Abstract
Background:
Musculoskeletal ultrasound (MSKUS) is becoming more and more popular in the evaluation of different musculoskeletal abnormalities. The aim of this retrospective study was to document the prevalence and spectrum of MSKUS findings at the painful knee.
Materials and Methods:
All the studies of MSKUS that were performed for the evaluation of knee pain during the previous 2 years at the Department of Radiology in Nazareth hospital were reviewed. Demographic and clinical parameters including age, gender, side, and MSKUS findings were documented.
Results:
Two hundred and seventy-six patients were included in the review. In 21 of them, both knees were evaluated at the same setting (total number of knees evaluated was 297). One hundred and forty-four knees were of the left side. Thirty-three pathologies were identified. 34% of the studies were negative. The most common MSKUS findings were medial meniscal tear (MMT) (20%), Baker's cyst (BC) (16%), and osteoarthritis (OA) (11%). Only one knee of all the knees evaluated in our study showed synovitis. Fifty-three knees (18% of all the knees evaluated) had more than one imaging finding, mosty two and while some had three findings. The most common combination of findings was MMT and BC (8 knees), MMT with OA (8 knees), and MMT with fluid (6 knee). In 67% of the patients who had simultaneous bilateral knee evaluation, at least one knee had no abnormal findings and in 43%, both knees were negative.
Conclusions:
MSKUS has the potential for revealing huge spectrum of abnormalities. In nearly 90% of the positive studies, degenerative/mechanical abnormalities were reported, with MMT, BC, and osteoarthritic changes being the most common.
Keywords: Abnormal findings, knee, pathology, ultrasound
INTRODUCTION

Musculoskeletal ultrasound (MSKUS) is becoming more and more popular in the evaluation and management of different problems in rheumatology. Its first clinical application in rheumatology was reported in 1974 with the differentiation of a Baker's cyst (BC) from thrombophlebitis.[1] MSKUS has been shown to be helpful in the evaluation of joint, tendon, muscle, bursa, bone, and other soft tissue abnormalities.[2,3,4,5,6] It has the ability to directly visualize, characterize, and quantify the earliest and smallest inflammatory and structural changes. These qualities can also help in directing appropriate treatment and monitoring response and disease progression.
MSKUS has several unique features, which not only aid in performance of the above measurements but also confer significant advantages over other imaging techniques. It is safe, non-invasive, and has no ionizing radiation. It is portable and can be made available in an out-patient setting, enabling rapid, “real-time,” and dynamic examination of one or more joints or areas.
The Doppler dimension of this modality adds important information regarding vascular components that ultimately help in identifying abnormalities like synovitis, hemangiomas, and tumors.[7,8] Enhanced-contrast ultrasound and 3-D ultrasonography (US) improve the sensitivity, specificity, and accuracy of this modality.[9,10] Knees are rich in tendons, muscles, blood vessels, nerves, and bursa that can be the source of different complaints of the patient. Knee pain in patients is a common problem facing family physicians, orthopedics, or rheumatologists. This retrospective study was designed to evaluate the results of all MSKUS studies of the painful knee performed at the Nazareth hospital during the last 2 years.
MATERIALS AND METHODS
All MSKUS studies of the knee that were done from January 2012 to December 2013 at the Nazareth hospital were identified from the registry of MSKUS studies in the Department of Radiology. Only those studies that were performed for the evaluation of knee pain were included in our review. Exclusion criteria included studies that were performed for causes other than evaluation of knee pain, such as guidance for arthrocentesis or local injections. All studies carried out on the same patient were considered as one study (the first study). Demographic and clinical parameters including age, gender, complaint, side of the knee evaluated (right, left, or both), and MSKUS findings were documented. Philips HD 11 (Amsterdam, the Netherlands) ultrasound machine with Philips (New York, USA) L12-3 MHz probe was used.
The term “osteoarthritis” (OA) was used when there was a difference in cartilage thickness between the medial and lateral compartments, osteophytes, meniscal protrusion, or cartilage damage. The term “tendinopathy” was used for degenerative changes or for calcifications observed at the patellar or quadriceps tendons.
In case of more than one finding documented by the evaluating radiologist, all the findings were included if every finding could be associated with knee pain. These findings were listed as belonging to one knee.
This study was approved by the local ethics committee of the Nazareth hospital.
RESULTS
Three hundred and two patients were identified for this study. In 26 patients, MSKUS studies were done to guide intra-articular corticosteroid injections and were excluded from the review. The rest of the patients (276) were included in our review. Ninety-one percent of the patients were referred from outside the hospital and mainly by family physicians. Twenty-one patients had both knees evaluated at the same sitting, so the total number of evaluated knees included in our study was 297. One hundred and forty-four knees were on the left side. One hundred knees (34%) had no abnormal findings, 138 knees had just one finding on the report, 45 (~15%) knees had two findings, and 8 knees (~3%) had three findings. None had four findings reported. Eight knees were reported to have subcutaneous lipoma (as one finding only) that was felt not to be associated with knee pain, so the total number of positive findings in all the knees evaluated was 244.
All the studies during the years 2012-2013 were conducted by the first author who is an experienced radiologist in the field of MSKUS.
