Abstract
Background: Over the past decades, our knowledge and understanding of adhesions and adhesion-related complications has increasingly grown and it has become evident that adhesions have significant implications for patients, physicians and the healthcare system. The question arises whether this has resulted in greater awareness of adhesion-related problems among practicing physicians and appropriate patient education on this topic in daily practice. The following article provides a brief overview of the important subject of adhesions, discusses current awareness of adhesions among patients and doctors and addresses the consequences of failure to provide patient education and consent from a medical perspective. Methods: Selective literature searches were conducted in PubMed and the Cochrane Library. A patient information and consent form was developed based on several yearsʼ experience and expertise in the field of adhesions. Results: Adhesions are the most common type of complication in abdominopelvic surgery today, with devastating consequences for some patients. Surveys investigating the awareness of adhesions among physicians and patients clearly showed that even well-informed physicians fail to educate their patients adequately. Such failure could potentially lead to successful medical malpractice lawsuits against doctors. Conclusion: Considering their clear clinical impact, adhesions and related consequences should always be discussed with patients preoperatively. A newly developed consent form that specifically addresses adhesion formation may serve to thoroughly educate patients preoperatively and to adequately document the process of doing so.
Key words: adhesions, adhesion prophylaxis, awareness, patient education, lawsuit
Abstract
Zusammenfassung
Hintergrund: In den letzten Jahrzehnten hat das Wissen über Adhäsionen und adhäsionsbedingte Komplikationen stetig zugenommen, wobei gezeigt werden konnte, dass Adhäsionen beträchtliche Folgen für Patienten, Ärzte und das Gesundheitssystem haben. Aufgrund dieser Erkenntnisse stellt sich ärztlicherseits die Frage, ob die Forschungsergebnisse zu einer verstärkten Wahrnehmung von Adhäsionen bei praktisch tätigen Ärzten geführt haben, und es in der Folge auch zu einer verstärkten Aufklärung der Patienten über adhäsionsbedingte Komplikationen gekommen ist. Der vorliegende Artikel gibt einen kurzen Überblick über das wichtige Thema der Adhäsionen und beschäftigt sich mit der Wahrnehmung von Adhäsionen durch Ärzte und Patienten sowie mit den möglichen rechtlichen Konsequenzen einer nicht erfolgten Aufklärung aus ärztlicher Sicht. Methodik: Für die Erstellung des Artikels wurde eine selektive Literaturrecherche in PubMed und der Cochrane Library durchgeführt. Ferner wurde ein Aufklärungsbogen auf der Grundlage langjähriger Erfahrung und Expertise auf dem Gebiet der Adhäsionen entwickelt. Ergebnisse: Adhäsionen sind heutzutage die häufigste Komplikation abdominopelviner Operationen mit z. T. schwerwiegenden Auswirkungen für die betroffenen Patienten. Befragungen bez. der Wahrnehmung von Adhäsionen durch Ärzte und Patienten ergaben, dass selbst gut informierte Ärzte ihre Patienten nicht über adhäsionsbedingte Komplikationen aufklären, obgleich dies rechtliche Konsequenzen haben könnte. Schlussfolgerung: Aufgrund der großen klinischen Bedeutung von Adhäsionen sollten Patienten routinemäßig über Adhäsionen und die potenziell damit verbundenen Komplikationen aufgeklärt werden. Ein neu erstellter Aufklärungsbogen über Adhäsionen kann helfen, Patienten nachweislich und gründlich aufzuklären.
Schlüsselwörter: Adhäsionen, Adhäsionsprophylaxe, Wahrnehmung, Aufklärung, rechtliche Konsequenzen
Background
Adhesions following surgery have long been known, and the first scientific paper on the subject was written more than 100 years ago 1. However, an understanding of the fundamental pathomechanisms involved has only been achieved over the last decades. Numerous studies have been performed on the consequences of adhesions for patients as well as on the associated implications for the health system 2, 3, 4. The results of these studies are clear and pose the question of whether the scientific work of the last few decades has influenced awareness of adhesions in daily practice. In particular, surgeons who perform abdominopelvic operations should have a specific interest in the subject since patients should be educated as a matter of course on high-incidence complications. The occurrence of adhesions varies from study to study and lies generally between 20 and 93 percent 5, 6, 7, 8, 9, 10. Adhesions can currently be considered the most commonly recorded complication following abdominopelvic surgery.
