Abstract
Caesarean section is one of the most common operations worldwide and more than 30 % of procedures in perinatal centres in Germany are caesarean sections. In the last few years the technique used for caesarean sections has been simplified, resulting in a lower postoperative morbidity. But persistent problems associated with all caesarean section techniques include high intraoperative loss of blood, the risk of injury to the child during uterotomy and postoperative wound dehiscence of the uterine scar. We present here a modification of the most common Misgav-Ladach method. The initial skin incision is done along the natural skin folds and is extended intraoperatively depending on the circumference of the babyʼs head. After blunt expansion of the uterine incision using an anatomical forceps, the distal uterine wall is pushed behind the babyʼs head. The babyʼs head is rotated into the occipito-anterior or posterior position and delivery occurs through the application of gentle pressure on the uterine fundus. Closure of the uterotomy is done using 2 continuous sutures, which are then knotted together resulting in a short double-layer closure. The two ends of the skin suture are left open to allow for natural drainage. Our experience at the University Gynaecological Hospitals in Novi Sad and Magdeburg has shown that this modification is associated with shorter operating times, minimal blood loss and shorter in-hospital stay of patients as well as high rates of patient satisfaction.
Key words: Caesarean section, section modification, Vejnović method
Abstract
Zusammenfassung
Die Sectio caesarea ist weltweit eine der am häufigsten durchgeführten Operationen, und ihr Anteil in Perinatalzentren in Deutschland beträgt über 30 %. In den letzten Jahren wurde die Technik der Sectio caesarea vereinfacht, was zu einer niedrigeren postoperativen Morbidität führte. Weiterhin bestehende Probleme aller Sectio-Techniken sind hohe intraoperative Blutverluste, die Gefahr der Verletzung des Kindes bei der Uterotomie und die spätere Nahtdehiszenz im Bereich der Uterotomienarbe. Wir stellen eine Modifikation der am häufigsten durchgeführten Methode nach Misgav-Ladach vor. Die Hautinzision wird in den Hautlinien durchgeführt und intraoperativ entsprechend der kindlichen Kopfgröße erweitert. Nach stumpfer Uterotomie wird der distale Uterotomierand über den führenden Teil des Neugeborenen geschoben und dieser durch leichten Druck geboren. Der Verschluss der Uterotomie erfolgt durch 2 fortlaufende Nähte, derer Verknotung zu einem kurzen, doppelschichtigen Verschluss führt. Bei der Hautnaht werden die beiden Enden offen, im Sinne einer natürlichen Drainage belassen. Die Erfahrungen an den Universitäts-Frauenkliniken Novi Sad und Magdeburg zeigen eine deutliche Verkürzung der Operationszeit mit geringem Blutverlust und verkürztem stationären Aufenthalt, kombiniert mit einer hohen Zufriedenheit der Patientinnen.
Schlüsselwörter: Sectio caesarea, Sectio-Modifikation, Vejnović-Methode
Introduction
Caesarean section is one of the most commonly performed operations for women all over the world. Until the middle of the last century caesarean section rates in Europe rarely exceeded 3–5 % 1. Currently around every 3rd baby (31.3 % on average) born in German hospitals is delivered by caesarean section 2, 3, 4.
The increase in the numbers of caesarean sections performed has been ascribed to the increased range of indications, increased numbers of preterm deliveries and increased legal disputes. The most important indications for caesarean section include breech presentation, protracted birth including failure to progress in labour, incipient intrauterine hypoxia and previous C-section 5, 6, 7, 8. In the past few years it appears that the rate of elective C-sections has also risen, but no reliable figures are available on this point. It is also assumed that improvements in C-section techniques resulting in decreased maternal and foetal morbidity and mortality have also contributed to a more general use of this method of delivery 9, 10. Over the past few decades the “classic” Pfannenstiel technique has been replaced, first by the Joel-Cohen method and then by the “gentle” Misgav-Ladach technique 11, 12, 13. The changes in operative techniques have resulted in shorter operating times, less loss of blood, reduced tissue trauma and a greater patient satisfaction 14, 15, 16.
