mean firing rate between the LA and MAC conditions was different significantly, to examine whether the mean firing rate is affected by bursting and non-bursting patterns and whether there is the interaction effects of anesthesia and pattern on the mean firing rate, ANOVA was performed. ANOVA showed a significant difference in pattern (PATTERN, P<0.001), but no significant differences in anesthesia and the combination of two factors (ANESTHESIA, P=0.174: PATTERN×ANESTHESIA, P=0.247, respectively).
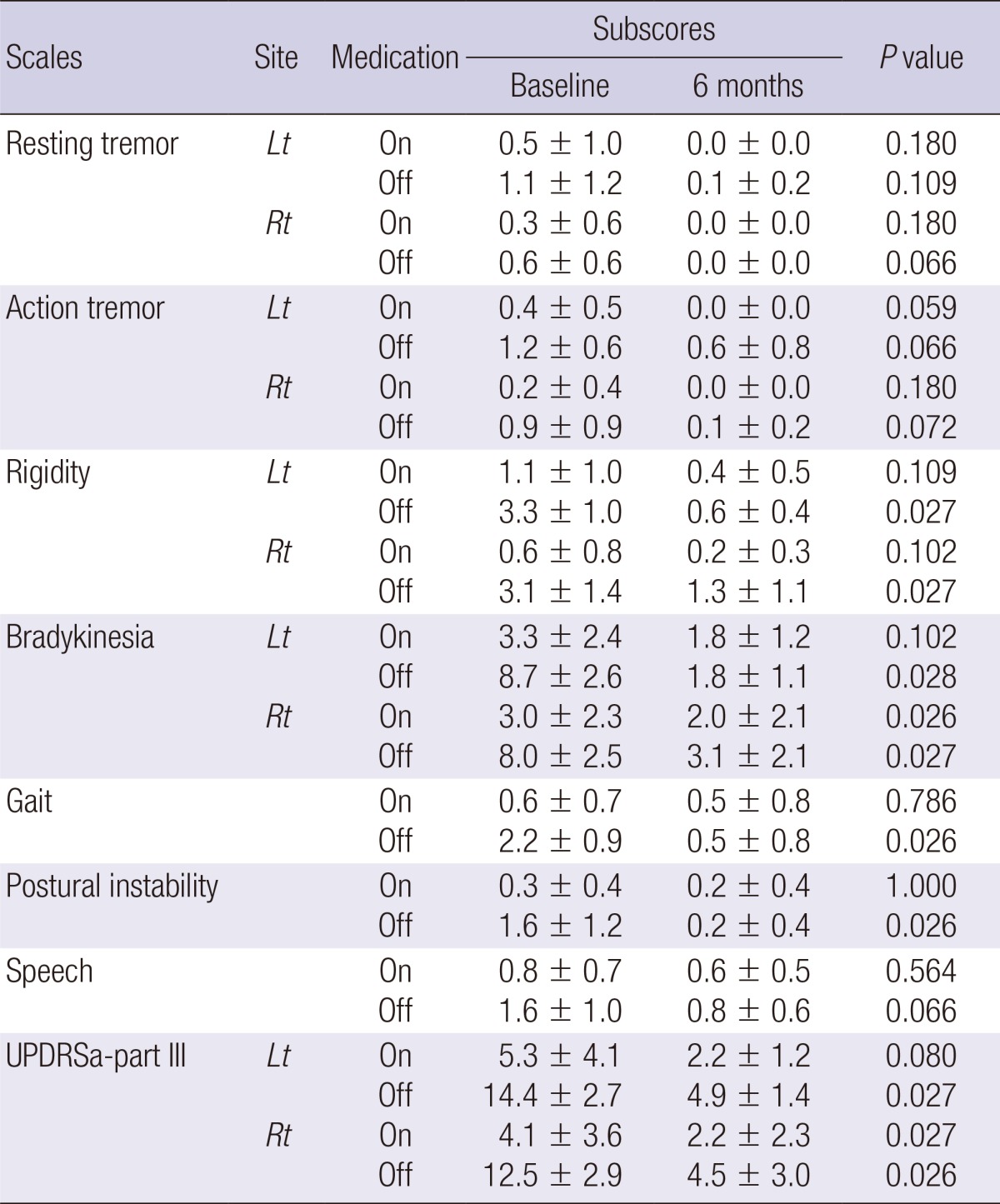
Results of electrode position after bilateral STN DBS
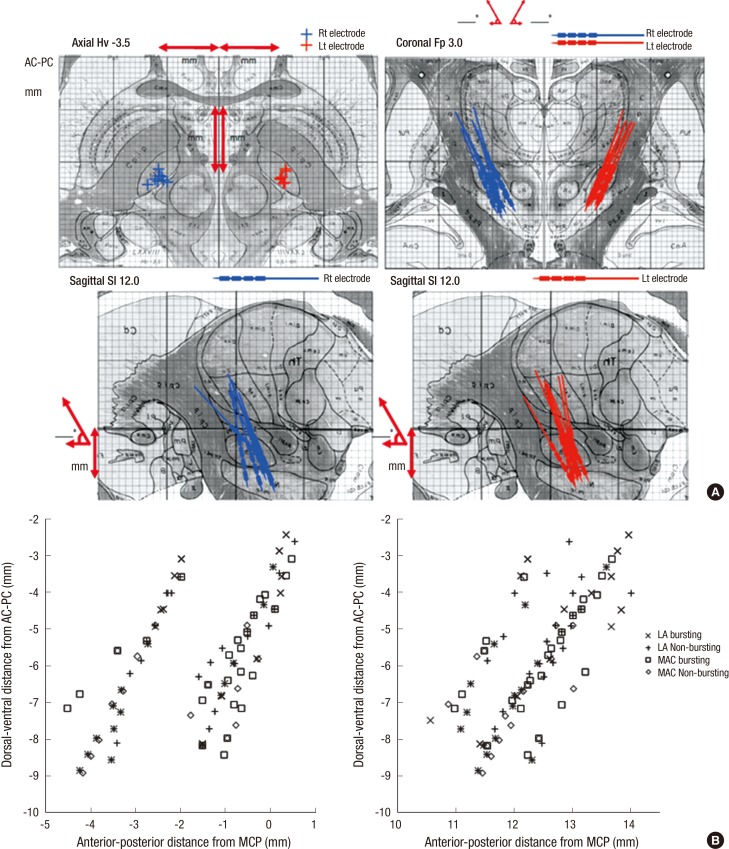
Based on the intraoperative MER findings, the microelectrodes positions were plotted in the sagittal and coronal planes aligned along the AC-PC line. All the electrode positions of 8 patients were within the STNs on both sides in the reformatted axial images of the fused images between the preoperative MRI and postoperative CT taken one month after surgery (Fig. 4).
Fig. 4.
Location of the electrodes plotted onto the human brain atlas. Based on the CT-MRI fusion images of the preoperative brain MRI and postoperative brain CT scan taken one month after surgery. All the electrode positions are mostly located to the middle one third part of the STNs on both sides in the fused images. (A) It shows location of the electrodes plotted onto the human brain atlas of Schaltenbrand and Wahren. (B) The microelectrodes positions were plotted in the sagittal and coronal planes aligned along anterior commissure and posterior commissure line (AC-PC line).
