Abstract
South African men who have sex with men (MSM) are at increased risk for HIV infection, and male condoms are fundamental to HIV prevention programs. We explored condom use experiences through in-depth interviews with 34 MSM in Cape Town and Port Elizabeth, South Africa. For data analysis, we generated a codebook and used the constant comparison method. Condom use reinforcing elements included use of alternative sexual strategies, having a high level of self-worth that was linked to protective behaviors, and use of ready-made condom negotiation scripts. Elements inhibiting condom use included perceiving substantial declines in sexual pleasure/performance, experiences of condom failure (possibly related to petroleum-based lubricant), and being in trusted relationships. Our findings suggest nuanced HIV prevention approaches such as bolstering condom negotiation skills based on successful tactics already in use. Further research is needed to address how to mitigate perceptions and experiences that condoms negatively impact sexual pleasure and performance.
Introduction
Consistent with data from other low- and middle-income settings, Sub-Saharan African men who have sex with men (MSM) are at increased risk of HIV infection relative to the general Sub-Saharan African population (1). These increased risks are, in part, related to factors inherent to all MSM epidemics, such as biologic vulnerability linked to anal intercourse (2) and increased prevalence of HIV infection in male sex partners (3). Additionally, a range of context-specific factors at individual, social, and structural levels also influence HIV transmission and acquisition risks (3). Male condoms are a key component of HIV prevention programs for MSM; condoms are estimated to decrease HIV transmission for anal sex between men by approximately 78% (4). Behavioral change interventions may increase uptake; a recent meta-analysis found behavioral programs targeting increased condom use in USA and Europe produced a 27% average decrease in unprotected anal intercourse (UAI) among MSM (5). Yet a recent review found few instances of rigorous assessment of behaviorally-based HIV intervention programs for MSM in lower- and middle-income settings (4). Additionally, HIV prevention programs aimed at MSM are rare relative to national-level programs targeted to heterosexuals (6), including in South Africa (7).
Although nationally representative data regarding HIV prevalence among MSM in South Africa are not available, point HIV prevalence assessments from three studies with participant having median age less than 25 were 33% in Soweto (year data collection: 2008, sample size (n)=378)) (8), 50% in Johannesburg (year: 2008, n=285) (9), and 26% in Cape Town (year: 2009, n=200) (10). These estimates suggest high absolute HIV levels, and an increased HIV burden relative to the 5.1% national for 20–24 year old South African males (year: 2009) (11).
A number of individual and dyadic factors have been found to be associated with UAI among MSM in South Africa, including alcohol consumption (12), having a stable, familiar or trusted main partner (13, 14), self-efficacy in using and negotiating condoms (15), and depression (15). These correlations are not unique to studies in South Africa, because each of these factors has also been associated with UAI outside of South African settings (16–21). These studies indicate that in South Africa, type of sexual partnership, the role of alcohol, condom skills, and mental health should be considered in condom promotion interventions. Yet more detailed information in these areas is needed to identify how, and in what manner, to seek change. For instance, how can programs best support condom use in main partnerships, tailor promotional messages regarding condoms to MSM, or improve condom negotiation skills.
Services and HIV prevention programs that have been tailored to MSM in South Africa indicate promising potential, such as a pilot program among MSM in Cape Town that provided information, condoms and water-based lubricant access to 98 participants (22). Other MSM-targeted HIV prevention programs in Eastern and Sub-Saharan Africa also indicated promise. In Kenya, MSM sex workers who reported ever attending a MSM-friendly center or clinic were less likely to report UAI than their peers (23). In Senegal, men who had participated in at least one HIV prevention program targeting MSM (such as HIV testing and counseling) were also less likely to report UAI than their peers (24). Knowledge about HIV related to male-male sex, such as anal sex being a mode for HIV transmission, was also associated with higher levels of condom use for anal intercourse in studies from Eastern and Sub-Saharan Africa, including one from South Africa (12, 23, 25). Together, these data indicate the importance of providing MSM-specific condom promotion elements for HIV prevention programs in South Africa.
The present qualitative study sought to explore how a group of MSM in Cape Town and Port Elizabeth, South Africa make decisions about using condoms with their male partners. In order to understand at a more granular level the factors that influence men’s choices to use or not use condoms, we qualitatively assessed successful strategies that men used to navigate condom-protected sex on a routine basis. We also attempted to identify instances of positive deviance, which are instances where individuals have an improved outcome in a given situation relative to others in their community (26). We sought to assess condom negotiation tactics in consideration of various relationships and physical environments in which sex takes place, and to explore consistent condom use, defined for this study as using condoms for all anal sex acts. Information generated from this study can be considered in developing HIV prevention programs in South Africa, and would likely benefit the development of condom promotion messages tailored to MSM in South Africa.
Methods
Ethics Statement
Ethical clearance to conduct the study was provided by the Emory Institutional Review Board and by ethical review boards at Desmond Tutu Healthcare Foundation and the Human Sciences Research Council. All participants provided written informed consent.
Sample
The current study was part of a larger project aimed at developing a combination package of HIV prevention interventions for MSM at sites in Cape Town (CT) and Port Elizabeth (PE), South Africa. Sampling of MSM for the qualitative component of this research aimed to assess attitudes towards enhanced services, and to explore sex frequency and partnership characteristics through activity-based assessments such as network maps. To ensure that we gained sufficient sample size for the variety of different assessments, we recruited a large sample, intending to use the full sample to inform quantitative analysis and to use a portion of the sample to inform qualitative assessment. The final total sample included 79 MSM in-depth interviews.
