Abstract
Objectives :
Shoulder disorders have an important impact on a patient’s capacity to work. We investigated whether there is a relationship between subjective or objective outcome measures and the ability and time for returning to work (RTW) after a proximal humerus fracture (PHF).
Design :
Retrospective single-centre study from March 2003 to June 2008.
Setting :
City hospital, trauma level one centre.
Intervention :
All PHF stabilized with a PHILOS®.
Main Outcome Measurements :
Routine follow-up examinations (X-ray, Constant-Murley Score (CMS), Short-Form 36 (SF-36)) were performed prospectively after 1.5, 3, 6 and 12 months or until RTW. Primary interest was the comparison of the outcome scores with the time needed for RTW.
Results :
72 patients (52 years (22-64), 37 (51%) women) fulfilled the inclusion criteria. We distinguished “office-workers” (OW) (n = 49, 68%) from patients who worked at a physically demanding job (PW) (n = 23, 32%). Although time for RTW was fundamentally different (42 (OW) vs 118 days (PW), p<0.001), CMS (64.7 vs 64.1) and SF-36 (66.8 vs 69.9) at time of RTW were almost identical. At follow-up, CMS and SF-36 were always lower in the PW group.
Conclusion :
Jobs which require higher physical demands were likely to influence and to delay RTW. This study identifies cut off values for CMS and SF-36 at which a patient feels capable or willing to RTW after PHF. These values show the importance and impact of a patient’s occupation or demands on RTW. We were able to show, that besides age, sex and fracture, the type of occupation might alter the scores in postoperative outcomes.
Keywords: CMS, fracture, proximal humerus, return to work, SF-36, workers compensation.
INTRODUCTION
There are many different and well-known shoulder outcome measures that gauge pain and function. Researchers and clinicians, trying to classify the outcome after a certain operation, use these scores frequently. In recent literature, not only the degree of functional impairment of the affected joint or extremity, but also measures of general health and social implications have gained more interest. Newer questionnaires often combine subjective and objective components.
However, the goal of rehabilitating any injured patient should be functional independence and return-to-work (RTW). Insurance companies, which have gained much more influence in the health care system, are especially interested in a patient’s work-specific rehabilitation time, for which the company has to pay. By itself, the functional assessment is non-descriptive of these two goals.
If value is defined as patient outcomes in relation to healthcare costs, we need to collect information about both [1, 2]. In the future, orthopaedic and trauma surgeons might be evaluated and compensated by implementing value-based health care. Therefore, it is important to measure patient-centred and risk-adjusted patient specific outcomes. It is essential that the information is relevant to the patient’s condition and lifestyle, including the educational and cultural background of each patient [3].
The purpose of this study was to find out if there is a relation between subjective or objective outcome measures and the ability to RTW. It would be useful to be able to define a certain cut-off value for shoulder function, which allows RTW after a shoulder operation. A subjective self-reported level of function or well-being might be a better predictor for a patient’s reintegration into the working process after having injured a certain extremity.
It was the study’s aim to examine and compare two commonly used shoulder outcome measures (the SF-36 and the Constant-Murley Score [CMS]) with respect to the ability to return back to a former job. Additionally, we wondered if employees who still had limited range of motion were able to return earlier, if they did not have a physically challenging occupation.
PATIENTS AND METHODS
In a time period from March 2003 to June 2008, all isolated traumatic proximal humerus fractures (PHF), stabilized with the PHILOS® plate (Proximal Humeral Interlocking System;Depuy Synthes, Inc.; West Chester, PA, USA), were evaluated for this prospective observational single-centre study.
Since we were interested especially in the population of working people, we defined an age limit of 65 years. In Switzerland where the study was performed, there is a retirement benefit starting at the age of 65 years.
Exclusion criteria were the above-mentioned age limit, unemployment at time of injury, multiple injuries and pathologic fractures. Indication for operative treatment was based on fragment displacement as described by Neer [4]. Patients were asked to participate in routine follow-up including X-ray, a physical examination (CMS) and the completion of the SF-36 questionnaire at 1.5, 3, 6 and 12 months postoperatively or until RTW. The patient completed the SF-36 unaided. A study nurse checked for completeness.
