Abstract
This paper focuses on how the acoustical differences between the ear canals of adults and children affect amplification requirements and describes efficient strategies to allow for these differences when prescribing and verifying amplification. We will first summarize the problem for hearing assessment and then describe how adult-equivalent hearing loss can be calculated to circumvent this problem. Example cases demonstrate manual calculation and automatic derivation by using the NAL-NL1 software. The advantage of using real-ear aided gain prescriptions rather than real-ear insertion gain prescriptions for young children is explained. The practical benefit of deriving coupler gain targets to achieve the required real-ear aided gain by using individually measured real-ear-to-coupler differences is emphasized, together with a discussion on the practical issues relating to calibration and probe tube placement in measuring real-ear-to-coupler differences. Finally, an illustrative case exemplifies the derivation of individualized coupler gain targets by using the NAL-NL1 software system to achieve the required real-ear aided gain for a young child.
Introduction
It is highly desirable to fit hearing aids to hearing-impaired children as early in life as possible (Moeller, 2000; Yoshinaga-Itano et al., 1998). With universal hearing screening programs now existing in many places, it is possible to detect hearing impairment and fit amplification in early infancy. Ching (2003, in press) summarizes the issues that are important in providing effective amplification to young children. This article focuses on how acoustical differences between the ear canals of adults and children affect amplification requirements, and describes efficient strategies to allow for these differences when prescribing and verifying amplification.
Effect of Interaction between Transducers and Ear Canals in Determining Thresholds
The Problem
Marcoux and Hansen (this issue) rightly point out that ear canal acoustics affect the accuracy of measurement and the recording of hearing thresholds. Because transducers have conventionally been calibrated such that an average adult person who has normal hearing has thresholds of 0 dB HL, the same will not be true for a child who has shorter and narrower ear canals than an average adult.
If insert earphones are used in determining thresholds, the volume of the ear canal directly affects the sound pressure level generated at the eardrum. As the child grows, the canal volume increases, and the SPL generated at the eardrum decreases. This, in turn, causes apparent hearing thresholds to “deteriorate” with increases in age. If sound field assessment is used, the length of the ear canal determines its resonance properties, which determines the real-ear unaided gain (REUG) of the ear, and hence the real-ear threshold. As a child grows from 1 month to 3 years, the resonance peak in REUG moves from around 6 kHz to 3 kHz (Kruger, 1987). Therefore, the child's apparent hearing thresholds will deteriorate at 6 kHz, but improve at 3 kHz over this time, assuming that there are no other maturation effects. If headphones are used, both the volume and the length of the ear canal will affect thresholds. All these effects mean that the audiometer dial readings do not accurately reflect the child's thresholds, and that results measured by using any of the audiometric transducers (insert earphones, sound field loudspeakers, TDH series headphones) are not equivalent across measurement conditions.
Solutions
Effective solutions are well-developed and are based on the fact that the SPL at the eardrum required to hear a test signal will be the same, regardless of the transducer used to deliver the signal or the geometry of the ear canal. Seewald and Scollie (1999) proposed that all thresholds be expressed in terms of dB SPL at the eardrum, and represented on an SPLogram. The procedure involves converting the measured dial readings into SPL at the eardrum by using individually measured real-ear-to-coupler differences (RECD) or real-ear-to-dial differences (REDD). Because this method will, no doubt, be discussed in a companion article by its proponents (Seewald and Scollie, this issue), we will focus on a different but equally effective solution, which is to express thresholds as equivalent adult hearing level (Dillon, 2001). The adult-equivalent hearing loss (HLa.e.) is the threshold level that an average adult would have if the adult has the same threshold in dB SPL at the eardrum as the child. The units are dB HL, and can be plotted on a standard audiogram.
