Abstract
Background
Consistently reported prognostic factors for glioblastoma (GBM) are age, extent of surgery, performance status, IDH1 mutational status, and MGMT promoter methylation status. We aimed to integrate biological and clinical prognostic factors into a nomogram intended to predict the survival time of an individual GBM patient treated with a standard regimen. In a previous study we showed that the methylation status of the DGKI promoter identified patients with MGMT-methylated tumors that responded poorly to the standard regimen. We further evaluated the potential prognostic value of DGKI methylation status.
Methods
399 patients with newly diagnosed GBM and treated with a standard regimen were retrospectively included in this study. Survival modelling was performed on two patient populations: intention-to-treat population of all included patients (population 1) and MGMT-methylated patients (population 2). Cox proportional hazard models were fitted to identify the main prognostic factors. A nomogram was developed for population 1. The prognostic value of DGKI promoter methylation status was evaluated on population 1 and population 2.
Results
The nomogram-based stratification of the cohort identified two risk groups (high/low) with significantly different median survival. We validated the prognostic value of DGKI methylation status for MGMT-methylated patients. We also demonstrated that the DGKI methylation status identified 22% of poorly responding patients in the low-risk group defined by the nomogram.
Conclusions
Our results improve the conventional MGMT stratification of GBM patients receiving standard treatment. These results could help the interpretation of published or ongoing clinical trial outcomes and refine patient recruitment in the future.
Introduction
Glioblastoma (GBM) is the most common and aggressive primary brain tumor in adults. Its prognosis remains extremely poor, despite multimodal treatment by surgery, radiotherapy, and temozolomide-based chemotherapy (standard regimen) [1]. The most consistently reported clinical prognostic factors for GBM are age, extent of surgery, and performance status [2], [3], [4]. The somatic mutation affecting amino acid 132 in the isocitrate dehydrogenases 1 gene (IDH1) is also associated with a better clinical outcome in gliomas, including glioblastoma. However, this mutation is rare in primary GBMs (approximately 6%) [5], [6], [7]. The methylation status of the O6-methylguanine DNA methyltransferase gene (MGMT) promoter is currently the strongest predictive biomarker of outcome and benefit from temozolomide-based treatment of GBM [8]. In 2008, Gorlia et al. integrated biological and clinical prognostic factors and their independent and combined predictive powers into nomograms for GBM patients treated with the standard regimen [9]. These nomograms can be used to predict an individual patient's median survival and the probability of survival at two years. These nomograms can be of interest in patient counselling and in the design and interpretation of clinical trials. However, the authors stressed a lack of statistical power in their subgroup analysis of patients who had an available MGMT promoter methylation status (n = 103).
In this study, we retrospectively analysed 399 GBM patients treated with the standard regimen (intention-to-treat). We identified the main clinical prognostic factors in this cohort and compared our results with those of the EORTC (European Organisation for Research and Treatment of Cancer) and NCIC (National Cancer Institute of Canada) trial 26981-22981/CE.3. We propose an updated nomogram intended to predict the survival time of an individual GBM patient. In a previous study on 50 GBM patients treated with the standard regimen, we showed that the methylation status of the diacylglycerol kinase iota gene (DGKI) promoter identified patients with MGMT-methylated tumors that responded poorly to the standard regimen [10]. The role of DGKI and the functional consequences of its methylation status have never been investigated in gliomas but DGKI regulates Ras signalling, an oncogenic pathway frequently altered in GBM [11], [12]. We further evaluated the potential predictive value of DGKI methylation status in the context of both MGMT-methylated and intention-to-treat populations.
Materials and Methods
Patients and tissue samples
This multi-center retrospective cohort included 399 patients treated in the Departments of Neurosurgery/Neuro-oncology of Angers (n = 28), Marseille (n = 52), Paris-Salpêtrière (n = 227), Rennes (n = 50), and Poitiers (n = 42) between 2006 and 2011. The inclusion criteria were as follows: 1) patients aged 18 years or more, 2) diagnosis of a primary GBM (WHO grade IV), 3) detailed clinical information at diagnosis and during follow-up, 4) treatment with radiotherapy and concurrent/adjuvant temozolomide (standard regimen), and 5) availability of tumor tissue with informed consent in accordance with French regulations and the Helsinki Declaration. All patients included in this study fulfilled the inclusion criteria. Particularly, all patients received a radio-chemotherapy regimen in accordance with the standard of care. Follow-up for included patients ranged from 24 days to 5.2 years (median, 15.5 months). Tumor samples were snap-frozen immediately after resection and stored in tumor banks under the following authorization numbers: (Centre de Ressources Biologiques, DC-2011-1467, Angers), 2008/70 (AP-HM Tumor Bank, Marseille), DC 2009-957 (OncoNeuroTheque Salpêtrière, Paris), DHOS/2004/04056 (Hospital Tumor Bank, Poitiers), and AC-2010-77 (Centre de Ressources Biologiques, Rennes). The extent of surgery was evaluated with an enhanced magnetic resonance imaging (MRI) performed within 24 hours after the resection. All samples presented at least 70% of tumor cells. For each tumor sample, DNA was extracted using the NucleoSpin Tissue Kit (Macherey Nagel) according to the manufacturer's instructions. The quality of the DNA samples was assessed by electrophoresis on a 1% agarose gel. Only high quality genomic DNAs were selected for further analyses.