The present article provides a short overview and pays particular attention to the level of awareness of adhesions among physicians and patients. The potential legal consequences of patient education and consent are discussed, and a patient information form developed by the authors is proposed.
Formation of Adhesions
Adhesions are bands of connective tissue which join two normally separate anatomical structures. As a reaction to a peritoneal trauma, for instance due to inflammation (inflammatory processes) or surgery, increased vessel permeability occurs during normal healing, resulting in a migration of inflammatory cells and accumulation of fibrin. Among others, fibroblasts also migrate into the fibrin matrix where they produce extracellular matrix components, thereby modifying the fibrin matrix. The accumulated fibrin can normally be broken down by the fibrinolytic system. However, if the fibrin is not degraded due to reduced fibrinolysis, the fibrin matrix becomes the basis for adhesion formation 11, 12. In a further process, the initially reversible connective tissue bands can undergo stable reconstruction and become vascularised and innervated 13, 14. The formation of adhesions is a complex process involving changes in the fibrinolytic system itself and the various cytokines which influence the fibrinolytic system 15, 16. Hypoxia is an important factor. Studies on fibroblasts have shown that collagen synthesis is stimulated under hypoxia conditions, and factors in the fibrinolytic system are influenced in terms of antifibrinolytic activity 17, 18. Other influencing factors are the cytokines released during an inflammatory reaction. Increased concentrations of proinflammatory cytokines are found in the peritoneal fluid of patients with adhesions 19, 20. These cytokines are capable of stimulating the fibrinolytic system factors, thereby causing an antifibrinolytic effect 21, 22. In abdominopelvic surgery, an inflammatory reaction as well as hypoxia can be more marked as a result of an extensive surgical trauma, peritoneal sutures or the use of electrocoagulation. Moreover, laparoscopic interventions can result in damage to the peritoneum through a negative effect of the pneumoperitoneum on the peritoneal cells or dehydration of the cells when using dry insufflation gas. The formation of adhesions is thus stimulated 23, 24, 25, 26.
Complications Resulting From Adhesions
Adhesions form within 3–5 days; however, complications associated with the adhesions often become clinically relevant and indicate symptoms only some time after the initial operation. One of the most significant complications is mechanical ileus, with adhesions representing the most common aetiology. A recent review of 29 studies investigating the causes of acute ileus indicated that adhesions accounted for 85 % of acute small bowel obstructions. In general, acute ileus is responsible for 5 % of hospital admissions, and 50 % of these cases are treated surgically 27. Furthermore, adhesions can have a negative impact on fertility. However, only a few studies, some of which are older, have been conducted on the influence of adhesions on fertility 28, 29, 30. Two small, prospective studies have indicated that the use of an adhesion barrier resulted in a higher pregnancy rate in comparison with the control group 31, 32. Other complications caused by adhesions include the development of chronic pelvic pain 33 as well as difficult and prolonged subsequent surgeries with the risk of inadvertent damage to the intestine, blood vessels or urethra 3, 34. The considerable costs of treating complications caused by adhesions constitute a burden on the health system 4, 35. Considering the significant consequences of adhesions, it is essential that surgeons performing abdominopelvic operations establish a strategy for preventing adhesions. Patients should be informed as a matter of course on the risks associated with adhesions and ways of minimising these risks.
Prevention of Adhesions
In addition to meticulous surgical techniques and careful handling of connective tissues, strategies for minimising the risk of adhesion formation include reduced suturing and minimised tissue trauma by limited use of electrocoagulation. Coagulation time and frequency should be reduced, and aerosolised tissue arising from electrocoagulation should be aspirated. Foreign bodies, such as materials with loose fibres, should be avoided. The use of wet instead of dry cloths or sponges and the use of starch-free and latex-free gloves during laparotomy are recommended measures. A reduction of pressure and duration of the pneumoperitoneum during laparoscopy can limit the occurrence of adhesions. The peritoneum should be thoroughly rinsed during laparoscopy as well as laparotomy in order to reduce dehydration of the peritoneal cells 36.