About half of participants were recruited based on previously-developed lists of MSM in the community gathered by collaborating Community-Based Organizations (CBO). Of this group, participants from Cape Town were affiliated with the Men’s Division of the Desmond Tutu HIV Foundation (a CBO offering MSM-specific services for healthcare and HIV prevention) and participants from Port Elizabeth were affiliated with Masiphume (a local CBO support group for LGBT). The other half of participants were recruited through snowball sampling methods (27), which were used to increase and diversify the sample. Eligible participants were male at birth, reported anal sex with another man in the last six months, were aged 18 years or older, and were able to understand and respond to study questions in one of the predominant languages of the study sites: English, Xhosa, or Afrikaans. Participants were contacted through phone calls, and given a brief description of study procedures and aims. Interested men were invited to participate in face-to-face interviews scheduled at several private sites at conveniently located local clinics and CBO offices.
Based on our sampling strategy, we anticipated for the present analysis that we would reach data saturation prior to analyzing all 79 in-depth interviews. We therefore sub-sampled 34 interviews using a typical case purposive sampling strategy, seeking to understand the experiences of a broad cross-section of MSM (27). To obtain variation in the subsample that may be reflective of major groups in the general population, we sampled across categories of race (white, coloured, black), HIV status (self-reported negative, positive), and age (18–25, >25). Following data analysis, we determined that we had reached saturation based on guidance from Charmaz, including assessment of depth of data between and within categories, and how further analysis illuminated theoretical categories (28).
Procedures
In early 2012, a series of in-depth interviews were conducted by four research assistant interviewers with extensive qualitative research experience. This group included two authors of this manuscript, AdV and ZK. The interviewers used a semi-structured, in-depth interview guide that addressed domains of sexual identity, coming out experiences, sexual practices, HIV prevention experiences, community involvement, resilience, and social/sexual network visual diagramming exercises. For this study, we focused on interview sections regarding sexual practices and HIV prevention experiences, but did not exclude informative data coming from other interview sections. Questions from these sections included items exploring condom use; for instance, men reporting condom use were asked, “Why did you (start/stop) using condoms with your current partner?” and “What kinds of challenges did condom use cause you?” For men who reported not using condoms, we explored past experiences and current reasons for not using condoms. Follow-up questions addressed the impacts of condom use across time, such as, “How did condom use affect or change your relationship?” HIV prevention experiences were explored through questions about test seeking such as, “What made you decide to get tested for HIV?”, while HIV-protective behaviors were explored through items such as, “Please describe the way (specific sexual experience) changed the way you viewed yourself.” Interviews were conducted in private, lasted an average of 90-minutes, were audio-recorded with permission, and were later transcribed for data analysis. All participants completed informed consent procedures and received 80 Rand (approximately $10 USD) for their time and travel expenses.
Data Analysis
Because this study was exploratory, data analysis was based on the constant comparison method, drawing on Grounded Theory techniques (29). The inductive codebook underpinning the present analysis was developed based on iterations of independent analysis among three coders, followed by consensus revisions. A code system, consisting of 66 different codes or sub-codes, was established to categorize themes emerging from the data. Examples of codes include: ‘condom hedonism’, defined as positive or negative beliefs regarding the intersection of condoms and pleasure, ‘condom rationales’ defined as reasons listed for use or non-use of condoms, and other codes such as ‘petroleum-based lubricant’ or ‘exchange sex’.
Analyses based on codes, code definitions, and memos assessed emergent themes and theme intersections through conceptual mapping, a technique of developing visual images that locate concepts, and direct movement between them (28). Applied to our data, we looked at codes such as ‘alcohol and sex’, and sought to situate them within a broader understanding of how men make condom use decisions. This process, grounded in continually returning to the data to test relationships and groupings, facilitated a deeper understanding of identified themes. Some themes developed for the visual model, such as “negotiation scripts”, which are pre-scripted strategies men utilized to negotiate condom use, we identified based on emic themes from the data. After development of the visual model, the data were recoded, where each model component was assigned a code and applied to the data. This technique allowed us both to assess the frequency of themes identified in our model, and to more systematically explore interactions across themes. We report theme frequency in our data, despite the non-generalizable nature of the qualitative process, to provide a general sense of how salient the theme was in our dataset in order to facilitate application of our findings to program development. Data management and analysis was conducted in maxQDA software (30).
