Abstract
Objective
The impact of knee arthroplasty on subsequent body weight gain has not been fully explored. Clinically important weight gain following knee arthroplasty would pose potentially important health risks.
Methods
We used one of the largest US-based knee arthroplasty registries and a population- based control sample from the same geographic region to determine whether knee arthroplasty increases risk of clinically important weight gain of 5% or more of baseline body weight over a 5-year postoperative period.
Results
Of the persons in the knee arthroplasty sample, 30.0% gained 5% or more of baseline body weight five years following surgery as compared to 19.7% of the control sample. The multivariable adjusted (age, sex, BMI, education, comorbidity and pre-surgical weight change) odds ratio was 1.6 (95% CI, 1.2, 2.2) in persons with knee arthroplasty as compared to the control sample. Additional arthroplasty procedures during the 5-year follow-up further increased risk for weight gain (OR=2.1, 95% CI, 1.4, 3.1) relative to the control sample. Specifically among patients with knee arthroplasty, younger patients and those who lost greater amounts of weight in the 5-year pre-operative period were at greater risk for clinically important weight gain.
Conclusions
Patients who undergo knee arthroplasty are at increased risk of clinically important weight gain following surgery. Future research should develop weight loss/maintenance interventions particularly for younger patients who have lost a substantial amount of weight prior to surgery as they are most at risk for substantial postsurgical weight gain.
Managing patients who are overweight or obese is one of the major challenges facing orthopaedic surgeons caring for patients with knee osteoarthritis. Obesity increases risk of knee osteoarthritis by four to five fold1 and is especially high2, consequential3,4 and costly5 for persons with lower extremity arthroplasty2,6. Total knee arthroplasty (TKA) is the most common type of arthroplasty surgery with over 700,000 procedures conducted in 20087 and a projected 3.5 million in 20308. Given the well established link between obesity in older adults and increased risk for cardiovascular disease and some cancers9, many patients who undergo TKA are at particularly high risk for adverse health events as a consequence of excessive weight and, potentially, weight gain after surgery10. Public health implications of weight gain are particularly important for persons in their 50s and 60s, a common age range for TKA. Weight gain during these decades is more likely than in older age groups which contributes to a greater risk of obesity related disorders11–13.
The logical assumption may be that persons who are overweight or obese prior to surgery are more likely to lose weight following surgery. Because there is less pain and improved mobility, the impediments to increased activity and exercise are eased following surgery and weight loss would logically follow. However, research exploring the impact of TKA on subsequent weight change has been inconclusive. One study reported a majority of patients gain weight after surgery10 while others report essentially no change14–18 or overall weight loss19. Variations among this evidence may be due to a variety of issues. Some studies, for example, examined small sample sizes and may have been underpowered14,17. Follow-up times varied from 3-months to two-years and no studies recruited a population-based sample of similarly aged persons without TKA to account for weight gain attributable to normal aging20–22. In the only study reporting significant weight gains, patients gained an average of 2.5 kg over the 2 years while the convenience sample of 31 control subjects gained 0.2kg10.
We found no literature that compared longer term weight changes in a large cohort of patients with TKA to a population-based control sample. The purpose of our study was to determine if persons undergoing TKA are at greater risk for clinically important weight gain (defined as a 5% or greater increase in weight relative to baseline)23–26 over a 5-year period as compared to an age and gender matched population-based sample. Our second purpose was to identify variables that increased risk of clinically important weight gain specifically among persons with TKA.
METHODS
Study Samples
We used two data sources. The first was the Mayo Clinic electronic and administrative knee joint registry databases. The registry prospectively collects follow-up outcomes data at 2 and 5 year intervals from all persons who have provided informed consent and have undergone TKA at Mayo Clinic. The registry has been functional since 1971.
All primary (not revision) TKA surgeries during the period of January 1, 1995 to December 31, 2005 were considered for study inclusion. This time period allowed us to: a) collect data on a large sample of patients receiving TKA and, b) use consistent definitions of both potential confounders and similar methods of height and weight data collection during clinic visits and, c) potentially collect 5 year follow-up data on all persons. We excluded persons who had the following medical procedures or disorders ≤2 years prior to or up to 5 years following the index arthroplasty date: a) bariatric surgery (n=17), and b) all forms of cancer other than basal cell carcinoma because of risk of cancer related weight loss (n=135). In addition, 25 persons undergoing arthroplasty did not provide informed consent and 60 persons underwent bilateral TKA on the same day and were excluded. The American Society of Anesthesiology27,28 score was retrieved using a registry maintained by the department of Anesthesiology. There were 1,122 TKAs, in 917 patients, meeting criteria for inclusion in the study over the time period. Overall, yearly body weight collection rates from the chart reviews for the 5 years following surgery ranged from 99.2% at baseline to 64.3% at 5 years.
The second data source was the Rochester Epidemiology Project (REP) a population-based medical records linkage system based in Olmsted County, Minnesota, home of Mayo Clinic. The REP has been continuously funded by NIH since 196629. Previous work has indicated that in any 3-year period, over 90% of Olmsted County residents are examined in the Mayo Clinic healthcare system which includes the Mayo Clinic, Mayo Clinic-St. Mary’s Hospital and Mayo Clinic-Methodist Hospital in Rochester, Minnesota30. The REP has been used extensively to study the epidemiology of a variety of health problems including rheumatic diseases31 and obesity32. The Institutional Review Board at the Mayo Clinic approved the study and all patients signed consent to have their data included in either the knee arthroplasty or the REP databases.