Other modifications to the C-section method were developed at the beginning of 2000 at the University of Novi Sad (Serbia) and have been retrospectively compared with the classic C-section technique 17. A Doerfler C-section was done in 600 patients 18 and 5648 patients were operated using the newly modified method. A comparison with the classic caesarean section method showed that the modified technique reduced blood loss (342 vs. 495 ml) and postoperative pain and shortened the time required for surgery (average time: 12 vs. 40 min). The in-hospital stay was also significantly shorter (3.3 vs. 6.7 days) 17. Overall, intraoperative and postoperative morbidity were significantly reduced with the modified technique.
We describe this technique in detail below and present the first data of a prospective comparative study comparing the “classic” C-section method and the modified technique.
Patients and Methods
Study design
The prospective study was carried out between 1 May 2008 and 1 March 2009 in the Department for Gynaecology and Obstetrics of the Clinical Centre Vojvodina in Novi Sad, Serbia. Inclusion criteria were primiparity and planned elective C-section together with informed consent signed by the patient. Patients were randomised into one of two groups by computer randomisation. A total of 122 patients were investigated in the study; the new C-section method was used in 72 patients (59.1 %) (Group A) while the classic Doerfler C-section method was used in 50 patients (40.9 %) (Group B). Exclusion criteria were emergency C-section for various reasons, refusal of patient consent to take part in the study and incomplete follow-up data.
The surgeon was only informed a short time prior to the operation which technique would be used. On the day of discharge patients were informed which arm of the study they had been randomised to. Operations were performed under local or spinal anaesthesia. The time required for surgery, duration of inpatient stay and blood loss were recorded for comparison. The operating time was measured from starting the skin incision at the start of the operation to completion of skin suturing at the end of the operation. Blood loss was measured using a suction device which suctioned only blood and not amniotic fluid. Blood loss was also measured indirectly through the determination of preoperative and postoperative Hb levels. A total of 10 surgeons were involved in the study, half of them operated the women using the classic method and the other half used the modified technique. All surgeons had performed at least 30 C-sections using their chosen method prior to taking part in the study. The number of patients of each group operated on by each surgeon was relatively balanced and evenly distributed. Each surgeon operated on at least 10 patients.
Postoperative clinical follow-up was done at regular intervals; laboratory tests were done as needed. Postoperatively, scar length, local reddening, swelling, seroma or haematoma formation and pain in the area around the scar were evaluated. Patient satisfaction was also investigated.
Comparison of Classic Caesarean Section with New Operative Technique
Description of the classic operative technique
The skin incision in the classic C-section technique is done as a horizontal Pfannenstiel incision 2 cm above the pubic symphysis; subcutaneous adipose tissue and the abdominal fascia are also sharply dissected using a scalpel and the aponeurosis of the transverse abdominal muscles is detached from the straight abdominal muscles. The rectus abdominis muscles are then pushed apart. This is followed by cranio-caudal incision of the peritoneum. The peritoneum is severed from the front uterine wall and pushed away caudally. In the classic C-section method the uterine wall is completely dissected using a scalpel, and the incision is then extended manually in a slight horizontal curve. The child is delivered manually after opening the amniotic sac. After determining the neonatal pH-value, the placenta is removed by hand. Curettage of the uterus is done if there is any suspicion that remnants of the placenta have been retained. Depending on the extent of cervical dilation, manual cervical dilatation or dilatation using Hegar pins is done to a width of around 3 cm. The uterus is closed using continuous or interrupted sutures. The peritoneum and the musculature are sutured with continuous or interrupted sutures. The fascia is closed as usual with a continuous suture. Finally the skin incision is closed with intracutaneous continuous sutures.