How does the audiologist calculate the adult-equivalent hearing loss from the audiometer dial reading? Depending on the transducer used in measurement, the correction factors for calculating adult-equivalent hearing loss are different:
-
When an insert earphone is used (either with a foam tip or a custom earmold) in hearing assessment, it is necessary to measure the individual's RECD (RECDindiv.) as well. The audiometer dial reading (HLdial) can then be converted by using Equation 1:
where HLdial is the audiometer dial reading, synonymous with the term “DL” coined by Marcoux and Hansen (this issue), and RECDa.avg. is the RECD for an average adult.(1) Alternatively, if sound pressure level at the eardrum (SPLcanal) is recorded, Equation 2 can be used:
where REDDa.avg. is the REDD for an average adult. The average adult RECD and REDD values are given in Table 1.(2) - When a loudspeaker is used in the sound field, it is necessary to measure the individual's real-ear unaided gain (REUGindiv.). Where the audiometer has been calibrated so that 0 dB on the dial causes an SPL in the sound field equal to adult average minimum audible field or MAF (ie, the dial correctly indicates HL), dial readings can be converted using Equation 3:
If threshold has been recorded as sound pressure level in the sound field (SPLfield), use Equation 4:(3)
where MAF is Minimum Audible Field. The REUGa.avg. and MAF values are given in Table 1.(4) When a TDH-series headphone is used in hearing assessment, adult-equivalent hearing loss could be calculated if it is assumed that the difference at the eardrum between adult and child is the same for a supra-aural headphone as it is for sound field.
Table 1.
Average Adult REDD, RECD, and REUG Values
| Frequency (Hz) | ||||||||
|---|---|---|---|---|---|---|---|---|
| 250 | 500 | 1000 | 2000 | 3000 | 4000 | 6000 | ||
| MAF (dBSPL) | 12.7 | 7.5 | 5.7 | 2.5 | −1.6 | −1.9 | 10.4 | |
| REDDa.avg. | 18.0 | 9.5 | 5.0 | 10.5 | 12.5 | 12.0 | 11.5 | |
| RECDa.avg. | HA-1 | 3.5 | 3.5 | 5.0 | 8.0 | 10.0 | 12.0 | 14.0 |
| HA-2 | 4.0 | 4.0 | 5.0 | 7.5 | 9.0 | 6.5 | 9.5 | |
| REUGa.avg. | 0° | 0 | 0 | 1.0 | 12.0 | 14.0 | 12.0 | 3.0 |
| 45° | 0 | 0 | 1.0 | 12.0 | 17.0 | 15.0 | 7.0 | |
Minimum audible field (MAF) values, adult average real-ear-to-dial difference (REDDa.avg.) values, adult average real-ear-to-coupler difference (RECDa.avg.), and adult average real-ear unaided gain (REUGa.avg.) values measured with a control microphone and sound source at 0° and 45° azimuth. All values are in dB. MAF values are from Bentler and Pavlovic, 1989. REUGa.avg. values are from Dillon, 2001, p.99; RECDa.avg. HA-1 values are from Sachs and Burkhard, 1972; REDDa.avg. are calculated from the sum of RECDa.avg.(HA-1) and RETSPL(HA-1), ANSI S3.6, 1996; RECDa.avg. (HA-2) values are calculated from the difference between REDDa.avg. and RETSPL(HA-2), ANSI S3.6, 1996.
However, this is not likely to be a good assumption because the ears will differ in volume and leakage as well as in resonance characteristics. This method of assessment is therefore not recommended for infants.
Illustrative Cases
Simple Calculation
Table 2 shows a worksheet for calculating adult-equivalent hearing loss for stimuli presented from either insert earphones or a loudspeaker in the sound field, each with the stimuli calibrated in either dB SPL or dB HL.
Table 2.
Worksheet for Calculating Adult-Equivalent Hearing Loss
| Frequency (Hz) | |||||||
|---|---|---|---|---|---|---|---|
| 250 | 500 | 1000 | 2000 | 3000 | 4000 | 6000 | |
| Insert earphone + own mold (dB HL): Eq. 1 | |||||||
| HLdial | 60 | 60 | 60 | 60 | 60 | 60 | 60 |
| + RECDindiv | 5 | 10 | 14 | 15 | 13 | 13 | 13 |
| − RECDa.avg. | 4 | 4 | 5 | 8 | 9 | 7 | 10 |
| = HLa.e. | 61 | 66 | 69 | 67 | 64 | 66 | 63 |
| Insert earphone + own mold (dB SPL): Eq. 2 | |||||||
| SPLcanal | 60 | 60 | 60 | 60 | 60 | 60 | 60 |
| − REDDa.avg. | 18 | 10 | 5 | 11 | 13 | 12 | 12 |
| = HLa.e. | 42 | 50 | 55 | 49 | 47 | 48 | 48 |
| Loudspeaker in sound field (dB HL): Eq. 3 | |||||||
| HLdial | 60 | 60 | 60 | 60 | 60 | 60 | 60 |
| + REUGindiv | 1 | 1 | 2 | 5 | 5 | 6 | 14 |
| − REUGa.avg. | 0 | 0 | 1 | 12 | 17 | 15 | 7 |
| = HLa.e. | 61 | 61 | 61 | 53 | 48 | 51 | 67 |
| Loudspeaker in sound field (dB SPL): Eq. 4 | |||||||
| SPLfield | 60 | 60 | 60 | 60 | 60 | 60 | 60 |
| − MAF | 13 | 8 | 6 | 3 | −2 | −2 | 10 |
| + REUGindiv | 1 | 1 | 2 | 5 | 5 | 6 | 14 |
| − REUGa.avg. | 0 | 0 | 1 | 12 | 17 | 15 | 7 |
| = HLa.e. | 48 | 53 | 55 | 50 | 50 | 53 | 57 |
The adult-equivalent hearing loss (HLa.e) is shown with the measured values in italics, and the calculated HLa.e values in bold.