Results
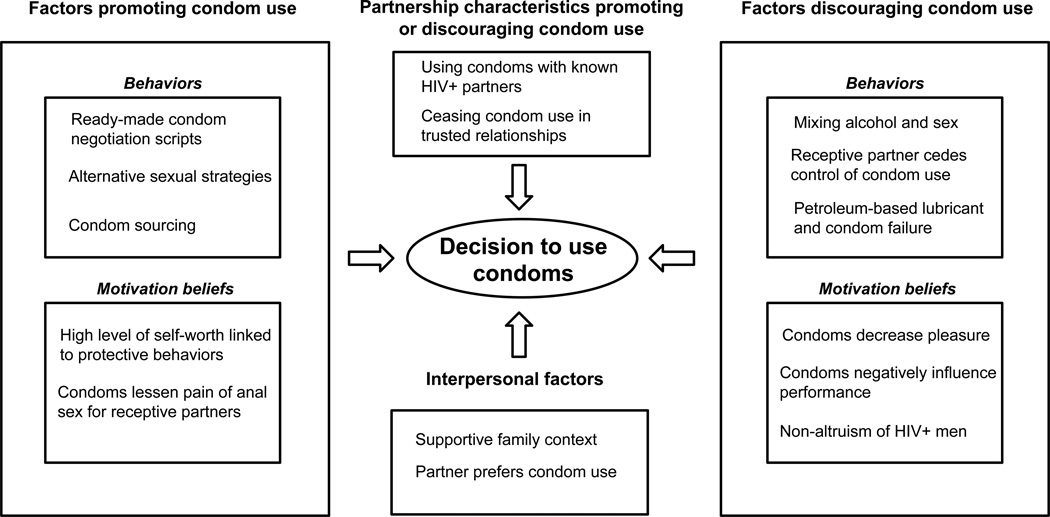
Descriptive analysis of demographics and other characteristics for 34 participants are detailed in Table 1. Based on our analysis of the qualitative data, the visual model of factors that influenced condom use decisions (Figure 1) had four principal domains: (1) factors promoting condom use, (2) factors discouraging condom use, (3) partnership characteristics promoting or discouraging condom use and (4) interpersonal factors. Within the first two domains, factors were found to fit into classification of either behaviors or motivational beliefs. Each model component is explored below, followed by assessment of how multiple factors coalesced within individuals to influence condom use. Demographic trend and differences between study sites, were assessed for each factor, and when present, are noted. We conclude with discussion of implications for HIV prevention interventions and future research.
Table 1.
Characteristics of 34 participants in Cape Town and Port Elizabeth, South Africa, 2012
| All | Cape Town | Port Elizabeth | |
|---|---|---|---|
| % (n) | % (n) | % (n) | |
| Total | (34) | (16) | (18) |
| Age | |||
| 18–25 | 50 (17) | 38 (6) | 61 (11) |
| 26–35 | 29 (10) | 25 (4) | 33 (6) |
| >35 | 21 (7) | 38 (6) | 6 (1) |
| Race | |||
| Black | 62 (21) | 50 (8) | 72 (13) |
| White | 18 (6) | 19 (3) | 17 (3) |
| Coloured | 21 (7) | 31 (5) | 11 (2) |
| Self-reported HIV Status | |||
| HIV Negative | 76 (26) | 81 (13) | 72 (13) |
| HIV Positive | 24 (8) | 19 (3) | 28 (5) |
| Level of educational attainment | |||
| Primary or less | 29 (10) | 25 (4) | 33 (6) |
| Secondary | 53 (18) | 50 (8) | 56 (10) |
| College or higher | 18 (6) | 25 (4) | 11 (2) |
| Current Employment Status | |||
| Unemployed | 47 (16) | 50 (8) | 44 (8) |
| Employed | 41 (14) | 44 (7) | 39 (7) |
| Student | 12 (4) | 6 (1) | 17 (3) |
| Current Relationship Status | |||
| Single | 15 (5) | 19 (3) | 11 (2) |
| Dating | 29 (10) | 38 (6) | 22 (4) |
| Monogamous partnership | 47 (16) | 44 (7) | 50 (9) |
| Married | 9 (3) | 0 | 17 (3) |
| Condom use with last anal sex partner | |||
| Always | 62 (18) | 57 (8) | 67 (10) |
| Sometimes | 3 (1) | 7 (1) | 0 |
| Never | 34 (10) | 36 (5) | 33 (5) |
Figure 1.
Visual model of qualitative data from 34 participants in Cape Town and Port Elizabeth, South Africa, 2012
Behaviors promoting condom use
Ready-made condom negotiation scripts
About one in four men applied prepared negotiation scripts to situations where they encountered barriers to condom use. The most common script was implemented with surprising homogeneity and brevity: “If there are no condoms, there’s no sex” (HIV-Black, CT, 19 years). This script not only served as an internal heuristic supporting condom use, but also an effective method of negotiating condom use. Men who mentioned this specific script were all consistent condom users. Another participant used a standard negotiation strategy to convince his sex partners to use condoms:
Each and every time I have sex with guys, the only thing [is], we always negotiate about sex … ‘Do we like condom? Do we like oral or what? Do we like bareback?’ If maybe he says ‘no I want bareback’, I say … ‘I don’t mind to do bareback, the only thing I’m not sure is our status. You don’t know me’. … And then I say ‘No, we can use condoms’ … (HIV-Black, CT, 33 years)
Alternative sexual strategies
In situations where men did not have access to condoms or their partner refused condoms, about one in eight men offered oral (most frequently) or other non-penetrative sexual alternatives. One man described coping with a partner who disliked condoms:
Once [we had anal], and we did use a condom, but he doesn’t feel comfortable so … [now I am] just on top, without penetration. I just come on top of him … or sometimes he sucks my cock. (HIV-Black, CT, 23 years)
Condom sourcing
Nearly one in four men had an expectation regarding which partner was responsible for providing condoms. This quarter was about evenly split between men who procured their own condoms and men who relied on their partner(s) to procure them. Of men who provided condoms, all described either regularly carrying condoms in their pocket or having a stock of condoms at home. For some men, the hosting household had responsibility to provide condoms, “I’m the one that always carry condoms because most of them, they used to come over to my place” (HIV+ Black, PE, 24 years).
