Abstract
A large body of research has been produced in recent years investigating posttraumatic stress disorder (PTSD) among military personnel following deployment to Iraq and Afghanistan, resulting in apparent differences in PTSD prevalence. We compare prevalence estimates for current PTSD between military subgroups, providing insight into how groups may be differentially affected by deployment. Systematic literature searches using the terms PTSD, stress disorder, and acute stress, combined with terms relating to military personnel, identified 49 relevant papers. Studies with a sample size of less than 100 and studies based on data for treatment seeking or injured populations were excluded. Studies were categorized according to theatre of deployment (Iraq or Afghanistan), combat and noncombat deployed samples, sex, enlistment type (regular or reserve and [or] National Guard), and service branch (for example, army, navy, and air force). Meta-analysis was used to assess PTSD prevalence across subgroups. There was large variability in PTSD prevalence between studies, but, regardless of heterogeneity, prevalence rates of PTSD were higher among studies of Iraq-deployed personnel (12.9%; 95% CI 11.3% to 14.4%), compared with personnel deployed to Afghanistan (7.1%; 95% CI 4.6% to 9.6%), combat deployed personnel, and personnel serving in the Canadian, US, or UK army or the navy or marines (12.4%; 95% CI 10.9% to 13.4%), compared with the other services (4.9%; 95% CI 1.4% to 8.4%). Contrary to findings from within-study comparisons, we did not find a difference in PTSD prevalence for regular active-duty and reserve or National Guard personnel. Categorizing studies according to deployment location and branch of service identified differences among subgroups that provide further support for factors underlying the development of PTSD.
Keywords: military subgroups, posttraumatic stress disorder, armed forces, meta-analysis, deployment, prevalence, systematic review
Abstract
Un vaste ensemble d’études ont été produites ces dernières années sur le trouble de stress post-traumatique (TSPT) au sein du personnel militaire suite au déploiement en Irak et en Afghanistan, et il en a résulté des différences apparentes de prévalence du TSPT. Nous comparons les estimations de prévalence du TSPT actuel entre les sous-groupes militaires, en tentant d’expliquer comment les groupes peuvent être affectés différemment par le déploiement. Des recherches systématiques de la littérature à l’aide des termes TSPT, trouble de stress, et stress aigu combinés à des termes relatifs au personnel militaire ont relevé 49 articles pertinents. Les études dont la taille d’échantillon était de moins de 100 ou qui étaient basées sur des données de recherche de traitement ou de populations blessées ont été exclues. Les études ont été catégorisées selon le théâtre du déploiement (Irak ou Afghanistan), les échantillons déployés de combat ou de non-combat, le sexe, le type d’enrôlement (régulier ou réserve, et [ou] Garde nationale) et branche de service (par exemple, armée, marine, et force aérienne). Une méta-analyse a servi à évaluer la prévalence du TSPT dans les sous-groupes. Il y avait une grande variabilité de la prévalence du TSPT entre les études, mais, sans égard à l’hétérogénéité, les taux de prévalence du TSPT étaient plus élevés dans les études du personnel déployé en Irak (12,9 %; IC à 95 % 11,3 % à 14,4 %), comparé au personnel déployé en Afghanistan (7,1 %; IC à 95 % 4,6 % à 9,6 %), au personnel de combat déployé, et au personnel servant dans l’armée canadienne, américaine ou britannique, ou servant dans la marine ou l’infanterie de marine (12,4 %; IC à 95 % 10,9 % à 13,4 %), et comparé aux autres services (4,9 %; IC à 95 % 1,4 % à 8,4 %). Contrairement aux conclusions tirées des comparaisons à l’intérieur d’une étude, nous n’avons pas trouvé de différence de prévalence du TSPT chez le personnel de service actif et de réserve ou de la Garde nationale. La catégorisation des études selon l’endroit de déploiement et la branche de service a identifié les différences parmi les sous-groupes qui apportent plus d’appui aux facteurs sous-jacents du développement du TSPT.
Posttraumatic stress disorder among military personnel is an issue that receives a large amount of media attention.1 It has a significant impact on the functioning and lives of people with this condition.2 Although recognition of the psychological impact of war dates back at least to the First World War,3 there is little doubt that the introduction of the term PTSD into DSM-III in 1980 changed views, largely because of the change in the etiological importance given to immediate trauma, compared with longer-term predisposition.4 The result was that, after some initial skepticism,4 the new label and formulation gained widespread acceptance.
The increase in rates of PTSD immediately after deployment5 and later, perhaps via the emergence of delayed-onset PTSD,6 is now a growing health concern and interest. The long international military operations in Iraq and Afghanistan have been of a very different nature to the short 1991 Gulf War or the United Nations peacekeeping missions that many militaries were involved in during the past 20 years, and personnel have been increasingly exposed to injury and mortality from improvised explosive devices.
Estimates of PTSD prevalence from conflicts before 1985 are, by necessity, drawn from retrospective samples, and can vary widely owing to recall bias—epidemiologic studies of Vietnam veterans have reported a wide range of current and lifetime prevalences,7 leading to debate around the true PTSD prevalence among military personnel. In contrast, recent operations in Iraq and Afghanistan have allowed for PTSD measurement while operations are ongoing and shortly after personnel have returned from deployment.8 However, the prevalence of PTSD has still been found to differ across different militaries, ranging from 4% to 17% for those in the United States returning from the Iraq War and from 3% to 6% for those returning in the United Kingdom.9,10 Prevalences in other countries of the world are less well documented.
Current PTSD prevalence is affected by many factors. The likelihood of developing PTSD is greater for people in combat roles and has been found to almost double in some studies.11 Personnel in the reserve forces have also been found to have worse health outcomes following deployment, compared with those in the regular forces.10 Among the general population, females are seen to be at increased risk of PTSD.12 However, studies of military samples have shown that women are less likely or at similar risk to men for developing PTSD.12,13 The different proportions of regular, reservist, combat-exposed, and female personnel within military populations may affect PTSD prevalence estimates.
Highlights
PTSD is an important issue across military subpopulations.
Personnel in a combat role have the highest prevalence of probable PTSD.
Numerous reviews have been produced investigating PTSD following the Iraq and Afghanistan wars11,14,15; however, to date, none has assessed differences in PTSD prevalence among different subgroups of the military population. Our review aims to assess how prevalences differ among theatre of deployment, combat deployment, sex, enlistment status, and service, providing insight into how deployment may be differentially affecting these subgroups. This will be useful for informing health care provision and understanding of the factors underlying the development of PTSD within the military population, and has the potential to better inform discussion around the differing rates of current PTSD since 2001.