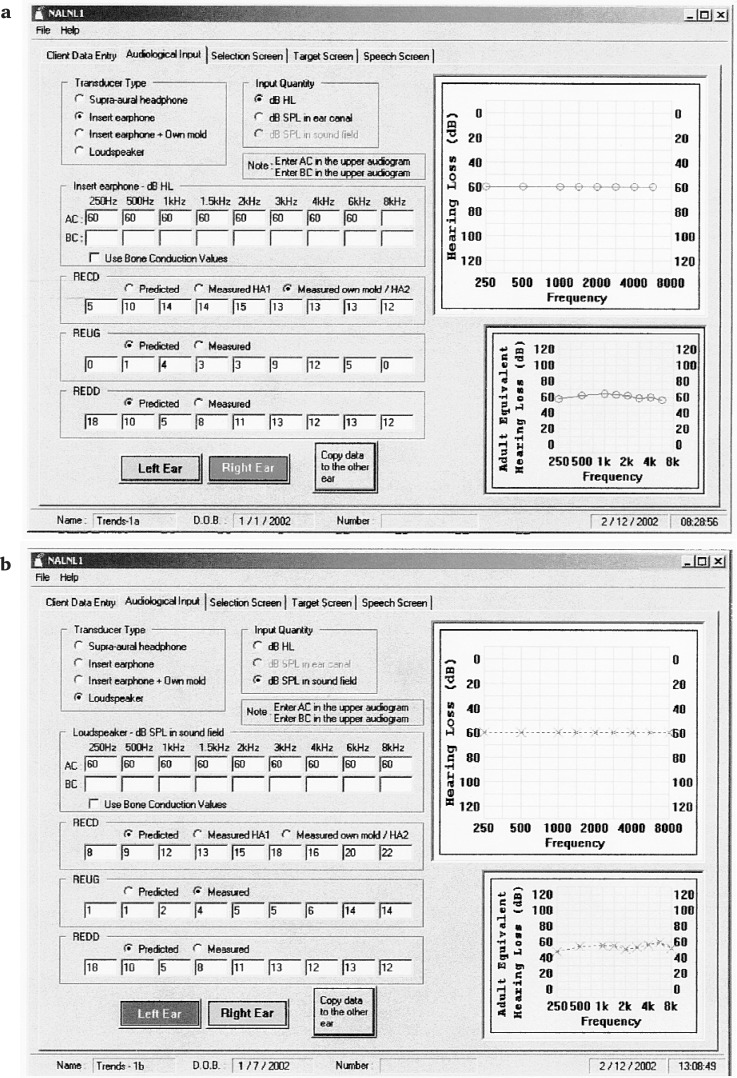
Automatic Calculation Using the NAL-NL1 Software If the NAL-NL1 (Dillon, 1999) software is used for selecting hearing aids, the calculation of adult-equivalent hearing loss is done automatically. In the Audiological Input screen, the audiologist selects the transducer and units used in measurement before entering the data, and the software uses a conventional audiogram format to display the adult-equivalent hearing loss. Figures 1a and b show the Audiological Input screens that display the adult-equivalent hearing loss for dial readings measured using insert earphones (Figure 1a), and sound pressure levels in the sound field measured using loudspeakers (Figure 1b).
Figure 1a.
