Abstract
Purpose
The purpose of the pilot study was to examine the feasibility and preliminary efficacy of an age-specific diabetes prevention program in young adults with prediabetes.
Methods
One group pretest-posttest design was conducted. The inclusion criteria were young adults age 18–29 years with prediabetes [either Impaird fasting glucose [IFG] (100–125 mg/dL), or an A1C of 5.7%–6.4%]. Fifteen participants were enrolled in this study. A technology based lifestyle coaching program focused on diet and physical activity and incorporating a hand-held device and digital platforms was developed and tested. Psychosocial factors (health literacy, illness perception, self-efficacy, therapeutic efficacy) based on social cognitive theory, changes in diet and physical activity, and cardiometabolic risk factors were assessed at baseline and week 12 after intervention. A paired-samples t-test was performed to examine changes between baseline and post-intervention on each psychosocial and physical variable.
Results
Participants (n= 13 completers) were mean age 24.4 yrs [SD: 2.2], 23.1% male, and 53.8% were African American. Overall, the participants were satisfied with the intervention (M = 4.15 on a 5-point Likert scale). Between pre and post testing, BMI and A1C decreased from 41.0 ±7.3 to 40.1±7.0 and 6.0% ± .5 to 5.6% ± .5, respectively, while fasting glucose did not significantly change (92.6±11 mg/dl to 97.6 ±14.3 mg/dl).
Conclusion
The intervention resulted in reduced A1C and a trend for decreased BMI in obese sedentary young adults with prediabetes after 12 weeks of intervention. Further study through a randomized clinical trial with a longer intervention period is warranted.
Keywords: Diabetes prevention, young adults, technology, feasibility
The prevalence of type 2 diabetes (T2D) in younger populations is increasing, which is a major public health concern.1–3 The obesity epidemic and increasing prevalence of physical inactivity contribute to this trend. 4, 5 A study using NHANES 03-04 found that about 19.1% of men and 9.8% of women, aged 20–29 have prediabetes defined by impaired fasting glucose and/or impaired glucose tolerance.6 Our preliminary study revealed that about 30% of overweight and obese sedentary young adults aged 18–29 had prediabetes defined by fasting glucose or A1C test.7 When persons with prediabetes do not take appropriate preventive actions, 25% to 40% of them develop T2D in 5 years.8 This evidence has prompted more research on diabetes prevention for young adults, an age group that has been understudied in the past.2, 7, 9
The Diabetes Prevention Program (DPP), a milestone study in diabetes care, demonstrated the success of diabetes prevention through moderate weight loss (a 5–7 % loss of body weight) with dietary changes ( less fat, fewer calorie) and increased physical activity ( 150 minutes per week) .5 There was 58% reduction of T2D incidence in pre-diabetic adults during a 3-year follow-up.5 However, the participants in the DPP study were middle aged (mean age= 50.6 years) prediabetic individuals who were moderately obese (BMI= 34.0 ± 6.7) and had both impaired fasting glucose (106.5 ± 8.3 mg/dL) and impaired glucose tolerance (164.6±17.0 mg/dL).5, 10 It is unclear whether the DPP approach is generalizable and appropriate for a younger population.
Young adults with prediabetes may have different characteristics with regards to age, disease perception and progression, obesity conditions, and lifestyle habits7, 11, 12 They also have different communication and interaction channels through digital platforms (e.g., smart phone, apps, eLerarning environment) and hand-held devices.13–15 Therefore, there is a pressing need to develop a diabetes prevention program for this age group with a different empirical basis for the design using such technology. However, an intervention study using distal platforms and hand-held devices for weight management or a diabetes prevention in young adults is very rare.15 This study incorporating digital platforms (mobile applications, online activities), phone counseling, and a hand-held device was developed to reduce this current scientific gap. A former mixed-methods study (Phase 1) employing focus group interviews and a cross-sectional survey in overweight and obese young adults ages 18–29 provided the bases for the intervention. 7, 16, 17
The purpose of this pilot study was to examine the feasibility and preliminary efficacy of an age-specific diabetes prevention program to inform a larger randomized trial to be conducted in the future. The primary specific aims were to examine: 1) participants’ satisfaction of the program, 2) psychosocial variable changes (health literacy, illness perception, self-efficacy, therapeutic efficacy), and 3) behavioral changes (dietary habits and physical activity) over a 12- week period. Unlike the DPP study, weight loss was not a primary focus of the intervention or an outcome. However, it was included in the variables for a secondary aim along with the changes of other cardiometabolic risk factors (weight, A1C, fasting glucose, blood pressure, and lipids) over that time period. Also, the study examined attrition rate during the intervention period to determine the feasibility of implementation of this intervention on a larger scale.
Method
Study design
A pilot intervention using a one group pretest-posttest design was conducted to explore the feasibility of the developed diabetes prevention program for young adults (DPP-Y) and to obtain lessons to guide the planning of a full-scale study.
Participants and Setting
Fifteen participants were enrolled in this study. Fourteen participants were recruited from the phase 1 study, which assessed characteristics of young adults with prediabetes one year before, 7 and 1 participant was newly recruited. The inclusion criteria of this pilot intervention (phase 2 study) were young adults, age 18–29 years, with prediabetes (either impaired fasting glucose [IFG:100–125 mg/dL)] or an A1C of 5.7%–6.4%). Young adults diagnosed with diabetes, cardiovascular diseases, serious illness and unstable condition requiring physician-supervised dietary and exercise regimens, conditions affecting erythrocyte turnover (e.g., hemolysis, blood loss), or who were pregnant were excluded.