Description of the new operative technique
Opening the abdomen (abdominotomy)
The site for the skin incision is selected by gently pressing the abdominal wall caudally. The incision is then done along the skin fold created by this gentle pressure (Fig. 1 a) at approximately 5 cm above the pubic symphysis. The initial length of the incision is approx. 6–7 cm. Later during the operation the incision is adapted to the circumference of the babyʼs head (fronto-occipital diameter) or the breech presentation. This can be achieved without difficulty if the skin is incised precisely along the skin fold. The abdominal fascia are then sharply severed with a scalpel above the pyramidalis muscles (Fig. 1 b). The abdomen is opened at the linea alba through traction on and dissection of the fascia and access is subsequently enlarged through vertical and transversal traction and blunt dissection.
Fig. 1 a.
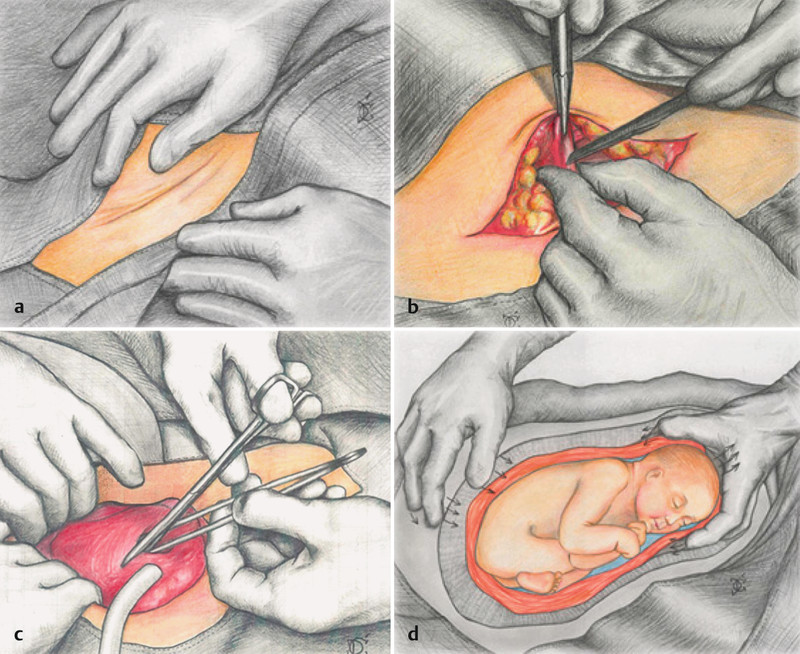
to d Skin incision, uterotomy and delivery of the baby. a The skin incision is done along the skin folds and b the fascia are dissected above pyramidalis muscles. c The uterotomy is done using blunt forceps and scissors. d The baby is “born” by expanding the uterine wound using the fingertips to cranially push the edges of the wound (arrows pointing cranially) over the babyʼs head like a collar and exerting pressure on the uterine fundus (from 12). The pressure on the fundus moves the babyʼs head in a caudal direction (s. arrows).
Uterotomy
After incising (approx. 2 cm) the uterine serosa 2 cm above the uterovesical fold, gentle pressure is used to introduce a long anatomical forceps into the uterine cavity at the level of the isthmic cervical segment at an oblique angle of approx. 30° past the foetal head or breech presentation (Fig. 1 c). Using scissors positioned between the two arms of the forceps, the uterine wall is incised along a length of 5 to 6 cm and bluntly expanded manually.
Delivery of the baby
The lower pole of the presenting part of the foetus is visible in the uterine opening and is rotated into position. In the second phase the presenting part is “born” by pushing the upper (“front”) and lower (“back”) uterine wound using the fingers of the left hand cranially over the foetal presentation (Fig. 1 d). The “birth” is assisted by pressure exerted on the uterine fundus. The uterotomy and the skin incision can be bluntly extended (digital manoeuvre) to adapt the incision to the circumference of the foetal head. The right hand of the surgeon or assistant is used to “press the baby out” of the uterus by pressing on the uterine fundus. No wound retractors (i.e. no Fritsch or Roux retractors) are required during delivery of the baby as skin elasticity is sufficient.