To estimate weight changes over time in the general population, we used the REP to select from all persons residing in Olmsted County and matched, within 30 days, to the dates of the TKA surgeries based on clinic visit dates. We selected a random sample of 237 persons using frequency matching and stratifying on age (groupings of 18–55, 56–65, 66–75, >75), sex, and year of TKA (1995–2005), from the approximately 124,000 people (2000 US census) in Olmsted County. Persons with a diagnosis of any form of cancer other than basal cell carcinoma or who underwent bariatric surgery during the study period were excluded. For the REP data, body weight collection rates ranged from 100% for the baseline surgery index date to 56% for the 5-year postoperative index date.
A total of 3 trained chart abstractors extracted data from charts of all persons in both the TKA cohort and the random sample of REP community residents for a total of 1,154 chart reviews. All weight data used in the study was collected from validated weight scales in the Mayo Clinic system. Abstractors reviewed medical charts for height, weight and education status. Deyo-Charlson comorbidity scores33,34, and cancer diagnoses were found through electronic medical record searches. International classification of Diseases ninth edition diagnosis codes, or cancer diagnostic labels in cases where abstractors found additional cancer diagnoses, indicated the presence of all cancers not including basal cell cancer during the study period (1995 to 2005).
An a priori power assessment was conducted to estimate the number of persons required to detect a difference among TKA and REP groups. Assuming a common standard deviation for weight change over five years of 4.5 kgs10,16 and using a two-sided, two-sample t test to compare five year weight change, we needed approximately 1,100 patients with TKA and 235 community residents to provide greater than 90% power to detect a difference in group means of 1 kg or more.
Assessment of Body Weight and BMI
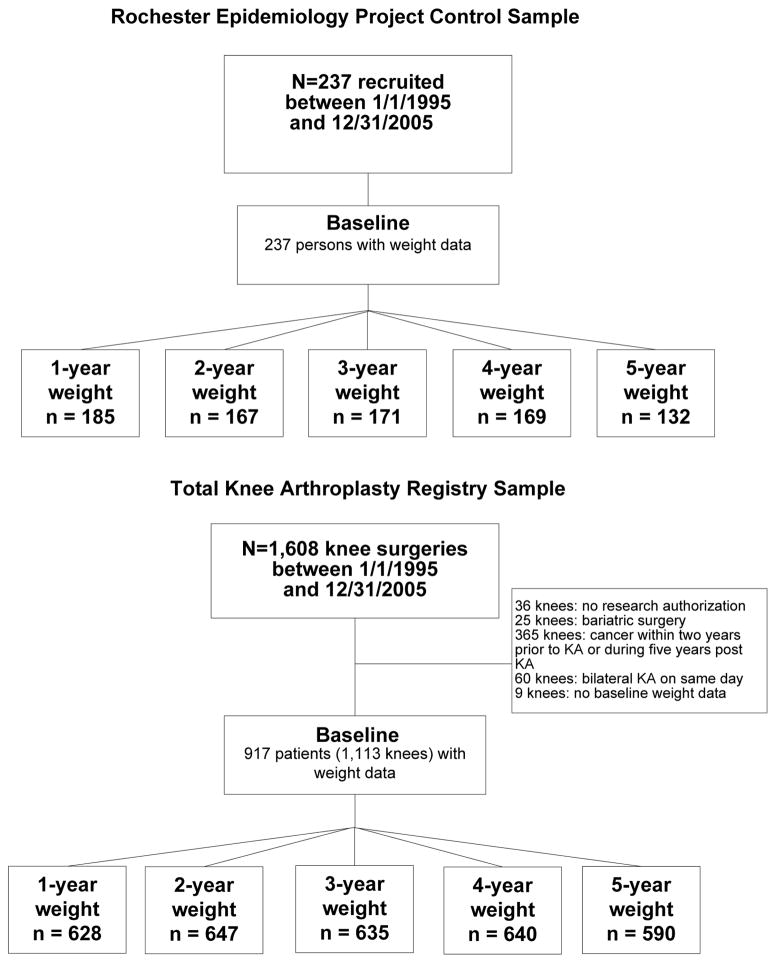
During each medical visit, whether for TKA follow-up or for any type of medical visit, all persons in the Mayo Clinic health system undergo routine height and weight measurements on digital scales that are calibrated yearly by hospital and clinic staff. For the patients undergoing TKA, height and weight data were collected on the day of surgery (i.e., the index visit). Chart abstractors extracted yearly height and weight data each year for 5 years prior to and 5 years after the TKA surgery date (in total, this covered years 1990 to 2010, depending on the index surgery date). Abstractors were instructed to extract yearly height and weight data that were as close to the yearly anniversary dates of the index surgery date. For the REP subjects, chart abstractors extracted height and weight data 5 years prior to and 5 years following the matched cases’ TKA index dates. The flow of patients through the study for both the REP and TKA samples is illustrated in the Figure.
Figure.
The Figure illustrates the flow of knee arthroplasty and Rochester Epidemiology patients through the study and the number of patients with bodyweight data at each time point.
Outcome variable of interest
All subjects were categorized as weight gainers if they gained ≥5% of body weight from the index date to final follow-up. Persons who did not gain ≥ 5% of their body weight from the index date to the final follow-up were classified as weight maintainers. A 5% or greater gain in body weight has been found in multiple studies to lead to clinically meaningful effects on cardiovascular and diabetes related risk as well as pain and function9,25,26. and has been recommended as a threshold for clinically meaningful weight loss in multiple guidelines23,24.
