Abstract
Context
Total Knee Arthroplasty (TKA) is one of the most common and costly surgical procedures performed in the United States (U.S.).
Objective
To examine longitudinal trends in volume, utilization and outcomes for primary and revision TKA between 1991 and 2010 in the U.S. Medicare population.
Design, Setting, and Participants
Observational cohort of 3,271,851 patients who underwent primary TKA and 318,563 who underwent revision TKA identified in Medicare Part A data files.
Outcomes
We examined changes in primary and revision TKA volume, per-capita utilization, hospital length of stay (LOS), readmission rates, and adverse outcomes.
Results
Between 1991 and 2010 annual primary TKA volume increased 161.5% from 93,230 to 226,177 while per-capita utilization increased 99.2%. Revision TKA volume increased 105.9% from 9,650 to 19,871 while utilization increased 56.8%. For primary TKA, LOS decreased from 7.9 days (95% CI, 7.8–7.9) in 1991–1994 to 3.5 days (95% CI, 3.5-3.5) in 2007–2010 (P< 0.001). For primary TKA rates of adverse outcomes resulting in readmission remained stable between 1991–2010, but rates of all-cause 30-day readmission increased from 4.2% (95% CI, 4.1–4.2) to 5.0% (95% CI, 4.9–5.0) (P<0.001). For revision TKA, the decline in hospital LOS was accompanied by an increase in 30-day readmission from 6.1% (95% CI, 5.9–6.4) to 8.9% (95% CI, 8.7–9.2) (P<.001) and an increase in wound infection rates from 1.4% (95% CI, 1.3–1.5) to 3.0% (95% CI, 2.9–3.1) (P<.001).
Conclusions
Increases in TKA volume have largely been driven by increases in per-capita utilization. We also observed decreases in hospital LOS that were accompanied by increases in hospital readmission rates.
BACKGROUND
Total knee arthroplasty (TKA) is a common and safe procedure typically performed for relief of symptoms in patients with severe knee arthritis. Available data suggest that there are approximately 500,000 TKA procedures performed annually in the United States (U.S.) at a cost of approximately $20,000 per procedure ($10 billion per-year in aggregate).1–4 While TKA does not typically reduce mortality, the procedure results in marked improvements in health related quality of life and functional status and is highly cost-effective.2,5 TKA is now among the most common major surgical procedures performed in the U.S.6
The growth in TKA can certainly be viewed as an indication of the success of this procedure in safely reducing pain and improving functional status for an aging population.7,8 Alternatively, the growth in TKA can also be viewed as yet another source of strain on government, insurers, individuals, and businesses struggling with unremitting growth in healthcare spending.9–11 Despite the clinical and economic policy importance of TKA, there are few analyses evaluating recent trends over time in use of and outcomes associated with TKA.1,12–14
Thus, the objective our study was to comprehensively evaluate longitudinal trends in primary and revision TKA volume, per-capita utilization, and outcomes in the U.S. Medicare population.
METHODS
Data
We linked two sequential Medicare Provider Analysis and Review (MedPAR) Part A data files (one running from 1991–2005 and a second from 2006–2010) each containing a 100% sample of hospitalizations for fee-for-service beneficiaries. These data were used to identify all enrollees age 65 years and older who underwent primary or revision TKA between 1991 and 2010. Patients were identified using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD9-CM) procedure codes (81.54 for primary and 80.06, 81.55, 00.80, 00.81, 00.82, 00.83, 00.84 for revision TKA).15–18 The Part A files contain a range of data collected from discharge abstracts for all hospitalized fee-for-service Medicare enrollees including: patient demographics; ICD9-CM codes for primary and secondary diagnoses and procedures; admission source (e.g., emergency department or transfer from outside hospital); admission and discharge dates; discharge disposition (e.g., home, nursing home, inpatient rehabilitation, transfer to another acute-care hospital, dead); death occurring up to three years after discharge; each patient’s unique Medicare beneficiary number allowing for identification of patient readmissions; and each hospital’s unique six digit identification number. Comorbid illnesses present on the index admission were identified using algorithms described by Elixhauser et al.19,20 which consider 30 specific conditions and exclude comorbid conditions that may represent complications of care or that are related to the primary reason for hospitalization. This project was approved by the University of Iowa Institutional Review Board. The sponsors had no role in the design and conduct of the study; in the collection, analysis, and interpretation of data; in the preparation of the manuscript; or in the review or approval of the manuscript.
Our intention was to examine changes in volume, utilization and outcomes of patients undergoing primary and revision TKA procedures. In order to generate appropriate analytical cohorts we applied several inclusion and exclusion criteria (See Web Appendix Figures A and B). First, we excluded Medicare HMO enrollees as the MedPAR data is incomplete for enrollees in such plans. Second, we limited our cohort to the first primary (or revision) TKA performed on a given patient during any 30-day period using methods we have described previously.21 We also excluded bilateral or “staged” procedures that occurred within the 30-day window; this exclusion is necessary because Medicare data historically has not included “sidedness” for a specific procedure; thus, for a patient who underwent two primary TKA procedures in close temporal proximity, it is impossible to know if this represented an initial primary followed by an early complication requiring a second procedure or a planned bilateral (aka, staged) procedure. Third, as primary TKA is most often an elective procedure while revision TKA can be either an elective or more urgent procedure, we applied separate exclusion criteria to the primary and revision TKA populations in accordance with prior studies as described below. For primary TKA we sequentially excluded patients admitted through the emergency department (N=18947), and patients admitted after transfer from another acute-care hospital (N=3295); these exclusion criteria were developed to select a population of primary elective TKA patients. Our revision TKA population did not exclude these types of patients because revision TKA can be an emergent or unscheduled procedure and thus exclusion of these populations would not make sense.
Statistical Analysis
We examined the demographic characteristics and prevalence of key comorbid illnesses for patients who underwent TKA between 1991 and 2010; for simplicity, data are presented separately for each four-year period (e.g., 1991–94, 1995–98, etc). We examined changes in the mean number of comorbid illnesses per-patient during each four-year period. We used analysis of variance for comparisons of continuous variables and the chi-squared test for categorical variables and tested for differences in linear trends. All analyses were performed separately for primary and revision TKA patients.
We used graphical methods to plot the annual primary and revision TKA Medicare volume over time. We calculated per-capita TKA utilization rates by dividing the number of procedures performed each year by the number of beneficiaries enrolled in the fee-for-service Medicare program and plotted these results graphically.
We compared linear trends in several important outcomes of interest for primary and revision TKA: 1) hospital length-of-stay (LOS); 2) discharge disposition; 3) selected arthroplasty complications resulting in readmission within 30-days of discharge; and 4) all-cause readmission rates within 30-days of discharge. Discharge disposition was categorized as home, skilled or intermediate care (which also incorporates outpatient rehabilitation), inpatient rehabilitation, and other. We examined changes in the rates of six separate adverse outcomes resulting in hospital admission within 30-days of discharge (mortality, pulmonary embolism, deep vein thrombosis (DVT), wound infection, post-operative sepsis, and myocardial infarction) that have been examined in prior studies of arthroplasty using administrative data.7,18,22
We also examined changes in rates of a composite outcome representing the occurrence of one-or-more of the individual adverse outcomes as well as all-cause readmission within 30-days of discharge. In order to evaluate the causes of readmission among the primary and revision TKA cohorts, we applied the Agency for Healthcare Research and Quality (AHRQ) Clinical Classification Software (CCS).23 This software synthesizes more than 14,000 ICD9-CM codes into 231 mutually exclusive clinically meaningful disease categories. For each four-year study period we examined the five most common categories associated with readmission and the proportion of all readmissions during each period that were associated with each category; this allowed us to examine how the causes of readmission have changed over time.
