Abstract
Hearing instrument fitting with infants and young children differs in several important ways relative to the fitting process with adults. In developing the Desired Sensation Level method, we have attempted to account for those factors that are uniquely associated with pediatric hearing instrument fitting. Within this article we describe how the external ear acoustics of infants and young children have been systematically accounted for in developing the Desired Sensation Level method. Specific evidence-based procedures that can be applied with infants and young children for the purposes of audiometric assessment, electroacoustic selection, and verification of hearing instrument performance are described.
Introduction
It is now possible to identify hearing loss in early infancy. Consequently, early hearing detection and intervention programs are being implemented worldwide. It is a generally accepted goal of such programs to enroll infants in comprehensive and effective family-centered intervention programs by 6 months of age. A second recent development in the hearing health care field relates to the availability of a new generation of fully digital hearing instruments. These new hearing aids embody a remarkable array of capabilities and options. However, a real challenge to professionals working with these early-diagnosed infants is to know how to achieve the best match between the unique auditory characteristics of each infant and the advanced and relatively complex capabilities that are now available in modern digital hearing instruments. Without the application of scientifically based approaches to fitting, it is possible for a hearing aid fitting to be well off the mark. An unfortunate consequence of an inaccurate fitting is to lose the developmental advantages in auditory learning that result from early identification.
Our clinical research program in pediatric hearing aid fitting has evolved from the innovative approaches to pediatric hearing aid fitting that emerged in the 1970s (Byrne and Fifield, 1974; Erber, 1973; Gengel, Pascoe and Shore, 1971; Erber, 1973; Ross, 1975) and is based on the premise that the process of fitting amplification in infants and young children differs in several important ways relative to the fitting of hearing aids in adults. This has led to the development and evaluation of child-friendly protocols for the selection and verification of hearing aids aimed at ensuring the consistent provision of audibility of speech (Bagatto, 2001; Bagatto et al., 2002; Gagné et al., 1991a and 1991b; Moodie et al., 1994 and 2000; Scollie and Seewald, 2002a and 2002b; Scollie et al., 1998; Seewald et al., 1993, 1996, 1997, and 1999; Sinclair et al., 1996; Stelmachowicz et al., 1998; Seewald and Scollie, 1999; Zelisko et al., 1992). Within this paper we will consider the major points Marcoux and Hansen (this issue) discuss relative to the procedures we have developed and implemented within the Desired Sensation Level (DSL) method for pediatric hearing instrument fitting.
Audiometric Considerations
One of the major issues Marcoux and Hansen raise relates to the validity of audiometric data that is used for prescribing hearing instrument performance in infants and young children. Marcoux and Hansen observe that most infants have smaller external ears than most adults and conclude that this fact has implications for both audiometric assessment and the electroacoustic fitting of hearing instruments in infants. They also observe that prescriptive approaches to hearing instrument fitting calculate the desired electroacoustic performance characteristics for an individual on the basis of audiometric threshold values, typically defined in dB HL. Thus, as they correctly point out, the appropriateness of the prescription is directly linked to the validity of the threshold estimates that are applied within the prescriptive process.
Marcoux and Hansen conclude that the validity of audiometric data collected in dB HL in infants and young children is open to question, particularly for the purposes of hearing instrument prescription and fitting. We certainly agree with this conclusion. In fact, in our paper entitled “Infants are not Average Adults: Implications for Audiometric Testing” (Seewald and Scollie, 1999) we discussed the very same concerns regarding the use of the dB HL reference in pediatric testing.
In routine clinical practice, it is assumed that when any of the standard signal transducers (ie, sound field loudspeaker, TDH-series earphone, and insert earphone) are used to measure hearing sensitivity, the results, expressed in dB HL, will be equivalent regardless of the signal transducer used in the testing. This assumption generally holds in the audiometric testing of adult listeners because the reference equivalent threshold SPLs (RETSPLs) for the sound field, supra-aural, and insert earphone conditions have been derived from group data collected with normal adult subjects. However, when hearing is measured in dB HL, equivalence across audiometric conditions (ie, signal transducers) cannot be assumed in the testing of infants and young children (Seewald and Scollie, 1999).
This problem can be explained by what is known about the transfer of sound from audiometric signal transducer to the eardrum of infants and young children (Feigin et al., 1989; Kruger, 1987; Lewis and Stelmachowicz, 1993). When hearing sensitivity is measured in dB HL, the audiometric calibration includes average adult ear canal resonance: this assumes that we are testing an individual who has the physical characteristics of the “average adult.” Unfortunately, because of head size and external ear geometry, this assumption is violated in the testing of infants and young children. Consequently, in the audiometric testing of infants and young children, different hearing level estimates will be obtained depending on which signal transducer is used to perform the test (Seewald and Scollie, 1999).
Marcoux and Hansen have illustrated this problem graphically in Figure 1, a figure that they have adapted from our earlier publication (Seewald and Scollie, 1999). Furthermore, on the basis of available data (Bagatto et al., 2002; Feigin et al., 1989; Kruger, 1987; Lewis and Stelmachowicz, 1993), it can be predicted that the magnitude of these “signal transducer effects” increases inversely with age. For example, we would predict greater differences in hearing levels measured across the three signal transducers for a 7-month-old infant relative to those obtained for an 18-month-old child.