Potential Baseline Confounder Variables
We examined the following variables in the TKA and REP control cohorts in both univariate and multivariable analyses: (1) age, categorized in approximate quartiles as follows, <60 years, 61 to 69 years, 70 to 75 years and >75 years; (2) sex; (3) comorbidity, assessed using the Deyo-Charlson index, a validated comorbidity scale that includes 17 comorbidities with higher scores indicating greater comorbidity33,34; (5) baseline BMI (kg/m2) categorized into <25, 25.1 to <30, 30 to <35, and ≥35 with <25 (mild thinness to normal weight) being the referent group; 35 (6) education, categorized into three groups (< high school diploma, high school diploma or some college, at least 4 years of college); (7) contralateral or hip arthroplasty procedures conducted during the 5 year postoperative period, and (8) two additional variables created to account for extent of weight gain in the 5 years prior to surgery. For maximum pre-TKA weight loss, we subtracted the largest weight in the five years prior to surgery from the index weight. If the subject demonstrated no weight loss in the 5 years prior to the index date, this variable was coded as 0. A similar strategy was used to indicate the extent of weight gain up to 5 years prior to the index surgery date. We reasoned that if the subject had either lost or gained weight in the years leading up to the index date, the extent of weight gain or loss following surgery may be impacted by this pre-surgical weight variation36.
Source of Funding
The funding source played no role in the conduct or reporting of this study.
Statistical Analyses
Descriptive statistics are reported for the characteristics of the TKA patients and the REP community residents. A t-test or Chi square test, as appropriate, was used to compare baseline characteristics of patients with the population-based controls (see Table 1) and those with and those without missing data at years 2 and 4 (see Table 2).
Table 1.
Baseline characteristics and extent if missing follow-up weight data for the study samples a
| N(%) | REP Controls (n=237) | TKA Cases (n=917) | P-value b |
|---|---|---|---|
| Baseline weight (kgs) | 76.4 (17.3) | 90.0 (21.8) | <0.001 |
| Male Gender | 85(36) | 331(36) | 0.96 |
| Education | 0.13 | ||
| < HS | 24(11) | 156(14) | |
| HS or Some College | 142(68) | 659(60) | |
| >=4 years College | 43(21) | 275(25) | |
| Deyo-Charlson Index | 0.48 | ||
| 0 | 90(38) | 365(40) | |
| 1 | 45(19) | 196(21) | |
| >1 | 102(43) | 357(39) | |
| Age in yrs | 0.67 | ||
| <=50 | 18 (8) | 54 (6) | |
| 50–59 | 35(15) | 161(18) | |
| 60–69 | 73(31) | 298(32) | |
| 70–80 | 83(35) | 310(34) | |
| >80 | 28(12) | 95(10) | |
| Baseline BMI | <0.001 | ||
| <25 | 80(34) | 124(14) | |
| 25 to 30 | 87(37) | 273(30) | |
| 30 to 35 | 45(19) | 246(27) | |
| 35 to 40 | 17(7) | 160(18) | |
| >=40 | 8(3) | 108(12) | |
| 1-year data present | 185 (78) | 628 (68) | 0.003 |
| 2-year data present | 167(70) | 647(70) | 0.93 |
| 3-year data present | 171(72) | 635(69) | 0.47 |
| 4-year data present | 169(71) | 640(70) | 0.85 |
| 5-year data present | 132(56) | 590(64) | 0.85 |
| Pre-surgical 5-yr max wt loss (kg)c | 3.2 (4.0) | 4.5 (6.0) | 0.001 |
| Pre-surgical 5-yr max wt gain (kg)d | 3.2 (5.0) | 3.7 (5.4) | 0.20 |
Abbreviations: BMI, body mass index (calculated as the weight in kilograms divided by height in meters squared); HS, high school.
Data are given as mean (SD) for continuous variables and percentage for categorical variables unless otherwise indicated.
p value for t-test was used for continuous variables and X2 for categorical variables.
Maximum weight loss (in Kgs), relative to baseline, during the 5-years prior to the baseline knee arthroplasty.
Maximum weight gain (in Kgs), relative to baseline, during the 5-years prior to the baseline knee arthroplasty.
Table 2.
Relationship between non-missing 2- and 4-year weight data and baseline characteristics for the total sample a
| N(%) | Non-missing Two-Year Data | P-value b | Non-missing Four-Year Data | P-value b |
|---|---|---|---|---|
| Gender, | 0.41 | 0.26 | ||
| Female | 527(71) | 526(71) | ||
| Male | 287(69) | 283(68) | ||
| Education | 0.16 | 0.14 | ||
| < H.S. | 98(65) | 97(65) | ||
| H.S. or Some College | 498(73) | 495(73) | ||
| >=4 years College | 190(70) | 196(73) | ||
| Deyo-Charlson Index | <0.001 | 0.007 | ||
| =0 | 294(65) | 315(69) | ||
| =1 | 192(80) | 188(78) | ||
| >1 | 328(71) | 306(67) | ||
| Age | 0.49 | 0.27 | ||
| <=50 | 59(68) | 50(69) | ||
| 50–59 | 135(69) | 132(67) | ||
| 60–69 | 263(71) | 272(73) | ||
| 70–80 | 287(73) | 277(70) | ||
| >80 | 80(65) | 78(63) | ||
| Baseline BMI | 0.88 | 0.08 | ||
| <25 | 144(71) | 140(69) | ||
| 25 to 30 | 259(72) | 241(67) | ||
| 30 to 35 | 210(72) | 223(77) | ||
| 35 to 40 | 122(69) | 121(68) | ||
| >=40 | 79(68) | 84(72) |
Abbreviations: HS, high school; BMI, body mass index (calculated as the weight in kilograms divided by height in meters squared).
Data are given percentage for categorical variables.
P for X2 for categorical variables.
Logistic regression was used to analyze variables associated with clinically important weight gain using all data collected over the 5-year post-operative period and accounting for within subject correlation (Proc Genmod in SAS with repeated statement). Clinically important weight gain was defined as a 5% or greater body weight gain during the 5-year follow-up as compared to baseline. All weight/height assessments post-surgery were included in the analyses. In addition to subject group (TKA vs. REP), other patient factors considered in these models included baseline BMI, age, sex, education, Deyo-Charlson Index, maximum loss in weight from 5-years prior to the index date, and maximum gain in weight 5-years prior to the index date. In all analyses we examined for all two-way interactions with other variables in the models. The alpha level was set at 0.05 for statistical significance. We conducted a sensitivity analysis to account for the imbalance in baseline BMI distributions between the THA and REP groups. The marginal structural models method as described by Robbins and colleagues37 uses case weights to balance the distribution of baseline BMI between the THA and REP patients to allow for statistical comparisons when baseline BMI distribution were equivalent.