Results of Clinical Outcome 6 months after bilateral STN DBS
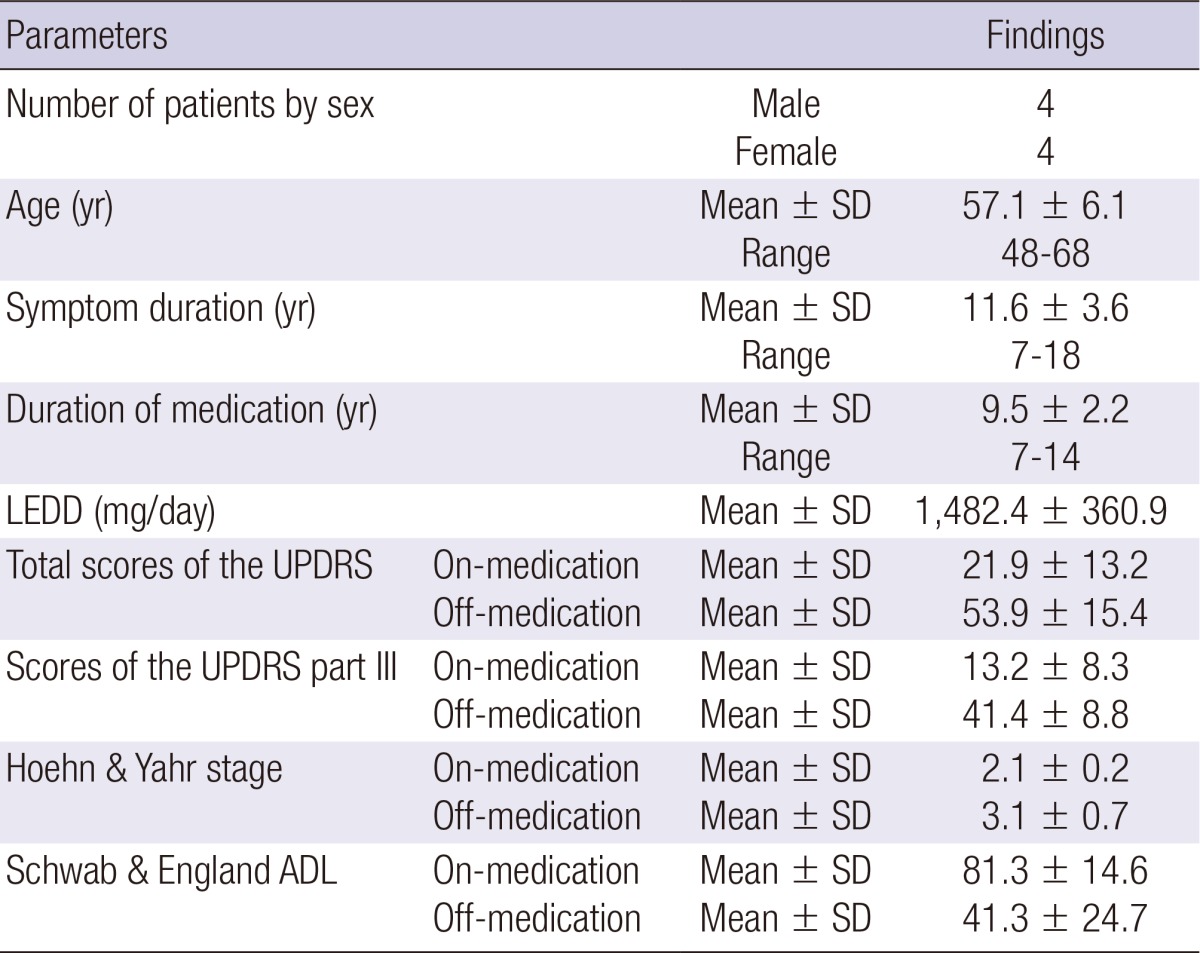
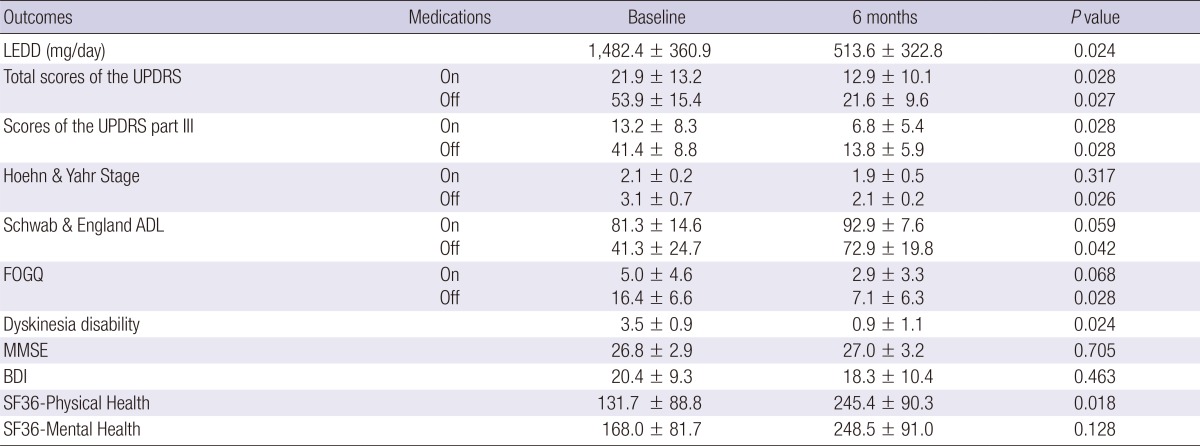
The clinical outcome was compared between the preoperative and postoperative status 6 months after bilateral STN stimulation (Tables 2 and 3). Significant improvement in the off-time scores for the total UPDRS, UPDRS III, H&Y scores, SEADL, and dyskinesia disability with decreased LEDD was observed 6 months after surgery. The LEDD was decreased 6 months after surgery (1,482.4±360.9 mg/day at baseline and 513.6±322.8 mg/day at 6 months; P=0.024). Regarding the eight sub-scales of the SF-36, the scores for bodily pain and summary scores for physical health and mental health were improved 6 months after the surgery.
Table 2.
Clinical outcomes of the 8 patients with advanced Parkinson's disease 6 months after bilateral subthalamic nucleus deep brain stimulation
ADL, Activities of Daily Life; BDI, Beck Depression Inventory; FOGQ, Freezing of Gait Questionnaire; LEDD, Levodopa equivalent daily dose; MMSE, Mini-mental state examination; SF 36, Short Form-36; UPDRS, Unified Parkinson's Disease Rating Scale.
Table 3.
UPDRS III subscores of the 8 patients with advanced Parkinson's disease
UPDRS, Unified Parkinson's Disease Rating Scale.
From the neuropsychological evaluation, the verbal memory test using the Rey-Kim memory battery showed a decline in recognition 6 months after the surgery (P=0.002), whereas nonverbal memory showed no meaningful change. In the frontal lobe function tests, the Stroop test (Stroop-a, P=0.006; Stroop-b, P=0.004; Stroop-c, P=0.034) and the fluency test (P=0.013) scores tended to