The fracture type was documented with the use of the ATO/ASIF classification system [5].
All included patients were retrospectively grouped in either an “office-workers” group (OW) (such as language teacher, bank clerk, call centre agent, or computer scientist) or a “physically working” group (PW) (such as painter, blacksmith, road construction worker, or farmer).
None of the patients had an examination at the exact day of RTW. Thus, to get the most applicable cut-off values for that day, we only evaluated patients with examinations within 7 days before or after their RTW for this specific calculation. RTW was defined as the time in days until a patient was able to fully return back to his or her former occupation again.
SF-36
Quality of life was measured by using the German versionof the Medical Outcomes Study (MOS) 36-item Short Form (SF-36) [6]. Reliability and validity have been well documented by the developers of this instrument [6-10]. Calculation of the scores and the scoring checks were performed in accordance with the SF-36 Manual and Interpretation Guide [6].
Constant-Murley Score (CMS) [11]
A clinician performed the examination. For strength testing we used a mechanical dynamometer. The subjective component, relating to pain and activities of daily living, accounts for 35% of the total score. The remaining 65% is objective, assessing range of motion and power. Scores range from 0 to 100, with a high score indicating less pain and better function. Final scores were adapted to gender and age and classified from poor to very good, analogous to Neer [4] as described and proposed by Tingart [12]. A difference of 10 points was interpreted as clinically relevant [4, 12].
Operative Technique and Rehabilitation
The operative technique was standardized and followed the guidelines of the manufacturer of the implant (http://www.shoulderdoc.co.uk/documents/Philos.pdf). Beach-chair position, deltopectoral approach and general anaesthesia were performed exclusively. Pendulum exercises of the shoulder were initiated 7 days after the intervention. Free range of motion with elevation of more than 90° and strengthening was started after 1.5 months.
Statistical Analysis
All tests were computed by using the Student-T-test at a significance level of 5%, using SPSS (version 17.0, SPSS, Inc., Chicago, IL, USA). Continuous variables are presented as the mean and standard deviation. Comparison between different groups was performed with the use Student-T-test.
Source of Funding
No external funding was received in support of this study.
RESULTS
During the study’s period of time, 100 patients who were younger than 65 years were treated with a PHILOS® plate due to a PHF. All operations were performed within the first 10 days after injury.
A total of 28 (28%) patients did not meet the study criteria (25 retired before the age of 65 years or were unemployed, 3 patients had incomplete follow-up).
Finally, 72 patients fulfilled all the criteria of this study.
Eighteen (25%) had a second operation related to the primary one. There has been one revision due to an early hematoma, which had to be evacuated surgically. Bacterial infection was found and antibiotic treatment was started. The patient recovered well in follow-up.
Hardware removal due to subacromial impingement or by a patient’s request was performed in 17 (23%) mostly younger patients.
Median age was 52 years (22-64), 37 (51%) were women. The median follow-up was 270 days (73-471), while the mean time in hospital was 7 days (1-23 [one patient had additional soft tissue injuries, which required a longer hospital stay]).
The majority of patients worked in a sitting position (OW) (49, 68%), while 23 (32%) patients worked in a physically demanding job (PW) (Table 1). There was no significant difference (p > 0.05) concerning age, sex, type of fracture or length of hospital stay between the two groups (Table 2).
Table 1.
Occupation of the patients.
| OW-Group | n = | PW-Group | n = |
|---|---|---|---|
| Bank/Insurance clerk | 9 | Waitress/Waiter | 8 |
| Clerical assistant | 7 | Cook | 3 |
| Computer scientist | 7 | Elderly care nurse | 3 |
| Secretary | 6 | Service technician | 2 |
| Language teacher/Social worker | 5 | Kindergarten teacher | 2 |
| Salesperson | 4 | Blacksmith | 1 |
| Telephonist | 4 | Painter | 1 |
| Graphic designer | 3 | Physiotherapist | 1 |
| Engineer | 2 | Bike courier | 1 |
| Manager | 2 | Police-officer | 1 |
| Total: | 49 | Total: | 23 |
Table 2.
