Abstract
Background
In vivo studies reporting tibial plateau slope as a risk factor for anterior cruciate ligament (ACL) injury have been published with greatly increasing frequency.
Purpose
To examine and summarize the in vivo evidence comparing tibial slope in ACL-injured and uninjured populations.
Study Design
Systematic review and meta-analysis.
Methods
We reviewed publications in Scopus, SPORTDiscus, CINAHL, and PubMed to identify all studies reporting a measure of tibial plateau slope between ACL-injured groups and controls. A meta-analysis was performed including calculation of effect size and 95% confidence interval as well as 95% confidence intervals for the mean values of the measurement in each study.
Results
Fourteen studies met our inclusion/exclusion criteria. Five of 6 radiographic studies reporting medial tibial plateau slope (MTPS) demonstrated significant differences between controls and ACL-injured groups, while only 1 of 7 magnetic resonance imaging (MRI) studies reported significant differences between groups. Mean MTPS measurements and standard deviations reported for controls ranged from 2.9° ± 2.8° anterior to 9.5° ± 3° posterior. For ACL-injured patients, MTPS ranged from 1.8° ± 3.5° anterior to 12.1° ± 3.3° posterior. Lateral tibial plateau slope (LTPS) was reported to be significantly greater in ACL-injured groups in all 5 MRI-based studies reporting group comparisons. Mean values for LTPS in controls ranged from 0.3° ± 3.6° anterior slope to 9° ± 4° posterior slope. In ACL-injured groups, mean reported LTPS values ranged from 1.8° ± 3.2° to 11.5° ± 3.54° posterior slope.
Conclusion
Despite high measures of reliability for the various methods reported in current studies, there is vast disagreement regarding the actual values of the slope that would be considered “at risk.” Reported tibial slope values for control groups vary greatly between studies. In many cases, the study-to-study differences in “normal” tibial slope exceed the difference between controls and ACL-injured patients. The clinical utility of imaging-based measurement methods for the determination of ACL injury risk requires more reliable techniques that demonstrate consistency between studies.
Keywords: tibial slope, anterior cruciate ligament, ACL risk factors, noncontact injury
Anterior cruciate ligament (ACL) injury occurs predominantly via noncontact mechanisms.10 Because of a high incidence of long-term sequelae to ACL injury including pain, instability, and early development of osteoarthritis, a great deal of the sports medicine literature has focused on prevention.8,20,31 Identification of risk factors for ACL injury is an important step in the development of injury prevention algorithms.15,28–30 Currently, it is generally accepted that there are both modifiable and nonmodifiable risk factors that determine how likely a person is to suffer an injury to the ACL.10 Nonmodifiable risk factors are often inherent to an individual person, such as anatomic, hormonal, and sex-based traits.4,10,11,32 Modifiable risk factors include neuromuscular control patterns, gross biomechanical movement patterns, and environmental factors.1,14,16,27
Recently in the literature, there has been a great deal of focus on anatomic risk factors. Most notably, the posterior slope of the tibia has been increasingly studied as a potential risk factor, with increased frequency and widely varied results.†† Biomechanically, a higher tibial slope in the presence of a compressive load will generate a higher anterior shear component of the tibiofemoral reaction force, resulting in increased anterior motion of the tibia relative to the femur.6 Because the ACL is the primary restraint against this type of motion in the knee, it logically follows that an increase in posterior tibial slope will generate an increased load in the ACL.5 McLean et al24 have also suggested that axial compression of a knee with a higher lateral tibial plateau slope (LTPS) compared with a medial tibial plateau slope (MTPS) may cause greater anterior motion of the lateral compartment of the tibia compared with the medial compartment, creating a net internal rotation of the tibia with respect to the femur, which may increase loading on the ACL. However, despite several reports relating increased posterior slope of the medial or lateral tibial plateau to ACL injury, the level of risk posed by this intrinsic factor remains unclear. The purpose of this systematic review and meta-analysis was to identify all studies that compared one or more measures of tibial slope between an ACL-injured and a control uninjured group. The hypothesis tested was that the studies examined would demonstrate a greater posterior tibial slope in the ACL-injured compared with the control group. It was also hypothesized a priori that the relevant literature would show broad variability in absolute measured tibial plateau angle in both groups.
MATERIALS AND METHODS
We performed a systematic review of peer-reviewed, published primary research articles in the search engines CINAHL, SPORTDiscus, PubMed, and Scopus. The goal of the review was to identify all existing literature that directly related posterior tibial slope to ACL injury. We used the following search terms: “Anterior Cruciate Ligament AND Tibial Slope,” “Anterior Cruciate Ligament AND Geometry,” “Tibial Slope,” “Tibia AND Anterior Cruciate Ligament,” “Tibia AND Slope,” “Anterior Cruciate Ligament AND Anterior Tibial Translation,” “Anterior Tibial Translation AND Tibial Slope,” “Anterior Cruciate Ligament AND Risk Factor AND Tibia,” and “Tibial Slope AND Risk Factor.”