Figure 1.
Illustration of how audiometric thresholds, measured in dB HL, are transformed in the DSL®[i/o] v4.1 software system to predict the ear canal level in dB SPL. When possible, infant-specific RECD values are applied in the transformation process.
As Dillon (2001) has recently observed, this problem has two equally effective solutions and both have been implemented within the DSL software systems for the past decade (Seewald et al., 1993 and 1997). The first solution is to express audiometric measures in dB SPL in the ear canal, rather than using dB HL. The second is to correct for the difference in external ear acoustics between the infants and the “average adult” and to apply this correction in predicting the hearing threshold level that an average adult would have if the adult had the same threshold in dB SPL at the eardrum as the infant (Dillon, 2001). These corrected hearing levels are referred to as “predicted hearing levels” (HLp) within the DSL software systems (Seewald et al., 1993 and 1997) and as “equivalent adult hearing levels” in the NAL-NL1 procedure (Dillon, 1999; also see Ching and Dillon, this issue). For reasons they describe in some detail, Marcoux and Hansen express a preference for the second of these two options.
Expressing Thresholds in dB SPL in the Ear Canal
Over the years, many have asked why we have recommended that audiometric variables be defined in dB SPL in the ear canal. One reason is contained within the preceding discussion regarding the invalidity of dB HL measures for pediatric applications. By expressing audiometric variables in dB SPL in the ear canal, the problems associated with average adult-referenced HL measures are resolved. As we have stated elsewhere (Seewald and Scollie, 1999), the SPL at the eardrum required to hear a given test signal will be the same regardless of the transducer that is used to deliver the signal. Thus, the problem described by Marcoux and Hansen can be eliminated by simply moving to a different point of reference in expressing auditory threshold values (ie, dB SPL in the ear canal). In addition to solving this problem, a further advantage of defining audiometric variables in dB SPL, and plotting them in the SPLogram format, is that the important interrelationships among hearing and hearing instrument performance variables can be studied and evaluated (Scollie and Seewald, 2002a; Seewald et al., 1996). Within the following section, we describe how this approach to audiometric variable definition is implemented within the current version of the DSL®[i/o] software system (Seewald et al., 1997).
Assessment Procedures
For the reasons discussed to this point, it is important to know which of the alternative signal transducers has been used in audiometric assessment. Consequently, the DSL software system requires that the transducer used in testing be specified. Figure 2 shows the pull-down menu for Assessment. The clinician uses the menu to indicate which of the alternative signal transducers has been used in audiometry. Note that the options include the ER-3A insert earphone, TDH-series headphones, and the sound field loudspeaker located at 0°, 45°, or 90° azimuth. This menu displays two additional options. It is also possible to measure hearing using the infant's custom earmold coupled to an insert earphone, or to make direct SPL measures, using a probe microphone, of the ear canal level during audiometric testing (ie, real-ear SPL). Consequently, menu choices are available to support the implementation of these two measurement options.
Figure 2.
Pull-down menu from the DSL®[i/o] v4.1 software system for selecting the transducer type used in audiometric testing.
As shown in Figure 3, the software system also requires information regarding which HL to SPL transform to apply to the entered audiometric data. If the clinician selects the “predicted” option, the software retrieves and applies a set of average age-appropriate values to transform the entered dB HL values to dB SPL in the ear canal. However, the clinician also has the option to measure the appropriate transform (ie, real-ear to coupler difference [RECD], real-ear unaided response [REUR], real-ear to dial difference [REDD]) for the transducer used in the audiometric testing. Several years ago, we reported data that address the predictive validity of this approach to transforming audiometric data from HL to ear canal SPL (Scollie et al., 1998).
Figure 3.
Pull-down menu from the DSL®[i/o] v4.1 software system for selecting the HL to SPL transform to be applied to the audiometric data.
As we have stated elsewhere (Seewald and Scollie, 1999), regardless of whether an electrophysiologic or behavioral method is used in threshold estimation with infants, we recommend the use of an insert earphone for audiometry, whenever possible. Because the insert earphone is calibrated in a 2 cc coupler, the coupler SPL is known for any dB HL attenuator setting on the audiometer. The insert earphone is also used to measure the infant's RECD values across frequencies. Thus, it is possible to simply add the RECD values to the 2 cc coupler levels for threshold to derive a prediction of the ear canal level at threshold for the infant. The process for predicting the ear canal SPL at threshold is illustrated in Figure 1.
For the purposes of clinical implementation, this approach to expressing audiometric thresholds can be facilitated by having the software system keep track of the necessary details and perform the required computational work. In clinical practice, we would need to perform two measurements. First, we would measure the infant's thresholds using an insert earphone and record the dB HL values across frequencies. Second, we would measure the infant's RECD according to the procedures described by Moodie et al. (1994). As shown in Figure 4, the dB HL and RECD values are entered into the software system. Once these values have been entered, the software has all of the information it needs to calculate the predicted ear canal SPL thresholds for the infant. In the DSL method, these ear canal SPL thresholds are used for computing the prescriptive targets for amplification, rather than the HL thresholds.