We used standard logistic regression to calculate risk-adjusted 30-day readmission rates and composite outcome (o/e * unadjusted 20-year rate), and used standard linear regression to calculate risk-adjusted hospital LOS (o−e + unadjusted 20-year LOS).24 These models adjusted for age (categorized as 65–69, 70–74, 75–79, and 80 and older), sex, race (categorized as white, black and other), and comorbidities to account for the changing demographics of the TKA populations over time.25 Race was included in these models to allow us to account for previously documented racial disparities in joint arthroplasty when calculating standardized utilization rates for our analysis.26,27 We used graphical methods to plot discharge disposition, hospital LOS, readmission rates, and composite outcome between 1991 and 2010. Again, all analyses were conducted separately for the primary and revision TKA cohorts.
We conducted several supplemental analyses of interest. Focusing on the most recent four-years of data (2007–2010), we examined the relationship between patient and hospital factors and hospital readmission; as in prior analyses, primary and revision TKA were examined separately. We used bivariate methods to compare differences in patient and hospital factors among patients who were and were not readmitted. We then examined both patient-level and hospital-level factors which may have affected the 30-day readmission rate by employing a series of four standard logistic regression models that progressively adjusted for an increasing array of factors. In all models, the dependent variable was a binary variable with the value of 1 if the patient had been readmitted, and 0 otherwise. Model I, adjusted for patient demographics alone (i.e., age, race, sex); model II added adjustment for the number of comorbidities; model III added adjustment for hospital teaching status (major, minor, and non-teaching) and hospital procedural volume (calculated separately for the primary and revision TKA cohort and categorized by hospital volume quartiles); model IV added additional adjustment for each patient’s hospital length-of-stay, modeled in its log-transformed state. In all four models, to control for any temporal changes, we also included calendar year (2007, 2008, 2009 and 2010).
We conducted an array of sensitivity analyses. In particular, we repeated our analyses after adding back excluded populations (e.g., primary TKA cases admitted through the emergency department). We also repeated our analyses looking at 90-day outcomes rather than 30-day outcomes. All p-values are 2-tailed, with p-values less 0.05 deemed statistically significant. All statistical analyses were performed using SAS 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
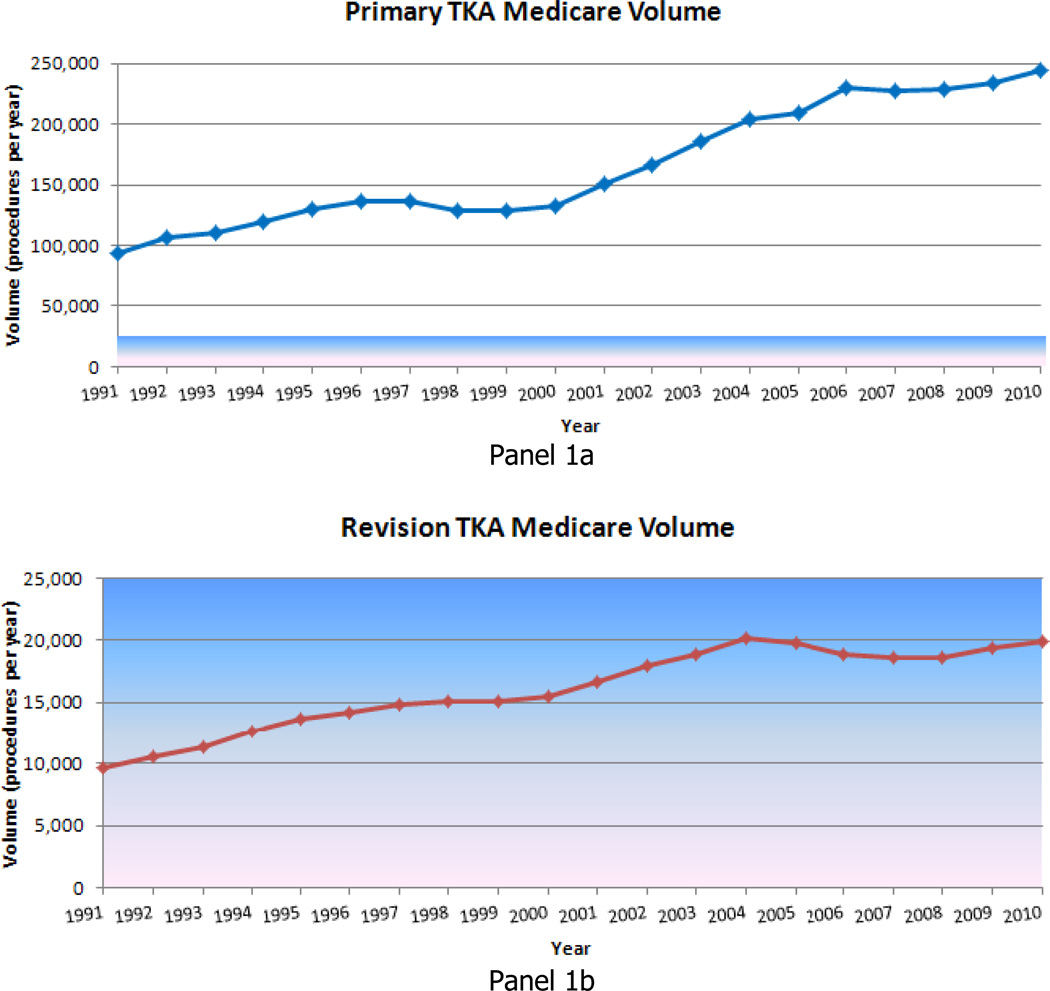
Our final study population included 3,271,851 elective primary TKAs and 318,563 revision TKAs between 1991 and 2010. The total number of fee-for-service Medicare enrollees increased from 29,892,351 in 1991 to 39,250,746 in 2010 while the number of primary TKA procedures increased from 93,230 in 1991 to 243,802 in 2010 (an increase of 161.5%)(Figure 1a). The number of revision TKA procedures increased from 9,650 in 1991 to 19,871 in 2010 (an increase of 105.9%)(Figure 1b).
Figure 1.
Primary (panel 1a) and revision (panel 1b) TKA Medicare Volume between 1991 and 2010
During the same period, the per-capita utilization of primary TKA increased by 99.2% (Figure 2a) and the utilization of revision TKA increased by 56.8% (Figure 2b). For primary TKA (Table 1) mean (standard deviation [SD]) age increased from 73.8 (5.8) years (95% confidence interval [CI], 73.8–73.8) in 1991–1994 to 74.2(6.2) years (95% CI, 74.2–74.2) in 2007–2010 (P=0.56); the prevalence of diabetes increased from 10.5% (95% CI, 10.4–10.6) to 21.7% (95% CI, 21.6–21.7); and the prevalence of obesity increased from 4.0% (95% CI, 3.9–4.0) to 11.5% (95% CI, 11.4–11.6) (P< 0.001 for each). Trends were similar for revision TKA (Table 2). In particular, mean age increased from 74.2 (5.9) years (95% CI, 74.1–74.3) in 1991–1994 to 74.8 (6.5) years (95% CI, 74.7–74.8) in 2007–2010 (P=0.46); the prevalence of diabetes increased from 11.0% (95% CI, 10.7–11.3) to 24.2% (95% CI, 23.9–24.5); and the prevalence of obesity increased from 3.7% (95% CI, 3.5–3.8) to 10.1% (95% CI, 9.9–10.3) (P< 0.001 for each).
Figure 2.
Primary (panel 2a) and revision (panel 2b) Medicare TKA Utilization between 1991 and 2010
Error bars indicate 95% confidence interval.
Table 1.