Currently there is no certain way of predicting which operations and which patients will present with symptomatic adhesions. Adhesion prophylaxis should be considered in the form of anti-adhesion devices following abdominopelvic surgery. Currently no systemic pharmaceutical products are available for reducing adhesions. All available products are designed to mechanically separate the injured tissue from the surrounding organs during the healing process. There is no doubt that these products can in principle reduce adhesions following abdominopelvic surgery. However, current data do not clearly indicate the factor by which a reduction is possible because the reductions achieved vary depending on the device used and the study undertaken. A large, randomised, double-blind study (n = 402) comparing the use of an adhesion barrier with a purely Ringer lactate solution instillation indicated a significant difference in the reduction of new adhesions. In the treatment group (n = 203), 47 % of patients developed new adhesions compared with 57 % in the control group (n = 199). In this study, clinical success was defined as a reduction in the number of sites of adhesion occurrence of at least 3 or 30 % following adhesiolysis. In the treatment group, clinical success was recorded in 49 % of patients compared with 38 % in the control group. In the subgroup of infertile female patients, 55 % in the treatment group (n = 102) indicated clinical success compared with 33 % in the control group (n = 112) 37. A further large, prospective blind study (n = 546) investigated the efficacy of the adhesion barrier following myomectomy. The incidence of adhesions was assessed in a second-look laparoscopy and indicated the following: abdominal myomectomy without adhesion barrier (28.1 %; n = 154), laparoscopic myomectomy without adhesion barrier (22.6 %; n = 155), abdominal myomectomy with adhesion barrier (22 %; n = 154) and laparoscopic myomectomy with adhesion barrier (15.9 %; n = 157) 6. Other studies have been the subject of meta-analyses 38, 39. Due to uncertainty of the efficacy of anti-adhesion agents, it is difficult for physicians to decide on which agent to use. Moreover, many adhesion barriers are still very expensive and are seldom reimbursed by health funds. A validated, scientific re-evaluation of the efficacy of anti-adhesion products, combined with a thorough patient education are urgently needed in order to establish the use of these products.
Physician Awareness
Questions are increasingly being asked about adhesion awareness on the part of the physicians and patients. One might expect that the results of experimental and clinical studies during the past decades would have increased awareness among physicians, and that patients are being better informed on adhesions. The following paragraphs provide an overview of three studies on physician awareness in relation to adhesions. Surgically active gynaecologists in Germany 40 and Great Britain 41 as well as general surgeons and gynaecologists in The Netherlands 42 were surveyed.
In Germany, a questionnaire was sent to all gynaecological clinics and was completed by the respective head physician or one of the specialists. The results of the study indicated a high level of awareness by German gynaecologists. The response rate was 34 % (279/833), suggesting that the questionnaires tended to be completed by physicians with a specific interest in the subject. The majority of surveyed gynaecologists (66 %) confirmed that patients with adhesions made up a significant proportion of their daily surgical activities. Although over 60 % of the respondents agreed that adhesions were accompanied by considerable morbidity in their patients, only 38 % used adhesion barriers in routine practice 40.
In Great Britain, the questionnaire was sent to all members of the Royal College of Obstetricians and Gynaecologists, with a response rate of 10 % (390/4010). About 94 % of the surveyed gynaecologists confirmed that adhesions gave rise to serious consequences and agreed that adhesion barriers should be used in operations with a high risk of adhesion formation. 65 % of the respondents were even of the opinion that adhesion barriers should be used in all operations. When asked about their current anti-adhesion strategy, however, less than 10 % indicated the use of adhesion barriers in their daily routine 41.
The response rate from the Netherlands was 34 % (501/1455) and showed a similar outcome: 67 % of those surveyed confirmed the clinical relevance of adhesions, but only 13 % had used an anti-adhesion agent during the year preceding the survey 42.