Figure 4.
Assessment data entry window from the DSL®[i/o] v4.1 software system.
When this approach to defining audiometric measures is taken, the acoustic transform applied in the prediction of ear canal SPL at threshold is not derived from adult data. Rather, it is individualized for the infant under consideration. This more individualized approach to threshold definition has been fully implemented for routine clinical practice in several contemporary hearing instrument fitting systems (Cole and Sinclair, 1998; Dillon, 1999; Seewald et al., 1993 and 1997; Stelmachowicz et al., 1994) and was developed specifically to deal with the concerns Marcoux and Hansen discussed.
Predicted Hearing Levels
For a number of reasons, Marcoux and Hansen argue against expressing audiometric variables in dB SPL (ear canal level) and in favor of what Dillon (2001) calls the “equivalent adult hearing level.” According to Dillon (2001), the threshold (in decibels equivalent adult hearing level) is “the hearing threshold level that an average adult would have if the adult had the same threshold in dB SPL at the eardrum as the child.” According to Marcoux and Hansen, the main advantage of the equivalent adult hearing level is that it provides for a direct comparison between the audiometric data of a child and that of a normally hearing adult.
Under certain specific conditions, this concept has been implemented in the DSL software system for the past decade (Seewald et al., 1993) and is described in detail in Seewald and Scollie (1999). Briefly, in the fitting of behind-the-ear instruments on infants and young children, we recommend that, whenever possible, the thresholds be measured using an insert earphone with the infant's custom earmold. Technically speaking, this approach violates the assumptions for measuring hearing in dB HL using insert earphones. This is because custom earmolds will typically have greater tubing length than the standard foam tip coupling of an insert earphone. The acoustic effect of the increased tubing length is a high-frequency roll-off for the custom mold relative to the response that is measured for the standard foam tip coupling (Bagatto et al., 2002). Consequently, when thresholds have been measured using an insert receiver with the custom earmold, we have departed from the assumptions for dB HL measures (Seewald and Scollie, 1999). However, many clinicians wish to report the test findings in dB HL. Recognizing this need, we developed and have implemented the following solution in the DSL software systems (Seewald et al., 1993 and 1997).
In our recommended protocol for fitting amplification in infants, both thresholds and RECDs are measured with the infant's custom earmold coupled to an insert earphone. The RECD measure (ie, customized transform) captures the unique acoustic signature of the custom earmold. The DSL software corrects for the acoustic difference between the infant's RECD with the custom earmold and the average adult RECD measured with a standard foam tip. This correction factor is then applied to the measured threshold values in deriving a set of predicted HL values (HLp; also called “equivalent adult hearing level”, Dillon, 2001). These HLp values are reported in the Auditory Area window of the DSL software system (see Figure 5). Note that the Auditory Area window also provides the user with the predicted ear canal SPLs at threshold across frequencies. The HLp values can then be transferred to a conventional audiogram and provide an estimate of an infant's HL thresholds over time and are not influenced by changes in external ear geometry. Thus, in summary, the DSL software system provides the clinician with threshold estimates both in dB SPL (ear canal level) and, under specific measurement conditions, in predicted HL (HLp).
Figure 5.
The Auditory Area window from the DSL®[i/o] v4.1 software system. Values are shown for the predicted HL (HLp) thresholds in addition to the predicted ear canal SPL values.
As shown in Figure 6, the results of data entry (ie, thresholds and RECDs) and data transformation can be plotted graphically in the DSL®[i/o] v4.1 software system. Specifically, this graph shows (from bottom to top), average normal hearing sensitivity (ie, minimum audible pressure [MAP]), the child's predicted thresholds across frequencies, and the predicted upper limit of comfort in dB SPL (ear canal level) as a function of frequency. The DSL[i/o] algorithm uses the threshold values shown in this figure to select a set of hearing instrument electroacoustic characteristics for this child.
Figure 6.
SPLogram from the DSL®[i/o] v4.1 software system showing (from bottom to top) average normal hearing sensitivity (MAP) [▿-▿], the child's thresholds [□-□] and the predicted upper limit of comfort [▪-▪] in dB SPL (ear canal level) as a function of frequency.
From our perspective, an important limitation of the approach advocated by Marcoux and Hansen (ie, use of HLp only) is that it creates the quintessential “apples and oranges” problem where audiometric data are expressed using one metric (dB HL) with hearing instrument performance measures expressed using another (dB SPL). An important goal of pediatric hearing instrument fitting is to ensure that we have achieved a good match between the amplification characteristics of hearing instruments and the auditory characteristics of infants and young children so that the use of residual auditory capacity can be maximized. When the metrics used for expressing hearing instrument performance characteristics and an infant's auditory characteristics are different (ie, dB HL and dB SPL), it is difficult, if not impossible, to know about the important interrelationships between these two sets of variables. If one is willing to depart from adult referenced audiometric values, the relative advantages of using a common point of reference (ie, ear canal SPL) to define all relevant audiometric and electroacoustic variables can be realized.