Minimal criteria for inclusion in the review were peer-reviewed, primary research articles published in the English language between publication year 1980 and December 2011 using live human patients. The year 1980 was chosen as the earliest a study would be included because this was the year that Butler et al5 demonstrated the biomechanical function of the ACL as the primary passive restraint to anterior tibial translation. Study groups had to include an ACL-injured group and a control group without ACL injury. Additionally, included studies were required to have used a medical imaging modality including, but not limited to, magnetic resonance imaging (MRI), radiographs, or computed tomography to measure anatomic tibial slope. A statistical comparison between injured and control groups was required. Studies were excluded if a nonrelated surgical procedure such as total or partial knee arthroplasty or high tibial osteotomy was performed in the study or if the study reported patient or control groups with diffuse chondral lesions or osteoarthritis. No requirements were placed on patient age, skeletal maturity, or sex.
All titles resulting from the search criteria were reviewed, and those that were clearly unrelated to the topic at hand were excluded or if terminology in the title of the study clearly eliminated that study from inclusion. Title terms including “arthroplasty,” “osteotomy,” “in vitro,” and “cadaveric” were the primary terms that led to exclusion of studies at this level of review. Abstracts of studies that could not be excluded by their title were reviewed based on the above criteria. The methods sections of remaining studies were reviewed for criteria that explicitly excluded them from the study. At this level of the review, studies were also required to report measurement of any tibial anatomic index. Studies chosen for full article review were included in the systematic review if they met all of the above inclusion criteria and none of the exclusion criteria. All references from each article included for full review were subjected to the above criteria to ensure a thorough analysis of the literature.
A meta-analysis was performed for all studies meeting the inclusion/exclusion criteria that included calculation of effect size and 95% confidence interval of injury status on reported measures of tibial plateau slope of effect size. Means and 95% confidence intervals for measures of tibial plateau slope for control and ACL-injured groups were also calculated. Effect size was calculated by dividing the difference in control and ACL-injured population mean tibial slopes by the pooled standard deviation of the study population. Pooled standard deviation was defined as
where σ represents the corresponding standard deviation. Unweighted and weighted mean effect sizes were defined as the sum of the effect sizes for each study divided by the number of studies and the sum of the products of effect size and total sample population for all studies divided by the sum of the sample populations for all studies, respectively.
RESULTS
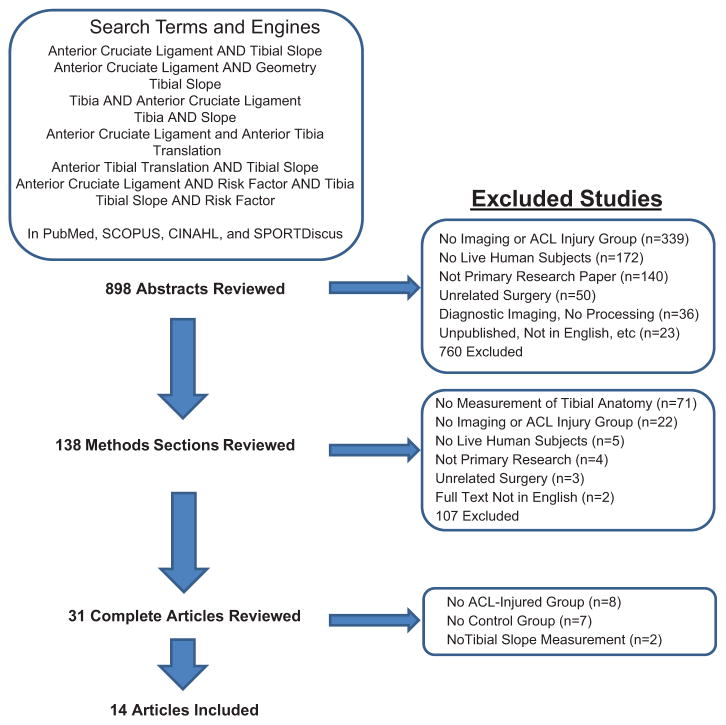
A total of 31 articles were given a full review, including a search of all references, of which a final subset of 14 met all inclusion/exclusion criteria. Figure 1 summarizes the results of the literature search, which produced 14 studies that met all inclusion/exclusion criteria. Table 1 summarizes the study designs and methodological parameters for the 14 articles included in this review.
Figure 1.
Flow chart showing the process and results for systematic review and article exclusion.
TABLE 1.