Characteristics of Medicare beneficiaries receiving primary and revision TKA between 1991 and 2010
| Primary TKA | Revision TKA | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1991–1994 | 1995–1998 | 1999–2002 | 2003–2006 | 2007–2010 | 1991–1994 | 1995–1998 | 1999–2002 | 2003–2006 | 2007–2010 | |
| Characteristics | ||||||||||
| No. of hospitalizations | 431050 | 530128 | 578614 | 816497 | 915562 | 44120 | 57785 | 65197 | 76526 | 74935 |
| Age, mean(SD), y | 73.8 (5.8) | 74.5 (5.9) | 74.7 (5.9) | 74.7 (5.9) | 74.2 (6.2) | 74.2 (5.9) | 75.2 (6.1) | 75.4 (6.2) | 75.3 (6.3) | 74.8 (6.5) |
| Sex, female | 283353 (65.7) | 346827 (65.4) | 379650 (65.6) | 535181 (65.5) | 592777 (64.7) | 26772 (60.7) | 35062 (60.7) | 38948 (59.7) | 44654 (58.4) | 43535 (58.1) |
| Race | ||||||||||
| White | 389996 (90.5) | 487200 (91.9) | 529078 (91.4) | 744882 (91.2) | 831082 (90.8) | 39850 (90.3) | 52787 (91.4) | 58781 (90.2) | 68770 (89.9) | 66981 (89.4) |
| Black | 21515 (5.0) | 28685 (5.4) | 30563 (5.3) | 42442 (5.2) | 49477 (5.4) | 2531 (5.7) | 3704 (6.4) | 4606 (7.1) | 5413 (7.1) | 5581 (7.4) |
| Other | 7376 (1.7) | 10774 (2.0) | 16654 (2.9) | 25908 (3.2) | 32195 (3.5) | 622 (1.4) | 975 (1.7) | 1586 (2.4) | 2078 (2.7) | 2158 (2.9) |
| Missing | 12163 (2.8) | 3469 (0.7) | 2314 (0.4) | 3265 (0.4) | 2808 (0.3) | 1117 (2.5) | 319 (0.6) | 224 (0.3) | 265 (0.3) | 215 (0.3) |
| Comorbidity | ||||||||||
| Diabetes | 45158 (10.5) | 69141 (13.0) | 89230 (15.4) | 152877 (18.7) | 198241 (21.7) | 4863 (11.0) | 8660 (15.0) | 11638 (17.9) | 16358 (21.4) | 18129 (24.2) |
| CHF | 14732 (3.4) | 22041 (4.2) | 24940 (4.3) | 37622 (4.6) | 35652 (3.9) | 2173 (4.9) | 3966 (6.9) | 5147 (7.9) | 6909 (9.0) | 5893 (7.9) |
| Obesity | 17092 (4.0) | 27415 (5.2) | 35684 (6.2) | 67120 (8.2) | 105251 (11.5) | 1619 (3.7) | 2906 (5.0) | 3956 (6.1) | 6115 (8.0) | 7555 (10.1) |
| Renal failure | 1742 (0.4) | 2383 (0.4) | 3443 (0.6) | 12531 (1.5) | 37335 (4.1) | 330 (0.7) | 556 (1.0) | 950 (1.5) | 2525 (3.3) | 5088 (6.8) |
| Number of comorbid conditions, mean (SD) | 1.2 (1.2) | 1.4 (1.3) | 1.6 (1.3) | 1.9 (1.4) | 2.1 (1.4) | 1.2 (1.2) | 1.6 (1.4) | 1.8 (1.4) | 2.2 (1.5) | 2.3 (1.5) |
Abbreviation: SD, standard deviation
P values (test for trend) are less than 0.001 for all comparisons except age (primary TKA, P=0.56; revision TKA, P=0.46).
All values are presented as No. (%) unless otherwise indicated.
The race category of Other includes Asian, Hispanic, North American Native, or other not-specified individuals.
Table 2.
Unadjusted outcomes (LOS, complication rates, and 30-day readmission rates) for primary TKA between 1991 and 2010
| 1991–1994 | 1995–1998 | 1999–2002 | 2003–2006 | 2007–2010 | |
|---|---|---|---|---|---|
| No. of hospitalizations | 431050 | 530128 | 578614 | 816497 | 915562 |
| LOS, days | |||||
| Mean | 7.9 (7.8–7.9) | 4.9 (4.9–5.0) | 4.3 (4.3-4.3) | 3.9 (3.9-3.9) | 3.5 (3.5-3.5) |
| Median (IQR) | 7 (6–9) | 4 (4–6) | 4 (3–5) | 3 (3–4) | 3 (3–4) |
| Discharge Disposition | |||||
| Home | 67.5 (67.3–67.6) | 46.6 (46.4–46.7) | 39.9 (39.8–40.0) | 45.3 (45.2–45.4) | 56.2 (56.1–56.3) |
| Outpatient Skilled/intermediate care/rehabilitation | 16.6 (16.5–16.7) | 29.1 (29.0–29.2) | 28.4 (28.2–28.5) | 26.1 (26.0–26.2) | 30.1 (30.0–30.2) |
| Inpatient Rehabilitation | 14.6 (14.5–14.7) | 22.8 (22.7–23.0) | 29.4 (29.3–29.5) | 25.6 (25.5–25.7) | 11.4 (11.3–11.4) |
| Other | 1.3 (1.3–1.4) | 1.5 (1.4–1.5) | 2.4 (2.3–2.4) | 3.0 (3.0-3.0) | 2.3 (2.3-2.3) |
| Complications within 30-days of discharge | |||||
| Mortality | 0.5 (0.4–0.5) | 0.4 (0.4–0.5) | 0.4 (0.3–0.4) | 0.3 (0.3-0.3) | 0.3 (0.3-0.3) |
| Pulmonary embolism | 0.2 (0.2-0.2) | 0.2 (0.2-0.2) | 0.2 (0.2-0.2) | 0.2 (0.2-0.2) | 0.3 (0.3-0.3) |
| Deep vein thrombosis | 0.4 (0.4-0.4) | 0.4 (0.4-0.4) | 0.3 (0.3-0.3) | 0.3 (0.3-0.3) | 0.4 (0.4-0.4) |
| Wound infection | 0.7 (0.6–0.7) | 0.6 (0.6-0.6) | 0.6 (0.5–0.6) | 0.4 (0.4-0.4) | 0.4 (0.4-0.4) |
| Hemorrhage | 0.1 (0.1-0.1) | 0.1 (0.1-0.1) | 0.2 (0.2-0.2) | 0.2 (0.2–0.3) | 0.3 (0.3-0.3) |
| Sepsis | 0.1 (0.1-0.1) | 0.1 (0.1-0.1) | 0.1 (0.1-0.1) | 0.1 (0.1–0.2) | 0.2 (0.2-0.2) |
| Myocardial Infarction | 0.2 (0.2-0.2) | 0.2 (0.2–0.3) | 0.3 (0.2–0.3) | 0.3 (0.3-0.3) | 0.3 (0.3-0.3) |
| Composite outcome | 1.9 (1.9–2.0) | 1.9 (1.8–1.9) | 1.8 (1.7–1.8) | 1.7 (1.6–1.7) | 1.9 (1.9–1.9) |
| All-cause readmission | |||||
| 30-day | 4.2 (4.1–4.2) | 4.1 (4.1–4.2) | 4.0 (4.0–4.1) | 4.5 (4.5–4.6) | 5.0 (4.9–5.0) |
Abbreviations: IQR, interquartile range; LOS, length of stay; SD, standard deviation.
Values are presented as mean % (95% confidence interval), unless otherwise indicated
P values (test for trend) are less than 0.001 for all comparisons except for LOS (P=0.001) and deep vein thrombosis (P=0.001).