A separate logistic regression analysis was conducted to identify variables associated with clinically important weight gain specifically in the TKA group. For this analysis we also included as predictor variables, diagnosis (osteoarthritis (OA) versus rheumatoid arthritis (RA)) and American Society of Anesthesiologists (ASA) score, a validated measure of immediate postoperative morbidity and perioperative mortality and scored as classes I–II versus III–IV27,28. Statistical analyses were performed with SAS statistical software, version 9.2 (SAS Institute, Cary, North Carolina).
RESULTS
The TKA sample (n=917 persons with 205 undergoing additional primary hip or knee arthroplasty procedures during the 5-year follow-up) and the population-based control sample descriptions appear in Table 1. A total of 98.3% of the TKA sample and 93.8% of the REP sample contributed follow-up weight data to the analysis with 80.6% of the TKA sample and 78.2% of the REP sample with at least 3 years worth of follow-up weight data. Most attributes for both groups were similar with the exception of baseline BMI and weight, which was significantly higher for the TKA sample. With the exception of Deyo-Charlson comorbidity scores, characteristics of the total sample with and without missing data at years 2 and 4 were similar (see Table 2).
Over the 5-year post-operative period, the control group (n=237) lost a mean of −0.35 kg (SD= 5.0). The patients with subsequent additional knee or hip arthroplasty(ies) during the 5-year follow-up gained a mean of 2.62 (SD=6.0) kgs while cases with no additional lower extremity arthroplasty during 5-years of follow-up gained a mean of 1.23 kgs (SD=6.4). Percentages of patients in the TKA sample who gained ≥ 5% of body weight varied from 22.1% in year 1 to 32.3% in year 4 whereas 16.2% to 22.8% of the REP sample gained ≥ 5% body weight over the study period.
In a univariate analysis, patients undergoing a single TKA had an odds of gaining ≥ 5% body weight up to 5-years following surgery that was 70% higher than that of the REP control group (OR= 1.7, 95%CI, 1.3, 2.3). Patients undergoing at least one additional arthroplasty during the follow-up period had and increased odds (OR=2.3, 95%CI, 1.6, 3.2) of clinically important weight gain relative to the REP controls. In a multi-variable model that adjusted for potential confounders, estimates for clinically important weight gain in persons with a single TKA and persons with additional arthroplasty surgery were similar to those found in univariate models (see Table 4). In the sensitivity analysis that adjusted for the imbalance in baseline BMI between REP and TKA samples, the key estimates were very similar to those reported in the Appendix.
Table 4.
Logistic regression model of clinically important weight gain (≥ 5% body weight) and TKA case/REP control status
| Unadjusted Analysis | Adjusted Analysis | |||
|---|---|---|---|---|
|
| ||||
| Variable | Odds Ratio (95% CI) | P-value | Odds Ratio (95% CI) | P-value |
| Subject Status | ||||
| TKA (follow-up arthroplasty) | 2.3 (1.6, 3.2) | <0.001 | 2.1 (1.4, 3.1) | <0.001 |
| TKA (no follow-up arthroplasty) | 1.7 (1.3, 2.3) | <0.001 | 1.6 (1.2, 2.2) | 0.003 |
| REP Control | 1.0 (reference) | 1.0 (reference) | ||
| BMI | ||||
| >= 25.0 – < 30.0 | 0.7 (0.5, 1.0) | 0.054 | 0.7 (0.5, 1.0) | 0.09 |
| >= 30.0 – < 35.0 | 0.9 (0.7, 1.3) | 0.58 | 0.8 (0.6, 1.2) | 0.24 |
| >= 35 | 0.8 (0.6, 1.1) | 0.20 | 0.6 (0.4, 0.9) | 0.02 |
| <25 | 1.0 (reference) | 1.0 (reference) | ||
| Age | ||||
| <60 | 2.1 (1.5, 2.8) | <0.001 | 2.7 (1.8, 3.9) | <0.001 |
| 60 to 69 | 1.5 (1.1, 2.0) | 0.01 | 1.7 (1.2, 2.3) | 0.004 |
| 70 to 75 | 1.1 (0.9, 1.4) | 0.55 | 1.2 (0.8, 1.8) | 0.36 |
| >75 | 1.0 (reference) | 1.0 (reference) | ||
| Gender | ||||
| Male | 1.1 (0.9, 1.4) | 0.41 | 1.2 (0.9, 1.5) | 0.19 |
| Female | 1.0 (reference) | 1.0 (reference) | ||
| Education | ||||
| < HS diploma | 1.0 (0.7, 1.5) | 0.92 | 1.2 (0.8, 1.7) | 0.50 |
| HS or some college | 1.0 (0.7, 1.2) | 0.70 | 1.0 (0.7, 1.3) | 0.86 |
| College degree or > | 1.0 (reference) | 1.0 (reference) | ||
| Deyo-Charlson Index | ||||
| 0 | 0.9 (0.7, 1.1) | 0.19 | 0.8 (0.6, 1.0) | 0.08 |
| 1 | 1.0 (0.8, 1.4) | 0.89 | 0.9 (0.6, 1.2) | 0.36 |
| >1 | 1.0 (reference) | 1.0 (reference) | ||
| Pre-surgical 5-yr max wt loss, per 1 Kg* | 1.10 (1.07, 1.13) | <0.001 | 1.10 (1.07, 1.13) | <0.001 |
| Pre-surgical 5-yr max wt gain, per 1 Kg# | 0.99 (0.97, 1.01) | 0.92 | 0.99 (0.97, 1.01) | 0.44 |
TKA = total knee arthroplasty, REP = Rochester Epidemiology Project
Maximum weight loss (in Kgs), relative to baseline, during the 5-years prior to the baseline knee arthroplasty.