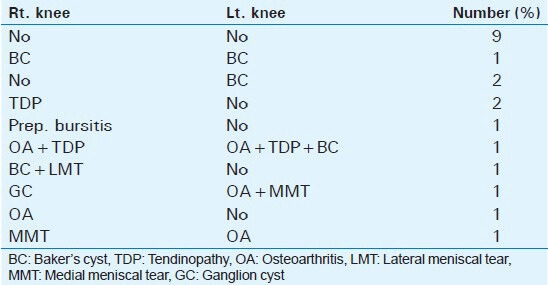
Table 1 summarizes the demographics, side, and the different findings of all of MSKUS studies at the knee, which could be associated with knee pain. Due to the fact that in the overwhelming majority of the referrals, the exact duration of symptoms was not included, no data regarding duration of symptoms/signs was included in the table. Overall, 33 types of abnormalities were recorded. Table 2 summarizes the combination of findings that were reported of the same knee and their frequencies. Table 3 summarizes the findings in each knee among patients who had both knees evaluated at the same sitting.
Table 1.
Demographic, clinical, and MSKUS findings of all the studies of the knee
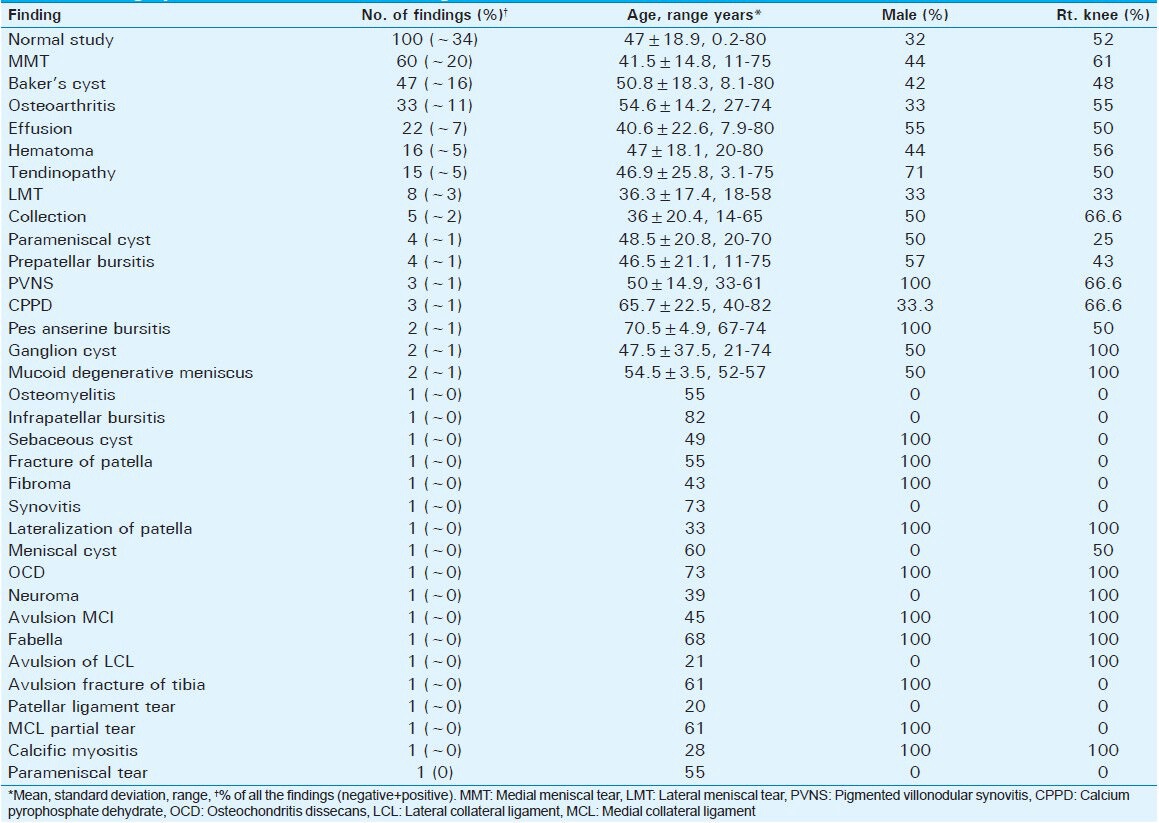
Table 2.
Findings of patients who had more than one finding on US evaluation of the same knee
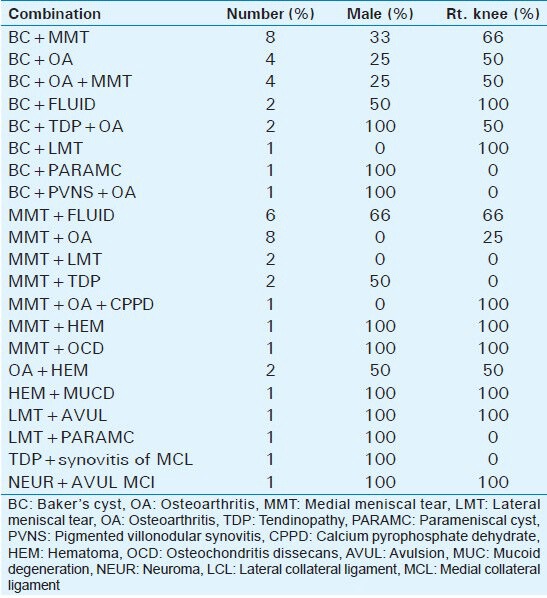
Table 3.