Composite outcome is the occurrence of one-or-more of the following within 30-days of discharge: death, pulmonary embolism, deep vein thrombosis, wound infection, hemorrhage, sepsis, or myocardial infarction
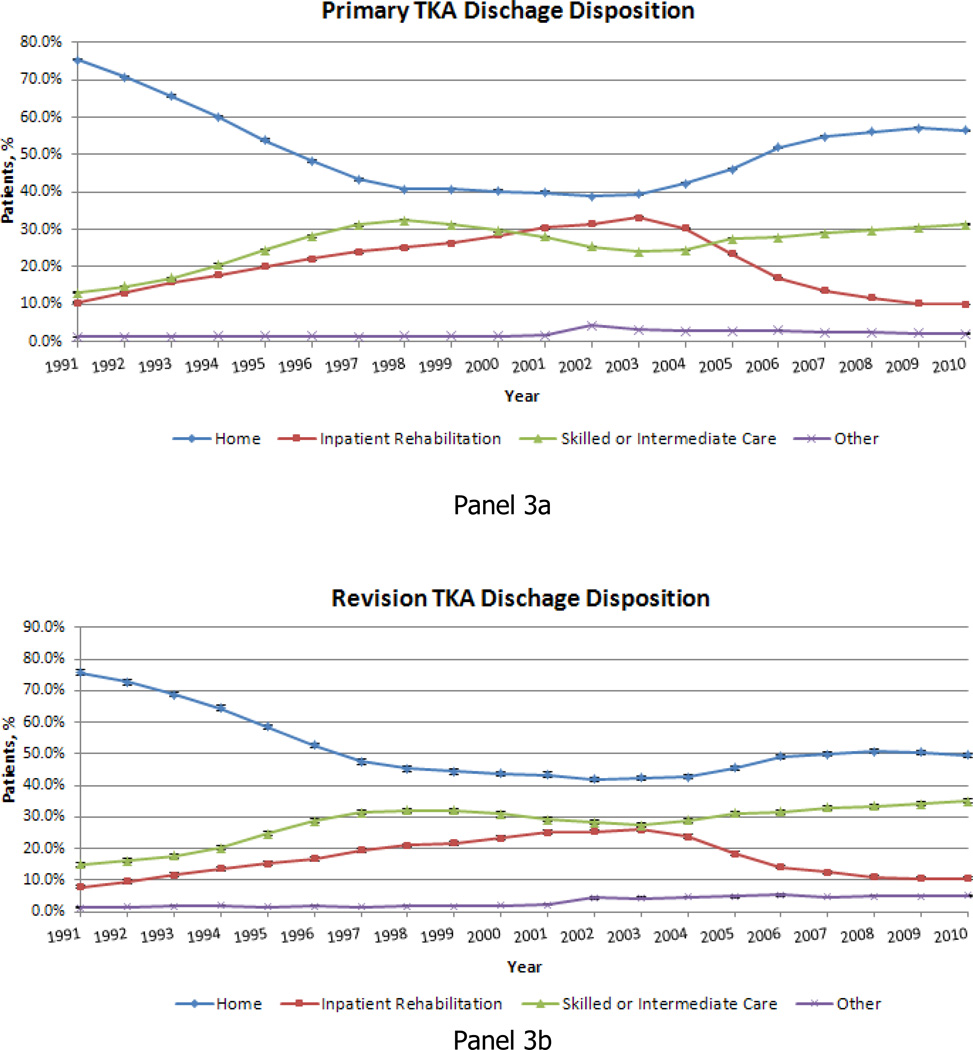
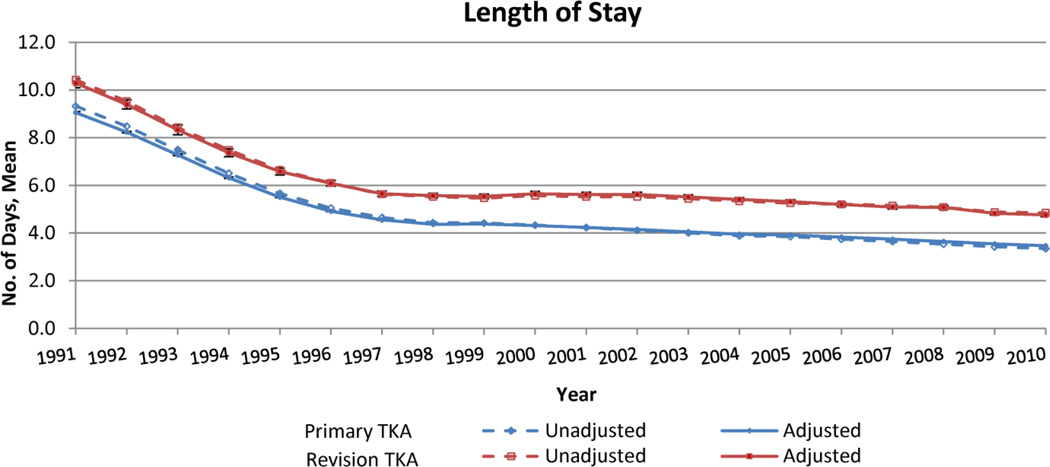
For primary TKA mean hospital LOS declined from 7.9 days (95% CI, 7.8–7.9) in 1991–1994 to 3.5 days (95% CI, 3.5–3.5) in 2007–2010 (Table 3), a relative decline of 55.7% (P< 0.001). The percentage of patients discharged home after primary TKA declined from 67.5% in 1991–1994 to 39.9% in 1999–2002 before increasing to 56.2% in 2007–2010 (Table 3 and Figure 3); alternatively the percentage of patients discharged to inpatient rehabilitation increased from 14.6% in 1991–1994 to 29.4% in 1999–2002 before declining to 11.4% in 2007–20120 and discharge to outpatient rehabilitation facilities increased steadily throughout the study period. Unadjusted mortality within 30-days after discharge dropped from 0.5% (95% CI, 0.4–0.5) in 1991–1994 to 0.3% (95% CI, 0.3-0.3) in 2007–2010, a 40% relative reduction (P< 0.001). Unadjusted rates of most other adverse outcomes remained relatively stable over the study period as did the rate of the composite outcome (Table 3). In contrast, all-cause 30-day readmission rates increased from 4.2% (95% CI, 4.1–4.2) in 1991–1994 to 5.0% (95% CI, 4.9–5.0) in 2007–2010 (P<.001)(Table 3). In adjusted analyses, we found that while hospital LOS for primary TKA declined throughout the study period (Figure 4), both 30-day all-cause readmission rates (Figure 5) and rates of the composite outcome (Figure 6) declined initially, but have been increasing in recent years. In an analysis of the diagnoses and conditions associated with readmission after primary TKA, we observed relatively little change over time (Web Appendix C) with surgical and cardiac complications being relatively common as well as GI hemorrhage and infection particularly in recent years.
Table 3.
Unadjusted outcomes (LOS, complication rates, and 30-day readmission rates) for revision TKA between 1991 and 2010
| 1991–1994 | 1995–1998 | 1999–2002 | 2003–2006 | 2007–2010 | |
|---|---|---|---|---|---|
| No. of hospitalizations | 44120 | 57785 | 65197 | 76526 | 74935 |
| LOS, days | |||||
| Mean | 8.9 (8.8–8.9) | 6.0 (5.9–6.0) | 5.5 (5.5–5.6) | 5.3 (5.3-5.3) | 5.0 (5.0-5.0) |
| Median (IQR) | 7 (5–10) | 5 (4–6) | 4 (3–6) | 4 (3–6) | 4 (3–5) |
| Discharge Disposition | |||||
| Home | 70.0 (69.6–70.4) | 50.8 (50.4–51.2) | 43.3 (43.0–43.7) | 44.9 (44.5–45.2) | 50.2 (49.8–50.5) |
| Outpatient Skilled/intermediate care/rehabilitation | 17.5 (17.1–17.8) | 29.3 (28.9–29.7) | 30.0 (29.6–30.3) | 29.8 (29.4–30.1) | 33.8 (33.5–34.2) |
| Inpatient Rehabilitation | 10.9 (10.6–11.2) | 18.2 (17.9–18.5) | 24.1 (23.7–24.4) | 20.7 (20.4–20.9) | 11.1 (10.9–11.3) |
| Other | 1.7 (1.5–1.8) | 1.7 (1.6–1.8) | 2.7 (2.5–2.8) | 4.7 (4.6–4.9) | 4.9 (4.7–5.0) |
| Complications within 30-days of discharge | |||||
| Mortality | 0.7 (0.6–0.7) | 0.7 (0.6–0.7) | 0.8 (0.7–0.9) | 0.8 (0.7–0.9) | 0.9 (0.8–0.9) |
| Pulmonary embolism | 0.2 (0.1–0.2) | 0.2 (0.1–0.2) | 0.2 (0.1–0.2) | 0.2 (0.1–0.2) | 0.3 (0.2–0.3) |
| Deep vein thrombosis | 0.3 (0.2–0.3) | 0.3 (0.2–0.3) | 0.3 (0.2–0.3) | 0.3 (0.3–0.4) | 0.4 (0.4–0.5) |
| Wound infection | 1.4 (1.3–1.5) | 1.5 (1.4–1.6) | 1.7 (1.6–1.8) | 2.2 (2.1–2.3) | 3.0 (2.9–3.1) |
| Hemorrhage | 0.1 (0.1–0.2) | 0.3 (0.3–0.4) | 0.5 (0.5–0.6) | 0.6 (0.6–0.7) | 0.7 (0.6–0.8) |
| Sepsis | 0.2 (0.1–0.2) | 0.3 (0.2–0.3) | 0.3 (0.3–0.4) | 0.6 (0.5–0.6) | 0.8 (0.7–0.8) |
| Myocardial Infarction | 0.2 (0.2–0.3) | 0.3 (0.3–0.4) | 0.4 (0.3–0.4) | 0.4 (0.4–0.5) | 0.5 (0.4–0.5) |
| Composite outcome | 2.7 (2.6–2.9) | 3.0 (2.9–3.2) | 3.6 (3.4–3.7) | 4.3 (4.2–4.5) | 5.3 (5.2–5.5) |
| All-cause readmission | |||||
| 30-day | 6.1 (5.9–6.4) | 6.2 (6.0–6.4) | 6.5 (6.3–6.7) | 7.7 (7.5–7.9) | 8.9 (8.7–9.2) |
Abbreviations: IQR, interquartile range; LOS, length of stay; SD, standard deviation.