Specification of Desired Hearing Instrument Performance
The second major issue that Marcoux and Hansen tackle in their article addresses the specification of electroacoustic performance criteria for fitting infants and young children with amplification. They state the problem by observing that, “A hearing aid which is set to give a certain amount of output/gain in the ear of an adult person will typically produce a higher output level in the ear canal of a child, just because of the smaller dimensions of the child's ear canal.” This, of course, is not a recently identified problem. We agree that external ear acoustics must be systematically accounted for in electroacoustic selection for infants and have developed and evaluated procedures that directly deal with these concerns (Bagatto, 2001; Bagatto et al., 2002; Moodie et al., 1994 and 2000; Seewald et al., 1999; Sinclair et al., 1996).
Acoustic Transforms in Hearing Instrument Fitting
The problem that Marcoux and Hansen discuss is that, in the electroacoustic selection stage of the fitting process, we are interested in specifying the levels of sound in two different locations (ie, the 2 cc coupler and the infant's occluded ear canal). The application of appropriate acoustic transforms can assist the clinician to answer the following important questions both at the selection and verification stages of the fitting process:
Selection: If I know (have specified) the levels of amplified sound that I want to deliver into an infant's ear canal (for a given set of inputs), what are the equivalent levels of sound that I want to measure in a 2 cc coupler?
Verification: If I know (have measured) the levels of amplified sound in a 2 cc coupler (for a given set of inputs), what levels of amplified sound will be delivered into the occluded ear canal of the infant by this hearing instrument?
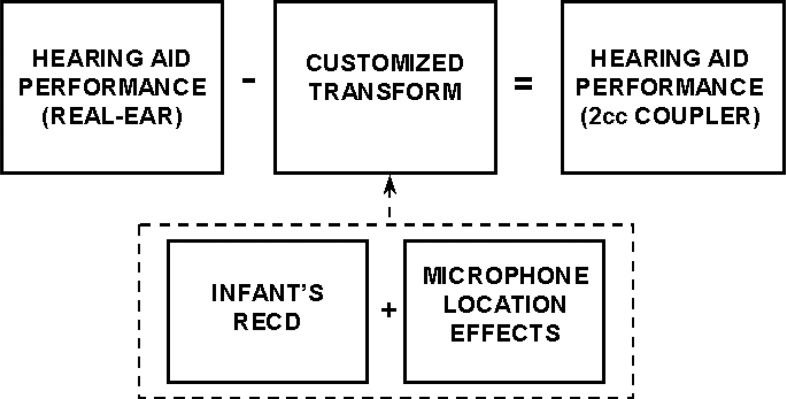
The general application of acoustic transforms in the hearing instrument fitting process is illustrated in Figure 7. The variables that comprise the transform depend on the variable under consideration (eg, real-ear aided response for a 90 dB narrowband input signal [REAR-90], real-ear aided gain or output for a speech-level input [REAG or REAR]) as well as the type of instrument to be fitted (eg, behind-the-ear, completely-in-the-canal). However, once the variables are known, it is possible to accurately transform electroacoustic variables between these two locations of interest with ease. Within the following section we describe how the issues raised by Marcoux and Hansen are resolved, rather simply, through the application of acoustic transforms within the DSL method.
Figure 7.
Illustration showing the general application of acoustic transforms in the hearing instrument selection and fitting process.
Electroacoustic Selection Procedures
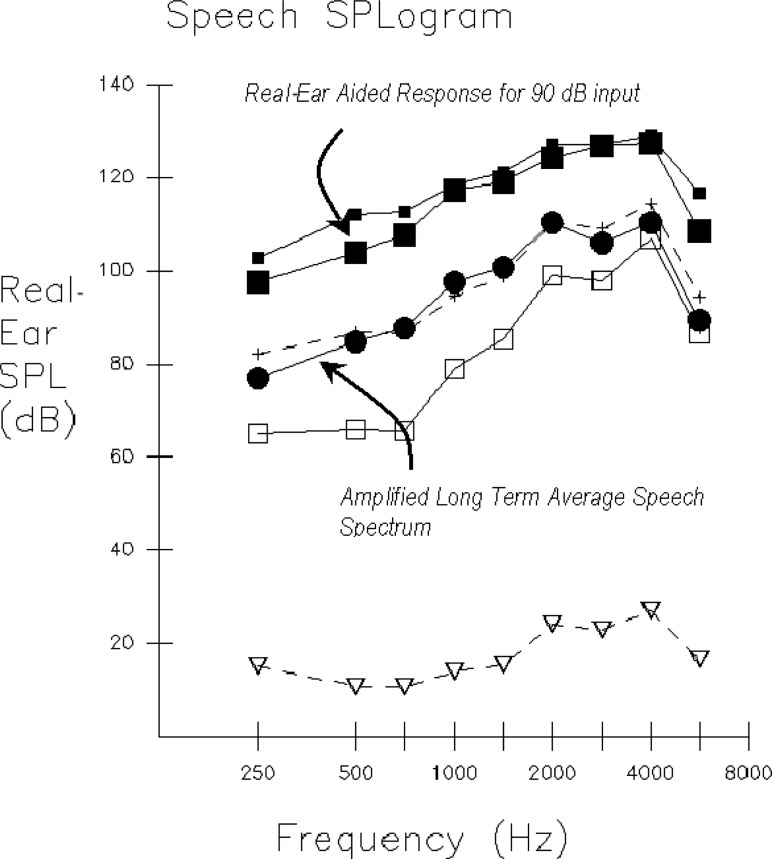
Recall that the threshold estimates for the infant or young child in dB SPL (ear canal level) are used by the DSL[i/o] algorithm to calculate targets for hearing aid performance. We have plotted the results of this process in Figure 8 for this example. Note that, in addition to the child's thresholds, the graph shows a set of target values for the amplified long-term average speech spectrum (LTASS) and target levels for limiting hearing instrument output. All variables shown in this figure are plotted in dB SPL (ear canal level) as a function of frequency. When fitting wide dynamic range compression instruments, the software also produces target values for low-level and high-level speech inputs. Note that at this point in the process, we have defined the electroacoustic performance criteria for the child in terms of the REAR and the REAR-90 with both variables expressed in dB SPL (ear canal level). By subtracting the assumed speech input levels, it is also possible to define the desired response characteristics in terms of the real-ear aided gain (REAG) as a function of frequency.
Figure 8.