After delivery of the baby and clamping of the cord, a piece of the umbilical cord between two clamps is removed to determine the neonatal pH-value, and the placenta is removed using cord traction (traction using the remaining Pean clamp) and pressure on the fundus. If the placenta is complete, digital exploration of the uterine cavity is sufficient. If there is a suspicion that part of the placenta has been retained, curettage of the uterine cavity is done using a large blunt curette. Depending on the extent of cervical dilation, manual cervical dilatation or dilatation using Hegar pins is done to a width of around 3 cm.
Uterine sutures
The uterine wall is closed using 2 sutures starting from the middle of the uterotomy (Fig. 2). The 1st suture is placed 3–4 cm medially from the anatomical corner of the wound. Traction on the suture thread is used to properly approximate the corner of the wound and the wound is closed using one or two transfixing sutures. The same thread is then used to create 2–4 continuous sutures and the ends of the suture threads are knotted and left long (Fig. 2 a). Using a second suture thread the contralateral side is closed analogously (Fig. 2 b). The middle of the uterus incision which is still open is then completely closed using one of the two threads to create a continuous line of sutures (Fig. 2 c). The wound is then shortened further by alternately knotting the two ends of the suture threads, burying the suture (Fig. 2 d).
Fig. 2 a.
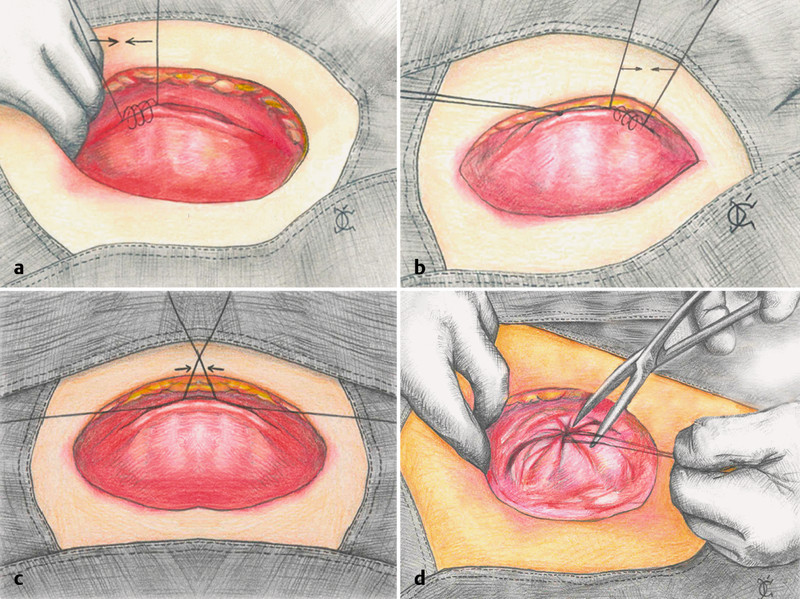
to d Uterine suture technique. The uterus is closed by 2 sutures starting from either end of the wound. a The first suture stitch is placed slightly medially from the anatomical corner of the wound. The same suture thread is used to make 2–4 more continuous sutures and the ends of the suture thread are knotted. b Analogously a second suture thread is used to close the uterine wall starting from the other side. c Both sutures are knotted in the middle and d subsequently the suture is buried by knotting the suture threads (from 12).
Closure of the peritoneum and the fascia
After inspecting both adnexa, the peritoneum is placed on the front wall of the uterus. The peritoneum is not sutured. The fascia is closed as usual using a continuous suture.
Skin suture
The skin is closed using intracutaneous continuous sutures starting and ending approx. 2 cm medial to the corners of the wound (Abb. 3). This modification permits natural drainage of wound secretions and blood. After disinfection, a large compress is placed on the wound. Although the subcutaneous adipose tissue will be free of blood at the end of the operation the compress will typically be soaked with blood after 2–3 hours and have to be replaced. Stitches are removed between the 8th and the 10th postoperative day.
Fig. 3 a.