be worse 6 months after the surgery (P=0.046 for Stroop-a; P=0.053 for fluency); however, they lacked statistical significance after a Bonferroni correction. Other tests including the Boston Naming test, Grooved Pegboard test, Mini-Mental state examination, Trail-Making test, Beck Depression Inventory, and Wisconsin Card Sorting test, did not show any significant changes.
DISCUSSION
Since the introduction of DBS by Benabid and colleagues in 1987, this technique has become the preferred treatment for patients with advanced PD showing motor fluctuation and dyskinesia after long-term medication (10). The clinical outcome of advanced PD patients after STN DBS depends on careful patient selection and optimal targeting of the STN. Precise positioning of the electrodes in the STN is considered the most important factor to achieve good clinical outcome following STN DBS in appropriately selected surgical candidates. However, many unexpected factors, such as brain shift due to CSF leakage, electrode artifacts in the MRI, errors in the image fusion, and manipulation errors from instruments make it difficult to precisely position the electrodes in the center of the STN using only the method of image-based targeting (11, 12, 13). Therefore, MER and intraoperative stimulation tests were adopted to improve the accuracy of the electrode location (2). Thus, STN DBS has been performed with awake and cooperative patients in most cases. For those reasons, anti-parkinsonian drugs should be stopped overnight before surgery and the patients fasted for approximately 12 hr on the day of surgery, which can be a painful memory for most patients with advanced PD.