Maximum weight gain (in Kgs), relative to baseline, during the 5-years prior to the baseline knee arthroplasty.
For the multi-variable logistic regression model examining only patients in the TKA group, those who were at higher risk for clinically important weight gain were younger than 70 years and had lost more weight in the 5-years prior to surgery. Baseline BMI was not related to risk of ≥ 5% weight gain in the TKA group (see Table 5).
Table 5.
Logistic regression model of clinically important weight gain (≥ 5% body weight) among persons with knee arthroplasty
| Variable | Unadjusted Analysis | Adjusted Analysis | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | P-value | Odds Ratio (95% CI) | P-value | |
| Subject Status | ||||
| TKA Case (follow-up arthroplasty) | 1.3 (1.0, 1.7) | 0.02 | 1.3 (0.9, 1.7) | 0.13 |
| TKA Case (no follow-up arthroplasty) | 1.0 (reference) | 1.0 (reference) | ||
| BMI | ||||
| >= 25.0 – < 30.0 | 0.7 (0.5, 1.0) | 0.08 | 0.8 (0.5 (1.2) | 0.25 |
| >= 30.0 – < 35.0 | 0.8 (0.6, 1.2) | 0.35 | 0.8 (0.5, 1.3) | 0.36 |
| >= 35 | 0.8 (0.5, 1.1) | 0.13 | 0.8 (0.5, 1.2) | 0.23 |
| <25 | 1.0 (reference) | 1.0 (reference) | ||
| Age | ||||
| <60 | 2.2 (1.6, 3.1) | <0.001 | 3.0 (1.9, 4.8) | <0.001 |
| 60 to 69 | 1.5 (1.1, 2.0) | 0.02 | 1.6 (1.1, 2.4) | 0.02 |
| 70 to 75 | 1.2 (0.8, 1.7) | 0.34 | 1.4 (0.9, 2.2) | 0.13 |
| >75 | 1.0 (reference) | 1.0 (reference) | ||
| Gender | ||||
| Male | 1.1 (0.8, 1.4) | 0.65 | 1.2 (0.9, 1.5) | 0.34 |
| Female | 1.0 (reference) | 1.0 (reference) | ||
| Diagnosis | ||||
| Osteoarthritis | 0.8 (0.5, 1.1) | 0.13 | 1.0 (0.6, 1.6) | 0.99 |
| Other | 1.0 (reference) | 1.0 (reference) | ||
| Education | ||||
| < HS diploma | 1.2 (0.8, 1.7) | 0.40 | 1.3 (0.8, 2.2) | 0.22 |
| HS or some college | 1.1 (0.8, 1.4) | 0.63 | 1.0 (0.7, 1.4) | 0.97 |
| College degree or > | 1.0 (reference) | 1.0 (reference) | ||
| ASA score | ||||
| III or IV | 0.9 (0.7, 1.2) | 0.44 | 0.9 (0.7, 1.2) | 0.50 |
| I or II | 1.0 (reference) | 1.0 (reference) | ||
| Charlson Index | ||||
| 0 | 0.9 (0.7, 1.2) | 0.41 | 0.8 (0.6, 1.1) | 0.24 |
| 1 | 1.1 (0.8, 1.4) | 0.77 | 0.8 (0.6, 1.2) | 0.39 |
| >1 | 1.0 (reference) | 1.0 (reference) | ||
| Pre-surgical 5-yr max wt loss, per 1 Kg* | 1.09 (1.06, 1.12) | <0.001 | 1.1 (1.07, 1.13) | <0.001 |
| Pre-surgical 5-yr max wt gain, per 1 Kg# | 1.0 (0.98, 1.02) | 0.84 | 0.98 (0.96, 1.01) | 0.19 |
TKA = total knee arthroplasty
Maximum weight loss (in Kgs), relative to baseline, during the 5-years prior to the baseline knee arthroplasty.
Maximum weight gain (in Kgs), relative to baseline, during the 5-years prior to the baseline knee arthroplasty.
DISCUSSION
The odds of gaining ≥ 5% of baseline bodyweight over the 5-year postoperative period for persons with TKA was 60% higher than peers who did not undergo TKA surgery. Odds of clinically important weight gain more than doubled, relative to that of non-TKA peers for persons who underwent at least one additional arthroplasty procedure during the 5-year post-operative period. For TKA patients, those who were younger than 70 years and those who experienced greater weight loss prior to surgery were at greatest risk for clinically important weight gain after TKA.
The finding of increased risk of postsurgical weight gain for younger patients takes on added importance because TKA surgery for younger patients is becoming more common in the US38 and internationally39,40. Kurtz and colleagues estimate that by 2016 the majority of persons undergoing TKA will be under 65 years of age38. Heisel and colleagues also found that younger patients gained more weight following TKA than older patients41.
Comparisons of our findings to the literature need to account for time since surgery. For example, our findings were similar to those reported by Zeni and Snyder Mackler who reported that 2-year average postoperative weight gains among TKA patients were 2.5 kgs10. Our patients gained an average of 1.5 kgs 2-years after surgery. Others reported essentially no weight change 2-years following knee arthroplasty in a sample of 188 overweight and obese patients15.
At 1-year, our patients gained an average of only 0.23 kg. Others found similar very small increases in body weight 1-year after surgery14,17,18,42. Patients should be advised that risk for clinically important weight gain increases, particularly after the first postsurgical year. Relative to the population, weight gain also is more likely for persons who undergo additional arthroplasty surgeries. The subsequent surgery likely reduces physical activity, increases pain and complications43 and leads to additional weight gain.