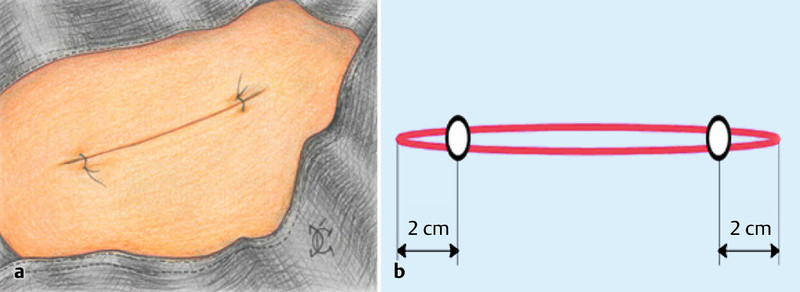
and b Skin suture. a The skin is closed using a continuous suture but both ends are left open for approx. 2 cm. b Schematic representation of the skin incision (from 12).
Instruments required
A not unimportant aspect of this modified C-section technique is the low number of instruments required, which results in a considerable reduction of costs. The following instruments are required: scalpel, Kocher forceps, 2 Pean clamps, a long anatomical forceps, long straight scissors, needle holder. Depending on the indication, obstetrical Hegar pins for cervical dilatation and a large blunt curette for curettage of the uterine cavity may be used. Both C-section techniques are described in Table 1.
Table 1 Differences between the classic and modified the procedure.
| Procedure | Vejnovic modification | Classic caesarean section |
| Skin incision | Joel-Cohen | Pfannenstiel |
| Incision of subcutaneous tissue | in the middle along a length of 3 cm | along the full length |
| Incision of the fascia | in the middle with minimal severing of the musculature | along the full length with severing of the musculature |
| Opening of the peritoneum | in the middle, blunt dissection, with minimal severing of the musculature | along the full length, sharp, bladder is pushed to one side |
| Uterotomy | superficial incision of the uterine serosa (scalpel), blunt introduction of forceps, horizontal expansion of incision using scissors | incision through all layers of the uterus using a scalpel, manual horizontal expansion |
| Placenta extraction | cord traction | manual extraction |
| Uterine suture | buried, short suture | continuous, long suture |
| Peritoneal suture | none | continuous |
| Myosuture | none | interrupted sutures |
| Subcutaneous tissue | none | interrupted sutures |
| Skin suture | intracutaneous, continuous, open at either end | intracutaneous, continuous |
Pain score
The patientʼs subjective pain sensation was assessed using the visual analogue pain scale. Pain intensity was recorded daily by the patient, with 0 representing no pain and 9 standing for worst possible pain. The pain intensity was recorded using a score: 0 no pain; 1–3 slight pain; 4–6 moderate to severe pain; 7–9 very severe pain.
Statistical evaluation
Data were obtained from questionnaires completed by the patients and from medical records (operation protocol, postoperative follow-up etc.). The data was then encoded and sent to a specially developed online database. The algorithm was subsequently additionally verified and validated (logic control). Basic descriptive methods were used for statistical analysis of the data. Absolute and relative figures, mean, standard deviation and ranges were calculated.
Statistical calculations were done using SPSS 18 (SPSS, Chicago, IL, USA). The correlation between C-section technique and clinical parameters was analysed using χ2 test and Fisherʼs exact test. Independent samples were analysed using the non-parametric Mann-Whitney U-test. Values < 0.05 were considered statistically significant.
Results
The mean age was statistically similar in both groups: 29.6 years for Group A and 28.7 for Group B (Table 2). There were no statistically significant differences between the two groups with regard to body mass index (BMI) or co-morbidities (e.g. diabetes mellitus, preoperative anaemia, etc.). A comparison with the classic C-section method showed that with the modified C-section technique the inpatient stay, particularly the postoperative in-hospital stay, could be distinctly reduced (Table 2). The comparison shows a clear decrease in blood loss (p = 0.013) and a reduction in operating times (p < 0.001). The mean loss of blood was 471 ml in Group A and 561 ml in Group B (Table 2). The mean operating time in Group A was 10 min less than the mean operating time for Group B (20.6 vs. 30.7 min).