SPLogram from the DSL®[i/o] v4.1 software system showing (from bottom to top) average normal hearing sensitivity (MAP) [▿- ▿], the child's thresholds [□-□], the targets for the amplified long term average speech spectrum (LTASS) [+-+], and the predicted upper limit of comfort [▪-▪] in dB SPL (ear canal level) as a function of frequency.
At this stage in the fitting process, it is helpful to redefine the desired hearing instrument performance characteristics in terms of the equivalent 2 cc coupler levels. This facilitates hearing instrument selection from manufacturers' specifications and subsequently facilitates the process of verifying hearing instrument performance. Figure 9 illustrates how the DSL software system transforms the desired hearing instrument performance characteristics from the real-ear values to the 2 cc coupler. It can be seen in this figure that the appropriate acoustic transform is subtracted from the real-ear values to derive a set of 2 cc coupler target values. Two variables comprise the transform that is applied, including the head diffraction/microphone location effect and the RECD, for converting the target values from the real-ear aided response (or real-ear aided gain) to the 2 cc coupler. Whenever possible, the infant/child's RECD measured with the custom earmold is applied. In this way, the acoustic properties of the infant/child's occluded external ear have been accounted for within the electroacoustic selection process. If an RECD measurement has not been obtained, the software system applies a set of age-appropriate values (Bagatto et al., 2002). However, in view of the relatively large variability in RECDs between subjects within the infant population, it is recommended that individual RECD measurements be obtained whenever possible (Bagatto et al., 2002).
Figure 9.
Illustration of the process of transforming the desired real-ear hearing instrument performance characteristics from the real-ear to the 2 cc coupler.
The end result of the real-ear value to 2 cc coupler transformation is shown in Figure 10. This figure, from the Hearing Instrument Specification Window of the DSL®[i/o] v4.1 software system, provides the clinician with 2 cc coupler values for the prescribed output sound pressure level for a 90 dB input (OSPL90), full-on gain, gain at user settings and compression ratios as a function of frequency. We have derived this information by entering the child's thresholds, RECDs, and the type of instrument to be fitted into the software. By using the child's RECD, preferably measured with the custom earmold, we have accounted for the unique acoustic characteristics of the child's occluded ear canal.
Figure 10.
The Hearing Instrument Specification window from the DSL®[i/o] v4.1 software system. Values are shown for the prescribed 2 cc coupler saturation sound pressure levels, full-on gain, user gain, and compression ratios across frequencies.
In their article, Marcoux and Hansen correctly observe that the real-ear unaided gain (REUG) in infants and young children does not approximate average adult values (Kruger, 1987). This creates a problem when insertion gain procedures are used with children. The average adult REUG is typically used in computing hearing aid targets, while individual REUG measures are used during probe microphone verification. This mismatch poses rather large potential errors for the pediatric population (Scollie and Seewald, 2002a).
As a solution to this problem, Marcoux and Hansen propose the concept of insertion gain for (pediatric) restored output (IGRO). They define IGRO as the insertion gain that the hearing aid needs to produce for a child in order to give the same “restored” output sound pressure level at the eardrum in the child as would be measured at the eardrum of an average adult with the hearing aid set to the corresponding equivalent adult insertion gain. This is an accurate solution to the specific problem of generating accurate prescriptive targets for hearing aid performance.