Summary of Studies Comparing Tibial Slope in Uninjured and ACL-Injured Subjectsa
| Author(s) | Study Design (Level of Evidence) | Patient Groups | Imaging Mode | Blinded Analysts | Tibial Anatomic Measurements | Specified Noncontact |
|---|---|---|---|---|---|---|
| Stijak et al38 | Case-control study (level III) | ACL: n = 33 (21 male, 12 female) CTL: n = 33 (21 male, 12 female)b |
Sagittal MRIc | Not specified | MTPS, LTPS | No |
| Bisson and Gurske-DePerio3 | Retrospective case-control study (level III) | ACL: n = 40 (20 male, 20 female) CTL: n = 40 (20 male, 20 female) |
Axial and parasagittal MRI | Not specified | MTPS, LTPS, AP-LTPD, AP-MTPD | Yes |
| Hashemi et al13 | Case-control study (level III) | ACL: n = 49 (22 male, 27 female) CTL: n = 55 (22 male, 33 female) |
Sagittal MRI | Yes | MTPS, LTPS, MPCD, CTS | No |
| Simon et al36 | Retrospective case-control study (level III) | ACL: n = 27 (17 male, 10 female) CTL: n = 27 (17 male, 10 female) |
3D-SPGR axial and sagittal MRI | Not specified | MTPS, LTPS | Yes |
| Hudek et al18 | Prognostic study (level II) | ACL: n = 55 (24 male, 31 female) CTL: n = 55 (24 male, 31 female)b |
Sagittal MRId | Not specified | MTPS, LTPS, MMS, LMS | Yes |
| Khan et al22 | Retrospective case-control study (level III) | ACL: n = 73 (53 male, 20 female) CTL: n = 51 (32 male, 19 female) |
Sagittal MRI | Yes | MTPS, LTPS, MPCD | No |
| Terauchi et al38 | Cross-sectional study (level III) | ACL: n = 77 (33 male, 40 female) CTL: n = 58 (28 male, 30 female) |
T2-weighted sagittal MRI | Not specified | MTPS | Yes |
| Meister et al26 | Retrospective cohort study (level III) | ACL: n = 49 (50 knees) CTL: n = 39 (50 knees)b |
Lateral radiograph | Not specified | MTPS-R | Yes |
| Brandon et al4 | Prognostic case-control study (level III) | ACL: n = 100 (66 male, 34 female) CTL: n = 100 (49 male, 51 female)b |
Lateral radiograph | Yes | MTPS-R | Yes |
| Todd et al40 | Case-control study (level III) | ACL: n = 140 (95 male, 45 female) CTL: n = 179 (126 male, 53 female)b |
Lateral radiograph | 2 analysts (1 blinded, 1 not) | MTPS-R | Yes |
| Hohmann et al17 | Case-control study (level III) | ACL: n = 272 (199 male, 73 female) CTL: n = 272 (199 male, 73 female) |
Lateral radiograph | Yes | NS-PTS | Yes |
| Şenişik et al33 | Prospective, longitudinal, controlled cohort study (level II) | ACL: 11 male CTL: 53 uninjured male elite soccer players Sedentary CTL: 45 nonactive male |
Lateral radiograph | Not specified if measured before injury | MTPS-R | Yes |
| Sonnery-Cottet et al37 | Retrospective case-control study (level III) | ACL: n = 50 (35 male, 15 female) CTL: n = 50 (35 male, 15 female) |
Lateral radiograph | Not specified | MTPS-R | No |
| Vyas et al41 | Retrospective cohort study (level III) | Teenagers with open physes (55% male, 45% female) ACL: n = 16 CTL: n = 23 |
Lateral + anteroposterior radiograph | Yes | MTPS-R, LTPS-R | No |
ACL, anterior cruciate ligament; CTL, control; MRI, magnetic resonance imaging; MTPS, medial tibial plateau slope; LTPS, lateral tibial plateau slope; 3D-SPGR, 3-dimensional spoiled gradient-recalled echo; AP-LTPD, anterior-posterior lateral tibial plateau depth; AP-MTPD, anterior-posterior medial tibial plateau depth; MPCD, medial tibial plateau concave depth; CTS, coronal plane tibial slope; MMS, medial meniscal slope; LMS, lateral meniscal slope; MTPS-R, medial tibial plateau slope (radiographic); NS-PTS, nonspecified (medial or lateral) posterior tibial slope; LTPS-R, lateral tibial plateau slope (radiographic).
Patellofemoral pain syndrome/anterior knee pain control group.
Proximal tibial anatomic axis determined on lateral radiographs and anatomic measurements on MRI.
Parameters available in article.
Of the 14 studies included in this meta-analysis, one study specifically limited its cohort to skeletally immature patients with open physes.41 Four other studies either specifically excluded skeletally immature patients from their patient base or included only “elite” athletes assumed (by the authors) to be skeletally mature.3,13,33,37 None of the other 9 studies included in the review specified whether they included or excluded skeletally immature patients from the cohort. Effect size for medial tibial slope as measured on MRI showed stronger agreement across studies than the same measure on lateral radiographs with 1 exception. Only 1 MRI study of MTPS showed statistically significantly higher MTPS in ACL-injured patients. Lateral tibial plateau slope was only measured on MRI and was statistically significant for all studies. The literature indicates a stronger likelihood for LTPS to be associated with ACL injury risk compared with MTPS. One radiographic study measured “posterior inferior tibial slope” without specifying whether it was the medial or lateral tibial slope and found insignificant group differences.