In summary, the majority of surgeons were relatively well informed with regard to the individual survey questions, but only a minority actually used adhesion barriers in routine practice. This result emphasises the difficulty in evaluating the benefits of anti-adhesion agents and operations performed according to anti-adhesion standards.
The studies also indicated that even the surveyed surgeons do not inform their patients sufficiently. Only 10 % of the surgeons in the Netherlands stated that they informed their patients about adhesions as a matter of routine, while 41 % stated that they had never mentioned adhesions to their patients. In Great Britain, only 23 % of gynaecologists informed their patients prior to all operations and 38 % prior to some operations. Only 2 % of the respondents offered their patients written information on the subject 40, 41, 42. In Germany, 83 % of the gynaecologists surveyed informed their patients on adhesions. However, a recent prospective study investigating the process of patient education in a German university clinic indicated that adhesions were discussed in only 44 % of consultations. If adhesions are not routinely discussed prior to all abdominopelvic operations, despite the fact that they are common and can have serious consequences, other sources are the only possibility to increase patient awareness of the issue. Ideally, however, the best source of information should be the consultation between doctor and patient.
Patient Awareness and Legal Consequences
A recent study of the awareness of adhesion by patients conducted in two hospitals in Great Britain and in one Germany university medical centre corroborated the hypothesis that patients are not being sufficiently educated on adhesions 43. In Germany, 44 % of doctors at the university medical centre discussed adhesions during their patient consultations, but only 39 % of these patients felt satisfactorily informed. In Great Britain, 27 % of patients were informed about adhesions during consultations. The authors assumed that the variance in percentages between Germany and Great Britain was due to the difference in type of consultation. Since no written consent form is used in Great Britain, the authors assumed that doctors often forgot to discuss adhesions. In Germany, on the contrary, written consent forms are used in which adhesions are listed together with other complications. By virtue of this fact, the information rates indicated in Germany are to be considered particularly low. Nevertheless, the study showed that patients who had been informed about adhesions indicated their doctor had been the main source of information. This further emphasises the importance of consultations 43.
An information form specifically aimed at discussing the problem of adhesions is a very useful aid for patient and doctor during a consultation. For the patient, a form written in clear and simple language can help prepare for the discussion with the doctor. For doctors, the routine use of a form can be a reminder to discuss the risk of adhesions with the patient and can provide professional information with which to correctly inform the patient. Professor De Wilde has worked in collaboration with the medical publisher Perimed Fachbuch Verlag to develop an information form focused on adhesions in abdominopelvic operations, see Fig. 1. An information form can and should never be a substitute for a personal consultation. Nevertheless, it offers patients important information and can serve as evidence for the physician at any time, especially in cases of legal disputes, that the patient was informed about adhesions and the associated complications.
Fig. 1.
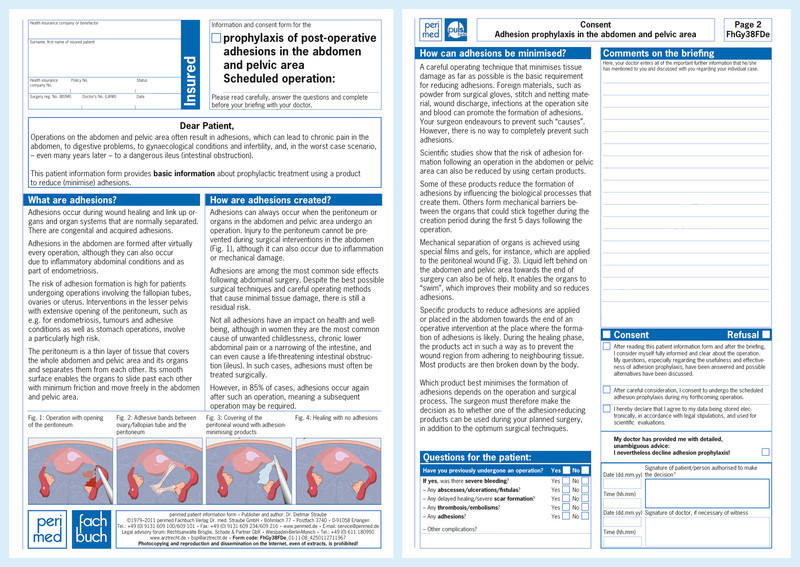
Perimed information form.