Methods
Systematic Literature Search
To determine the prevalence of PTSD in subpopulations of military personnel who were deployed to either Iraq or Afghanistan, literature was searched using the Ovid, MEDLINE, and PubMed databases on May 14, 2012.
The search terms PTSD, stress disorder, and acute stress were used to systematically identify the abstracts of papers relating to the outcome of interest, and were combined with terms relating to military personnel to identify the maximum number of studies on PTSD with a military sample. Search terms were combined with Boolean operators: combat or military personnel or troops or soldiers or armed forces or service personnel or peacekeepers or army or navy or marines or air force or special forces; and PTSD or stress disorder or acute stress. Prevalence and incidence were not included in the search terms to avoid excluding papers that reported prevalence but did not have this as a main focus. The search was limited to words that appeared in the abstracts of papers and excluded book chapters and previous reviews, but did include conference abstracts.
Eligible Papers
Initial searches resulted in 1818 potentially relevant studies. Papers were excluded if they did not assess PTSD prevalence, if they did not report on military samples deployed to Iraq and (or) Afghanistan, if they reported the prevalence rate of PTSD only when comorbid with another health problem, including traumatic brain injury (if PTSD prevalence in a population was reported separately from comorbidity prevalence the paper was still included), if they reported on a treatment sample or used a case–control sample, as these would not have given an estimate of prevalence in whole population, if they focused exclusively upon a specific age group (for example, retired personnel), or if they were not reported in English.
From this, 342 papers were identified that potentially reported the prevalence of PTSD following deployment to Iraq and (or) Afghanistan. A further triage removed papers focusing on a medical service sample, those that reported exclusively on married personnel, and (or) personnel with children, and any papers with a sample size of less than 100 (in an attempt to decrease heterogeneity between the studies). From papers reporting multiple results from the same sample, only one paper was selected for inclusion to avoid reporting from overlapping samples. This resulted in 49 papers eligible for review (see online eFigure 1 for a flow chart showing paper inclusion numbers).
Papers were rated and quality ratings were agreed on by 2 researchers based on criteria including type of study, sample selection method, sample size, and aims of the study (see online eTable 1 for full criteria). Papers that scored above 11 points on these criteria were rated as very high. High-quality papers scored between 9 and 11, moderate papers scored between 6 and 8, and papers were rated as poor if they scored under 6. Among the 49 papers included in the analysis, 1 paper was rated as very high quality, 17 were rated as high quality, 29 were rated as moderate quality, and 2 papers were rated as poor quality. Full quality ratings are included in online eTable 1. Quality ratings are provided for information only as all papers were kept in the analysis regardless of quality. Previous studies have found that study type makes little difference to analysis.16
Methods of Measurement Within Papers
There was variety among the papers in the measures used to determine PTSD. As most of the measures used were self-report with no clinical diagnosis of PTSD, we have used the term probable PTSD throughout the paper. Among the papers in the analysis, 31 (63%) used the PTSD Checklist self-report measure of PTSD symptoms,17 9 (18%) used the Primary Care-PTSD measure (PC-PTSD), which is used in primary care for identifying PTSD symptoms, 2 (4%) used the PTSD Symptom Scale, which is derived from the DSM-III-R criteria for PTSD,18 3 (6%) used the International Statistical Classification of Diseases and Related Health Problems, Ninth Revision, criteria for PTSD, 1 (2%) used the Screen for Post-Traumatic Stress Symptoms, which uses DSM-IV criteria, and 1 (2%) used the Self-Rating Inventory for PTSD, which also used DSM-IV criteria to diagnose probable PTSD.19
Data Analyses
For all studies, the sample size and prevalence of current probable PTSD were extracted and the standard error of the prevalence was calculated. If the denominator was not provided, the prevalence and the numerator were used to estimate the standard error. To analyze the probable PTSD case prevalence for subpopulations, the prevalence of probable PTSD cases was assessed across studies, and subgroup analysis was used to identify how this varied across subpopulations. Forest plots were generated in STATA 11 (StataCorp, College Station TX, 2009) with the metan command. Random effects models were fitted to account for residual heterogeneity not explained by the stratification. Chi-square test for heterogeneity is reported together with tau and I2, which is an estimate of the variability in results across studies that can be attributed to heterogeneity, rather than chance.20 I2 ranges between 0% and 100%, and suggested benchmarks that characterize less than 25% as low, 25% to 50% as modest, and more than 50% as high heterogeneity. All tests were 2-sided and the P value was set at 0.05
Results
Theatre of Deployment
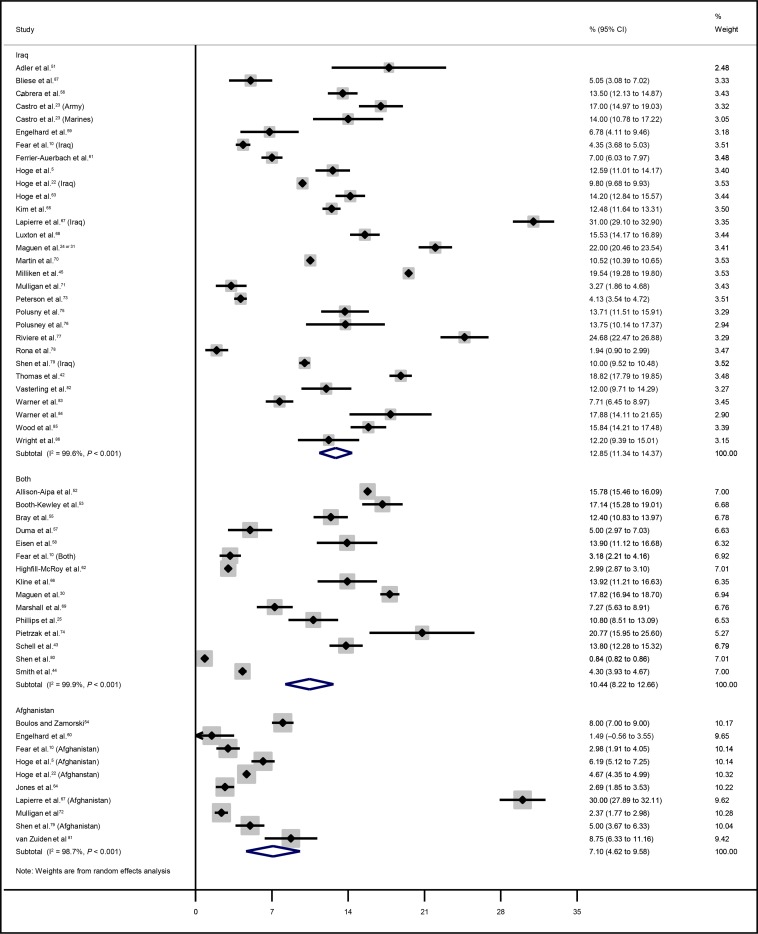
Most studies (that is, 30 of them) reported the prevalence of probable PTSD cases from samples that had deployed to Iraq, 10 studies reported the prevalence on samples that had deployed to Afghanistan, and 15 studies reported the prevalence on samples that had deployed to both Iraq and Afghanistan (online eTable 1). There was overlap in prevalence of probable PTSD cases between samples deployed to Iraq and Afghanistan, but studies of samples deployed to Afghanistan tended to report a lower prevalence, compared with studies of samples deployed to Iraq. The pooled estimate for Afghanistan samples was 7.1%, with a 95% confidence interval of 4.8% to 9.6%. Iraq-deployed samples had a pooled estimate of 12.9% (95% CI 11.3% to 14.4%), and samples deployed to both Iraq and Afghanistan had a pooled estimate of 10.4% (95% CI 8.2% to 12.7%). There was significant heterogeneity in all 3 subgroups (Iraq χ2 = 7142.2, df = 29, P < 0.001; Afghanistan χ2 = 710.2, df = 9, P < 0.001; both χ2 = 12526.4, df = 14, P < 0.001) and every I2 was greater than 95% (Figure 2).