The Audiological Input screen from the NAL-NL1 software system with the entered values in the top graph and the adult-equivalent hearing loss displayed in the bottom graph on each screen. Figure 1a shows thresholds measured with insert earphones and recorded as audiometer dial readings in dB HL. The child's real-ear-to-coupler difference (RECD) was also measured using insert earphones and custom earmolds, and was entered in the same screen by selecting Measured under RECD. Figure 1b shows thresholds measured with a loudspeaker in the sound field, and recorded as dB sound pressure level (SPL) in the sound field.
Discussion and Summary
For hearing assessment, we recommend that audiologists use insert earphones coupled with the individual's earmold, so that hearing loss for individual ears can be obtained for hearing aid fitting. As explained in the next section, the RECDindiv. measurement that is used to help interpret the threshold assessment will also facilitate the adjustment and verification of a hearing aid in the coupler (Moodie et al., 1994; Seewald et al., 1999). Conversely, measuring thresholds in the sound field makes it difficult to obtain thresholds for individual ears, or impossible when the loss is markedly asymmetrical. Also, accurate interpretation of sound field thresholds requires REUG to be measured, and this measurement is susceptible to effects of head and ear diffraction. Even though a control microphone can be used to minimize head diffraction effects, the child needs to remain relatively still during the measurement. This can be difficult with a young child. Further, retention of the probe in the ear canal is much easier for the RECD measurement than for the REUG measurement, as the earmold prevents the probe from moving and lessens the tickling effect of a loose probe tube in the ear canal.
We consider that the calculation and display of adult-equivalent hearing loss is accurate, understandable, and practical when applied in a clinical setting. It is accurate in that it uses individual acoustic transforms, rather than age-appropriate averages, to convert dial readings to adult-equivalent hearing loss. The representation is understandable in that it uses the standard audiogram notation familiar to clinicians. In practical terms, the conventional notation facilitates a consistent record of accurate changes in hearing thresholds over time, which is valuable for monitoring fluctuations in hearing loss and for counseling parents and teachers about the child's amplification needs. Adult-equivalent hearing loss can be easily calculated from audiometer dial readings by using the worksheet in Table 2, or obtained via the NAL-NL1 software system.
Prescribing Amplification for Children
What Type of Gain Should Be Prescribed for Children?
Marcoux and Hansen argue that children require a different gain prescription compared to an adult with a similar hearing loss. This is valid when it is assumed that hearing aid prescription is expressed in terms of real-ear insertion gain (REIG). An REIG procedure prescribes an increase in signal level at the eardrum relative to the level that would have been received unaided. The unaided sound pressure level (SPL) at the eardrum may be regarded as a combination of the SPL in the sound field (at the position of the eardrum but with the listener absent) plus the natural amplification provided by the sound collecting and resonance characteristics of the external ear. This “natural amplification,” or real-ear unaided gain, will vary from person to person and is highly frequency-dependent. When a hearing aid is fitted, the natural amplification of the ear is mostly lost, because the earmold will fill the concha. The ear canal, beyond the tip of the earmold, will be considerably shortened and its resonance changed from a quarter-wave to a half-wave resonance. Consequently, its main resonance is moved to a much higher frequency, probably beyond the effective range of the hearing aid. The result is that the difference between unaided and aided SPL (ie, the insertion gain) will vary from an adult to a child for the same hearing aid, and a major factor in this variation will be individual differences in the unaided ear-canal resonance.
The problem outlined above would not occur if the prescription were in terms of real-ear aided gain (REAG), that is, the increase in signal level when aided relative to the level in the sound field. A prescription that provides an REIG target can be easily converted into an REAG target by adding the adult-average real-ear unaided gain (REUGa.avg.) to the REIG values using the following equation:
| (5) |
Dillon (2001, chapter 4) gives a detailed discussion of this transform together with the equations.
For an REAG prescription, the corresponding coupler gain prescriptive targets are affected only by the difference between the coupler-measured and the real-ear gain. No corrections for individual ear canal resonance will be necessary. It therefore makes sense to use REAG targets for children and adults who have atypical ear canal resonances, such as those resulting from ear surgery. When selecting a hearing aid on the basis of the coupler gain that will provide the required real-ear aided gain, an accurate method is to use the RECD measured with the individual's own earmold and an insert earphone to derive the required coupler gain (CG) targets:
| (6) |
The NAL-NL1 software provides both REIG and REAG targets. The CG targets to achieve both types of real-ear targets are derived by using either individually measured RECD or age-appropriate average values. Ching et al. (2002) provide a practical guide to using the NAL-NL1 software for adjusting and verifying hearing aids accurately for children.
