Abstract
Probe-microphone testing was conducted in the laboratory as early as the 1940s (e.g., the classic work of Wiener and Ross, reported in 1946), however, it was not until the late 1970s that a “dispenser friendly” system was available for testing hearing aids in the real ear. In this case, the term “dispenser friendly,” is used somewhat loosely. The 1970s equipment that I'm referring to was first described in a paper that was presented by Earl Harford, Ph.D. in September of 1979 at the International Ear Clinics' Symposium in Minneapolis. At this meeting, Earl reported on his clinical experiences of testing hearing aids in the real ear using a miniature (by 1979 standards) Knowles microphone. The microphone was coupled to an interfacing impedance matching system (developed by David Preves, Ph.D., who at the time worked at Starkey Laboratories) which could be used with existing hearing aid analyzer systems (see Harford, 1980 for review of this early work). Unlike today's probe tube microphone systems, this early method of clinical real-ear measurement involved putting the entire microphone (about 4mm by 5mm by 2mm) in the ear canal down by the eardrum of the patient. If you think cerumen is a problem with probe-mic measurements today, you should have seen the condition of this microphone after a day's work!
While this early instrumentation was a bit cumbersome, we quickly learned the advantages that probe-microphone measures provided in the fitting of hearing aids. We frequently ran into calibration and equalization problems, not to mention a yelp or two from the patient, but the resulting information was worth the trouble.
Help soon arrived. In the early 1980s, the first computerized probe-tube microphone system, the Rastronics CCI-10 (developed in Denmark by Steen Rasmussen), entered the U.S. market (Nielsen and Rasmussen, 1984). This system had a silicone tube attached to the microphone (the transmission of sound through this tube was part of the calibration process), which eliminated the need to place the microphone itself in the ear canal. By early 1985, three or four different manufactures had introduced this new type of computerized probe-microphone equipment, and this hearing aid verification procedure became part of the standard protocol for many audiology clinics. At his time, the POGO (Prescription Of Gain and Output) and Libby 1/3 prescriptive fitting methods were at the peak of their popularity, and a revised NAL (National Acoustic Laboratories) procedure was just being introduced. All three of these methods were based on functional gain, but insertion gain easily could be substituted, and therefore, manufacturers included calculation of these prescriptive targets as part of the probe-microphone equipment software. Audiologists, frustrated with the tedious and unreliable functional gain procedure they had been using, soon developed a fascination with matching real-ear results to prescriptive targets on a computer monitor.
In some ways, not a lot has changed since those early days of probe-microphone measurements. Most people who use this equipment simply run a gain curve for a couple inputs and see if it's close to prescriptive target—something that could be accomplished using the equipment from 1985. Contrary to the predictions of many, probe-mic measures have not become the “standard hearing aid verification procedure.” (Mueller and Strouse, 1995). There also has been little or no increase in the use of this equipment in recent years. In 1998, I reported on a survey that was conducted by The Hearing Journal regarding the use of probe-microphone measures (Mueller, 1998). We first looked at what percent of people dispensing hearing aids own (or have immediate access to) probe-microphone equipment. Our results showed that 23% of hearing instrument specialists and 75% of audiologists have this equipment. Among audiologists, ownership varied among work settings: 91% for hospitals/clinics, 73% for audiologists working for physicians, and 69% for audiologists in private practice. But more importantly, and a bit puzzling, was the finding that showed that nearly one half of the people who fit hearing aids and have access to this equipment, seldom or never use it.
I doubt that the use rate of probe-microphone equipment has changed much in the last three years, and if anything, I suspect it has gone down. Why do I say that? As programmable hearing aids have become the standard fitting in many clinics, it is tempting to become enamoured with the simulated gain curves on the fitting screen, somehow believing that this is what really is happening in the real ear. Additionally, some dispensers have been told that you can't do reliable probe-mic testing with modern hearing aids—this of course is not true, and we'll address this issue in the Frequently Asked Questions portion of this paper.
The infrequent use of probe-mic testing among dispensers is discouraging, and let's hope that probe-mic equipment does not suffer the fate of the rowing machine stored in your garage. A lot has changed over the years with the equipment itself, and there are also expanded clinical applications and procedures. We have new manufacturers, procedures, acronyms and noises. We have test procedures that allow us to accurately predict the output of a hearing aid in an infant's ear. We now have digital hearing aids, which provide us the opportunity to conduct real-ear measures of the effects of digital noise reduction, speech enhancement, adaptive feedback, expansion, and all the other features. Directional microphone hearing aids have grown in popularity and what better way to assess the real-ear directivity than with probe-mic measures? The array of assistive listening devices has expanded, and so has the role of the real-ear assessment of these products. And finally, with today's PC -based systems, we can program our hearing aids and simultaneously observe the resulting real-ear effects on the same fitting screen, or even conduct an automated target fitting using earcanal monitoring of the output. There have been a lot of changes, and we'll talk about all of them in this issue of Trends.
Terminology
Before we start talking about procedures and applications, it's probably good to review the acronyms that are the vital components of probe-mic lingo. Some people cringe when they think about acronyms, but they do provide an easy way for us to talk to each other—requesting a SPAM sandwich just wouldn't be the same without them. There is now an ANSI standard for probe-mic measures (S3.46–1997), which among other things, helps to provide some acronym rules.
Deciding the appropriate probe-mic terminology was apparently not an easy task. In 1986, Dave Preves was quoted in the The Hearing Journal, stating:
“An Acoustical Society of America study group will meet this month [May, 1986] to begin discussing the standardization of real-ear measurement terminology.”
As you see from the reference, it was more than ten years before the standard was published. Like good wine, standards take time to reach maturity. While waiting for the phantom standard to emerge, some people published papers and book chapters using the terminology that was rumored to be part of the standard (e.g., Mueller, 1990; Schwietzer et al, 1990; Sullivan, 1990; Mueller, 1992a). These terms became accepted, and were commonly used by probe-mic manufacturers, researchers and clinicians. For the most part, the terms in the standard are similar to the now well-known terminology. You'll see that there are a couple of exceptions, however, so a little re-learning will be necessary.1
Terms and Definitions from the ANSI Standard
Listed here are the probe-mic terms from the 1997 ANSI standard (as summarized by Mueller and Hall, 1998). They should look familiar, but to help differentiate these terms from the pre-standard ones, there is a clarification that is important to remember. If a measure represents SPL in the ear canal, the term ends in an “R” for Response. An example would be the REUR. If a measure represents a difference value (e.g., the input has been subtracted from the output), the term ends in a “G” for Gain. An example would be the REUG. Consider that gain is always a difference value (e.g., REIG), and therefore, the REIR term, beloved and used by many, no longer exists.
REUR (Real-Ear Unaided Response): SPL as a function of frequency, at a specified measurement point in the ear canal, for a specified sound field, with the ear canal unoccluded.
REUG (Real-Ear Unaided Gain): Difference in decibels between the SPL as a function of frequency at a specified measurement point in the ear canal and the SPL at the field reference point, for a specified sound field, with the ear canal unoccluded.
REOR (Real-Ear Occluded Response): SPL as a function of frequency, at a specified measurement point in the ear canal, for a specified sound field, with the hearing aid (and it's acoustic coupling) in place and “turned off.”
REOG (Real-Ear Occluded Gain): Difference in decibels between the SPL as a function of frequency at a specified measurement point in the ear canal and the SPL at the field reference point, for a specified sound field, with the hearing aid (and it's acoustic coupling) in place and “turned off.”
REAR (Real-Ear Aided Response): SPL as a function of frequency, at a specified measurement point in the ear canal, for a specified sound field, with the hearing aid (and it's acoustic coupling) in place and “turned on.”
REAG (Real-Ear Aided Gain): Difference in decibels between the SPL as a function of frequency at a specified measurement point in the ear canal and the SPL at the field reference point, for a specified sound field, with the hearing aid (and it's acoustic coupling) in place and “turned on.”
REIG (Real Ear Insertion Gain): Difference in decibels, as a function of frequency, between the REAG and the REUG, taken with the same measurement point and the same sound field conditions.
If those definitions sounded a little too “ANSI-standard-like” for you, you might you might appreciate the following:
REUG: The patient's “natural” amplification; what he brings to the clinic with him.
REOG: What we do to the patient before we do something for him. That is, when turned off, what are the attenuation properties of the hearing aid or earmold?
REAG: The gain provided by the hearing aid.
REIG: The gain the patient has when he leaves the clinic that he didn't have when he entered the clinic.
Other Probe-Mic Terms
There are three probe-mic terms (complete with acronyms) that were not included in the standard, but they do have direct clinical applications. Here is a brief description of these terms (from Mueller and Hall, 1998):
RESR (Real Ear Saturation Response): SPL as a function of frequency, at a specified measurement point in the ear canal, for a specified sound field, with the hearing aid (and it's acoustic coupling) in place and “turned on,” with the VC adjusted to full-on (or just below feedback if full-on isn't possible). The input signal is sufficiently intense to operate the hearing aid at its maximum output level.
RECD (Real Ear Coupler Difference): Difference in decibels, as a function of frequency, between the output of the hearing aid (and it's acoustic coupling) in the real ear and in a 2-cc coupler, taken with the same input signal and hearing aid VC setting.
REDD (Real Ear Dial Difference): Difference in decibels, as a function of frequency, between the audiometer dial setting and the output from the audiometer earphone in the real ear.
Other Related Terms
When fitting hearing aids and conducting probe-mic measurements, there are three other terms that often are used.
RETSPL (Reference Equivalent Threshold in SPL): Don't be fooled—the “RE” in this term does not represent Real Ear. The RETSPL is the difference in decibels, as a function of frequency, between the audiometer dial setting and the output from an audiometer earphone in a coupler.
CORFIG (COupler Response for Flat Insertion Gain). Difference in decibels, as a function of frequency, between the gain of a hearing aid in the real ear and in a 2-cc coupler. Another reasonable explanation of the acronym would be CORrection FIGure.
GIFROC: Not a term for the acronym challenged. If indeed the CORFIG is used to convert real ear gain to coupler gain, then when we convert coupler gain to real ear gain, we are doing the opposite (adding the GIFROC is equivalent to subtracting the CORFIG). The GIFROC is a backward CORFIG2 In this paper, however, I will simply use the CORFIG term to describe corrections going in either direction.
General Clinical Applications
Now that we've taken care of the terminology issue, it seems appropriate to review the basic clinical applications of probe-mic measurements. In general, they fall into four different categories.
Verification of Prescriptive Fitting Targets
When probe-mic equipment was first introduced to the U.S., the default test procedure was in-situ measurements—what we now refer to as the REAR—as this was the verification strategy most commonly used at the time in Europe. Audiologists in the U.S., however, were using prescriptive methods that required verification using functional gain (e.g., POGO, Berger, etc). What was needed was a probe-mic measurement that provided values that could be interchanged with functional gain, so that the same prescriptive methods could be used. The equipment default settings quickly were changed to reflect this preference, and to this day, the REIG is the primary tool used to verify hearing aid performance.
It's important to recognize that probe-mic measures are not a way to fit hearing aids. Rather, they are a way to verify that you have achieved the gain and output that is consistent with the way that you fit hearing aids. It's no secret that some dispensers first obtain an REIG curve, then toggle through all possible prescriptive methods to see if by chance the curve on the screen matches one of them. The more prudent method, of course, would be to first decide what prescriptive fitting method agrees with your beliefs, then conduct probe-mic testing to see if your gold standard has been met. If it hasn't, continue to re-program the hearing aid until a reasonable match is obtained.
Since we typically fit hearing aids that are designed to deliver different gain for different inputs, for complete verification of the fitting it's helpful to also use a prescriptive method that provides multiple gain targets. There are three that meet this criterion, and they all are commonly used today with probe-mic measurements:
FIG6 for Windows: Provides REIG targets for three input levels: 45, 65, and 95 dB SPL (Killion et al, 1997).
NAL-NL1: Provides REIG or REAG targets for seven levels: 40, 50, 60, 65, 70, 80, and 90 dB (Dillon et al, 1999).
DSL v.4.1a: Provides REAR (and REAG) targets for 17 input levels: 20 dB to 100 dB SPL in 5 dB increments (Seewald et al, 1997).
A fourth fitting procedure, VIOLA (a component of the IHAFF protocol) also provides fitting targets for three input levels, and easily can be used with today's hearing aids (Mueller, 1997). The software, however, only displays 2-cc coupler targets (see Cox, 1995, and Cox and Flamme, 1998 for clinical applications of this procedure). With a few correction factors, these coupler values could be converted to REAR or REIG targets.
Some hearing aid manufacturers also have developed their own targets for using multiple input levels. A perplexing situation, however, is when the manufacturers' fitting software does not use a published prescriptive method, and does not display the desired real-ear targets. Obviously, it's impossible to verify that the real-ear gain and output is correct when targets are unknown. The up side of course, is that you don't have to look at your mistakes.
Although there is some concern about routinely conducting RESR measures (which we'll discuss later), probe-mic assessment also can be used to determine if the hearing aid's maximum output is set correctly. Most prescriptive fitting approaches include target gain or output values for high input levels. Individual target values also can be established by adding the frequency-specific REDD to the patient's pure-tone LDL values. RESR values can then serve as a supplement to, but not a replacement for, aided soundfield loudness judgments (see Mueller, 1999 for review).
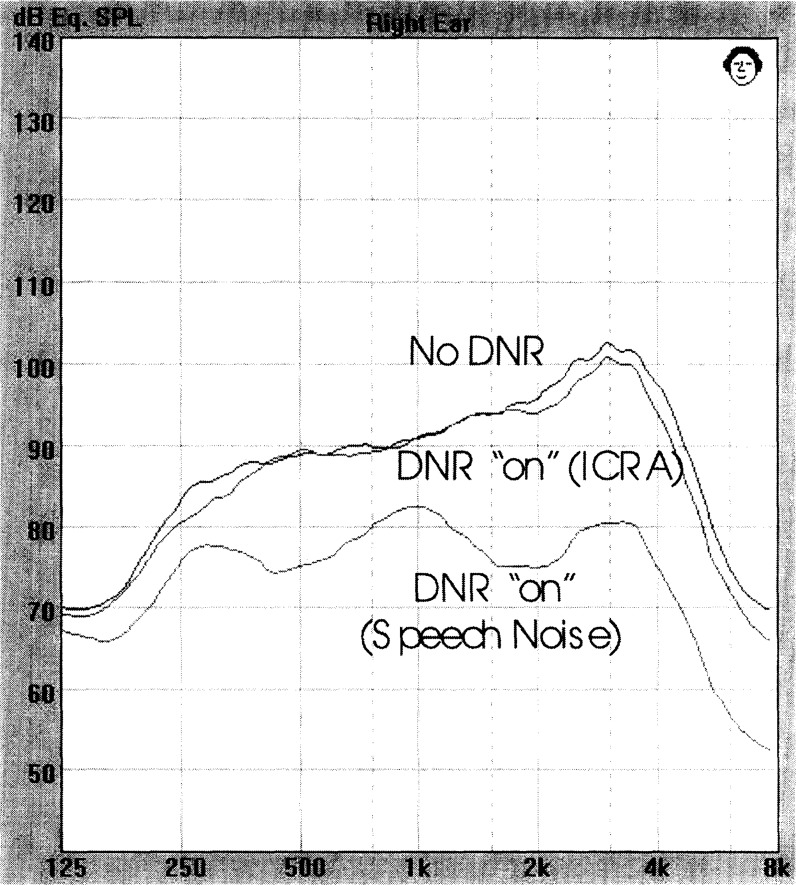
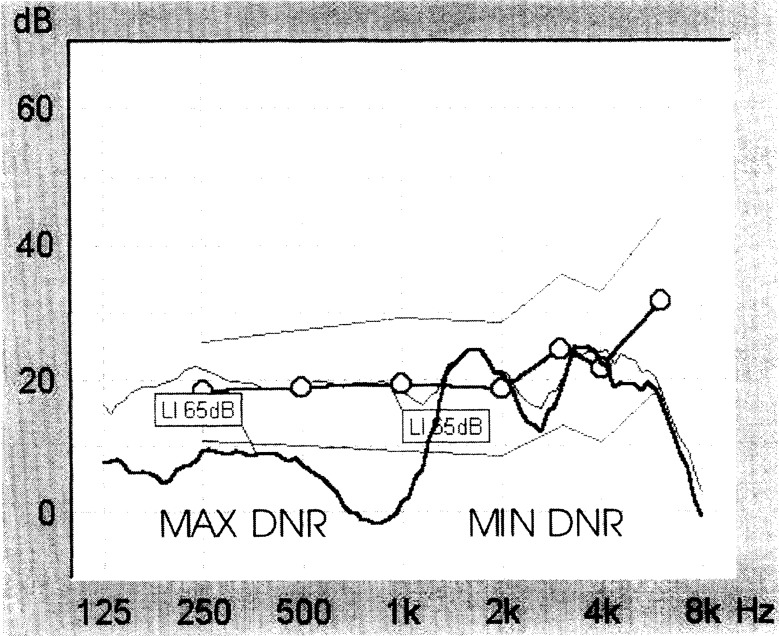
Verification of Hearing Aid Features
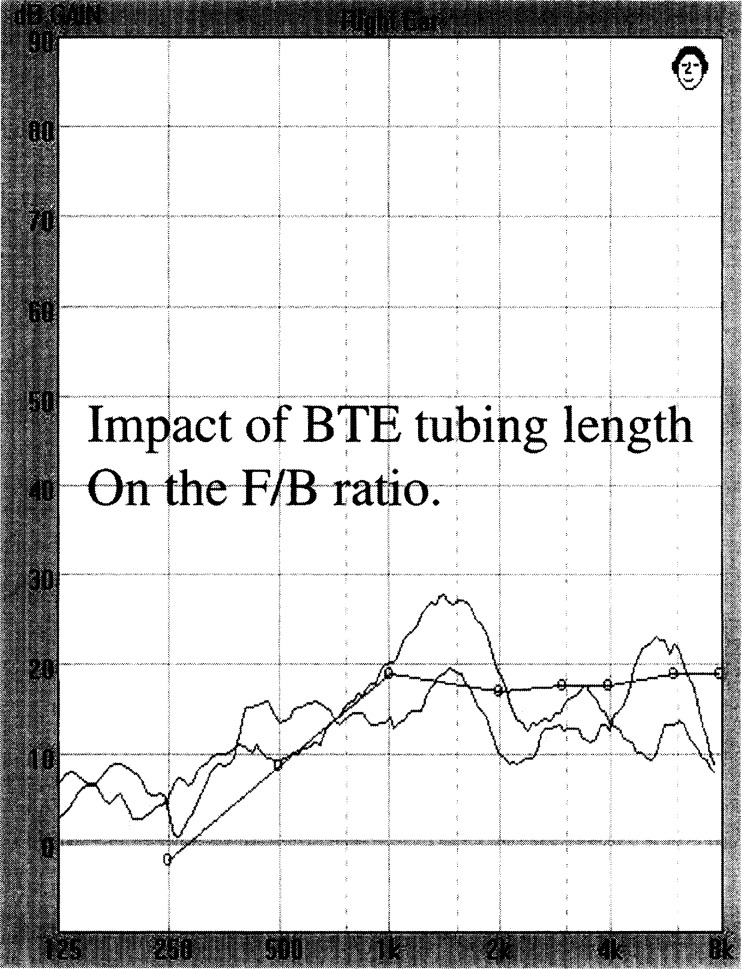
A second use of probe-mic measures in the daily fitting of hearing aids is the verification of various features of the hearing aid. If some cases this could be conducted in the 2-cc coupler, but many times assessment in the real-ear is necessary. As we continue to fit hearing aids with more features, and patients are “sold” these features, the importance of probe-mic verification only increases. For example, venting and slit leak can have significant effects on the real-ear compression ratio, directional microphone performance, and the strength of the digital noise reduction circuit. Another example where real ear measurements provide essential information is regarding the sensitivity of the hearing aid's telephone coil, especially for custom instruments. The telecoil response can be quite different when the hearing aid is positioned in the real ear than when it is measured in a hearing aid test box (Mueller, 1992b). In summary, some features of modern hearing aids that easily can be tested with probe-mic measures include:
The effects of WDRC compression (observation of output changes as a function of input level).