Figure 2.
Prevalence of posttraumatic stress disorder stratified by theatre of deployment (Iraq, Afghanistan, or both)
Combat Deployment
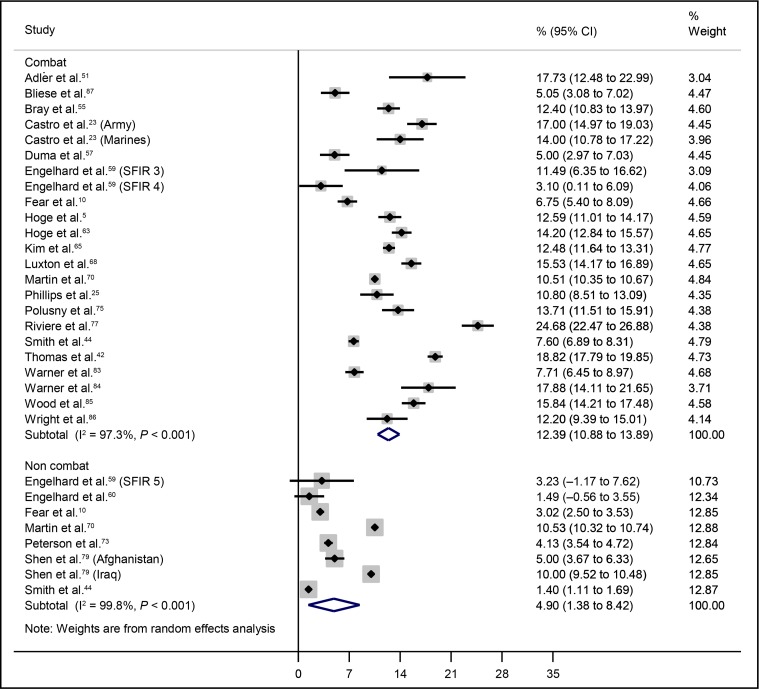
Studies were stratified by combat role; combat deployed samples, which included samples of infantry brigade combat teams and those who held a combat role on deployment, and noncombat deployed (Figure 3). There were 21 studies included that were either based on samples of infantry brigade combat teams or reported the probable PTSD case prevalence for those who had a combat role on deployment. The pooled estimate for these studies was 12.4% (95% CI 10.9% to 13.9%). Eight studies reported the probable PTSD case prevalence for personnel in support roles; there was some overlap in prevalence with combat deployed samples, although the prevalence for noncombat deployed samples tended to be much lower, with a pooled estimate of 4.9% (95% CI 1.4% to 8.4%). Heterogeneity in both subgroups was significant (combat χ2 = 821.6, df = 22, P < 0.001; noncombat χ2 = 3039.9, df = 7, P < 0.001), and the variability in prevalence estimates was largely due to heterogeneity (I2 < 95%).
Figure 3.
Prevalence of posttraumatic stress disorder stratified by combat deployment
Sex
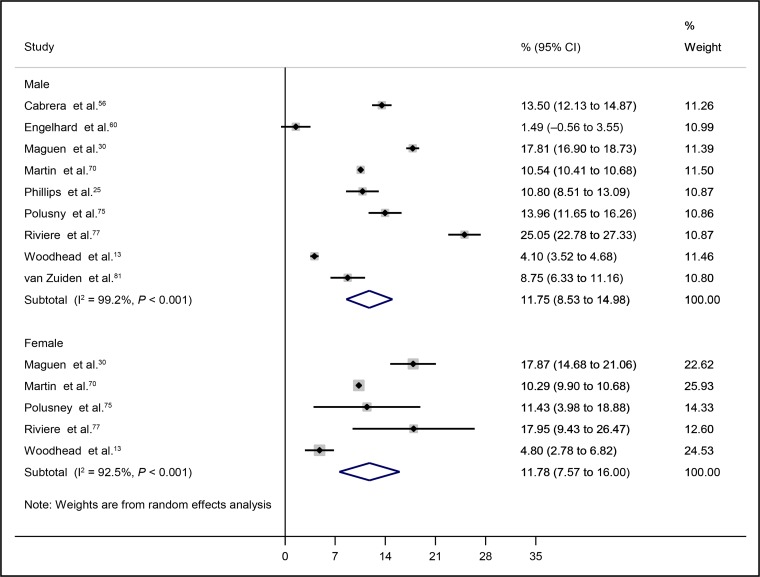
Most studies included in the review sampled both men and women deployed to Iraq and Afghanistan and did not report probable PTSD prevalence separately by sex. Four studies were based on samples of male personnel and 5 studies reported probable PTSD prevalence separately for men and women (Figure 4). There was no indication that prevalence of probable PTSD differed by sex. The rates had a pooled estimate of 11.8% (95% CI 8.5% to 15.0%) for the male samples and a pooled estimate of 11.8% (95% CI 7.6% to 16.0%) for female samples. Heterogeneity was again significant for both men (χ2 = 977.4, df = 8, P < 0.001; I2 = 99.2%) and women (χ2 = 53.2, df = 4, P < 0.001; I2 = 92.5%).
Figure 4.