Values are presented as mean % (95% confidence interval), unless otherwise indicated.
P values (test for trend) are less than 0.001 for all comparisons except LOS (P=0.005).
Composite outcome is the occurrence of one-or-more of the following within 30-days of discharge: death, pulmonary embolism, deep vein thrombosis, wound infection, hemorrhage, sepsis, or myocardial infarction
Figure 3.
(Online). Primary (panel 3a) and revision (panel 3b) TKA Discharge Disposition between 1991 and 2010
Error bars indicate 95% confidence interval.
Figure 4.
(Online). Unadjusted and adjusted primary and revision TKA hospital LOS between 1991 and 2010
Error bars indicate 95% confidence interval and are shown for adjusted data only.
Figure 5.
(Online). Unadjusted and adjusted primary and revision TKA 30-day readmission rates between 1991 and 2010
Error bars indicate 95% confidence interval and are shown for adjusted data only.
Figure 6.
(Online). Unadjusted and adjusted primary and revision TKA 30-day Composite Complication Rates1 between 1991 and 2010
Error bars indicate 95% confidence interval and are shown for adjusted data only.
1 Composite outcome is the occurrence of one-or-more of the following within 30-days of discharge: death, pulmonary embolism, deep vein thrombosis, wound infection, hemorrhage, sepsis, or myocardial infarction
For revision TKA mean hospital LOS declined from 8.9 days (95% CI, 8.8–8.9) in 1991–1994 to 5.0 days (95% CI, 5.0-5.0) in 2007–2010, a relative decline of 43.8% (P<.001)(Table 4). Trends in discharge disposition after revision TKA (Table 4 and Figure 3) demonstrated a similar pattern to what was observed for primary TKA; a decline in discharges to home or inpatient rehabilitation and an increase in discharge to skilled care/outpatient rehabilitation. Mortality within 30-days of discharge increased modestly from 0.7% in 1991–1994 to 0.9% in 2007–2010 (a 28.6% relative increase) and rates of wound infection, hemorrhage, sepsis, and myocardial infarction each increased by more than 100%(P<.001 for each). For revision TKA the unadjusted rate of the composite outcome increased from 2.7% (95% CI, 2.6–2.9) in 1991–1994 to 5.3% (95% CI, 5.2–5.5) in 2007–2010 (P<.001). All-cause unadjusted readmission rates within 30-days of discharge increased from 6.1% (95% CI, 5.9–6.4) to 8.9% (95% CI, 8.7–9.2) during the study period (Table 4); the most common causes of readmission after revision TKA are displayed in Web Appendix D.
Table 4.
Factors associated with increased odds of readmission for primary TKA (2007–2010)
| Primary TKA OR (95% CI) |
Revision TKA OR (95% CI) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 1 | Model 2 | Model 3 | Model 4 | |
| Age | ||||||||
| 65–74 | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 75–84 | 1.5 (1.4–1.5) | 1.4 (1.4–1.5) | 1.4 (1.4–1.5) | 1.4 (1.4-1.4) | 1.2 (1.2–1.3) | 1.2 (1.2–1.3) | 1.2 (1.2–1.3) | 1.2 (1.1–1.2) |
| 85+ | 2.0 (1.9–2.1) | 1.9 (1.9–2.0) | 1.9 (1.9–2.0) | 1.8 (1.8–1.9) | 1.6 (1.5–1.8) | 1.6 (1.5–1.7) | 1.6 (1.5–1.7) | 1.4 (1.3–1.5) |
| Race | ||||||||
| White | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Black | 1.4 (1.3–1.4) | 1.3 (1.2–1.3) | 1.3 (1.2–1.3) | 1.2 (1.2–1.3) | 1.3 (1.1–1.4) | 1.2 (1.1–1.3) | 1.2 (1.1–1.3) | 1.1 (1.0–1.2) |
| Other | 1.0 (0.9–1.0) | 1.0 (1.0–1.1) | 1.0 (0.9–1.0) | 0.9 (0.9–1.0) | 1.0 (0.9–1.2) | 1.0 (0.9–1.2) | 1.0 (0.9–1.2) | 0.9 (0.8–1.1) |
| Sex | ||||||||
| Female | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Male | 1.2 (1.2–1.3) | 1.3 (1.2–1.3) | 1.3 (1.2–1.3) | 1.3 (1.2–1.3) | 1.1 (1.0–1.2) | 1.1 (1.1–1.2) | 1.1 (1.1–1.2) | 1.1 (1.0–1.2) |
| Number of Comorbidities | ||||||||
| 0 | --- | Ref | Ref | Ref | --- | Ref | Ref | Ref |
| 1–2 | --- | 1.3 (1.3–1.4) | 1.3 (1.3–1.4) | 1.3 (1.2–1.3) | --- | 1.2 (1.1–1.4) | 1.2 (1.1–1.4) | 1.2 (1.0–1.3) |
| 3–4 | --- | 1.9 (1.9–2.0) | 1.9 (1.8–2.0) | 1.8 (1.7–1.8) | --- | 1.7 (1.5–1.9) | 1.7 (1.5–1.9) | 1.4 (1.3–1.6) |
| 4+ | --- | 2.7 (2.6–2.8) | 2.7 (2.5–2.8) | 2.3 (2.2–2.5) | --- | 2.3 (2.0–2.6) | 2.3 (2.0–2.6) | 1.8 (1.6–2.1) |
| Teaching Status | ||||||||
| Major Teaching | --- | --- | Ref | Ref | --- | --- | Ref | Ref |
| Minor Teaching | --- | --- | 0.9 (0.9–1.0) | 0.9 (0.9–1.0) | --- | --- | 0.9 (0.8–0.9) | 0.9 (0.9–1.0) |
| Non Teaching | --- | --- | 0.9 (0.9–0.9) | 0.9 (0.9–0.9) | --- | --- | 0.8 (0.8–0.9) | 0.9 (0.9–1.0) |
| Hospital Volume | ||||||||
| Quartile I | --- | --- | Ref | Ref | --- | --- | Ref | Ref |
| Quartile II | --- | --- | 0.8 (0.8–0.9) | 0.9 (0.8–0.9) | --- | --- | 0.9 (0.8–1.1) | 1.0 (0.8–1.1) |
| Quartile III | --- | --- | 0.8 (0.7–0.8) | 0.8 (0.8–0.9) | --- | --- | 0.9 (0.8–1.0) | 1.0 (0.8–1.1) |
| Quartile IV | --- | --- | 0.7 (0.7–0.7) | 0.8 (0.7–0.8) | --- | --- | 0.8 (0.7–1.0) | 0.9 (0.8–1.1) |
| Ln(LOS) | --- | --- | --- | 1.9 (1.9–2.0) | --- | --- | --- | 2.1 (2.0–2.2) |
| Year | ||||||||
| 2007 | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 2008 | 1.0 (1.0-1.0) | 1.0 (1.0-1.0) | 1.0 (1.0-1.0) | 1.0 (1.0-1.0) | 1.0 (1.0–1.1) | 1.0 (1.0–1.1) | 1.0 (1.0–1.1) | 1.1 (1.0–1.1) |
| 2009 | 1.0 (0.9–1.0) | 0.9 (0.9–1.0) | 0.9 (0.9–1.0) | 1.0 (1.0-1.0) | 1.0 (1.0–1.1) | 1.0 (1.0–1.1) | 1.0 (1.0–1.1) | 1.1 (1.0–1.2) |
| 2010 | 1.0 (0.9–1.0) | 1.0 (0.9–1.0) | 1.0 (0.9–1.0) | 1.0 (1.0-1.0) | 1.0 (0.9–1.1) | 1.0 (0.9–1.1) | 1.0 (0.9–1.1) | 1.0 (1.0–1.1) |
In adjusted analyses, revision TKA demonstrated a steady decline in hospital LOS (Figure 4) accompanied by an initial decline in readmissions that has reversed in recent years (Figure 5) and an increase in both unadjusted and adjusted rates of the composite outcome (Figure 6).