The effects of adaptive digital noise reduction (magnitude and time constants).
The front-to-back ratios of directional microphone hearing aids.
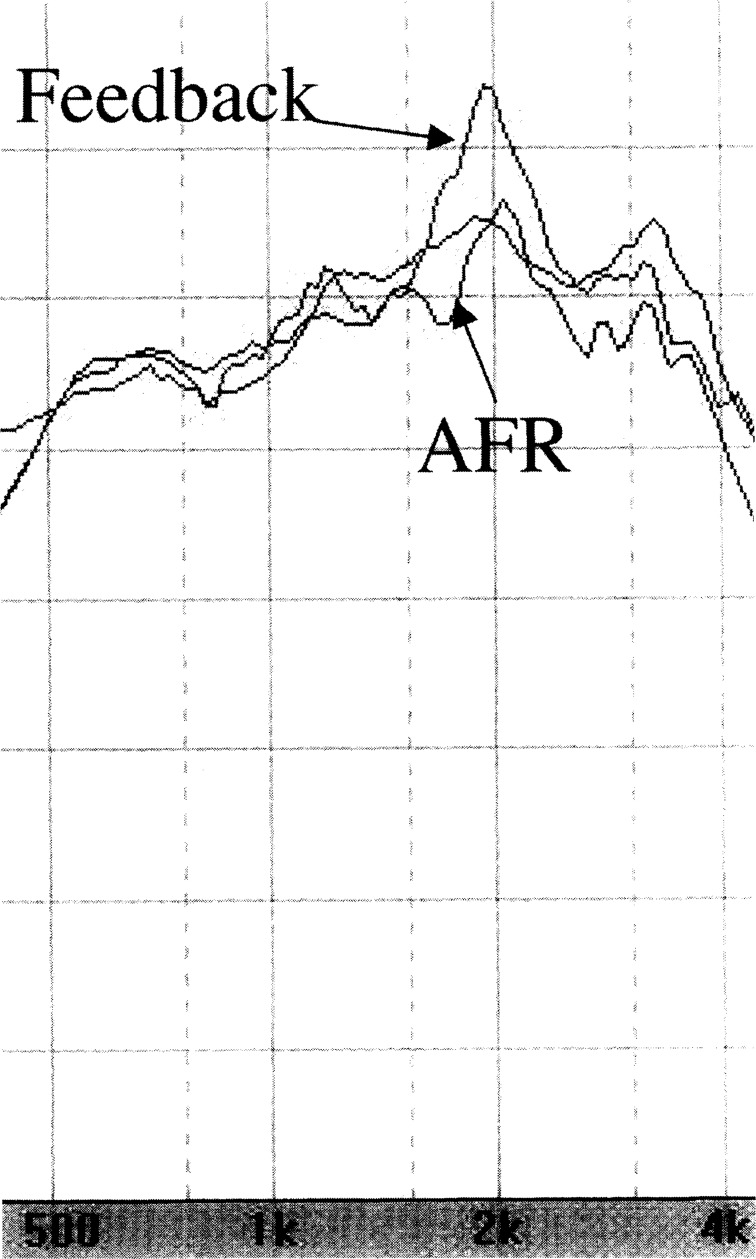
The effects of digital adaptive feedback (change in real-ear frequency response).
The real-ear response of the telecoil.
Establishing Individualized Correction Factors
When selecting and fitting hearing aids, it is often necessary to use average correction factors. In many cases, especially with infants and children, it is desirable to use individualized correction factors, rather than average values. For instance, you might want to convert from the audiometer dial reading in HL to real-ear SPL (that's the REDD), from output in the ear-canal to output in a 2-cc coupler (that's the RECD), or from gain in the coupler to gain in the real ear (that's the CORFIG). By conducting one or two real-ear measurements, these correction factors can be individualized, which adds to the precision of the hearing aid adjustments. In fact, if these individualized correction factors are known, the hearing aid can be fitted in the 2-cc coupler before the patient arrives—a distinct advantage when the patient is a hard-to-test infant or child.
Real-Ear Spectral Analysis
Some of the most interesting testing conducted with probe-mic equipment is when the system is used as a spectral analyzer—that is, the equipment loudspeaker is turned off, and the probe-tube serves as a mini sound level meter at the eardrum of the patient, (see Mueller, 1995 for review). This allows us to use all kinds of different types of acoustic stimuli, and observe the frequency-specific display of the real-ear output. Examples of when the spectral analysis mode would be used include:
Measurement of the occlusion effect, using the patient's own voice as the input signal.
Measurement of the REDD, using the audiometer's pure tones as the input signal.
Measurement of telecoil sensitivity using the output from the telephone receiver (speech, noise or dial tone) as the input signal.
Measurement of the hearing aid's digital noise reduction feature using cocktail party noise or other environmental sounds as the input signal.
Measurement of “hearing aid noise” using only ambient room noise as the input signal.
Measurement and fitting of musicians' earplugs.
The hearing aid occlusion effect is a common complaint among many hearing aid users, so it's worthwhile to spend some time discussing this measurement. Often, treatment of the occlusion effect problem is haphazard. That is, the dispenser is not always sure that the problem is the occlusion effect (as opposed to too much low frequency gain from the hearing aid), and the most common treatment is to modify the shell or earmold to create more venting and ask the patient, “does that sound better?” Extending the canal length of the hearing aid or earmold can be successful, but again, an objective measure of its effectiveness is helpful (Mueller, 1994; Pirzanski, 1998).
Ever since the classic Laurel Wilber “nacho flavored Doritos chewing” example, illustrated in the publication of Killion et al (1988), clinicians and researchers have used probe-mic assessment to examine the occlusion effect (see Mueller et al, 1996 for review). Probe-mic measures provide precise ear canal SPL information regarding the occlusion effect, which can be used for both diagnoses of the problem, and evaluation of the treatment.3
A sample protocol to measure the occlusion effect, which can be used with most probe-mic equipment, is as follows:
Configure the software of the probe-mic equipment for conducting occlusion effect testing (this will disable the loudspeaker, so sitting the patient directly in from of the speaker is not necessary).
Place the tip of the probe tube deep in the ear canal (within 5-mm of the TM).
Have the patient vocalize, and maintain a vowel (“eee” works the best). A strong vocalization (75–80 dB SPL) is necessary with most equipment.
When the vocalization is stabilized, the open ear SPL output is stored.
Place the hearing aid in the ear (turned off!) and repeat the testing.
The increase in output (in the low frequencies) with the hearing aid in the ear is the hearing aid occlusion effect.
If venting modifications are planned, leave the patient at the probe-mic equipment so that real-ear assessment of the modifications can be made.
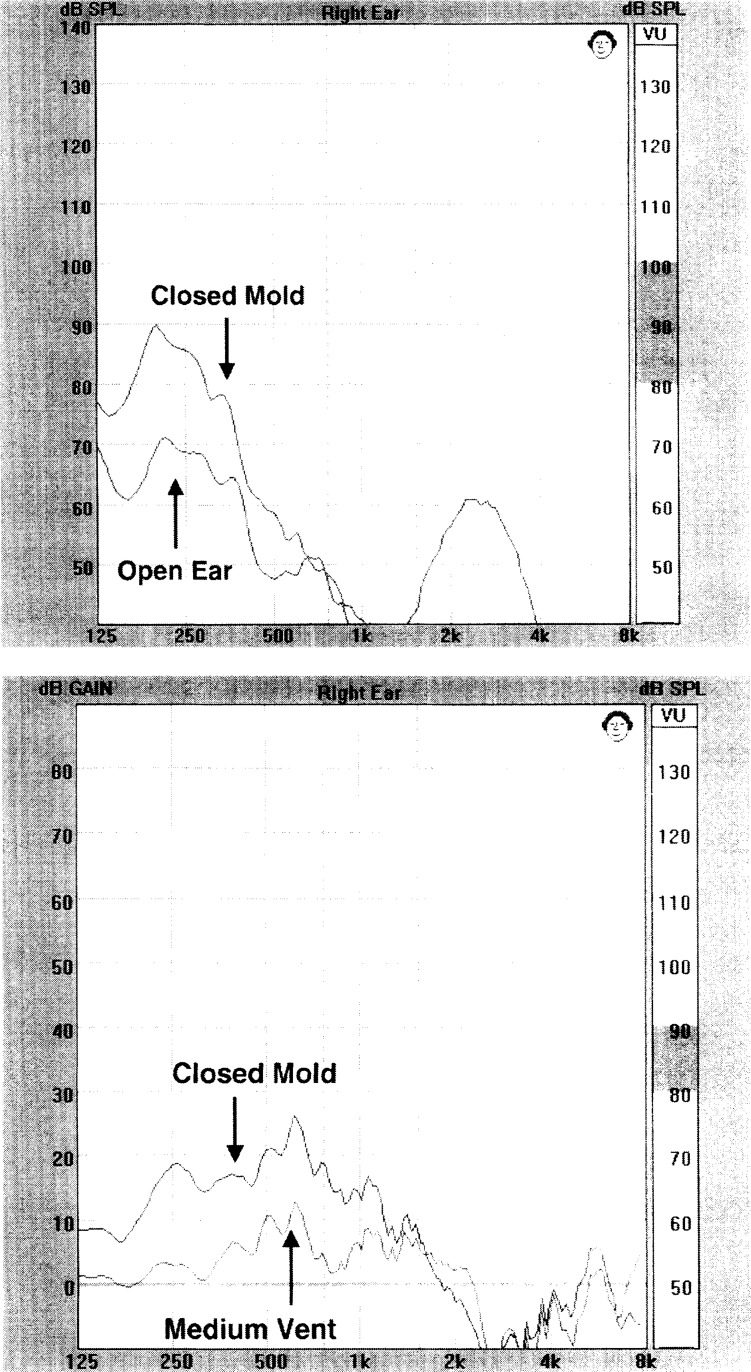
Figure 1 illustrates typical real-ear results when this testing is conducted. The upper panel displays the ear canal SPL for the open ear and closed ear conditions. Observe that in the 200 Hz region, there is a 20-dB increase in SPL when the earmold is placed in the ear (the occlusion effect). While 20 dB is a larger-then-average occlusion effect, from one standpoint this finding is encouraging, as 200 Hz is a frequency that is relatively easy to leak out of the ear with venting. Some patients have an occlusion effect of 20 dB at 500 Hz or higher—a region where venting has much less impact. These are the people you get to know very well. The peak that you see around 3000 Hz is of little interest and is unrelated to the occlusion effect—this is the ear canal resonance of the open ear, which is no longer present when the earmold is placed in the ear canal.
Figure 1.
Top panel: Ear canal SPL for patient's vocalization of “eee” for the open ear, and when ear mold was placed in ear. Diffference between the upper and lower curves in the low frequencies is the occlusion effect. Bottom panel: Illustration of the effect that a medium vent had on the occlusion effect.
In the lower panel of Figure 1, you see the results of occlusion effect testing displayed in a different manner. In this instance, we have configured the equipment to subtract the open ear SPL from the closed ear SPL, which then provided a graphic frequency-specific occlusion effect. Again, this patient has considerable occlusion effect through 1000 Hz when fitted with a closed earmold. Observe that when we placed a medium vent (2-mm) in the earmold, we eliminated nearly all the occlusion effect for the very low frequencies, but 10–12 dB still remains in the 500–700 Hz range. It could be, however, that this reduction is adequate to eliminate the complaint of the occlusion effect, even though the effect is still present. If the hearing aid has gain at this frequency, the effect will be even less noticeable (e.g., the ol' adding decibels rule applies here). Whenever modifications to reduce the occlusion effect are made, it's important not to lose sight of the overall fitting goals—maximize audibility and speech intelligibility. Creating new problems while solving one usually is not a reasonable trade-off.
The list of measurements that can be conducted in the spectral analysis mode could go on forever, and is limited only by your imagination. If you've ever wondered about the output of anything in the real ear, aided or unaided, your probe-mic equipment will provide you with the answer.
Specific Clinical Applications
To this point, we have discussed several different probe-mic test procedures, and four general clinical application areas. It's now time to take each one of the test procedures, and briefly discuss how and when each would be used in the everyday fitting of hearing aids.
REUG
For most people using probe-mic assessment, the REUG is the first measure conducted. The reason for this is that most audiologists verify hearing aid performance using the REIG, and it's not possible to calculate the REIG without the REUG (on the other hand, if you verify performance using the REAR, the REUG is of little interest—more on that later). Figure 2 shows the average REUG for adults (from Seewald, et al, 1997).
Figure 2.
Average REUG. From Seewald RC, Cornelisse LE, Richert FM, Block MG (1997). Acoustic transforms for fitting CIC hearing instruments. In Chasin M (ed.) CIC Handbook. San Diego: Singular Publishing Group. 83–100.
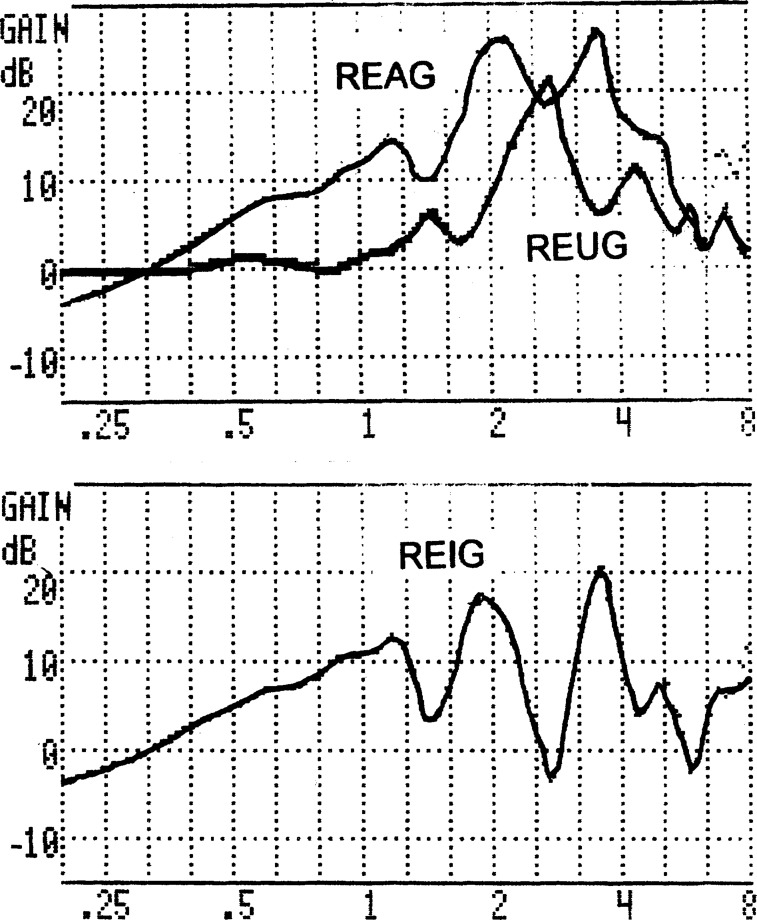
Because the REUG is always subtracted from the REAG, and REAG curves tend to be relatively smooth, it's common that bumps in the REUG become dips in REIG, and dips in the REUG become bumps in the REIG. An example of this is shown in Figure 3. This display shows the initial real-ear results using a 50 dB input signal, of a programmable BTE hearing aid fitted to a patient with a mild downward sloping hearing loss. It should be pointed out that this probably is not a “typical” finding, although it occurs often enough to warrant discussion.
Figure 3.
Top panel: Illustration of unusual REUG and REAG. Bottom panel: Resulting REIG, illustrating negative gain in the 3000 Hz region for this patient.
On the top panel, the REUG and REAG are shown. Observe that the REUG exceeds 20 dB in the 3000 Hz range, but the two primary peaks of the REAG are at 2000 and 4000 Hz. This results in the predictable REIG, shown in the lower panel. If we only consider gain at 3000 Hz, this patient would have better audibility if he simply used his own ear canal resonance rather than the hearing aid.