Sedatives have been used in some cases to alleviate severe anxiety, painful dystonia or respiratory difficulties experienced by the patients who were unable to tolerate the whole procedure of bilateral STN DBS (14). Propofol has been widely used alone or combined with remifentanyl. The mean infusion rate of propofol reported in the literature is approximately 50 µg/kg/min (15, 16). The use of propofol alleviates intraoperative patients' discomfort to make the operating time shorter and frees the patients from a bad memory of the painful procedure of bilateral STN DBS. It can also allow neurosurgeons to concentrate on the surgical procedure for the accurate positioning of the electrodes because there is no need to communicate with the sleeping patients. However, there are two concerns regarding the use of propofol in STN DBS. One is about the selective depression of cerebral activity and the reduction of electrophysiological signals by propofol. The other one is that the patients could not be cooperative during the operation to observe the clinical benefits and adverse effects from the intraoperative stimulation tests of STN.
Regarding depression of the electrophysiological signals, there are few reports in the literature on the use of propofol for STN DBS (4, 5, 6, 17, 18). In addition, neuronal firing patterns are not well characterized and there are no prospective, randomized, blinded studies to compare their clinical outcome with that of an awaken technique. In this study, we found that the continuous infusion of propofol and fentanyl did not significantly interfere with the mean firing rates of the STN in comparison with awake monitoring in the same patient and showed good clinical outcomes comparable to a previous report (7). The results of the mean firing rates in both awake and MAC conditions are similar to some previous reports ranging between 33.1 Hz and 42.3 Hz (3, 19, 20, 21, 22, 23, 24, 25). These results imply that the MAC has just minimal effects on the firing rate of STN neurons in PD patients. In this study, the typical STN bursting patterns in both awake and MAC conditions could be identified (Fig. 3). These results are consistent with the previous findings observed under various anesthetic conditions with propofol and remifentanyl in the literature (4, 9, 26). Most of the signal background noise baselines seemed to be slightly reduced under MAC compared with the awakened status. Meanwhile, they were significantly wider than the baseline outside the STN. Based on these observations, it is suggested that the MAC has little effect on the STN background activity.
The prominent burst discharge pattern of the STN is considered one of the characteristics in a parkinsonian state. We classified the single unit activity of STN neurons into two discharge patterns with a method based on the discharge density histogram. We found that the burst discharge pattern was a predominant feature in both conditions. To assess whether MAC could change the single unit discharge pattern of the STN, we compared the relative proportion of two main patterns between the awake and MAC conditions. The proportion of burst discharge pattern was increased in the MAC (75.4%) compared to the awaken status (52.6%). To assess the possibility of topographical recording bias within the STN, we present a topographical distribution of the burst and non-burst discharge patterns within the STN in each condition, respectively (Fig. 4). Because there was no particular different topographical distribution of the different discharge patterns, the recording bias cannot be regarded as a significant factor to influence the results. Therefore, the different patterns of burst discharge observed may be a result of the difference between the awake and MAC conditions rather than the recording bias within the STN.
Regarding the different patterns of burst discharge, Rodriguez-Oroz et al. found burst-like activity in 60.5% of the single unit STN neurons in awake PD patients, using a different analysis method and named it "irregular activity with long pause" (22). Likewise, Steigerwald et al. classified 70% of the single unit discharge activities of the STN neurons in the awake status as bursting using a method based on ISI distribution (24). Although there was some difference in the relative proportion between the awake and MAC conditions, our relative proportions are closely coincident with previous studies, supporting that our result is valid (3, 19, 20, 21, 22, 23, 24, 25).
The result of ANOVA showed a significant difference in the pattern (PATTERN, P<0.001; ANESTHESIA, P=0.174), confirming the different types of pattern did affect the mean firing rate, whereas indicating two types of anesthesia states did not affect the mean firing rate. In addition, the types of anesthesia did not interact with the types of pattern each other (PATTERN×ANESTHESIA, P=0.247), indicating that interpretation of the main effects is complete, namely, the mean firing rate was affected by the different types of pattern not by the types of anesthesia.