In bivariate analyses comparing patients who were and were not readmitted after primary TKA (Table X), we found that ABCD and EFG. In our regression models looking at risk-factors for readmission after primary TKA (Table XX), we found that older age, Black race, male sex, index hospital LOS and number of comorbid illnesses were all associated with a significantly increased risk for readmission. Alternatively, we found that teaching hospitals and increased procedure volume were both associated with reduced risk of readmission. Results focusing in revision TKA were generally similar. Likewise, our extensive sensitivity analyses yielded similar results and are available by request from the authors.
DISCUSSION
In an analysis of Medicare administrative data from 1991–2010, we identified a number of interesting trends related to TKA. First, we found a marked increase in the volume of primary TKA procedures being performed; an increase that appeared to be driven not only by an increase in the number of Medicare enrollees but also a substantial increase in the per-capita utilization of TKA procedures. Second, we observed changes in patients’ discharge disposition over time with a decline in the use of inpatient rehabilitation and an increase in the use of outpatient rehabilitation. Third, we found a significant decline in hospital LOS that was accompanied by increasing readmission rates over the past decade.
A number of our findings merit further discussion. Primary and revision Medicare TKA volumes increased by approximately 140% and 90% respectively over the past 20 years while primary and revision TKA utilization increased by 99% and 57% respectively. These figures suggest that growth in primary and revision TKA volume is being driven by both an increase in the number of Medicare enrollees and an increase in per-capita arthroplasty utilization. Our findings extend the findings of a limited body of prior research that has demonstrated rising volume and per-capita utilization of knee arthroplasty.1,28,29 This growth is likely driven by a combination of factors including an expansion in the types of patients considered likely to benefit from TKA, an ageing of the population, and a rising prevalence of certain conditions that predispose patients to osteoarthritis- most notably obesity.30
It is important to note the apparent stabilization of joint arthroplasty utilization in recent years. Our finding extends the work of Bini and colleagues who found evidence of slowing growth in joint arthroplasty utilization within the Kaiser-Permanente healthcare system between 2000 and 2009.31 It is unclear whether this slowing of joint arthroplasty growth is the result of the protracted U.S. economic downturn, saturation of patient demand for arthroplasty, changes in reimbursement or changes in provider beliefs about the risks and benefits of arthroplasty.32,33
The growth in TKA should cause us to give pause and ask whether we are performing too many (or too few) of these procedures both in aggregate and among key patient subgroups defined by race, sex, or age.27,34,35 Any effort to answer this question brings us quickly to the question of TKA indications and appropriateness. A number of clinical practice guidelines for TKA have been developed to guide clinicians and policy makers in evaluating appropriateness.36–40 These guidelines typically suggest consideration of TKA for patients with severe functional limitation unresponsive to conservative management (i.e., medications, physical therapy). While Cobos et al. estimated that as many as 25% of TKA procedures performed in Spain might be considered inappropriate,41 few such studies have been performed in the U.S.12 Conducting studies investigating appropriateness has historically been difficult because of a lack of a national joint arthroplasty registry, though there have been encouraging developments recently to suggest that this may change.42,43 Thus, it is difficult to determine the extent to which the growth in TKA utilization represents growth in appropriate use of a highly effective procedure or overuse of a highly reimbursed procedure where indications still depend on clinical judgment. It is likely that both factors are at play.
Our finding of significant changes in patient’s discharge dispositions following TKA over the 20-year study period is important and hints at the complexities of restraining cost growth. The increase in the percentage of TKA patients discharged to inpatient rehabilitation and skilled care during the 1990s is consistent with prior reports.44 These reports typically relate the increased use of post-acute care to the implementation of the prospective payment system for acute care hospitals in 1983, which, in turn, created a powerful incentive for hospitals to reduce hospital LOS by rapidly discharging patients to post-acute care settings when patients were too ill to safely be discharged home.45,46 However, the rapid rise in Medicare post-acute care spending in the 1990s prompted passage of the Balanced Budget Act (BBA) of 1997 and implementation of a prospective payment system for outpatient skilled care in 1998 and inpatient rehabilitation in 2002.45,47 Our results are consistent with the anticipated effects of these policy changes: a reduction in the use of post-acute care and an increase in the percentage of patients being discharged home after TKA since 2004.
The finding of declining hospital LOS accompanied by rising readmission rates mirrors results of a number of recent studies.48,49 The results of our study as well as other publications suggest that there are limitations in how much LOS can be reduced and that cost savings from further reductions are unlikely to materialize.48,49 In particular, our results and others suggest that there is an inherent tradeoff between shorter hospital LOS, greater need for post-acute care, and higher readmission rates.
A number of other findings merit brief mention. Our finding of increased comorbidity over time likely reflects a combination of factors including increasingly aggressive coding practices and rising prevalence of certain comorbidities (e.g., diabetes, obesity).50,51 The increasing rates of many surgical complications including myocardial infarction, infection, and hemorrhage particularly after revision TKA accompanied by a much smaller increase in mortality is interesting. It seems likely that many of these increases reflect more aggressive testing combined with detection bias resulting from newer more sensitive diagnostic tests (e.g., troponin for myocardial infarction, d-dimer for DVT) rather than a true increase in surgical complications.52 However it is also possible that the incidence of certain complications such as myocardial infarction may be rising, perhaps as a consequence of a greater burden of obesity and diabetes.
Arguably most concerning complication is the rise in readmissions for infection in the revision TKA cohort. While there are well recognized limitations in administrative data for identifying surgical site infections,53,54 our findings should not be discounted prematurely.55,56 There are several potential explanations for rising infection rates in our revision TKA population. One possibility is that the rise in infections represents an increase in revision TKAs being performed specifically to treat infected prostheses. If this were the case, the rise in revision TKA procedures performed would constitute infections that were “present on admission.”57,58 Alternatively, it is possible that the increase in infections represents a real increase in post-operative surgical infections after revision TKA perhaps as a consequence of the increasingly resistant organisms colonizing our hospitals. It is also possible that reduced hospital LOS may lead to reduced vigilance for early signs of superficial wound infection in the post-operative period resulting in higher rates of serious infectious complications. In either case, the rise in infection rates associated with revision TKA warrants close attention. Finally, it is important to comment on our finding that the increase in primary TKA utilization (76%) has been larger than the increase in revision TKA utilization (37%) over the past 20-years. It is possible that this reflects the durability of modern implants and improved surgical technique resulting in a reduced likelihood that patients undergoing primary TKA will require a revision procedure.59 Alternatively, it is possible that the rapid increase in primary TKA over the past 20-years will eventually result in a substantial increase in demand for revision TKA procedures as prosthetic devices wear over time- a possibility that would have significant clinical and economic implications.32
Our study has a number of limitations that warrant brief mention. First, our study was limited to fee-for-service Medicare beneficiaries who constitute approximately 60% of the TKA population.14,28 Our findings should be extrapolated to other populations including younger patients and Medicare managed care enrollees with caution. Second, our study relied upon administrative data and thus we were unable to evaluate a number of important arthroplasty outcomes including functional status and patient satisfaction. Third, we lacked clinical detail and thus were unable to determine the indications for TKA at the level of the individual patient. Likewise, we lacked chart review data for identification of TKA outcomes and complications. Fourth, we focused our analysis on TKA adverse outcomes resulting in hospital readmission within 30-days of discharge. We were unable to identify complications that did not result in an inpatient admission and our 30-day follow-up interval would not capture certain complications such as certain late complications (e.g., infection) that may have manifest themselves after more prolonged delay.60
In summary, over the past 20-years increases in TKA volume have been driven by significant increases in per-capita utilization. We also observed decreased in hospital LOS that were accompanied by increases in hospital readmission rates and rising rates of infections complications.