Since REIG bumps and dips usually are unsightly (they probably bother the fitter more than they do the patient), it is tempting to try and make the REAG more closely resemble the REUG so that the REIG has a smoother appearance and is a closer match to the target gain curve. In multichannel programmable hearing aids, this often can be accomplished at the time of the fitting. Prescriptive fitting methods like the NAL-NL1, also allow you to enter the patient's REUG, and if these values are different than average, desired 2-cc coupler gain will be influenced accordingly (desired REIG, however will remain the same). In essence, you have created a partially individualized CORFIG. The components of the CORFIG include the REUG, the RECD and the microphone location effects (MLEs) of the hearing aid that is being fitted (in general, MLEs become larger as the microphone inlet is recessed in the concha or ear canal). The CORFIG is calculated by subtracting the RECD and the MLE from the REUG. Therefore, the bigger the REUG, the more positive the CORFIG will become. The CORFIG is added to the REIG to obtain desired 2-cc coupler gain, so the bigger the REUG, the bigger the desired 2-cc coupler gain.
On the surface, correcting the CORFIG for the patient's REUG seems like a reasonable thing to do if your interest lies in observation of the REIG—fitting methods like the NAL-NL1 allow you to select this option. It can result in some rather bizarre desired 2-cc coupler values however, especially when you have a patient with little or no hearing loss at 2000 Hz, and his—I say his, because it seems to always be a male with a big ear canal—R EUG is 10–15 dB larger than average at 2000 Hz (see Mueller and Bryant, 1991, and Mueller, 1992c for case studies and review of this topic). Often, the use of “average” REUG values will provide a more desirable REAR spectrum.4
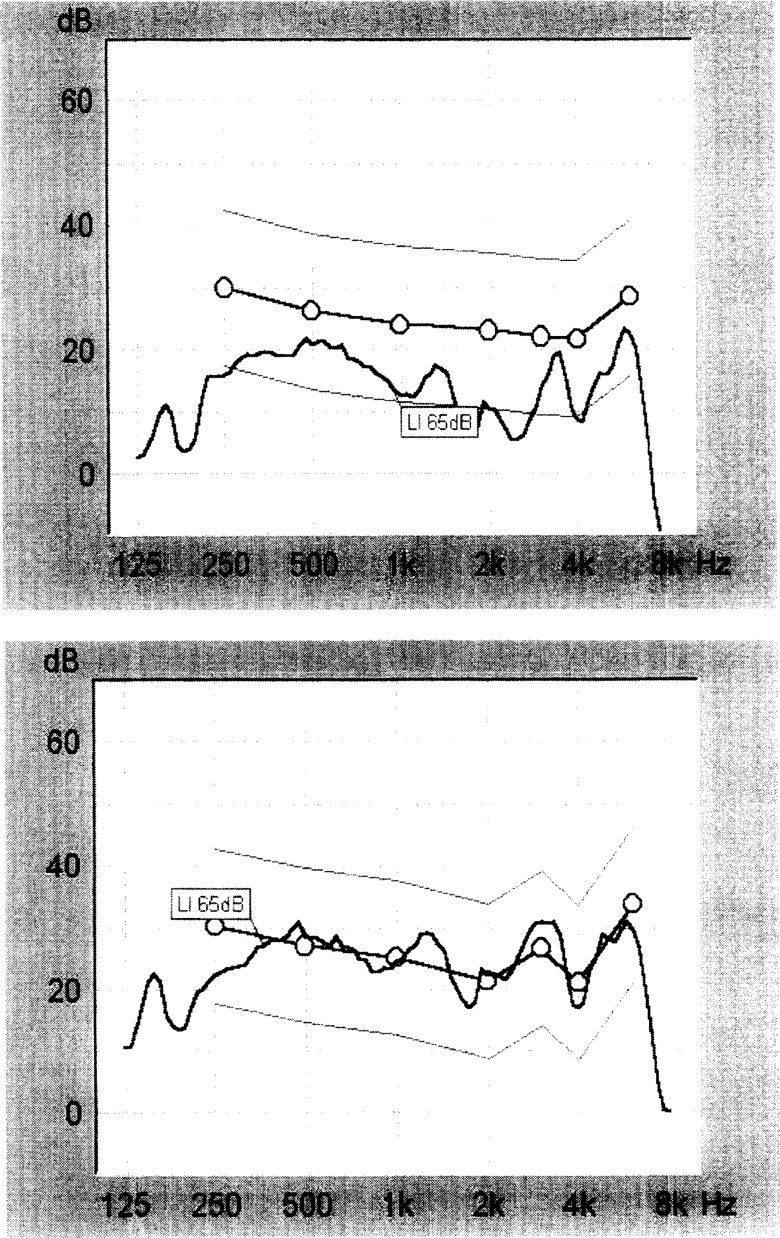
Some probe-mic equipment automatically adjusts the gain of the hearing aid to compensate for an unusual REUG. Shown in the top panel of Figure 4 is the REIG of a DSP hearing aid programmed by the fitting software to match the DSL target curve shown in the display. The fitting software used an average REUG, and although this resulted in a nearly perfect fit to target on the fitting screen, because this patient had an unusual REUG, the unacceptable REIG displayed in the top panel was obtained. With a simple mouse click, however, the hearing aid was re-fit in the real ear, taking the patient's unusual REUG into consideration. The result was the more acceptable REIG displayed in the lower panel.
Figure 4.
Top panel: Initial real-ear fit to target following programming using 65 dB input signal (connected circles are desired target). Bottom panel: Fit to target following automated real-ear “first fit” procedure (Courtesy of Siemens Hearing Instruments).
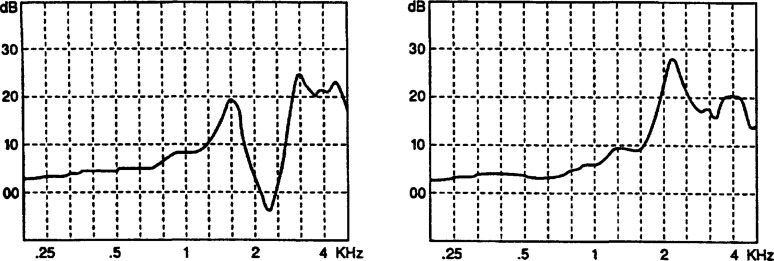
While the primary clinical purpose of conducting the REUG is to obtain the values for calculating the REIG, the configuration of the REUG also can provide useful information regarding the status of the middle ear. The most dramatic effect is observed when a TM perforation is present. As shown in Figure 5, left panel (from Moryl, et al, 1992), when a TM perforation is present, the characteristic REUG peak around 2700 Hz is absent, and a peak in the lower frequencies is observed. For more information on the effects of middle ear pathology on the REUG, see the review by de Jonge (1993).
Figure 5.
Left panel: REUG for a patient with a large tympanic membrane perforation. Right panel: REUG for the same patient after a tympanoplasty had closed the perforation. From Moryl C, Danhauer J, DiBartolomeo J (1992). Real ear unaided responses in ears with tympanic membrane perforations. Journal of the American Academy of Audiology, 3, 60–65.
REOG
The REOG is a measure of how well the hearing aid or earmold is acting like an earplug. Although there has been some research attempting to relate individual REOG values to speech understanding (e.g., Chasin, et al, 1997) the primary clinical application is to observe the sound inflow caused by venting or slit-leak. For example, if you had a patient with normal hearing at 500 Hz, and you wondered if the combined effects of slit leak and a pin-hole vent allowed 500 Hz signals to pass to the TM without attenuation, the REOG would give you this information (e.g., an REOG of 0 dB would show that sound was passing through without attenuation). Repeated REOG testing, therefore, can be used to assure that vents are sized appropriately, monitor the acoustic effects of vent modifications, and help to predict potential feedback problems (we assume that “inflow” values are predictive of “outflow”). In essence, these same effects can be observed by observing the REAG (although very few clinicians observe the REAG).
One of the most useful clinical applications of the REOG is to detect when vent-associated resonance is present, and when it adversely affects the real-ear gain. While bothersome vent-associated resonance is a fairly rare occurrence, it can be very annoying to the patient, and the problem often is misdiagnosed by the clinician. Vent-associated resonance, which is sometimes observed to be 10 dB or larger, usually results in increased gain in the 500 Hz region, and frequently occurs when the vent diameter is 1–2 mm.5 The patient might complain that his voice sounds “hollow” or “booming,” and the clinician might implement treatment strategies for the occlusion effect, which will not solve the problem. Because vent-associated resonance is an acoustic event, not an electroacoustic event, it is present with the hearing aid turned off—the measurement procedure for the REOG. If the hearing aid has gain at this frequency, which usually is not the case, it's possible that the REOG could be somewhat misleading. If the output of the hearing aid is phase reversed with the input, the gain shown in the REOG might not be as great as what would be present when the hearing aid was turned on (because of the phase interaction of the “through the vent” signal” versus the “through the hearing aid signal”). Again, REOG/REAG comparisons are useful.
Given that we normally are interested in the acoustic effects of venting, it seems reasonable that an REOG would be conducted routinely whenever hearing aids or earmolds with vents were fitted. There is little extra time required—simply run a quick curve with the hearing aid turned off before turning on the hearing aid and conducting the REAR—an extra 15 seconds or so of test time.
Now that we've talked about what the REOG does measure, it's important to mention what it does not measure:
It does not measure the occlusion effect. The occlusion effect is related to sound pressure levels in the ear canal generated by a bone-conducted signal (usually one's own voice). The REOG, unless it is at or near 0 dB through 1000 Hz, is a rather poor predictor of whether the occlusion effect is present (for one thing, some people, because of their voice quality and other characteristics, have little or no occlusion effect for their own voice regardless of how tightly the ear is plugged). A patient's REOG could range anywhere from 0 dB to −30 dB, and there possibly would be no occlusion effect. For example, if the canal portion of a custom instrument is very shallow (allowing considerable venting), the REOG will be at or near 0 dB in the low frequencies, and there probably will not be a significant occlusion effect (especially if the patient's primary occlusion effect is below 500 Hz). Compare this to a very different fitting where the canal of the custom instrument fits tightly and terminates in the bony margin of the ear canal. This will produce an REOG of around −30 dB, but again, there probably will not be a significant occlusion effect (see Mueller et al, 1996 for review).
It does not predict required hearing aid gain. Consider these two cases: Patient A has an REOG of −10 dB, and Patient B has an REOG of −30 dB. At first glance you might say, “Patient B needs more gain because he has more insertion loss.” It's important to remember, however that once the hearing aid is turned on, sound has a new pathway to reach the TM (through the hearing aid), and the negative REOG differences (the differences that exist below the 0-dB gain point) have been equalized. What have not been equalized are the effects that the insertion of the hearing aid had on the REUG, but that is taken care of by the way the insertion gain is calculated. Hence, the REOG is not a player in gain selection.
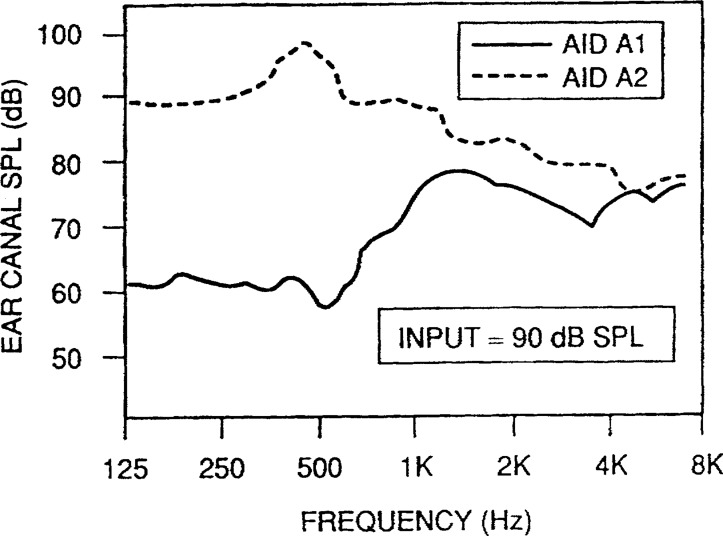
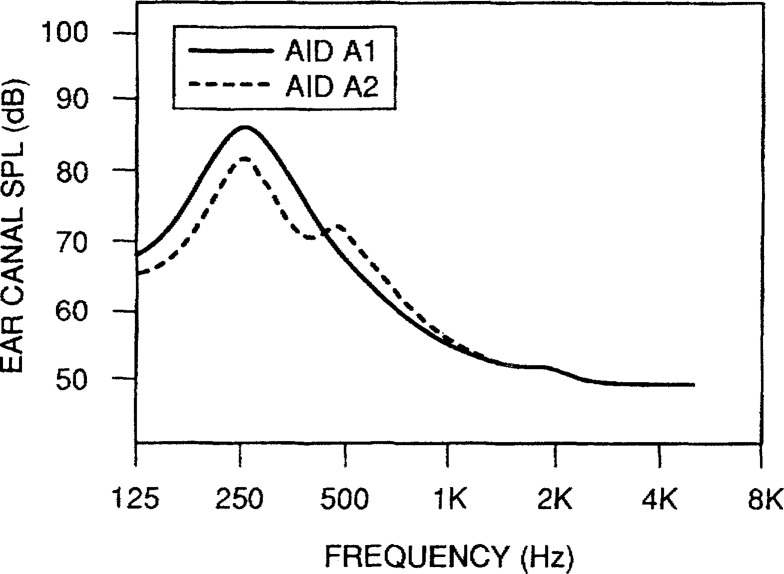
Figure 6 (from Mueller, 1994) shows the REOR (90 dB input) for two different CIC hearing aids made for the same ear. Aid A1 was a deep fitted CIC (about 5-mm from the patient's TM), made to conform to the configurations of the patient's ear canal. Aid A2 was equal in depth to Aid A1, except that the canal of the instrument was tapered (carrot shaped) to enhance patient comfort (which of course creates slit leak around the rim of the faceplate—a similar effect to adding a vent). Observe that the REOG for the tight fitting CIC (A1) was 30 dB in the low frequencies. In contrast, CIC A2 maintained a 0 dB REOG until 1000 Hz or so, at which point the ear canal output begins to fall below the 90-dB input.
Figure 6.
Illustration of REOGs for two different deep-fitted CICs made for the same ear. Aid A1 was formed to the contour of the ear canal, Aid A2 was tapered. From Mueller HG (1994) CIC hearing aids: What is the impact on the occlusion effect? The Hearing Journal, 47 (11) 29–35.
Which hearing aid had the least occlusion effect? It was CIC A1, because the cartilaginous portion of the ear canal was not allowed to vibrate. Which hearing aid had the most gain? Again it was CIC A1, as hearing aid A2 began to feedback whenever gain was raised above 20 dB.
REAR
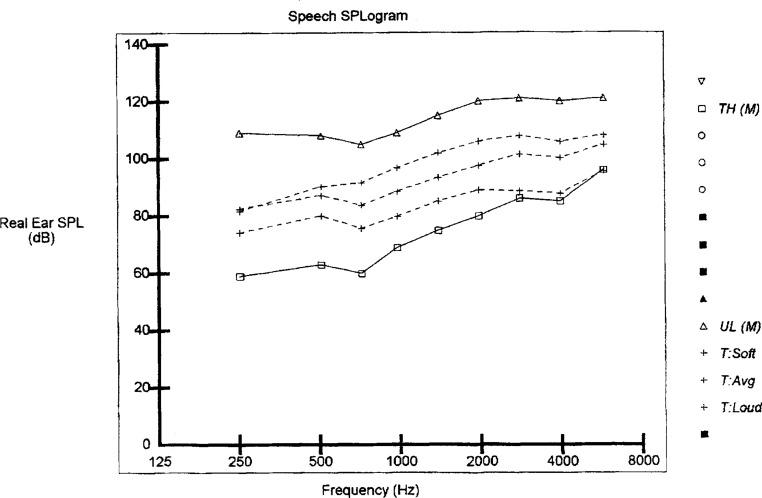
As mentioned earlier, most dispensers rely on the REIG for hearing aid verification, and it continues to be recommended as the primary verification method for adults (Storey and Dillon, 2001), so consequently the primary clinical use of the REAR is for the calculation of insertion gain (REAR minus REUR = REIG). It is also possible that the REAR (or REAG) itself can be used for verification purposes. This requires targets expressed in earcanal SPL, not gain. The most notable fitting method to use this approach is the DSL4.1. As shown in Figure 7, in what's referred to as a SPLogram, it's possible to display targets for soft, average and loud inputs. In this Figure, the extreme lower and upper plots represent the patient's threshold and ULC (Upper Level of Comfort) respectively. The three dashed lines in-between represent the target gain values, which would be verified using the REAR. If you desired to use these targets for verification, and your probe-mic equipment does not display DSL targets, it's relatively simple to print out the targets, take the printout to the probe-mic equipment, and then “eyeball” the goodness of fit when REAR measurements are taken.
Figure 7.
DSL 4.1 SPLogram showing, in ear canal SPL, the patient's hearing thresholds, upper level of comfort, and targets for soft, average and loud inputs.
Most probe-mic equipment does at least convert thresholds and LDLs to the SPLogram format (using average REDD corrections). While this does not provide specific REAR targets for various inputs, it does provide a general “window of acceptability” for the fitting. Though no targets are present, it is fairly intuitive that if the goal of the fitting is to make soft sounds audible, then the REAR for soft inputs must be above the bottom threshold curve. And, if we want to assure that loud inputs are not too loud, the REAR for high inputs must be below the top LDL curve. An example of this is shown in Figure 8, where the patient's thresholds and LDLs have been converted to ear canal SPL, and REARs for 55 and 75 dB SPL inputs have been conducted. This display quickly provides information regarding the audibility of speech signals for the higher frequencies. Observe that for 2000 Hz, the REAR for the 55-dB SPL input is above threshold. However, for 3000 Hz, even when a 75 dB SPL input is used, the REAR is not above threshold. The REAR for the 75-dB SPL input also suggests that higher inputs probably will exceed the patient's LDL in the 1500 Hz range. This information now can be used to re-program the instrument to obtain REARs that fit more appropriately within the patient's residual dynamic range.
Figure 8.