We, however, see two potential areas for concern. First, few pediatric audiologists perform real-ear measures of hearing aid performance with infants and young children (Arehart et al., 1998; Hedley-Williams et al., 1996). This is not entirely surprising, because it is unrealistic to expect young children to sit still and face a loudspeaker for repeated real-ear measurements. Second, with this population, we need to minimize the number of different measurements required to proceed efficiently through the fitting process. The child's measured REUG cannot be used in transforming any audiometric data from TDH or insert phone testing. Recommendations suggest that we use these transducers, rather than testing in sound field, to obtain ear-specific assessment data prior to hearing aid fitting (Pediatric Working Group, 1996). Maximum clinical utility is obtained by choosing a transducer and transform combination that may be used for both audiometric and hearing aid transforms. In all cases, this is the insert earphone. The rationale for this statement is discussed in further detail below.
Verification of Hearing Instrument Performance
The primary aim of the verification stage of the fitting process is to determine the extent to which real-ear hearing instrument performance corresponds to the desired characteristics that have been selected for a given infant or young child. The specific verification procedures that are applied clinically will depend on how the desired performance characteristics have been specified (eg, REIR, REAR) as well as the capabilities and characteristics of the infant or young child to be fitted.
In our view, the verification of hearing instrument performance is critical in the pediatric hearing instrument fitting process. As one of us recently stated “… whether it be an ear trumpet, an analog or a high-end digital instrument, it is the audiologist who is ultimately responsible for the appropriateness and accuracy of the hearing instrument fitting. The responsible audiologist wants to know as much as possible about the levels of sound that are delivered into the ears of infants and young children. To this end, the audiologist must apply comprehensive, evidence-based verification strategies that are compatible with the characteristics and capabilities of this unique population,” (Seewald, 2001). We will conclude by describing the procedures we routinely use and recommend for verifying hearing instrument performance with infants and young children.
DSL Software Implementation: Verification Procedures
For reasons we have described elsewhere (Scollie and Seewald, 2002a—see also Ching and Dillon, this issue), we abandoned the routine use of conventional insertion gain measures with infants and young children some years ago. Subsequently, we developed and have validated an alternative approach to hearing instrument verification specifically for pediatric applications (Moodie et al., 1994; Seewald et al., 1999).
Over the years, this verification procedure has been called either “coupler-based” or a “simulated real-ear” approach to electroacoustic verification. In essence, an appropriate acoustic transform that incorporates the infant/child's measured RECD is used to convert the results of electroacoustic measurements obtained in the 2 cc coupler in predicting the real-ear equivalents. This process is illustrated graphically in Figure 11. Note that the acoustic transform is now added to the 2 cc coupler-based performance measures to predict how the hearing instrument will perform when fitted to the ear of the infant or young child. Also note that when the infant/child's RECD has been measured with the custom earmold, the transform that is applied has been individualized for the infant being fitted.
Figure 11.
Illustration of the process of transforming the measured 2 cc coupler performance of a hearing instrument to predict how the instrument will perform when fitted to the ear of an infant or young child.
Our research has shown this approach to electroacoustic verification has very high predictive validity (Seewald et al., 1999) and offers several advantages relative to alternative procedures. First, the variability associated with conventional sound field probe-microphone measures is eliminated. Second, electroacoustic performance is measured under the highly controlled acoustic condition of the hearing instrument test chamber. Finally, the infant or child need not be present for the often-lengthy electroacoustic fine-tuning process. This significantly reduces the amount of measurement-related time that the infant or child needs to spend in the fitting process.
When this method is used, the steps in the verification process are as follows. First, a hearing instrument is selected which should provide a good match to the desired electroacoustic characteristics. Second, all electroacoustic response shaping is performed within the hearing instrument test chamber until the best match to desired performance is obtained. Third, the 2 cc coupler's performance at the final settings for both gain and maximum output is entered into the DSL software system. Finally, the software transforms the 2 cc coupler-based measures to predict how the hearing instrument will perform when fitted to the infant's ear. The end result of this process is illustrated in the SPLogram shown in Figure 12. This graphic presentation allows the clinician to compare the predicted performance of the instrument to the desired or target values. Note that, because a common reference is used (ie, dB SPL in the ear canal), one can directly study the predicted hearing instrument performance relative to the threshold estimates that were entered into the software at an earlier stage in the process. It is not possible to perform this type of comparison using insertion gain data. The same approach to hearing instrument verification (ie, simulated real-ear) is now fully implemented on several commercially available hearing instrument testing systems.
Figure 12.
SPLogram from the DSL®[i/o] v4.1 software system showing (from bottom to top) average normal hearing sensitivity (MAP) [▿-▿], the child's thresholds [□-□], the targets [+-+] and hearing aid responses [•-•] for the amplified long term average speech spectrum (LTASS), and the predicted upper limit of comfort [▪-▪] and the predicted corresponding Real-Ear Aided Response for a 90 dB input [▪-▪] in dB SPL (ear canal level) as a function of frequency.
The verification stage is essential for ensuring that consistent audibility is provided to all children. In the current clinical environment, it is becoming more common to automatically fit digital and programmable hearing aids to the manufacturer's recommended settings, without measuring the actual hearing instrument's performance. This fitting strategy can create a fitting that provides less audibility for speech than the clinician intended (Lewis et al., 2002). This is as great a concern to us as any of the assessment and specification concerns discussed in this issue.