Measuring RECD: Calibration and Probe Placement
Procedures for measuring real-ear-to-coupler differences are well established (Moodie et al., 1994). Typically, RECD is measured using a real-ear analyzer, an insert earphone, and a probe microphone. The real-ear part of the measurement is carried out by connecting the insert earphone to the individual's earmold and tubing, and a probe microphone is inserted together with the earmold in the ear canal. A swept tone or broad band signal is used as the stimulus. The coupler part is carried out by connecting the insert phone to an HA2 2 cc coupler via 25 mm of tubing, and the probe microphone is inserted into the coupler for measurement. The RECD is the difference between the two measurements.
Calibration for RECD Measurement
Some real-ear analyzer systems, such as the Aurical, incorporate RECD measurement as a standard procedure. These systems use the coupler microphone for the coupler part of the measurement and the probe microphone for the real-ear part of the measurement. Because two different microphones are used, the resulting RECD measurement is accurate only if the two microphones are correctly calibrated with respect to each other. This can be checked by performing an RECD measurement using an “ear” and a coupler that are known to have exactly the same characteristics. In such a case, the RECD should be zero across all frequencies, and deviations from zero would indicate a calibration or a tubing problem. The process simply involves the use of the 2 cc coupler for both parts of the measurement rather than finding an ear canal that closely matches the volume of the 2 cc coupler. Prior to measurement, a small hole of about 1 mm in diameter needs to be drilled in the body of the coupler, and the probe tube is inserted through this hole.
During the real-ear part of the RECD measurement, the output transducer of the earphone is connected to the coupler, and the signal level is measured with the probe tube. Then the test-box measurement microphone is used in the usual manner to obtain the coupler part of the measurement. The small hole can be blocked with putty after the check. A protocol for this procedure can be found on the NAL website (www.nal.gov.au).
Probe Placement
The accuracy of RECD measurement is directly related to the insertion depth of the probe tube in the ear canal. For measurement errors within 2 dB up to 4 kHz, the probe tip needs to be within 9 mm of the eardrum (Dillon, 2001; p.93). Accurate positioning of the probe tip can be achieved using a 6-kHz notch method (Storey and Dillon, 2001; Sullivan, 1988). When a warble tone at 6 kHz is presented, a minimum will occur in the ear canal at a region 15 mm from the eardrum. This region can be located by smoothly inserting a probe tube into the ear canal while observing the probe-tube output display. By using the insertion depth for the 6-kHz minimum as a guide, the probe tip can be accurately positioned at 9 mm from the eardrum for measuring RECD (Dillon, 2001, pp. 91–94). This procedure requires only a few minutes and is practical in a clinical situation with infants and children. A less accurate but feasible option when the child is not compliant is to use a fixed age-appropriate insertion depth with otoscopic monitoring during insertion (Moodie et al., 1994). The recommended insertion depths past the inter-tragal notch are 15 mm for babies under 12 months, 20 mm for children between 1 and 5 years, and 25 mm for older children and adults.
REAG and CG Prescriptions for Children: Illustrative Case
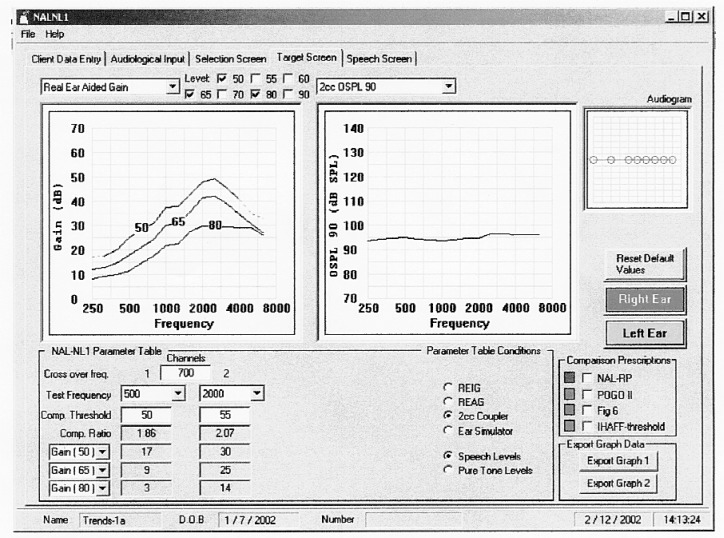
Figure 2 shows the Target screen from the NAL-NL1 software system illustrating the REAG and CG prescriptions for the 5-month-old child whose audiogram is represented in Figure 1a. The child's RECD was measured using insert earphones and custom earmolds and entered into the NAL-NL1 software. The REAG target curves for input levels of 50, 65, and 80 dB SPL appear in the left-hand graph, and the 2 cc OSPL 90 prescription in the right-hand graph. Below the graphs are the parameter tables, in this case for a two-channel hearing aid, showing the 2 cc coupler gain targets required to achieve the REAG targets for a broadband signal presented at different input levels together with the compression parameters.