Overviews of Intervention for Young Adults with Prediabetes
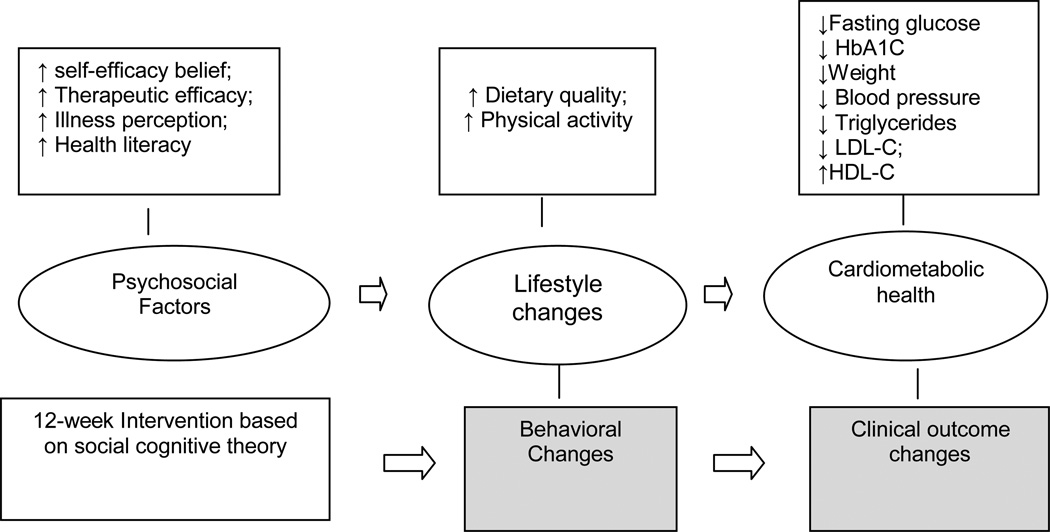
Social Cognitive Theory (SCT) and American Association of Diabetes Educators’ AADE 7 self-care Behavior (healthy eating, being active, monitoring, (taking medication), problem solving, healthy coping and reducing risk) provides a theoretical framework for the 12-week intervention.8, 18 According to SCT, psychosocial factors such as self-efficacy play a major role in improving behavioral outcomes.19 Persons with better behavioral outcomes have improved cardiometabolic health (See Figure 1). However, each individual has different baselines in knowledge, confidence, skills, facilitators and barriers, and current health behaviors. Thus, a tailored support program with agreed-upon behavioral goals is highly recommended to help individuals with prediabetes maximize their self-care confidence and skills to achieve a healthy lifestyle, which requires consistent effort and long-term commitment.8, 20, 21
Figure 1.
Theoretical Framework
Prior to the intervention, a detailed protocol for the study including recruitment, retention, data collection, and the intervention were developed by research team (a PhD nurse with CDE credential, an undergraduate, a graduate student in public health and a nurse practitioner students with RN and RD licenses) developed and all other forms, materials and activities for the intervention. Education content and delivery mechanisms were developed based on our phase 1 study activities and previous research.7, 16, 22
During focus group interviews in phase 1, the research team learned that people in this age group consistently have their own a hand-held device (e.g., smart phone) and utilize the latest digital platforms (e.g.,apps) to manage their busy lives. Thus, the main goal of this pilot intervention was to examine the feasibility of a technology based DPP-Y who use digital technology on a daily basis.13–15
Since previous studies reported very high attrition rates during 12–16 week interventions in this age group,23–25 this intervention was designed to minimize in-person didactic education and maximize the use of web-based platform, mobile applications, and email and phone communication. There was one required 2-hour in-person orientation session for participants and weekly 5–20 minute phone counseling sessions. The purpose of the phone counseling sessions were to progress with behavioral goals submitted online and review case study activities participants completed online every other week
In- Person Orientation
During the in-person orientation, participants viewed free mobile applications to input daily physical activity and food intake to assist them with improving self-efficacy and self-monitoring skills with regards to healthy eating and physical activity. Also, participants received a packet that included their individual health summary (dietary quality score and nutrient components consumed, physical activity level, and cardiometabolic risk, all from phase 1 study and/or pre-testing), the project overview, and education materials. Additionally, participants were given an iPod touch at the orientation to use during the study, or they signed a waiver to receive a $200 honorarium after the study ended if they chose to use their own device. All participants received $70 in appreciation for their participation at the post-testing.
The orientation started with a brief introduction to the study and participants’ responsibilities for the 12-week intervention period. The rest of the orientation consisted of three parts presented in lecture, demonstration and discussion format. Part 1- project website, weekly case study or behavioral goal setting activity, and mobile applications useful for self- monitoring. Part 2- healthy eating tips, portion size estimation, food label reading and mobile applications useful for dietary changes. Part 3- exercise tips and demonstrations, mobile applications useful for physical activity. All participants were encouraged to record their daily dietary and exercise habits in a wellness mobile application, which were introduced in Part 2.
The research team then counseled each participant on how to interpret the results of their health summary sheet and asked them to select a priority health area they desired to improve. Participants were assisted to set an overall behavioral goal they wanted to achieve by the end of the 12 weeks and their first bi-weekly SMART (Specific, Measurable, Attainable, Realistic, Time-bound) objective (to be achieved in next 2 weeks). The research team reviewed participants’ goal and SMART objectives and helped them to strengthen the goal and the SMART objective where needed.
Weekly intervention using digital platforms and a hand-held device
After the orientation, the primary contact person for participants was an undergraduate student on the research team. Before a call, she reviewed weekly dietary and exercise habits and bi-weekly assignments (case study or SMART objective) from the web-based platform which were reported by each participant via hand-held device and/or website log-in. A script was used to initiate the counseling session and discussed the past week dietary and exercise behaviors based on self-reported data by distal platforms, potential problem solving strategies to overcome barriers confronted. When the primary interventionist identified issues beyond her capability during weekly phone counsels (i.e., advanced dietary advice, exercise tips), she referred the participants to a graduate research assistant with more expertise. Each contact was recorded in the e-worksheet to facilitate research team communication. This e-worksheet recorded issues raised in the phone sessions, tips provided and amount of contact time for all participant-research team contact. Before making each call, research staff members were able to consult the e-worksheet to prepare for individualized phone counsel. These phone calls were made at an agreed upon time between the participant and research staff (majority of young adults wanted to have the calls in evening or on weekend). The PI, reviewed phone counseling e-worksheets to monitor the intervention fidelity and to provide timely feedback on the intervention content and messages needing to be stressed to participants by research team.