Our study also appears to be the first to indicate that preoperative weight loss prior to TKA surgery is an important independent risk factor for postsurgical weight gain. Intentional weight loss is known to frequently lead to subsequent weight gain44,45 and we suspect this was the case in our sample. Overweight and obese patients preparing for TKA are frequently encouraged to lose weight prior to surgery but in our experience, little instruction is typically provided for how to maintain weight loss. Evidence suggests preoperative weight loss will reduce risk of complications and potentially revision surgery43 and while pre-surgical weight loss may aid in enhancing early recovery, our data suggests at least some of the weight is gained back after surgery. Weight fluctuation also is known to increase risk of a variety of comorbidities46,47. Effective weight control strategies to reduce weight in overweight and obese patients and to maintain weight loss in those with substantial pre-operative weight loss should be the target of future research in this population. Our data suggests that patients younger than 70 years who have lost a substantial amount of weight pre-operatively are particularly at risk for important post-operative weight gain are particularly vulnerable and should be the risk group targeted for future research.
Our study has several strengths, most notably a 5-year follow-up, a large sample size and an age and gender matched population-based comparison group. There were also some notable limitations. Loss to follow-up was fairly substantial with over a third of patients and almost half of the REP subjects with missing weight data at 5 years. While differences among those with complete and those with missing data were not extensive (see Table 2), missing data combined with potential unmeasured confounding may have influenced our findings. For example, weight changes may have been related to unmeasured factors such as smoking status, medications, pain during recovery and multi-joint arthritis though we did exclude persons with postsurgical weight loss surgery or cancer. We also had a higher loss to follow-up of persons with no comorbidities relative to persons with more comorbidities particularly in the REP sample and this may have influenced our findings. We also do not know whether the weight changes in our subjects were intentional or unintentional. Reasons for weight change may influence outcome following TKA surgery48. Our REP control group weighed substantially less at baseline as compared to the knee arthroplasty group, which may have influenced our findings. We conducted a sensitivity analysis that adjusted for imbalances in baseline BMI differences among REP and TKA samples and our findings were not appreciably changed (see Appendix).
In conclusion, our study demonstrates an association between TKA surgery and subsequent clinically important weight gain relative to that seen in a population-based age and gender matched REP control sample. Risk factors for clinically important weight gain specifically for patients undergoing TKA were age (less than 70 years), and greater weight loss prior to surgery. Multi-disciplinary weight loss/maintenance interventions particularly directed to those TKA patients who are younger and have lost considerable weight prior to surgery should be considered. Given the challenges of losing or maintaining weight over the long term, research efforts should target this sub-group of patients.
Supplementary Material
Table 3.
Percentage of subjects in the total knee and Rochester Epidemiology Project samples who gained a clinically important amount of body weight over the 5-year follow-up period
| Total Knee Arthroplasty | Rochester Epidemiology Project | |||
|---|---|---|---|---|
|
| ||||
| Year | N | % with Clinically Important Gain | N | % with Clinically Important Gain |
| One | 624 | 138 (22.1%) | 185 | 30 (16.2%) |
| Two | 647 | 183 (28.3%) | 167 | 38 (22.8%) |
| Three | 635 | 196 (30.9%) | 171 | 37 (21.6%) |
| Four | 640 | 207 (32.3%) | 169 | 27 (16.0%) |
| Five | 590 | 177 (30.0%) | 132 | 26 (19.7%) |
Significance and Innovations.
Relative to a population-based sample, persons undergoing knee arthroplasty are at risk for clinically important 5-year post-operative weight gain.
Additional lower extremity arthroplasty procedures increase risk of clinically important weight gain relative to a population-based sample.
Sub-groups of patients undergoing knee arthroplasty who are under 70 years and who have lost a substantial amount of weight prior to surgery are at particularly high risk for postoperative weight gain.
Acknowledgments
The authors wish to thank Ms. Jennifer Krogman, Ms. Sheila Marsh and Ms. Cara Miller for their assistance with the chart reviews. The study was funded by a grant from the Virginia Commonwealth University Presidential Research Initiative Program. The funding source played no role in the design, data collection or reporting of the study.
Footnotes
Financial Support Statement: The authors disclose no financial support or other benefits from commercial sources for the work reported on in the manuscript, or any other financial interests which could create a potential conflict of interest or the appearance of a conflict of interest with regard to the work.
Contributor Information
Daniel L. Riddle, Email: dlriddle@vcu.edu, Virginia Commonwealth University, Departments of Physical Therapy and Orthopaedic Surgery, PO Box 980224, Richmond, Virginia, 23298-0224, (t) 804-828-0234, (f) 804-828-8111.
Jasvinder A. Singh, Birmingham Veterans Affairs Medical Center and the University of Alabama at Birmingham, University of Alabama at Birmingham, Faculty Office Tower 805B 510 20th Street South, Birmingham, AL 35294, Mayo Clinic.
William S Harmsen, Mayo Clinic, Division of Biomedical Statistics and Informatics (BSI) 200 First Street SW, Rochester, MN 55905.
Cathy D Schleck, Mayo Clinic, Mayo Clinic, Division of Biomedical Statistics and Informatics (BSI), 200 First Street SW, Rochester, MN 55905.
David G Lewallen, Mayo Clinic College of Medicine, Department of Orthopaedic Surgery, Rochester, MN 55905.