Motivation beliefs promoting condom use
High level of self-worth linked to protective behavior
A few men, about one in ten, described positive internal valuations that were linked to self-protective logic and condom use. One participant, in a monogamous relationship, described protecting himself from HIV as “more relevant now because I’m older and I feel like I have more invested in my life. Like drunk driving, I shouldn’t be doing it” (HIV-Coloured, CT, 24 years). At times, men’s positive self-valuations were more directly tied to the threat posed by HIV:
It’s like, I can’t risk my life. I see people, look, this HIV, it’s not a game. No, this is not like football game … People die like it’s nobody’s business. And I take my life serious. I love life. (HIV-Black, CT, 23 years)
Condoms lessen pain of anal sex for receptive partners
A few primarily receptive condom users had positive beliefs regarding condoms, pleasure and anal sex. Specifically, about one in ten men believed that condoms made dealing with pain “much better … [otherwise] it’s dry … you get cuts” (HIV-Black, PE, 20 years). Men framed this discussion in terms of pain reduction, not mentioning the potential HIV prevention benefits of avoiding anal trauma. Decreased sensations of pain were often discussed in terms of the combination of condoms and lubricant as a unitary action. For one participant, avoiding pain was sufficient motivation to both initiate and continue consistent condom use. Another respondent described his first anal sex as so painful that he abstained for a year afterwards; only upon using condoms and lubricant did sex become pleasurable for him.
Behaviors discouraging condom use
Mixing alcohol and sex
Many men (one in three) mentioned having sex while intoxicated. Some of these men succeeded in using condoms despite alcohol use, generally by employing strategies discussed above, such as having a pre-specified expectation regarding which partner would procure condoms (condom sourcing). Yet most men mentioned alcohol, in tandem with other factors, as a reason for not having used condoms. For instance, one man explained, “I was drunk and … I had crush for almost a year. So, I got an opportunity to date him and … he had no condoms with him. So, we did it without a condom” (HIV+ Black, PE, 24 years). Another participant had a similar experience, “When we were like drinking … I would ask ‘Where you got the condoms’, and ‘Come on! I don’t have them.’ Then we’re like, ‘OK fine.’ And then we do it” (HIV-Black, PE, 24 years).
Receptive partner cedes control of condom use
Some men reported being consistently receptive for anal sex, usually across their partnerships. Being receptive was sometimes tied to power and decision-making dynamics, in which the decision to use condoms belonged to the insertive partners. One receptive man noted that he stopped trying to convince his insertive partners to use condoms, “because guys didn’t really want to use condoms” (HIV-Coloured, CT, 50 years). In another case, an insertive participant described taking advantage of his partner’s flexibility: condom use, “depend(s) on the mood for me … [my partner] said it’s fine, and that it’s up to me” (HIV-Black, PE, 26 years).
Petroleum-based lubricant and condom failure
Several men, about one in six, discussed problems with condoms “bursting”. One man described numerous experiences with condom failure. “So it happened 3 times … the 4th time I didn’t offer him a condom, because I asked him, ‘What’s the point?’” (HIV+ Black, PE, 24 years). All the men in our sample who discussed condom failure were from Port Elizabeth and also reported using petroleum-based lubricants, such as Vaseline. Use of lubricant not compatible with condoms appears to be the probable cause of frequent condom failure, as a few participants concluded. For instance, one participant described how he and his partner had switched away from petroleum lubricants to a water-based lubricant to avoid the problem of condom breakage (HIV-White, PE, 31 years).
Motivational beliefs discouraging condom use
Condoms decrease pleasure or negatively influence performance
In discussing condoms, one in three cited experiences with condoms negatively impacting sex. Most described the primary limitation as reduction of pleasure, noting that sex without condoms “feels better.” Instances where reduced pleasure was cited as a reason for condom non-use were more common among older than younger participants. Other problems with condom performance included inhibition of particular sexual desires, such as wanting to “come without a condom” (HIV-Coloured, CT, 44 years). When condoms were used, sexual performance issues concerned a few men, particularly regarding maintaining erection or reaching orgasm.
Non-altruism of some HIV+ Men
A minority of men living with HIV in our sample, all from the Port Elizabeth site, reported not using condoms with partners of unknown HIV serostatus. Port Elizabeth is an area with lower availability of services for MSM. Those who did not use condoms with partners of unknown serostatus separated themselves from the responsibility to prevent HIV transmission, asserting that protecting the health of other men was not their responsibility. One man explained, “Why should I bother and think for someone else’s child?” (HIV+ Black, PE, 28 years). This group of men had largely uniform stances regarding disclosure, perceiving a norm of silence surrounding HIV and sex:
I’m reckless … No one knows my status except [name] … in this continent, the issue of one’s status isn’t an issue. When I go to bed with a person, very seldom that you talk about condom use or that you talk about HIV status. It’s as if it doesn’t exist … over the past 10 years, there may be only 3 or 4 people who ask for a condom. (HIV+ Black, PE, 60 years)
Partnership characteristics promoting or discouraging condom use
Condom use in known HIV serodiscordant relationships
About one in eight men in our sample were HIV negative and aware of a partner’s HIV positive serostatus. All of these men discussed using condoms when involved in these serodiscordant relationships: “When I went for HIV test, and I was negative, and [name] was positive … from there on I started using condoms” (HIV-Coloured, CT, 44 years). Yet men who practiced this protective strategy often reported unprotected anal sex with other partners whose HIV status they did not know. For these men, confirmation of HIV-positive serostatus was the only factor sufficiently motivating to encourage consistent condom use.