Findings on each knee in patients who had both knees evaluated at the same sitting
DISCUSSION
The most prominent finding in our study is the huge spectrum of MSKUS findings at the knee that could be the reason for knee pain or is associated with it [Table 1]. Also prominent is the near absence of inflammatory findings, with only one case (~0%) of synovitis at the knee joint. Such a finding points to the fact that in cases of knee synovitis, the diagnosis is usually made clinically and there is no special need for MSKUS assistance. Rheumatologic research using MSKUS of the knee in patients with synovitis had focused on quantification of the synovitis rather than diagnosis of synovitis.[11] On the other hand, non-inflammatory causes of knee pain are diverse and cannot be easily predicted clinically, and MSKUS is needed here to elucidate the etiology of the non-inflammatory causes of knee pain. Yet, it can be seen that in nearly 34% of the patients, the MSKUS report for the evaluation of knee pain was negative. Such report could be due to many reasons, including referred pain to the knee area, non-serious ligament problem, or mild intra-articular finding/s that could not be picked up by the MSKUS.
In general, there was no significant difference between the various findings of right and left knees. More patients with OA and medial meniscal tear (MMT) on the right knee were observed, but not significantly more.
The most common MSKUS findings associated with knee pain in our study were MMT [Figure 1], BC [Figure 2], OA [Figure 3], knee effusion [Figure 4] (other than BC), hematoma, and tendinopathy [Figure 5]. All these findings accounted for nearly 79% of the positive findings. In the literature, there are no reported studies about the spectrum of ultrasonographic findings from one or more centers over an extended period of time. This makes our study unique in its comprehensiveness.
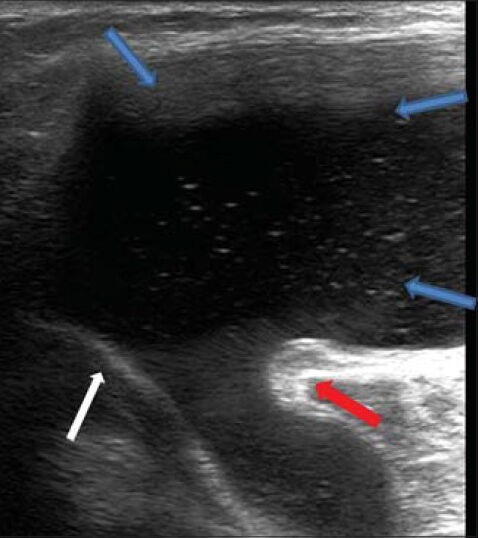
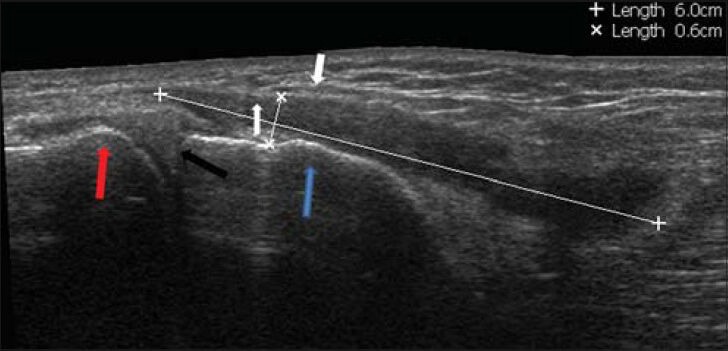
Figure 1.
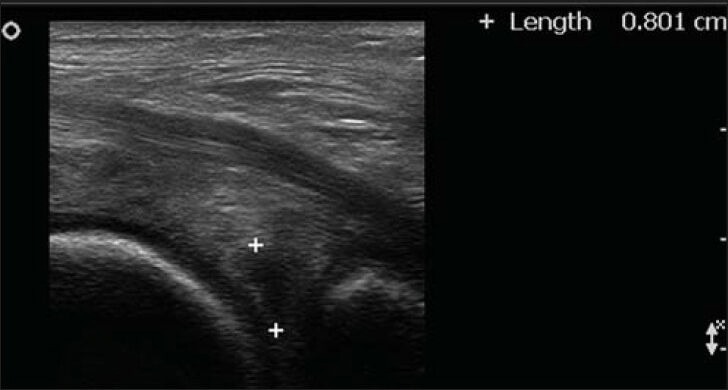
62-year-old male who had pain in the right knee mainly while going down the stairs diagnosed with medial meniscal tear. Ultrasound of the posterior medial part of the knee shows meniscal tear (hypoechoic lesion between plus signs) of the posterior horn of the medial meniscus.