Two patient populations were considered in this study: the population of all included patients (population 1) and the subgroup of MGMT-methylated patients (population 2). Population 1 was used to identify the main clinical prognostic factors and to compare our results with those of the EORTC and NCIC trial 26981-22981/CE.3 [9]. Population 2 was studied to evaluate the strength and importance of these prognostic factors after conventional MGMT stratification. The effect of DGKI promoter methylation status on the prognosis of GBM patients assigned to standard treatment was also evaluated in MGMT-methylated patients. Patients from population 2 were randomly assigned to a training cohort and a validation cohort of equal sizes in a randomized block design stratified by the hospital center. Table 1 shows the demographic and clinical characteristics of the patients included in this study.
Table 1. Patients demographic and clinical characteristics.
| Characteristics | Population 1 (n = 399) | EORTC cohort* (n = 103) | Population 2 training (n = 86) | Population 2 validation (n = 89) | |
| Age (years) | |||||
| Median | 59 | 57 | 59 | ||
| Range | 21–88 | 29–88 | 26–80 | ||
| Age - no. (%) | |||||
| ≤50 | 95 (24) | 44 (43) | 23 (27) | 22 (25) | |
| 51–60 | 130 (33) | 40 (39) | 30 (35) | 26 (29) | |
| >60 | 174 (44) | 19 (18) | 33 (38) | 41 (46) | |
| Sex - no. (%) | |||||
| Women | 161 (40) | 38 (37) | 41 (48) | 41 (46) | |
| Men | 238 (60) | 65 (63) | 45 (52) | 48 (54) | |
| KPS (%) | |||||
| Median | 80 | 80 | 80 | ||
| Range | 40–100 | 40–100 | 40–100 | ||
| KPS - no. (%) | |||||
| ≤70 | 37 (9) | 10 (12) | 10 (11) | ||
| >70 | 331 (83) | 69 (80) | 72 (81) | ||
| Missing | 31 (8) | 7 (8) | 7 (8) | ||
| Extent of surgery - no. (%) | |||||
| Biopsy | 30 (8) | 0 (0) | 10 (12) | 5 (6) | |
| Partial resection | 140 (35) | 56 (54) | 25 (29) | 34 (38) | |
| Complete resection | 220 (55) | 47 (46) | 50 (58) | 49 (55) | |
| Missing | 9 (2) | 0 (0) | 1 (1) | 1 (1) | |
| IDH1 mutational status - no. (%) | |||||
| Mutated | 18 (5) | 5 (6) | 8 (9) | ||
| Wild-type | 364 (91) | 80 (93) | 77 (87) | ||
| Missing | 17 (4) | 1 (1) | 4 (4) | ||
| MGMT methylation status - no. (%) | |||||
| Methylated | 175 (44) | 45 (44) | 86 (100) | 89 (100) | |
| Unmethylated | 224 (56) | 58 (56) | 0 (0) | 0 (0) | |
| DGKI methylation status - no. (%) | |||||
| Methylated | 95 (24) | 22 (26) | 21 (24) | ||
| Ummethylated | 304 (76) | 61 (74) | 68 (76) | ||
| Overall survival - mo | |||||
| Median | 19.1 | 29.6 | 30.2 | ||
| 95% CI | 17.1–20.8 | 22.5–46.7 | 24.1–46.8 | ||
| Progression-free survival - mo | |||||
| Median | 10.8 | 15.2 | 15.6 | ||
| 95% CI | 10.1–11.9 | 13.8–19.1 | 13.1–23.4 | ||
*EORTC and NCIC trial 26981-22981/CE.3 population 3: GBM patients who underwent partial or complete resection and were assigned temozolomide and radiotherapy in the presence of an MGMT promoter methylation assessment.