Ceasing condom use in trusted relationships
About half of participants indicated, without prior prompting, that trusted relationships merited condom-free sex. Most described trust as a facet of either being in a monogamous relationship or having known their partner for a long period of time. The majority of men in trusted relationships, however, either demanded or yielded to their partner’s demands unprotected sex despite the lack of up to date HIV tests. A few mentioned HIV testing, either together (couples testing) or at different times, using discussion of HIV test results as a component of trust-building. In contrast, a number of men described how lack of trust/familiarity in their relationship was a motivation for condom use, “Sometimes if I didn’t see [name] all week. … then I wanted to use condoms because I don’t know what he is doing when I don’t see him” (HIV-Black, CT, 26 years). Another man noted, “It was the first time I had seen (this partner) around, so I suggested the condom” (HIV-Black, PE, 22 years).
Interpersonal factors
Supportive family context
Some participants, about one in four, described their family as a source of encouragement and support to use condoms. For about half of these men, family encouragement of condom use was tied to the disclosure of their sexuality. One participant described such an interaction with his father, “He said that it’s OK if I’m gay. I must just use a condom.” (HIV-White, PE, 30 years) For the other half, familial support was unrelated to disclosure of their sexuality. In one typical case, an older brother showed his younger sibling how to use condoms, and then gave him a stock of condoms for future use (HIV-Black, PE, 24 years).
Partner prefers condom use
About one in three men described a partner’s preference in favor of condom use as having a direct bearing on their condom decisions. Partner’s preference held surprising sway; in the entire sample, no men mentioned refusing sex due to a partner’s insistence on condom use, no matter how negative their beliefs were regarding condoms. Moreover, a number of men who reported using condoms inconsistently ascribed this to a specific partner’s demand for condoms. For instance, one man explained never using condoms except with a particular sexual partner because, “(he) insists that we must use condoms!” (HIV+ Black, CT, 43 years). Another participant described his condom usage as, “on very rare occasions”, and then proceeded to clarify, “that’s an issue that never came from me!” (HIV+ Black, PE, 60 years)
Three men in the sample received money and other goods in exchange for sex. Two of these men reported consistent condom use, refusing to have sex with clients who did not want to use condoms. One sex worker, however, was unable to negotiate condom use:
I am not OK with [not using condoms] … When [the client] is going to say ‘I don’t have a condom’ [or] ‘I know my status. I’m not HIV positive’. You can’t talk, just you keep quiet and you do your job. (HIV-Black, CT, 25 years)
Findings unified across model domains
Participants experienced difficulty in explaining inconsistent condom use
Nearly one in seven men expressed a lack of understanding why they did not use condoms in particular situations. One respondent, typical of this group, was asked about why hed described using condoms is some situations and not others, and replied, “Honestly, I don’t know. It just happen, like, we don’t use a condom” (HIV+ Black, PE, 24 years). Another explained that, even within a given night, condom use might be inexplicably inconsistent: “I can’t really tell you … because even if, let’s say if we are doing a first round, we use a condom. And then the second and the third round, we don’t use it” (HIV-Black, PE, 22 years).
Conceptual model factors coalesce to influence condom use
When discussing previous use or non-use of condoms, about one in four men had a single factor dominated their decision-making, while other men navigated multiple factors. The main single factors related to decision-making were (1) perceiving that condoms substantially reduce pleasure and (2) being an HIV uninfected man with a partner living with HIV. Yet most men discussed multiple factors weighing on their decisions. One participant’s experience encompassed factors of (a) alcohol intake and sex, (b) condoms not systematically sourced, (c) pressure to not use condoms in trusted relationships and (d) prepared negotiation scripts.
I remember my boyfriend was drunk one time so he came to my flat … Then he asked me to have sex with him. Then I said, 'No, its fine, where is the condom?' He said he did not have a condom. 'Come on [name]! Come on [name]! … I am your boyfriend. How can you not trust me?' So he got angry. Then I said ‘If there’s no condom, then no sex.’ (HIV-Black, PE, 20 years)
This experience encompassed several factors that led some participants in our sample to have unprotected sex. Yet, like other men in the sample with the requisite negotiation skills and determination, this individual successfully negotiated condom use despite the challenges.
Discussion
Using a grounded theory approach, we found that condom use among MSM in two urban centers of South Africa was a function of behaviors, motivational beliefs, partnership characteristics, and interpersonal factors. Each component of our model has implications for the design of public health programs in South Africa. It is particularly important to develop tailored HIV prevention approaches for MSM in this setting, given that other research has found correlations between exposure to MSM-specific programming and decreased UAI (12, 23–25, 31).
Previous research in South Africa has demonstrated that MSM with lower scores on condom self-efficacy scales are more likely to have unprotected anal sex (15). Results from the current study underscore the importance of components of self-efficacy scales, such as condom negotiation skills and confidence in being able to use condoms consistently. What this study adds is detail and richness on how to enact programs to best address self-efficacy. For instance, many factors found to promote condom use among this sample of MSM could be viewed as instances of positive deviance, where individuals implement uncommon strategies, allowing them to solve problems better than peers facing similar environments (32). Because positive deviance solutions are community-derived, they have advantages of being culturally-appropriate and sustainable. Behaviors such as the use of condom negotiation scripts, alternative sexual strategies and condom sourcing arrangements are positive deviance subsets of self-efficacy that seem to be important to how South African MSM decide to negotiate condom use.
Interventions may benefit from helping men to develop scripts similar to those successfully employed by their peers, such as the simple but widely-cited “No condom, no sex” script. Such a script might also be useful for social marketing purposes. Programs that aim to promote self-efficacy might add components regarding negotiation of alternative sexual strategies if condoms are not desired by a partner, and how to arrange for condom sourcing with partners, based on strategies identified in our results. In particular, such skills could be incorporated into voluntary counseling and testing (VCT) or couples voluntary counseling and testing (CVCT) sessions. Motivational beliefs, such as a high level of self-worth linked to HIV prevention behaviors, can be used to bolster these behavioral strategies.