Demographics, absence of work and fracture type.
| Demographics | Absence of Work (d) | Fx-Type (OTA) | Fx-Type/RTW (d) | Total Follow-Up (d) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n= | fem. | male | age | mea. | med. | min. | max. | A | B | C | A | B | C | mea. | med. | min. | max. | |
| All | 72 | 37 | 35 | 52 | 72 | 47 | 4 | 240 | 13 | 27 | 32 | 58 | 53 | 89 | 270 | 277 | 76 | 431 |
| OW | 49 | 21 | 28 | 52 | 51 | 42 | 4 | 207 | 7 | 19 | 23 | 30 | 44 | 64 | 283 | 289 | 76 | 431 |
| PW | 23 | 16 | 7 | 52 | 117 | 118 | 18 | 240 | 6 | 8 | 9 | 118 | 73 | 146 | 238 | 191 | 85 | 398 |
| P = | n.s. | n.s. | n.s. | n.s. | <0.001 | - | - | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | - | - | |
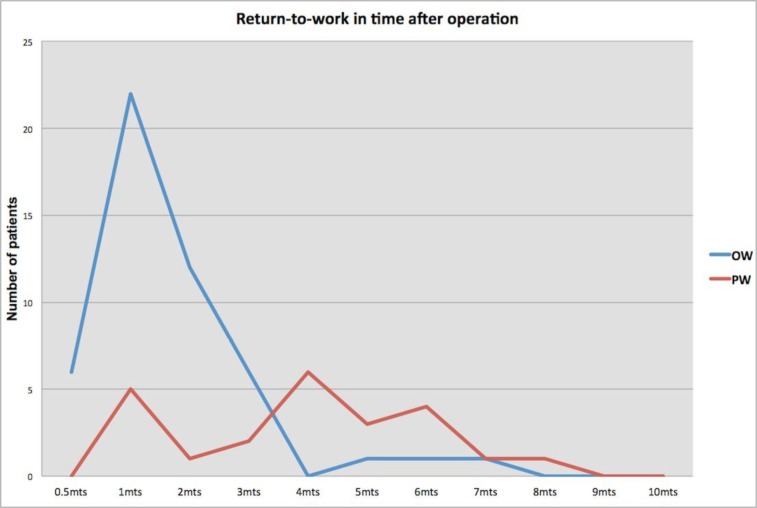
The mean time absent from work was 47 days (4-240) (Table 2). Overall, 48 patients (67%) returned back to unrestricted work during the first 3 months, 20 (28%) during the second 3 months, and only 4 (5%) patients needed more than 6 months for RTW. There was a significant difference in RTW between the OW group and the PW group. We found a mean RTW of 42 days (OW) vs 118 days (PW) in the two groups (p<0.001) (Table 3). While the majority of the OW group did RTW during the first month after operation, the RTW for the PW group peaked 4 months after the operation (Fig. 1).
Table 3.
CMS and SF-36 at return to work.
| d to Work | fu at RTW | fu at RTW | % fu at RTW | CMS | PCS | MCS | SF-36 | |
|---|---|---|---|---|---|---|---|---|
| OW | 70.5 | 66.7 d | n = 30 | 61 | 64.7 | 57.7 | 77 | 66.8 |
| PW | 109 | 106.7 d | n = 16 | 70 | 64.1 | 62.2 | 76.2 | 69.9 |
| p-value | <0.05 | <0.05 | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. |
Fu at RTW: Documenting the time when the follow-up examination prior to or after the RTW took place at our institution (including only the patients who had one 7 days prior to or after RTW).
%Fu at RTW: Showing how many patients actually had a follow-up examination 7 days prior to or after RTW. CMS, SF-36 and its compounds (PCS, MCS) at time of RTW.
Fig. (1).
RTW peaking 7 weeks after operation in the OW group, while the mean RTW of the PW group peaked 17 weeks after the injury.