SPLOgram showing, in ear canal SPL, the patient's hearing thresholds, loudness discomfort levels, and REARs for soft and average input levels. (Courtesy of Madsen Electronics)
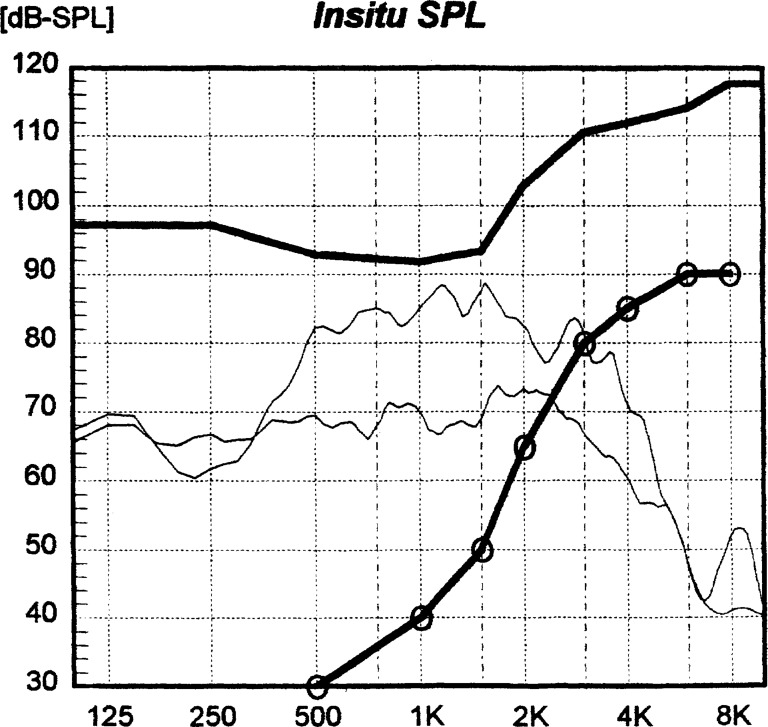
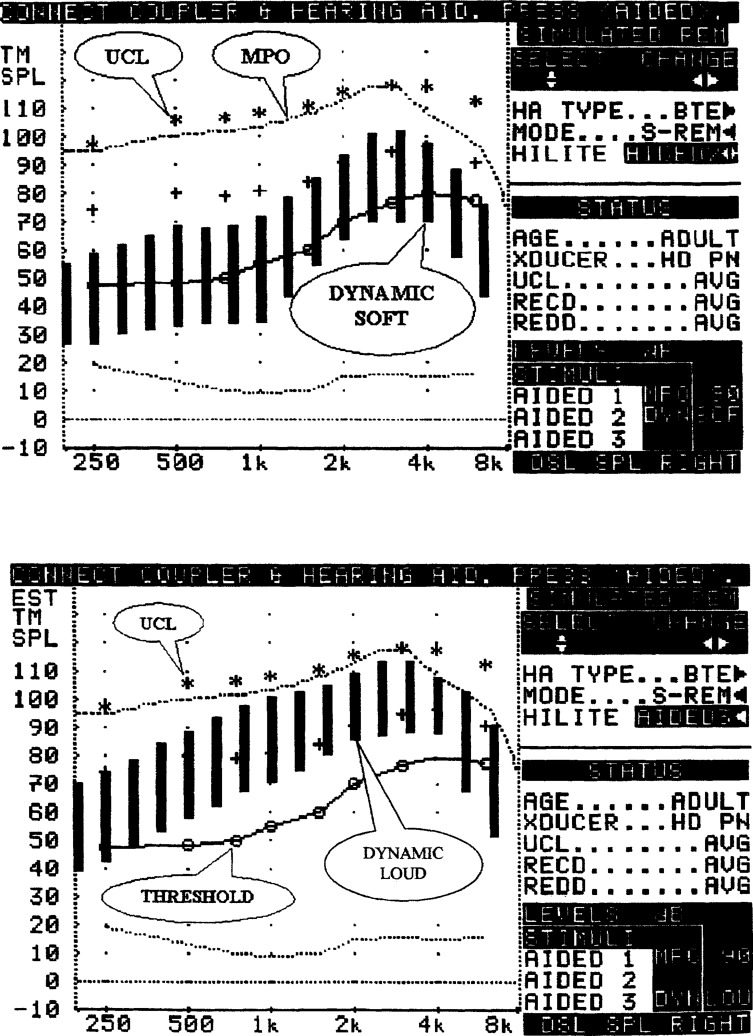
Shown in Figure 9 is the implementation of the REAR verification procedure that is used by one manufacturer of probe-mic equipment. At the top of each of the two graphs, observe the “snowflakes,” which represent the target RESR, and the line below is the actual maximum output of the hearing aid. Shown in the upper panel is the output of the hearing aid for signals representing the range of soft speech (30 dB range) and observe that a substantial portion of each bar exceed the patient's threshold, as desired. On the lower panel, observe a similar plot, except that this graph illustrates the hearing aid's output for signals representing loud speech (bars smaller than 30 dB indicate that the signal is compressed). Again, this is an acceptable finding, as the output falls nicely below the patient's target RESR.
Figure 9.
Top panel: Illustration of the patient's hearing thresholds, uncomfortable loudness levels, the hearing aid's maximum power output, and the range of output for a dynamic soft signal (represented by vertical black bars). Bottom panel: Same as top panel, except illustrating range of output for a dynamic loud signal.(Courtesy of Audioscan).
Using the REAR to verify the fitting seems quite logical, as everything is referenced to earcanal SPL, and the RECD allows us to easily go from the real ear to the 2-cc coupler. And, the upside-down audiogram really does start to look quite normal after a while. But, for some reason, the SPLogram verification approach seems to be shunned by most everyone using probe-mic measures. Three years ago, in a survey conducted by The Hearing Journal, (Mueller, 1998) a group of dispensers who owned probe-mic equipment were asked what probe-mic procedures they used “routinely.” The REAR and REIG tied for the highest rating; 36% of the respondents stated that they routinely used each. Since it's necessary to conduct a REAR to calculate the REIG, these results would suggest that the REAR is seldom used in isolation.
In addition to verification of prescriptive targets, the REAR can be used to verify special features of the hearing aid. A useful way to verify the performance of directional microphone hearing aids, for example, is to conduct REARs with the input signal originating at various azimuth locations. We'll talk more about that later in this article.
REIG
As we've already discussed, the clinical application of the REIG is to verify prescriptive fitting targets. If it's close to target, the fitting is verified. If it's not, repeated adjustments are necessary. But what is close? For 20 years audiologists have stood back, stared at the probe-mic monitor screen, squinted, and asked themselves “Is that response close enough to target to let this guy go?” Years before probe-mic testing was introduced, Supreme Court Justice Potter Stewart must have had a premonition that we would be faced with this dilemma when in 1964 he said:
“I shall not today attempt further to define it … and perhaps I never could succeed in intelligibly doing so. But I know it when I see it.”
It is unfortunate that prescriptive targets are displayed as a single value, as they really represent a range for an acceptable fitting. The single target value, often displayed for the dispenser and patient to see, encourages some people to try to attain a level of preciseness that isn't necessary (or even real). It's not uncommon that hearing thresholds are measured with old, floppy TDH earphones, using 5-dB steps, but an REIG finding that deviates by 3 dB from target is consider unacceptable. Each office or clinic must establish its own rules for what is “close enough”, but given the lack of preciseness in threshold measurement and the variability of applying average prescriptive targets to individual listeners, a ± 6 dB REIG deviation from target would certainly seem acceptable (see Mueller, 1992d for a review of acceptable REIG findings).
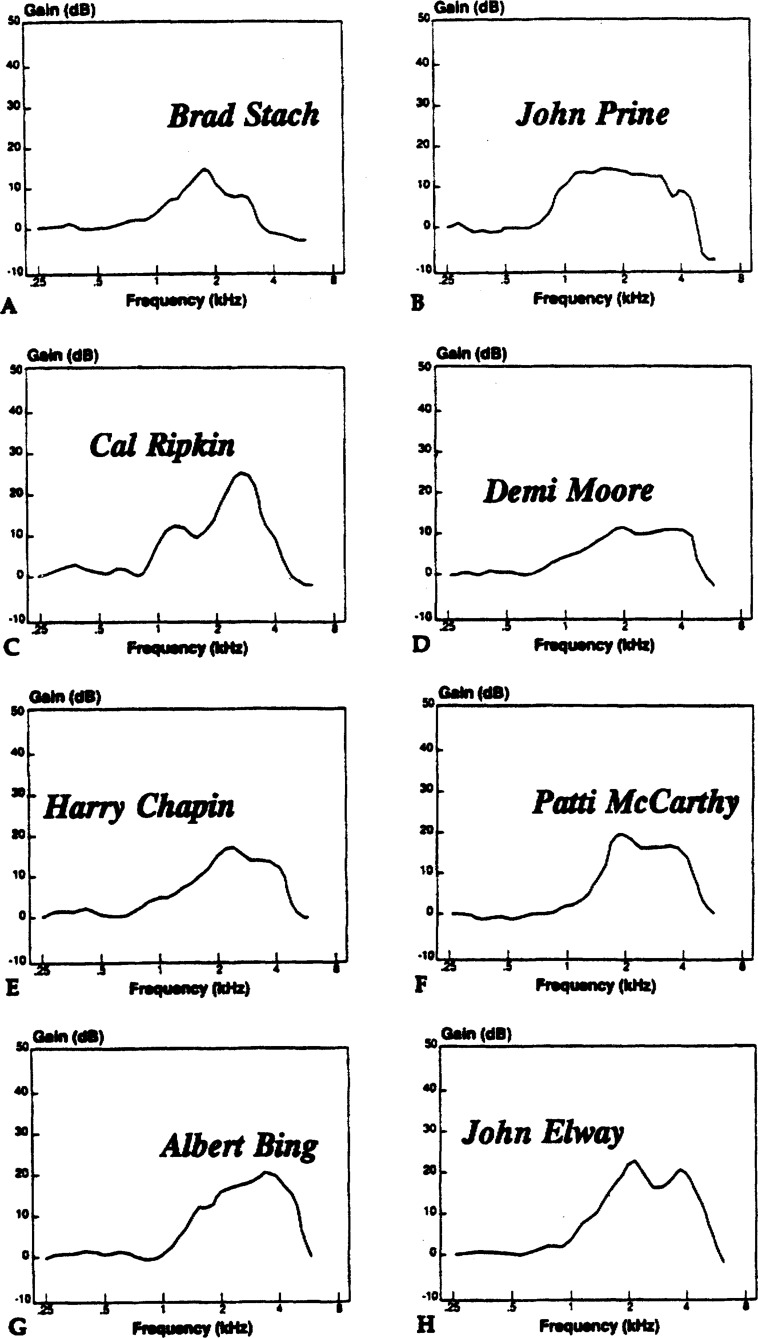
When comparing REIG findings to prescriptive targets, one cannot forget the huge influence of the individual's REUG. When we first started conducting probe-mic testing in the early 1980s, the hearing aid technology we were using had little or no insertion gain in the high frequencies. Graduate students often would ask, “How can I obtain more insertion gain at 3000 Hz?” My answer was always the same: “Find a patient who has an REUG of 0 dB at 3000 Hz!” A bit absurd, yes, but the point is that you can nearly always predict the goodness of the REIG as soon as you've measured the REUG. For example, take a look at the REUGs shown in Figure 10. We know that if the same ITE hearing aid were placed in each of these ears, the REAR would be very similar (we'll say that all RECDs are the same, which probably wouldn't be the case, but it will keep things simple). The REIG will vary based on the individual's REUG. Let's say that Demi Moore and Cal Ripkin both have a 50 dB hearing loss at 3000 Hz, and we're conducting probe-mic testing using a 50-dB input. We'd like to see about 30 dB of insertion gain for a 50-dB input. What might happen is that the latest DSP hearing aid would be considered “good” when it was fitted to Demi Moore, because there was 30 dB of gain at 3000 Hz (note that her REUG is only 10 dB at this frequency), but the same hearing aid would be considered “bad” when fitted to Cal Ripkin, because it only had 15 dB of gain at 3000 Hz (note that his REUG is 25 dB at 3000 Hz). Yet for both Demi and Cal, the SPL at the eardrum was the same, 90 dB SPL. Was one really a good fit and the other a bad fit?
Figure 10.
Examples of variations observed in the REUG.
As with the REAR, the REIG also can be used to verify several different hearing aid features. If the dispenser is used to looking at REIG curves, then it's probably best to continue to use this same reference when observing the effects of digital noise reduction, adaptive feedback, and other dynamic hearing aid signal processing.
RESR
Though not part of the ANSI standard, the use of the RESR term (and the measurement) dates back to the early days of probe-mic testing. This test is conducted with the volume control (VC) “full-on” (or just below feedback) using a 90 dB SPL input signal. Think of it as conducting the 2-cc coupler OSPL90 measure in the real ear (although this is only partially true, as the measurement is taken with the hearing aid's maximum output adjusted for the patient). In other words, we want to create a “worse case” measure in the clinic, to assure that there is not excessive aided loudness in the real world. If the patient's hearing aid doesn't have a VC, then the programmed gain setting would be the level for conducting the measure. The clinical application of the RECD is twofold: to assure that the hearing aid's maximum output does not exceed the patient's “comfort” levels, and to assure that the maximum output does not exceed “safe” levels.
A concern which has been associated with the RESR since it was first introduced is the potentially high levels of sound that can be present is the ear canal while conducting this procedure. In a worse case scenario, a linear hearing aid with a coupler output of 140 dB SPL could be driven to its maximum if the VC was set to “max” and the input was a pure-tone. If the residual ear canal volume was small (e.g., deep earmold, young child, or both), the output in the ear canal could be 150 dB SPL or higher. This raises the concern of acoustic trauma during the test procedure. We assume that the prudent dispenser would assure that levels of 150 dB would never be delivered to a patient, however, it could happen, and probably has. I suspect there could be a liability issue if the RESR procedure was encouraged by an ANSI standard. Fortunately, it's easy to predict the RESR if you know the patient's RECD.
The RESR procedure, especially with adults, is less critical today than it was ten years ago or so when the most common fitting was a linear peak clipping hearing aid. Today, we commonly fit WDRC hearing aids with low compression kneepoints. Hence, even if the hearing aid's maximum output is 120 dB SPL, if the WDRC kneepoint is set to 40 dB SPL, and a compression ratio of 2:1 or so is applied, it's unlikely that the ear canal SPL output of that hearing aid will ever reach the maximum. Additionally, many digital hearing aids have a front-end AGCi compressor, often with a kneepoint as low as 90 SPL (10:1 ratio). This too often has the effect of reducing the maximum output of the hearing aid in the real world.
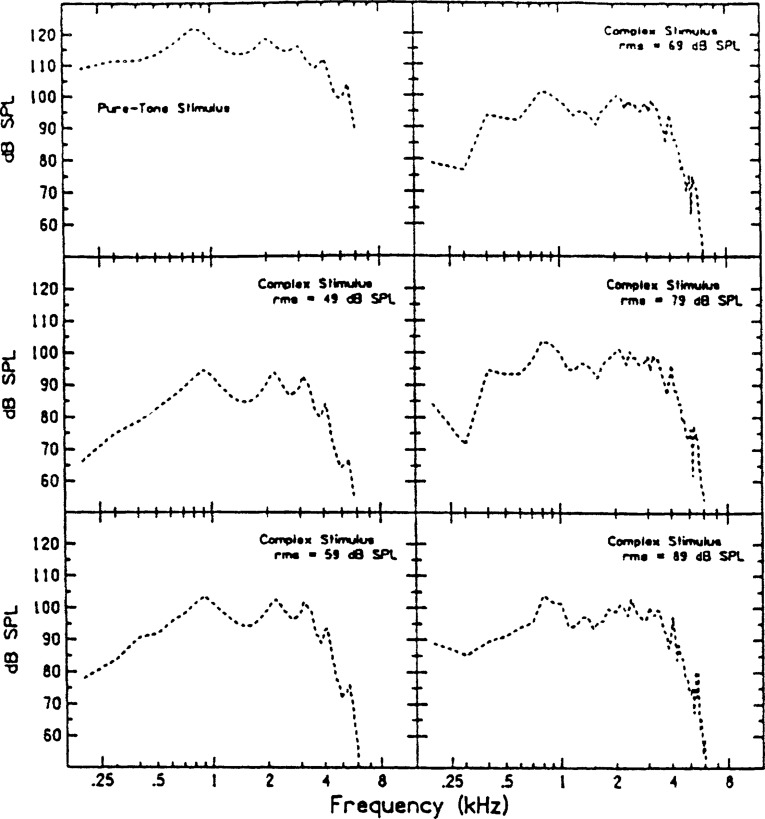
If you do choose to conduct RESR measurements, it's important to remember that the input signal significantly can influence the results—the spectrum level of the output at a particular frequency using a broadband signal will be lower than the total rms. output. The question then becomes, do you want to set the maximum output of the hearing aid for the most common signals the patient hears (broad-band signals like speech) or do you want to set the maximum output of the hearing aid for the occasional narrow-band signals the patient hears. There is significant difference in output values, as illustrated in Figure 11, taken from Stelmachowicz et al (1990). Observe the maximum output for this hearing aid for a pure tone (upper left panel) compared to the saturation output for a complex signal (lower right panel)—the maximum output is 15 to 20 dB higher for the pure tone input. A conservative approach would be to adjust the maximum output of the hearing aid using pure tone inputs, as many signals that the user experiences do have a narrow-band spectra and will drive the hearing aid output close to this level (see Stelmachowicz, 1991).
Figure 11.
Top left: Maximum output curve for a hearing aid with a 90 dB SPL pure-tone input. Other curves show the output from the same hearing aid with a complex noise ijnput at 49, 59, 69, and 89 dB SPL. The hearing aid is saturated at inputs of 59 dB SPL and above. From Stelmachowicz P, Lewis D, Seewald R, and Hawkins D (1990). Complex and pure-tone signals in the evaluation of hearing-aid characteristics. Journal of Speech and Hearing Research, 33, 380–385.
RECD
If you fit hearing aids to infants and children and do not own probe-mic equipment, the ability to conduct this procedure alone would justify the purchase. If we know a child's RECD, we have information that will assist us in selecting the appropriate hearing aid output and predicting the output in the child's ear (OSPL90 + RECD = Predicted RESR). Moreover, on the day of the fitting, the majority of the patient-specific hearing aid adjustments can be made in the 2-cc coupler, reducing the time and cooperation required from the child. The RECD of a child can be quite different than those of an adult. If this isn't something you've thought about before, take a look at the average RECDs for different ages shown in Table 1.