Interventionist Qualifications
A team approach (trained undergraduate and graduate students) was employed to deliver the intervention. Based on the feedback from focus group interviews, all interventionists chosen were young adults with similar characteristics of study participants. The graduate level exercise interventionist, for example, was a certified personnel trainer who had a similar body size to participants while the diet interventionist was selected because of her student status and Registered Dietician certification. The undergraduate student, well- versed in the challenges of campus life and staying healthy on-campus with a busy social and academic schedule, was an ideal candidate for the primary contact person to motivate and assist participants throughout the duration of the intervention. Training in the details of the intervention content and approach was conducted with retraining as necessary based on the PI’s review on the e-worksheets.
Variables and Measures
All variables except sociodemographic and feedback questionnaires were assessed as pre- and post- test measures. Sociodemographic questionnaire was collected at the baseline. Feedback questionnaires were collected directly after the in-person group orientation and the intervention completion (after 12 weeks).
Sociodemographics
The PI developed a Socio-Demographic Questionnaire (SDQ). Age, race/ ethnicity, health insurance status, and education years were measured. A self-reported item, "how often do you use the food label when making a food selection?" was also included to assess food label reading behavior on a 5-point Likert scale: from never (1) to always (5).
Prediabetes perception
Individuals’ perception of their prediabetes across 8 domains (identity, consequence, timeline, timeline cyclical, personal control, treatment control, emotional representations, and illness coherence) was assessed using a valid and reliable scale with 9 items (an item from each domain and an item for cause attribution), the Brief Illness Perception Questionnaire. The psychometric properties were evaluated. 26
Health literacy
Participants’ health literacy for reading food labels on an ice-cream container was assessed with a subscale of the Newest Vital Sign Scale (6 item, α=.76).27 This scale is widely used for assessing prose literacy, numeracy, and document literacy. Weiss et al., proposed a score of 4 as the cut-off of health literacy. Persons with scores of 4 and higher have very low likelihood to have healthy illiteracy while persons with scores below 4 may have limited or poor health literacy.27 In the previous research using Phase 1 study data (n=103), we utilized another scoring in the target population (overweight obese young adults aged 18–29). Three categories (High [5–6], Medium [ 3–4] and Low [0–2]) can be defined based on the obtained scores. The reported Cronbach’s alpha of the young adults aged 18–29 was .72.16
Self-efficacy
Two types of self-efficacy (physical activity (PA) self-efficacy and eating behavior self-efficacy) were assessed in this pilot intervention study. PA self-efficacy consists of two subscales measuring Task PA self-efficacy and Barrier PA self-efficacy. With the developer’s permission, one item was deleted from Barrier PA self-efficacy subscale due to the changes of populations (cancer survivors to healthy population). The item asked about participants’ confidence to do physical activity when they are nauseated. Therefore, only 12 items remained for our study. The reported Cronbach’s alphas of the original scales were α=.95 for the Barrier subscale (9 items) and α=.92 for Task subscale (4 items).28 In Phase 1 study, Cronbach’s alpha was .86 (n=106).
Eating behavior self-efficacy was measured with the Weight Efficacy Lifestyle Questionnaire (20 items, α=.70 – 90).29 The scale consists of five subscales: negative emotion, availability, social pressure, physical discomfort, and positive activity which assess the confidence to resist eating in various situations. Each subscale includes 4 items.
Therapeutic efficacy
Young adults’ outcome expectancy to prevent diabetes with lifestyle modifications was assessed with the Perceived Therapeutic Efficacy Scale (10 items, α=.93– .94).30 A sample item from the scale asks about young adults’ “level of confidence in the ability of changes of lifestyle (diet, physical activity) to control my prediabetes.” Options ranged from “no confidence [1]” to highest confidence [10]”.
Dietary behavior
A self-reported 152-item Youth/Adolescent Food Frequency Questionnaire (YAQ), which is a youth version of the food frequency questionnaire used in the Nurses’ Health Study (Willet FFQ) was used to assess dietary behavior. 31, 32 Based on participants' responses, amount of each nutrient components (e.g., dietary fiber [g], added sugar [g]) along with calories, sources of calories (e.g., carbohydrate, protein, fat) and serving sizes were recalculated. Then the values were compared by 2010 Dietary Guideline for Americans (DGA).33 The more detailed information was presented in another publication.16
Physical activity
A 7-item Modifiable Activity Questionnaire (MAQ), the primary questionnaire in the original DPP used to assess physical activity.34 As MAQ is an interviewer-administered questionnaire, the first author assessed leisure activity, occupational activity and inactivity in the past year and past week using this scale. Then, the reported activity was calculated as METs-hour per week to assess overall amount of physical activity.35
Feedback
Orientation and 12-week intervention feedback were assessed with semi-structured questionnaires. In the orientation feedback questionnaire, participants were asked about their accessibility to and usage of technology (a computer with internet, emails, Wi-Fi, Smartphone), familiarity of health-related mobile applications, and overall thoughts about orientation content and quality. The feedback questionnaire on the 12-week intervention asked about participants’ overall experience with the intervention and interventionists, usage and frequency of use of the mobile applications discussed during orientation, satisfaction with aspects of intervention (homework assignment : case studies, SMART goal formation), application of knowledge gained from the orientation, and advice for future directions. Multiple choice, short answer, and open-ended questions were included in the questionnaires.
Clinical outcomes
Cardiometabolic risk factors were assessed with anthropometric assessments and blood tests. A trained research nurse measured weight, height, blood pressure (BP), and waist circumference (WC) in a university hospital clinical research site based on the predetermined protocol. Then, body mass index (kg/m2) was calculated with the obtained weight and height. Fasting blood glucose, A1C, insulin, c-active protein and lipid were assessed using a blood sample collected from the antecubital vein after at least 8 hours of fasting.
Data analysis
Of 15 participants, 2 participants (1 woman –pregnancy, 1 man - attrition) were excluded for the data analysis. A paired-samples t-test was performed to examine changes between baseline and post-intervention on each psychosocial variables and physical markers. Because of the small sample size, the magnitudes of effect were estimated in addition to statistical significance.
Results
Sociodemographics
The majority of participants were women (76.9%, n=10), African Americans (53.8%, n=7). All participants learned their prediabetes status either when they participated in diabetes screening test in the past year or in the current year (pre-testing). All participants had their own cellular phones and access to a computer with internet access. Of 13 participants, 84.6% of participants (n=11) had a smart phone and Wi-Fi access at home. With regard to co-morbid conditions, more than half of participants had elevated blood pressure and/or dyslipidemia (See Table 1).