IDH1 mutation
Tumor DNA was screened for somatic mutations in IDH1 codon 132 via exon 4 PCR amplification and direct sequencing as previously described [13]. Because IDH1 mutation is sufficient to establish the “glioma-CpG island methylator phenotype” (G-CIMP), we did not take this phenotype into account in our analysis [14].
DNA methylation analysis
DNA was bisulfite-modified using the EZ DNA Methylation Kit (Zymo Research). The methylation percentage (%met) of the MGMT promoter was measured using the PyroMark Q96 CpG MGMT kit (Qiagen) (average percentage of the five tested CpG sites). The DGKI promoter's %met was measured using VeraCode GoldenGate Methylation technology (Illumina Inc.) or by pyrosequencing. PCR and pyrosequencing primers were designed using the Pyrosequencing Assay Design Software (Qiagen). The primers and PCR conditions are given in Figure S1. The reproducibility of the pyrosequencing assays was assessed on a subset of 21 patients for MGMT (Pearson correlation coefficient r = 0.999, p<1e-08) and of 26 patients for DGKI (Pearson correlation coefficient r = 0.994, p<1e-08). The consistency between VeraCode GoldenGate Methylation technology and pyrosequencing was assessed on 24 patients for DGKI (Pearson correlation coefficient r = 0.89, p<1e-08). The assessment of MGMT and DGKI %met was conducted at the Rennes hospital. For MGMT, we used the 8% methylation threshold defined on an independent data set by Quillien et al. [15]. The DGKI methylation threshold of 28% was determined in the training cohort using the risksetROC R package (AUC = 0.61).
Statistical analyses
Overall survival (OS) and progression-free survival (PFS) were estimated using the Kaplan-Meier method. Comparisons between survival groups were performed using a log-rank test for binary variables, and a log-rank trend test for ordered categories. Cox proportional hazard models provided estimates of the hazard ratios (HRs). From these tests, variables with p-values less than 5% were candidates for the multivariate analyses. In population 1, the Cox proportional hazards model was then used with forward stepwise model selection. We have checked that no evidence of violation of the proportional hazards assumption was found. The probability of inclusion of a factor in the multivariate model was estimated by using the bootstrap resampling technique as described in Gorlia et al. [9]. All tests were adjusted for hospital center. Analyses were carried out using the survival R package.
A nomogram was developed for population 1 to predict each patient's median survival and probability of survival at two years, taking into account their clinical characteristics. Variables with a probability of inclusion higher than 90% based on 1000 bootstrap samples were included in the final model. The definition of two risk groups (high/low) was based on the value of the linear predictor underlying the nomogram; values greater than or equal to zero were assigned to the high-risk group, and negative values were assigned to the low-risk group (the total points cut-off between high and low-risk is the value matching a linear predictor value equal to zero). The accuracy of predictions was assessed by estimating the model's calibration and discrimination measured by the Concordance index corrected for optimism (C-index). The nomogram was built using the rms R package.
Results
Survival analysis of all included patients (population 1)
In population 1, univariate Cox analyses showed that age, Karnofsky performance status (KPS), extent of surgery, IDH1 mutational status, MGMT promoter methylation status, and DGKI promoter methylation status were significantly associated with OS (Table 2). These variables remained significantly associated with OS in the multivariate Cox analyses (Table 3). The final multivariate Cox model used to build the nomogram included age, KPS, extent of surgery, IDH1 mutational status, and MGMT promoter methylation status. This model was associated with a C-index corrected for optimism of 68%.
Table 2. Univariate analyses of survival prognostic factors.