We conclude that the MAC does alter the single unit discharge pattern of the STN and it is the only type of pattern that affects the mean firing rate of the STN. Despite some differences in the MER signals between the LA and MAC conditions, there is no difficulty in identifying the MER signals characteristic of the STN under MAC with continuous infusion of propofol and fentanyl shown in Fig. 3.
It is very difficult for the patients to endure the whole procedure of bilateral STN DBS and properly respond to the intraoperative stimulation tests in the awaken status, although sedation might disturb the assessment of clinical responses and complications by DBS (27, 28). Fortunately, we found no difference in the electrode positions in all eight patients; all electrodes were located within STN on both sides (Fig. 4). The clinical outcomes of the eight patients were also comparable to the results of our previous reports in which both sides STN DBS were performed in the awaken status. There was no difference in the UDPRS total scores and part III subscores six months after STN DBS when compared to our previous results (26).
This study has several limitations. First, we did not monitor the depth of anesthesia in this study. The depth of sedation was estimated only by the degree of the patients' awakening response to loud sound and shaking as well as their response to pinching in this study. The monitoring of the depth of anesthesia to titrate sedation and the state of arousal during DBS insertion would be ideal. The Bispectral index (BIS) is used to monitor the depth of anesthesia (16, 29, 30). A BIS value of 65-85 is recommended for sedation and 40-65 for general anesthesia. Second, the number of patients in this study was limited and the analysis was done retrospectively.
In conclusion, we compared MER signals between awake and MAC conditions in eight advanced PD patients treated with bilateral STN DBS as well as their clinical outcomes six months after surgery. We found that the continuous infusion of propofol and fentanyl did not significantly interfere with the MER signals from the STN and with the clinical outcome after STN DBS surgery. The results of this study suggest that propofol and fentanyl can be used for STN DBS in patients with advanced PD improving the overall experience of the patients.
Footnotes
Funding: This work was supported by a grant from the Korea Institute of Planning & Evaluation for Technology in Food, Agriculture, Forestry, and Fisheries, Republic of Korea (No. 311011-05-3-SB020) and a grant from the Korea Healthcare Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (No. HI09C13540100, HI10C14110400 and HI12C02050101).
The authors declare no conflicts of interest to disclose.
References
- 1.Deep-Brain Stimulation for Parkinson's Disease Study Group. Deep-brain stimulation of the subthalamic nucleus or the pars interna of the globus pallidus in Parkinson's disease. N Engl J Med. 2001;345:956–963. doi: 10.1056/NEJMoa000827. [DOI] [PubMed] [Google Scholar]
- 2.Benabid AL. Deep brain stimulation for Parkinson's disease. Curr Opin Neurobiol. 2003;13:696–706. doi: 10.1016/j.conb.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 3.Hutchison WD, Allan RJ, Opitz H, Levy R, Dostrovsky JO, Lang AE, Lozano AM. Neurophysiological identification of the subthalamic nucleus in surgery for Parkinson's disease. Ann Neurol. 1998;44:622–628. doi: 10.1002/ana.410440407. [DOI] [PubMed] [Google Scholar]