Table 1.
Average RECD values by age
| A. RA-1 coupler | |||||||||
| Frequency (Hz) | |||||||||
| |
250 |
500 |
750 |
1000 |
1500 |
2000 |
3000 |
4000 |
6000 |
| 0–12 months | 5.4 | 9.8 | 10.0 | 13.0 | 14.4 | 14.5 | 18.5 | 21.6 | 22.4 |
| 13–24 months | 7.3 | 10.2 | 9.9 | 12.6 | 13.7 | 14.2 | 16.1 | 18.5 | 15.5 |
| 25–48 months | 4.0 | 8.5 | 8.7 | 11.8 | 13.2 | 13.2 | 15.5 | 16.2 | 15.4 |
| 49–60 months | 2.8 | 8.0 | 8.5 | 9.8 | 11.9 | 12.7 | 14.0 | 15.0 | 14.8 |
| > 60 months∗ |
2.2 |
4.6 |
4.3 |
6.3 |
7.7 |
8.8 |
11.2 |
13.1 |
13.7 |
| B. RA-2 coupler | |||||||||
| Frequency (Hz) | |||||||||
| |
250 |
500 |
750 |
1000 |
1500 |
2000 |
3000 |
4000 |
6000 |
| 0–12 months | 5.5 | 9.7 | 9.6 | 11.9 | 11.6 | 10.5 | 16.2 | 19.4 | 17.8 |
| 13–24 months | 7.4 | 10.1 | 9.5 | 11.5 | 10.9 | 10.2 | 13.8 | 16.3 | 10.9 |
| 25–48 months | 4.1 | 8.4 | 8.3 | 10.7 | 10.4 | 9.2 | 13.2 | 14.0 | 10.8 |
| 49–60 months | 2.9 | 7.9 | 8.1 | 8.7 | 9.1 | 8.7 | 11.7 | 12.8 | 10.2 |
| > 60 months | 2.3 | 4.5 | 3.9 | 5.2 | 4.9 | 4.8 | 8.9 | 10.9 | 9.1 |
While most everyone agrees that the RECD is an important measure, there does not seem to be a standard test procedure. And, different procedures do lead to different results. For example, the signal can be delivered to the ear using the patient's own hearing aid, an insert earphone coupled to the patients earmold, or an insert earmold coupled to a foam plug. The 2-cc coupler used for comparison could be either HA-1 or HA-2. In fact, if you wanted to push the RECD rules, you could deliver the signal to the ear with a TDH-series earphone, compare that to the output in a 6-cc coupler, and still call your findings an RECD. All this sheds some light on why the “ANSI standards people” did not include the RECD.
There are many factors that complicate the precise description of the measurement, and some of them are as follows:
If the measurement is conducted using the patient's own hearing aid, MLEs become part of the RECD (assuming the testing is conducted in the soundfield; if direct audio input is used, then the MLE is not included). If a given prescriptive fitting approach (such as DSL or NAL-NL1) or a manufacturers' software already includes average MLEs, and they allow you to enter the patient's RECD, then it's possible that the MLE will be added twice. Recall that the CORFIG is calculated by the formula: REUG -RECD + MLE, which assumes that the MLE is not part of the RECD.
The MLEs for a hearing aid tested using a moderate input level are not the same as the MLEs when the hearing aid is in saturation. One of the uses of the RECD is to predict the output of the hearing aid when it is in saturation, yet the hearing aid REAR measurement usually is conducted using a 60 dB input.
If the patient is fitted with a WDRC instrument, then it is necessary to consider the effects of WDRC on the MLE. That is, if a 60 dB signal at 4000 Hz becomes a 70 dB input because of an MLE of 10 dB (CIC fitting), the increase in output will not be proportional if the input signal is compressed (e.g., if the compression ratio is 2:1, the MLE will now only yield a 5 dB change in output).
If a HA-1 coupler is used, the RECD will be different than if a HA-2 coupler used (see Ricketts and Bentler, 1995 for review).
If an inset earphone is used, the output impedance effects need to be the same as for the patient's hearing aid.
If a foam plug is used, the placement depth in the ear canal should approximate the depth of the patient's hearing aid or earmold.
Some of these factors only amount to a couple of dB, but take two or three of these factors, which all might influence the RECD in the same direction, and you have significantly changed the hearing aid fitting. What to do?
At one time, in an attempt to address one of these issues, the relationship between the MLE and the RECD, Seewald et al (1997) suggested that we adopt a new term, the TEREO (Transform for Estimating Real-Ear Output), which is the RECD + MLE (See Mueller and Hall, 1998, page 362 for review). This would allow us to then use the TEREO when we converted 2-cc coupler output to the REAR, but still use the RECD when we were converting maximum output between the two references. Although it's a fun acronym to say, we haven't heard much about the TEREO since it's introduction.6
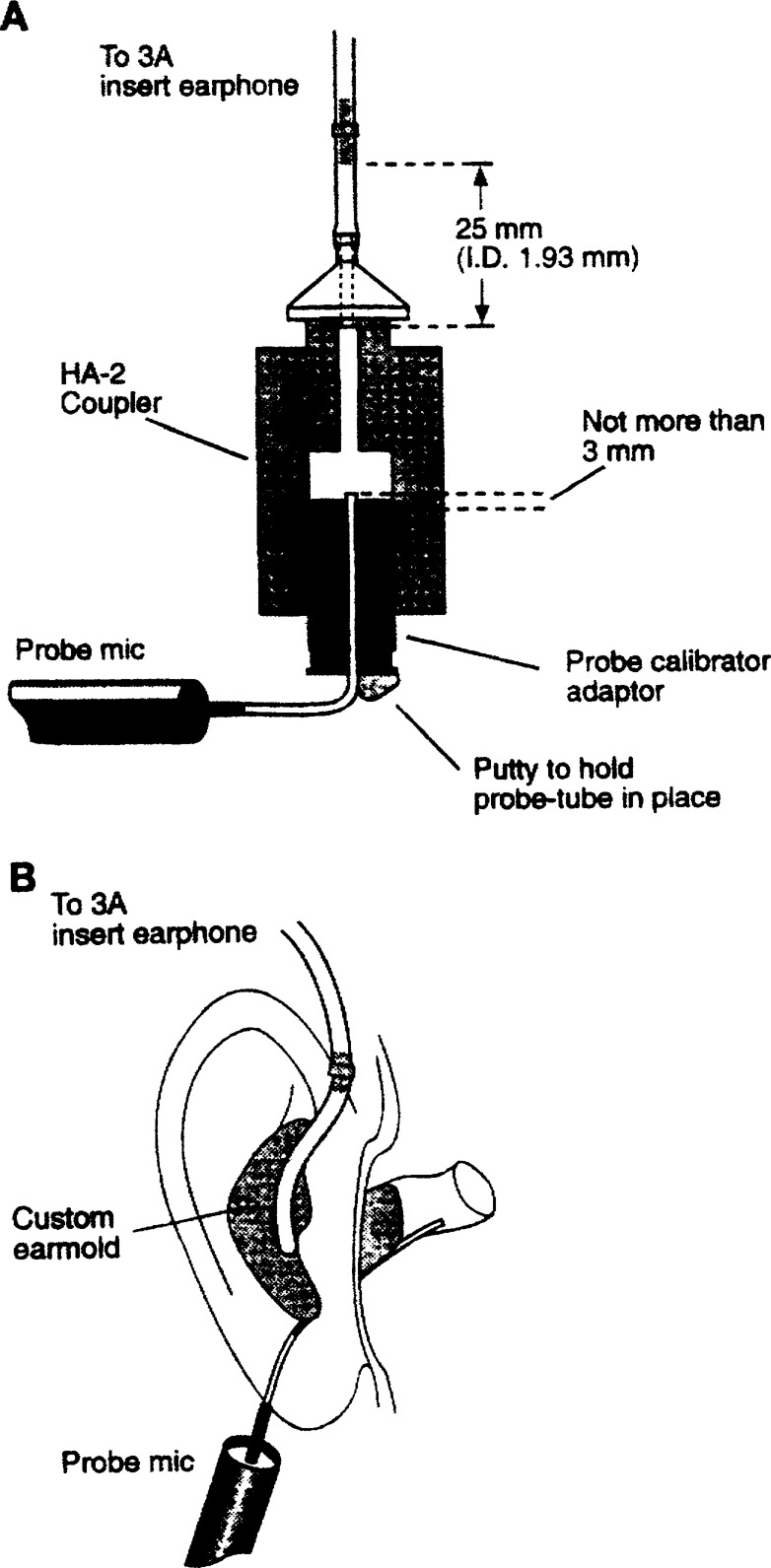
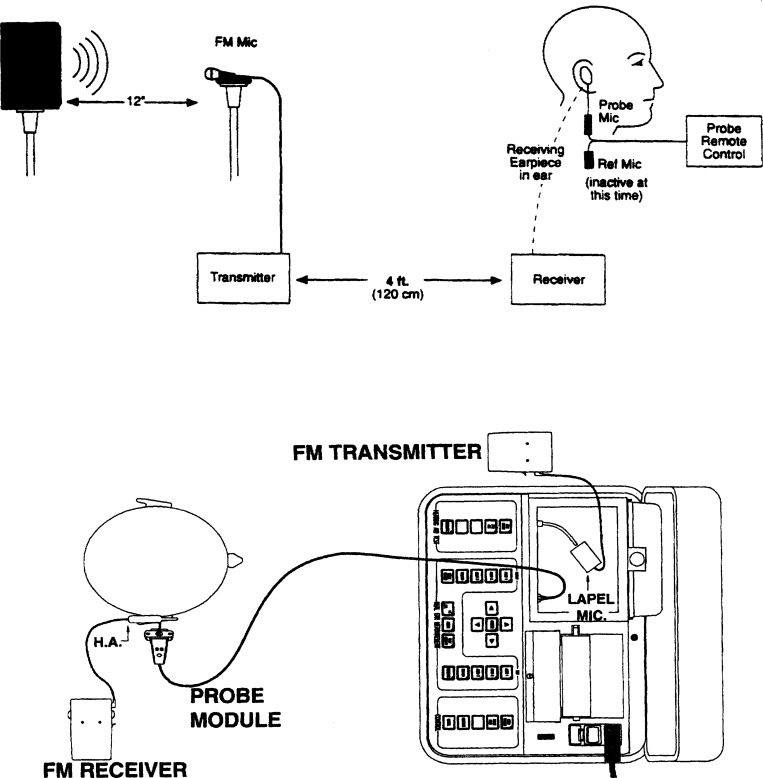
I think we all agree that the most important use of RECD measurements is with infants and children. Since there is no standard protocol, it seems reasonable that we should use the RECD procedures recommended by the people who have conducted the most research with this population. This of course is the research group from the National Centre for Audiology at the University of Western Ontario (see review by Seewald, 2000). In 1994, Moodie et al. described an RECD procedure, using the Foxix 6500 equipment, which utilized insert earphones, a HA-2 coupler, and the child's own earmold (see Figure 12). Specifically, the procedure they described is as follows:
Figure 12.
Illustration of apparatus for conducting the RECD. From Moodie KS, Seewald RC, Sinclair ST (1994). Procedure for predicting real-ear hearing aid performance in young children. American Journal of Audiology, 3(1), 23–31.
Conduct appropriate calibration and configure the software of the probe-mic equipment for RECD measurements (this procedure will vary depending on manufacturer of the probe-mic equipment).
Connect the insert earphone to the loudspeaker output terminal of the probe-mic equipment using a matching phone plug.
Thread the probe tube through the calibrator adapter plug so that the tip of the tube extends no more than 3mm above the surface of the plug.
Place the calibrator adapter plug into the microphone port of the HA-2 2-cc coupler.
Connect the probe tube to the probe microphone.
Connect the insert earphone tip to the tubing of the HA-2 2-cc coupler.
Deliver a speech-weighted signal of 50 dB SPL, and record the coupler output. Save this as the “unaided” measure (REUR).
Remove the probe-microphone apparatus from the coupler and place the tube in the patient's ear with the probe tip at the appropriate depth.
Place the patient's earmold in his or her ear.
Attach the insert earphone tip to the tubing of the earmold (the length of the earmold tubing should be appropriate for BTE hearing aid use).
Deliver a speech-weighted signal of 50 dB SPL, and record the real-ear output. Save this as the “aided” measure (REAR).
Either automatically, or through software command the probe-mic equipment will calculate an “REIG,” which in this case is not an REIG, but an RECD. What will be displayed is the coupler output subtracted from the real-ear output for all test frequencies.
Positive values are added to the OSPL90 to predict the RESR, and subtracted from ear canal SPL targets to determine appropriate 2-cc coupler output.
The above protocol is unique to a specific probe-mic system. The UWO group have published articles using other probe-mic equipment, and several of the above steps are not necessary, or differ slightly (e.g., see RECD applications notes at www.audioscan.com for review).
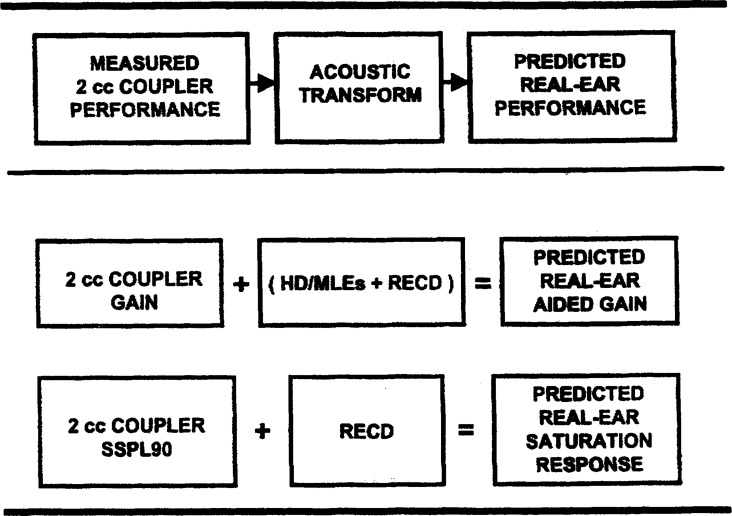
These procedures have been used successfully for several years, and have been found to be a highly accurate predictor of real-ear output. It all does become a little confusing, however, so perhaps the boxes shown in Figure 13 will help in understanding the relationships. In recent research using this approach, Seewald et al (1999) compared the predicted REAG and RESR to the respective measured values for 14 children fitted with BTE hearing aids (head diffraction and MLE effects were included for the REAG prediction). Their results showed a 95% confidence interval of ± 2.3 dB for the REAG and an average error range of 4.4 dB for the RESR. These finding illustrate that if appropriate probe-mic measures are employed with infants and children, the certainty of the hearing aid fitting is probably greater that the certainty of their audiometric thresholds.
Figure 13.
Illustration of acoustic transform steps. From Seewald RC, Moodie KS, Sinclair ST, Scollie SD (1999). Predictive validity of a procedure for pediatric hearing instrument fitting. American Journal of Audiology, 8(2), 143–152.
In addition to children, another group of patients where the individual's RECD is a useful transformation is people with middle ear pathology. Middle ear impedance can have a significant effect on the RECD—see review by Fiket-Pasa and Revit (1992). Because the RECD and REAG are proportional, it's important to consider these individual variations so that proscribed 2-cc coupler gain can be adjusted accordingly.
REDD
A final probe-microphone term which you may have heard of in recent years is the Real Ear Dial Difference (REDD) (Mueller, 1995). The purpose of the REDD is to allow you to plot SPLograms—the REDD is added to the HL thresholds (and LDLs if available) to obtain a plot of these values in ear canal SPL. Most of today's probe-microphone equipment will do this calculation and plotting for you using average REDD values. It's not too difficult to measure individual REDDs, but very few people do it. For one thing, it does require that your audiometer and probe equipment is located fairly close to each other. If you'd like to try it, it goes something like this (conduct the testing with the same audiometer and earphones that you use for evaluating the patient):
Set the probe-mic equipment to operate in the spectral analysis mode (no signal is presented from the probe-mic loudspeaker).
Place the probe tube in the ear canal.
Place the earphone in (insert) or on (supra aural) the ear.
Deliver a continuous pure-tone signal from your audiometer at a selected frequency (50–70 dB HL). It's a relative measure so the intensity of the input signal is not critical—it does need to be above the ambient noise level of the room and the equivalent input noise level of the probe microphone.
While the signal is present, conduct probe-mic analysis. Observe the output of the peak ear canal SPL of the pure tone.
Subtract the HL dial setting from the ear canal SPL reading (e.g., if a 70 dB HL tone was delivered at 1000 Hz, and the ear canal SPL was 82 dB SPL, the REDD for 1000 Hz would be 12 dB).
Positive values are added to the HL threshold to plot the SPLogram.
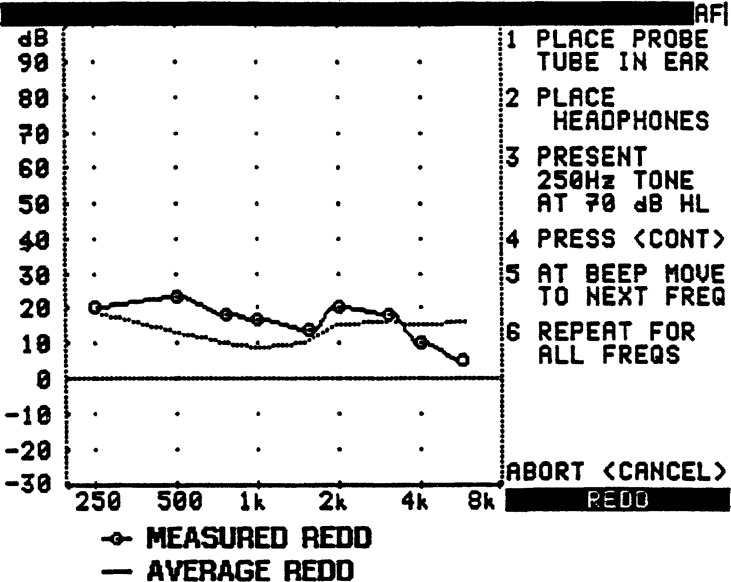
One manufacturer, Audioscan, has streamlined the measurement of the REDD, and Figure 14 is a screen display illustrating this procedure (also showing average REDDs for supra-aural earphones). Consider, that if you knew the difference between the HL dial setting and the coupler (the RETSPL), and you knew the difference between the coupler and the real ear (the patient's RECD), you could add these two correction factors together and have the REDD (which is why it's usually not necessary to measure it). For example, the average RECD for an adult at 3000 Hz is 9 dB, and the RETSPL for insert earphones is 3 dB (we'll assume that the audiometer is appropriately calibrated). So we would expect the average REDD at 3000 Hz for insert earphones to be around 12 dB (9 + 3 = 12), which is similar to what is displayed in Figure 14 for supra-aural earphones.