| Population 1 (n = 399) | Population 2 (n = 175) | |||||||||
| Training cohort (n = 86) | Validation cohort (n = 89) | |||||||||
| Median survival, months (95% CI) | HR (95% CI) | p | Median survival, months (95% CI) | HR (95% CI) | p | Median survival, months (95% CI) | HR (95% CI) | p | ||
| Age (years) | ||||||||||
| ≤50 | 33.1 (24.2–56.7) | .. | <0.001 | 42.5 (33.1-N) | .. | 0.01 | NA (37.8-N) | .. | 0.01 | |
| 51-60 | 19.3 (17.1–24.3) | 1.4 (1.2–1.7) | .. | 31.4 (19.7-N) | 1.7 (1.1–2.6) | .. | 30.2 (26.2-N) | 1.8 (1.1–2.8) | .. | |
| >60 | 15.6 (14.0–18.0) | .. | .. | 20.1 (16.3-N) | .. | .. | 16.5 (14.4–37.2) | .. | .. | |
| Sex | ||||||||||
| Women | 18.0 (16.3–26.0) | 1.0 | NS | 34.8 (25.0-N) | 1.0 | NS | 34.4 (17.8–N) | 1.0 | NS | |
| Men | 19.3 (17.1–21.1) | 1.2 (0.9–1.6) | .. | 24.6 (19.7-N) | 1.6 (0.8–3.3) | .. | 27.5 (21.5–46.8) | 0.9 (0.5–1.7) | .. | |
| KPS (%) | ||||||||||
| ≤70 | 11.7 (10.2–16.9) | 1.0 | <0.001 | 19.3 (9.5-N) | 1.0 | 0.002 | 13.3 (10.9-N) | 1.0 | 0.002 | |
| >70 | 19.8 (18.3–24.1) | 0.5 (0.3–0.7) | .. | 33.1 (26.2–52.6) | 0.1 (0.04–0.5) | .. | 34.4 (26.2-N) | 0.2 (0.1–0.6) | .. | |
| Extent of surgery | ||||||||||
| Biopsy | 14.5 (11.3–34.8) | .. | 0.002 | 14.5 (11.4-N) | .. | 0.01 | 20.3 (20.3-N) | .. | NS | |
| Partial | 19.2 (17.1–24.1) | 0.7 (0.6–0.9) | .. | 19.9 (19.1-N) | 0.6 (0.4–0.9) | .. | 37.8.1 (21.5-N) | 0.8 (0.5–1.5) | .. | |
| Complete | 19.6 (17.1–22.3) | .. | .. | 33.1 (25.0-N) | .. | .. | 27.5 (22.3-N) | .. | .. | |
| IDH1 mutational status | ||||||||||
| Mutated | 56.7 (38.6-N) | 1.0 | <0.001 | 56.7 (N-N) | 1.0 | NS | NA (38.6-N) | 1.0 | NS | |
| Wild-type | 18.3 (16.6–19.8) | 7.8 (2.5–24.3) | .. | 27.8 (21.1–42.5) | 4.4 (0.6–33.8) | .. | 24.8 (20.3–37.8) | 5.3 (0.7–39.5) | .. | |
| MGMT methylation status | ||||||||||
| Methylated | 30.2 (24.8–37.8) | 1.0 | <0.001 | |||||||
| Unmethylated | 14.9 (13.8–16.9) | 3.1 (2.3–4.2) | .. | |||||||
| DGKI methylation status | ||||||||||
| Methylated | 16.9 (14–19.9) | 1.0 | 0.004 | 19.9 (9.9–N) | 1.0 | <0.001 | 16.5 (13.3-N) | 1.0 | 0.01 | |
| Unmethylated | 19.6 (17.8–24.1) | 0.7 (0.5–0.9) | .. | 34.8 (27.8–52.6) | 0.3 (0.1–0.5) | .. | 37.8 (26.2-N) | 0.4 (0.2–0.8) | .. | |
NA = not available; N = not enough events to calculate upper 95% CI boundary; NS = not significant. Age, KPS and extent of surgery are treated as ordinal variables.
Table 3. Multivariate analyses of survival prognostic factors.
| Population 1 (n = 399) | |||
| HR (95% CI) | p (%inclusion) | ||
| Age (years) | |||
| ≤50 | .. | 0.006 (92) | |
| 51–60 | 1.3 (1.1–1.6) | .. | |
| >60 | .. | .. | |
| Karnofsky performance status (%) | |||
| ≤70 | 1.0 | <0.001 (99) | |
| >70 | 0.4 (0.2–0.6) | .. | |
| Extent of surgery | |||
| Biopsy | .. | <0.001 (98) | |
| Partial resection | 0.6 (0.5–0.8) | .. | |
| Complete resection | .. | .. | |
| IDH1 mutational status | |||
| Mutated | 1.0 | 0.02 (94) | |
| Wild-type | 4.1 (1.3–13.3) | .. | |
| MGMT methylation status | |||
| Methylated | 1.0 | <0.001 (100) | |
| Unmethylated | 3.0 (2.2–4.2) | .. | |
| DGKI methylation status | |||
| Methylated | 1.0 | 0.03 (74) | |
| Unmethylated | 0.7 (0.5–1.0) | .. | |
NA = not available; N = not enough events to calculate upper 95% CI boundary; NS = not significant. For ordered categorical factors, the first value is the reference.