Supplementary Material
ACKNOWLEDGEMENTS
None.
Dr. Cram is supported by a K24 award from NIAMS (AR062133) and by the Department of Veterans Affairs. This work is also funded in-part by R01 HL085347 from NHLBI and R01 AG033035 from NIA at the NIH. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. The funding sources had no role in the analyses or drafting of this manuscript. Dr. Cram has received consulting fees from The Consumers Union (publisher of Consumer Reports Magazine) and Vanguard Health Inc. for work advice on quality improvement initiatives. Dr. Kates receives institutional research funding from AHRQ, Synthes USA, the American Geriatric Society, the John Hartford Foundation and the AO Research Foundation. Dr. Singh receives institutional research funding from AHRQ, US Food and Drug Administration, NIA, Takeda pharmaceuticals and Savient pharmaceuticals, is a consultant for Takeda, Novartis, Savient, URL and Ardea and has received travel grants from Allergan, Wyeth, Amgen and Takeda and speaker honoraria from Abbott.
Footnotes
COMPETING INTERESTS: None of the authors have any conflicts of interest.
AUTHORS’ CONTRIBUTIONS: Dr. Cram and Ms. Lu had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. Journal of Bone and Joint Surgery. 2005 Jul;87(7):1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 2.Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Archives of Internal Medicine. 2009 Jun 22;169(12):1113–1121. doi: 10.1001/archinternmed.2009.136. discussion 1121-1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Healy WL, Rana AJ, Iorio R. Hospital Economics of Primary Total Knee Arthroplasty at a Teaching Hospital. Clin Orthop Relat Res. 2010 Aug 6; doi: 10.1007/s11999-010-1486-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agency for Healthcare Research and Quality. 2007 HCUP Nationwide Inpatient Sample Comparison Report Report 2010-03. [Accessed November 13, 2011]; http://www.hcup-us.ahrq.gov/reports/methods/2010_03.pdf.
- 5.Krummenauer F, Wolf C, Gunther KP, Kirschner S. Clinical Benefit and Cost Effectiveness of Total Knee Arthroplasty in the Older Patient. European Journal of Medical Research. 2009 Feb 18;14(2):76–84. doi: 10.1186/2047-783X-14-2-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011 Jun 2;364(22):2128–2137. doi: 10.1056/NEJMsa1010705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cram P, Vaughan-Sarrazin MS, Wolf B, Katz JN, Rosenthal GE. A comparison of total hip and knee replacement in specialty and general hospitals. J Bone Joint Surg Am. 2007 Aug;89(8):1675–1684. doi: 10.2106/JBJS.F.00873. [DOI] [PubMed] [Google Scholar]
- 8.Manley M, Ong K, Lau E, Kurtz SM. Total knee arthroplasty survivorship in the United States Medicare population: effect of hospital and surgeon procedure volume. Journal of Arthroplasty. 2009 Oct;24(7):1061–1067. doi: 10.1016/j.arth.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 9.Chernew M, Goldman D, Axeen S. How much savings can we wring from Medicare? N Engl J Med. 2011 Oct 6;365(14):e29. doi: 10.1056/NEJMp1110593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baicker K, Chernew ME. The economics of financing Medicare. N Engl J Med. 2011 Jul 28;365(4):e7. doi: 10.1056/NEJMp1107671. [DOI] [PubMed] [Google Scholar]
- 11.Smith-Bindman R, Miglioretti DL, Larson EB. Rising use of diagnostic medical imaging in a large integrated health system. Health Affairs. 2008 Nov-Dec;27(6):1491–1502. doi: 10.1377/hlthaff.27.6.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jain NB, Higgins LD, Ozumba D, et al. Trends in epidemiology of knee arthroplasty in the United States, 1990–2000. Arthritis and Rheumatism. 2005 Dec;52(12):3928–3933. doi: 10.1002/art.21420. [DOI] [PubMed] [Google Scholar]
- 13.Khatod M, Inacio M, Paxton EW, et al. Knee replacement: epidemiology, outcomes, and trends in Southern California: 17,080 replacements from 1995 through 2004. Acta Orthop. 2008 Dec;79(6):812–819. doi: 10.1080/17453670810016902. [DOI] [PubMed] [Google Scholar]
- 14.Memtsoudis SG, Della Valle AG, Besculides MC, Gaber L, Laskin R. Trends in demographics, comorbidity profiles, in-hospital complications and mortality associated with primary knee arthroplasty. J Arthroplasty. 2009 Jun;24(4):518–527. doi: 10.1016/j.arth.2008.01.307. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell JB, Bubolz T, Paul JE, et al. Using Medicare claims for outcomes research. Medical Care. 1994 Jul;32(7 Suppl):JS38–JS51. [PubMed] [Google Scholar]
- 16.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. Journal of Bone & Joint Surgery - American Volume. 2004 Sep;86-A(9):1909–1916. doi: 10.2106/00004623-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Losina E, Barrett J, Mahomed NN, Baron JA, Katz JN. Early failures of total hip replacement: effect of surgeon volume. Arthritis & Rheumatism. 2004 Apr;50(4):1338–1343. doi: 10.1002/art.20148. [DOI] [PubMed] [Google Scholar]
- 18.Katz JN, Losina E, Barrett J, et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. Journal of Bone & Joint Surgery - American Volume. 2001 Nov;83-A(11):1622–1629. doi: 10.2106/00004623-200111000-00002. [see comment]. [DOI] [PubMed] [Google Scholar]
- 19.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical Care. 1998 Jan;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005 Nov;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 21.Cram P, Lu X, Callaghan JJ, Vaughan-Sarrazin MS, Cai X, Li Y. Long-Term Trends in Hip Arthroplasty Use and Volume. J Arthroplasty. 2011 Jul 11; doi: 10.1016/j.arth.2011.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hagen TP, Vaughan-Sarrazin MS, Cram P. Relation between hospital orthopaedic specialisation and outcomes in patients aged 65 and older: retrospective analysis of US Medicare data. BMJ. 2010 Feb 11;340:165. doi: 10.1136/bmj.c165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clinical Classification Software (CCS) for ICD9-CM Codes. [Accessed May 16, 2012]; Available at: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/CCSUsersGuide.pdf.