Figure 14.
Illustration of the measured REDD compared to the average REDD using the Audioscan REDD test procedure.
CORFIG
For simplicity, we'll only use the CORFIG term, and forget about Mr. GIFROC for now. The CORFIG is not really a probe-mic procedure, although most published average CORFIG values were determined using the results from probe-mic testing. And, if you wanted to individualize the CORFIG, you would need to conduct an RECD and an REUG (and you could use your probe-mic equipment to measure MLEs too, or do them simultaneously with the RECD). The clinical application of the CORFIG is to allow us to predict real-ear gain when coupler gain is known, and vice versa. Many of you use the CORFIG more than you realize, as whenever the fitting software from your favorite hearing aid manufacturer plots “simulated real-ear gain” the software is using CORFIGs. In fact, if you were to toggle back and forth between coupler gain and simulated REIG, you could observe the exact CORFIG that is being used (and it probably is different for different companies). It also of course will be different for different hearing aid styles, as the MLE is a critical component of the calculation. Different prescriptive fitting approaches also use different CORFIGs (for both NAL-NL1 and FIG6, on-screen REIG vs. coupler gain comparisons easily can be made).
One might think that converting real-ear gain to coupler gain would be like converting HL to SPL—one set of numbers used by all. It's not that simple. Because of the variability and design of the measurement procedures, CORFIG values from different research labs vary by 5 dB or more with greatest variance in the higher frequencies. All this only increases the importance of conducting real-ear testing rather than relying on average correction values.
RETSPL
The final term we'll discuss is the RETSPL, which allows us to convert HL values to 2-cc coupler SPL. This correction factor is not directly related to probe-mic measures, but certainly relates to hearing aid selection and verification. Most clinics today have their audiometer calibrated by a local Special Instruments Dealer (SID), who is probably a member of NASED (National Association of Special Equipment Dealers). Today's audiometers nearly always can be calibrated within 0.3 to 0.5 dB of the ANSI standard values (the SID will let you know how close you are), so usually you can assume that the values listed in ANSI S3.6–1996 are reliable RETSPLs for you to use (in this maze of acronyms, it's important to remember that audiometers have RETSPLs, people don't). In addition to REDD calculations, a common clinical application of RETSPLs is to convert LDL values to 2-cc coupler values when considering the appropriate maximum output of a hearing aid. For example, if your patient had an LDL of 102 dB HL at 3000 Hz (measured with insert earphones), and you knew the RETSPL for 3000 Hz was 3 dB, you could add the 3 dB RETSPL to 102 dB HL value and conclude that this person's LDL, referenced to a 2-cc coupler, was 105 dB SPL. This provides you with guidance for what matrix to order, or where the AGCo kneepoint should be set. For multiple channel AGCo products, this procedure can be applied to shape the maximum output to the patient's loudness function.
We've reviewed several probe-mic procedures, and there are a lot of acronyms and clinical applications to remember—I've provided a quick reference chart in Table 2. Additionally, I've included a chart from Revit (1997)—see Table 3. This Table nicely illustrates the relationship between the various measures that we have discussed. For some of you, much of this does not fit conveniently into your “need to know” compartment. However, probe-mic measures have been identified as the preferred verification procedure in recent consensus publications on hearing aid fitting for both adults and children (Bess, et al, 1996; Valente et al 1998). There's no question that the use of these procedures will add an improved level of preciseness to the hearing aid fitting process—in fact, when these procedure are used, the hearing aid is actually fit, rather than simply dispensed.
Table 2.
A quick reference of the procedures and correction factors related to the real-ear assessment and fitting of hearing aids
| Procedure | Primary Clinical Purpose |
|---|---|
| REUG | To establish a reference for REIG calculation (the UG is subtracted for the AG). |
| REOG | To determine the extent of slit leak, if sound is passing through the vent as desired, and to assure that vent resonance is not excessive. |
| REAG | To verify prescriptive targets (e.g., when using DSL4.1) or to calculate the REIG (AG minus UG = IG). Also for verification of hearing aid features. |
| REIG | To verify prescriptive targets (e.g., NAL-NL1, FIG6), and for verification of hearing aid features. |
| RESR | To assure that the real-ear output of the hearing aid for high inputs is safe and comfortable. |
| RECD | To select appropriate 2-cc coupler output and predict aided maximum output in the real ear based on 2-cc coupler findings (OSPL90 + RECD is the predicted RESR). |
| REDD | To convert from dB HL to ear canal SPL for establishing REAR targets (RECD + RETSPL = REDD). |
| TEREO | To predict output in the real ear (REAR) when the output in the 2-cc coupler is known (TEREO = RECD + MLE). |
| CORFIG | To calculate desired 2-cc coupler gain when desired REIG is known (REUG - RECD + MLE = CORFIG). |
| RETSPL | To convert from dB HL to 2-cc coupler for insert earphones, to 6-cc coupler for supra-aural earphones. |
Table 3.
Comprehensive instructions for navigating the Circle of Decibels
| If you have | And you want | Direct path | Long way around |
|---|---|---|---|
| dB HL | Eardrum SPL | Add the REDD; | Add the 2cc/DD and add the RECD. |
| dB HL | 2cc SPL | Add the 2cc/DD; | Add the REDD and subtract the RECD. |
| 2cc SPL | Eardrum SPL | Add the RECD; | Subtract the 2cc/DD and add the REDD. |
| 2cc SPL | dB HL | Subtract the 2cc/DD; | Add the RECD and subtract the REDD. |
| Eardrum SPL | 2cc SPL | Subtract the RECD; | Subtract the REDD and add the 2cc/DD. |
| Eardrum SPL | dB HL | Subtract the REDD; | Subtract the RECD and subtract the 2cc/DD. |
Frequently Asked Questions
There are many issues surrounding the use of probe-microphone measurements, and space does not permit me to review all of them—see Mueller et al (1992) or Revit (2001) for a more complete review. In this final section, however, I will address some of the more commonly asked clinical questions, including some procedural issues, the assessment of compression, directional microphone technology, the features of digital hearing aids, and other special amplification features.
Procedural Issues
Is there as easy way to know if the probe tube has been placed correctly?
The general rule is that you'd like to have the tip of the probe tube within 5-mm of the TM, and 3–5 mm beyond the medial tip of the hearing aid (or ear mold). There are three commonly used procedures to help you accomplish this:
Bump-and-pull. This method is used quite frequently, although often not intentionally. The probe tube is gently slid down the ear canal until the tip of the tube bumps the patient's TM—don't worry, they'll tell you when you're there. Warn them in advance that they might feel a “little tickle.” Once you obtain the patient's response, pull the tube back a little, and you know you're deep enough. This method is not recommended for infants and children or highly excitable people.
30-mm rule. We know that the average ear canal is around 25-mm long and the average distance from the opening of the ear canal to the intertragal notch is 10 mm. So if we put the probe tube sleeve marker 30-mm from the tip and slide the tube down the ear canal until the marker is at the intertragal notch, we should be about 5-mm from the TM. If it's obvious that a person has a short ear canal (usually a petite female), or a short distance between the intertragal notch and the opening of the ear canal, place the marker at around 25–27 mm (or you'll be doing bump and pull). This method also is not recommended for infants and children, as the dimensions of their ears are quite variable.
Earmold or hearing aid as a guide. This is the method that many people use for children. Position the probe tube along the inferior portion of the child's earmold or custom hearing aid, extending the tip of the tube 2 or 3-mm beyond the tip of the earmold (hearing aid) and then place the sleeve marker equal to the inferior lateral portion of the earmold (hearing aid). This should result in the marker being placed in the region of the intertragal notch.
Is probe tube placement different for deep CIC fittings?
For the most part the rules are the same, although when the hearing aid extends deeper into the earcanal, and the residual volume becomes smaller, it's not necessary to extend the tip of the probe tube beyond the tip of the hearing aid (see Scollie et al, 1998, for review of probe placement with CIC hearing aids). Also, if it's a tight fitting CIC (or any tight fitting hearing aid style), it's likely that the tube itself will cause a slit leak, so if you don't already have a vented fit, you'll probably underestimate true gain at 250 Hz and below.
Is there a probe-mic measure that will help determine if the tube is deep enough?
Yes there is, although it's not commonly used. By observing standing waves in the ear canal, the distance between the probe-tube tip and the eardrum can be predicted fairly accurately. First, the examiner finds the position of the tube in the ear canal where a 6000 Hz warble tone is at it's minimum, which will be close to 14 mm from the eardrum for most adults. The tube then can be further inserted a known distance, to reach the desired point—e.g., an additional insertion of 8 mm would place the tube approximately 6 mm from the tympanic membrane. This procedure was first suggested by Sullivan in 1988, and more recently reviewed by Storey and Dillon (2001).
Is it okay to place the probe tube through the hearing aid vent?
It sure is tempting to put it there, isn't it? If your tube is small and your vent is big, it's okay. One thing that is being measured when we conduct probe-mic testing is the acoustic affects of venting. If the probe tube fills all or most of the vent, then the resulting measurement will not represent true gain (the greatest mistake will be in the low frequencies). On the other hand, if it's an IROS vent, I doubt that placing a probe tube through the vent will influence the test results.
For children wearing hearing aids, who are followed every three months or so, is it worth ordering a “probe tube vent” for their earmold?
Your earmold manufacturer can place a vent in the earmold for the purpose of conducting probe-mic measures (since probe tubes do come in different diameters, I would send a sample tube of what you use along with the ear impression). When you do the testing, the probe tube is threaded through this vent (it's a little difficult to do—you'll need to use a good lubricant) and can be held in place with Fun-Tak during testing. This procedure helps assure that that the tip of the probe tube extends beyond the tip of the earmold. A second advantage is that you only have one thing to hold on to when you place the earmold in the ear. When testing is competed, the vent is plugged. Is it worth the time and effort? I know people who frequently test children who do not use this approach. If you're fairly new to pediatric evaluations, it might add some “comfort” to the test procedure knowing that you have a good placement of the probe tube tip.
How often does the probe tube get “squashed” and give unreliable results?
People tell me that this happens, but I wonder if maybe they just didn't have the tip of the tube past the end of the hearing aid. I think it's unlikely that this will happen. A few years back we compared REIG to functional gain on 28 ears of people fitted with deep-canal CIC instruments (Mueller and Ebinger, 1997). It would seem that if the tube were going to be crimped, this would be the type of fitting when it would happen. Our results showed the same gain for both procedures at 4000 Hz—if there had been a problem, it would have had the greatest effect on the gain for higher frequencies; functional gain for 4000 Hz would have been higher than REIG. Seewald et al. (1996) conducted a similar study with deep fitted CICs, using a probe tube from a different manufacturer. These researchers also reported the same gain at 4000 Hz for both functional gain and REIG.
Should probe tubes be thrown away after each use?
Yes. Infection control is a concern is any office or clinic. I doubt that anyone would use the same tube on different people, but I know some clinics have a protocol that recommends taping the tube in the patient's chart for use on follow-up visits. Not a good thing to do, as this simply allows time for the growth of bacteria. The last time I checked, probe tubes were selling for around $1.00. Given that they are normally used for testing hearing aids that sell for thousands of dollars, a $1.00 investment to help avoid spreading infection doesn't seem like an unreasonable expenditure.
What if the tube becomes plugged with cerumen? Is there a way to clean it?
This usually is a “throw-away” situation, and a persistent clinician can go through many tubes during a single test session. I doubt that cleaning would work very well (you don't want moisture in the tube), but if your clinic is on a tight budget, there could be a solution. If your probe-mic system calibrates the probe tube (and not all do), then you simply could snip off the tip that is plugged, recalibrate the tube, and continue to use it for testing.
Are there rules for how the patient should be seated relative to the loudspeaker of the system?
There are several procedural considerations when conducting probe-mic measures, and most of them can influence the test results (see Hawkins and Mueller, 1992, for review). Regarding loudspeaker placement, most people do the testing with the loudspeaker directly in front of the patient, and it should be at a horizontal plane with the patient's head (if anything, higher, not lower than the patient's head). One manufacturer recommends testing using a 45-degree azimuth. While you can obtain fairly reliable results with most equipment with the patient sitting six feet from the loudspeaker, I prefer something more like 1.5 feet. There are some advantages of having the hearing aid closer to the sound source.
When testing hearing aids with low compression kneepoints, you'll often want to use a low-level input to obtain the best estimate for gain for soft speech. This input must be above the noise floor of the test room for the equipment to operate properly. As the patient sits closer to the loudspeaker, you improve the signal-to-noise ratio, which allows for testing at lower inputs.
When testing using high inputs (80 dB or higher), it's possible to overdrive the loudspeaker of the system (some units will abort the run when this happens). This usually isn't a problem if the patient is seated 1–2 feet from the loudspeaker, rather than 2–4 feet (the old half-the-distance rule).
Of course, no matter how carefully you position them; patients will do many things to disturb the reliability of the testing. Here are a few to watch out for (modified from Tecca, 1991):
The “No-Neck.” This person will continually scrunch down in the chair making it virtually impossible to position the tube or align the head for testing.
The “Crane.” The opposite of Mr. “No-Neck.” This person sits as straight as possible, craning the neck to the ceiling—only to bring it to a more natural position right in the middle of a test run.
The “Scooter.” After being seated appropriately close to the loudspeaker, he scoots the chair back the moment he thinks that you are not looking.
The “Professor.” His eyes are glued to the monitor, and he will lean forward to observe the results even more carefully the moment a curve begins to appear.
The “Impressionist.” As soon as the test signal begins, he will turn the test ear toward the loudspeaker.
The “Motor Mouth.” This person cannot wait for the test to be completed before commenting on the results, and he probably shouts out “I hear it” as soon as the input signal is presented.
What is the best input signal to use?
There may not be a “best,” as it is somewhat dependant on the purpose of the measurement you are making. Most people prefer a “speech like” signal, however, some prescriptive targets are based on narrow-band signals. Also, if you're trying to determine the maximum output of the hearing aid (especially for an infant or child), you might want to use narrow-band signals.
Is it possible to use real speech as the input signal?
Real speech would seem like the ideal signal for many applications, and at least one manufacturer of probe-mic equipment promotes this approach. But, if you're using real speech, you then would need fitting targets for this input, which are not the same as for swept tones or speech weighted composite noise. I would expect however, that we'll see more applications of different speech signals inputs—see the work of Stelmachowicz and colleagues (1996) for a review.
How reliable are probe-mic test procedures?
Quite good. A few years' back David Hawkins and colleagues (1991) provided us with some test-retest data. They showed mean test-retest differences for the REUG to be from 1.0 to 1.6 dB from 1000 to 3000 Hz. As expected, the mean test-retest differences for the REIG were a little higher (because now we have the variable of hearing aid or earmold insertion), but these values were still a respectable test-retest of 1.5 to 2.0 dB from 1000 Hz to 3000 Hz. These values are even more impressive when you consider that the alternative is sound field testing, which has much poorer test-retest reliability.
Compression Instruments
Is it possible to see the difference between peak clipping and AGCo using probe-mic measures?
Probably not, although I have noticed that using a composite speech signal the response curve for a peak-clipping instrument will become somewhat jagged when high inputs are used—whether you observe this might depend on the degree of curve smoothing that you are using. In general, however, the REAR for a high input level will look pretty much the same for peak clipping and AGCo if the output is limited at the same point for both instruments (you might be able to spot curvilinear AGCo, depending on the ratio). If it's a hearing aid with multichannel AGCo, then you might should a difference if you do a family of curves (e.g., 70, 80, and 90 dB SPL), as compression will be activated at different input levels in each channel. Some probe-mic equipment allows you to listen (using earphones) to the output in the real ear while the testing is being conducted, which would provide useful information for this particular comparison (using the earphones is also a nice way to hear the patient's occlusion effect, but that's another question).
Are there special procedures for testing hearing aids with WDRC?
Nothing too special; in fact nothing more than what I'd suggest doing with all hearing aid evaluations. First, I'd avoid using pure-tone sweeps as you might see some strange results if your input level centers on the compression kneepoint (the hearing aid could go in and out of compression during the testing). Second, you would want to observe the effects of different inputs on the REIG; most dispensers use the inputs of 50, 65 and 80 dB SPL as a routine protocol, which provides an estimate of gain for soft, average and loud speech.
How do you conduct probe-mic assessment of WDRC instruments if the hearing aid is always in compression?
One of the goals of most hearing aid fittings is to assure that soft speech has been made audible. This means that you would like to know the real-ear gain for inputs of 40–45 dB SPL. Many WDRC hearing aids have kneepoints of 45 dB SPL or lower, which makes it difficult to measure the true gain for soft sounds. Probe-mic systems do not work well when the input level drops into the noise floor of the test room, and anything above the noise floor puts the hearing aid into compression. There are a couple of solutions:
Programmable hearing aids have adjustable compression kneepoints and/or ratios. For determining gain for soft sounds, simply move the kneepoint to a level above the input you wish to use (e.g., place the kneepoint at 65 dB SPL or higher), or adjust the ratio to linear (i.e., 1:1). After the soft input measurement has been made, reset the kneepoints and/or ratios to the appropriate settings, and complete testing for the other input levels.
If you're fitting a WDRC hearing aid that is not programmable, or it does not have a setting for linear, you still can estimate gain for soft speech by doing a little math. For example, if the compression kneepoint of the hearing aid is 45 dB SPL and the ratio is 2:1, you know that gain for soft speech (45 dB SPL) will be about 5 dB greater than the gain you obtain for a 55 dB input, as 10 dB of the input would be in compression (it helps if you know the frequency specific kneepoints of the instrument that you are fitting—just because the specification sheet says “kneepoint = 45 dB SPL,” does not mean it is 45 dB SPL for all frequencies).