Table 1.
Sample Characteristics (n=13)
| n(%) / Mean ± SD | ||
|---|---|---|
| Gender | Male | 3(23.1) |
| Female | 10(76.9) | |
| Race/ethnicity | ||
| African Americans | 7 (53.8) | |
| Non-African Americans | 6 (46.2) | |
| Age | 24.38±2.24 (ranges : 21.08–28.11) |
|
| Education years | 16.08±1.12 (ranges : 14–18 years) |
|
| Health insurances | Yes | 8 (61.5) |
| No | 5 (38.5) | |
| Employment | Full time student | 5 (38.5) |
| Part time student | 3 (23.1) | |
| Full time worker | 4 (30.8) | |
| Looking for a job | 1(7.7) | |
| Obesity classification | Obesity 1 (30 >= BMI & BMI < 35) | 4(30.8) |
| Obesity 2 (35 >= BMI & BMI < 40) | 2(15.4) | |
| Obesity 3 (40 >= BMI) | 7(53.8) | |
| Participation in Phase 1 study ( diabetes screening in the past year) |
Yes | 12(92.3) |
| No | 1(7.7) | |
| Where did you learn you had prediabetes | Annual check-up with a doctor | 1(7.7) |
| Past year diabetes screening | 7(53.8) | |
| Diabetes screening as a part of pre-test | 5 (38.5) | |
| Have own cell-phone | 13 (100.0) | |
| Have smart-phone | 11(84.6) | |
| Access to computer | 13(100) | |
| Access to wifi | At home | 11(84.6) |
| At school / office | 8 (61.5) | |
| Prediabtes with elevated blood pressure † | 3 (23.1) | |
| Prediabtes with dyslipidemia †† | 4(30.8) | |
Elevated blood pressure indicates either systolic blood pressure is higher than 130mmHg or diastolic blood pressure is higher than 85mmHg .
dyslipidemia refers to either triglyceride is higher than 150 mg/dL or HDL is lower than 40 mg/dL in men or 50 mg/dL in women.
Participant satisfaction with orientation and overall intervention
Overall, the intervention was well received by participants. Table 2 shows the details regarding the responses of the participants. On a 5-point satisfaction scale, participants gave the overall intervention score a 4.15. The participants emphasized the support team and the phone counseling (46.2%) as the best aspects of the intervention experience while the case studies were least helpful to the participants. They also reported many other benefits from applying knowledge learned during the intervention. About 92% of participants reported a portion size was decreased during the intervention period and 69.2% of participants had felt an increase in their energy levels. With regard to lifestyle changes, the participants reported that increasing physical activity was the hardest, while eating right was the easiest (See Table 2).
Table 2.
Intervention Feedback (n=13)
| n (%) | Possible score |
Obtained scores (mean ± SD) |
|
|---|---|---|---|
| Overall rating of Intervention | 1–5 | 4.2 ±.7 | |
| Portion Size changes | Decreased : 12 (92.3) | ||
| Energy Level changes | Increased: 9 (69.2) | ||
| Application used most | My fitness pal : 8(61.5) | ||
| Application used least | Mood tracker: 4(30.8) | ||
| Most helpful learning method | Phone counseling : 6(46.2) | ||
| How helpful was the phone counseling | 1–5 | 4.1±.8 | |
| Least helpful learning method | Case studies : 8(61.5) | ||
| How helpful were the case studies | 1–5 | 3.1±1.2 | |
| Extent achieve SMART goals | 1–5 | 3.5 ± .8 | |
| Hardest thing to accomplish | Increasing Physical activity : 6 (46.2) | ||
| Easiest thing to accomplish | Improving diet : 8 (61.5) |
Psychological factor changes
Over 12 weeks, there was a significant decrease in health literacy on food label use. However, the participants reported they had a significantly better understanding of their prediabetes (therapeutic efficacy). They were significantly more confident in their ability to resist eating although they were experiencing significantly more negative emotions. The participants were more confident in performing physical activity even amidst barriers and challenges. Their task physical activity self-efficacy (e.g., brisk walking for 20 minutes without stopping) was also increased. However, there was no significant difference between pre-testing and post-testing with regard to therapeutic efficacy (See Table 3).
Table 3.
Changes of psychological variables
| Variables | Pre-test | Post-test | p-value | Effect size | ||
|---|---|---|---|---|---|---|
| Mean ± SD | Obtained ranges | Mean ± SD | Obtained ranges | |||
| Health literacy | 5.2±1.0 | 3–6 | 4.0±1.2 | 1–5 | <.001 | −1.03 |
| Illness perception | ||||||
| Consequence | 5.5 ± 3.9 | 0–10 | 5.1 ± 3.0 | 2–10 | .624 | −0.11 |
| Timeline | 3.1 ± 2.7 | 0–8 | 2.9 ± 2.4 | 0–7 | .598 | −0.09 |
| Personal control | 7.1 ± 2.1 | 3–10 | 7.9 ± 2.4 | 1–10 | .305 | 0.34 |
| Treatment control | 8.7 ± 1.7 | 4–10 | 9.1 ± 1.6 | 5–10 | .293 | 0.24 |
| Identify | 3.4 ± 2.8 | 0–9 | 3.9 ± 2.7 | 0–8 | .573 | 0.17 |
| Emotional representation | 6.8 ± 2.6 | 3–10 | 6.5 ± 2.0 | 2–10 | .774 | −0.10 |
| Illness comprehensibility | 6.1 ± 1.8 | 3–9 | 8.6 ± 1.3 | 7–10 | <.001 | 1.64 |
| Eating behavior Self-efficacy | ||||||
| Negative emotion | 3.8±1.9 | 0–6.5 | 5.6±1.5 | 3.8–8.5 | .002 | 1.04 |
| Food availability | 5.0±.78 | 3.3 – 6.0 | 5.2±1.3 | 1.8–6.3 | .675 | 0.18 |
| Social pressure | 5.7±1.8 | 2.5–8.5 | 5.7± 1.7 | 3.3–7.8 | .946 | 0.02 |
| Physical discomfort | 6.3±1.3 | 4.8–8.3 | 6.6 ± 0.9 | 5.0–7.8 | .511 | 0.27 |
| Other activity | 6.3±1.7 | 2.0–8.8 | 6.9 ±1.2 | 5.0–8.5 | .308 | 0.37 |
| Physical activity (PA) self-efficacy | ||||||
| Barrier PA self-efficacy | 27.2±17.3 | 0.00 –56.3 | 37.0 ±17.4 | 11.3 –76.3 | .166 | 0.57 |
| Task PA self-efficacy | 58.7±21.1 | 12.5–90.0 | 66.5±23.3 | 27.5–100.0 | .055 | 0.36 |
| Therapeutic self-efficacy | 8.4±1.4 | 5.33–10 | 8.4±2.0 | 3.2–10 | .908 | 0.03 |
Behavioral changes
Table 4 shows the behavioral changes over 12 weeks. The food label use behaviors were improved over 12 weeks. The average amount of physical activity at 12 weeks was 37.34 METs- hour/week, a 2.66-fold increase compared to the pre-test measure(large effect size, Cohen’s d=.80). Also, participants adopted better dietary habits over the 12-week intervention period. While carbohydrate, trans fat, saturated fat, sodium and added sugar intake decreased; protein, dietary fiber and vegetable consumption were increased. Other changes in dietary habits were also reported: cholesterol consumption was increased and calcium intake was reduced (See Table 4).