Even though we saw all the patients (100%) in our outpatient clinic during follow-up and all were followed until RTW, there were only 46 of the 72 patients (64%) who completed a follow-up examination up to 7 days prior to or after RTW. These patients (30/49 OW, 16/23 PW) were analysed to calculate the score cut-off values at the time of RTW and they turned out to be almost identical (CMS: 64.7 vs 64.1 and SF-36: 66.8 vs 69.9, respectively [p>0.05]) (Table 3).
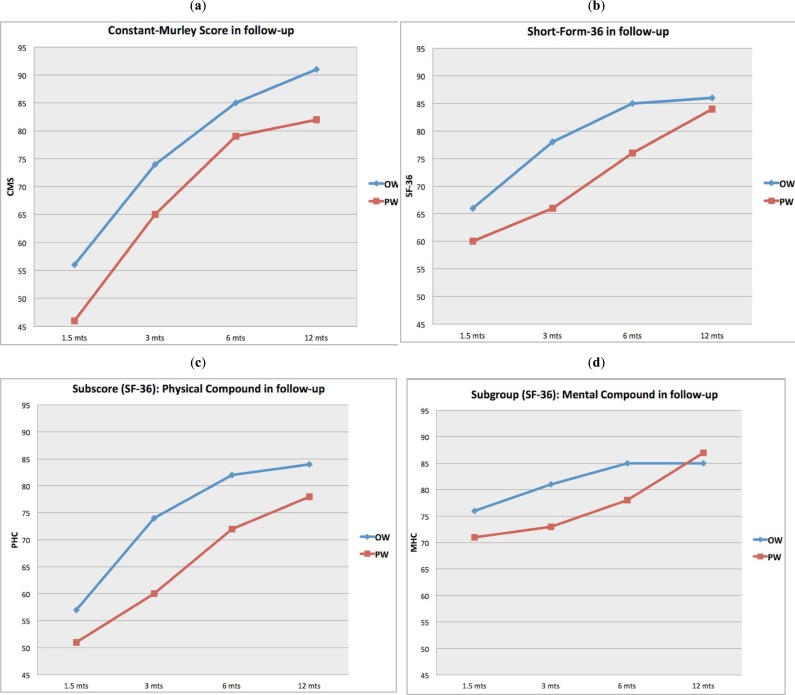
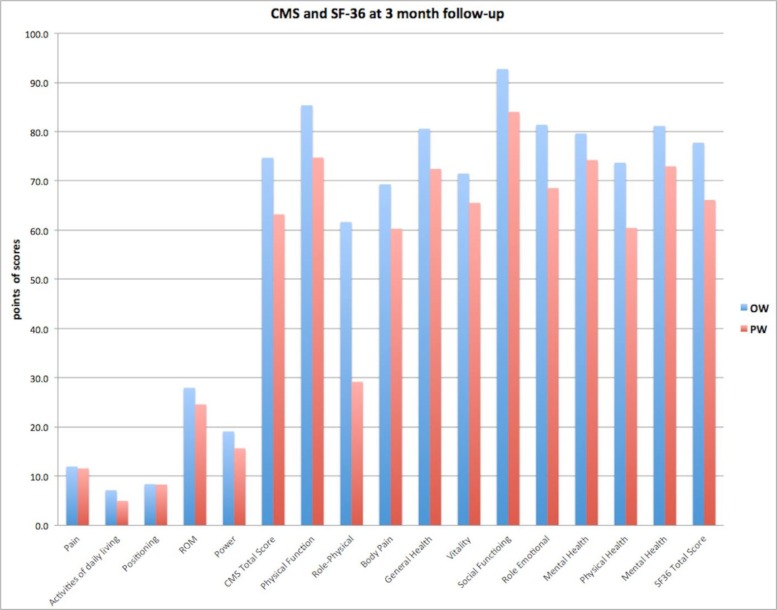
The values for the CMS and the SF-36 including its two subgroups of Physical Health (PH) and Mental Health (MH) are seen in Table 4 and demonstrated graphically in Fig. (2). At the 3 months follow-up there was a significant (p<0.05) difference in the scores of the CMS and the SF-36 in favor of the OW group (Table 4). Although not statistically significant throughout, all the scores were lower in the PW group after 3 months (Fig. 3).