Figure 2.
The NAL-NL1 software Target screen showing REAG prescription and 2 cc OSPL 90 prescription in the two graphs, together with parameter tables showing the 2 cc coupler gain targets corresponding to the REAG targets for a speech-weighted noise.
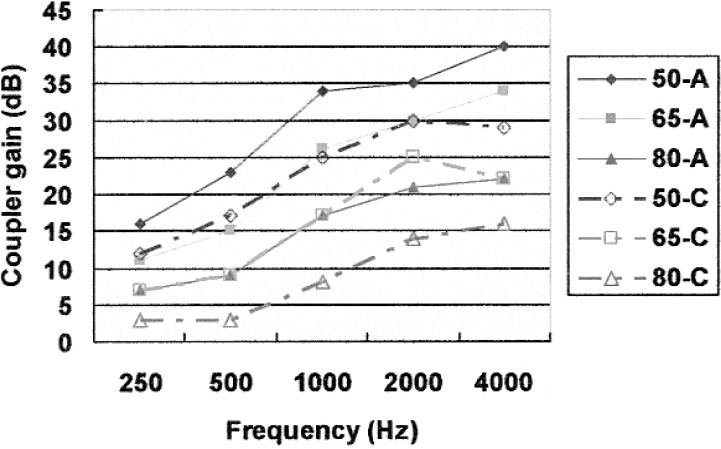
Figure 3 shows the NAL-NL1 coupler gain prescriptions for the child compared to an adult with the same adult-equivalent hearing loss. In the latter case, the adult average RECD values were used to derive the coupler gain targets.
Figure 3.
NAL-NL1 coupler gain targets corresponding to the REAG prescription for an average adult (solid line, filled symbols) and a 5-month-old child with individually measured RECD (broken line, open symbols) who have the same adult-equivalent hearing loss. Targets for input levels of 50, 65, and 80 dB SPL are displayed for the child (50-C, 65-C, 80-C) and for an average adult (50-A, 65-A, 80-A).
If a hearing-aid-fitting software system does not take into account an individual RECD in prescribing coupler gain targets, it is necessary to correct the targets by adding the difference between the RECDindiv and the RECDa.avg. to the standard coupler gain prescription.
Discussion and Summary
An REAG prescription specifies gain from the sound field to the eardrum. An REIG prescription specifies increase in SPL at the eardrum when aided, relative to the SPL at the eardrum when unaided. Hence, the individual's real-ear unaided gain has no effect on an REAG prescription, whereas it does affect the REIG prescription. As shown previously, an REIG target can be easily converted into an REAG target by adding the REUGa.avg. (Eq. 5). So, for an adult with a real-ear unaided gain close to REUGa.avg., it does not matter what type of gain is prescribed. The same is not true for a child whose ears have acoustic characteristics that are different from those of an average adult.
Are there any advantages in preserving the real-ear unaided gain of a young child when amplification is prescribed? Research on speech perception of infants and characteristics of infant-directed speech (Kuhl, 1992; Kuhl et al., 1997) does not suggest that infants take advantage of their superior sensitivity at the very high frequencies. It appears that the unique resonance characteristics of young children are an acoustical consequence of the physical size of a child compared to an adult. In practical terms, it is simpler to use an REAG prescription than an REIG prescription because it is not necessary to measure, or correct for, REUGindiv.. The coupler gains (CG) required to achieve an REAG prescription can be individualized if RECDindiv. values, which were measured using an insert earphone and a custom earmold, are available. The CG targets can be used to adjust and verify a hearing aid in a 2 cc coupler.