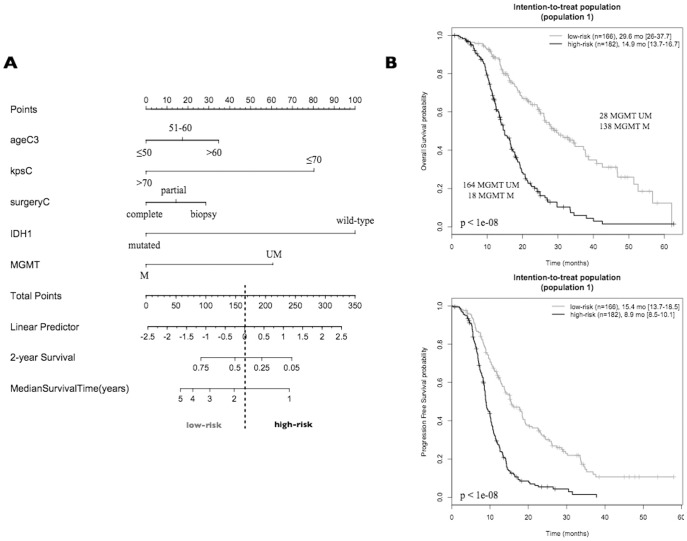
Figure 1A shows the nomogram for population 1. The total number of points for each patient is obtained by summing the points for each of the individual factors in the nomogram. The median survival and probability of survival at two years for a given patient are obtained by drawing a vertical line from the “total points” axis down to the outcome axes. For example, a 55-year-old patient with a KPS of 80 and a partly resected/IDH1 wild-type/MGMT-methylated tumor has a total prognostic score of 129 and is predicted to have a median survival of approximately 30 months and a 60% probability of surviving two years. Because the cut-off between high and low risk is 165 points, this patient is assigned to the low-risk group. Patients in the low-risk group had a median OS of 29.6 months (95% CI, 26.0–37.7), which was significantly longer than 14.9 months (95% CI, 13.7–16.7) for patients in the high-risk group (p<1e-08). A similar stratification was observed for the PFS (Figure 1B).
Figure 1. GBM patients assigned to standard treatment (population 1).
(A) Nomogram for predicting median survival, probability of survival at two years, and risk category. The total number of points for each patient is obtained by summing the points for each of the individual factors in the nomogram. The median survival and probability of survival at two years for a given patient are obtained by drawing a vertical line from the “total points” axis down to the outcome axes. The definition of two risk groups (high/low) is based on the value of the linear predictor underlying the nomogram: values greater than or equal to zero were assigned to the high-risk group, and negative values were assigned to the low-risk group. The total point value matching the null value of the linear predictor is 165. Example: a 55-year-old patient with a KPS of 80 and a partly resected/IDH1 wild-type/MGMT-methylated tumor has a total prognostic score of 129 and is predicted to have a median survival of approximately 30 months and a 60% probability of surviving two years. This patient is assigned to the low-risk group. (B) Kaplan-Meier estimation of OS and PFS. M: methylated patients, UM: unmethylated patients, LR: low-risk patients, HR: high-risk patients, mo: month. The difference in survival between groups is reported (log-rank test p-value). The size and the median survival of each group are also specified.
Survival analysis of MGMT-methylated patients (population 2)
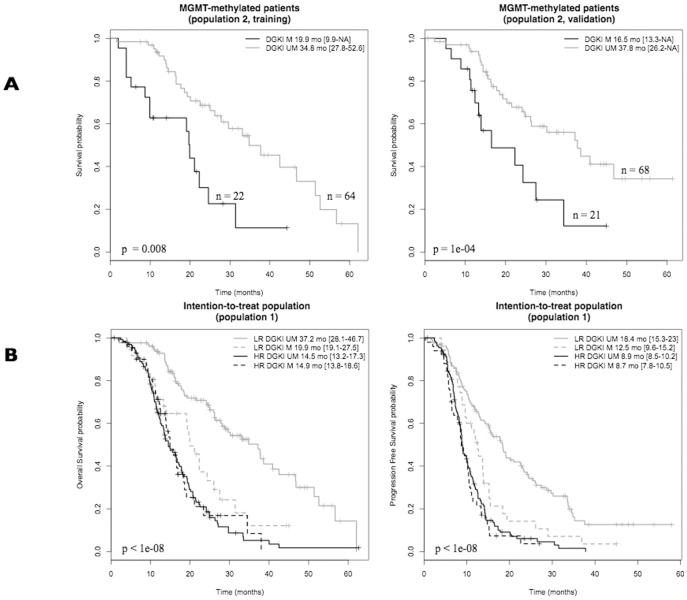
In population 2, univariate Cox analyses showed that age, KPS, and DGKI promoter methylation status were significantly associated with OS in both the training and validation cohorts (Table 2). In the multivariate Cox analyses, DGKI promoter methylation status was the only variable with a probability of inclusion higher than 90% in the training cohort. DGKI methylation status stratified the MGMT-methylated patients into two groups with significant differences in OS (19.9 months vs. 34.8 months, p = 0.008, 16.5 months vs. 37.8 months, p = 1e-4, training and validation, respectively, figure 2A). The MGMT %met was not significantly different (Student's t-test) between the DGKI-methylated and DGKI-unmethylated patients (p = 0.23).