- 4.Hertel F, Züchner M, Weimar I, Gemmar P, Noll B, Bettag M, Decker C. Implantation of electrodes for deep brain stimulation of the subthalamic nucleus in advanced Parkinson's disease with the aid of intraoperative microrecording under general anesthesia. Neurosurgery. 2006;59:E1138. doi: 10.1227/01.NEU.0000245603.77075.55. [DOI] [PubMed] [Google Scholar]
- 5.Lefaucheur JP, Gurruchaga JM, Pollin B, von Raison F, Mohsen N, Shin M, Ménard-Lefaucheur I, Oshino S, Kishima H, Fénelon G, et al. Outcome of bilateral subthalamic nucleus stimulation in the treatment of Parkinson's disease: correlation with intra-operative multi-unit recordings but not with the type of anaesthesia. Eur Neurol. 2008;60:186–199. doi: 10.1159/000148246. [DOI] [PubMed] [Google Scholar]
- 6.Maltête D, Navarro S, Welter ML, Roche S, Bonnet AM, Houeto JL, Mesnage V, Pidoux B, Dormont D, Cornu P, et al. Subthalamic stimulation in Parkinson disease: with or without anesthesia? Arch Neurol. 2004;61:390–392. doi: 10.1001/archneur.61.3.390. [DOI] [PubMed] [Google Scholar]
- 7.Paek SH, Kim HJ, Yoon JY, Heo JH, Kim C, Kim MR, Lim YH, Kim KR, Kim JW, Han JH, et al. Fusion image-based programming after subthalamic nucleus deep brain stimulation. World Neurosurg. 2011;75:517–524. doi: 10.1016/j.wneu.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 8.Schaltenbrand G, Wharen W. Atlas of stereotaxy of the human brain. New York: Thieme; 1998. [Google Scholar]
- 9.Harries AM, Kausar J, Roberts SA, Mocroft AP, Hodson JA, Pall HS, Mitchell RD. Deep brain stimulation of the subthalamic nucleus for advanced Parkinson disease using general anesthesia: long-term results. J Neurosurg. 2012;116:107–113. doi: 10.3171/2011.7.JNS11319. [DOI] [PubMed] [Google Scholar]
- 10.Benabid AL, Pollak P, Louveau A, Henry S, de Rougemont J. Combined (thalamotomy and stimulation) stereotactic surgery of the VIM thalamic nucleus for bilateral Parkinson disease. Appl Neurophysiol. 1987;50:344–346. doi: 10.1159/000100803. [DOI] [PubMed] [Google Scholar]
- 11.Khan MF, Mewes K, Gross RE, Skrinjar O. Assessment of brain shift related to deep brain stimulation surgery. Stereotact Funct Neurosurg. 2008;86:44–53. doi: 10.1159/000108588. [DOI] [PubMed] [Google Scholar]
- 12.Martinez-Santiesteban FM, Swanson SD, Noll DC, Anderson DJ. Magnetic field perturbation of neural recording and stimulating microelectrodes. Phys Med Biol. 2007;52:2073–2088. doi: 10.1088/0031-9155/52/8/003. [DOI] [PubMed] [Google Scholar]
- 13.Miyagi Y, Shima F, Sasaki T. Brain shift: an error factor during implantation of deep brain stimulation electrodes. J Neurosurg. 2007;107:989–997. doi: 10.3171/JNS-07/11/0989. [DOI] [PubMed] [Google Scholar]
- 14.Benarroch EE. Subthalamic nucleus and its connections: anatomic substrate for the network effects of deep brain stimulation. Neurology. 2008;70:1991–1995. doi: 10.1212/01.wnl.0000313022.39329.65. [DOI] [PubMed] [Google Scholar]
- 15.Deiner S, Hagen J. Parkinson's disease and deep brain stimulator placement. Anesthesiol Clin. 2009;27:391–415. doi: 10.1016/j.anclin.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Duque P, Mateo O, Ruiz F, de Viloria JG, Contreras A, Grandas F. Intraoperative microrecording under general anaesthesia with bispectral analysis monitoring in a case of deep brain stimulation surgery for Parkinson's disease. Eur J Neurol. 2008;15:e76–e77. doi: 10.1111/j.1468-1331.2008.02166.x. [DOI] [PubMed] [Google Scholar]
- 17.Lin SH, Chen TY, Lin SZ, Shyr MH, Chou YC, Hsieh WA, Tsai ST, Chen SY. Subthalamic deep brain stimulation after anesthetic inhalation in Parkinson disease: a preliminary study. J Neurosurg. 2008;109:238–244. doi: 10.3171/JNS/2008/109/8/0238. [DOI] [PubMed] [Google Scholar]