Table 2 Patient age, in-hospital stay, duration of surgery and blood loss in both study groups.
| Group A | Group B | ||
| Parameter | n = 72 | n = 50 | p-value |
| Age (years) | 29.6 | 28.7 | 0.350 |
| Inpatient stay (days) | 5.56 | 6.08 | 0.018 |
| Duration of surgery (minutes) | 20.6 | 30.7 | < 0.001 |
| Blood loss (ml) | 471 | 561 | 0.013 |
In addition, other outcomes such as scar length, skin reddening, formation of seroma and haematoma and administration of antibiotics were analysed in relation to the chosen surgical technique. The patients operated on using the modified technique reported significantly less pain in the first 4 days postoperatively (Table 3, p < 0.001). The average length of the scar in Group A was shorter (12.6 cm) compared to the length of the scar in the control group (14.1 cm). Fewer incidences of reddening and swelling were noted in Group A compared to patients in Group B (Table 3). There were no differences between groups with regard to seroma and haematoma formation, skin dehiscence, inflammation or fever. A total 68 of 72 patients (94.4 %) in Group A and only 34 of 50 patients (68 %) in Group B reported that they were very satisfied with the C-section scar and this difference was statistically significant (p < 0.001).
Table 3 Complications in both study groups.
| Group A | Group B | ||
| Parameter | n = 72 | n = 50 | p-value |
| Pain (subjective) | Score | Score | < 0.001 |
|
2.89 | 4.1 | |
|
2.22 | 2.96 | |
|
0.71 | 1.18 | |
|
0.06 | 0.3 | |
| Length of scar (skin) | 12.6 cm | 14.1 cm | < 0.001 |
| Fever | 2.8 % | 4 % | 1.000 |
| Wound healing | |||
|
13.9 % | 32 % | 0.029 |
|
2.8 % | 14 % | 0.048 |
|
1.4 % | 0 | 1.000 |
|
0 % | 2 % | 0.854 |
|
4.2 % | 8 % | 0.617 |
Discussion
The operative technique presented here represents a further development of the so-called “gentle” Misgav-Ladach C-section technique, which is already very popular all over the world as the optimal method for caesarean section 13. Use of the modified method was introduced in the University Gynaecological Clinic of Novi Sad in Serbia in 2000 and it has been used there ever since 17. Since 3 years it has also been used very successfully in the University Gynaecological Clinic Magdeburg. The aim of the modifications was to reduce tissue trauma and minimise perioperative morbidity. These basic aims of the modified method are already discernable when performing the skin incision. In the horizontal Pfannenstiel incision and the Misgav-Ladach C-section the skin is incised 2 cm above the pubic symphysis or 2 cm below the linea interspinalis 11, 13. The incision is done using a scalpel along a length of 10–15 cm. In the Vejnovic modification, the skin is incised along the skin folds which initially results in a relatively small incision. The incision is later bluntly expanded depending on the circumference of the babyʼs head and is thus adapted to fit the circumstances. This creates a scar with an optimal length and generally with a very good cosmesis because it is not very visible in the skin folds.
The fascia are initially incised and the incision is then expanded manually (bluntly). Caudally they are no longer severed from the pyramidalis muscles. The fascia incision can also be adapted to the circumference of the babyʼs head during delivery of the baby. In contrast to classic methods and analogously to the Misgav-Ladach technique the peritoneum is opened bluntly and horizontally 11, 12, 13. This helps prevent injury to the bladder and the vasculature and excessive bleeding.