Table 4.
Behavioral changes over 12 weeks.
| Variables | Recommendations | Pre-test | Post-test | p-value | Effect size |
|---|---|---|---|---|---|
| Physical activity | ≥ 10 METs-hour/week | 14.1±14.0 (Median : 8.4) |
37.3±39.0 (Median :17.1) |
.035 | 0.80 |
| Dietary habits | 2010 Dietary Guidelines a | ||||
| † Total calorie intakes (Kcal) | 1800–2000Kcal for women; 2400–2600Kcal for men | 1623.1±658.7 | 1497.1 ± 500.8 | .58 | −0.22 |
| % of carbohydrate of total calorie intake | 45–65% | 54.4 ± 6.8 | 51.8 ±7.5 | .05 | −0.37 |
| % of protein of total calorie intake | 10–35% | 17.8 ± 3.6 | 19.7 ±3.8 | .08 | 0.52 |
| % of total fat of total calorie intakes | 20–35% | 29.2 ± 5.3 | 29.7 ± 6.6 | .72 | 0.09 |
| % of saturated fat of total calorie intake | <10% | 9.7 ± 2.1 | 9.2 ± 2.2 | .39 | −0.23 |
| Cholesterol (mg) | < 300mg | 220.5 ± 114.7 | 241.2 ± 95.7 | .58 | 0.20 |
| Transfat | 0 | 2.1 ± 1.3 | 1.5 ± 0.5 | .13 | −0.59 |
| Calcium | 1000mg | 767.6 ± 302.9 | 704.6 ± 347.3 | .55 | −0.19 |
| §§ Fruit | 1 &1/2–2 cups | 1.7 ± 1.0 | 1.5 ± 0.9 | .51 | −0.21 |
| §§ Vegetables | 2& 1/2–3 cups | 3.2 ± 1.7 | 3.6 ± 1.9 | .59 | 0.23 |
| Dietary fiber (g) | 14g/1000 Kcal | 19.5 ± 8.1 | 19.1±8.4 | .90 | −0.05 |
| § Sodium (mg) | < 2300mg/day | 1857.5 ± 864.0 | 1665.6 ± 605.5 | .51 | −0.26 |
| ††Added sugar (g) | < 25g for women; < 37.5g for men | 47.4 ± 23.7 | 39.5 ± 17.0 | .24 | −0.39 |
2010 dietary guidelines for American.
AHA recommendation for added sugar 31
Calorie intakes for sedentary individuals ages 19–30
2300 mg/day is the tolerable upper intake level; 1500mg/day is adequate intake for individuals ages 9 years and older.
Based on 1,800–2,600 Kcal/day
Cardiometabolic risk changes
There were significant decreases in BMI, weight, and A1C. There were no statistically significant differences on participants’ fasting glucose. After 12 weeks, one participant actually developed asymptomatic diabetes (fasting glucose =140, A1C =7.0%) while 5 young adults reverted back to euglycemia (fasting glucose was less than 100mg/dL and A1C was less than 5.7%). Systolic blood pressure marginally decreased (p=.052), but no significant difference was identified on the diastolic blood pressure. Overall, no statistical difference was identified on the lipids although the numbers increased, especially with triglycerides. Table 5 shows the details of the cardiometabolic changes over 12 weeks (See Table 5).
Table 5.