- 24.Shahian DM, Torchiana DF, Shemin RJ, Rawn JD, Normand SL. Massachusetts cardiac surgery report card: implications of statistical methodology. Ann Thorac Surg. 2005 Dec;80(6):2106–2113. doi: 10.1016/j.athoracsur.2005.06.078. [DOI] [PubMed] [Google Scholar]
- 25.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. Philadelphia, PA: Lippincott, Williams, and Wilkins; 2008. [Google Scholar]
- 26.Hausmann LR, Mor M, Hanusa BH, et al. The effect of patient race on total joint replacement recommendations and utilization in the orthopedic setting. J Gen Intern Med. 2010 Sep;25(9):982–988. doi: 10.1007/s11606-010-1399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones A, Kwoh CK, Kelley ME, Ibrahim SA. Racial disparity in knee arthroplasty utilization in the veterans health administration. Arthritis Rheum. 2005 Dec 15;53(6):979–981. doi: 10.1002/art.21596. [DOI] [PubMed] [Google Scholar]
- 28.Kim S. Changes in surgical loads and economic burden of hip and knee replacements in the US: 1997–2004. Arthritis Rheum. 2008 Apr 15;59(4):481–488. doi: 10.1002/art.23525. [DOI] [PubMed] [Google Scholar]
- 29.Freid VM, Bernstein AB. Health care utilization among adults aged 55–64 years: how has it changed over the past 10 years? NCHS Data Brief. 2010 Mar;(32):1–8. [PubMed] [Google Scholar]
- 30.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012 Feb 1;94(3):201–207. doi: 10.2106/JBJS.J.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bini SA, Sidney S, Sorel M. Slowing demand for total joint arthroplasty in a population of 3.2 million. J Arthroplasty. 2011 Sep;26(6 Suppl):124–128. doi: 10.1016/j.arth.2011.03.043. [DOI] [PubMed] [Google Scholar]
- 32.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 33.Iorio R, Davis CM, 3rd, Healy WL, Fehring TK, O'Connor MI, York S. Impact of the economic downturn on adult reconstruction surgery: a survey of the American Association of Hip and Knee Surgeons. J Arthroplasty. 2010 Oct;25(7):1005–1014. doi: 10.1016/j.arth.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 34.Borrero S, Kwoh CK, Sartorius J, Ibrahim SA. Brief report: Gender and total knee/hip arthroplasty utilization rate in the VA system. J Gen Intern Med. 2006 Mar;21(Suppl 3):S54–S57. doi: 10.1111/j.1525-1497.2006.00375.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Understanding ethnic differences in the utilization of joint replacement for osteoarthritis: the role of patient-level factors. Med Care. 2002 Jan;40(1 Suppl):I44–I51. doi: 10.1097/00005650-200201001-00006. [DOI] [PubMed] [Google Scholar]
- 36.Gossec L, Paternotte S, Maillefert JF, et al. The role of pain and functional impairment in the decision to recommend total joint replacement in hip and knee osteoarthritis: an international cross-sectional study of 1909 patients. Report of the OARSI-OMERACT Task Force on total joint replacement. Osteoarthritis Cartilage. 2011 Feb;19(2):147–154. doi: 10.1016/j.joca.2010.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Naylor CD, Williams JI. Primary hip and knee replacement surgery: Ontario criteria for case selection and surgical priority. Qual Health Care. 1996 Mar;5(1):20–30. doi: 10.1136/qshc.5.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Escobar A, Quintana JM, Arostegui I, et al. Development of explicit criteria for total knee replacement. Int J Technol Assess Health Care. 2003 Winter;19(1):57–70. doi: 10.1017/s0266462303000060. [DOI] [PubMed] [Google Scholar]
- 39.Dieppe P, Lim K, Lohmander S. Who should have knee joint replacement surgery for osteoarthritis? Int J Rheum Dis. 2011 May;14(2):175–180. doi: 10.1111/j.1756-185X.2011.01611.x. [DOI] [PubMed] [Google Scholar]
- 40.Escobar A, Quintana JM, Bilbao A, et al. Development of explicit criteria for prioritization of hip and knee replacement. J Eval Clin Pract. 2007 Jun;13(3):429–434. doi: 10.1111/j.1365-2753.2006.00733.x. [DOI] [PubMed] [Google Scholar]
- 41.Cobos R, Latorre A, Aizpuru F, et al. Variability of indication criteria in knee and hip replacement: an observational study. BMC Musculoskelet Disord. 2010;11:249. doi: 10.1186/1471-2474-11-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lonner JH. National joint replacement registry. Am J Orthop (Belle Mead NJ) 2009 Oct;38(10):497–498. [PubMed] [Google Scholar]
- 43.Paxton EW, Ake CF, Inacio MC, Khatod M, Marinac-Dabic D, Sedrakyan A. Evaluation of total hip arthroplasty devices using a total joint replacement registry. Pharmacoepidemiology and Drug Safety. 2012;21:53–59. doi: 10.1002/pds.3228. [DOI] [PubMed] [Google Scholar]
- 44.MedPAC. Report to the Congress: variation and innovation in medicare. 2003 Jun [Google Scholar]
- 45.McCall N, Korb J, Petersons A, Moore S. Reforming Medicare payment: early effects of the 1997 Balanced Budget Act on postacute care. Milbank Q. 2003;81(2):277–303. 172–273. doi: 10.1111/1468-0009.t01-1-00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chan L, Koepsell TD, Deyo RA, et al. The effect of Medicare's payment system for rehabilitation hospitals on length of stay, charges, and total payments. N Engl J Med. 1997 Oct 2;337(14):978–985. doi: 10.1056/NEJM199710023371406. [DOI] [PubMed] [Google Scholar]
- 47.Buntin MB, Colla CH, Escarce JJ. Effects of payment changes on trends in post-acute care. Health Serv Res. 2009 Aug;44(4):1188–1210. doi: 10.1111/j.1475-6773.2009.00968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010 Jun 2;303(21):2141–2147. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cram P, Lu X, Kaboli PJ, et al. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991–2008. JAMA. 2011 Apr 20;305(15):1560–1567. doi: 10.1001/jama.2011.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Silverman E, Skinner J. Medicare upcoding and hospital ownership. J Health Econ. 2004 Mar;23(2):369–389. doi: 10.1016/j.jhealeco.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 51.Vaughan-Sarrazin MS, Lu X, Cram P. The impact of paradoxical comorbidities on risk-adjusted mortality of Medicare beneficiaries with cardiovascular disease. Medicare Medicaid Res Rev. 2011;1(3) doi: 10.5600/mmrr.001.03.a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Welch HG, Schwartz L, Woloshin S. Overdiagnosed: making people sick in the persuit of health. Boston, MA: Beacon Press; 2011. [Google Scholar]
- 53.Stevenson KB, Khan Y, Dickman J, et al. Administrative coding data, compared with CDC/NHSN criteria, are poor indicators of health care-associated infections. Am J Infect Control. 2008 Apr;36(3):155–164. doi: 10.1016/j.ajic.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 54.Schweizer ML, Eber MR, Laxminarayan R, et al. Validity of ICD-9-CM coding for identifying incident methicillin-resistant Staphylococcus aureus (MRSA) infections: is MRSA infection coded as a chronic disease? Infect Control Hosp Epidemiol. 2011 Feb;32(2):148–154. doi: 10.1086/657936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Calderwood MS, Ma A, Khan YM, et al. Use of Medicare diagnosis and procedure codes to improve detection of surgical site infections following hip arthroplasty, knee arthroplasty, and vascular surgery. Infect Control Hosp Epidemiol. 2012 Jan;33(1):40–49. doi: 10.1086/663207. [DOI] [PubMed] [Google Scholar]
- 56.Thomas C, Cadwallader HL, Riley TV. Surgical-site infections after orthopaedic surgery: statewide surveillance using linked administrative databases. J Hosp Infect. 2004 May;57(1):25–30. doi: 10.1016/j.jhin.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 57.Glance LG, Osler TM, Mukamel DB, Dick AW. Impact of the present-on-admission indicator on hospital quality measurement: experience with the Agency for Healthcare Research and Quality (AHRQ) Inpatient Quality Indicators. Medical Care. 2008 Feb;46(2):112–119. doi: 10.1097/MLR.0b013e318158aed6. [DOI] [PubMed] [Google Scholar]
- 58.Glance LG, Dick AW, Osler TM, Mukamel DB. Does date stamping ICD-9-CM codes increase the value of clinical information in administrative data? Health Services Research. 2006 Feb;41(1):231–251. doi: 10.1111/j.1475-6773.2005.00419.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Carr AJ, Robertsson O, Graves S, et al. Knee replacement. Lancet. 2012 Mar 5; doi: 10.1016/S0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 60.Cram P, Ibrahim SA, Lu X, Wolf BR. Impact of Alternative Coding Schemes on Incidence Rates of Key Complications After Total Hip Arthroplasty. Geriatric Orthopaedic Surgery & Rehabilitation. 2012 Mar 1;3(1):17–26. doi: 10.1177/2151458511435723. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.