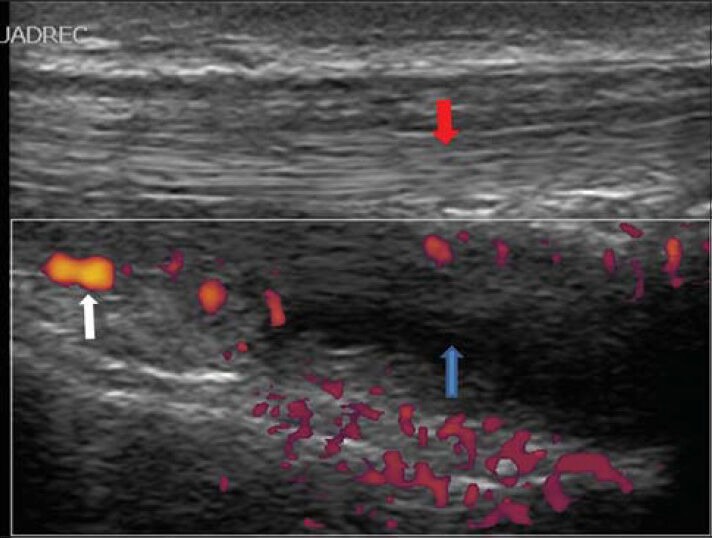
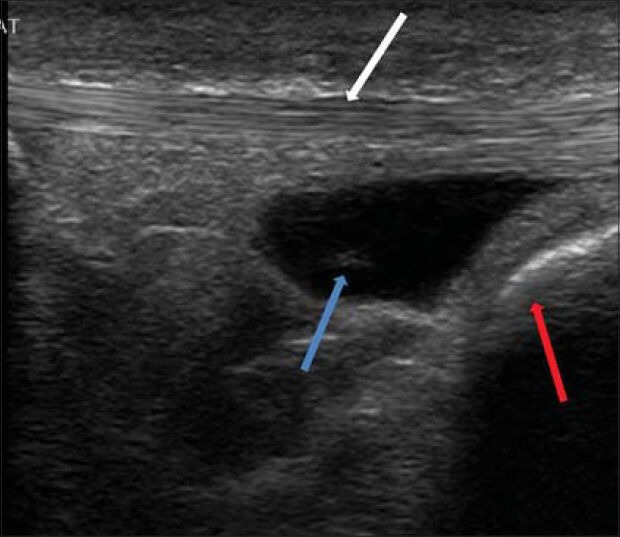
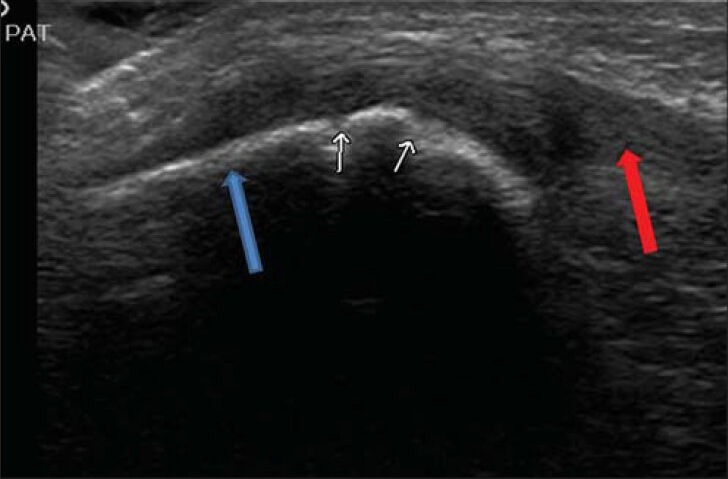
Figure 2.
41-year-old man who complained of painful mass in the posterior aspect of the right knee diagnosed as due to Baker's cyst. Ultrasound of the right posterior medial aspect of the knee shows a huge Baker's cyst (between blue arrows) with a connecting neck, lying between the medial gastrocnemius muscle (red arrow) and the semi-membranous tendon (white arrow).
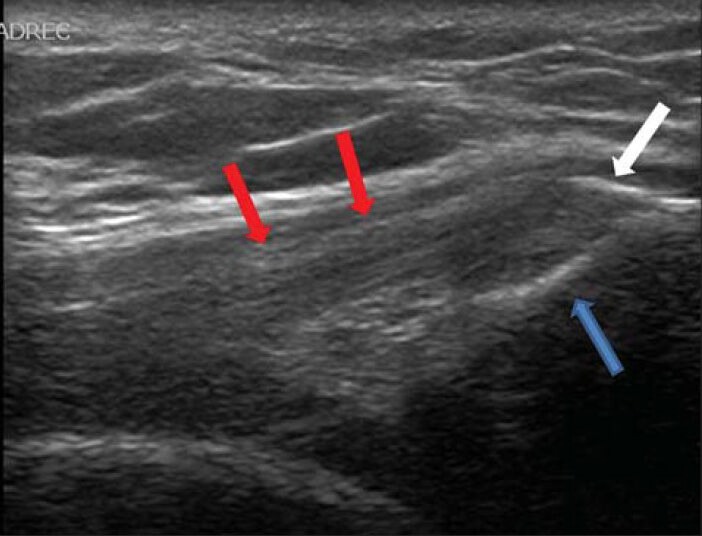
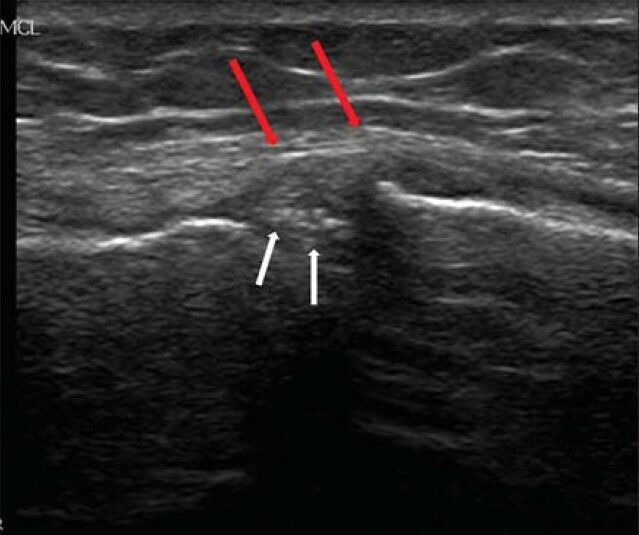
Figure 3.

67-year-old female who had right knee pain with difficulty in walking diagnosed with osteoarthritis. Ultrasound of the right knee shows normal thick cartilage at the level of the lateral femoral condyle, hypoechoic, elongated structure (a, white arrows), and loss of cartilage at the medial femoral condyle (b, between red arrows). Such a finding is suggestive of severe osteoarthritis.