Prevalence of posttraumatic stress disorder stratified by sex
Enlistment Status
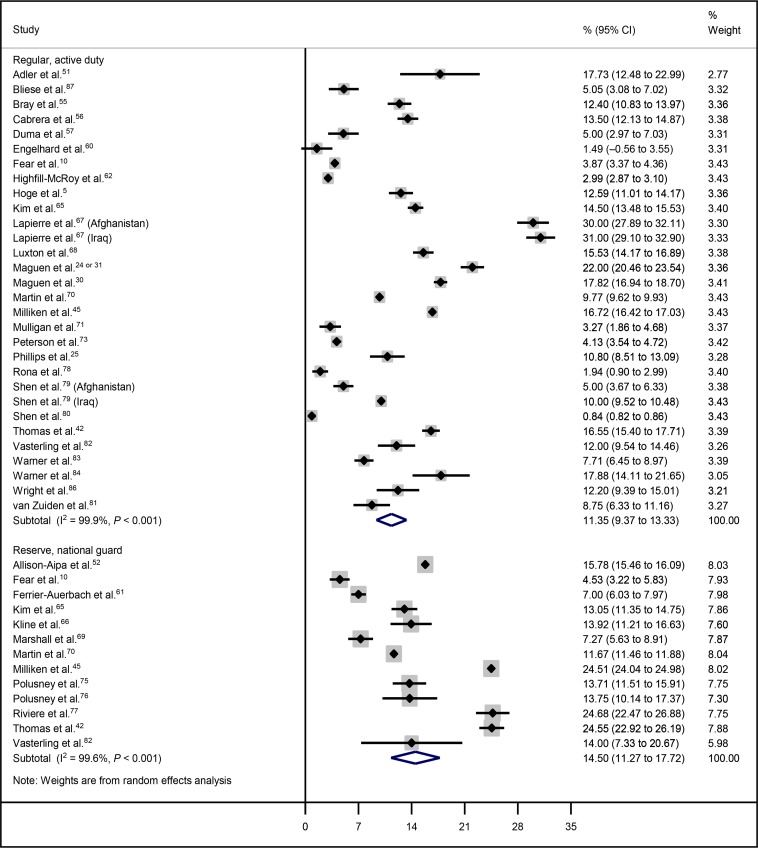
The prevalence of probable PTSD among the regular and (or) active-duty sample had a pooled estimate of 11.4% (95% CI 9.4% to 13.3%) (Figure 5). The prevalence was slightly higher in the reserve and (or) National Guard samples, with a pooled estimate of 14.5% (95% CI 11.3% to 17.7%). Heterogeneity was significant in both subgroups (regular–active-duty χ2 = 31122.8, df = 29, P < 0.001; reserves–National Guard χ2 = 3201.7, df = 12, P < 0.001; and I2 were all greater than 95%).
Figure 5.
Prevalence of posttraumatic stress disorder stratified by enlistment status
Service
Most studies of PTSD among military personnel deployed to Iraq and Afghanistan have focused on the army, and studies that are, in general, representative of the armed forces as a whole generally do not report the PTSD prevalence separately by service. Stratifying prevalence rates of probable PTSD by service showed that rates tended to be higher for personnel in the army and marines and lower in the navy and the air force (Figure 6). The prevalence for army samples varied, but had a pooled estimate of 13.2% (95% CI 10.9% to 15.5%). A slightly lower prevalence is found in samples of marines, with a pooled estimate of 10.4% (95% CI 7.7% to 13.1%). Based on the studies included in this review, the navy tends to have a lower prevalence of probable PTSD, compared with the army, with a pooled estimate of 7.3% (95% CI 5.2% to 9.5%). Four studies reported probable PTSD prevalence separately for the air force, and it had the lowest prevalence, with a pooled estimate of 2.6% (95% CI 1.6% to 3.4%). There was significant heterogeneity in all subgroups (army χ2 = 17 548.5, df = 36, P < 0.001; marines χ2 = 1905.3, df = 7, P < 0.001; navy χ2 = 1267.6, df = 10, P < 0.001; air force χ2 = 85.4, df = 3, P < 0.001) and the variation in estimates within subgroups was largely attributable to heterogeneity (all I2 were greater than 99%).
Figure 6.
Prevalence of posttraumatic stress disorder stratified by service
Discussion
The wars in Iraq and Afghanistan have renewed attention to the mental health effects of deployment, including PTSD, and, as a result, there is a large amount of research on the prevalence of PTSD in service personnel who were deployed to these countries.14,21 Our review contributes new knowledge through examining prevalence of probable PTSD cases in military subgroups. Based on studies that have reported probable PTSD case prevalence separately for personnel deployed to Iraq and Afghanistan, we found support for higher rates of probable PTSD among the Iraq-deployed samples, compared with samples of Afghanistan-deployed personnel. This is likely a reflection of studies carried out during the early stages of the Afghanistan war when combat operations were of relatively low intensity.5,22 As the military operations in Afghanistan have continued, this difference has been reduced, and recent studies have found similar prevalence rates of probable PTSD between personnel deployed to Iraq and Afghanistan.10 Further, as the engagements in Iraq and Afghanistan have continued up to 2010, many military personnel have been deployed to both theatres, making it difficult to classify samples by individual theatre.
The association between combat exposure and PTSD is well established in the literature, and studies have generally found that personnel who deploy in a combat role or have combat exposure are at higher risk of PTSD.10,23–29 A review of the association between combat units in Iraq and Afghanistan and PTSD provides a detailed summary of PTSD prevalence categorized by combat groups and method of assessment.11 They reported weighted prevalence of 13% among operational infantry units and 6% in population samples. We found similar estimates in probable PTSD prevalence in our comparison between people who reported having deployed in a combat role or were sampled from infantry brigade combat units (12%) and those who reported having deployed in a noncombat role (5%).
The number of women in the military has increased during the last few decades, and, concurrently, the roles of women on deployment have expanded; as a consequence, women are experiencing higher rates of war zone exposures.13,30 Comparatively little research has focused on PTSD in women deployed to Iraq and Afghanistan. In our analysis, there was no significant difference between men (12%) and women (12%). Research of men and women deployed to Iraq and Afghanistan shows mixed results, and some studies have suggested this may be due to role distribution, but this finding is not universal.13,30–34 Recent research has also suggested that men and women can experience different stressors on deployment.35 Studies that have looked at PTSD by sex have found higher prevalence of PTSD and greater perceived need for mental health care among nondeployed women, compared with men.36,37 Two studies38,39 that have looked at the interaction between sex and combat exposure for PTSD have found that women with high levels of exposure were at higher risk of PTSD, compared with men at the same level of exposure. Women have been shown to experience the same PTSD rate as men, even when the level of trauma exposure is similar,13 but these results may be affected by women not having a combat role. However, the lack of sex difference fits with research that has been carried out on sex differences in mental health prevalence in the general population, which has shown that some of these differences disappear when controlling for occupation.40
Most Western militaries have seen their reserve forces increasingly supplement the regular forces in operations abroad. Research has shown that there are several differences between the reserve and regular forces, both in the context of their deployments and in their experiences after coming back home.41,42 Concerns have been raised about the mental health risks of deployment for reserve personnel, and studies have found that rates of PTSD are higher among reserve and National Guard personnel, compared with regular active-duty personnel who were deployed to Iraq and Afghanistan.41,43,44 Recent US research has also found that rates of PTSD among reserve and National Guard personnel increase significantly during the year after their return from deployment, above the increases that have been found in regular personnel.42,45 UK research has found that, although deployment to Iraq and Afghanistan is associated with PTSD in reserve personnel, prevalence rates of PTSD are similar between regular and reserve personnel deployed to the later operations in Iraq and Afghanistan.10 UK reserves continue to experience difficulties with the transition from military deployment to civilian life, including being more likely than regular personnel to feel unsupported by the military and to have difficulties with social functioning in the postdeployment period.46 Despite these differences found within studies, we did not find a significant difference in the prevalence of probable PTSD between regular (11%) and reserve or National Guard (15%) personnel deployed to Iraq and Afghanistan.