We have shown that the individualized coupler gain targets corresponding to an REAG prescription can be generated automatically using the NAL-NL1 software system once the hearing thresholds and individual RECD values are entered. If measured RECD values are not available, the software system uses age-appropriate values based on the individual's date of birth to calculate coupler gain targets.
Summary and Conclusions
The impact of ear canal acoustics of young children on determining thresholds and prescribing and verifying hearing aid performance has been examined with a view to providing practical solutions for the clinician. The following conclusions can be drawn:
Hearing thresholds that are measured using different transducers can be accurately represented in terms of adult-equivalent hearing loss. The preferred assessment method is to use an insert earphone together with the child's earmold. Audiometer dial readings or sound pressure levels in the ear canal can be converted into adult-equivalent hearing loss either by manual calculation using the worksheet provided, or by using the NAL-NL1 software system. The system includes options for entering thresholds measured using a range of transducers and displays the adult-equivalent hearing loss corresponding to the measurements entered in terms of dial readings or sound pressure levels.
An REAG prescription is preferred to an REIG prescription for young children, because the ear canal resonance has no effect on an REAG prescription and no measurement of REUG is required. The NAL-NL1 software system supports this approach and prescribes REAG targets and coupler gain targets that are customized using individually measured RECD values.
References
- ANSI S3.6 The American National Standards Institute S3.6 Specification for Audiometers, 1996
- Bentler RA, Pavlovic CV. Transfer functions and correction factors used in hearing aid evaluation and research. Ear and Hearing 10: 58–63, 1989 [DOI] [PubMed] [Google Scholar]
- Ching TYC. Selecting, verifying, and evaluating hearing aids for children. J Audiol Medicine, in press, 2003 [Google Scholar]
- Ching TYC, Britton L, Dillon H, Agung K. NAL-NL1, RECD & REAG: Accurate and practical methods for fitting non-linear hearing aids to infants and children. The Hearing Review 9(8):12–20, 52, 2002 [Google Scholar]
- Dillon H. NAL-NL1: A new procedure for fitting non-linear hearing aids. Hearing Journal 52(4):10–16, 1999 [Google Scholar]
- Dillon H. Hearing Aids. New York City: Thieme, 2001 [Google Scholar]
- Kuhl PK. Infants' perception and representation of speech: Development of a new theory. In Proceedings of the International Conference on Spoken Language Processing, (eds.) Ohala, et al. University of Alberta Press, Edmonton, pp. 449–456, 1992 [Google Scholar]
- Kuhl PK, Andruski JE, Chistovich IA, Chistovich LA, Kozhevnikova EV, Ryskina VL, Stolyarova EI, Sundberg U, Lacerda F. Cross-language analysis of phonetic units in language addressed to infants. Science 277: 684–686, 1997 [DOI] [PubMed] [Google Scholar]
- Kruger B. An update on the external ear resonance in infants and young children. Ear and Hearing 8(6):333–336, 1987 [DOI] [PubMed] [Google Scholar]
- Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics 106(3):E43, 2000 [DOI] [PubMed] [Google Scholar]
- Moodie KS, Seewald RC, Sinclair ST, Scollie S. Procedure for predicting real-ear hearing aid performance in young children. Am J Audiol 3(1):23–31, 1994 [Google Scholar]
- Sachs RM, Burkhard MD. Zwislocki coupler evaluation with insert earphones. Report no.20022-1, Knowles Electronics Inc., Illinois, 1972
- Seewald RC, Scollie SD. Infants are not average adults: Implications for audiometric testing. The Hearing Journal 52(10):64–72, 1999 [Google Scholar]
- Seewald RC, Moodie KS, Sinclair ST, Scollie SD. Predictive validity of a procedure for pediatric hearing instrument fitting. Am J Audiol 8: 143–152, 1999 [DOI] [PubMed] [Google Scholar]
- Storey L, Dillon H. Estimating the location of probe microphones relative to the tympanic membrane. J Am Acad Audiol 12(3):150–154, 2001 [PubMed] [Google Scholar]
- Sullivan RF. Probe tube microphone placement near the tympanic membrane. Hearing Instruments, 39(7), 1988 [Google Scholar]
- Yoshinaga-Itano C, Sedey AL, Coulter DK, Mehl AL. Language of early- and later-identified chidlren with hearing loss. Pediatrics 102(5):1161–1171, 1998 [DOI] [PubMed] [Google Scholar]