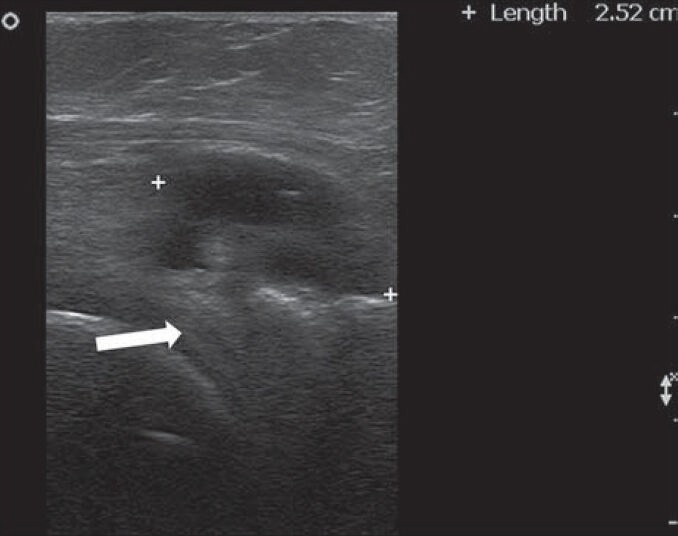
Figure 4.
14-year-old male who suffered from painful and limited movement of the right knee diagnosed with knee effusion. Ultrasound power Doppler shows fluid in the suprapatellar bursa (blue arrow) deep to the quadriceps ligament (red arrow) with increased flow (white arrow), a sign of active arthritis.
Figure 5.
53-year-old lady who suffered from anterior knee pain diagnosed as tendinopathy. Ultrasound of left knee shows tendinopathy with calcifications (white arrow) at the patellar side (blue arrow) of the quadriceps ligament (red arrows).
Medial and lateral menisci are important components of the knee. They provide shock absorption and load transmission.[9] Meniscal tear could be degenerative or acute due to trauma. Risk factors for the development of meniscal tear include age (>60 years), male gender, and occupational factors such as work-related squatting, kneeling, and stair climbing.[10] Meniscal tear is usually associated with knee pain and functional impairment. It could be longitudinal, horizontal, radial, vertical flap, horizontal flap, or complex. Surgery is usually needed to reduce pain and improve the function. The characteristic sonographic findings of meniscal tear are protrusion and hypoechoic stripe through the meniscus. In one study, it was found that the sensitivity, specificity, positive and negative predictive values of sonography as compared to arthroscopy were 85.4%, 85.7%, 67.3%, and 94.4%, respectively.[12]
Other meniscal abnormalities that were reported in our study include parameniscal and meniscal cyst [Figure 6] (<1%) and mucoid meniscal degeneration. These findings were relatively rare.
Figure 6.
60-year-old lady who suffered from increasing right knee pain while walking diagnosed as due to meniscal cyst. Ultrasound of the posterior aspect of right knee shows cyst (between plus signs) of the posterior lateral meniscal horn (white arrow).
Baker's cyst, as mentioned in the Introduction, was the first sonographic finding of the first application of MSKUS.[1] It represents a loculated fluid in the popliteal fossa with different sizes that could be associated with complaints ranging from asymptomatic to excruciating pain at the back of the knee or calf as a result of rupture of the BC, or dissecting down through the calf muscles. BC results from intra-articular effusion secondary to both mechanical and inflammatory causes. The prevalence of BC ranges from 6.6 to 25% in the literature.[13,14] It correlated with knee effusion and osteoarthritic findings. The prevalence of BC in our study was not different from the average reported in the literature (14%). Usually BCs are classified as simple or complex and the classic sonographic findings include anechoic cystic lesion with continuation through a neck between the semi-membranous tendon and the medial gatrocnemius muscle. It could also be associated with internal septations and debris due to previous bleeding.
Knee effusion (other than BC) is one of the major clinical and sonographic findings of the knee. Knee effusion usually represents an intra-articular derangement, mainly OA, and the evaluation of the knee joint fluid following arthrocentesis can help differentiate degenerative from inflammatory causes. It can also give a hint for diagnosis in the case of hemarthrosis [trauma, anticoagulation problems, or pigmented villonodular synovitis (PVNS)]. Knee effusion is mostly seen at the suprapatellar pouch in the supine position, especially at the anterior side.[15] Also, 30° flexion position of the knee is the most sensitive position for the detection of knee fluid.[16]
OA changes of the knee can also be clearly visualized by MSKUS [Figure 3]. In the evaluation of knee osteoarthritic changes, the cartilage and synovial thicknesses are appreciated, in addition to fluid, marginal femorotibial osteophytes, and meniscal protrusion.[17] It had been shown that 3-D US correlates strongly with magnetic resonance imaging regarding cartilage thickness.[18] It had been also shown that MSKUS is a promising modality in evaluating subchondral bone changes in OA of the knee.
Tendinopathy, especially of the patellar and qudrifemoris tendons (anterior side) [Figure 5] in addition to the hamstring and semi-membranous tendons (posterior side), can all cause knee pain. The patellar tendon is the most evaluated tendon at the knee area, where increased blood flow and calcification could be an evidence of tendinopathy. Patellar tendinopathy usually occurs among athletes, especially those who jump (volleyball and basketball players), in what is called “jumper's” knee.[19] Subcutaneous hematoma around the knee is usually the result of trauma or occurs subsequent to total knee arthroplasty or arthroscopy, especially among patients on low-molecular-weight heparin. Other than typical superficial skin features of hematoma, usually there are MSKUS findings of loculated hematoma.