Figure 2. Prognostic value of DGKI methylation status.
(A) MGMT-methylated GBM patients assigned to standard treatment (population 2). Kaplan-Meier estimation of OS in training and validation cohorts. (B) GBM patients assigned to standard treatment (population 1). Kaplan-Meier estimation of OS and PFS. M: methylated patients, UM: unmethylated patients, LR: low-risk patients, HR: high-risk patients, mo: month. The difference in survival between groups is reported (log-rank test p-value). The size and the median survival of each group are also specified.
The OS and PFS of the MGMT-methylated and DGKI-methylated patients were not significantly different from the OS and PFS of the MGMT-unmethylated patients (19.7 months vs. 14.9 months, 12.0 months vs. 9.0 months, OS and PFS, respectively, Figure S2).
Prognostic value of DGKI methylation status in risk groups (population 1)
The DGKI methylation status stratified the low-risk patients into two groups with significant differences in OS and PFS (37.2 months vs. 19.9 months, 18.4 months vs. 12.5 months, OS and PFS, respectively, figure 2B). The OS of low-risk and DGKI-methylated patients was not significantly different from the OS of high-risk patients (19.9 months vs. 14.9 months, p = 0.21). The DGKI methylation status did not stratify the subgroup of high-risk patients in the intention-to-treat population.
Discussion
We studied a retrospective cohort of 399 GBM patients homogeneously treated with the standard regimen. The higher OS at 6 and 12 months observed in our cohort in comparison to the reference cohort of the EORTC trial [16] (Table S1) can be explained by an improvement of surgical practices (55% of complete resection in our cohort vs. 39% in EORTC trial), continuation of standard treatment despite pseudoprogression, and an earlier and/or easier access to bevacizumab treatment at recurrence for patients progressing after 2007. This cohort was used to identify the main clinical prognostic factors and to design a nomogram intended to predict the survival time of an individual patient. A nomogram-based stratification of the cohort identified two risk groups (high/low) with significantly different median survival. In the low-risk group, the DGKI promoter methylation status identified poorly responding patients.
The prognostic factors identified in our study were age, KPS, extent of surgery, IDH1 mutational status, and MGMT promoter methylation status. This result is in agreement with the most consistently reported prognostic factors for GBM [2], [3], [4], [5], [6], [8]. From an individual patient's perspective, a nomogram offers a more tailored approach, taking into account their clinical characteristics. This can be of interest in patient counselling and in the design and interpretation of clinical trials. Therefore, we propose a nomogram based on the prognostic factors identified in our study. The nomogram can be used to predict an individual patient's median survival and probability of survival at two years. The DGKI methylation status was not included in this nomogram as it did not identify clinically relevant groups of patients in the intention-to-treat population. However, the interaction between MGMT and DGKI in a multivariate Cox model including all significant prognostic factors (age+KPS+surgery+IDH1+MGMT+DGKI+MGMT:DGKI) was significant (p = 0.0007). This indicated that the prognostic value of DGKI was to find in the context of the MGMT methylation status. A nomogram including this interaction can be found in Figure S3.
In 2008, Gorlia et al. proposed a nomogram for GBM patients who underwent either a partial or complete resection and were assigned to temozolomide and radiotherapy in the presence of a MGMT promoter methylation assessment (population 3 of the EORTC and NCIC trial 26981-22981/CE.3). Their nomogram includes MGMT promoter methylation status, Folstein Mini-Mental State Examination (MMSE) score, and WHO performance status [9]. We propose an updated version of this nomogram that includes not only MGMT promoter methylation status and Karnofsky performance score but also age, IDH1 mutational status, and extent of surgery. In the EORTC trial, elderly patients (>70 years) were excluded, and the prognostic value of IDH1 was not evident when the trial was designed. Furthermore, the authors discussed the restricted reliability of the extent of surgery in their study. Age and extent of surgery were nonetheless identified by Gorlia et al. in the population of GBM patients who underwent partial or complete resection and were assigned to temozolomide and radiotherapy without the knowledge of the MGMT promoter methylation status (population 2 of the EORTC trial). Because it was not routine to collect MMSE score in the neurosurgical units involved, we were unable to evaluate the prognostic value of these nomograms on our cohort. However, the nomogram proposed in the present study showed better performance evaluation (AUC) than MGMT status alone (0.71[0.65–0.78] vs. 0.65[0.59–0.71], p<1e-08). The potential skewing effect of treatment at recurrence on patient survival was not controlled; however, the validity of our PFS results indicated that our findings could be independent of these treatments. A recent study showed that the nomogram designed by Gorlia et al. for the intention-to-treat population (radiotherapy only or temozolomide and radiotherapy) was a poor predictor of an individual patient's survival because the standard of care has evolved since the EORTC trial [17]. Unfortunately, the nomograms proposed by Gorlia et al. for GBM patients who received the standard treatment (population 2 and population 3 of the EORTC trial) were not evaluated in the study by Parks et al. However, our study confirmed the appropriateness of Gorlia et al. findings as we also identified MGMT methylation status, performance status, age and extent of surgery in the nomogram for the population of GBM patients assigned to standard treatment.