In assessing the occurrence of themes regarding condom use, we found little evidence of patterns by demographics we recorded, such as race, age and HIV status. The lone trend we identified was that older men more frequently discussed problems with condoms reducing pleasure. Yet previous research has not found age to be associated with rates of unprotected anal sex (14, 33). Nonetheless, future research into condom problems experienced by older MSM may be warranted.
Perceptions regarding condoms and reduced pleasure seem well-situated for future intervention. For instance, negative beliefs about condoms and pleasure might be addressed by programming that eroticizes condoms and condom compatible lubricants by highlighting their ability to increase comfort for receptive partners. Additionally, development of new kinds of condoms through innovating materials, shapes and/or sizes may be useful in addressing concerns regarding condom pleasure and the impact on sexual performance.
Previous research has established that trusted partnerships are associated with unprotected anal sex (13, 14), termed by one paper a “fallacy of intimacy”, which is similar to our findings regarding avoidance of condoms with trusted partners. Authors of one of these studies (13) called for further exploration of trust and condom use. Our data indicate a wide diversity of trust interpretations and resulting protective actions for different couples. Some couples developed trust in a partnership and sought joint HIV testing, whereas other couples identified trust as a more fluid mix of physical proximity, emotional closeness and familiarity. For these couples, HIV prevention strategies were often less defined, with less discussion of HIV testing. For both couple types, unprotected sex was common. Yet mathematical modeling estimates indicate that main partners may account for as much as two-thirds of HIV transmission among US MSM (17), effectively debunking the assumption that sex with any regular and trusted partner is safe and does not require condoms. Future programming should assess the best ways to communicate to MSM couples the results of such modeling studies, and how to link that information to HIV risk reduction plans.
Couples HIV risk reduction discussions, and the requisite testing and disclosure of HIV serostatus, are important areas for future intervention and research. In our model, serostatus discussion or assumed partner serostatus impacted several themes: condom use with known HIV+ serostatus partners, non-altruism of HIV+ serostatus men, and ceasing condom use in trusted relationships. Across these themes, discussion of serostatus usually led to safer actions such as condom use or joint testing, whereas silence regarding serostatus more often led to unprotected sex. Future research is needed to further explore serostatus discussions, particularly in how stigma in low-service access areas such as Port Elizabeth may impact such discussion. Research into discussion of serostatus and risk reduction is particularly timely given the increasing availability of HIV prevention strategies such as MSM-tailored CVCT (34) and pre- and post-exposure chemoprophylaxis (PrEP and nPEP) (35–38) that should be considered in such discussions.
Some interpersonal factors, such as the composition of MSM wider social/economic networks, are difficult to shift with existing interventions. It is, however, encouraging that some men in our sample successfully negotiated condom use despite barriers such as power dynamics associated with sex work or unwilling partners. It is also notable, and perhaps an important message to provide to MSM, that no instances were reported where sex was refused due to a participant’s (or his partner’s) insistence on condom use. Simply put, men in this study did not report turning down sex or sexual alternatives when a partner insisted on safe sex. In contrast to other studies that indicated MSM frequently hold negative attitudes towards condoms (39–41), men who demanded safe sex rarely reported such negative attitudes from their partners. This finding indicates initial support for social marketing campaigns that promote protective relationships and condom use for MSM, such as the “I love my Boo” campaign in the United States (42), a strategy that might be applicable in South Africa based on our data regarding the importance of relationships in condom use decisions.
This study has several limitations. The sample was recruited through CBO and contacts of MSM in two areas of South Africa, possibly giving additional emphasis to certain groups. For example, younger men comprised the majority of the sample. Of particular concern is that we may not have included men who do not access HIV prevention programs. For instance, of the 34 men interviewed for the study, only one reported currently having sex with women. MSM who are more hidden from such programs, or who are not well networked, may have substantially different knowledge, perceptions and life experiences related to condom use during anal sex that could yield useful information. A further study limitation, albeit an expected one, is that men focused on proximal factors when discussing their experiences. Environmental exposures, such as access to HIV prevention programs, social network factors, or experienced stigma, likely feed into the proximal components influencing condom use identified in our model, and our data did not allow for a full exploration of these relationships.
In conclusion, this qualitative study of MSM in two communities in South Africa presents a framework of factors influencing condom use decision-making. Future research should seek to incorporate a more formal understanding of the context of condom use into development of culturally-appropriate behavioral interventions. Future HIV prevention programs may benefit from directly targeting key factors that influence condom use, allowing for development of more nuanced and effective HIV prevention messages.
Acknowledgments
Funding
This study was supported by the National Institute of Allergy and Infectious Diseases, R01AI094575, and was facilitated by the Emory Center for AIDS Research, P30AI050409. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The authors have no conflicts of interest to disclose.