The knee joint is surrounded by different bursa including prepatellar, infrapatellar, suprapatellar, and pes anserine bursa. All these bursa could be inflamed and be the source of knee pain. There are relatively few US studies about different types of bursitis around the knee area. Pes anserine bursitis [Figure 7] is not uncommon and is usually associated with knee pain at the medial side. It occurs more in diabetic patients and possibly also in obese patients with OA of the knee.[20] There could be normal anatomic variations in the location of this bursa, most commonly between the pes anserine tendons and the patella.[21]
Figure 7.
39-year-old man who suffered from pain in the medial aspect of the distal right knee diagnosed with Pes anserine bursitis. Extended panoramic ultrasound view of the medial part of the knee shows fluid in the pes anserinus bursa (asterisks), that was located between the pes anserine ligament (white arrows), medial condyle of the femur (red arrow), medial meniscus (black arrow), and medial distal part of the tibia (blue arrow).
Infrapatellar bursitis [Figure 8] is more common in male workers exposed to heavy workloads and frequent kneeling.[22] Prepatellar bursa is located exactly at the front of the patella. Pain and tenderness of the bursa with no skin redness suggests prepatellar bursitis or the so-called housemaid's knee [Figure 9]. The differential diagnosis includes cellulitis, synovitis, septic arthritis, and patellar osteomyelitis.[23]
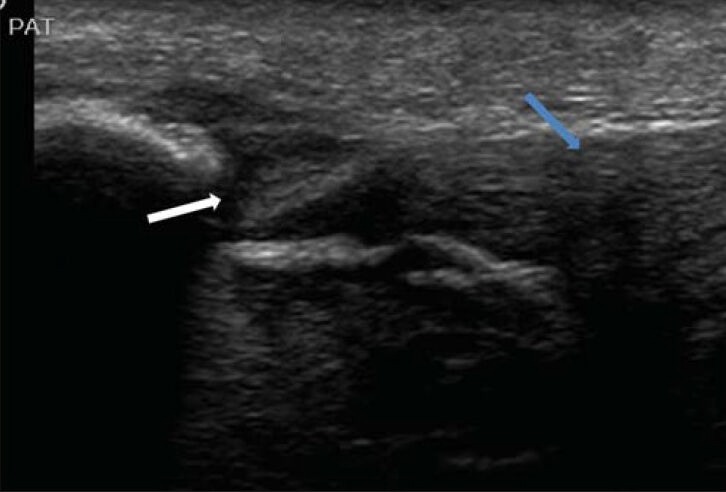
Figure 8.
57-year-old male who suffered from pain in the distal portion of the anterior knee diagnosed with infra-patellar bursitis. Ultrasound shows fluid in the infrapatellar bursa (blue arrow) that was confined between the patellar tendon (white arrow) and distally with the anterior tibial tuberosity (red arrow).
Figure 9.
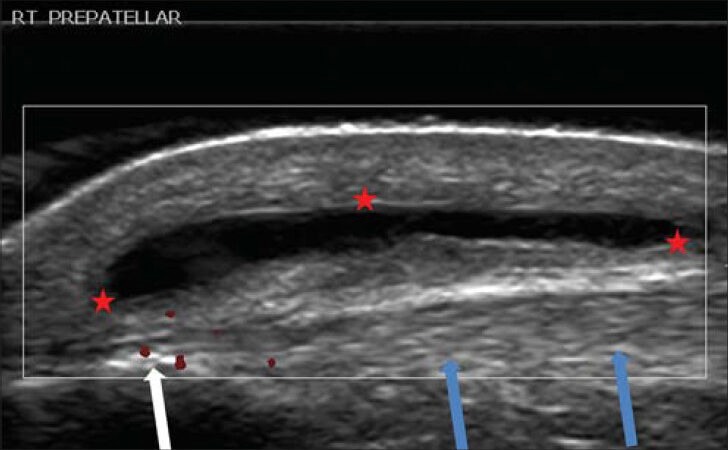
33-year-old female who suffered from painful mass in the anterior part of the right knee diagnosed as having housemaid's knee. Ultrasound of the anterior knee shows prepatellar bursitis (between red asterisks), the so-called housemaid's knee. This bursa was situated superficial to the patellar ligament (blue arrows) and to the patella (white arrow).
Medial collateral ligament is the most frequently injured ligament at the knee.[24] It usually results from sport activity and treatment is mostly conservative. Injuries, in general, might include blunt or shear trauma that leads to partial or full tear of tendons and ligaments [Figure 10]. In more serious cases, avulsion of the ligaments, which means complete or partial detachment of its insertion accompanied by meniscal or bone site fracture [Figure 11], might occur. Other than severe pain, serious injury could result in instability of the knee. Radiology sometimes misses the finding, especially when the detached bone is so small, but US has higher sensitivity.
Figure 10.
37-year-old female who suffered from limited range of flexion of the knee, associated with pain and swelling of the knee, after falling down with a flexed knee while running. Ultrasound shows partial tear (white arrow) of the patellar tendon (blue arrow).
Figure 11.
8-year-old girl suffered from pain at the anterior part of the right knee after falling down on a pedestrian walk. X-ray of the patella revealed no pathology. Ultrasound of knee shows avulsion fracture (white small arrows) of the anterior part of the patella (blue arrow) with partial tear of the proximal section of the patellar tendon (red arrow).