Cardiometabolic risk changes (n=13)
| Metabolic risk cut-offs | Having metabolic risk n (%) |
Mean ± SD | p- value |
Effect size | |||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||
| BMI | Obesity ≥ 35.0 | 41.0±7.3 (ranges: 31.0 – 51.3) |
40.1±7.0 (ranges : 30.7–51.8) |
.027 | −0.13 | ||
| Weight (pound) | N/A | 255.9 ± 56.2 (ranges : 186.3– 363.8) |
249.5±51.5 (ranges : 184.3 – 340.2) |
.031 | −0.12 | ||
| Systolic blood pressure (mmHg) | ≥130mmHg | 4 | 2 | 124.9±17.5 (ranges :105–161) |
117.5±16.8 (ranges : 82–149) |
.052 | −0.43 |
| Diastolic blood pressure (mmHg) | ≥ 85 mmHg | 2 | 2 | 76.3 ±14.6 (ranges: 56–109) |
74.7±11.7 (ranges:61–103) |
.665 | −0.12 |
| Fasting glucose (mg/dL) | ≥100mg/dL | 3 | 3 | 92.5±11.3 (ranges: 81–118) |
97.6±14.3 (ranges: 82–140) |
.112 | 0.39 |
| A1C (%) | ≥ 5.7% | 11 | 6 | 6.0±0.5 (ranges: 5.2–6.8) |
5.6±.5 (ranges: 4.9–7.0) |
.007 | −0.76 |
| Insulin (mmol) | N/A | N/A | N/A | 28.2±13.1 (ranges:15.3–64.7) |
26.4±15.5 (ranges: 16.2–63.9) |
.497 | −0.13 |
| hsCRP | N/A | N/A | N/A | 8.5±9.5 (ranges: 1.6–37.8) |
7.7±6.0 (ranges :1.7 – 22.4) |
.614 | −0.09 |
| Total cholesterol (mg/dL) | ≥200 mg/dL | 3 | 3 | 182.3±23.9 (ranges : 134–221) |
184.9±18.8 (ranges: 155–224) |
.636 | 0.12 |
| Triglyceride(mg/dL) | ≥150 mg/dL | 2 | 2 | 97.9±48.6 (ranges: 39–208) |
109.5±61.4 (ranges : 45–246) |
.318 | 0.21 |
| LDL (mg/dL) | ≥100mg/dL | 8 | 10 | 114.3±26.3 (ranges:78–151) |
117.0±18.3 (ranges:89–150) |
.520 | 0.12 |
| HDL (mg/dL) | < 40 in men; < 50 in women |
48.5±13.2 (31–71) |
46.2±8.9 (29–62) |
.367 | −0.21 | ||
Discussion
Prediabetes is a state of higher than normal blood glucose level without symptoms but a starting point for tissue damage and cardiovascular complications.8, 36, 37 Fortunately, this precursor condition of type 2 diabetes (T2D) can be reversed with an appropriate intervention in many people.8, 38 Therefore, it is important to inform young adults with prediabetes of their T2D risk and refer them to a primary care provider or an effective ongoing support program.21, 39
There is a consensus that early detection and prevention targeting young adults with prediabetes, especially minority populations is urgent and significant.1, 2, 40 Young adults do not reap the benefits from advanced science of diabetes care since they often perceive themselves as being healthy and therefore rarely see a doctor.41 Also, health care professionals often advise these prediabetic patients to “just to do annual checks”, or assure them that there is “nothing to worry about.” 42, 43 Therefore, there is a need for an effective diabetes prevention program employing adult learning theory and other appropriate strategies targeted to this age group. The incorporation of strategies to promote behavioral changes (being active, eating right) and modify lifestyles to ultimately prevent or manage young adults’ prediabetes is essential.8, 44 The current study contributes evidence toward this type of intervention.
This intervention showed great potential to prevent T2D in young adults with prediabetes. Overall, participants were satisfied with the education content and contact with research team. The retention rate over the 12 week intervention period was 86.7 %, which was very high in this age group compared to other studies.23, 24 A previously conducted 12- week intervention showed a 42.9 % attrition rate while a much shorter intervention lasting 4 weeks had a 15.8 % attrition rate after the randomization. Weekly contact served as motivation and triggers which are two important factors to produce a target behavior.44 Also, this contact provided participants with practical tips and feedback based on reviews of their current behaviors, which facilitated behavior change. 44 Changes in behavioral and clinical outcomes were very promising.
Several psychological factors (e.g., prediabetes perception, self-efficacy) were improved. Positive changes in psychological factors generated healthier lifestyles, which eventually produced clinical outcome improvements, such as reduction in A1C and weight (Figure 1). However, as previously discussed, clinical outcomes (A1C and weight loss) were secondary aims and behavior change was prioritized in the current study. After the 12- week behavioral intervention, participants were more physically active and their dietary habits were healthier. Participants consumed less calories, carbohydrates, saturated fat, trans fat, sodium, and added sugar while they consumed more protein and vegetables. Although the participants reported lower consumption of dietary fiber, calcium and fruit, and higher consumption of cholesterol, the findings should be cautiously interpreted due to the following reasons. First, total grams of dietary fiber were decreased but the total calorie intake was also decreased. That is, a ratio of fiber to total calories was increased. Second, decreased calcium intake may be related to the reduction of overall dairy intake (cheese, whole milk, etc), which was replaced with vegetables, and nuts. Since calcium intake with vitamin D 8, 45 is important to prevent type 2 diabetes, adequate replacement (e.g., whole milk to 1% milk) and calcium supplement intakes need to be emphasized in the future intervention. 6, 44 Next, the decrease in fruit consumption among the participants may be related to our education emphasis. Since all our participants were obese, we stressed being careful when selecting the “right” beverage in the orientation. Since fruit juice includes dense calories in relatively small amounts, we encouraged the participants to eat raw fruits instead of fruit juice. Also, we emphasized food diversity and vegetable consumptions rather than “fruit/vegetable consumption itself”, since those are the areas to be focused on in nutrition education in overweight and obese young adults according to our phase 1 study results. Finally, cholesterol consumption slightly increased but statistically not significant. The increased intake was still in the recommended ranges (< 300 mg for cholesterol), and changes in serum cholesterol level was negligible (See Table 5).
While Hebden and colleagues reported BMI reduction from 27.3 to 26.7 in an intervention using mHealth in young adults,15 the reduction of BMI in the current study was larger ( from 41.0 to 40.1). Also, A1C (from 6.0% to 5.6%) and systolic blood pressure (124.9 to 117.5) were decreased while fasting glucose was not improved (See Table 5) which was similar to the finding of a previous study.46 These, in fact, were interesting differences between the original DPP trial and the current study.5 In the DPP, fasting glucose was decreased from 106 to 102 while A1C was very marginally decreased from 5.91 to 5.81 during the 6 months in the lifestyle group.5 Potential reasons of these differences may be the differences in sociodemographics, current lifestyle factors (e.g., physical activity level). 7 A future study with a larger sample and a longer intervention period is required to provide more effective answers regarding these differences.
The major weaknesses of the study were the limited number of participants, a short intervention period, and a quasi-experimental study design to examine actual intervention effects. However, the study provided the researchers with information on feasibility, effect size and how to modify the diabetes prevention program for young adults to be more effective and acceptable in a larger clinical trial. Therefore, this pilot study is an excellent starting point for the development of a full-scale study, diabetes prevention program for young adults with prediabetes in the future.
Conclusions
In general, young adults with prediabetes had favorable experiences with our intervention and implementing this intervention to promote T2D prevention and management for this population is very feasible. The participants reported that the intervention was practical and helpful in motivating them to make behavioral changes. In particular, they liked being able to access the research team by phone and became very comfortable seeking advice, practical tips, and answers to their questions. From the researchers’ perspectives, we have gained insights regarding accessing and recruiting at-risk young adults, important programmatic foci, and intervention delivery methods that can be refined in the future to help young adults with prediabetes improve their healthy lifestyle habits and reduce the overall burden of type 2 diabetes.