A nomogram-based stratification of our cohort of primary GBM patients treated with the standard regimen identified two risk groups (high/low) with significantly different median survival. The low-risk group was almost exclusively composed of MGMT-methylated patients. Interestingly, our previous study showed that the methylation status of the DGKI promoter identified GBM patients with MGMT-methylated tumors who responded poorly to the standard regimen [10]. In this study, we have validated the prognostic value of DGKI methylation status for MGMT-methylated patients (population 2). However, this finding could be restricted by the limited size of the training and validation cohorts. We further evaluated the potential predictive value of DGKI methylation status on the intention-to-treat population (population 1). The methylation status of the DGKI promoter identified 22% of poorly responding patients in the low-risk group but had no prognostic value for high-risk patients. The role of DGKI and the functional consequences of its methylation status have never been investigated in gliomas but DGKI regulates Ras signalling, an oncogenic pathway frequently altered in GBM [11], [12]. Recently, Revill et al. showed that DGKI was hypermethylated in primary hepatocellular carcinoma and was re-expressed in liver cancer cell lines after exposure to reagents reversing DNA methylation [18]. This study suggests that DGKI expression is regulated by its promoter methylation. In GBM, we observed an anti-correlation between DGKI expression and methylation levels, in a private cohort and in the TCGA cohort (data not shown). Further functional studies on DGKI are clearly required.
Our results improve the conventional MGMT stratification of GBM patients receiving standard treatment. In particular, the DGKI methylation status identified poorly responding patients in the group of low-risk or MGMT-methylated patients. A retrospective study precluding the establishment of firm conclusions, these results need to be validated in a prospectively recruited cohort. They could however be of help in the interpretation of published or ongoing clinical trial outcomes and refine patient recruitment in the future.
Supporting Information
Primers and cycling conditions for the pyrosequencing analysis of DGKI_7.
(TIFF)
Prognostic value of DGKI methylation status for GBM patients assigned to standard treatment (population 1). Kaplan-Meier estimation of OS and PFS. M: methylated patients, UM: unmethylated patients, mo: month. The difference in survival between groups is reported (log-rank test p-value). The size and the median survival of each group are also specified.
(TIFF)
Nomogram including the interaction between MGMT and DGKI (population 1).
(TIFF)
OS ans PFS - % (95% IC).
(DOC)
Acknowledgments
We gratefully acknowledge the help of Dr Karima Mokhtari, Dr Sophie Michalack, Dr Audrey Rousseau, Dr Dan Christian, Dr Stephan Saikali, Dr Anne Clavreul and the Tumor Banks from Angers, Marseille, Paris, Poitiers and Rennes for their constant support in the collection, processing and histological analysis of tumor samples. We are most grateful to Frédérique Guénot, Cyrille Surbled, the Biogenouest Genomics core facility (Rennes Villejean, France) and the Genotyping GENTYANE core facility (Clermont-Ferrand, France) for their technical support. We thank Anaïs Peyre for her help in formatting the figures.
Data Availability
The authors confirm that, for approved reasons, some access restrictions apply to the data underlying the findings. Data are available upon request because the multicentric cohort is subjected to legal restrictions. To have access to the data, the readers may contact Pr. Jean Mosser (jean.mosser@univ-rennes1.fr).