Both UK and US studies of PTSD have found increased risk in army personnel deployed to Iraq and Afghanistan.43,47–49 Several US studies have also found higher prevalence of PTSD in marines deployed to Iraq and Afghanistan.41–43 A US study found that combat exposure and trauma history varied by service, with higher levels of exposure among army, marines, and National Guard personnel, compared with navy personnel.49 In contrast, UK research has shown that prevalence rates of PTSD are lower among Royal Marine, compared with Army, personnel deployed to Iraq.50 In this review, we found that army (13%) and marine personnel (10%) had the highest prevalence of probable PTSD cases, although these 2 groups also had the broadest range in prevalence, in particular the army (between 2% and 31%). They were followed by the navy (7%), which had a lower pooled prevalence compared to the army, and finally the air force (3%), which had a lower pooled prevalence, compared with all 3 of the other services.
Limitations
Our review aimed to compare probable PTSD case prevalence after deployments to Iraq and Afghanistan. However, as an increasing proportion of personnel have deployed on multiple occasions and to both theatres, there is likely to be some overlap. Therefore, it is not possible to draw a clear-cut conclusion regarding differences in prevalence of probable PTSD between deployments to Iraq and Afghanistan.
A second limitation is that we were unable to include papers published in a language other than English. However, this only excluded a small number of papers (17 out of 1818). Third, it was necessary to include papers with both population samples and convenience samples in the evidence base to improve the power of the analysis. Fourth, most of the included papers focused on US military samples. The length of a single deployment is usually longer in the US military than for other allied forces, which may affect prevalence. Fifth, we were unable to control for other covariates in stratified analysis.
Finally, only 4 studies reported the probable PTSD prevalence separately for air force personnel, limiting the conclusions that can be drawn regarding the prevalence of probable PTSD in this service.
Note, there was significant heterogeneity in all the subgroup analyses, and the I2 statistics indicate that the proportion of variation in the pooled estimate attributable to heterogeneity was large. We were unable to account for multiple subgroups in our analyses, and other sources of heterogeneity include country, which we were not able to assess, owing to small numbers of non-US studies, year of study, variability in the use of an assessment tool, the time of postdeployment assessment, and other factors that may have spuriously increased heterogeneity. There were numerous methodological differences between studies regarding the length of time for which symptoms were required to have occurred before a participant was considered a case, owing to various measures used to assess PTSD. High heterogeneity is an often unavoidable cause for caution in the interpretation of results, and should be kept in mind when considering the results of this meta-analysis.
In addition to differences between samples of combat- and noncombat-deployed personnel, we also found differences in probable PTSD prevalence across studies for theatre of deployment, with higher prevalence among personnel deployed to Iraq, and by service, with the highest prevalence rates for the army and the marines. Service may represent an area of variation and differences in prevalence of probable PTSD among services are likely to reflect differences in tasks and involvement in the conflict to which personnel were deployed. Despite the large body of research on PTSD in personnel deployed to Iraq and Afghanistan, there are areas where more research into subgroup variation is needed to reach a conclusion regarding the underlying causes, and, contrary to findings from within-study comparisons, we did not find a difference in prevalence for regular active-duty and reserve or National Guard personnel.
Conclusions
While role on deployment is an important factor for prevalence of probable PTSD, it is not the only source of differences. Categorizing studies according to deployment location and branch of service identified differences among subgroups that provide further support for factors underlying the development of PTSD, but heterogeneity between studies means that further research is required to fully explore this issue.
Acknowledgments
Declaration of interest: all authors are based at King’s College London, which receives funding from the UK Ministry of Defence. Professor Wessely is consultant adviser in psychiatry to the British Army and a trustee of Combat Stress.
The Canadian Psychiatric Association proudly supports the In Review series by providing an honorarium to the authors.