Acknowledgment
We acknowledge the National Institute of Nursing Research (K01NR012779), the Emory University (University Research Committee and Atlanta Clinical & Translational Science Institute (ACTSI) collaborative grant), and Atlanta Clinical and Translational Science Institute (UL1 RR025008) for their support of this study. The authors sincerely express greatest gratitude to Dr. Judith A Erlen (University of Pittsburgh School of Nursing), all research staff, nurses in ACTSI’s clinical research unit, study participants, community partners and reviewers.
References
- 1.Dabelea D, Bell RA, D'Agostino RB, Jr, Imperatore G, Johansen JM, Linder B, Waitzfelder B. Incidence of diabetes in youth in the United States. JAMA. 2007;297(24):2716–2724. doi: 10.1001/jama.297.24.2716. [DOI] [PubMed] [Google Scholar]
- 2.Mainous AG, 3rd, Baker R, Koopman RJ, Saxena S, Diaz VA, Everett CJ, Majeed A. Impact of the population at risk of diabetes on projections of diabetes burden in the United States: an epidemic on the way. Diabetologia. 2007;50(5):934–940. doi: 10.1007/s00125-006-0528-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Diabetes Association. Fast Facts: Data and Statistics about diabetes March 2013. American Diabetes Association; 2013. [Google Scholar]
- 4.Jackson L. Translating the Diabetes Prevention Program into practice: a review of community interventions. Diabetes Educ. 2009;35(2):309–320. doi: 10.1177/0145721708330153. [DOI] [PubMed] [Google Scholar]
- 5.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park J, Mendoza JA, O'Neil CE, Hilmers DC, Liu Y, Nicklas TA, Nicklas TA. A comparison of the prevalence of the metabolic syndrome in the United States (US) and Korea in young adults aged 20 to 39 years. Asia Pac J Clin Nutr. 2008;17(3):471–482. [PubMed] [Google Scholar]
- 7.Cha E, Umpierrez G, Kim KH, Bello MK, Dunbar SB. Characteristics of American young adults with increased risk for type 2 diabetes: a pilot study. Diabetes Educ. 2013;39(4):454–463. doi: 10.1177/0145721713486199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Association of Diabetes Educators. The Art and Science of Diabetes Self-Management Education Desk Reference. 2nd ed. AADE: 2011. [Google Scholar]
- 9.Morrell JS, Lofgren IE, Burke JD, Reilly RA. Metabolic syndrome, obesity, and related risk factors among college men and women. Journal of American college health : J of ACH. 2012;60(1):82–89. doi: 10.1080/07448481.2011.582208. [DOI] [PubMed] [Google Scholar]
- 10.The Diabetes Prevention Program Research Group. The 10-year cost-effectiveness of lifestyle intervention or metformin for diabetes prevention: an intent-to-treat analysis of the DPP/DPPOS. Diabetes care. 2012;35(4):723–730. doi: 10.2337/dc11-1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andersson S, Ekman I, Lindblad U, Friberg F. It's up to me! Experiences of living with pre-diabetes and the increased risk of developing type 2 diabetes mellitus. Primary Care Diabetes. 2008;2(4):187–193. doi: 10.1016/j.pcd.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 12.Adriaanse MC, Snoek FJ, Dekker JM, van der Ploeg HM, Heine RJ. Screening for Type 2 diabetes: an exploration of subjects' perceptions regarding diagnosis and procedure. Diabet Med. 2002;19:406–411. doi: 10.1046/j.1464-5491.2002.00710.x. [DOI] [PubMed] [Google Scholar]
- 13.Newport F. U.S. Young Adults Admit Too Much Time on Cell Phones, Web. [Accessed January 29, 2014];Gallup. 2012 Apr 12; Available at: http://www.gallup.com/poll/153863/young-adults-admit-time-cell-phones-web.aspx.
- 14.Vitak J. New communication technologies' impact on young adults. [Accessed Januray 29, 2014];The Pew Research Center's Internet & American Life Project. 2008 May 15; Available at: http://www.pewinternet.org/Commentary/2008/May/New-communication-technologies-impact-on-young-adults.aspx.
- 15.Hebden L, Cook A, van der Ploeg HP, King L, Bauman A, Allman-Farinelli M. A mobile health intervention for weight management among young adults: a pilot randomised controlled trial. J Hum Nutr Diet. doi: 10.1111/jhn.12155. In press. [DOI] [PubMed] [Google Scholar]
- 16.Cha E, Kim KH, Lerner HM, Dawkin CR, Bello MK, Umpierrez G, Dunbar SB. Health Literacy, Self-efficacy, Food Label Use, and Diet in Young Adults. Am J Health Behav. 2014;38(3):331–339. doi: 10.5993/AJHB.38.3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cha ES, Jennings B, Lerner H, Dunbar SB. How young adults with prediabetes perceive their condition and prevention activities. Ann Behav Med. 2014;47(Supplement):S107. [Google Scholar]
- 18.Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice Hall: Englewood Cliffs, N.J; 1986. [Google Scholar]
- 19.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 20.Katula JA, Vitolins MZ, Morgan TM, Lawlor MS, Blackwell CS, Isom SP, Goff DC., Jr The Healthy Living Partnerships to Prevent Diabetes study: 2-year outcomes of a randomized controlled trial. Am J Prev Med. 2013;44(Suppl 4):S324–S332. doi: 10.1016/j.amepre.2012.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Diabetes Association. Standards of medical care in diabetes--2014. Diabetes care. 2014;37(Suppl 1):S14–S80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 22.Korkiakangas EE, Alahuhta MA, Laitinen JH. Barriers to regular exercise among adults at high risk or diagnosed with type 2 diabetes: a systematic review. Health Promot Int. 2009;24(4):416–427. doi: 10.1093/heapro/dap031. [DOI] [PubMed] [Google Scholar]
- 23.Middleton KR, Perri MG. A randomized trial investigating the effect of a brief lifestyle intervention on freshman-year weight gain. J Am Coll Health. 2014;62(2):101–109. doi: 10.1080/07448481.2013.849259. [DOI] [PubMed] [Google Scholar]