Injured Versus Uninjured Group Comparisons
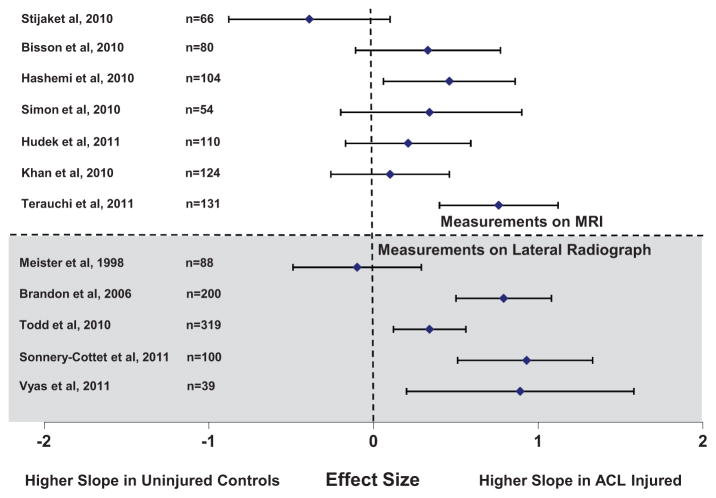
Medial tibial plateau slope was the most commonly reported measure of tibial slope. Thirteen of 14 studies reported MTPS measurement between ACL-injured and control groups. Six of these studies were performed on lateral radiographs, and 7 were performed using MRI. Of those on lateral radiographs, 5 of the 6 report significantly higher MTPS in ACL-injured patients compared with controls.4,33,37,40,41 Of the 7 performed on MRI, 1 study reported significance between groups,13 and 1 did not perform a statistical group comparison.39 A summary of the results of studies reporting MTPS, the most frequently reported measure, is shown in Figure 2. Note that in this figure, an effect size greater than zero indicates that the mean tibial slope of the ACL-injured group was more posteriorly oriented than the mean tibial slope of the control group. An effect size less than zero denotes a study where the control group showed a more posteriorly oriented tibial slope than ACL-injured patients. Because Senisik et al33 had an active control group and a sedentary control group, and there were major differences in sample size between each of these groups and the ACL-injured group, no effect size calculation was performed for this study, although they report significant differences between groups based on injury.
Figure 2.
Effect size for medial tibial plateau slope with respect to injury status.
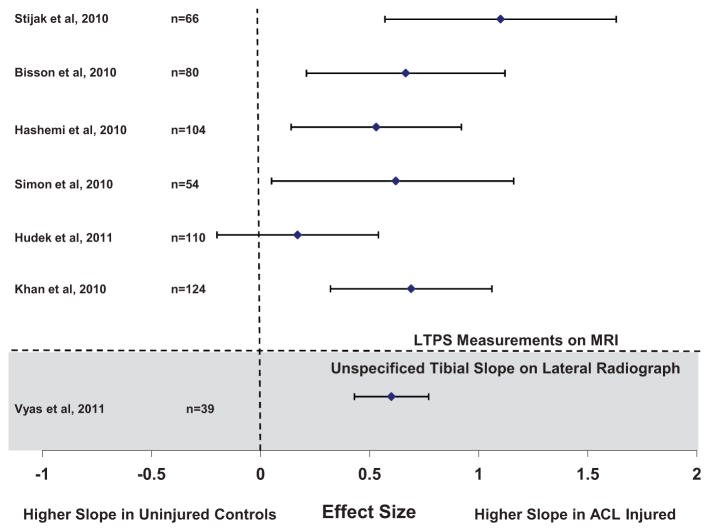
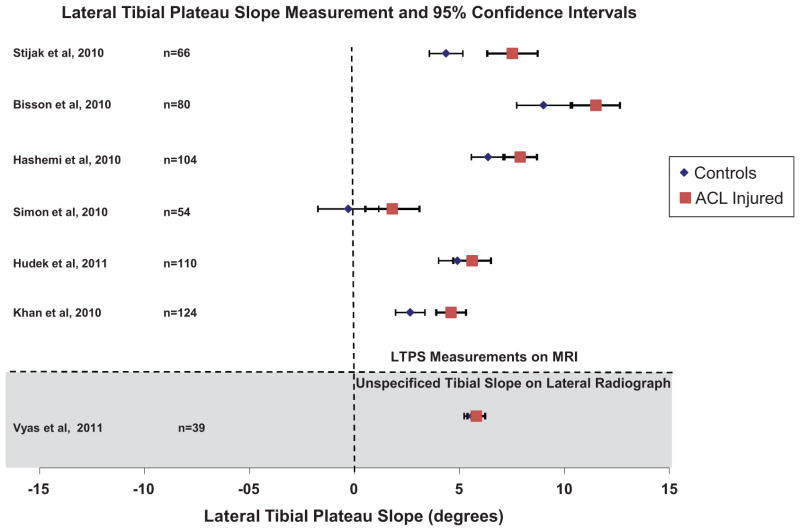
A summary of the results of studies that reported LTPS or unspecified radiographic tibial slope (n = 7; 6 MRI and 1 radiograph17) is shown in Figure 3. Because other studies reported specific measurement of the medial slope, the unspecified posterior tibial slope measurement reported by Hohmann et al17 was included in the assessment of lateral slope. One study did not report grouped statistical comparisons of ACL-injured versus uninjured LTPS measurements.3 Of the 6 studies that compared LTPS in ACL-injured and uninjured groups as a whole, 1 radiographic study and 1 MRI-based study found no significant difference between injured and uninjured groups.18,41
Figure 3.