The most important modifications are related to the uterotomy and its closure. With this uterotomy technique, after incising the uterine serosa with a scalpel, long anatomical forceps are introduced through the uterus wall into the uterine cavity. By introducing the forceps obliquely past the babyʼs head, it is possible to avoid injuries to the babyʼs skin. In the classic C-section the uterine wall is completely incised, which can occasionally (e.g. if the amnion has already ruptured and the amniotic fluid is no longer present or if there is increased bleeding because the placenta is on the anterior uterine wall) result in cuts to the babyʼs skin. In the Vejnovic modification the uterotomy is incised using scissors between the arms of the forceps and is then extended bluntly. The uterotomy is “adapted” to the circumference of the babyʼs head when the head is delivered. The vertical cut using scissors through all the uterine wall layers results in a better adaptation of the two wound edges of the uterotomy, which may otherwise not always occur if they are simply bluntly “torn apart”. Closure of the uterine wall is done in a single layer as with the Misgav-Ladach method, but there are a few differences. Thus, the uterine suture is started approx. 3 cm from both corners of the wound and suturing is then continued laterally. Traction on the suture thread gives an optimal view of the wound edges. Knotting the different suture threads together reduces the size of the uterotomy to around 50 % and buries the suture. This helps avoid additional secondary sutures to treat bleeding from the uterine wall. The resulting scar is short with a relatively thick myometrium and very stable. This is done with the aim of decreasing the incidence of uterine rupture and suture dehiscence and minimising placental disorders in subsequent pregnancies. While complete uterine rupture after a classic or Misgav-Ladach C-section is rare (0.7 % after one and 0.9 % after repeated C-section deliveries, cf. 19, 20), the length of the uterotomy scar, measured ultrasonographically after a C-section, appears to correlate with suture dehiscence during birth. It has been shown that suture dehiscence or uterine rupture occurs in 5.3 % of cases with smaller scars compared to 42.9 % with large scars 21. Whether this suture technique could be an important factor in preventing uterine rupture in subsequent pregnancies will only be clear with longer follow-up times. As more than 7000 C-sections have been carried out using the new technique at the University Gynaecological Clinics of Novi Sad and Magdeburg, the data obtained could offer a good basis to answer such questions.
In contrast to other C-section techniques, in the modified C-section technique presented here the fascia and skin incisions are adapted to the size of the babyʼs head or breech position by manually pushing back the anterior and posterior uterine walls. The baby is literally “born” through pressure exerted on the uterine fundus. It is conceivable that this compression pressure could help expel amniotic fluid from the lungs as occurs in vaginal births. Only a prospective study in a defined patient collective could show whether there are fewer respiratory adjustment disorders with the method described here compared to classic caesarean sections.
The fascia is closed using a continuous suture as is done in other C-section techniques. The two ends of the skin suture are left 2 cm open. This modification creates “natural drainage” and helps prevent haematomas and seromas. The cosmesis with this method is very good as the initially open edges of the wound close within a few hours and no fluid-filled cavities remain subcutaneously.
Conclusion
C-sections are the most common obstetrical operations. In Germany around one third or all children are now delivered by caesarean section. This amounts to approximately 200 000 C-sections annually. The “gentle” Misgav-Ladach C-section technique is currently the standard procedure used in Germany. The modification of the caesarean section technique described here changes the position and length of the skin incision, avoids injury to the baby by the blunt introduction of forceps into the uterus and involves a different type of closure of the uterine wall. This new type of closure should help reduce complications in subsequent pregnancies. The first promising results are expected from prospective studies in a defined patient collective.
Footnotes
Conflict of Interest The authors declared they have no financial ties to any company relevant for this paper.