Guidelines can prompt physicians to discuss serious complications during each consultation, even when the probability of occurrence is low. Less serious complications must be discussed if their occurrence is common 44. Since a precedence setting case in Great Britain, physicians are deemed negligent if they do not inform patients of complications with a risk of over 1–2 % 45. Depending on the operation, the 5-year risk of a hospital admission due to complications caused by adhesions lies well over the 1–2 % risk factor 46. Nevertheless, a study conducted in Great Britain indicates that complications caused by adhesions are only noted on 9 % of information forms 47.
The number of successful lawsuits due to adhesion-related complications is increasing 48. It is in the interests of surgeons, therefore, to be prepared for potential claims and to be in a position to provide evidence that patients are routinely informed on possible complications from adhesions. This is particularly important since a reversal of evidence may be imposed by law in Germany by virtue of which the physician is obliged to provide proof of informing the patient 49.
Conclusion
Adhesions are of major clinical significance and should be considered to be the most frequent complication following abdominopelvic surgery. Although physicians consider the issue important, a considerable number of patients are not being routinely informed about adhesions and the potential associated complications. It is in the interests of patients and physicians to educate patients on the risks of adhesions and on the currently available preventive measures. Although the information form cannot and should not be a substitute for a personal consultation, it is a very useful communication aid between physician and patient and serves as documentary evidence of the consultation.
Five Key Statements
Today, adhesions are the most common complications following abdominopelvic operations.
Adhesions potentially have serious consequences for patients, such as acute small bowel obstruction, infertility, chronic pelvic pain and complications during follow-on operations.
A sound surgical technique and the use of laparoscopy cannot totally prevent the formation of adhesions; the use of adhesion barriers in abdominopelvic operations should be considered.
Currently, patients are not being sufficiently informed about adhesions and the potential resulting complications; this may lead to successful lawsuits against treating physicians.
Prior to any abdominal operation, patients should be routinely informed about adhesions by means of a written consent form.
Conflict of Interest Professor De Wilde is a scientific consultant for Nordic Pharma GmbH, perimed Fachbuch Verlag Dr. med. Straube GmbH, Baxter GmbH and Shire GmbH. Dr. Hackethal is a scientific consultant for Nordic Pharma, Fisher & Paykel Healthcare and Ethicon EndoSurgery.
Joint first authors and equal contributors.
Supporting Information
German supporting information for this article
References
- 1.Uhlmann C. Ueber das Auftreten peritonealer Adhäsionen nach Laparotomien, mit besonderer Berücksichtigung des Verhältnisses zwischen trockener und feuchter Asepsis. Arch Gynecol Obstet. 1897;54:384–411. [Google Scholar]
- 2.Ellis H, Moran B, Thompson J. et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1999;353:1476–1480. doi: 10.1016/S0140-6736(98)09337-4. [DOI] [PubMed] [Google Scholar]
- 3.van der Krabben A A, Dijkstra F R, Nieuwenhuijzen M. et al. Morbidity and mortality of inadvertent enterotomy during adhesiotomy. Br J Surg. 2000;87:467–471. doi: 10.1046/j.1365-2168.2000.01394.x. [DOI] [PubMed] [Google Scholar]