To illustrate, we have compared the hearing aid responses from three digital hearing aids if fitted to one manufacturer's algorithm versus those from the DSL [i/o] (Seewald et al., 1997) and NAL-NL1 (National Acoustic Laboratories, 2002) methods. In all cases, the hearing aids have been fitted for a flat 50 dB HL audiogram, using wide dynamic range compression circuitry. We summarized the speech audibility across conditions by computing the speech intelligibility index (SII) resulting from each fitting, for soft, average, and loud speech inputs (American National Standards Institute, 1997). The SII value ranges from 0 to 1, and represents the amount of the speech envelope that is audible to the listener. Figure 13 shows that, particularly for low-level speech, the various fitting procedures produce SII values that vary by greater than 30%. These inconsistencies are large enough that behavioral differences may result, particularly for low-level speech signals. Assuming that the goal of hearing aid fitting is to ensure consistent audibility across listening conditions, the effects of choosing different prescriptive goals must be considered. Further, verification that these goals have been achieved is essential.
Figure 13.
Speech intelligibility index values for five hearing aid prescriptions, as a function of input level. All hearing aids were programmed assuming a flat 50 dB HL audiogram and using wide-dynamic range compression circuitry.
Summary Statement
At present, the fitting software provided by some hearing instrument manufacturers does not account for the pediatric-specific issues that Marcoux and Hansen discuss. Consequently, when working with young infants in particular, one cannot assume an accurate fitting by simply entering dB HL threshold values into the software and selecting the “quick fit” function. Marcoux and Hansen have raised several important issues in their article and we are pleased to see serious concerns for these issues expressed by a manufacturer of hearing instruments. In our view, all who are involved in the delivery of hearing health care to infants and young children, including clinicians, researchers, and hearing instrument manufacturers, need to work cooperatively toward the development and uniform application of effective, evidence-based strategies in this important work. Ultimately, this should be the goal of our collective efforts. The long-term implications of the fitting decisions we make are too important for anything less.
References
- Arehart KH, Yoshinaga-Itano C, Thompson V, Gabbard SA, Brown A. State of the states: The status of universal newborn hearing identification and intervention systems in 16 states. Am J Audiol 7(2):101–114, 1998 [DOI] [PubMed] [Google Scholar]
- American National Standards Institute Methods for calculation of the Speech Intelligibility Index, ANSI S3.5–1997. New York: Acoustical Society of America; 1997 [Google Scholar]
- Bagatto MP. Optimizing your RECD measurements. Hear J 54:32, 34–36, 2001 [Google Scholar]
- Bagatto MP, Scollie SD, Seewald RC, Moodie KS, Hoover BM. Real-ear-to-coupler difference predictions as a function of age for two coupling procedures. J Am Acad Audiol 13(8):407–415, 2002 [PubMed] [Google Scholar]
- Byrne D, Fifield D. Evaluation of hearing aid fitting for infants. Brit J Audiol 8: 47–54, 1974 [Google Scholar]
- Cole WA, Sinclair ST. The Audioscan RM500 Speech-map/DSL fitting system. Trends Ampl 3(4):125–139, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon H. NAL-NL1: A new prescriptive fitting procedure for non-linear hearing aids. Hear J 52(4):10–16, 1999 [Google Scholar]
- Dillon H. Hearing Aids. New York. Thieme. pp. 407–408, 2001
- Erber NP. Body-baffle and real-ear effects in the selection of hearing aids for deaf children. J Speech Hear Dis 38: 224–231, 1973 [DOI] [PubMed] [Google Scholar]
- Feigin JA, Kopun JG, Stelmachowicz PG, Gorga MP. Probe-tube microphone measures of ear-canal sound pressure levels in infants and children. Ear Hear 10(4):23–29, 1989 [DOI] [PubMed] [Google Scholar]
- Gagné JP, Seewald RC, Zelisko DL, Hudson SP. Procedure for defining the auditory area of hearing-impaired adolescents with severe/profound hearing loss. I: Detection thresholds J Speech Lang Pathol Aud 12: 13–20, 1991a [Google Scholar]
- Gagné JP, Seewald RC, Zelisko DL, Hudson SP. Procedure for defining the auditory area of hearing-impaired adolescents with severe/profound hearing loss. II: Loudness discomfort levels J Speech Lang Pathol Aud 12: 27–32, 1991b [Google Scholar]
- Gengel R, Pascoe DP, Shaw L. A frequency-response procedure for evaluating and selecting hearing aids for severely hearing-impaired children. J Speech Hear Dis 36: 341–353, 1971 [DOI] [PubMed] [Google Scholar]