Supporting Information
German supporting information for this article
References
- 1.Keunen JHrsg.Der Kaiserschnitt München: Elsevier, Urban & Fischer Verlag; 2008100–108. [Google Scholar]
- 2.http://www.destatis.de/jetspeed/portal/cms/Sites/destatis/Internet/DE/Presse/Pm/2011/03/PD11__117__231,templateId=renderPrint.psmlStand: 13.10.2011
- 3.Wacker J. Geburtshilfe. Kaiserschnitt vs. Natürliche Geburt. Geburtsh Frauenheilk. 2010;70:840–843. [Google Scholar]
- 4.Beckmann M W, Bader W, Bechtold I. et al. Finanzierung und finanzielle Probleme von Leistungen und Strukturen im Fachgebiet Gynäkologie und Geburtshilfe im Jahr 2011 – allgemeine Aspekte und geburtshilfliche Versorgung. Geburtsh Frauenheilk. 2011;71:367–380. [Google Scholar]
- 5.Dudenhausen J W, Golic M, Kirschner R. et al. Geburtsleitung bei dichorialen Zwillingen am Termin bei vorangehendem Zwilling in Schädellage – eine monozentrische retrospektive Kohortenstudie. Geburtsh Frauenheilk. 2010;70:985–989. doi: 10.1055/s-0030-1267218. [DOI] [PubMed] [Google Scholar]
- 6.Hickl E J. Wandlungen in der Kaiserschnittsindikation. Gynäkol Geburtsh Rundschau. 2002;42:15–18. doi: 10.1159/000057933. [DOI] [PubMed] [Google Scholar]
- 7.Schlembach D. Pränatalmedizin. Intrauterine Wachstumsrestriktion – Diagnostik und Management. Geburtsh Frauenheilk. 2012;72:373–375. [Google Scholar]
- 8.Ladendorf B. Placenta percreta, Vasa praevia und Placenta praevia marginalis. Geburtsh Frauenheilk. 2010;70:A20. [Google Scholar]
- 9.Welsch H, Wischnik A. Berlin: Springer Verlag; 2006. Müttersterblichkeit; pp. 1049–1063. [Google Scholar]
- 10.Kunze M Hart J Lynch A et al. Intrapartales Management von Patientinnen mit vorzeitigem Blasensprung: maternales und fetales Outcome Geburtsh Frauenheilk 201171 - V_16 [Google Scholar]
- 11.Pfannenstiel J. Über die Vorteile des surprasymphysären Faszienquerschnittes für die gynäkologischen Koliotomien, zugleich ein Beitrag zu der Indikationsstellung der Operationswege. Samml Klein Vortr Gynäkol. 1900;97:68–98. [Google Scholar]
- 12.Joel-Cohen S J. London: William Heinemann Medical Books; 1972. Abdominal and vaginal hysterectomy. New techniques based on time and motion studies; p. 170. [Google Scholar]
- 13.Stark M. München: Elsevier, Urban & Fischer Verlag; 2008. Optimierte operative Methode; pp. 160–176. [Google Scholar]
- 14.Hofmeyer G J Mathai M Shah A et al. Techniques for caesarean section Cochrane Database Syst Rev 20081CD004662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hofmeyer G J, Novikova N, Mathai M. et al. Techniques for caesarean section. Am J Obstet Gynecol. 2009;201:431–444. doi: 10.1016/j.ajog.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 16.Rasenack R, Schneider C, Jahnz E. et al. Factors associated with the duration of breastfeeding in the Freiburg birth collective, Germany (FreiStill) Geburtsh Frauenheilk. 2012;72:64–69. doi: 10.1055/s-0031-1280470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vejnović T R Cesarean delivery – Vejnović modification Srp Arh Celok Lek 200813602109–115.(Serbian) [DOI] [PubMed] [Google Scholar]
- 18.Doerfler H. 30 Jahre Schnittentbindung. Münch Med Wochenschr. 1929;1:2–6. [Google Scholar]
- 19.Lydon-Rochelle M, Holt V L, Easterling T R. et al. Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med. 2001;345:3–8. doi: 10.1056/NEJM200107053450101. [DOI] [PubMed] [Google Scholar]
- 20.Landon M B, Spong C Y, Thom E. et al. Risk of uterine rupture with a trial of labor in women with multiple and single prior cesarean delivery. Obstet Gynecol. 2006;108:12–20. doi: 10.1097/01.AOG.0000224694.32531.f3. [DOI] [PubMed] [Google Scholar]
- 21.Vikhareva Osser O, Valentin L. Clinical importance of appearance of caesarean hysterotomy scar at transvaginal ultrasonography in nonpregnant women. Obstet Gynecol. 2011;117:525–532. doi: 10.1097/AOG.0b013e318209abf0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
German supporting information for this article