- 4.Wilson M S, Menzies D, Knight A D. et al. Demonstrating the clinical and cost effectiveness of adhesion reduction strategies. Colorect Dis. 2002;4:355–360. doi: 10.1046/j.1463-1318.2002.00374.x. [DOI] [PubMed] [Google Scholar]
- 5.Dubuisson J, Botchorishvili R, Perrette S. et al. Incidence of intraabdominal adhesions in a continuous series of 1000 laparoscopic procedures. Am J ObstetGynecol. 2010;203:1110. doi: 10.1016/j.ajog.2010.03.031. [DOI] [PubMed] [Google Scholar]
- 6.Tinelli A, Malvasi A, Guido M. et al. Adhesion formation after intracapsular myomectomy with or without adhesion barrier. Fertil Steril. 2011;95:1780–1785. doi: 10.1016/j.fertnstert.2010.12.049. [DOI] [PubMed] [Google Scholar]
- 7.Takeuchi H, Kitade M, Kikuchi I. et al. Influencing factors of adhesion development and the efficacy of adhesion-preventing agents in patients undergoing laparoscopic myomectomy as evaluated by a second-look laparoscopy. Fertil Steril. 2008;89:1247–1253. doi: 10.1016/j.fertnstert.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 8.Brill A I, Nezhat F, Nezhat C H. et al. The incidence of adhesions after prior laparotomy: a laparoscopic appraisal. Obstet Gynecol. 1995;85:269–272. doi: 10.1016/0029-7844(94)00352-E. [DOI] [PubMed] [Google Scholar]
- 9.Mercorio F, Mercorio A, Di Spiezio Sardo A. et al. Evaluation of ovarian adhesion formation after laparoscopic ovarian drilling by second-look minilaparoscopy. Fertil Steril. 2008;89:1229–1233. doi: 10.1016/j.fertnstert.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 10.Menzies D, Ellis H. Intestinal obstruction from adhesions–how big is the problem? Ann R Coll Surg Eng. 1990;72:60–63. [PMC free article] [PubMed] [Google Scholar]
- 11.di Zerega G S, Campeau J D. Peritoneal repair and post-surgical adhesion formation. Hum Reprod Update. 2001;7:547–555. doi: 10.1093/humupd/7.6.547. [DOI] [PubMed] [Google Scholar]
- 12.Imudia A N, Kumar S, Saed G M. et al. Pathogenesis of intra-abdominal and pelvic adhesion development. Semin Reprod Med. 2008;26:289–297. doi: 10.1055/s-0028-1082387. [DOI] [PubMed] [Google Scholar]
- 13.Herrick S E, Mutsaers S E, Ozua P. et al. Human peritoneal adhesions are highly cellular, innervated, and vascularized. J Pathol. 2000;192:67–72. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH678>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 14.Tulandi T, Fong Chen M, Al-Took S. et al. A study of nerve fibers and histopathology of postsurgical, postinfectious, and endometriosis-related adhesions. Obstet Gynecol. 1998;92:766–768. doi: 10.1016/s0029-7844(98)00298-1. [DOI] [PubMed] [Google Scholar]
- 15.Cheong Y C, Laird S M, Li T C. et al. Peritoneal healing and adhesion formation/reformation. Hum Reprod Update. 2001;7:556–566. doi: 10.1093/humupd/7.6.556. [DOI] [PubMed] [Google Scholar]
- 16.Hellebrekers B W, Kooistra T. Pathogenesis of postoperative adhesion formation. Br J Surg. 2011;98:1503–1516. doi: 10.1002/bjs.7657. [DOI] [PubMed] [Google Scholar]
- 17.Saed G M, Diamond M P. Hypoxia-induced irreversible up-regulation of type I collagen and transforming growth factor-β1 in human peritoneal fibroblasts. Fertil Steril. 2002;78:144–147. doi: 10.1016/s0015-0282(02)03146-1. [DOI] [PubMed] [Google Scholar]
- 18.Saed G M, Diamond M P. Modulation of the expression of tissue plasminogen activator and its inhibitor by hypoxia in human peritoneal and adhesion fibroblasts. Fertil Steril. 2003;79:164–168. doi: 10.1016/s0015-0282(02)04557-0. [DOI] [PubMed] [Google Scholar]