- Hedley-Williams A, Tharpe AM, Bess FH. Fitting hearing aids in the pediatric population: A survey of practice procedures. In: Bess FH, Gravel JS, Tharpe AM. eds, Amplification for children with auditory deficits Nashville, TN: Bill Wilkerson Center Press; pp. 107–122, 1996 [Google Scholar]
- Kruger B. An update on the external ear resonance in infants and young children. Ear Hear 8: 333–336, 1987 [DOI] [PubMed] [Google Scholar]
- Lewis DE, Stelmachowicz PG. Real-ear to 6-cm3 coupler differences in young children. J Speech Hear Res 36(1):204–209, 1993 [DOI] [PubMed] [Google Scholar]
- Lewis DE, Pittman AL, Hoover BM, Stelmachowicz PG. Interaction between amplification and the spectral characteristics of self-generated speech in children. Poster presentation at the International Hearing Aid Conference, Lake Tahoe, CA, 2002
- Moodie KS, Seewald RC, Sinclair ST. Procedure for predicting real-ear hearing aid performance in young children. Am J Audiol 8(3):23–31, 1994 [Google Scholar]
- Moodie KS, Sinclair ST, Fisk T, Seewald RC. Individualizing hearing instrument fitting for infants. In: Seewald RC. ed. A Sound Foundation Through Early Amplification: Proceedings of an International Conference. Stafa Switzerland. Phonak AG. pp. 213–217, 2000 [Google Scholar]
- National Acoustic Laboratories NAL-NL1 version 1.39 experimenter edition. Australian Hearing Services, 2002
- Pediatric Working Group Amplification for infants and children with hearing loss. Am J Audiol 5(1):53–68, 1996 [Google Scholar]
- Ross M. Hearing aid selection for preverbal hearing impaired children. In: Pollack MC. ed. Amplification for the Hearing-Impaired. New York. Grune and Stratton. pp. 207–242, 1975 [Google Scholar]
- Scollie SD, Seewald RC, Cornelisse LE, Jenstad LM. Validity and repeatability of level-independent HL-to-SPL transforms. Ear Hear 19: 407–413, 1998 [DOI] [PubMed] [Google Scholar]
- Scollie SD, Seewald RC. Electroacoustic verification measures with modern hearing instrument technology. In: Seewald RC, Gravel JS. eds. A Sound Foundation Through Early Amplification: Proceedings of the Second International Conference. Stafa, Switzerland. Phonak AG. pp. 121–137, 2002a [Google Scholar]
- Scollie SD, Seewald RC. Hearing aid fitting and verification procedures for children. In Katz J. ed. Handbook of Clinical Audiology. Fifth Ed. Philadelphia. Lippincott Williams and Wilkins. pp. 687–706, 2002b [Google Scholar]
- Seewald RC. Pediatric fitting: The aided audiogram and (hopefully) beyond. Presentation at the 13th annual convention of the American Academy of Audiology. San Diego, 2001
- Seewald RC, Cornelisse LE, Ramji KV, Sinclair ST, Moodie KS, Jamieson DG. DSL v4.1 for Windows: A software implementation of the desired sensation level (DSL[i/o]) method for fitting linear gain and wide-dynamic-range compression hearing instruments. Users' manual. London, ON: Hearing Health Care Research Unit; 1997 [Google Scholar]
- Seewald RC, Moodie KS, Sinclair ST, Cornelisse LE. Traditional and theoretical approaches to selecting amplification for infants and young children. In: Bess FH, Gravel JS, Tharpe AM. eds. Amplification for Children with Auditory Deficits. Nashville, TN: Bill Wilkerson Center Press. pp. 161–192, 1996 [Google Scholar]
- Seewald RC, Moodie KS, Sinclair ST, Scollie SD. Predictive validity of a procedure for pediatric hearing instrument fitting. Am J Audiol 8(2):143–152, 1999 [DOI] [PubMed] [Google Scholar]
- Seewald RC, Ramji KV, Sinclair ST, Moodie KS, Jamieson DG. A computer- assisted implementation of the desired sensation level method for electroacoustic selection and fitting in children: User's manual. London, ON: Hearing Health Care Research Unit, 1993 [Google Scholar]
- Seewald RC, Scollie SD. Infants are not average adults: Implications for audiometric testing. Hear J 52(10):64–72, 1999 [Google Scholar]
- Sinclair ST, Beauchaine KL, Moodie KS, Feigin JA, Seewald RC, Stelmachowicz PG. Repeatability of a real-ear-to-coupler difference measurement as a function of age. Am J Audiol 5(3):52–56, 1996 [Google Scholar]
- Stelmachowicz PG, Lewis DE, Kalberer A, Cruetz T. Situational hearing-aid response profile (SHARP), Version 2.0: User's manual. Omaha, NE: Boys Town National Research Hospital. 1994 [Google Scholar]
- Stelmachowicz PG, Seewald RC, Gorga MP. Strategies for fitting amplification in early infancy. In: Bess FH. ed. Children with Hearing Impairment: Contemporary Trends. Nashville, TN: Bill Wilkerson Center Press. pp. 231–248, 1998 [Google Scholar]
- Zelisko DL, Seewald RC, Gagné JP. Signal delivery/real-ear measurement system for hearing aid selection and fitting. Ear Hear 13(6):460–463, 1992 [PubMed] [Google Scholar]