Effect size for lateral tibial plateau slope with respect to injury status.
Variability in Absolute Measures of Tibial Plateau Angle
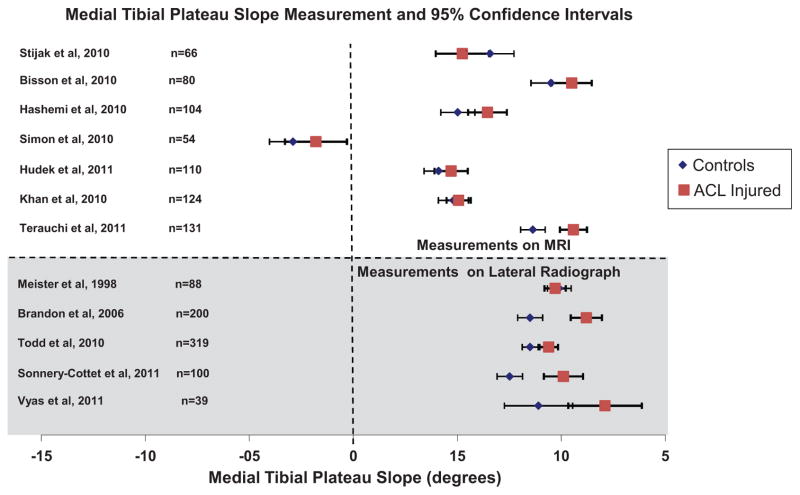
Absolute measures of medial or lateral tibial plateau angle between studies demonstrated a large range of variability. Mean MTPS measurements and standard deviations reported for controls ranged from 2.9° ± 2.80° anterior to 9.5° ± 3° posterior.3,36 For ACL-injured patients, the medial slope ranged from 1.8° ± 3.5° anterior to 12.1° ± 3.3° posterior.3,41 Figure 4 shows the absolute measurements for MTPS by study. The unweighted mean effect size for the 13 studies was .388, indicating a more posterior MTPS in ACL-injured populations than controls. Weighted by study population size, the mean effect size was .416 toward a higher slope in ACL-injured patients.
Figure 4.
Absolute measures of medial tibial plateau slope in controls and anterior cruciate ligament–injured patients by study.
Mean values for LTPS in control groups ranged from 0.3° ± 3.6° anterior slope in Simon et al36 to 9° ± 4° posterior slope in Bisson and Gurske-DePerio3 and are shown in Figure 5. In ACL-injured groups, mean reported LTPS values ranged from 1.8° ± 3.2° posterior in Simon et al36 to 11.5° ± 3.54° posterior slope in Bisson and Gurske-DePerio.3 Unweighted mean effect size for LTPS was .6291 toward a higher LTPS. Weighted mean effect size was .596.
Figure 5.
Absolute measures of lateral tibial plateau slope in controls and anterior cruciate ligament–injured patients by study.
DISCUSSION
The biomechanical basis for an association between posterior tibial slope and ACL injury risk has been defined in the literature. Dejour and Bonnin6 used lateral radiographs to demonstrate a mean 6-mm increase in anterior tibial translation (ATT) for each 10° increase in posterior tibial slope in ACL-deficient patients and healthy controls. Giffin et al9 used high tibial osteotomy in vitro to increase mean tibial plateau slope from 8.8° to 13.2° in 10 cadaveric knees. They reported a 3.6-mm increased ATT at rest and an additional 1.9-mm increased ATT under axial compression. In contrast, Fening et al7 found increased ATT in vitro at resting alignment, but they demonstrated decreased strain in the ACL after posterior tibial slope–increasing high tibial osteotomy. More recently, McLean et al25 reported that posterior tibial slope in vitro was associated with increased anterior tibial acceleration. Furthermore, they found that strain in the anteromedial band of the ACL correlates to peak anterior tibial acceleration upon impact simulating a single-legged landing. In another study, these authors reported significant associations between medial and lateral posterior tibial slopes and peak knee abduction moment, a prospectively established predictor of ACL injury risk, in healthy, recreationally active women in vivo.14,24 Shelburne et al35 and Shao et al34 used computer modeling and electromyography-driven computational modeling, respectively, to demonstrate the effect of increasing tibial slope on tibiofemoral contact and ACL loading. Their results demonstrate increased force transmission through the ACL during standing and gait as the tibial slope increases.
Despite an abundance of in vitro cadaveric studies, animal studies, and biomechanical theory-based literature highlighting the potential effects of high posterior tibial slope on ACL strain generation, this review focuses on in vivo observations that directly relate injury to tibial anatomic variability. The studies included in this review compose the body of in vivo literature associating posterior tibial slope to ACL injury.