Our study did not include any case of anterior cruciate ligament (ACL) problem. Injuries of ACL usually occur in athletics. Sonography is not routinely used for the evaluation of ACLs. It is not easy or convenient to inspect ACL directly by MSKUS.[25] Methods for direct visualization of the ACL using MSKUS are being developed. It could be that ACL injuries are under-represented in our study and, hopefully, we will have more experience in the near future in our hospital and elsewhere for routine inspection of ACLs in the evaluation of knee pain.
MSKUS had a sensitivity of 84.3% and specificity of 100% in detecting calcium pyrophosphate dehydrate (CPPD) crystals [Figure 12].[26] It can detect Type I deposits (hyperechoic), Type II deposits (punctuate), and Type III deposits (hyperechoic nodular and/or oval deposits).
Figure 12.
74-year-old female who suffered from knee pain daily while walking diagnosed as due to presence of calcium pyrophosphate dehydrate crystals. Ultrasound of the right knee shows punctuate calcification “hyperechoic foci” in the medial meniscus (white arrows) that was medially located to the medial collateral ligament (red arrows).
When looking at the combinations of findings (double findings only), the most common combination was MMT with BC (8 knees), MMT with OA (8 knees), followed by MMT with knee effusion (6 knees) and BC with OA (4 knees). There are few studies addressing the association between different findings at the knee.[27] However, the association of meniscal tears with OA, mainly cartilage changes, is well known.[28]
There were eight knees with triple findings. The most common triple findings were MMT with BC and OA (4 knees), followed by BC with OA and tendinopathy. In the literature, there is no data about association of three entities similar to what we mention in this study. Such combinations are not surprising, especially when the pathogenesis of either one of them overlaps with the other. It could also be that the low frequencies of such combination in the literature are due to under-reporting.
The results of patients who had simultaneous bilateral evaluation of both knees showed that the most frequent combination was negative findings in nine patients (~43%), followed by BC in one and no findings in the other knee [2 (5%) patients] and tendinopathy in one knee with no findings in the other knee (2 patients). It is interesting to note also that in 67% of the patients who had simultaneous bilateral knee evaluation, at least one knee had no abnormal findings. In clinical practice, symmetrical joint pain usually results from soft tissue problem/s that are not usually visualized by MSKUS, rather than due to prominent articular pathologies. It might also be that when a patient asks for Ultrasound of the knee, the tendency of the patient is to ask for an evaluation of the other knee that might have less degree of pain with negative clinical findings.
CONCLUSION
Our study revealed that ultrasound can be used to assess a large number of pathologies of the knee. No difference was seen between the pathologies of the right knee and the left knee. MSKUS is a safe, non-ionic, dynamic study that should be used as the first line of imaging in evaluating a painful knee.
Footnotes
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/45/139735
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Meire H, Lindsay DJ, Swinson DR, Hamilton EB. Comparison of ultrasound and positive contrast arthrography in the diagnosis of popliteal and calf swellings. Ann Rheum Dis. 1974;33:408. doi: 10.1136/ard.33.4.408-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Micu MC, Nestorova R, Petranova T, Porta F, Radunovic G, Vlad V, et al. Ultrasound of the ankle and foot in rheumatology. Med Ultrason. 2012;14:34–41. [PubMed] [Google Scholar]
- 3.Coates LC, Hodgson R, Conaghan PG, Freeston JE. MRI and ultrasonography for diagnosis and monitoring of psoriatic arthritis. Best Pract Res Clin Rheumatol. 2012;26:805–22. doi: 10.1016/j.berh.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Lee SJ, Jacobson JA, Kim SM, Fessell D, Jiang Y, Dong Q, et al. Ultrasound and MRI of the peroneal tendons and associated pathology. Skeletal Radiol. 2013;42:1191–200. doi: 10.1007/s00256-013-1631-6. [DOI] [PubMed] [Google Scholar]
- 5.Hayashi D, Hamilton B, Guermazi A, de Villiers R, Crema MD, Roemer FW. 5.Traumatic injuries of thigh and calf muscles in athletes: Role and clinical relevance of MR imaging and ultrasound. Insights Imaging. 2012;3:591–601. doi: 10.1007/s13244-012-0190-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Langmann GA, Vujevich KT, Medich D, Miller ME, Perera S, Greenspan SL. Heel ultrasound can assess maintenance of bone mass in women with breast cancer. J Clin Densitom. 2012;15:290–4. doi: 10.1016/j.jocd.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Falcao S, de Miguel E, Castillo-Gallego C, Peiteado D, Branco J, Martín Mola E. Achilles enthesis ultrasound: The importance of the bursa in spondyloarthritis. Clin Exp Rheumatol. 2013;31:422–7. [PubMed] [Google Scholar]