References
- 1.Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000–2006: a systematic review. PLoS Med. 2007 Dec;4(12):e339. doi: 10.1371/journal.pmed.0040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baggaley RF, White RG, Boily MC. HIV transmission risk through anal intercourse: systematic review, meta-analysis and implications for HIV prevention. International journal of epidemiology. 2010 Aug;39(4):1048–1063. doi: 10.1093/ije/dyq057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012 Jul 28;380(9839):367–377. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sullivan PS, Carballo-Dieguez A, Coates T, Goodreau SM, McGowan I, Sanders EJ, et al. Successes and challenges of HIV prevention in men who have sex with men. Lancet. 2012 Jul 28;380(9839):388–399. doi: 10.1016/S0140-6736(12)60955-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, et al. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane database of systematic reviews (Online) 2008;3 doi: 10.1002/14651858.CD001230.pub2. CD001230. [DOI] [PubMed] [Google Scholar]
- 6.Smith AD, Tapsoba P, Peshu N, Sanders EJ, Jaffe HW. Men who have sex with men and HIV/AIDS in sub-Saharan Africa. Lancet. 2009 Aug 1;374(9687):416–422. doi: 10.1016/S0140-6736(09)61118-1. [DOI] [PubMed] [Google Scholar]
- 7.Rispel LC, Metcalf CA. Breaking the silence: South African HIV policies and the needs of men who have sex with men. Reproductive health matters. 2009 May;17(33):133–142. doi: 10.1016/S0968-8080(09)33442-4. [DOI] [PubMed] [Google Scholar]
- 8.Lane T, Raymond HF, Dladla S, Rasethe J, Struthers H, McFarland W, et al. High HIV prevalence among men who have sex with men in Soweto, South Africa: results from the Soweto Men's Study. AIDS Behav. 2011 Apr;15(3):626–634. doi: 10.1007/s10461-009-9598-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rispel LC, Metcalf CA, Cloete A, Reddy V, Lombard C. HIV prevalence and risk practices among men who have sex with men in two South African cities. J Acquir Immune Defic Syndr. 2011 May;57(1):69–76. doi: 10.1097/QAI.0b013e318211b40a. [DOI] [PubMed] [Google Scholar]
- 10.Baral S, Burrell E, Scheibe A, Brown B, Beyrer C, Bekker LG. HIV risk and associations of HIV infection among men who have sex with men in peri-urban Cape Town, South Africa. BMC Public Health. 2011;11:766. doi: 10.1186/1471-2458-11-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.South African National AIDS Council. Global AIDS Response and Progress Report 2012. The Republic of South Africa. 2012 [Google Scholar]
- 12.Lane T, Shade SB, McIntyre J, Morin SF. Alcohol and sexual risk behavior among men who have sex with men in South african township communities. AIDS Behav. 2008 Jul;12(4 Suppl):S78–S85. doi: 10.1007/s10461-008-9389-x. [DOI] [PubMed] [Google Scholar]
- 13.Knox J, Yi H, Reddy V, Maimane S, Sandfort T. The fallacy of intimacy: sexual risk behaviour and beliefs about trust and condom use among men who have sex with men in South Africa. Psychol Health Med. 2010 Dec;15(6):660–671. doi: 10.1080/13548506.2010.507772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sandfort T, Yi H, Knox J, Reddy V. Sexual partnership types as determinant of HIV risk in South African MSM: an event-level cluster analysis. AIDS Behav. 2013 May;17(Suppl 1):S23–S32. doi: 10.1007/s10461-012-0294-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tucker A, Liht J, de Swardt G, Jobson G, Rebe K, McIntyre J, et al. Homophobic stigma, depression, self-efficacy and unprotected anal intercourse for peri-urban township men who have sex with men in Cape Town, South Africa: a cross-sectional association model. AIDS Care. 2013 Dec 2; doi: 10.1080/09540121.2013.859652. [DOI] [PubMed] [Google Scholar]
- 16.Goodreau SM, Carnegie NB, Vittinghoff E, Lama JR, Sanchez J, Grinsztejn B, et al. What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PLoS One. 2012;7(11):e50522. doi: 10.1371/journal.pone.0050522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009 Jun 1;23(9):1153–1162. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- 18.Bedoya CA, Mimiaga MJ, Beauchamp G, Donnell D, Mayer KH, Safren SA. Predictors of HIV transmission risk behavior and seroconversion among Latino men who have sex with men in Project EXPLORE. AIDS Behav. 2012 Apr;16(3):608–617. doi: 10.1007/s10461-011-9911-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Csepe P, Amirkhanian YA, Kelly JA, McAuliffe TL, Mocsonoki L. HIV risk behaviour among gay and bisexual men in Budapest, Hungary. International journal of STD & AIDS. 2002 Mar;13(3):192–200. doi: 10.1258/0956462021924785. [DOI] [PubMed] [Google Scholar]
- 20.Ko NY, Lee HC, Hung CC, Chang JL, Lee NY, Chang CM, et al. Effects of structural intervention on increasing condom availability and reducing risky sexual behaviours in gay bathhouse attendees. AIDS Care. 2009 Dec;21(12):1499–1507. doi: 10.1080/09540120902923022. [DOI] [PubMed] [Google Scholar]
- 21.Tang W, Huan X, Mahapatra T, Tang S, Li J, Yan H, et al. Factors Associated with Unprotected Anal Intercourse Among Men Who Have Sex with Men: Results from a Respondent Driven Sampling Survey in Nanjing, China, 2008. AIDS Behav. 2013 Jan 20; doi: 10.1007/s10461-013-0413-4. [DOI] [PubMed] [Google Scholar]