The current review highlights the consistencies and inconsistencies in the literature regarding MTPS and LTPS as potential risk factors for ACL injury. While nearly all studies that reported tibial slope values in ACL-injured and uninjured patients report greater slope in those with injury, there is considerable inconsistency regarding the values of slope that would be considered “at risk.” Some of the inconsistency in these reports may be attributed to use of different measurement methodology; however, several studies reported use of the same techniques with varying results. More so, reports of high interrater and intrarater intraclass correlation coefficients (ICCs) often accompanied each of these studies. Five MRI-based studies used the methodology defined by Hashemi et al11 in 2008 to measure MTPS. One of these 5 studies, Khan et al,22 did not report measures of tibial slope using this method but instead defined and used a different method based on their report of greater reliability. Simon et al36 used a slight modification of the method defined by Hashemi et al11 based on 3-dimensional reconstruction of the tibial geometry and subsequent analysis of the tibial slope. Of the 3 other studies using the exact Hashemi et al11 methodology, Bisson and Gurske-DePerio3 and Terauchi et al39 reported the most similar results. Differences between means in control groups vary by only 0.87°; however, a difference of 0.87° corresponds to nearly the mean difference between control and ACL-injured values reported by Bisson and Gurske-DePerio.3 This also corresponds to 60% of the difference between injured patients and controls for Hashemi et al13 and 50% of the difference in means between controls and ACL-injured patients for Terauchi et al.39 Reported interrater ICCs for this method range from .73 to .98 for MTPS.22,39
Three studies in this report used the method defined by Hashemi et al11 to measure LTPS with greatly different results. The smallest between-study difference for mean LTPS values in control groups using the Hashemi et al method is 2.64° between Hashemi et al13 and Bisson and Gurske-DePerio,3 while the largest within-study difference between ACL-injured patients and controls is 2.5° for Bisson and Gurske-DePerio.3 Reported interrater ICCs for this method used for LTPS range from .81 to .88.12,22
The lack of a consistently employed gold-standard method for the measurement of tibial slope severely hinders the interpretation of the existing literature. Across studies, there is an overwhelming intersection of values for tibial slope that are reportedly associated with uninjured patients and those associated with ACL injury. There is no clearly, or even vaguely, defined threshold for posterior tibial slope that demonstrates a distinction between controls and ACL-injured patients. Given that the average difference in tibial slope between controls and ACL-injured patients reported in this review was 1.51° ± 1.3°, it is imperative that a methodology emerges that provides significantly greater interrater reliability.
There are several potential sources of error that may account for the high level of variability between the studies analyzed. Investigators should carefully consider the question that they are trying to answer when choosing the imaging modality they wish to use. Lee et al23 demonstrated significant increases in tibial plateau slope measurements within the same population when lateral radiographs were used compared with sagittal plane MRI. These differences were more significant on the lateral side. Hudek et al19 noted typical interobserver and intraobserver errors of ±1.4° and ±1.2°, respectively, while some studies have demonstrated much larger errors using radiographs.21 One of the greatest strengths of using MRI for this application is the ability to visualize the surface geometry of the articular cartilage.2 Because this represents the functional point of tibiofemoral articulation and is not visible on radiographs, a strong case can be made for preference to MRI over radiographs.2 In defining the posterior tibial slope from sagittal plane MRI, one must first determine the tibial anatomic axis. Next, the proper anatomic slice that best characterizes the tibiofemoral articulation on the side of the tibia of interest should be chosen and the tibial anatomic axis superimposed onto the image. Finally, the line defining the medial or lateral articular surface of the tibia must be defined. The posterior tibial slope angle is defined as the angle between this articular surface and a vector perpendicular to the tibial axis.6,9,12,19
In addition to potential errors at each of the above-mentioned steps is the potential for misalignment of the patient within the magnetic resonance device during imaging. Careful steps should be taken to align the patient such that a true anatomic sagittal view is obtained. This may include standardization of knee flexion angle and foot alignment, palpation of anatomic landmarks at the proximal and distal tibia during positioning to adjust alignment, and immobilization of hip internal/external rotation during positioning and imaging. When possible, automated 3-dimensional reconstructions of the tibiofemoral geometry and articular surfaces should be used to ensure the greatest consistency in slice alignment and anatomic position for the analysis. Given the sensitivity required of this measurement for utility as a risk-identifying tool, clinical recommendations for each of these steps that can be universally employed with high repeatability should be the next step in advancement of this line of research.
Future studies should explore more reliable methods of imaging and image processing with the goal of creating a cohesive body of literature that enhances the use of tibial slope measurement as a predictive tool for ACL risk. Data from this meta-analysis show that each of the measurement methods currently employed has shortcomings in their reliability. The method defined by Hashemi et al11 is the most frequently used and shows moderate repeatability across studies. This should be the preferred methodology until a significantly more reliable and standardized protocol is defined and validated in the literature. Such a method should rigidly define the tibial slope measurement process from initial imaging parameters to actual tibial slope measurement. The goal of the line of research relating tibial plateau slope to ACL injury risk should be to establish not only the extent of the role of tibial slope in injury risk but also the extent to which that risk can be decreased by prophylactic interventions such as neuromuscular training. Such methodologies will also enhance the objectivity of tibial slope as a factor in the assessment of postinjury stability and long-term sequelae. Studies should use prospective enrollment of consecutive noncontact ACL-injured patients with blinded image analysts.