Table 4.
CMS and SF-36 at each follow-up examination.
| 1.5 months | 3 months | 6 months | 12 months | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Score | CMS | PCS | MCS | SF36 | CMS | PCS | MCS | SF36 | CMS | PCS | MCS | SF36 | CMS | PCS | MCS | SF36 |
| OW | 56 | 57 | 76 | 66 | 74 | 74 | 81 | 78 | 85 | 82 | 85 | 85 | 91 | 84 | 85 | 86 |
| PW | 46 | 51 | 71 | 60 | 65 | 60 | 73 | 66 | 79 | 72 | 78 | 76 | 82 | 78 | 87 | 84 |
| p-value | n.s. | n.s. | n.s. | n.s. | 0.02 | 0.02 | n.s. | 0.02 | n.s. | 0.04 | n.s. | 0.04 | n.s. | n.s. | n.s. | n.s. |
CMS (Constant-Murley-Score), SF36 (Short Form 36) and its compounds: PCS and MCS (Physical Health and Mental Health).
Fig. (2).
The figures (a-d) show the scores (and its compounds) of the OW and PW during the different follow-up examinations after the shoulder operation.
Fig. (3).
Illustrating the compounds of CMS and SF-36 at the 3-month follow-up examination.
DISCUSSION
Fractures of the proximal humerus have a peak incidence in woman older than 50 years and in men between 30 and 50 years [13]. Considering these age-related incidences of PHF, men especially are prone to be absent from their work after such a trauma, which is an economic burden. This study included only patients with PHF who were working at the time of injury, with special attention to the time to RTW, including the function (CMS) and SF-36 scores needed to RTW. To our knowledge, this is the first study which points out these social-economic consequences for patients with PHF. It shows that the rate of full RTW after PHF is high, but the time to recovery varies widely, depending also on the physical requirements of someone’s job. Patients with physically demanding work needed longer to RTW. Furthermore, they had slower functional recovery and lower quality of life during follow-up. However, at the time of unrestricted RTW, both office workers and physical workers had the same CMS and SF-36 scores, which identifies a cut-off value of these scores for the ability to return to any kind of work in our study.
Concerning RTW of patients after a PHF, the literature is insufficient. Hanson et al. [14] included 42 labourers in their study on patients with conservatively treated PHFs. All except one of them did RTW from 2 to 4months after injury. They found no difference in sick leave between manual and non-manual workers. Their overall findings are comparable to our OW group, which is quite interesting as it suggests advantages to the non-operative treatment of manual workers (comparable to our PW group) with PHFs. However, the RTW was not the primary endpoint of their study and their inclusion criteria differed from this study; thus, they can’t be fully compared. There are various prognostic factors without consensus concerning RTW after traumatic injuries in the literature and there is increasing evidence that RTW may be predicted by some variables such as education, gender, blue-collar type of work, injury severity, number of surgical procedures, and self-efficacy [15, 16]. Furthermore isolated upper extremity injuries are more likely to RTW early [17]. It appears that psychosocial factors are of primary importance. However, the current study shows that RTW is basically dependent on the type of job rather than on other criteria (sex, age, fracture type). The outcome that the OW group did RTW earlier is understandable and seems reasonable. However, the explicit lower CMS and SF-36 of the PW group is not explained satisfactorily and might be related to a lower psychosocial status of these patients. Especially at the 3 month follow-up, when most of the patients in the OW group had already returned to their jobs for almost 1.5 months, all scores and subscores were significantly lower in the PW group. The well-known phenomenon of “workers’ compensation” might also be part of the explanation for this. A potential association between psychosocial and secondary gain factors may be hypothesized. While the OW group usually is better educated and has more intellectually demanding work, which is normally better paid and has an elevated social prestige and status, the physically demanding jobs are monotonous, less well-paid and of course more physically demanding and exhausting. As described by McKee and Yoo [15] and Frank Henn III [18], we also found that patients in the blue-collar-worker group had lower postoperative SF-36-scores as compared with those in the white-collar-worker group [16, 17]. Patients claiming workers compensation do RTW later than others or have lower SF-36 scores [15, 18]. As mentioned before, we also found that the functional status was significantly lower for the Workers’ Compensation group as assessed with the CMS and its subgroups. Morse et al. [19] showed that these persons were also found to have more difficulty in completing activities of daily living such as bathing, tooth brushing and caring for a child. A meta-analysis of 129 studies performed by Harris et al. [20] found a significant association between compensation status and outcome after surgery in shoulder and spine surgery.