Abbreviations
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- PTSD
posttraumatic stress disorder
Footnotes
References
- 1.Castro C. Impact of combat on the mental health and well being of soldiers and marines. Smith Coll Stud Soc Work. 2009;79:247–262. [Google Scholar]
- 2.Rona RJ, Jones M, Iversen A, et al. The impact of posttraumatic stress disorder on impairment in the UK military at the time of the Iraq war. J Psychiatr Res. 2009;43(6):649–655. doi: 10.1016/j.jpsychires.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 3.Jones EW, Wessely S. Shell shock to PTSD: military psychiatry from 1900 to the Gulf War. Hove (NY): Psychology Press; 2005. [Google Scholar]
- 4.Jones E, Wessely S. A paradigm shift in the conceptualization of psychological trauma in the 20th century. J Anxiety Disord. 2007;21(2):164–175. doi: 10.1016/j.janxdis.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 5.Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 6.Andrews B, Brewin CR, Philpott R, et al. Delayed-onset posttraumatic stress disorder: a systematic review of the evidence. Am J Psychiatry. 2007;164(9):1319–1326. doi: 10.1176/appi.ajp.2007.06091491. [DOI] [PubMed] [Google Scholar]
- 7.Wessely S, Jones E. Psychiatry and the the lessons of Vietnam: what were they, and are they still relevant? War Soc. 2004;22:89–103. [Google Scholar]
- 8.Wells TS, Miller SC, Adler AB, et al. Mental health impact of the Iraq and Afghanistan conflicts: a review of US research, service provision, and programmatic responses. Int Rev Psychiatry. 2011;23(2):144–152. doi: 10.3109/09540261.2011.558833. [DOI] [PubMed] [Google Scholar]
- 9.Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry. 2010;44(1):4–19. doi: 10.3109/00048670903393597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fear NT, Jones M, Murphy D, et al. What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK Armed Forces? A cohort study. Lancet. 2010;375(9728):1783–1797. doi: 10.1016/S0140-6736(10)60672-1. [DOI] [PubMed] [Google Scholar]
- 11.Kok BC, Herrell RK, Thomas JL, et al. Posttraumatic stress disorder associated with combat service in Iraq or Afghanistan: reconciling prevalence differences between studies. JNMD. 2012;200(5):444–450. doi: 10.1097/NMD.0b013e3182532312. [DOI] [PubMed] [Google Scholar]
- 12.Chaumba J, Bride BE. Trauma experiences and posttraumatic stress disorder among women in the United States military. Soc Work Ment Health Aff. 2010;8:280–303. [Google Scholar]
- 13.Woodhead C, Wessely S, Jones N, et al. Impact of exposure to combat during deployment to Iraq and Afghanistan on mental health by gender. Psychol Med. 2012;42(9):1985–1996. doi: 10.1017/S003329171100290X. [DOI] [PubMed] [Google Scholar]
- 14.Sundin J, Fear NT, Iversen A, et al. PTSD after deployment to Iraq: conflicting rates, conflicting claims. Psychol Med. 2010;40(3):367–382. doi: 10.1017/S0033291709990791. [DOI] [PubMed] [Google Scholar]
- 15.Buckman JE, Sundin J, Greene T, et al. The impact of deployment length on the health and well-being of military personnel: a systematic review of the literature. Occup Environ Med. 2011;68(1):69–76. doi: 10.1136/oem.2009.054692. Epub 2010 Sep 30. [DOI] [PubMed] [Google Scholar]
- 16.Sundin J, Fear NT, Iversen A, et al. PTSD after deployment to Iraq: conflicting rates, conflicting claims. Psychol Med. 2010;40(3):367–382. doi: 10.1017/S0033291709990791. [DOI] [PubMed] [Google Scholar]
- 17.Blanchard EB, Jones-Alexander J, Buckley TC, et al. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 18.Foa EB, Riggs DS, Dancu CV, et al. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress. 1993;6(4):459–473. [Google Scholar]
- 19.Hovens JE, van der Ploeg HM, Bramsen I, et al. The development of the Self-Rating Inventory for Posttraumatic Stress Disorder. Acta Psychiatr Scand. 1994;90(3):172–183. doi: 10.1111/j.1600-0447.1994.tb01574.x. [DOI] [PubMed] [Google Scholar]
- 20.Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramchand R, Schell TL, Karney BR, et al. Disparate prevalence estimates of PTSD among service members who served in Iraq and Afghanistan: possible explanations. J Trauma Stress. 2010;23(1):59–68. doi: 10.1002/jts.20486. [DOI] [PubMed] [Google Scholar]
- 22.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- 23.Castro CA, McGurk D. The intensity of combat and behavioral health status. Traumatology. 2007;13(4):6–23. [Google Scholar]
- 24.Maguen S, Lucenko BA, Reger MA, et al. The impact of reported direct and indirect killing on mental health symptoms in Iraq war veterans. J Trauma Stress. 2010;23(1):86–90. doi: 10.1002/jts.20434. [DOI] [PubMed] [Google Scholar]
- 25.Phillips CJ, Leardmann CA, Gumbs GR, et al. Risk factors for posttraumatic stress disorder among deployed US male Marines. BMC Psychiatry. 2010;10:52. doi: 10.1186/1471-244X-10-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jacobson IG, Horton JL, Leardmann CA, et al. Posttraumatic stress disorder and depression among US military health care professionals deployed in support of operations in Iraq and Afghanistan. J Trauma Stress. 2012;25(6):616–623. doi: 10.1002/jts.21753. [DOI] [PubMed] [Google Scholar]
- 27.Osório C, Greenberg N, Jones N, et al. Combat exposure and posttraumatic stress disorder among Portuguese special operation forces deployed in Afghanistan. Mil Psychol. 2013;25(1):70–81. [Google Scholar]
- 28.Jones M, Sundin J, Goodwin L, et al. What explains post-traumatic stress disorder (PTSD) in UK service personnel: deployment or something else? Psychol Med. 2013;43(08):1703–7012. doi: 10.1017/S0033291712002619. [DOI] [PubMed] [Google Scholar]
- 29.Sundin J, Herrell RK, Hoge CW, et al. Mental health outcomes in US and UK military personnel returning from Iraq. Br J Psychiatry. 2014;204(3):200–207. doi: 10.1192/bjp.bp.113.129569. [DOI] [PubMed] [Google Scholar]
- 30.Maguen S, Luxton DD, Skopp NA, et al. Gender differences in traumatic experiences and mental health in active duty soldiers redeployed from Iraq and Afghanistan. J Psychiatr Res. 2012;46(3):311–316. doi: 10.1016/j.jpsychires.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 31.Maguen S, Ren L, Bosch JO, et al. Gender differences in mental health diagnoses among Iraq and Afghanistan veterans enrolled in Veterans Affairs health care. Am J Public Health. 2010;100(12):2450–2456. doi: 10.2105/AJPH.2009.166165. Epub 2010 Oct 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vogt D, Vaughn R, Glickman ME, et al. Gender differences in combat-related stressors and their association with postdeployment mental health in a nationally representative sample of US OEF/OIF veterans. J Abnorm Psychol. 2011;120(4):797–806. doi: 10.1037/a0023452. [DOI] [PubMed] [Google Scholar]