Funding Statement
Ligue contre le Cancer foundation; European Union FEDER; COmité de la REcherche Clinique COREC du CHU de Rennes; INCa DGOS-Inserm 6038; Région Bretagne. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Wen PY, Kesari S (2008) Malignant gliomas in adults. N Engl J Med 359: 492–507. [DOI] [PubMed] [Google Scholar]
- 2. Siker ML, Wang M, Porter K, Nelson DF, Curran WJ, et al. (2011) Age as an independent prognostic factor in patients with glioblastoma: a Radiation Therapy Oncology Group and American College of Surgeons National Cancer Data Base comparison. J Neurooncol 104: 351–356. [DOI] [PubMed] [Google Scholar]
- 3. Stummer W, van den Bent MJ, Westphal M (2011) Cytoreductive surgery of glioblastoma as the key to successful adjuvant therapies: new arguments in an old discussion. Acta Neurochir (Wien) 153: 1211–1218. [DOI] [PubMed] [Google Scholar]
- 4. Filippini G, Falcone C, Boiardi A, Broggi G, Bruzzone MG, et al. (2008) Prognostic factors for survival in 676 consecutive patients with newly diagnosed primary glioblastoma. Neuro Oncol 10: 79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ichimura K, Pearson DM, Kocialkowski S, Backlund LM, Chan R, et al. (2009) IDH1 mutations are present in the majority of common adult gliomas but rare in primary glioblastomas. Neuro Oncol 11: 341–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, et al. (2009) IDH1 and IDH2 mutations in gliomas. N Engl J Med 360: 765–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sanson M, Marie Y, Paris S, Idbaih A, Laffaire J, et al. (2009) Isocitrate dehydrogenase 1 codon 132 mutation is an important prognostic biomarker in gliomas. J Clin Oncol 27: 4150–4154. [DOI] [PubMed] [Google Scholar]
- 8. Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, et al. (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10: 459–466. [DOI] [PubMed] [Google Scholar]
- 9. Gorlia T, van den Bent MJ, Hegi ME, Mirimanoff RO, Weller M, et al. (2008) Nomograms for predicting survival of patients with newly diagnosed glioblastoma: prognostic factor analysis of EORTC and NCIC trial 26981-22981/CE.3. Lancet Oncol 9: 29–38. [DOI] [PubMed] [Google Scholar]
- 10. Etcheverry A, Aubry M, de Tayrac M, Vauleon E, Boniface R, et al. (2010) DNA methylation in glioblastoma: impact on gene expression and clinical outcome. BMC Genomics 11: 701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Regier DS, Higbee J, Lund KM, Sakane F, Prescott SM, et al. (2005) Diacylglycerol kinase iota regulates Ras guanyl-releasing protein 3 and inhibits Rap1 signaling. Proc Natl Acad Sci U S A 102: 7595–7600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. The Cancer Genome Atlas Network (2008) Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 455: 1061–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kang MR, Kim MS, Oh JE, Kim YR, Song SY, et al. (2009) Mutational analysis of IDH1 codon 132 in glioblastomas and other common cancers. Int J Cancer 125: 353–355. [DOI] [PubMed] [Google Scholar]
- 14. Turcan S, Rohle D, Goenka A, Walsh LA, Fang F, et al. (2012) IDH1 mutation is sufficient to establish the glioma hypermethylator phenotype. Nature 483: 479–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Quillien V, Lavenu A, Karayan-Tapon L, Carpentier C, Labussiere M, et al.. (2012) Comparative assessment of 5 methods (methylation-specific polymerase chain reaction, methylight, pyrosequencing, methylation-sensitive high-resolution melting, and immunohistochemistry) to analyze O6-methylguanine-DNA-methyltranferase in a series of 100 glioblastoma patients. Cancer. [DOI] [PubMed]
- 16. Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, et al. (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352: 987–996. [DOI] [PubMed] [Google Scholar]
- 17.Parks C, Heald J, Hall G, Kamaly-Asl I (2013) Can the prognosis of individual patients with glioblastoma be predicted using an online calculator? Neuro Oncol. [DOI] [PMC free article] [PubMed]
- 18.Revill K, Wang T, Lachenmayer A, Kojima K, Harrington A, et al. (2013) Genome-wide methylation analysis and epigenetic unmasking identify tumor suppressor genes in hepatocellular carcinoma. Gastroenterology 145: : 1424–1435 e1421–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Primers and cycling conditions for the pyrosequencing analysis of DGKI_7.
(TIFF)
Prognostic value of DGKI methylation status for GBM patients assigned to standard treatment (population 1). Kaplan-Meier estimation of OS and PFS. M: methylated patients, UM: unmethylated patients, mo: month. The difference in survival between groups is reported (log-rank test p-value). The size and the median survival of each group are also specified.
(TIFF)
Nomogram including the interaction between MGMT and DGKI (population 1).
(TIFF)
OS ans PFS - % (95% IC).
(DOC)
Data Availability Statement
The authors confirm that, for approved reasons, some access restrictions apply to the data underlying the findings. Data are available upon request because the multicentric cohort is subjected to legal restrictions. To have access to the data, the readers may contact Pr. Jean Mosser (jean.mosser@univ-rennes1.fr).