With some compression hearing aids there are dips in the REIG, that seem to occur at the same frequencies for different patients. What's causing these dips?
My guess is that you are testing a multichannel hearing aid, are sampling at a fairly high rate, and what you are observing is the crossover frequencies. It could be that the programming software tends to set them at the same frequencies for different patients. Try changing the channel crossover frequency, and see if the REIG dips move. Unless the dips are pronounced, I wouldn't consider this a problem.
Is there a special input signal that should be used for probe-mic testing with hearing aids that have multichannel compression?
The key is to use the signal that is appropriate for the hearing aid and the prescriptive method that you are using. There is an interaction among prescriptive fitting targets, number of compression channels, and the input signal used for probe-mic testing, and this is most noticeable when WDRC is employed. The real-ear gain targets that are appropriate for a single channel instrument using a swept pure tone input (consider that the tone is only in one channel at a time) probably would not represent appropriate gain for an eight-channel WDRC instrument using a broad-band signal (e.g., a broad band signal of 60 dB SPL would not be 60 dB SPL in each channel—the input in the eight channels would sum to 60 dB SPL—so the WDRC “sees” a lower input than 60 dB SPL, which increases channel gain, which is then summed among channels). There is no simple rule to correct for this. I'd suggest that you consult the manual for the prescriptive fitting software you are using, the manufacturer of the probe-mic equipment, or the hearing aid manufacturer of the multichannel product you are testing (some manufacturers have attempted to account for this in their fitting software).
Are real-ear compression ratios the same as what are observed on the fitting screen?
Maybe. A benefit of conducting real-ear measures for a variety of inputs is that you easily will be able to calculate the instrument's “effective” compression ratio, which might not be what you see on the computer screen or in the coupler. If you're already conducting REIGs for inputs of 50, 65, and 80 dB SPL (as most people do), simply look at the reduction in gain as your input increases. For example: the input is increasing in 15 dB steps; if a gain drop of 7 dB or so results for each step, then you can conclude that your effective compression ratio is close to 2:1. If you compute a 1.5:1 ratio for the 50 to 65 dB SPL input step, and a 3:1 ratio for the 65 to 80 dB input step, then you can assume you're evaluating a hearing aid with curvilinear (variable ratio) compression. Compression ratios that are calculated from measurements in the real ear will reflect the effects of the spectrum of the input signal, the duration of the input signal, and the vent effects of the hearing aid (yes, even slit leaks can influence the real-ear compression ratio). In general, I would expect the ratio to be smaller than expected from 2-cc coupler data, especially in the lower frequencies.
It is possible to test the compression release time with probe-mic measures?
It's certainly is not commonly done, and I don't see anyway you could get precise measures, but here's something you could try which at least should separate a hearing aid with a release time of several seconds from one with syllabic compression. Use the spectral analysis mode and set the probe-mic equipment to conduct a continuous monitoring of ear canal output. Talk to the patient in a soft voice (around 50 dB SPL); observe the ear canal output. Then quickly raise your voice to a loud level (80 dB SPL), and after a few seconds drop your voice back to the 50-dB level. If the hearing has a quick release, the output should be the same as what you originally observed for the soft input. If the initial output for soft is lower than it was before, then you can assume that the hearing aid has a longer release time. This procedure is interesting, but not too precise, so you might just want to look up the release time in the hearing aid specification sheet, or utilize 2-cc coupler measures.
Directional Microphone Hearing Aids
How do you use probe microphone measures to assess the integrity of directional microphone hearing aids?
Probe-microphone measurements could be used to construct a fairly valid “real-ear polar plot,” which could show frequency-specific attenuation and the effects of head diffraction and head shadow. This would require a fair amount of work, however, and really is overkill for the everyday fitting of hearing aids. Rather, my thought would be that the average clinician simply would want to use probe-mic measures to assure that the directional microphone hearing aid is working appropriately (see Mueller and Ricketts, 2000 for review). When this is the goal, running two REAR curves, one at 0° azimuth and another at 180° azimuth should be all you need (easy to do if patient is in swivel chair). Let's say that you usually fit one of two models of directional instruments, either a Sonotone or a Radioear. After testing four or five different models of the Sonotone, which has a cardiod directional pattern, you find that the typical real-ear front-to-back difference (REAR @ 180° subtracted from the REAR @ 0°) for the 1000 to 4000 Hz range is around 20 dB. The Radioear has a hypercardiod pattern, and the typical front-to-back difference for this product is 15 dB. This gives you some clinic norms to work with. Now, if you're testing a patient with his new digital directional Sonotones and you only see a 5 dB front-to-back difference, you know that something is wrong.
Rather than eyeball the differences in the REAR curves, you might want to have the probe-mic equipment plot the frequency-specific front-to-back difference. If so, then try out this test protocol:
Place the patient in a swivel chair.
Set the WDRC to “linear” (if not, the WDRC processing will work to counteract the effects of the directional microphone, producing results that underestimate directionality in the real world).
Use an input signal of 65–70 dB SPL. If you're testing a digital hearing aid, turn off the noise reduction feature, or use test signals designed for assessing digital instruments (e.g., ICRA signals).
Turn your patient around so that you conduct the first run with the loudspeaker of the probe system located behind the patient, at a distance of around 3 feet. Tell your probe system that this run is the REUR.
Now turn your patient back so that he or she is facing forward and conduct the second run with the loudspeaker located directly in front of the patient. Tell your probe system that this run is the REAR.
The probe system will automatically subtract the first run from the second. What is then presented on the monitor is the frequency-specific front-to-back ratio of the directional hearing aid.
An example of using this approach is shown in Figure 15 (ignore the line connecting the circles on the chart—remember that the probe-mic equipment thinks we are conducting an REIG measurement, and therefore it has plotted REIG targets). Observe from the top curve that this hearing aid is providing relatively good attenuation of the signal from the back, and the overall front-to-back difference is around 15–20 dB. In this case, we were interested in the effect of using longer tubing on the earmold, which caused the BTE hearing to slide farther back behind the pinna, but often are more comfortable for the patient. Notice that changing the positioning of the hearing aid lowered the front-to-back difference by nearly 10 dB in the mid-frequencies. Something important to know when tubing length is considered.
Figure 15.
Display of the change in front-to-back ratio for a BTE directional hearing aid by changing the positioning of the instrument on the ear.
How is directionality affected by hearing aids utilizing wide dynamic range compression?
The short answer is, it isn't, but I'll go on. Most of today's hearing aids that employ directional technology also have WDRC, so this is a reasonable question, especially when you think about how WDRC works. We all know that when WDRC is employed, greater gain is applied, as the signal becomes softer. So consider this example: Your patient's WDRC hearing aid (2:1 compression ratio) is programmed to apply 20 dB of gain for a 70 dB input, and he is in a room where there is a 70 dB input originating from in front of him (the person he's talking to) and there is also 70 dB originating from behind him (party noise). With an omnidirectional instrument, the amplified S/N ratio would be 0 dB. But you wisely fit him with a directional instrument, and we'll say that it reduces the input from the back by 8 dB, so now the S/N ratio would be +8 dB (70 + 20 = 90; 62 + 20 = 82; 90 minus 82 = 8 dB). Remember, however, that as the input goes down, gain goes up for a WDRC instrument. This makes it tempting to think that the noise from the back would receive more gain than 20 dB (e.g., for a 2:1 compression ratio, a 62 dB input would receive 4 dB more gain than a 70 dB input, and hence the gain would be 24 dB, not 20 dB. In other words, the WDRC is adding back in 1/2 of the gain that the directional microphone so diligently took away. This doesn't sound like a good thing. This effect, however, only occurs when the sound in question occurs in isolation, with no other sounds present; an unlikely event in the real world, and a situation when directional amplification isn't needed (This situation does exist, however, when probemic measurements are conducted, which is why it is necessary to turn off the WDRC during this testing). It's possible to conduct polar plots with both the signals of interest and competing noise on at the same time. When this method is used, the polar plot is the same for both the WDRC and linear settings of the hearing aid.
If you need more convincing, or just find this topic really interesting, I suggest you check out a recent article from Ricketts et al, 2001. These authors compared four different models of directional hearing aids that could be switched from WDRC to linear processing. Testing was conducted in moderately reverberant rooms, and uncorrected cafeteria noise from five loudspeakers surrounding the subjects was the competing stimulus. The subject's performance for both the HINT and the CST was not significantly different between WDRC and linear processing for any hearing aid model.
What if the probe-mic testing showed no difference between the front and back measurements?
That's certainly possible, which is the main reason that we are doing this testing—to identify a poorly functioning product (before assuming it's the hearing aid, assure that there is not a procedural problem—e.g., the patient turning his head, sound bouncing off a wall near the patient, the back loudspeaker not positioned appropriately for the hearing aid's polar pattern. With ITEs, it's possible that during the buffing of the faceplate, debris was lodged in one or both of the inlet ports, which could disturb the directionality. With some single-microphone directional products, I suspect it's even possible that the microphone attachment to the ports could be reversed during assembly, which would then give the patient the opposite effect of what is desired (e.g., the result would be maximum speech intelligibility in background noise when someone is talking from behind him).
Digital Hearing Aids
When testing digital hearing aids, on occasion there have been symmetrical “bumps” in the lower frequencies (usually below 500 Hz) of the REIG. What's causing this?
My guess is that you are using swept pure tone input, a high sampling rate, and are testing a hearing aid with a fairly large vent. Digital processing takes some time (see review by Agnew and Thornton, 2000), and what you are seeing is the interaction between the unamplified sound passing through the vent, and digitally-delayed amplified signal at the same frequency. I doubt that you will observe this when you use one of the input signals designed for testing digital instruments.
Isn't there a problem conducting probe-mic testing with digital hearing aids that have digital noise reduction?
Only in isolated cases. Many of the digital hearing aids on the market don't even have digital noise reduction, so there's nothing to worry about with these. Of the ones that do, you can turn off the noise reduction feature in the fitting software for nearly all of them. When verifying your desired targets, I would suggest that you turn off the feature before you measure input-specific gain and output, then turn the feature on and do some probe-mic tests to see how the noise reduction works in the real ear. If you don't want to take the time to turn the feature off, or you happen to be fitting a hearing aid where the manufacturer doesn't allow you to turn it off, you can still obtain valid gain values by using input signals designed for testing digital hearing aids. So no, there is no problem.
Is there a way to obtain valid results without turning off the digital noise reduction?
Yes, although turning it off would be my first choice. Of the seven different manufacturers of probe-mic equipment that I'm familiar with (and I don't think there are many others), all of them have some type of signal that can be used to obtain valid hearing aid gain values even when the digital noise reduction feature is on. The key is to have a signal that has random modulations so that the hearing aid does not think that the input is noise and reduce the gain of the instrument (swept pure tones can be interpreted as “noise” by the hearing aid). Depending on the manufacturer, you'll see terms like Dynamic Roving Tone (DRT), Digital Speech In Noise (DSIN), or Modulated Speech Noise (MSN)—check out the articles in this issue of Trends to get the details. Several manufacturers of probe-mic equipment also have incorporated the recently developed ICRA-Noise signals.
What are ICRA noise signals?
Pronounced “eye-crah,” I-C-R-A is an abbreviation for International Collegium of Rehabilitative Audiologists, the organization that the signals were prepared for by a working group dubbed Hearing Aid Clinical Test Environment Standardization (HACTES). There are different types of babble signals available (e.g., male, female, 6 person) for different voice levels (normal, raised, loud), and these “noise” signals have modulation characteristic like natural speech. The signals are available on CD, and as I mentioned, one or more of them have been incorporated into several of the new probe-microphone units (and are available as upgrades to existing units). To evaluate the effectiveness of the ICRA signal, we conducted comparative testing with a DSP instrument—see Figure 16. The top curve shows the ear canal SPL for the ICRA signal with the digital noise reduction (DNR) turned off. The next lower and closely aligned curve was a second measure with the DNR turned on (max setting). Observe that no more than a 2-dB difference was observed. The third and lowest curve is the ear canal SPL when we switched from the ICRA signal to a speech-weighted noise, showing the expected drop in SPL caused by the DNR feature.
Figure 16.
Top two REARs show the effects of digital noise reduction when an ICRA signal is used as the input. The lower curve shows effects of digital noise reduction when speech noise was used as the input signal.
Is it possible to measure how well the digital noise reduction feature is working?
Of course it's possible, and probably should be part of the standard verification protocol anytime that a digital hearing is fitted. It's really quite easy (and fun) to do—especially when you're doing it intentionally and not by accident. You might think it would add a lot of time to the verification process, but assuming that you have the person set up for probe-mic testing anyway, it probably adds no more than another 5 minutes or so per ear. If digital noise reduction is one of the main features that you are “selling,” spending 10 minutes to verify that it is working appropriately does not seem unreasonable to me. And, my guess is that a good demonstration of this feature will improve the patient's understanding (they'll know the attack and release time), which likely will save time on post-fitting visits. Additionally, most of us learn a few things ourselves when we do these measures, which usually improves our troubleshooting and counseling skills.
Here's a protocol that I've used with several different products that seems to work quite well:
Position the patient so he or she can observe the probe-mic display monitor.
Begin testing with the noise reduction feature turned off (if possible).
Present a continuous broadband “noise” signal to the patient at 65–70 dB SPL. This signal remains on for the duration of testing.
Observe the measured REAR (if you want to display the results in REIG, you would first have to store the patient's REUG).
Turn on noise reduction for all channels. Observe the drop in real-ear output (gain). Note the time that it takes for maximum reduction to occur—discussion of the attack time of this feature is important during patient counseling—it's easier to explain if the patient has already observed the change while the hearing aid was in his or her ear.
Now talk to the patient at a level in excess of the continuous noise. Observe that output (or gain) will return to previous levels (at least for some channels) when speech becomes the dominant signal. Note the time that it takes for the noise reduction feature to “release.” Again, the release time of this feature is something that needs to be explained to the patient.
Based on these results, you might decide to change the strength of noise reduction feature, or try using speech and/or noise signals at different input levels to determine how this feature will work for different listening conditions.
Figure 17 is an example of how the results of this testing might look. In this case, we were testing an eight-channel hearing aid, and had the digital noise reduction feature set to “max” for the first four channels (lower frequencies), to “min” for the other four channels. What is barely visible on the chart is the initial gain that we obtained before we activated the noise reduction—this is the faint line that is intertwined with the line connecting the circles (the circles represent target gain for average inputs for the DSL4.1 procedure). Most importantly, observe the dark lower line, which shows that the DNR provided a significant reduction in the noise input for the first four channels. As expected from the programming, for the upper four channels, noise reduction was minimal.
Figure 17.
Display of the effects of digital noise reduction using a speech noise input for an eight channel instrument. Noise reduction was turned “on” for the lower four channels, and “off for the higher channels.
Most digital hearing aids have an expansion circuit Is it possible to test this using probe-mic measures?
Maybe—it depends on the noise in the room where you do your probe-mic testing and the expansion kneepoints of the instrument that you are testing. In many fitting rooms, ambient noise levels are above the expansion kneepoints, which may vary from channel-to-channel, and manufacturer-to-manufacturer, but usually are around 35–45 dB SPL. You could try delivering the lowest input possible from you probe-mic equipment, and then turn the expansion circuit “on” and “off.” If the input is below the kneepoint, the ear canal SPL should be reduced. An alternative method would be to use the spectral analysis feature of your probe-mic equipment, and measure amplified ambient noise (or circuit noise, or microphone noise—you'll measure whatever is the loudest) in the ear canal with the expansion circuit turned “on” and “off.” If your test room is too noisy for either of these approaches, you can always check out the expansion feature using a 2-cc coupler in a test box.
Many digital hearing aids have an adaptive feedback reduction system. Is there a way to use probe-mic testing to observe the effects of this feedback control strategy on the frequency response?
These adaptive feedback systems seem to work pretty well, as we now can detect where feedback is occurring (or will occur) and conduct band-specific gain reductions to reduce it (accomplished through narrow-band notch filters, or through phase alterations). But, rather than looking at simulated results on the computer monitor, it's important to see what is happening in the real ear. If my “digital feedback suppression algorithm” resulted in eliminating all the real-ear gain above 2000 Hz, I just might want to think of a different way of treating the feedback problem.
The real-ear evaluation of the adaptive feedback feature is shown in Figure 18. What I usually do is first conduct an REAR with no feedback present, and leave this on the screen for reference (this is the middle curve on the chart—which is a different color on the screen—most easily observed in the 3000 Hz region). Then, have the person perform a task that will cause acoustic feedback to occur (e.g., opening their mouth widely, holding a telephone receiver to their ear, etc). This is the upper curve in Figure 18, with the peak at 2000 Hz. Allow the adaptive control to cancel the feedback, and then run another REAR. It's easy to observe the effect that the adaptive suppression has on the frequency response, and you then can determine if this degree of change is acceptable (it usually is). This is the curve labeled “AFR” in (Figure 18. Notice that we have maintained the configuration of the original REAR, and are within 2–4 dB of the REAR before feedback. This result certainly is more desirable than having the patient turn down gain, or worse yet, to stop using the hearing aid when feedback situations are anticipated. But, what if we would have observed a 10–15-dB notch taken out of the REAR at 2000 Hz when the adaptive feedback was activated? Without probe-mic testing—how would you know?
Figure 18.
Display of three REARs: 1) middle curve is initial REAR, 2) top curve is REAR when feedback occurred (holding telephone receiver to the patient's ear) and 3) lower curve is the resulting REAR after the adaptive feedback control was activated.
Other Applications
When measuring the occlusion effect, how does the probe-mic results show that occlusion is a problem, or whether the treatment has worked?
As shown back in Figure 1 (lower panel), you can use the probe-mic equipment to calculate the degree of the occlusion effect. You'll find that some people, even with a tight fitting earmold or hearing aid, only have 5–8 dB of occlusion effect (at least for their own voice, it could be greater when they are chewing something hard). I don't have data on this, by my hunch (based on a fair amount of occlusion effect testing) is that if you can reduce the occlusion effect to a level below 10 dB; it probably won't bother the patient very much. And, as I stated earlier, it also will depend on whether the hearing aid has gain at this frequency—the more the hearing aid gain, the less the annoyance from the occlusion effect. If you can take an occlusion effect of 20 dB and reduce to 5 dB or so, I think you've done a pretty good job (of course, you can't make this treatment in isolation, and must consider the goals of the overall fitting—adding unnecessary gain in the lows could reduce the patient's speech understanding in background noise).