- 8.Ikeda K, Nakagomi D, Sanayama Y, Yamagata M, Okubo A, Iwamoto T, et al. Correlation of radiographic progression with the cumulative activity of synovitis estimated by power Doppler Ultrasound in rheumatoid arthritis: Difference between patients treated with methotrexate and those treated with biological agents. J Rheumatol. 2013;40:1967–76. doi: 10.3899/jrheum.130556. [DOI] [PubMed] [Google Scholar]
- 9.Maffulli N, Longo UG, Campi S, Denaro V. Meniscal tears. Open Access J Sports Med. 2010;1:45–54. doi: 10.2147/oajsm.s7753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Snoeker BA, Bakker EW, Kegel CA, Lucas C. Risk factors for meniscal tears: A systematic review including meta-analysis. J Orthop Sports Phys Ther. 2013;43:352–67. doi: 10.2519/jospt.2013.4295. [DOI] [PubMed] [Google Scholar]
- 11.Vlad V, Iagnocco A. Ultrasound of the knee in rheumatology. Med Ultrason. 2012;14:318–25. [PubMed] [Google Scholar]
- 12.Wareluk P, Szopinski KT. Value of modern sonography in the assesment of meniscal lesions. Eur J Radiol. 2012;81:2366–9. doi: 10.1016/j.ejrad.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 13.Picerno V, Filippou G, Bertoldi I, Adinolfi A, Di Sabatino V, Galeazzi M, et al. Prevalence of Baker's cyst in patients with knee pain: An ultrasonographic study. Reumatismo. 2014;65:264–70. doi: 10.4081/reumatismo.2013.715. [DOI] [PubMed] [Google Scholar]
- 14.Iagnocco A, Meenagh G, Riente L, Filippucci E, Delle Sedie A, Scirè CA, et al. Ultrasound imaging for the rheumatologist XXIX. Sonographic assessment of the knee in patients with osteoarthritis. Clin Exp Rheumatol. 2010;28:643–6. [PubMed] [Google Scholar]
- 15.Hirsch G, O’Neill T, Kitas G, Klocke R. Distribution of effusion in knee arthritis as measured by high-resolution ultrasound. Clin Rheumatol. 2012;31:1243–6. doi: 10.1007/s10067-012-1987-3. [DOI] [PubMed] [Google Scholar]
- 16.Mandl P, Brossard M, Aegerter P, Backhaus M, Bruyn GA, Chary-Valckenaere I, et al. Ultrasound evaluation of fluid in knee recesses at varying degrees of flexion. Arthritis Care Res (Hoboken) 2012;64:773–9. doi: 10.1002/acr.21598. [DOI] [PubMed] [Google Scholar]
- 17.Yanagisawa S, Ohsawa T, Saito T, Kobayashi T, Yamamoto A, Takagishi K. Morphological evaluation and diagnosis of medial type osteoarthritis of the knee using ultrasound. J Orthop Sci. 2014;19:270–4. doi: 10.1007/s00776-013-0524-9. [DOI] [PubMed] [Google Scholar]
- 18.Ohashi S, Ohnishi I, Matsumoto T, Bessho M, Matsuyama J, Tobita K, et al. Measurment of articular cartilage thickness by using a three-dimentional image reconstructed from B-mode ultrasonography mechanical scans feasibility study by comparison with MRI-derived data. Ultrasound Med Biol. 2012;38:402–11. doi: 10.1016/j.ultrasmedbio.2011.11.019. [DOI] [PubMed] [Google Scholar]
- 19.Visnes H, Tegnander A, Bahr R. Ultrasound characteristics of the patellar and quadriceps tendons among young elite athletes. Scand J Med Sci Sports. 2014 doi: 10.1111/sms.12191. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Alvarez-Nemegyei J, Canoso JJ. Evidence-based soft tissue rheumatology IV. Anserine bursitis. J Clin Rheumatol. 2004;10:205–6. doi: 10.1097/01.rhu.0000135561.41660.b0. [DOI] [PubMed] [Google Scholar]
- 21.Imani F, Rahimzadeh P, Abolhasan-Gharehdag F, Faiz SH. Sonographic variation of pes anserine bursa. Korean J Pain. 2013;26:249–54. doi: 10.3344/kjp.2013.26.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Le Manac’h AP, Ha C, Descatha A, Imbernon E, Roquelaure Y. Prevalence of knee bursitis in workforce. Occup Med (Lond) 2012;62:658–60. doi: 10.1093/occmed/kqs113. [DOI] [PubMed] [Google Scholar]
- 23.Choi HR. Patellar osteomyelitis presenting as prepatellar bursitis. Knee. 2007;14:333–5. doi: 10.1016/j.knee.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 24.Duffy PS, Miyomoto RG. Management of medial collateral ligament injuries in the knee: An update and review. Phys Sportsmed. 2010;38:48–54. doi: 10.3810/psm.2010.06.1782. [DOI] [PubMed] [Google Scholar]
- 25.Chen P, Wu C, Yu C, Wang J, Shih T, Wang T, et al. Sonography of the normal anterior cruciate ligament: A preliminary report. J Med Ultrasound. 2013;21:16–20. [Google Scholar]
- 26.Ellabban AS, Kamel SR, Omar HA, El-Sherif AM, Abdel-Magied RA. Ultrasonographic diagnosis of articular chondrocalcinosis. Rheumatol Int. 2012;32:3863–8. doi: 10.1007/s00296-011-2320-1. [DOI] [PubMed] [Google Scholar]
- 27.Stein D, Cantlon M, Mackay B, Hoelscher C. Cysts about the knee: Evaluation and management. J Am Acad Orthop Surg. 2013;21:469–79. doi: 10.5435/JAAOS-21-08-469. [DOI] [PubMed] [Google Scholar]
- 28.Guermazi A, Hayashi D, Jarraya M, Roemer FW, Zhang Y, Niu J, et al. Medial posterior meniscal root tears are associated with development or worsening of medial tibiofemoral cartilage damage: The multicenter osteoarthritis study. Radiology. 2013;268:814–21. doi: 10.1148/radiol.13122544. [DOI] [PMC free article] [PubMed] [Google Scholar]