Reference List
- 1.Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first national Health and Nutrition Examination Survey (HANES I). Evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol. 1988 Jul;128(1):179–89. doi: 10.1093/oxfordjournals.aje.a114939. [DOI] [PubMed] [Google Scholar]
- 2.Fehring TK, Odum SM, Griffin WL, Mason JB, McCoy TH. The obesity epidemic: its effect on total joint arthroplasty. J Arthroplasty. 2007 Sep;22(6 Suppl 2):71–6. doi: 10.1016/j.arth.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 3.Lubbeke A, Moons KG, Garavaglia G, Hoffmeyer P. Outcomes of obese and nonobese patients undergoing revision total hip arthroplasty. Arthritis Rheum. 2008 May 15;59(5):738–45. doi: 10.1002/art.23562. [DOI] [PubMed] [Google Scholar]
- 4.Jain NB, Guller U, Pietrobon R, Bond TK, Higgins LD. Comorbidities increase complication rates in patients having arthroplasty. Clin Orthop Relat Res. 2005 Jun;(435):232–8. doi: 10.1097/01.blo.0000156479.97488.a2. [DOI] [PubMed] [Google Scholar]
- 5.Dowsey MM, Liew D, Choong PF. Economic burden of obesity in primary total knee arthroplasty. Arthritis Care Res (Hoboken) 2011 Oct;63(10):1375–81. doi: 10.1002/acr.20563. [DOI] [PubMed] [Google Scholar]
- 6.Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am. 2011 Sep 7;93(17):1588–96. doi: 10.2106/JBJS.J.00772. [DOI] [PubMed] [Google Scholar]
- 7.Kurtz SM, Ong KL, Lau E, Widmer M, Maravic M, Gomez-Barrena E, et al. International survey of primary and revision total knee replacement. Int Orthop. 2011 Dec;35(12):1783–9. doi: 10.1007/s00264-011-1235-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780–5. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 9.Leblanc ES, O’Connor E, Whitlock EP, Patnode CD, Kapka T. Effectiveness of primary care-relevant treatments for obesity in adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011 Oct 4;155(7):434–47. doi: 10.7326/0003-4819-155-7-201110040-00006. [DOI] [PubMed] [Google Scholar]
- 10.Zeni JA, Jr, Snyder-Mackler L. Most patients gain weight in the 2 years after total knee arthroplasty: comparison to a healthy control group. Osteoarthritis Cartilage. 2009 Dec 21; doi: 10.1016/j.joca.2009.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kahn HS, Cheng YJ. Longitudinal changes in BMI and in an index estimating excess lipids among white and black adults in the United States. Int J Obes (Lond) 2008 Jan;32(1):136–43. doi: 10.1038/sj.ijo.0803697. [DOI] [PubMed] [Google Scholar]
- 12.Eng SM, Gammon MD, Terry MB, Kushi LH, Teitelbaum SL, Britton JA, et al. Body size changes in relation to postmenopausal breast cancer among women on Long Island, New York. Am J Epidemiol. 2005 Aug 1;162(3):229–37. doi: 10.1093/aje/kwi195. [DOI] [PubMed] [Google Scholar]
- 13.Koh-Banerjee P, Wang Y, Hu FB, Spiegelman D, Willett WC, Rimm EB. Changes in body weight and body fat distribution as risk factors for clinical diabetes in US men. Am J Epidemiol. 2004 Jun 15;159(12):1150–9. doi: 10.1093/aje/kwh167. [DOI] [PubMed] [Google Scholar]
- 14.Woodruff MJ, Stone MH. Comparison of weight changes after total hip or knee arthroplasty. J Arthroplasty. 2001 Jan;16(1):22–4. doi: 10.1054/arth.2001.9826. [DOI] [PubMed] [Google Scholar]
- 15.Lachiewicz AM, Lachiewicz PF. Weight and activity change in overweight and obese patients after primary total knee arthroplasty. J Arthroplasty. 2008 Jan;23(1):33–40. doi: 10.1016/j.arth.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 16.Dowsey MM, Liew D, Stoney JD, Choong PF. The impact of pre-operative obesity on weight change and outcome in total knee replacement: a prospective study of 529 consecutive patients. J Bone Joint Surg Br. 2010 Apr;92(4):513–20. doi: 10.1302/0301-620X.92B4.23174. [DOI] [PubMed] [Google Scholar]
- 17.Donovan J, Dingwall I, McChesney S. Weight change 1 year following total knee or hip arthroplasty. ANZ J Surg. 2006 Apr;76(4):222–5. doi: 10.1111/j.1445-2197.2006.03696.x. [DOI] [PubMed] [Google Scholar]
- 18.bu-Rajab RB, Findlay H, Young D, Jones B, Ingram R. Weight changes following lower limb arthroplasty: a prospective observational study. Scott Med J. 2009 Feb;54(1):26–8. doi: 10.1258/rsmsmj.54.1.26. [DOI] [PubMed] [Google Scholar]
- 19.Stets K, Koehler SM, Bronson W, Chen M, Yang K, Bronson M. Weight and body mass index change after total joint arthroplasty. Orthopedics. 2010 Jun;33(6):386. doi: 10.3928/01477447-20100429-13. [DOI] [PubMed] [Google Scholar]
- 20.Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003 Jan 1;289(1):76–9. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 21.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010 Jan 20;303(3):235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 22.He XZ, Baker DW. Changes in weight among a nationally representative cohort of adults aged 51 to 61, 1992 to 2000. Am J Prev Med. 2004 Jul;27(1):8–15. doi: 10.1016/j.amepre.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 23.Dietitians Association of Australia best practice guidelines for the treatment of overweight and obesity in adults. [Accessed on 4/15/12];Internet. 2005 Available from: URL: http://www.daa.collaborative.net.au/files/DINER/
- 24.Center for Drug Evaluation and Research, United States Food and Frug Administration. Guidance for Industry: developing products for weight management. Rockville, MD: FDA; 2007. [Google Scholar]