- 19.Cheong Y C, Shelton J B, Laird S M. et al. IL-1, IL-6 and TNF-αconcentrations in the peritoneal fluid of women with pelvic adhesions. Hum Reprod Update. 2002;17:69–75. doi: 10.1093/humrep/17.1.69. [DOI] [PubMed] [Google Scholar]
- 20.Cheong Y C, Laird S M, Shelton J B. et al. The correlation of adhesions and peritoneal fluid cytokine concentrations: a pilot study. Hum Reprod Update. 2002;17:1039–1045. doi: 10.1093/humrep/17.4.1039. [DOI] [PubMed] [Google Scholar]
- 21.Sitter T, Toet K, Fricke H. et al. Modulation of procoagulant and fibrinolytic system components of mesothelial cells by inflammatory mediators. Am J Physiol. 1996;271(5 Pt 2):R1256–R1263. doi: 10.1152/ajpregu.1996.271.5.R1256. [DOI] [PubMed] [Google Scholar]
- 22.Tietze L, Elbrecht A, Schauerte C. et al. Modulation of pro- and antifibrinolytic properties of human peritoneal mesothelial cells by transforming growth factor beta1 (TGF-beta1), tumor necrosis factor alpha (TNF-alpha) and interleukin 1beta (IL-1beta) Thromb Haemost. 1998;79:362–370. [PubMed] [Google Scholar]
- 23.Molinas C R, Mynbaev O, Pauwels A. et al. Peritoneal mesothelial hypoxia during pneumoperitoneum is a cofactor in adhesion formation in a laparoscopic mouse model. Fertil Steril. 2001;76:560–567. doi: 10.1016/s0015-0282(01)01964-1. [DOI] [PubMed] [Google Scholar]
- 24.Molinas C R, Elkelani O, Campo R. et al. Role of the plasminogen system in basal adhesion formation and carbon dioxide pneumoperitoneum-enhanced adhesion formation after laparoscopic surgery in transgenic mice. Fertil Steril. 2003;80:184–192. doi: 10.1016/s0015-0282(03)00496-5. [DOI] [PubMed] [Google Scholar]
- 25.Binda M M, Molinas C R, Hansen P. et al. Effect of desiccation and temperature during laparoscopy on adhesion formation in mice. Fertil Steril. 2006;86:166–175. doi: 10.1016/j.fertnstert.2005.11.079. [DOI] [PubMed] [Google Scholar]
- 26.Brokelman W J, Holmdahl L, Janssen I M. et al. Decreased peritoneal tissue plasminogen activator during prolonged laparoscopic surgery. J Surg Res. 2009;151:89–93. doi: 10.1016/j.jss.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 27.OʼConnor D B, Winter D C. The role of laparoscopy in the management of acute small-bowel obstruction: a review of over 2,000 cases. Surg Endosc. 2012;26:12–17. doi: 10.1007/s00464-011-1885-9. [DOI] [PubMed] [Google Scholar]
- 28.Caspi E, Halperin Y. Surgical management of periadnexal adhesions. Int J Fertil. 1981;26:49–52. [PubMed] [Google Scholar]
- 29.Tulandi T, Collins J A, Burrows E. et al. Treatment-dependent and treatment-independent pregnancy among women with periadnexal adhesions. Am J Obstet Gynecol. 1990;162:354–357. doi: 10.1016/0002-9378(90)90384-j. [DOI] [PubMed] [Google Scholar]
- 30.Strandell A, Bryman I, Janson P O. et al. Background factors and scoring systems in relation to pregnancy outcome after fertility surgery. Acta Obstet Gynecol Scand. 1995;74:281–287. doi: 10.3109/00016349509024450. [DOI] [PubMed] [Google Scholar]
- 31.Sawada T, Nishizawa H, Nishio E. et al. Postoperative adhesion prevention with an oxidized regenerated cellulose adhesion barrier in infertile women. J Reprod Med. 2000;45:387–389. [PubMed] [Google Scholar]
- 32.Pellicano M, Guida M, Bramante S. et al. Reproductive outcome after autocrosslinked hyaluronic acid gel application in infertile patients who underwent laparoscopic myomectomy. Fertil Steril. 2005;83:498–500. doi: 10.1016/j.fertnstert.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 33.Hammoud A, Gago L A, Diamond M P. Adhesions in patients with chronic pelvic pain: a role for adhesiolysis? Fertil Steril. 2004;82:1483–1491. doi: 10.1016/j.fertnstert.2004.07.948. [DOI] [PubMed] [Google Scholar]