- 22.Batist E, Brown B, Scheibe A, Baral SD, Bekker LG. Outcomes of a community-based HIV-prevention pilot programme for township men who have sex with men in Cape Town, South Africa. J Int AIDS Soc. 2013;16(Suppl 3):18754. doi: 10.7448/IAS.16.4.18754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geibel S, Luchters S, King'Ola N, Esu-Williams E, Rinyiru A, Tun W. Factors associated with self-reported unprotected anal sex among male sex workers in Mombasa, Kenya. Sex Transm Dis. 2008 Aug;35(8):746–752. doi: 10.1097/OLQ.0b013e318170589d. [DOI] [PubMed] [Google Scholar]
- 24.Larmarange J, Wade AS, Diop AK, Diop O, Gueye K, Marra A, et al. Men who have sex with men (MSM) and factors associated with not using a condom at last sexual intercourse with a man and with a woman in Senegal. PLoS One. 2010;5(10) doi: 10.1371/journal.pone.0013189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baral S, Adams D, Lebona J, Kaibe B, Letsie P, Tshehlo R, et al. A cross-sectional assessment of population demographics, HIV risks and human rights contexts among men who have sex with men in Lesotho. J Int AIDS Soc. 2011;14:36. doi: 10.1186/1758-2652-14-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marsh DR, Schroeder DG, Dearden KA, Sternin J, Sternin M. The power of positive deviance. In: Clinical research, editor. BMJ. 7475. Vol. 329. 2004. Nov 13, pp. 1177–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patton MQ. Qualitative Research & Evaluation Methods. 3 ed. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 28.Charmaz K. In: Constructing grounded theory: A practical guide through qualitative analysis. 1st ed. Silverman D, editor. London: SAGE Publications; p. 208. [Google Scholar]
- 29.Strauss AL, Corbin JM. Basics of qualitative research : techniques and procedures for developing grounded theory. 2nd ed. Thousand Oaks: Sage Publications; 1998. p. xiii.p. 312. [Google Scholar]
- 30.maxQDA. Software for qualitative data analysis. 10 ed. Berlin: VERBI Software; 2012. [Google Scholar]
- 31.Henry E, Marcellin F, Yomb Y, Fugon L, Nemande S, Gueboguo C, et al. Factors associated with unprotected anal intercourse among men who have sex with men in Douala, Cameroon. Sex Transm Infect. 2010 Apr;86(2):136–40. doi: 10.1136/sti.2009.036939. [DOI] [PubMed] [Google Scholar]
- 32.Walker LO, Sterling BS, Hoke MM, Dearden KA. Applying the concept of positive deviance to public health data: a tool for reducing health disparities. Public health nursing (Boston, Mass) 2007 Nov-Dec;(6):571–576. doi: 10.1111/j.1525-1446.2007.00670.x. [DOI] [PubMed] [Google Scholar]
- 33.Arnold EA, Hazelton P, Lane T, Christopoulos KA, Galindo GR, Steward WT, et al. A Qualitative Study of Provider Thoughts on Implementing Pre-Exposure Prophylaxis (PrEP) in Clinical Settings to Prevent HIV Infection. PLoS One. 2012;7(7):e40603. doi: 10.1371/journal.pone.0040603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stephenson R, Rentsch C, Sullivan P, McAdams-Mahmoud A, Jobson G, Struthers H, et al. Attitudes Toward Couples-Based HIV Counseling and Testing Among MSM in Cape Town, South Africa. AIDS Behav. 2013 May;17(Suppl 1):43–50. doi: 10.1007/s10461-012-0293-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abdool Karim Q, Abdool Karim SS, Frohlich JA, Grobler AC, Baxter C, Mansoor LE, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science (New York, NY) 2010 Sep 3;329(5996):1168–1174. doi: 10.1126/science.1193748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eakle R, Venter WD, Rees H. Pre-exposure prophylaxis for HIV prevention: ready for prime time in South Africa? South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 2013 Aug;103(8):515–516. doi: 10.7196/samj.6937. [DOI] [PubMed] [Google Scholar]
- 37.Alistar SS, Grant PM, Bendavid E. Comparative effectiveness and cost-effectiveness of antiretroviral therapy and pre-exposure prophylaxis for HIV prevention in South Africa. BMC medicine. 2014;12:46. doi: 10.1186/1741-7015-12-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van der Straten A, Stadler J, Montgomery E, Hartmann M, Magazi B, Mathebula F, et al. Women's Experiences with Oral and Vaginal Pre-Exposure Prophylaxis: The VOICE-C Qualitative Study in Johannesburg, South Africa. PLoS One. 2014;9(2):e89118. doi: 10.1371/journal.pone.0089118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Calabrese SK, Reisen CA, Zea MC, Poppen PJ, Bianchi FT. The pleasure principle: the effect of perceived pleasure loss associated with condoms on unprotected anal intercourse among immigrant Latino men who have sex with men. AIDS Patient Care STDS. 2012 Jul;26(7):430–435. doi: 10.1089/apc.2011.0428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carballo-Dieguez A, Ventuneac A, Dowsett GW, Balan I, Bauermeister J, Remien RH, et al. Sexual pleasure and intimacy among men who engage in "bareback sex". AIDS Behav. 2011 Apr;15(Suppl 1):S57–S65. doi: 10.1007/s10461-011-9900-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scott-Sheldon LA, Marsh KL, Johnson BT, Glasford DE. Condoms + pleasure = safer sex? A missing addend in the safer sex message. AIDS Care. 2006 Oct;18(7):750–754. doi: 10.1080/09540120500411073. [DOI] [PubMed] [Google Scholar]
- 42.Gay Men's Health Crisis (GMHC) [Accessed August 28 2013];I love my boo. http://www.gmhc.org/i-love-my-boo-4. [Google Scholar]