In our opinion, the positive effect of RTW influences the rehabilitation mentally and therefore also physically, which could be another explanation of the faster recovery and better scores of the OW group. This accords well with Hou et al. [21], who showed that RTW has a positive and independent influence on health-related quality of life. There is a growing realization that patients, not surgeons, define whether an orthopaedic procedure is successful and whether to seek additional treatment [22, 23]. It is important that patients and surgeons share an understanding of what defines “success”. Patients are initially concerned with symptom relief, but their long-term expectations include returning to symptom-free function, especially in terms of activities that are personally important [3].
Interestingly, we documented almost identical scores for the two groups at the time of RTW. There seems to be a “range” at around 65 points in CMS or 70 points in SF-36 where patients are capable or willing to RTW. Considering the economic and social implications of such injuries, it is imperative that these patients are able to RTW within a reasonable time, with the goal of returning to pre-injury levels of activity. Orthopaedic surgeons treating patients in this challenging population should be aware of these findings to better inform patients of their recovery expectations. There is a need for greater attention to the process of informing patients of the outcomes for certain orthopaedic procedures, so that patients and providers may achieve greater alignment of expectations and increased acceptance of both the benefits and limitations of alternative treatments [3].
There are certain limitations in this study which must be mentioned. For the comparison of the scores and the exact time of RTW, we had to do an approximation, as none of the patient had the examination on exactly that day. Thus we only included patients with scores in a range of 7 days before and after the RTW, which made the number of patients for this calculation small, but still gives an idea of the cut-off values for RTW. Second, we only differentiated by office jobs and physically demanding jobs and only counted RTW as a positive event when a patient was able to fully return back to his or her former occupation again. The financial reimbursement and the exact type of job could not be taken into account.
Third, the orthopaedic surgeon may withhold the release to return to work longer when a patient says that the job requires heavy manual lifting and might therefore influence RTW by his behaviour rather than the patient’s preference.
CONCLUSION
The number of lost working days and lost productivity associated with a PHF is high. Jobs which require higher physical demands were likely to influence and to delay RTW. Independent of one’s type of work, there seems to be a cut-off score level reflected by the CMS and SF-36 values at which a patient feels capable of and willing to RTW after uncomplicated angular stable Osteosynthesis of a PHF. Besides the well-described confounding factors of age, sex and fracture type, these results show the importance and the impact of a patient’s occupation or demands. We were able to show that the type of occupation might alter the scores for postoperative outcome and must be kept in mind.
ACKNOWLEDGEMENTS
The authors, their immediate family, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ETHICS
The institutional review board and the local ethical committee approved the study protocol, EK: STZ 24/06. Informed consent, which included surgical treatment and follow-up examinations, was obtained from each patient.