CONCLUSION
Conflicting, highly variable evidence for the role of tibial plateau slope and other anatomic measures in injury risk assessment makes interpretation of the current literature difficult. Inconsistencies within and between tibial slope measurement methodologies have precluded repeatable demonstration of an “at ACL injury risk” range of tibial slope values. Noncontact ACL injury is likely a multifactorial phenomenon, so identification of new risk factors is paramount to prevention. While trends in the current literature indicate a potential relationship between ACL injury and posterior tibial slope, standardized techniques and more consistent and repeatable data are required to definitively link the two.
Acknowledgments
The authors acknowledge the clinical and research staff members at the Sports Health and Performance Institute and the Cincinnati Children’s Hospital Sports Medicine Biodynamics Center.
Footnotes
For reprints and permission queries, please visit SAGE’s Web site at http://www.sagepub.com/journalsPermissions.nav
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported by National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases grants R01-AR049735, R01-AR05563, and R01-AR056259.
References
- 1.Anderson AF, Dome DC, Gautam S, Awh MH, Rennirt GW. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29(1):58–66. doi: 10.1177/03635465010290011501. [DOI] [PubMed] [Google Scholar]
- 2.Biedert R, Sigg A, Gal I, Gerber H. 3D representation of the surface topography of normal and dysplastic trochlea using MRI. Knee. 2011;18(5):340–346. doi: 10.1016/j.knee.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 3.Bisson LJ, Gurske-DePerio J. Axial and sagittal knee geometry as a risk factor for noncontact anterior cruciate ligament tear: a case-control study. Arthroscopy. 2010;26(7):901–906. doi: 10.1016/j.arthro.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 4.Brandon ML, Haynes PT, Bonamo JR, et al. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy. 2006;22(8):894–899. doi: 10.1016/j.arthro.2006.04.098. [DOI] [PubMed] [Google Scholar]
- 5.Butler DL, Noyes FR, Grood ES. Ligamentous restraints to anterior-posterior drawer in the human knee: a biomechanical study. J Bone Joint Surg Am. 1980;62(2):259–270. [PubMed] [Google Scholar]
- 6.Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture: two radiological tests compared. J Bone Joint Surg Br. 1994;76(5):745–749. [PubMed] [Google Scholar]
- 7.Fening SD, Kovacic J, Kambic H, McLean S, Scott J, Miniaci A. The effects of modified posterior tibial slope on anterior cruciate ligament strain and knee kinematics: a human cadaveric study. J Knee Surg. 2008;21(3):205–211. doi: 10.1055/s-0030-1247820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fink C, Hoser C, Hackl W, Navarro RA, Benedetto KP. Long-term outcome of operative or nonoperative treatment of anterior cruciate ligament rupture: is sports activity a determining variable? Int J Sports Med. 2001;22(4):304–309. doi: 10.1055/s-2001-13823. [DOI] [PubMed] [Google Scholar]
- 9.Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376–382. doi: 10.1177/0363546503258880. [DOI] [PubMed] [Google Scholar]
- 10.Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Hashemi J, Chandrashekar N, Gill B, et al. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;90(12):2724–2734. doi: 10.2106/JBJS.G.01358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hashemi J, Chandrashekar N, Gill B, et al. The tibial plateau geometry: impact on biomechanics of the tibiofemoral joint and anterior cruciate ligament injury. Br J Sports Med. 2008;42(6):522. [Google Scholar]
- 13.Hashemi J, Chandrashekar N, Mansouri H, et al. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):54–62. doi: 10.1177/0363546509349055. [DOI] [PubMed] [Google Scholar]
- 14.Hewett TE. Neuromuscular and hormonal factors associated with knee injuries in female athletes: strategies for intervention. Sports Med. 2000;29(5):313–327. doi: 10.2165/00007256-200029050-00003. [DOI] [PubMed] [Google Scholar]
- 15.Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes, part 1: mechanisms and risk factors. Am J Sports Med. 2006;34(2):299–311. doi: 10.1177/0363546505284183. [DOI] [PubMed] [Google Scholar]
- 16.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 17.Hohmann E, Bryant A, Reaburn P, Tetsworth K. Is there a correlation between posterior tibial slope and non-contact anterior cruciate ligament injuries? Knee Surg Sports Traumatol Arthrosc. 2011;19(Suppl 1):S109–S114. doi: 10.1007/s00167-011-1547-4. [DOI] [PubMed] [Google Scholar]
- 18.Hudek R, Fuchs B, Regenfelder F, Koch PP. Is noncontact ACL injury associated with the posterior tibial and meniscal slope? Clin Orthop Relat Res. 2011;469:2377–2384. doi: 10.1007/s11999-011-1802-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467(8):2066–2072. doi: 10.1007/s11999-009-0711-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kessler MA, Behrend H, Henz S, et al. Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc. 2008;16(5):442–448. doi: 10.1007/s00167-008-0498-x. [DOI] [PubMed] [Google Scholar]