- 33.Rona RJ, Fear NT, Hull L, et al. Women in novel occupational roles: mental health trends in the UK Armed Forces. Int J Epidemiol. 2007;36(2):319–326. doi: 10.1093/ije/dyl273. [DOI] [PubMed] [Google Scholar]
- 34.Kline A, Ciccone DS, Weiner M, et al. Gender differences in the risk and protective factors associated with PTSD: a prospective study of National Guard troops deployed to Iraq. Psychiatry. 2013;76(3):256–272. doi: 10.1521/psyc.2013.76.3.256. [DOI] [PubMed] [Google Scholar]
- 35.Street AE, Gradus JL, Giasson HL, et al. Gender differences among veterans deployed in support of the wars in Afghanistan and Iraq. J Gen Intern Med. 2013;28(Suppl 2):S556–S562. doi: 10.1007/s11606-013-2333-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Riddle JR, Smith TC, Smith B, et al. Millennium Cohort: the 2001–2003 baseline prevalence of mental disorders in the US military. J Clin Epidemiol. 2007;60(2):192–201. doi: 10.1016/j.jclinepi.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 37.Sareen J, Belik SL, Stein MB, et al. Correlates of perceived need for mental health care among active military personnel. Psychiatr Serv. 2010;61(1):50–57. doi: 10.1176/ps.2010.61.1.50. [DOI] [PubMed] [Google Scholar]
- 38.Skopp NA, Reger MA, Reger GM, et al. The role of intimate relationships, appraisals of military service, and gender on the development of posttraumatic stress symptoms following Iraq deployment. J Trauma Stress. 2011;24(3):277–286. doi: 10.1002/jts.20632. [DOI] [PubMed] [Google Scholar]
- 39.Luxton DD, Skopp NA, Maguen S. Gender differences in depression and PTSD symptoms following combat exposure. Depress Anxiety. 2010;27(11):1027–1033. doi: 10.1002/da.20730. [DOI] [PubMed] [Google Scholar]
- 40.Jenkins R. Sex differences in minor psychiatric morbidity: a survey of a homogeneous population. Soc Sci Med. 1985;20(9):887–899. doi: 10.1016/0277-9536(85)90345-4. [DOI] [PubMed] [Google Scholar]
- 41.Browne T, Hull L, Horn O, et al. Explanations for the increase in mental health problems in UK reserve forces who have served in Iraq. Br J Psychiatry. 2007;190(6):484–489. doi: 10.1192/bjp.bp.106.030544. [DOI] [PubMed] [Google Scholar]
- 42.Thomas JLP, Wilk JEP, Riviere LAP, et al. Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Arch Gen Psychiatry. 2010;67(6):614–623. doi: 10.1001/archgenpsychiatry.2010.54. [DOI] [PubMed] [Google Scholar]
- 43.Schell TL, Marshall GN. Survey of individuals previously deployed for OEF/OIF. Santa Monica (CA): RAND; 2008. [Google Scholar]
- 44.Smith TC, Ryan MAK, Wingard DL, et al. New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: prospective population based US military cohort study. BMJ. 2008;336(7640):366–371. doi: 10.1136/bmj.39430.638241.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298(18):2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- 46.Harvey SB, Hatch SL, Jones M, et al. Coming home: social functioning and the mental health of UK Reservists on return from deployment to Iraq or Afghanistan. Ann Epidemiol. 2011;21(9):666–672. doi: 10.1016/j.annepidem.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 47.Iversen A, Fear NT, Ehlers A, et al. Risk factors for post-traumatic stress disorder among UK Armed Forces personnel. Psychol Med. 2008;38(4):511–522. doi: 10.1017/S0033291708002778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Smith TC, Corbeil TE, Ryan MA, et al. In-theater hospitalizations of US and allied personnel during the 1991 Gulf War. Am J Epidemiol. 2004;159(11):1064–1076. doi: 10.1093/aje/kwh152. [DOI] [PubMed] [Google Scholar]
- 49.Baker DG, Heppner P, Afari N, et al. Trauma exposure, branch of service, and physical injury in relation to mental health among US veterans returning from Iraq and Afghanistan. Mil Med. 2009;174(8):773–778. [PubMed] [Google Scholar]
- 50.Sundin J, Jones N, Greenberg N, et al. Mental health among commando, airborne and other UK infantry personnel. Occup Med. 2010;60(7):552–559. doi: 10.1093/occmed/kqq129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Adler AB, Wright KM, Bliese PD, et al. A2 diagnostic criterion for combat-related posttraumatic stress disorder. J Trauma Stress. 2008;21(3):301–308. doi: 10.1002/jts.20336. [DOI] [PubMed] [Google Scholar]
- 52.Allison-Aipa TS, Ritter C, Sikes P, et al. The impact of deployment on the psychological health status, level of alcohol consumption, and use of psychological health resources of postdeployed US Army Reserve soldiers. Mil Med. 2010;175(9):630–637. doi: 10.7205/milmed-d-09-00212. [DOI] [PubMed] [Google Scholar]
- 53.Booth-Kewley S, Larson GE, Highfill-McRoy RM, et al. Correlates of posttraumatic stress disorder symptoms in marines back from war. J Trauma Stress. 2010;23(1):69–77. doi: 10.1002/jts.20485. [DOI] [PubMed] [Google Scholar]
- 54.Boulos D, Zamorski M. Cumulative incidence of operational stress injuries in Canadian Forces personnel deployed in support of the mission in Afghanistan, 2001–2008. Ottawa (ON): Department of National Defence; 2011. [Google Scholar]
- 55.Bray RM, Pemberton MR, Lane ME, et al. Substance use and mental health trends among US military active duty personnel: key findings from the 2008 DoD Health Behavior Survey. Mil Med. 2010;175(6):390–399. doi: 10.7205/milmed-d-09-00132. [DOI] [PubMed] [Google Scholar]
- 56.Cabrera OA, Hoge CW, Bliese PD, et al. Childhood adversity and combat as predictors of depression and post-traumatic stress in deployed troops. Am J Prev Med. 2007;33(2):77–82. doi: 10.1016/j.amepre.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 57.Duma SJ, Reger MA, Canning SS, et al. Longitudinal mental health screening results among postdeployed US soldiers preparing to deploy again. J Trauma Stress. 2010;23(1):52–58. doi: 10.1002/jts.20484. [DOI] [PubMed] [Google Scholar]
- 58.Eisen SV, Schultz MR, Vogt D, et al. Mental and physical health status and alcohol and drug use following return from deployment to Iraq or Afghanistan. Am J Public Health. 2012;102(Suppl 1):S66–S73. doi: 10.2105/AJPH.2011.300609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Engelhard IM, van den Hout MA, Weerts J, et al. Deployment-related stress and trauma in Dutch soldiers returning from Iraq: prospective study. Br J Psychiatry. 2007;191:140–145. doi: 10.1192/bjp.bp.106.034884. [DOI] [PubMed] [Google Scholar]