REFERENCES
- 1.Andrawis JP, Chenok KE, Bozic KJ. Health policy implications of outcome smeasurement in orthopaedics. Clin Orthop Relat Res. 2013;471(11): 3475–81. doi: 10.1007/s11999-013-3014-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Porter ME. What is value in health care?. N Engl J Med. 2010;363: 2477–81. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 3.Noble PC, Fuller-Lafreniere S, Meftah M , et al. Challenges in outcome measurement discrepancies between patient and provider definitions of success. Clin Orthop Relat Res. 2013;471(11): 3437–45. doi: 10.1007/s11999-013-3198-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neer CS 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6): 1077–89. [PubMed] [Google Scholar]
- 5.Marsh JL, Slongo TF, Agel J , et al. Fracture and dislocation classification compendium - 2007,: orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma. 2007;21(Suppl 10 ): S1–163. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 6.Ware JE ., Jr SF-36 Health Survey manual and interpretation guide. Boston The health Institute New England Medical Centre 1993. [Google Scholar]
- 7.Hopman WM, Towheed T, Anastassiades T , et al. Canadian normative data for the SF-36 health survey.Canadian Multicentre Osteoporosis Study Research Group. CMAJ. 2000;163(3): 265–71. [PMC free article] [PubMed] [Google Scholar]
- 8.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3): 247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Ware JE Jr, editor. 2nd ed. Philadelphia: Lippincott-Raven Publishers.; 1996. SF-36 Health Survey.In Siker Quality of life and pharmaco-economics in clinical trials. pp. 337–47. [Google Scholar]
- 10.Ware JE Jr Sherbourne, CD.; The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6): 473–83. [PubMed] [Google Scholar]
- 11.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214): 160–4. [PubMed] [Google Scholar]
- 12.Tingart M, Bäthis H, Lefering R , et al. Constant Score and Neer Score. A comparison of score results and subjective patient satisfaction. Unfallchirurg. 2001;104(11): 1048–54. doi: 10.1007/s001130170019. [DOI] [PubMed] [Google Scholar]
- 13.Rose SH, Melton LJ, Morrey BF , et al. Epidemiologic features of humeral fractures. Clin Orthop Related Res. 1982;(168): 24–30. [PubMed] [Google Scholar]
- 14.Hanson B, Neidenbach P, de Boer P , et al. Functional outcomes after nonoperative management of fractures of the proximal humerus. J Shoulder Elbow Surg. 2009;18(4): 612–21. doi: 10.1016/j.jse.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 15.McKee MD, Yoo DJ. The effect of surgery for rotator cuff disease on general health status. Results of a prospective trial. J Bone Joint Surg Am. 2000;82: 970–9. doi: 10.2106/00004623-200007000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Clay FJ, Newstead SV, McClure RJ. A systematic review of early prognostic factors for return to work following acute orthopaedic trauma. Injury. 2010;41(8): 787–803. doi: 10.1016/j.injury.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 17.Clay FJ, Newstead SV, Watson WL , et al. Determinants of return to work following non life threatening acute orthopaedic trauma a prospective cohort study. J Rehabil Med. 2010;42(2): 162–9. doi: 10.2340/16501977-0495. [DOI] [PubMed] [Google Scholar]
- 18.Henn RF, 3rd, Kang L, Tashjian RZ , et al. ARTICLE TITLE. J Bone Joint Surg Am. 2008;90(10): 2105–13. doi: 10.2106/JBJS.F.00260. [DOI] [PubMed] [Google Scholar]
- 19.Keogh JP, Newayhid I, Gordon JL , et al. The impact of occupational injury of injured worker and family Outcomes of upper extremity cumulative trauma disorders in Maryland workers. Am J INd Med. 2000;38(5): 498–506. doi: 10.1002/1097-0274(200011)38:5<498::aid-ajim2>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 20.Harris I, Mulford J, Solomon M , et al. Association between compensation status and outcome after surgery a meta analysis. JAMA. 2005;293: 1644–52. doi: 10.1001/jama.293.13.1644. [DOI] [PubMed] [Google Scholar]
- 21.Hou WH, Liang HW, Sheu CF , et al. Return to work and quality of life in workers with traumatic limb injuries a 2-year repeated-measurements study. Arch Phys Med Rehabil. 2013;94(4): 703–10. doi: 10.1016/j.apmr.2012.10.033. [DOI] [PubMed] [Google Scholar]
- 22.Bayley KB, London MR, Grunkemeier GL , et al. Measuring the success of treatment in patient terms. Med Care. 1995;33(4 Suppl): AS226–35. [PubMed] [Google Scholar]
- 23.Brokelman RB, van Loon CJ, Rijnberg WJ. Patient versus surgeon satisfaction after total hip arthroplasty. J Bone Joint Surg Br. 2003;85(4): 495–8. [PubMed] [Google Scholar]