What if the patient is unable to sustain a good vocalization for the occlusion effect measure?
This is a problem on occasion, especially with the elderly. As shown in Figure 19, and written about by Revit (1992) and others, you can do occlusion effect testing using a bone oscillator. You might be able to simply plug the oscillator into your probe-mic equipment, or if this isn't possible, a portable audiometer will work just as well (in desperation, you could even use a tuning fork). Figure 19 (from Mueller, 1994) does not show the unaided response (which was around 70 dB SPL at 250), but what is shown is the occlusion effect for two different CIC hearing aids for a 250 Hz bone-conducted input (the hearing aids are turned off). Some limitations of using a bone oscillator are that you do not have information for a broad frequency range, you need to carefully place the oscillator at the same mastoid location each time, and the occlusion effect using this method may not reliably predict an occlusion effect problem for the patient's own voice.
Figure 19.
Illustration of the occlusion effect obtained from two different CICs using a bone conduction oscillator to deliver the stimulus. From Mueller HG (1994). CIC hearing aids: What is the impact on the occlusion effect? The Hearing Journal, 47 (11) 29–35.
Is it possible to evaluate FM systems using probe-mic measures?
It's not only possible, it's recommended. A significant advantage over other methods of evaluating FM systems is that different inputs can be used that represent typical speech inputs experienced by the FM user. Additionally, either measured directly or through the use of the RECD, probe-mic measurements will provide information concerning the maximum ear canal SPL levels of the system. Evaluating FM systems, however, does require some thought, as placement of the FM microphone, the environmental microphone, and the effects of the probe-mic reference microphone can influence the results significantly. If you're interested in this type of testing, I'd suggest you read the review article by Lewis (1999) and also order the instructional video by Lewis et al (1998), which is part of the Phonak Video Focus Series. A helpful booklet accompanies the video.
To provide you with a sample of the set-up for evaluating FM fittings, Figure 20 shows the recommended procedure from two different manufacturers of probe-mic equipment (the top panel is from Frye Electronics and the bottom panel is from Audioscan).
Figure 20.
Sample methods for the probe-mic evaluation of FM systems from Frye Electronics (top panel) and Audioscan (bottom panel).
Is there a standard way to conduct real-ear telecoil testing?
It depends somewhat on why you're testing the telecoil. If it were because the telecoil is used with other technology, then I'd recommend using the procedures that include that technology—telecoil performance for a FM system with a neck loop might be different that the performance obtained in a looped room. The references I provided for the previous question will be helpful.
What about the real-ear testing of the hearing aid telecoil when the patient's only use of the telecoil will be listening on the telephone?
The real-ear verification of telecoil sensitivity is an important measure to conduct during the fitting process, especially with custom instruments, as the orientation of the coil might not be optimized for telephone use. When the telecoil of a custom instrument is evaluated in the test box, it is positioned so that maximum sensitivity is present. This might not be the same orientation that is present between the telephone receiver and the hearing aid in the real ear.
I prefer to do the testing using the output from a real telephone. To do the measurement, place the hearing aid in the telecoil mode, configure the probe-mic equipment for spectral analysis, place the probe tube deep in the ear canal, place to telephone to the ear, and analyze the ear canal output of the telephone signal, which most commonly is the dial tone. After testing your own ear canal output of the dial tone while wearing several different hearing aids, you'll have a good idea of what the aided output should look like, and will quickly be able to identify a telecoil that is not working effectively. Allowing the patient to watch the change in ear canal SPL when the receiver is moved to different locations around the ear also is a good counseling aide for proper receiver placement.
While using the dial tone as an input signal is convenient, and is a fairly effective screening tool, it does not provide any information concerning telecoil gain for the higher frequencies. The truly dedicated dispenser simply would put speech noise on his or her home telephone answering machine, and then “call home” whenever a broadband signal from the telephone was needed. There are other methods, however, which might be less annoying to your friends and relatives—see Hawkins and Mueller, 1992, and Mueller, 1995.
What else can be tested with probe-mic measures?
Well, as I said earlier, the only limitation is your imagination. Want to know the gain that is achieved by cupping your hand behind your ear? What to know how loud your teenager's music is at his eardrum? What to know the spectrum and intensity of “rattling dishes?” What is the SPL of acoustic feedback when the hearing aid is in the patient's ear? What is the SPL of your own voice in the back of your throat (not recommended for beginners!)? Whether the measurement is triggered by necessary, curiosity, or by prudent clinical practice, your probe-mic equipment will be your best friend.
Footnotes
Changing terms in mid-stream is not new for audiologists. You older readers might remember back in the '70s and early '80s when “speech discrimination” became “word recognition,” “impedance” became “immittance,” and “BSER” became “ABR”.
Remembering when to use a CORFIG and when to use a GIFROC, when to add and when to subtract is no easy task, but if you're interested in things like CORFIGs and GIFROCs, you'll enjoy the book chapters by Killion and Monser, (1980) and Killion and Revit, 1993.
The most portable of all probe-mic systems is the ER-33 Occlusion Effect Meter, available from Eytmotic Research. If you're only interested in measuring the occlusion effect, this handy device will let you know if significant hearing aid occlusion is present, and whether a reduction in occlusion occurs following treatment.
Researchers, such as Revit (1991, 2001) have suggested that average REUG values are a more appropriate measure for determining REIG (or in this case “pseudo-REIG”) than the patient's own REUG. This notion is based in part on the fact that prescriptive methods are referenced to soundfield thresholds, yet we typically use earphone thresholds for target calculations. Most probe-microphone units do offer the option of substituting an average REUG when REIG is calculated. While Revit's arguments are compelling, the measurement and use of individual REUGs appears to be a well-ingrained clinical practice.
The reason that a medium sized vent normally is employed is that the patient has normal hearing for the low frequencies, and no hearing aid gain for the low frequencies is programmed in the hearing aid. Hence, the people for whom vent-associated resonance is the most bothersome, are the very people who are the most likely to have it—real-ear gain may be 10 dB or more greater than desired. On the other hand, if the patient has hearing loss in the low frequencies, and 10 dB of hearing aid gain is present, the 10 dB of vent-associated resonance gain is less noticeable (adding equal decibel values is an approximate 3 dB increase in gain).
Since we're speaking of interesting acronyms related to the RECD, we should mention that to the surprise of no one, Larry Revit once proposed that the RECD be termed the Real Ear Volume Impedance Transformation.
References
- Agnew J, Thornton J. Just noticeable and objectionable group delays in digital hearing aids. J Am Acad Audiol 11(6):330–336, 2000 [PubMed] [Google Scholar]
- American National Standards Institute American National Standard Methods of Measurement of Real-Ear Performance Characteristics of Hearing Aids (ANSI S3.46). Standards Secretariat, Acoustical Society of America, New York City, 1997 [Google Scholar]
- American National Standards Institute American National Standard Specification for Audiometers (ANSI S3.6). Standards Secretariat, Acoustical Society of America, New York City, 1996 [Google Scholar]
- Bess FH, Chase PA, Gravel JS, et al. Amplification for infants and children with hearing loss. In Bess FH, Gravel JS, Tharpe AM. (eds). Amplification for children with auditory deficits. Nashville: Bill Wilkerson Center Press, 399–430, 1996 [Google Scholar]
- Chasin M, Pirzanski C, Hayes D, Mueller HG. Real ear occluded gain as a clinical predictor. Hear Rev 4(4):22–26, 1997 [Google Scholar]
- Cox RM. Using loudness data for hearing aid selection: The IHAFF approach. Hear J 48(2):10–17, 1995 [Google Scholar]
- Cox RM, Flamme GA. Accuracy of predicted ear canal speech levels using the VIOLA input/output-based fitting strategy. Ear Hear 19: 139–148, 1998 [DOI] [PubMed] [Google Scholar]
- De Jonge R. Real-ear measures: Individual variation and measurement error. In: Valente M. ed. Hearing Aids: Standards, Options, and Limitations. New York: Thieme Medical Publishers, 72–125, 1996 [Google Scholar]
- Dillon H, Byrne D, Brewer S, Katch R, Ching T, Keidser G. NAL non-linear, Version 1.1. User Manual. Sydney: Australian Hearing, 1999 [Google Scholar]
- Etymotic Research Elk Grove Village, IL, 1977
- Fikret-Pasa S, Revit LJ. Individualized correction factors in the preselection of hearing aids. J Speech Hear Res 35(2):384–400, 1992 [DOI] [PubMed] [Google Scholar]
- Harford ER. The use of a miniature microphone in the ear canal for the verification of hearing aid performance. Ear Hear 1(6):329–337, 1980 [DOI] [PubMed] [Google Scholar]
- Hawkins DB, Alvarez E, Houlihan J. Reliability of three types of probe tube microphone measurements. Hear Instr 42: 14–16, 1991 [Google Scholar]
- Hawkins DB, Mueller HG. Procedural considerations in probe-microphone measurements. In: Mueller HG, Hawkins DB, Northern JL. Probe Microphone Measurements. San Diego: Singular Publishing, 67–90, 1992 [Google Scholar]
- Killion MC, Monser EL. CORFIG: Coupler response for flat insertion gain. In Studebaker GA, Hochberg I. (eds.). Acoustical factors affecting hearing aid response. Baltimore: University Park Press, 149–168, 1980 [Google Scholar]
- Killion MC, Revit LJ. CORFIG and GIFROC: Real ear to coupler and back. In: Studebaker GA, Hochberg I. eds. Acoustical Factors Affecting Hearing Aid Performance, Second Edition. Boston: Allyn and Bacon, 65–85, 1993 [Google Scholar]
- Killion MC, Wilber LA, Gudmundson GI. Zwislocki was right… Hear Instr 39(1):14–18, 1988 [Google Scholar]
- Lewis D, Eiten L, Hoover B, Stelmachowicz P. FM systems for children: Rationale, selection and verification strategies. Booklet accompanying video in Phonak Video focus series. Switzerland: Phonak AG, 1998
- Lewis DE. Selecting and evaluating FM systems. Hear J 52(9):10–17, 1999 [Google Scholar]
- Moryl C, Danhauer J, DiBartolomeo J. Real ear unaided responses in ears with tympanic membrane perforations. J Am Acad Aud 3: 60–65, 1992 [PubMed] [Google Scholar]
- Moodie KS, Seewald RC, Sinclair ST. Procedure for predicting real-ear hearing aid performance in young children. Am J Audiol 3(1):23–31, 1994 [Google Scholar]
- Mueller HG. Probe-mic assessment of digital hearing aids? Yes, you can! Hear J 54(1):10–17, 2001 [Google Scholar]
- Mueller HG. Just make it audible, comfortable and loud, but okay. Hear J 52(1):10–17, 1999 [Google Scholar]
- Mueller HG. Probe-microphone measurements: Yesterday, today, and tomorrow. Hear J 51(4):17–22, 1998 [Google Scholar]
- Mueller HG. Prescriptive fitting methods: The next generation. Hear J 50(1):10–17, 1997 [Google Scholar]
- Mueller HG. Probe-microphone measurements: Unplugged. Hear J 48(1):10–12, 34–36, 1995 [Google Scholar]
- Mueller HG. CIC hearing aids: What is the impact on the occlusion effect? Hear J 47(11):29–35, 1994 [Google Scholar]
- Mueller HG. Terminology and Procedures. In: Mueller HG, Hawkins DB, Northern JL. Probe Microphone Measurements. San Diego: Singular Publishing; 41–66, 1992a [Google Scholar]
- Mueller HG. Assessment of telecoils and assistive listening devices. In: Mueller HG, Hawkins DB, Northern JL. Probe Microphone Measurements. San Diego: Singular Publishing; 227–249, 1992b [Google Scholar]
- Mueller HG. Individualizing the ordering of custom instruments. In: Mueller HG, Hawkins DB, Northern JL. Probe Microphone Measurements. San Diego: Singular Publishing; 183–200, 1992c [Google Scholar]
- Mueller HG. Insertion gain measurements. In: Mueller HG, Hawkins DB, Northern JL. Probe Microphone Measurements. San Diego: Singular Publishing; 113–144, 1992d [Google Scholar]
- Mueller HG. Probe tube microphone measures: Some opinions on terminology and procedures. Hear J 42(1):1–5, 1990 [Google Scholar]
- Mueller HG, Ricketts T. Directional microphone hearing aids: An update. Hear J 53(5):10–17, 2000 [Google Scholar]
- Mueller HG, Hall JW. Audiologists' Desk Reference. San Diego: Singular Publishing Group, 1998 [Google Scholar]
- Mueller HG, Ebinger KA. Verification of the performance of CIC hearing aids. In Chasin M. (ed.) CIC Handbook. San Diego: Singular Publishing Group; 101–126, 1997 [Google Scholar]
- Mueller HG, Bright KE, Northern JL. Studies of the hearing aid occlusion effect. Sem Hear 17(1):21–32, 1996 [Google Scholar]
- Mueller HG, Strouse AL. Survey shows that user judgment remains dispensers' favorite fitting procedure. Hear J 48(10):25–31, 1995 [Google Scholar]
- Mueller HG, Hawkins DB, Northern JL. Probe Microphone Measurements. San Diego: Singular Publishing, 1992 [Google Scholar]
- Mueller HG, Bryant M. Some overlooked uses of probe microphone measures. Sem Hear 1(12):73–92, 1991 [Google Scholar]
- Nielsen HB, Rasmussen SB. New aspects in hearing aid fittings. Hear Instr January 18–20,48, 1984
- Pirzanski CZ. Diminishing the occlusion effect: Clinical and manufacturer related factors. Hear J 51(4):66–78, 1998 [Google Scholar]
- Revit LJ. Real-ear measures. In Valente M. (Ed). Strategies for Selecting and Verifying Hearing Aid Fittings, 2nd edition. New York, Thieme Medical Publishers Inc; (in press), 2001 [Google Scholar]
- Revit LJ. The Circle of Decibels: Relating the hearing test, to the hearing aid, to the real-ear response. Hear Rev 4(11):35–38, 1997 [Google Scholar]
- Revit LJ. Two methods for dealing with the occlusion effect. Hear Instr 43(12):16–18, 1992 [Google Scholar]
- Revit LJ. An open letter: New thinking on the proper application of real-ear measurements to prescriptions and fittings. New Zealand J Audiol 1: 1–17, 1991 [Google Scholar]
- Ricketts TA, Bentler R. Impact of “standard” earmold on RECD. Am J Audiol 4: 43–45, 1995 [Google Scholar]
- Ricketts T, Lindley G, Henry P. Impact of compression and hearing aid style on directional hearing aid benefit and performance. Ear Hear 22(3):(in press), 2001 [DOI] [PubMed] [Google Scholar]
- Schwietzer H, Sullivan R, Beck L, Cole L. Developing a consensus for real-ear hearing instrument terms. Hear Instr 41:28,46, 1990 [Google Scholar]
- Seewald RC. An update on DSL[i/o]. Hear J 53(4):10–16, 2000 [Google Scholar]
- Seewald RC, Moodie KS, Sinclair ST, Scollie SD. Predictive validity of a procedure for pediatric hearing instrument fitting. Am J Audiol 8(2):143–152, 1999 [DOI] [PubMed] [Google Scholar]
- Seewald RC, Cornelisse LE, Richert FM, Block MG. Acoustic transforms for fitting CIC hearing instruments. In Chasin M. (ed.) CIC Handbook. San Diego: Singular Publishing Group; 83–100, 1997 [Google Scholar]
- Seewald RC, Cornelisse LE, Ramji KV, Sinclair ST, Moodie KS, Jamieson DG. A software implementation of the Desired Sensation Level (DSL[i/o]) method for fitting linear gain and wide dynamic range compression hearing instruments: Version 4.1a. User's Manual. London: The University of Western Ontario, 1997
- Seewald RC, Cornelisse LE, Black SL, Block MG. Verifying the real-ear gain in CIC instruments. Hear J 49(6):25–33, 1996 [Google Scholar]
- Scollie SD, Seewald RC, Cornelisse LE, Miller SM. Procedural considerations in the real-ear measurement of completely-in-the-canal instruments. J Am Acad Audiol 9: 216–220, 1998 [PubMed] [Google Scholar]
- Stelmachowicz PG, Kopun J, Mace AL, Lewis DE. Measures of hearing aid gain for real speech. Ear Hear 17(6):520–527, 1996 [DOI] [PubMed] [Google Scholar]
- Stelmachowicz P. Clinical issues related to hearing aid maximum output. In Studebaker G, Bess F, Beck L. (Eds). The Vanderbilt Hearing Aid Report II (pp. 141–148). Parkton MD: York Press, 1991 [Google Scholar]
- Stelmachowicz P, Lewis D, Seewald R, Hawkins D. Complex and pure-tone signals in the evaluation of hearing-aid characteristics. J Speech Hear Res 33: 380–385, 1990 [DOI] [PubMed] [Google Scholar]
- Storey L, Dillon H. Estimating the location of probe microphones relative to the tympanic membrane. J Am Acad Aud 12: 150–154, 2001 [PubMed] [Google Scholar]
- Sullivan R. Acoustic coupling classification system and custom hearing aids. Hear Instr Tech 2: 15–22, 1990 [Google Scholar]
- Sullivan RF. Probe microphone placement near the tympanic membrane. Hear Instr 39: 43–44, 60, 1988 [Google Scholar]
- Tecca JE. Clinical application of real-ear probe-tube measurement. In Sandlin RE. (ed.) Handbook of Hearing Aid Amplification, Boston: College-Hill Press, 225–256, 1991 [Google Scholar]
- Valente M, Bentler RA, Kaplan HS, et al. Guidelines for hearing aid fitting for adults. Am J Audiol 7(1):5–13, 1998 [Google Scholar]
- Wiener FM, Ross DA. The pressure distribution in the auditory canal in a progressive sound field. J Acoust Soc Am 18(2):401–408, 1946 [Google Scholar]