- 60.Engelhard IM, Olatunji BO, de Jong PJ. Disgust and the development of posttraumatic stress among soldiers deployed to Afghanistan. J Anxiety Disord. 2011;25(1):58–63. doi: 10.1016/j.janxdis.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 61.Ferrier-Auerbach AG, Erbes CR, Polusny MA, et al. Predictors of emotional distress reported by soldiers in the combat zone. J Psychiatr Res. 2010;44(7):470–476. doi: 10.1016/j.jpsychires.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 62.Highfill-McRoy RM, Larson GE, Booth-Kewley S, et al. Psychiatric diagnoses and punishment for misconduct: the effects of PTSD in combat-deployed marines. BMC Psychiatry. 2010;10(1):88. doi: 10.1186/1471-244X-10-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hoge CW, McGurk D, Thomas JL, et al. Mild traumatic brain injury in US soldiers returning from Iraq. N Engl J Med. 2008;358(5):453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- 64.Jones N, Seddon R, Fear NT, et al. Leadership, cohesion, morale, and the mental health of UK Armed Forces in Afghanistan. Psychiatry. 2012;75(1):49–59. doi: 10.1521/psyc.2012.75.1.49. [DOI] [PubMed] [Google Scholar]
- 65.Kim PY, Thomas JL, Wilk JE, et al. Stigma, barriers to care, and use of mental health services among active duty and National Guard soldiers after combat. Psychiatr Serv. 2010;61(6):582–588. doi: 10.1176/ps.2010.61.6.582. [DOI] [PubMed] [Google Scholar]
- 66.Kline A, Falca-Dodson M, Sussner B, et al. Effects of repeated deployment to Iraq and Afghanistan on the health of New Jersey Army National Guard troops: implications for military readiness. Am J Public Health. 2010;100(2):276–283. doi: 10.2105/AJPH.2009.162925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lapierre CB, Schwegler AF, Labauve BJ. Posttraumatic stress and depression symptoms in soldiers returning from combat operations in Iraq and Afghanistan. J Trauma Stress. 2007;20(6):933–943. doi: 10.1002/jts.20278. [DOI] [PubMed] [Google Scholar]
- 68.Luxton DD, Greenburg D, Ryan J, et al. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34(9):1189–1195. doi: 10.5665/SLEEP.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Marshall BD, Prescott MR, Liberzon I, et al. Coincident posttraumatic stress disorder and depression predict alcohol abuse during and after deployment among Army National Guard soldiers. Drug Alcohol Depend. 2012;124(3):193–199. doi: 10.1016/j.drugalcdep.2011.12.027. Epub 2012 Feb 17. [DOI] [PubMed] [Google Scholar]
- 70.Martin CB. Routine screening and referrals for post-traumatic stress disorder (PTSD) after returning from Operation Iraqi Freedom in 2005, US Armed Forces. MSMR. 2007;14(6):2–7. [Google Scholar]
- 71.Mulligan K, Jones N, Woodhead C, et al. Mental health of UK military personnel while on deployment in Iraq. Br J Psychiatry. 2010;197:405–410. doi: 10.1192/bjp.bp.110.077263. [DOI] [PubMed] [Google Scholar]
- 72.Mulligan K, Fear NT, Jones N, et al. Postdeployment Battlemind training for the UK Armed Forces: a cluster randomized controlled trial. J Consult Clin Psychol. 2012;80(3):331–341. doi: 10.1037/a0027664. Epub 2012 Mar 12. [DOI] [PubMed] [Google Scholar]
- 73.Peterson AL, Wong V, Haynes MF, et al. Documented combat-related mental health problems in military noncombatants. J Trauma Stress. 2010;23(6):674–681. doi: 10.1002/jts.20585. [DOI] [PubMed] [Google Scholar]
- 74.Pietrzak RH, Johnson DC, Goldstein MB, et al. Psychological resilience and postdeployment social support protect against traumatic stress and depressive symptoms in soldiers returning from Operations Enduring Freedom and Iraqi Freedom. Depress Anxiety. 2009;26(8):745–751. doi: 10.1002/da.20558. [DOI] [PubMed] [Google Scholar]
- 75.Polusny MA, Kehle SM, Nelson NW, et al. Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in National Guard soldiers deployed to Iraq. Arch Gen Psychiatry. 2011;68(1):79–89. doi: 10.1001/archgenpsychiatry.2010.172. [DOI] [PubMed] [Google Scholar]
- 76.Polusny MA, Erbes CR, Murdoch M, et al. Prospective risk factors for new-onset post-traumatic stress disorder in National Guard soldiers deployed to Iraq. Psychol Med. 2011;41(4):687–698. doi: 10.1017/S0033291710002047. [DOI] [PubMed] [Google Scholar]
- 77.Riviere LA, Kendall-Robbins A, McGurk D, et al. Coming home may hurt: risk factors for mental ill health in US reservists after deployment in Iraq. Br J Psychiatry. 2011;198(2):136–142. doi: 10.1192/bjp.bp.110.084863. [DOI] [PubMed] [Google Scholar]
- 78.Rona RJ, Hooper R, Jones M, et al. Mental health screening in armed forces before the Iraq war and prevention of subsequent psychological morbidity: follow-up study. BMJ. 2006;333(7576):991. doi: 10.1136/bmj.38985.610949.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shen YC, Arkes J, Pilgrim J. The effects of deployment intensity on post-traumatic stress disorder: 2002–2006. Mil Med. 2009;174(3):217–223. doi: 10.7205/milmed-d-03-4307. [DOI] [PubMed] [Google Scholar]
- 80.Shen YC, Arkes J, Kwan BW, et al. Effects of Iraq/Afghanistan deployments on PTSD diagnoses for still active personnel in all four services. Mil Med. 2010;175(10):763–769. doi: 10.7205/milmed-d-10-00086. [DOI] [PubMed] [Google Scholar]
- 81.van Zuiden M, Heijnen CJ, Maas M, et al. Glucocorticoid sensitivity of leukocytes predicts PTSD, depressive and fatigue symptoms after military deployment: a prospective study. Psychoneuroendocrinology. 2012;37(11):1822–1836. doi: 10.1016/j.psyneuen.2012.03.018. Epub 2012 Apr 12. [DOI] [PubMed] [Google Scholar]
- 82.Vasterling JJ, Proctor SP, Friedman MJ, et al. PTSD symptom increases in Iraq-deployed soldiers: comparison with nondeployed soldiers and associations with baseline symptoms, deployment experiences, and postdeployment stress. J Trauma Stress. 2010;23(1):41–51. doi: 10.1002/jts.20487. [DOI] [PubMed] [Google Scholar]
- 83.Warner CH, Appenzeller GN, Grieger T, et al. Importance of anonymity to encourage honest reporting in mental health screening after combat deployment. Arch Gen Psychiatry. 2011;68(10):1065–1071. doi: 10.1001/archgenpsychiatry.2011.112. [DOI] [PubMed] [Google Scholar]
- 84.Warner CH, Appenzeller GN, Mobbs A, et al. Effectiveness of battlefield-ethics training during combat deployment: a programme assessment. Lancet. 2011;378(9794):915–924. doi: 10.1016/S0140-6736(11)61039-8. [DOI] [PubMed] [Google Scholar]
- 85.Wood MD, Britt TW, Thomas JL, et al. Buffering effects of benefit finding in a war environment. Mil Psychol. 2011;23(2):202–219. [Google Scholar]
- 86.Wright KM, Cabrera OA, Eckford RD, et al. The impact of predeployment functional impairment on mental health after combat. Psychol Trauma. 2012;4(3):260–269. [Google Scholar]
- 87.Bliese PD, Wright KM, Adler AB, et al. Timing of postcombat mental health assessments. Psychol Serv. 2007;4(3):141–148. doi: 10.1037/1541-1559.4.3.141. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.