- 25.de las FL, Waggoner AD, Mohammed BS, Stein RI, Miller BV, III, Foster GD, et al. Effect of moderate diet-induced weight loss and weight regain on cardiovascular structure and function. J Am Coll Cardiol. 2009 Dec 15;54(25):2376–81. doi: 10.1016/j.jacc.2009.07.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Messier SP. Diet and exercise for obese adults with knee osteoarthritis. Clin Geriatr Med. 2010 Aug;26(3):461–77. doi: 10.1016/j.cger.2010.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weaver F, Hynes D, Hopkinson W, Wixson R, Khuri S, Daley J, et al. Preoperative risks and outcomes of hip and knee arthroplasty in the Veterans Health Administration. J Arthroplasty. 2003 Sep;18(6):693–708. doi: 10.1016/s0883-5403(03)00259-6. [DOI] [PubMed] [Google Scholar]
- 28.Dripps RD, LAMONT A, ECKENHOFF JE. The role of anesthesia in surgical mortality. JAMA. 1961 Oct 21;178:261–6. doi: 10.1001/jama.1961.03040420001001. [DOI] [PubMed] [Google Scholar]
- 29.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, III, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. Am J Epidemiol. 2011 May 1;173(9):1059–68. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Melton LJ., III History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996 Mar;71(3):266–74. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 31.Doran MF, Crowson CS, O’Fallon WM, Hunder GG, Gabriel SE. Trends in the incidence of polymyalgia rheumatica over a 30 year period in Olmsted County, Minnesota, USA. J Rheumatol. 2002 Aug;29(8):1694–7. [PubMed] [Google Scholar]
- 32.Batsis JA, Huddleston JM, Melton LJ, Huddleston PM, Lopez-Jimenez F, Larson DR, et al. Body mass index and risk of adverse cardiac events in elderly patients with hip fracture: a population-based study. J Am Geriatr Soc. 2009 Mar;57(3):419–26. doi: 10.1111/j.1532-5415.2008.02141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Charlson ME, Sax FL, MacKenzie CR, Braham RL, Fields SD, Douglas RG., Jr Morbidity during hospitalization: can we predict it? J Chronic Dis. 1987;40(7):705–12. doi: 10.1016/0021-9681(87)90107-x. [DOI] [PubMed] [Google Scholar]
- 34.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 35.BMI Classification. World Health Organization; 2012. Jan 3, [Google Scholar]
- 36.Lee JS, Kritchevsky SB, Tylavsky F, Harris T, Simonsick EM, Rubin SM, et al. Weight change, weight change intention, and the incidence of mobility limitation in well-functioning community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2005 Aug;60(8):1007–12. doi: 10.1093/gerona/60.8.1007. [DOI] [PubMed] [Google Scholar]
- 37.Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000 Sep;11(5):550–60. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 38.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009 Oct;467(10):2606–12. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Losina E, Katz JN. Total knee arthroplasty on the rise in younger patients: Are we sure that past performance will guarantee future success? Arthritis Rheum. 2012 Jan 17; doi: 10.1002/art.33371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Leskinen J, Eskelinen A, Huhtala H, Paavolainen P, Remes V. The incidence of knee arthrolasty for primary osteoarthritis grows rapidly among baby-boomers - a population-based study. Arthritis Rheum. 2012 Jan 17; doi: 10.1002/art.33367. [DOI] [PubMed] [Google Scholar]
- 41.Heisel C, Silva M, la Rosa MA, Schmalzried TP. The effects of lower-extremity total joint replacement for arthritis on obesity. Orthopedics. 2005 Feb;28(2):157–9. doi: 10.3928/0147-7447-20050201-18. [DOI] [PubMed] [Google Scholar]
- 42.Lee GC, Cushner FD, Cannella LY, Scott WN. The effect of total knee arthroplasty on body weight. Orthopedics. 2005 Mar;28(3):321–3. doi: 10.3928/0147-7447-20050301-19. [DOI] [PubMed] [Google Scholar]
- 43.NIH Consensus Panel. NIH Consensus Statement on total knee replacement December 8–10, 2003. J Bone Joint Surg Am. 2004 Jun;86-A(6):1328–35. doi: 10.2106/00004623-200406000-00031. [DOI] [PubMed] [Google Scholar]
- 44.Curioni CC, Lourenco PM. Long-term weight loss after diet and exercise: a systematic review. Int J Obes (Lond) 2005 Oct;29(10):1168–74. doi: 10.1038/sj.ijo.0803015. [DOI] [PubMed] [Google Scholar]
- 45.Kroke A, Liese AD, Schulz M, Bergmann MM, Klipstein-Grobusch K, Hoffmann K, et al. Recent weight changes and weight cycling as predictors of subsequent two year weight change in a middle-aged cohort. Int J Obes Relat Metab Disord. 2002 Mar;26(3):403–9. doi: 10.1038/sj.ijo.0801920. [DOI] [PubMed] [Google Scholar]
- 46.Kataja-Tuomola M, Sundell J, Mannisto S, Virtanen MJ, Kontto J, Albanes D, et al. Short-term weight change and fluctuation as risk factors for type 2 diabetes in Finnish male smokers. Eur J Epidemiol. 2010 May;25(5):333–9. doi: 10.1007/s10654-010-9444-6. [DOI] [PubMed] [Google Scholar]
- 47.Tsai CJ, Leitzmann MF, Willett WC, Giovannucci EL. Weight cycling and risk of gallstone disease in men. Arch Intern Med. 2006 Nov 27;166(21):2369–74. doi: 10.1001/archinte.166.21.2369. [DOI] [PubMed] [Google Scholar]
- 48.French SA, Jeffery RW, Folsom AR, Williamson DF, Byers T. History of intentional and unintentional weight loss in a population-based sample of women aged 55 to 69 years. Obes Res. 1995 Mar;3(2):163–70. doi: 10.1002/j.1550-8528.1995.tb00132.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.