- 24.Pearson ES, Irwin JD, Morrow D, Hall CR. The CHANGE program: comparing an interactive versus prescriptive obesity intervention on university students' self-esteem and quality of life. Appl Psychol Health Well Being. 2012;4(3):369–389. doi: 10.1111/j.1758-0854.2012.01080.x. [DOI] [PubMed] [Google Scholar]
- 25.D'Alonzo KT, Stevenson JS, Davis SE. Outcomes of a program to enhance exercise self-efficacy and improve fitness in Black and Hispanic college-age women. Res Nurs Health. 2004;27(5):357–369. doi: 10.1002/nur.20029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Broadbent E, Petrie KJ, Main J, Weinman J. The Brief Illness Perception Questionnaire. J Psychosom Res. 2006;60(6):631–637. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 27.Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, Hale FA. Quick Assessment of Literacy in Primary Care: The Newest Vital Sign. Ann Fam Med. 2005;3(6):514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rogers LQ, McAuley E, Courneya KS, Verhulst SJ. Correlates of physical activity self-efficacy among breast cancer survivors. Am J Health Behav. 2008;32(6):594–603. doi: 10.5555/ajhb.2008.32.6.594. [DOI] [PubMed] [Google Scholar]
- 29.Clark MM, Abrams DB, Niaura RSE, C A, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol. 1991;59:739–744. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- 30.Dunbar-Jacob J. Perceived Treatment Efficacy: Assessment in Rheumatoid Arthritis. Ann Behav Med. 1993;15S:S147. [Google Scholar]
- 31.Rockett HR, Wolf AM, Colditz GA. Development and reproducibility of a food frequency questionnaire to assess diets of older children and adolescents. J Am Diet Assoc. 1995;95(3):336–340. doi: 10.1016/S0002-8223(95)00086-0. [DOI] [PubMed] [Google Scholar]
- 32.Rockett HR, Breitenbach M, Frazier AL, Witschi J, Wolf AM, Field AE, Colditz GA. Validation of a youth/adolescent food frequency questionnaire. Prev Med. 1997;26(6):808–816. doi: 10.1006/pmed.1997.0200. [DOI] [PubMed] [Google Scholar]
- 33.U. S. Department of Agriculture and U. S Department of Health and Human Service. Dietary guidelines for American 2010. Washinton DC: US Government Printing Office; 2010. [Google Scholar]
- 34.Kriska AM. Modifiable Activity Questionnaire. Med Sci Sports Exerc. 1997;29(Suppl 6):S73–S78. [Google Scholar]
- 35.Kriska AM, Edelstein SL, Hamman RF, Otto A, Bray GA, Mayer-Davis EJ, Regensteiner JG. Physical activity in individuals at risk for diabetes: Diabetes Prevention Program. Med Sci Sports Exerc. 2006;38(5):826–832. doi: 10.1249/01.mss.0000218138.91812.f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Huebschmann AG, Regensteiner JG, Vlassara H, Reusch JE. Diabetes and advanced glycoxidation end products. Diabetes care. 2006;29(6):1420–1432. doi: 10.2337/dc05-2096. [DOI] [PubMed] [Google Scholar]
- 37.Hu FB, Stampfer MJ, Haffner SM, Solomon CG, Willett WC, Manson JE. Elevated risk of cardiovascular disease prior to clinical diagnosis of type 2 diabetes. Diabetes care. 2002;25(7):1129–1134. doi: 10.2337/diacare.25.7.1129. [DOI] [PubMed] [Google Scholar]
- 38.American Diabetes Association. Standards of medical care in diabetes-2013. Diabetes Care. 2013;36(Sppl 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Perreault L, Pan Q, Mather KJ, Watson KE, Hamman RF, Kahn SE. Effect of regression from prediabetes to normal glucose regulation on long-term reduction in diabetes risk: results from the Diabetes Prevention Program Outcomes Study. Lancet. 2012;379(9833):2243–2251. doi: 10.1016/S0140-6736(12)60525-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang ES, Basu A, O'Grady M, Capretta JC. Projecting the future diabetes population size and related costs for the U.S. Diabetes care. 2009;32(12):2225–2229. doi: 10.2337/dc09-0459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gores SE. Addressing nutritional issues in the college-aged client: strategies for the nurse practitioner. J Am Acad Nurse Pract. 2008;20(1):5–10. doi: 10.1111/j.1745-7599.2007.00273.x. [DOI] [PubMed] [Google Scholar]
- 42.Troughton J, Jarvis J, Skinner C, Robertson N, Khunti K, Davies M. Waiting for diabetes: Perception of people with pre-diabetes: A qualitative study. Patient Educ Couns. 2008;72:88–93. doi: 10.1016/j.pec.2008.01.026. [DOI] [PubMed] [Google Scholar]
- 43.Eborall H, Davies R, Kinmonth A-L, Griffin S, Lawton J. Patients’ experiences of screening for type 2 diabetes: prospective qualitative study embedded in the ADDITION(Cambridge) randomised controlled trial. BMJ. 2007;335(7618):490. doi: 10.1136/bmj.39308.392176.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fogg B. Proceedings of the 4th International Conference on Persuasive Technology. Claremont, California: ACM; 2009. A behavior model for persuasive design; pp. 1–7. [Google Scholar]
- 45.Fung GJ, Steffen LM, Zhou X, Harnack L, Tang W, Lutsey PL, Van Horn LV. Vitamin D intake is inversely related to risk of developing metabolic syndrome in African American and white men and women over 20 y: the Coronary Artery Risk Development in Young Adults study. Am J Clin Nutr. 2012;96(1):24–29. doi: 10.3945/ajcn.112.036863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Orchard TJ, Temprosa M, Barrett-Connor E, Fowler SE, Goldberg RB, Mather KJ, Watson KE. Long-term effects of the Diabetes Prevention Program interventions on cardiovascular risk factors: a report from the DPP Outcomes Study. Diabet Med. 2013;30(1):46–55. doi: 10.1111/j.1464-5491.2012.03750.x. [DOI] [PMC free article] [PubMed] [Google Scholar]