- 21.Kessler MA, Burkart A, Martinek V, Beer A, Imhoff AB. Development of a 3-dimensional method to determine the tibial slope with multislice-CT. Z Orthop Ihre Grenzgeb. 2003;141(2):143–147. doi: 10.1055/s-2003-38658. [DOI] [PubMed] [Google Scholar]
- 22.Khan MS, Seon JK, Song EK. Risk factors for anterior cruciate ligament injury: assessment of tibial plateau anatomic variables on conventional MRI using a new combined method. Int Orthop. 2011;35(8):1251–1256. doi: 10.1007/s00264-011-1217-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee YS, Kim JG, Lim HC, et al. The relationship between tibial slope and meniscal insertion. Knee Surg Sports Traumatol Arthrosc. 2009;17(12):1416–1420. doi: 10.1007/s00167-009-0847-4. [DOI] [PubMed] [Google Scholar]
- 24.McLean SG, Lucey SM, Rohrer S, Brandon C. Knee joint anatomy predicts high-risk in vivo dynamic landing knee biomechanics. Clin Biomech. 2010;25(8):781–788. doi: 10.1016/j.clinbiomech.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 25.McLean SG, Oh YK, Palmer ML, et al. The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. J Bone Joint Surg Am. 2011;93(14):1310–1317. doi: 10.2106/JBJS.J.00259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meister K, Talley MC, Horodyski MB, et al. Caudal slope of the tibia and its relationship to noncontact injuries to the ACL. Am J Knee Surg. 1998;11(4):217–219. [PubMed] [Google Scholar]
- 27.Myer GD, Ford KR, Hewett TE. The effects of gender on quadriceps muscle activation strategies during a maneuver that mimics a high ACL injury risk position. J Electromyogr Kinesiol. 2005;15(2):181–189. doi: 10.1016/j.jelekin.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 28.Myer GD, Ford KR, Hewett TE. New method to identify athletes at high risk of ACL injury using clinic-based measurements and free-ware computer analysis. Br J Sports Med. 2011;45(4):238–244. doi: 10.1136/bjsm.2010.072843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Biomechanics laboratory-based prediction algorithm to identify female athletes with high knee loads that increase risk of ACL injury. Br J Sports Med. 2011;45(4):245–252. doi: 10.1136/bjsm.2009.069351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Clinical correlates to laboratory measures for use in non-contact anterior cruciate ligament injury risk prediction algorithm. Clin Biomech. 2010;25(7):693–699. doi: 10.1016/j.clinbiomech.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nebelung W, Wuschech H. Thirty-five years of follow-up of anterior cruciate ligament: deficient knees in high-level athletes. Arthroscopy. 2005;21(6):696–702. doi: 10.1016/j.arthro.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 32.Posthumus M, Collins M, September AV, Schwellnus MP. The intrinsic risk factors for ACL ruptures: an evidence-based review. Phys Sportsmed. 2011;39(1):62–73. doi: 10.3810/psm.2011.02.1863. [DOI] [PubMed] [Google Scholar]
- 33.Şenişik S, Özgürbüz C, Ergün M, et al. Posterior tibial slope as a risk factor for anterior cruciate ligament rupture in soccer players. J Sports Sci Med. 2011;10(4):763–767. [PMC free article] [PubMed] [Google Scholar]
- 34.Shao Q, MacLeod TD, Manal K, Buchanan TW. Estimation of ligament loading and anterior tibial translation in healthy and ACL-deficient knees during gait and the influence of increasing tibial slope using EMG-driven approach. Ann Biomed Eng. 2011;39(1):110–121. doi: 10.1007/s10439-010-0131-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shelburne KB, Kim H, Sterett WI, Pandy MG. Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res. 2011;29(2):223–231. doi: 10.1002/jor.21242. [DOI] [PubMed] [Google Scholar]
- 36.Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM. A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43(9):1702–1707. doi: 10.1016/j.jbiomech.2010.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sonnery-Cottet B, Archbold P, Cucurulo T, et al. The influence of the tibial slope and the size of the intercondylar notch on rupture of the anterior cruciate ligament. J Bone Joint Surg Br. 2011;93(11):1475–1478. doi: 10.1302/0301-620X.93B11.26905. [DOI] [PubMed] [Google Scholar]
- 38.Stijak L, Herzog RF, Schai P. Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surg Sports Traumatol Arthrosc. 2008;16(2):112–117. doi: 10.1007/s00167-007-0438-1. [DOI] [PubMed] [Google Scholar]
- 39.Terauchi M, Hatayama K, Yanagisawa S, Saito K, Takagishi K. Sagittal alignment of the knee and its relationship to noncontact anterior cruciate ligament injuries. Am J Sports Med. 2011;39(5):1090–1094. doi: 10.1177/0363546510393305. [DOI] [PubMed] [Google Scholar]
- 40.Todd MS, Lalliss S, Garcia E, DeBerardino TM, Cameron KL. The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):63–67. doi: 10.1177/0363546509343198. [DOI] [PubMed] [Google Scholar]
- 41.Vyas S, van Eck CF, Vyas N, Fu FH, Otsuka NY. Increased medial tibial slope in teenage pediatric population with open physes and anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2011;19(3):372–377. doi: 10.1007/s00167-010-1216-z. [DOI] [PMC free article] [PubMed] [Google Scholar]