- 34.Kumakiri J, Kikuchi I, Kitade M. et al. Incidence of complications during gynecologic laparoscopic surgery in patients after previous laparotomy. J Minim Invasive Gynecol. 2012;17(4):480–486. doi: 10.1016/j.jmig.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 35.Tingstedt B, Isaksson J, Andersson R. Long-term follow-up and cost analysis following surgery for small bowel obstruction caused by intra-abdominal adhesions. Br J Surg. 2007;94:743–748. doi: 10.1002/bjs.5634. [DOI] [PubMed] [Google Scholar]
- 36.De Wilde R L, Trew G. Postoperative abdominal adhesions and their prevention in gynaecological surgery. Expert consensus position. Part 2 – steps to reduce adhesions. Gynecol Surg. 2007;4:243–253. [Google Scholar]
- 37.Brown C B, Luciano A A, Martin D. et al. Adept (icodextrin 4 % solution) reduces adhesions after laparoscopic surgery for adhesiolysis: a double-blind, randomized, controlled study. Fertil Steril. 2007;88:1413–1426. doi: 10.1016/j.fertnstert.2006.12.084. [DOI] [PubMed] [Google Scholar]
- 38.Metwally M E Watson A Lilford R et al. Fluid and pharmacological agents for adhesion prevention after gynaecological surgery Cochrane Database Syst Rev 20062CD001298 [DOI] [PubMed] [Google Scholar]
- 39.Ahmad G Duffi J M Farquhar C et al. Barrier agents for adhesion prevention after gynaecological surgery Cochrane Database Syst Rev 20082CD000475 [DOI] [PubMed] [Google Scholar]
- 40.Hackethal A, Sick C, Brueggmann D. et al. Awareness and perception of intra-abdominal adhesions and related consequences: survey of gynaecologists in German hospitals. Eur J Obstet Gynecol Reprod Biol. 2010;150:180–189. doi: 10.1016/j.ejogrb.2010.02.017. [DOI] [PubMed] [Google Scholar]
- 41.Trew G, Cooke I, Lower A. et al. Post-operative abdominal adhesions – awareness of UK gynaecologists – a survey of members of the Royal College of Obstetricians and Gynaecologists. Gynecol Surg. 2009;6:25–37. [Google Scholar]
- 42.Schreinemacher M H, ten Broek R P, Bakkum E A. et al. Adhesion awareness: a national survey of surgeons. World J Surg. 2010;34:2805–2812. doi: 10.1007/s00268-010-0778-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kraemer B, Birch J C, Birch J V. et al. Patientsʼ awareness of postoperative adhesions: results from a multi-centre study and online survey. Arch Gynecol Obstet. 2011;283:1069–1073. doi: 10.1007/s00404-010-1504-3. [DOI] [PubMed] [Google Scholar]
- 44.General Medical Council Consent: patients and doctors making decisions together http://www.gmc-uk.org/static/documents/content/Consent_0510.pdflast access: 9.2.2012
- 45.NHS Litigation Authority Informed ConsentNHSLA Risk Alert2004. Issue 4.http://www.nhsla.com/NR/rdonlyres/AD7A7848-E9A3-4668-839F-43E54BBFA3A1/0/RiskManagementAlert4.pdflast access: 9.2.2012
- 46.Stanciu D, Menzies D. The magnitude of adhesion-related problems. Colorect Dis. 2007;9 02:35–38. doi: 10.1111/j.1463-1318.2007.01346.x. [DOI] [PubMed] [Google Scholar]
- 47.Rajab T K, Wallwiener M, Talukdar S. et al. Adhesion-related complications are common, but rarely discussed in preoperative consent: a multicenter study. World J Surg. 2009;33:748–750. doi: 10.1007/s00268-008-9917-x. [DOI] [PubMed] [Google Scholar]
- 48.Ellis H, Crowe A. Medico-legal consequences of post-operative intra-abdominal adhesions. Int J Surg. 2009;7:187–191. doi: 10.1016/j.ijsu.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 49.Informationsdienst Medizinrecht Beweislast und Beweislastumkehr http://aerztehaftung.de/Beweislast-und-Beweislastumkehr-im-Arzthaftungsprozess.htmllast access: 9.2.2012
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
German supporting information for this article