- 18.Yamada K, Goto S, Kuratsu J, Matsuzaki K, Tamura T, Nagahiro S, Murase N, Shimazu H, Kaji R. Stereotactic surgery for subthalamic nucleus stimulation under general anesthesia: a retrospective evaluation of Japanese patients with Parkinson's disease. Parkinsonism Relat Disord. 2007;13:101–107. doi: 10.1016/j.parkreldis.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 19.Benazzouz A, Breit S, Koudsie A, Pollak P, Krack P, Benabid AL. Intraoperative microrecordings of the subthalamic nucleus in Parkinson's disease. Mov Disord. 2002;17:S145–S149. doi: 10.1002/mds.10156. [DOI] [PubMed] [Google Scholar]
- 20.Maciver MB, Bronte-Stewart HM, Henderson JM, Jaffe RA, Brock-Utne JG. Human subthalamic neuron spiking exhibits subtle responses to sedatives. Anesthesiology. 2011;115:254–264. doi: 10.1097/ALN.0b013e3182217126. [DOI] [PubMed] [Google Scholar]
- 21.Magnin M, Morel A, Jeanmonod D. Single-unit analysis of the pallidum, thalamus and subthalamic nucleus in parkinsonian patients. Neuroscience. 2000;96:549–564. doi: 10.1016/s0306-4522(99)00583-7. [DOI] [PubMed] [Google Scholar]
- 22.Rodriguez-Oroz MC, Rodriguez M, Guridi J, Mewes K, Chockkman V, Vitek J, DeLong MR, Obeso JA. The subthalamic nucleus in Parkinson's disease: somatotopic organization and physiological characteristics. Brain. 2001;124:1777–1790. doi: 10.1093/brain/124.9.1777. [DOI] [PubMed] [Google Scholar]
- 23.Schrock LE, Ostrem JL, Turner RS, Shimamoto SA, Starr PA. The subthalamic nucleus in primary dystonia: single-unit discharge characteristics. J Neurophysiol. 2009;102:3740–3752. doi: 10.1152/jn.00544.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steigerwald F, Pötter M, Herzog J, Pinsker M, Kopper F, Mehdorn H, Deuschl G, Volkmann J. Neuronal activity of the human subthalamic nucleus in the parkinsonian and nonparkinsonian state. J Neurophysiol. 2008;100:2515–2524. doi: 10.1152/jn.90574.2008. [DOI] [PubMed] [Google Scholar]
- 25.Weinberger M, Mahant N, Hutchison WD, Lozano AM, Moro E, Hodaie M, Lang AE, Dostrovsky JO. Beta oscillatory activity in the subthalamic nucleus and its relation to dopaminergic response in Parkinson's disease. J Neurophysiol. 2006;96:3248–3256. doi: 10.1152/jn.00697.2006. [DOI] [PubMed] [Google Scholar]
- 26.Hutchison WD, Lang AE, Dostrovsky JO, Lozano AM. Pallidal neuronal activity: implications for models of dystonia. Ann Neurol. 2003;53:480–488. doi: 10.1002/ana.10474. [DOI] [PubMed] [Google Scholar]
- 27.Anderson BJ, Marks PV, Futter ME. Propofol: contrasting effects in movement disorders. Br J Neurosurg. 1994;8:387–388. doi: 10.3109/02688699409029633. [DOI] [PubMed] [Google Scholar]
- 28.Böhmdorfer W, Schwarzinger P, Binder S, Sporn P. Temporary suppression of tremor by remifentanil in a patient with Parkinson's disease during cataract extraction under local anesthesia. Anaesthesist. 2003;52:795–797. doi: 10.1007/s00101-003-0522-y. [DOI] [PubMed] [Google Scholar]
- 29.Velly LJ, Rey MF, Bruder NJ, Gouvitsos FA, Witjas T, Regis JM, Peragut JC, Gouin FM. Differential dynamic of action on cortical and subcortical structures of anesthetic agents during induction of anesthesia. Anesthesiology. 2007;107:202–212. doi: 10.1097/01.anes.0000270734.99298.b4. [DOI] [PubMed] [Google Scholar]
- 30.Venkatraghavan L, Luciano M, Manninen P. Review article: anesthetic management of patients undergoing deep brain stimulator insertion. Anesth Analg. 2010;110:1138–1145. doi: 10.1213/ANE.0b013e3181d2a782. [DOI] [PubMed] [Google Scholar]